Marginal and Para-Marginal Technique in Late Germectomy of Lower Third Molars
Abstract
1. Introduction
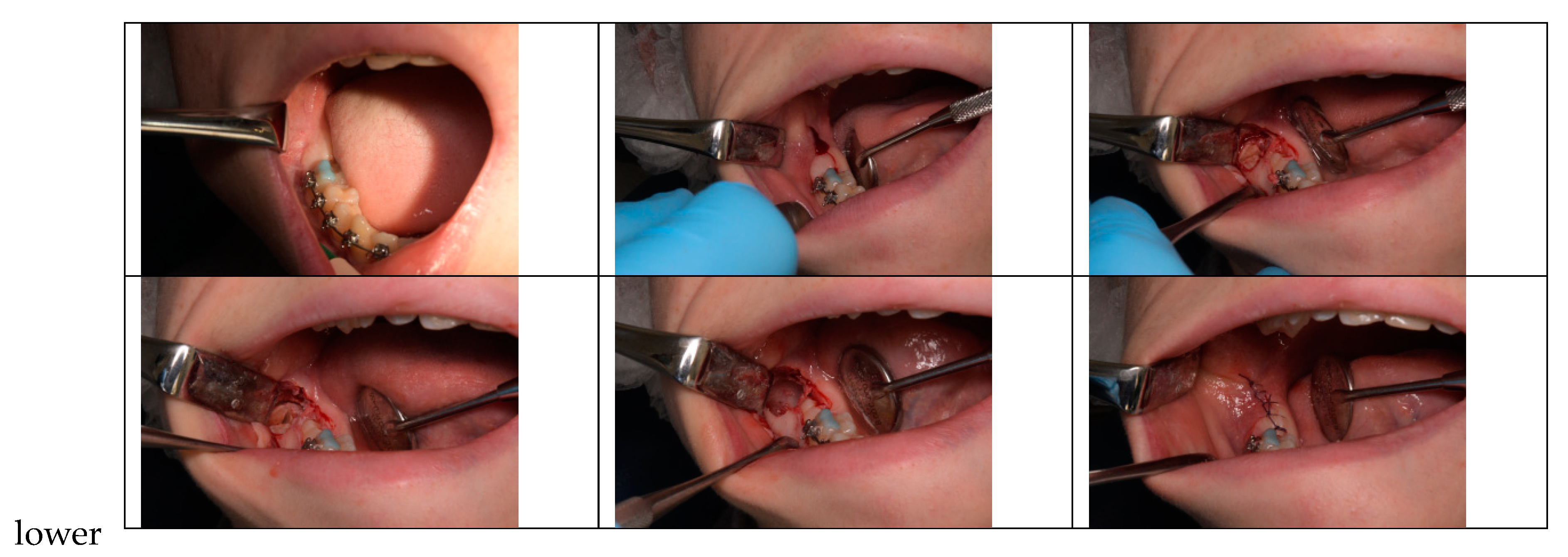
2. Materials and Methods
3. Results
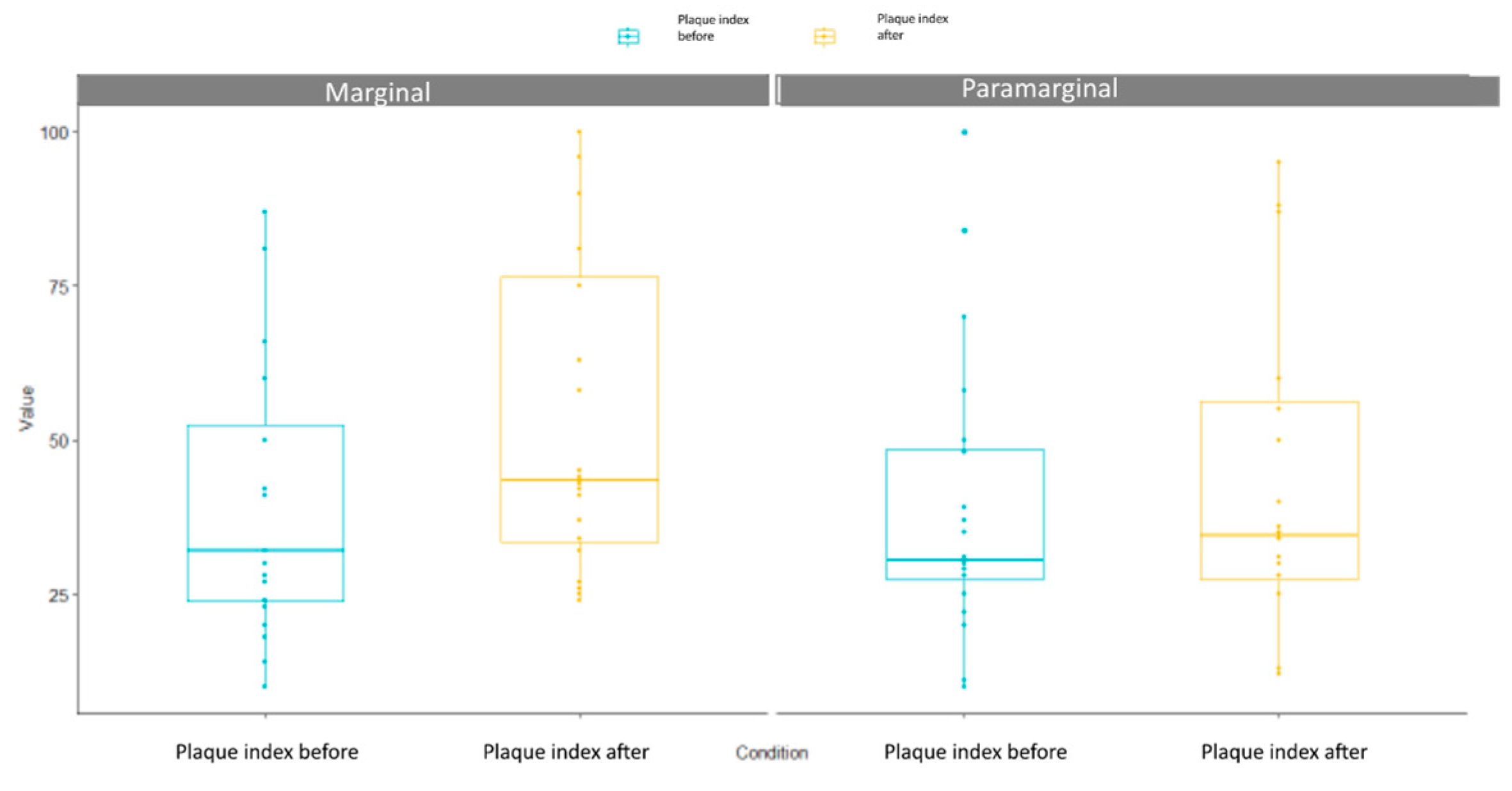
3.1. Plaque Index
3.2. BoP Index
3.3. Maximum Mouth Opening Index
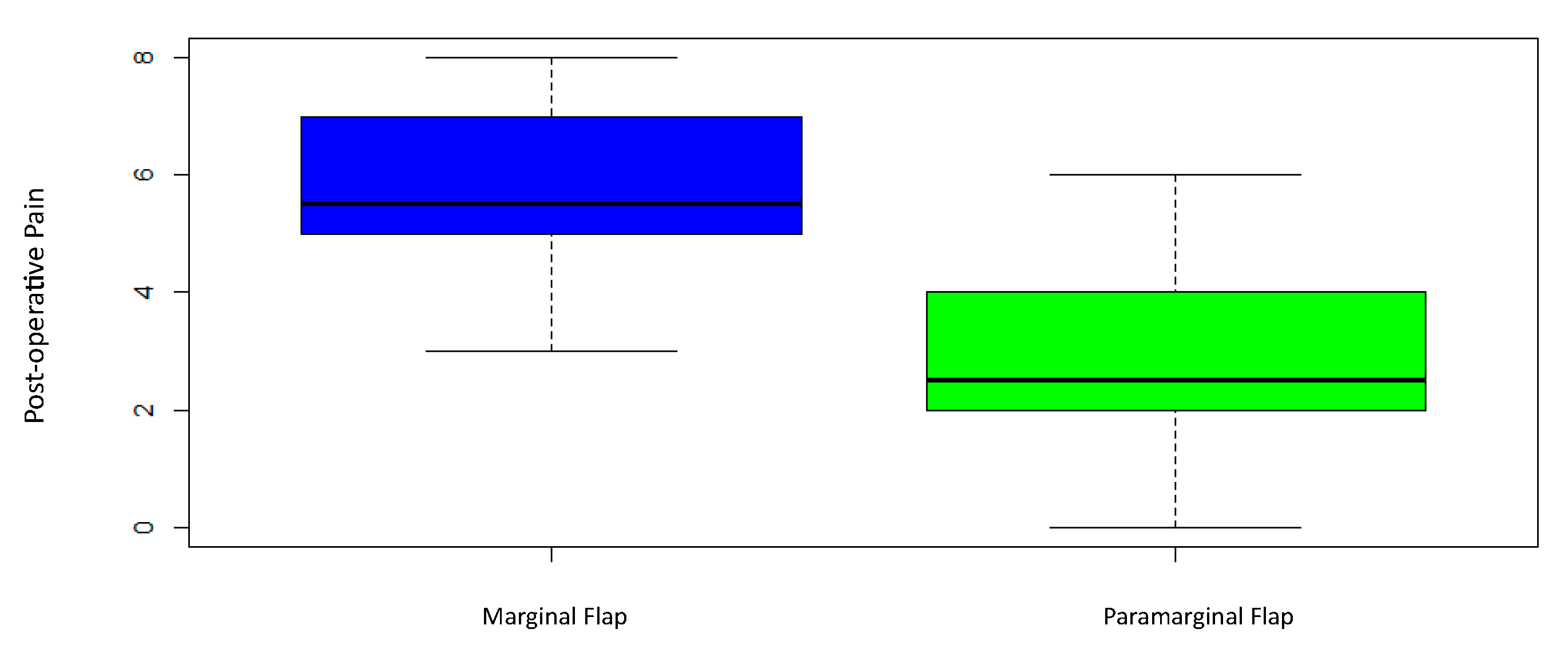
3.4. Post-Operative Pain Perception
3.5. Post-Operative Swelling
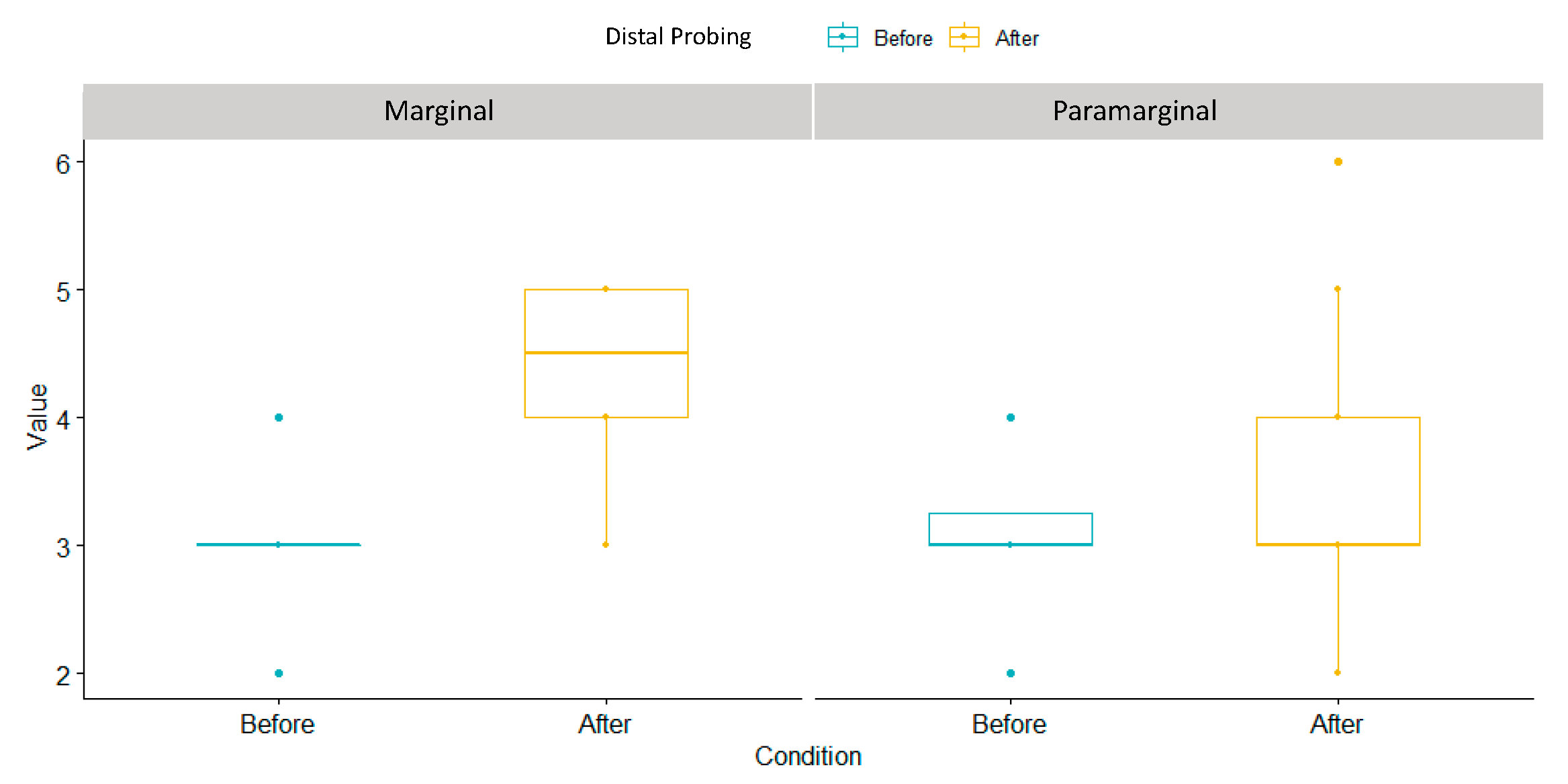
3.6. Distal Probing
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Garn, S.M.; Lewis, A.B.; Vicinus, J.H. Third molar polymorphism and its significance to dental genetics. J. Dent. Res. 1963, 42, 1344–1363. [Google Scholar] [CrossRef] [PubMed]
- Richardson, M. Impacted third molars. Br. Dent. J. 1995, 178, 92. [Google Scholar] [CrossRef] [PubMed]
- Seward, G.R.; Harris, M.; McGowan, D.A. (Eds.) An Outline of Oral Surgery I; Wright: Oxford, UK, 1999; pp. 52–92. [Google Scholar]
- Peñarrocha-Diago, M.; Camps-Font, O.; Sánchez-Torres, A.; Figueiredo, R.; Sánchez-Garcés, M.A.; Gay-Escoda, C. Indications of the extraction of symptomatic impacted third molars: A systematic review. J. Clin. Exp. Dent. 2021, 13, e278–e286. [Google Scholar] [CrossRef]
- Ghaeminia, H.; Nienhuijs, M.E.; Toedtling, V.; Perry, J.; Tummers, M.; Hoppenreijs, T.J.; Van der Sanden, W.J.; Mettes, T.G. Surgical removal versus retention for the management of asymptomatic disease-free impacted wisdom teeth. Cochrane Database Syst. Rev. 2020, 5, CD003879. [Google Scholar] [CrossRef] [PubMed]
- Mazur, M.; Ndokaj, A.; Marasca, B.; Sfasciotti, G.L.; Marasca, R.; Bossù, M.; Ottolenghi, L.; Polimeni, A. Clinical Indications to Germectomy in Pediatric Dentistry: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 740. [Google Scholar] [CrossRef]
- Sbricoli, L.; Cerrato, A.; Frigo, A.C.; Zanette, G.; Bacci, C. Third Molar Extraction: Irrigation and Cooling with Water or Sterile Physiological Solution: A Double-Blind Randomized Study. Dent. J. 2021, 9, 40. [Google Scholar] [CrossRef]
- Staderini, E.; Patini, R.; Guglielmi, F.; Camodeca, A.; Gallenzi, P. How to Manage Impacted Third Molars: Germectomy or Delayed Removal? A Systematic Literature Review. Medicina 2019, 55, 79. [Google Scholar] [CrossRef]
- Angelo, C.; Nicole, P.C.; Garg, A.K. Early Third Molar Extraction: When Germectomy Is the Best Choise. Interv. Pediatr. Dent. Open Access J. 2020, 4, 350–353. [Google Scholar] [CrossRef]
- Lysell, L.; Rohlin, M. A study of indications used for removal of mandibular third molar. Int. J. Oral Maxillofac. Surg. 1988, 17, 161–164. [Google Scholar] [CrossRef]
- Chen, Y.-W.; Lee, C.-T.; Hum, L.; Chuang, S.-K. Effect of flap design on periodontal healing after impacted third molar extraction: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2017, 46, 363–372. [Google Scholar] [CrossRef]
- Woolf, R.H.; Malmquist, J.P.; Wright, W.H. Third molar extractions: Periodontal implication of two flap designs. Gen. Dent. 1978, 26, 52–56. [Google Scholar]
- Shofield, I.D.; Kogon, S.L.; Donner, A. Long-term comparison of two surgical flap designs for third molar surgery on the health of the periodontal tissue of the second molar tooth. J. Can. Dent. Assoc. 1988, 54, 689–691. [Google Scholar]
- Suarez-Cunqueiro, M.M.; Gutwald, R.; Reichman, J.; Otero-Cepeda, X.L.; Schmelzeisen, R. Marginal flap versus paramarginal flap in impacted third molar surgery: A prospective study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2003, 95, 403–408. [Google Scholar] [CrossRef]
- Shahzad, M.A.; Chatha, M.R.; Sohail, A. Outcome of management of mandibular third molar impaction by comparing two different flap designs. Pak. Oral Dent. J. 2014, 34, pp. 235–238. Available online: https://Link.gale.com/apps/doc/A381474429/AONE?u=anon~19344d62&sid=googleScholar&xid=96bb8df2 (accessed on 20 February 2023).
- Shahzad, M.A.; Munir, M.F.; Chatha, M.R.; Sohail, A. Effect of two triangular flap designs for removal of impacted third molar on maximal mouth opening. Pak. Oral Dent. J. 2015, 35, 190. [Google Scholar]
- Köşger, H.; Polat, H.B.; Demirer, S.; Ozdemir, H.; Ay, S. Periodontal healing of marginal flap versus paramarginal flap in palatally impacted canine surgery: A prospective study. J. Oral Maxillofac. Surg. 2009, 67, 1826–1831. [Google Scholar] [CrossRef]
- Ottria, L.; Luciani, F.; Piva, P.; Alagna, A.M.; Arcuri, C.; Bartuli, F.N. The flap recovery on the impacted lower third molar surgery comparing 3 different flap designs: A clinical study. Oral Implantol. 2017, 10, 270–275. [Google Scholar] [CrossRef]
- Barbato, L.; Kalemaj, Z.; Buti, J.; Baccini, M.; La Marca, M.; Duvina, M.; Tonelli, P. Effect of Surgical Intervention for Removal of Mandibular Third Molar on Periodontal Healing of Adjacent Mandibular Second Molar: A Systematic Review and Bayesian Network Meta-Analysis. J. Periodontol. 2016, 87, 291–302. [Google Scholar] [CrossRef]
- Jakse, N.; Bankaoglu, V.; Wimmer, G.; Eskici, A.; Pertl, C. Primary wound healing after lower third molar surgery: Evaluation of 2 different flap designs. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 93, 7–12. [Google Scholar] [CrossRef]
- Shevel, E.; Koepp, W.G.; Butow, K.W. A subjective assessment of pain and swelling following the surgical removal of impacted third molar teeth using different surgical techniques. SADJ 2001, 56, 238–241. [Google Scholar]
- Glera-Suárez, P.; Soto-Peñaloza, D.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M. Patient morbidity after impacted third molar extraction with different flap designs. A systematic review and meta-analysis. Med. Oral Patol. Oral y Cirugía Buccal 2020, 25, e233–e239. [Google Scholar] [CrossRef] [PubMed]
- de Marco, G.; Lanza, A.; Cristache, C.M.; Capcha, E.B.; Espinoza, K.I.; Rullo, R.; Vernal, R.; Cafferata, E.A.; di Francesco, F. The influence of flap design on patients’ experiencing pain, swelling, and trismus after mandibular third molar surgery: A scoping systematic review. J. Appl. Oral Sci. 2021, 29, e20200932. [Google Scholar] [CrossRef] [PubMed]
- Garcia Garcia, A.; Gude Sampedro, F.; Gandara Rey, J.; Gallas Torreira, M. Trismus and pain after removal of impacted lower third molars. J. Oral Maxillofac. Surg. 1997, 55, 1223–1226. [Google Scholar] [CrossRef] [PubMed]
- Rivera-Herrera, R.S.; Esparza-Villalpando, V.; Bermeo-Escalona, J.R.; Martínez-Rider, R.; Pozos-Guillén, A. Agreement analysis of three mandibular third molar retention classifications. Gac. Med. Mex. 2020, 156, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Karaca, I.; Şimşek, Ş.; Uğar, D.; Bozkaya, S. Review of flap design influence on the health of the periodontium after mandibular third molar surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 104, 18–23. [Google Scholar] [CrossRef]
- do Nascimento-Júnior, E.M.; Dos Santos, G.M.S.; Tavares Mendes, M.L.; Cenci, M.; Correa, M.B.; Pereira-Cenci, T.; Martins-Filho, P.R.S. Cryotherapy in reducing pain, trismus, and facial swelling after third-molar surgery: Systematic review and meta-analysis of randomized clinical trials. J. Am. Dent. Assoc. 2019, 150, 269–277.e1. [Google Scholar] [CrossRef]
- Duarte de Oliveira, F.J.; Brasil, G.M.L.C.; Araújo Soares, G.P.; Fernandes Paiva, D.F.; de Assis de Souza Júnior, F. Use of low-level laser therapy to reduce postoperative pain, edema, and trismus following third molar surgery: A systematic review and meta-analysis. J. Craniomaxillofac. Surg. 2021, 49, 1088–1096. [Google Scholar] [CrossRef]
- Passarelli, P.C.; Lopez, M.A.; Netti, A.; Rella, E.; Leonardis, M.; Svaluto Ferro, L.; Lopez, A.; Garcia-Godoy, F.; D’Addona, A. Effects of Flap Design on the Periodontal Health of Second Lower Molars after Impacted Third Molar Extraction. Healthcare 2022, 10, 2410. [Google Scholar] [CrossRef]
- Low, S.H.; Lu, S.L.; Lu, H.K. Evidence-based clinical decision making for the management of patients with periodontal osseous defect after impacted third molar extraction: A systematic review and meta-analysis. J. Dent. Sci. 2021, 16, 71–84. [Google Scholar] [CrossRef]
- Hassan, K.S.; Marei, H.F.; Alagl, A.S. Does grafting of third molar extraction sockets enhance periodontal measures in 30- to 35-year-old patients? J. Oral Maxillofac. Surg. 2012, 70, 757–764. [Google Scholar] [CrossRef]


| Flap Design | Min | Median | Mean | Variance | Standar Deviation | Max | p-Value |
|---|---|---|---|---|---|---|---|
| Marginal | 2 | 12.5 | 13.3 | 106 | 10.3 | 49 | 0.001264 |
| Paramarginal | −5 | 3 | 3.85 | 35.6 | 5.97 | 18 |
| Pre-Surgical BoP | Flap Design | n | prop |
|---|---|---|---|
| No bleeding | Marginal | 13 | 65% |
| No bleeding | Paramarginal | 11 | 55% |
| Bleeding | Marginal | 7 | 35% |
| Bleeding | Paramarginal | 9 | 45% |
| Post-surgical Bop | Flap design | n | prop |
| No bleeding | Marginal | 1 | 5% |
| No bleeding | Paramarginal | 14 | 70% |
| Bleeding | Marginal | 19 | 95% |
| Bleeding | Paramarginal | 6 | 30% |
| Flap Design | Min | Median | Mean | Variance | Standar Deviation | Max | p-Value |
|---|---|---|---|---|---|---|---|
| Marginal | −8 | −3 | −3.5 | 3.32 | 1.82 | 0 | 0.001264 |
| Paramarginal | −6 | −0.5 | −0.7 | 4.75 | 2.18 | 3 |
| Flap Design | Min | Median | Mean | Variance | Standar Deviation | Max | p-Value |
|---|---|---|---|---|---|---|---|
| Marginal | 3 | 5.5 | 5.75 | 1.88 | 1.37 | 8 | 0.000005 |
| Paramarginal | 0 | 2.5 | 2.95 | 3.73 | 1.93 | 6 |
| Post-Operative Swelling | Flap Design | n | prop |
|---|---|---|---|
| No | Paramarginal | 11 | 55% |
| Yes | Paramarginal | 9 | 45% |
| Yes | Marginal | 20 | 100% |
| Flap Design | Min | Median | Mean | Variance | Standar Deviation | Max | p-Value |
|---|---|---|---|---|---|---|---|
| Marginal | 1 | 1 | 1.3 | 0.221 | 0.47 | 2 | 0.0000275 |
| Paramarginal | −1 | 0 | 0.4 | 0.463 | 0.681 | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ludovichetti, F.S.; Mazzoleni, S.; Menin, M.; Parcianello, R.G.; Romanowski, F.; Stellini, E.; Zuccon, A. Marginal and Para-Marginal Technique in Late Germectomy of Lower Third Molars. Children 2023, 10, 1077. https://doi.org/10.3390/children10061077
Ludovichetti FS, Mazzoleni S, Menin M, Parcianello RG, Romanowski F, Stellini E, Zuccon A. Marginal and Para-Marginal Technique in Late Germectomy of Lower Third Molars. Children. 2023; 10(6):1077. https://doi.org/10.3390/children10061077
Chicago/Turabian StyleLudovichetti, Francesco Saverio, Sergio Mazzoleni, Manuel Menin, Roberta Gaia Parcianello, Francielle Romanowski, Edoardo Stellini, and Andrea Zuccon. 2023. "Marginal and Para-Marginal Technique in Late Germectomy of Lower Third Molars" Children 10, no. 6: 1077. https://doi.org/10.3390/children10061077
APA StyleLudovichetti, F. S., Mazzoleni, S., Menin, M., Parcianello, R. G., Romanowski, F., Stellini, E., & Zuccon, A. (2023). Marginal and Para-Marginal Technique in Late Germectomy of Lower Third Molars. Children, 10(6), 1077. https://doi.org/10.3390/children10061077







