Abstract
Kidney transplantation is the preferred treatment for end-stage renal failure, but the limited availability of donors and the risk of immune rejection pose significant challenges. Early detection of acute renal rejection is a critical step to increasing the lifespan of the transplanted kidney. Investigating the clinical, genetic, and histopathological markers correlated to acute renal rejection, as well as finding noninvasive markers for early detection, is urgently needed. It is also crucial to identify which markers are associated with different types of acute renal rejection to manage treatment effectively. This short review summarizes recent studies that investigated various markers, including genomics, histopathology, and clinical markers, to differentiate between different types of acute kidney rejection. Our review identifies the markers that can aid in the early detection of acute renal rejection, potentially leading to better treatment and prognosis for renal-transplant patients.
1. Introduction
Kidney transplantation is a superior treatment to dialysis for individuals with chronic kidney disease or end-stage renal failure, boasting up to 97% survival rates for transplanted kidneys within one year []. Nevertheless, a significant hurdle is the limited availability of donors, mainly due to the risk of immune rejection. When genetically dissimilar donor tissue is transplanted, the recipient’s immune system may perceive it as foreign, leading to potential graft rejection [].
Lymphocytes, essential white blood cells, are vital components of the adaptive immune response, with B-cells producing pathogen-specific antibodies and T-cells capable of killing infected cells or seeking support from other cells []. The interaction between the innate and adaptive immune systems defends the body against foreign pathogens and abnormal cells [,]. Recent advancements in technology have enabled personalized immunosuppressive therapies based on recipient-specific biomarkers related to immune response activation []. Toll-like receptors (TLRs) are extensively studied pattern-recognition receptors (PRRs) that play a critical role in initiating innate responses and guiding adaptive immunity []. They are expressed in various hemopoietic cells, including DCs, B-cells, mast cells, T-cells, and endothelial cells. Their stimulation leads to the activation of transcription factors NF-KB and AP-1, which subsequently induce the transcription of inflammation-related genes. This results in the production of proinflammatory cytokines, chemokines, antimicrobial peptides, adhesion molecules, enhanced antigen presentation, and increased expression of costimulatory molecules in APCs. The intricate interplay among these components significantly influences the immune response against transplanted organs and tissues, ultimately impacting the rejection outcome [].
Acute renal rejection, classified based on histopathological and immunological characteristics, has distinct forms []. Hyperacute rejection is a severe type that occurs suddenly within minutes of transplant [], but it is rare due to successful prevention through tissue cross-matching. Acute rejection can happen at any time after transplantation and includes antibody-mediated rejection (ABMR) and T-cell-mediated rejection (TCMR). ABMR involves immunological damage caused by antibodies and donor-specific alloantibodies in circulation, while TCMR results in lymphocytic infiltration affecting the interstitium, tubules, and sometimes the artery intima. Tubular injury markers differentiate between ABMR and TCMR based on specific histological features. For instance, TCMR is characterized by mononuclear tubulitis and interstitial inflammation, while ABMR exhibits microvascular inflammation, arteritis, acute tubular injury, or thrombotic microangiopathy. Additionally, the presence of complement component C4d in peritubular capillaries indicates the antibody–endothelium interaction in ABMR, although its reproducibility is poor and staining results may vary [].
The prohibitive expense of postsurgical maintenance, amounting to thousands of dollars per month for antirejection medications, presents a significant challenge for some patients []. Untreated rejection can lead to major health problems []. To address this issue and enhance transplant outcomes, early detection of renal rejection through innovative biomarkers is essential []. These markers include histological, clinical, and genetic indicators. While biopsy remains the gold standard, from these markers, clinical biomarkers such as KIM-1 and CXCL-10 show potential for early diagnosis and prognosis prediction of renal rejection [].
The aim of this short review is to provide an overview of the current state of biomarkers for acute renal rejections and their correlation with the type of acute renal rejections (refer to Figure 1). In addition, we will highlight which markers are noninvasive and may lead to the development of new noninvasive technology for the early detection of acute renal rejection and its associated type.
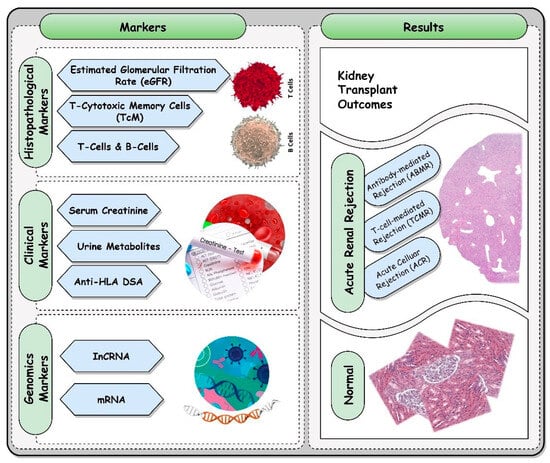
Figure 1.
A brief overview of different markers utilized in the early identification of acute renal rejection.
This review presents the state of the art regarding markers used to detect renal rejection. It is structured as follows: Section 2 provides an overview of studies utilizing histopathological markers, Section 3 discusses studies employing clinical markers, and Section 4 examines studies using genetic markers. The review highlights the strengths and limitations of the reviewed studies in Section 5 and presents overall conclusions and future research directions in Section 6. Data regarding the three types of markers and their usage for determining renal rejection were collected through a search of articles over the last decade.
2. Extraction of RNA and Clinical Markers from Histological Samples
Histopathological markers refer to changes in tissue structure that are observed through a microscope, and they aid in identifying and monitoring renal-transplant rejection. These markers offer valuable insights into the cellular and molecular changes that occur during rejection and can be challenging to detect with clinical markers alone []. The presence of infiltrating lymphocytes, which can be detected through a biopsy sample taken from the transplanted kidney, is one of the most commonly used histopathological markers of renal rejection. It indicates an active immune reaction against the grafted tissue. The severity of rejection can be graded based on the number and distribution of infiltrating lymphocytes, with higher numbers indicating more severe rejection [,]. Other histopathological markers of renal rejection include changes in the capillary basement membrane, alterations in the glomerular filtration barrier, and modifications in the tubulointerstitium. These changes may indicate acute tissue injury and early lesions of endothelial injury and can be visualized using light microscopy or electron microscopy [].
Table 1 utilizes histopathological measures and immune markers to identify acute renal rejection and confirm the effectiveness of the selected markers. A study conducted by Arai et al. [] used light and electron microscopy to detect histological evidence of acute tissue and endothelial injury in 269 kidney-transplant recipients. The results showed no worsening of clinical or microscopic features in patients with short-term follow-up. Similarly, in a cross-sectional study, Garcia-Covarrubias et al. [] examined the levels of interleukin in urine samples and biopsies from 37 kidney-transplant recipients, including both rejected and nonrejected patients, as well as a group of healthy individuals. The primary objective of the study was to determine whether there were any variations in interleukin expression levels across the groups. However, when comparing the transplant patients who had been rejected and those who had not with the healthy group, the interleukin analysis did not show any appreciable differences. The findings of both studies raise questions about the reliability and significance of these markers in predicting rejection outcomes.

Table 1.
A review of the existing literature regarding histopathological markers used to anticipate acute rejection in patients.
In their meta-analysis, Eiamsitrakoon et al. [] aimed to investigate the effect of the IFNG rs2430561 gene on the likelihood of acute rejection in transplant patients. The study found a significant increase in the risk of rejection in only the black subgroup. However, the results were deemed weak due to a low sample size and a wide confidence interval. Rohan et al. [] conducted a study to assess the efficacy of allospecific CD154+ TcM in 22 individuals who received kidney transplants. Out of the 22 patients, 6 experienced TCMR and 7 showed ABMR. Among the 11 patients who tested positive, 6 experienced acute cellular rejection (ACR) or antibody-mediated rejection (ABMR), whereas 10 out of the 11 patients who tested negative did not encounter rejection.
Shimizu et al. [] analyzed 22 renal-allograft-biopsy specimens from 20 transplant recipients to investigate the clinical and pathological significance of borderline changes (BCs) after transplantation. BC was diagnosed around 500 days post-transplantation and was characterized by tubulitis, interstitial inflammation, peritubular capillaritis, and varying degrees of interstitial fibrosis and tubular atrophy. Glomerulitis and intimal arteritis were not observed. While no graft loss occurred, 45% of patients experienced deterioration in renal-allograft function. The findings highlight the importance of monitoring and treating BCs appropriately. A cross-sectional study by Zhuang et al. [] aimed to evaluate B-cell subsets in immunologically stable renal-transplant patients and those with end-stage renal disease (ESRD). Flow cytometry was used to analyze B-cell subsets in 73 stable transplant recipients, 35 ESRD patients, and 36 healthy volunteers. The findings revealed lower percentages of total B-cells and regulatory B-cells in transplant recipients compared to healthy controls. Transitional and marginal-zone B-cells were also reduced in transplant recipients compared to ESRD patients and healthy volunteers. ESRD patients exhibited higher percentages of plasma cells. Overall, B-cell subsets differed significantly between immunologically stable renal-transplant recipients and healthy controls, with minimal differences observed between ESRD patients and transplant recipients.
Mueller et al. [] conducted an RNA sequencing study on 34 kidney allograft biopsies to investigate differences between normal biopsies and those exhibiting T-cell-mediated rejection. The study revealed that biopsies with T-cell-mediated rejection had higher mRNA levels for pattern-recognition receptors and calcineurin, indicating reduced immunosuppression compared to healthy biopsies. Nowanska et al. [] used immunohistochemistry techniques to examine the presence of endothelin receptors (ETARs) in 162 kidney-transplant-biopsy samples. The study found that patients who tested positive for ETARs had a higher rate of graft loss one year after the biopsy, but the findings were not statistically significant.
De Leur et al. [] explored the control of B-cell-mediated immunity in acute T-cell-mediated rejection by examining 15 biopsy samples from kidney-transplant recipients. The study found that 40% of the biopsies contained dense cellular aggregates. Biopsies displaying acute T-cell-mediated rejection (aTCMRI) had these clusters in 80% of cases, while the aTCMRII and a/aABMR groups only exhibited them in 20% of cases. Wu et al. [] performed a study that employed single-cell RNA sequencing to identify and classify different cell types and conditions present in a human kidney biopsy. The study examined 8746 individual cell transcriptomes from a healthy adult kidney and a solitary kidney transplant. Upon histological inspection, the biopsy of the transplant exhibited acute T-cell-mediated rejection with plasma cells evaluated as Banff 1B, along with acute C4d-negative antibody-mediated rejection (ABMR).
McRae et al. [] investigated the expression of CD4+ CD25+/CD39+ in the peripheral blood of 17 end-stage renal-failure patients. The study found that patients with acute T-cell-mediated rejection had lower levels of CD4+ CD25+/CD39+ mTreg and CD4+ CD25+ CD39+ mTeff cells compared to nonrejected patients as determined by flow cytometry analysis. The objective of Jiang et al. [] was to identify CD20-positive B-cell effectiveness in biopsy specimens from 216 patients. The findings indicated that, out of the total participants, 83 patients were categorized as belonging to the CD20-negative group, while 133 patients were classified as part of the CD20-positive group.
Sentis et al. [] aimed to predict graft failure that is censored for death by examining the count of CD68+ macrophage glomerular cells during an incident of acute rejection in 57 patients who underwent renal transplantation. The study found that 42% of patients who experienced acute rejection lost their graft after a median of 1236 days, and concluded that CD68+ macrophage cell count can predict graft failure that is censored for death. Matingon et al. [] conducted research on 43 kidney-transplant-biopsy samples to assess the alloimmune responses of Th-17. Using molecular analysis, the study identified patients who expressed mRNA IL17 but had low-mRNA Foxp3 expression. These patients had a much higher rate of treatment failure (87.5%) compared to those who did not express mRNA IL17 or had high-mRNA Foxp3 expression (26.7%, p = 0.017).
Visona et al. [] investigated the role of lymphomononuclear inflammation (nephritis) in kidney transplants and were involved in the analysis of 113 kidney-transplant biopsies.
According to the study, 66 cases (58.4%) of the analyzed kidney-transplant biopsies had nephritis in both the medulla and cortex, while 47 cases (41.6%) showed nephritis exclusively in the medulla. The findings indicate that the existence of medullary nephritis in kidney-transplant biopsies could indicate the occurrence of acute cellular rejection. Lee et al. [] examined the effect of anti-AT1R antibodies on renal-allograft rejection by analyzing 53 patients who were diagnosed with rejection through biopsy. This included 22 patients with antibody-mediated rejection, 29 with T-cell-mediated rejection, and 2 with mixed rejection. According to the study, anti-AT1Rs were detected in 9.4% of the patients who experienced rejection, and this was strongly linked with HLA class-I DSAs.
Crespo et al. [] investigated the connection between peripheral blood NK-cell subsets, clinical characteristics, and circulating anti-HLA antibodies (DSAs and non-DSAs) in a group of 393 recipients of renal allografts. After performing multivariate analysis, the study found that patients without detectable anti-HLA antibodies had lower levels of NK cells but had a more significant rise in CD56 bright and NKG2A+ subsets, particularly in cases with DSAs. In a separate study, Bhat et al. [] aimed to examine the function of p-S6RP plasma cells in instances of acute renal-allograft rejection. The research involved analyzing a group of 28 patients to determine their response to antirejection treatment, measured by the serum creatinine ratio. The findings revealed that patients with high-p-S6RP staining had a significantly higher creatinine ratio compared to those with low-p-S6RP staining, indicating a less favorable response to treatment. These outcomes suggest that p-S6RP plasma cells play a role in acute rejection.
De Vos et al. [] examined the monitoring of de novo DSAs (dDSAs) in a substantial group of renal-transplant recipients from multiple ethnicities. Through a nested case-control study, the research found that, among the 503 recipients, 24% developed dDSAs, with 73% of those individuals having dDSAs directed against the DQ antigen. Recipients with dDSA had a greater probability of encountering various types of acute rejection, such as antibody-mediated acute rejection (16%), acute rejection caused by noncompliance (8%), and recurrent acute rejection (6%), compared to those without dDSAs. Additionally, they had a higher chance of experiencing acute rejection overall (35%). In another study by Zhao et al. [], the mechanism by which CD4+ T-cells secrete sFGL2 in the onset of acute rejection was explored in a sample of 40 cases. The study concluded that renal-allograft recipients with acute rejection confirmed through biopsy had significantly higher levels of sFGL2, TNF-α, IFN-γ, and CD4+ T-cells in their peripheral blood.
Ge et al. [] conducted a meta-analysis on 525 cases of acute renal-allograft rejection to investigate the correlation between the IFNG +874 T > A polymorphism and susceptibility to AR. The research found a significant association between possessing the T allele and increased susceptibility to AR. The correlation was particularly notable in Caucasians and individuals who received a kidney transplant from a cadaveric donor. Another study by Loupy et al. [] explored the relationship between the ability of anti-HLA antibodies to bind to complement and kidney-transplant failure. The study analyzed 1016 patients for circulating anti-HLA antibodies and revealed that patients with anti-HLA antibodies capable of binding to the complement had a much lower rate of graft survival (54%) compared to those without these antibodies (93–94%).
Li et al. [] investigated the use of immunophenotyping to distinguish between BK virus nephropathy and acute rejection in 65 kidney-transplant recipients. The study found that quantities of CD3, CD4, CD8, and CD20 cells, as well as the count of CD20 cells detected in renal biopsies, could aid in distinguishing between the two conditions. In another study, Xu et al. [] examined the immune phenotype of T-lymphocyte infiltrations in renal biopsies taken from 125 transplant recipients with stable renal function. The research revealed that individuals with a regulatory T-lymphocyte phenotype had a lower frequency of acute rejection (83.2%) compared to those with a cytotoxic T-lymphocyte phenotype, where all instances resulted in clinically diagnosed or biopsy-proven acute rejection.
Chang et al. [] conducted a study on 56 sequential biopsies of renal transplants to predict the outcomes of grafts after acute rejection. They analyzed plasma cell densities and glomerular filtration rates and found that plasma cell density was a crucial predictor of graft failure. The research also showed a trend towards statistical significance to B-cell density.
In summary, the studies mentioned in the text provide diverse results regarding the detection of kidney-transplant rejection. While some histopathological and clinical markers show promise for predicting rejection, there are conflicting findings among the studies, possibly due to variations in sample sizes, study designs, and patient characteristics. The lack of information on the replication and validation of findings raises uncertainty about the overall reliability of some results. Larger sample sizes in some studies enhance the credibility of the conclusions, but smaller sample sizes in others may limit the statistical power. The discussed markers have potential applications in clinical practice, but further validation and research in larger and diverse patient populations are needed to ensure their reliability and widespread implementation. Healthcare providers must keep abreast of evolving research to make evidence-based decisions in diagnosing and monitoring renal-transplant rejection.
The mentioned studies investigated different types of rejection in kidney-transplant recipients. A common finding among these studies was the importance of T-cell mediated rejection (TCMR) and antibody-mediated rejection (ABMR) in acute rejection [,,,,,]. Several studies identified the biomarker CD4+ CD25+/CD39+ expression to predict acute cellular rejection (ACR) as well [,,]. The studies also highlighted the importance of detecting and treating acute rejection, as it was found to increase the risk of graft loss [,]. Additionally, they identified various risk factors for acute rejection, including endothelial injury, low levels of CD4+ CD25+/CD39+ mTreg and CD4+ CD25+ CD39+ mTeff cells, and the alloimmune responses of Th-17 [,,]. These histological samples emphasize their critical importance in identifying different types of renal rejection, which provide valuable insights into the mechanisms underlying kidney-transplant rejection and may help improve treatment outcomes for kidney-transplant patients.
3. Clinical Markers
Clinical markers play a critical role in identifying and monitoring the progression of renal rejection, allowing for timely intervention to prevent further damage to the transplanted kidney. Common clinical markers used to detect renal rejection include serum creatinine levels, blood urea nitrogen (BUN) levels, urine output, and proteinuria []. An increase in serum creatinine levels may suggest a decrease in kidney function, potentially indicating the onset of rejection. Elevated BUN levels can also indicate a reduction in kidney function. Decreased urine output may be a sign of decreased kidney function or possible obstruction of the urinary tract, both of which can be linked to rejection []. Proteinuria, which refers to an excessive amount of protein in the urine, may indicate damage to the glomeruli, the small filtration units within the kidney. Despite having a critical role in identifying rejection, these markers have some limitations detecting renal rejection. They are influenced by nonrenal factors, making early detection of rejection challenging []. To address these limitations, researchers have explored other biomarkers, such as interleukin-18 (IL-18) and neutrophil-gelatinase-associated lipocalin (NGAL), released by injured kidneys, which show promise in providing early and sensitive detection of kidney-transplant rejection []. It is essential to note that these clinical markers are usually used in combination with other tests, such as biopsy or imaging, to confirm a rejection type and diagnosis, in addition to allowing real-time monitoring of the transplanted kidney. With early detection and prompt treatment, the prognosis for most cases of renal rejection is favorable, and the transplanted kidney can often be salvaged []. Additional markers include: urinary β2-microglobulin, N-acetyl-β-glucosaminidase (NAG), and L-FABP, which are markers of rejection in urine tests used in real clinical practice, with β2-microglobulin assessing proximal tubule injury [], NAG serving as a sensitive marker of tubular injury [], and L-FABP being a valuable biomarker for diagnosing acute kidney injury and predicting long-term graft outcomes in kidney-transplant patients []. Additionally, the researchers investigated other clinical markers that may be correlated with acute renal rejection, and their studies and findings will be highlighted below.
Heidari et al. [] conducted a study to examine a novel biomarker to diagnose antibody-mediated rejection (ABMR) in 36 patients who had undergone kidney transplants. The study utilized an RF algorithm to identify a panel of three proteins, namely EGF, COL6A, and NID-1, that demonstrated potential as a useful method for identifying ABMR early on, with high accuracy and precision.
Zhang et al. [] conducted a study on 282 patients from a public repository of the high-throughput Gene Expression Omnibus database at the National Center of Biotechnology Information that identified four specific long noncoding RNAs (lncRNAs) that could potentially serve as biomarkers to diagnose acute rejection (AR) and predict the likelihood of kidney-transplant failure. These lncRNAs are ATP1A1-AS1, LINC00645, EMX2OS, and CTD-3080P12.3. By using univariate and multivariate Cox regression analyses, the researchers developed a 4-lncRNA risk score model based on 17 prognostic DElncRNAs, indicating the potential of these lncRNAs as diagnostic and prognostic biomarkers. Similarly, Nolan et al. [] examined the efficacy of the urinary Q-Score in detecting the acute rejection of renal allografts. They collected 223 urine samples from patients of all ages who had undergone renal transplants and measured 6 QSant biomarkers. The statistical models developed achieved a 99.8% ROC and 98.2% accuracy, suggesting that the Q-Score is an effective tool for identifying patients with subclinical rejection who do not show high levels of serum creatinine but have been detected through a protocol biopsy.
The study by Banas et al. [] investigated the potential of urine metabolites as a biomarker for the noninvasive detection of acute rejection in renal allografts. The researchers analyzed urine samples from 109 renal-transplant recipients and developed a metabolite rejection score. They concluded that the metabolite constellation could serve as a useful biomarker for the noninvasive detection of acute allograft rejection, based on an examination of 46 instances and 520 control samples. Similarly, Chen et al. [] conducted a study to determine whether urinary CXCL13 levels could be used as a reflection of ongoing immune processes in renal allografts. The researchers quantified urinary CXCL13 levels in 146 renal-allograft recipients and 40 healthy individuals, and found that the method could distinguish between acute cellular rejection and acute antibody-mediated rejection (ABMR) with an area under the curve (AUC) of 0.856. These findings suggest that urinary CXCL13 could serve as a valuable diagnostic indicator for acute rejection in renal allografts. Both Banas et al. [] and Chen et al. [] used different methods to analyze urinary metabolites and CXCL13 levels for distinguishing acute rejection from stable groups, affected by various potential confounding factors, such as differences in immunosuppressive treatments, the timing of urine-sample collection, and varying diagnostic criteria for rejection. Patient-specific factors, such as underlying health conditions and genetic variations, can also influence biomarker levels and their predictive accuracy.
In the study conducted by Xu et al. [], the objective was to identify biomarkers that could effectively predict early acute renal-allograft rejection. The most effective biomarker was found to be a combination of fractalkine on day 0, and IP-10 and IFN-γ on day 7. This combination had an area under the curve (AUC) of 0.866, a sensitivity of 86.8%, and a specificity of 89.8%. Zheng et al. [] utilized gas chromatography–mass spectrometry to distinguish between acute rejection and stable groups by analyzing urine metabolites in 15 individuals who had received renal allografts and were experiencing acute rejection, and 15 individuals who had stable renal transplants. Overall, their study found fourteen metabolites to be significantly different between the acute-rejection group and the stable-transplant group.
Seibert et al. [] evaluated the diagnostic ability of urinary calprotectin in distinguishing between prerenal and intrinsic acute renal-allograft failure in 328 individuals. The study found that levels of urinary calprotectin were 36 times higher in intrinsic AKI compared to prerenal AKI. Additionally, the ROC curve analysis showed that urinary calprotectin had a high accuracy (AUC = 0.94) in differentiating intrinsic from prerenal AKI. These results demonstrate that urinary calprotectin is able in distinguishing prerenal from intrinsic acute renal-allograft failure. Low levels suggest prerenal AKI and may require immediate fluid repletion, while high levels indicate intrinsic renal failure, possibly necessitating biopsy and specific treatment. However, limitations due to various kidney diseases and infections require further investigation for accurate interpretation. Nonetheless, low-calprotectin concentrations suggest less severe intrarenal damage, while high concentrations warrant further evaluation to rule out other factors.
Viglietti et al. [] conducted a prospective study involving 851 kidney-transplant recipients to investigate whether systematic monitoring of donor-specific antibodies (DSAs) improves the prediction of kidney-allograft loss. They found that monitoring DSA characteristics and incorporating allograft biopsies into the usual predictors of allograft loss resulted in better accuracy of allograft-loss prediction. Standardized monitoring of anti-HLA DSAs within 2 years post-transplantation, including the IgG3 subclass and complement-binding capacity, enhances allograft-loss prediction beyond conventional approaches. Early detection of subclinical ABMR allows timely intervention and personalized clinical management.
Galichon et al. [] investigated the potential of urinary mRNA as diagnostic markers for renal-allograft rejection. They analyzed 108 urine samples collected during allograft biopsy and evaluated IP-10 and CD3∈mRNA as potential markers. Normalizing the data based on total RNA quantity did not significantly improve the results, and some conventional reference genes that were overexpressed during rejection even worsened the normalization process. The study highlights the complexities of using urinary mRNA as diagnostic markers for renal-allograft rejection and emphasizes the importance of a urothelial-cell-specific reference gene for accurate normalization. Although the diagnostic value of IP-10 and CD3∈mRNA was not enhanced by reference-gene normalization, the researchers suggest that GAPDH and UPK1A are preferable reference genes over 18S or HPRT RNA due to their more stable expression levels. These findings offer valuable insights for optimizing normalization methods and improving the reliability of urinary mRNA markers in clinical practice. Venner et al. [] employed microarray analysis to identify alterations in kidney-transplant biopsies of 315 individuals with pure antibody-mediated rejection (ABMR). They discovered 2603 significantly different transcripts in ABMR biopsies compared to all other biopsies within the total set of 703 biopsies. The study highlighted the importance of transcripts expressed in cultured cell endothelial cells closely related to ABMR. The findings offer valuable insights into using microarray analysis to understand ABMR and provide potential targets for therapeutic intervention, emphasizing the significance of individualized assessment and the need for well-phenotyped biopsy cohorts in modeling human disease states for mechanistic insights.
Shabir et al. [] studied 73 de novo transplant recipients to explore the link between transitional B lymphocytes and kidney-allograft-rejection rates. They found no significant correlation between transitional B-cells and the development of de novo donor-specific or nondonor-specific antibodies. However, maintaining appropriate transitional B-cell levels was associated with lower rejection rates in patients with de novo donor-specific antibodies. HLA-DR mismatch predicted the time to dnDSA appearance, and prior dnDSA development and repeat transplantation were predictors of dnNDSA appearance. ABMR showed a strong association with microvascular inflammation, and adherent patients with dnDSAs displayed reduced rejection risk. Peripheral cellular regulation may play a role in reducing rejection risk in patients with circulating HLA antibodies. Sigdel et al. [] utilized iTRAQ-based proteomic discovery and targeted ELISA validation to identify urine protein biomarkers for renal-allograft damage. They found 69 urine proteins with significant differences in abundance between acute rejection (AR) and stable graft, with 12 proteins upregulated in AR and 9 highly specific to AR. These noninvasive biomarkers offer noninvasive advantages over invasive diagnostic methods such as kidney biopsies, aiding risk stratification and personalized management for kidney-transplant patients. The study revealed distinct protein profiles for different injury types (AR, CAI, and BKV), providing insights into underlying mechanisms. Proteins such as PEDF and CD44 show potential as robust AR biomarkers, while common injury-associated proteins suggest autoimmune inflammatory mechanisms in all transplant injuries.
Freitas et al. [] examined the impact of immunoglobulin-G subclasses and C1q on kidney-transplantation outcomes in recipients with de novo HLA-DQ donor-specific antibodies (DSAs). The study included 284 kidney-transplant recipients who had either persistent DQ-only DSAs or DQ plus other DSAs. Results indicated that individuals with these DSAs had higher rates of acute rejection episodes, allograft loss, and lower 5-year allograft survival rates compared to those without DSAs. Additionally, C1q-positive DSAs were linked to worse pathology and significantly increased graft-loss risk, especially in patients who transitioned from C1q-negative before transplantation to C1q-positive after transplantation. This information aids clinicians in risk stratification and personalized management for transplant recipients. Banasik et al. [] studied 78 kidney-transplant recipients, with 44% developing de novo donor-specific anti-HLA antibodies (DSAs) within the first year after transplantation. Among DSA-positive patients, seven experienced antibody-mediated rejection, while none of the DSA-negative patients did. The results support prior studies, indicating that newly developed DSAs have a substantial negative effect on graft function and long-term survival. However, caution is necessary due to limitations and potential confounders. While de novo DSAs had a significant impact on graft failure, some patients with DSAs did not experience graft insufficiency during the study, suggesting variability in DSA production and the role of inflammatory events in DSA formation. The mechanism of accommodation and the long-term effects of DSAs on graft outcomes remain unclear, warranting further research. Routine DSA monitoring and early intervention may improve renal-transplant outcomes, requiring better understanding of DSA dynamics beyond the first-year post-transplantation.
Loupy et al. [] conducted research to investigate the impact of the complement-binding capacity in anti-HLA antibodies on kidney-allograft failure. Their findings suggest that lower graft survival rates associated with complement-binding donor-specific anti-HLA antibodies may be due to complement cascade activation, leading to graft injury and loss independently of C4d deposition, indicating a potential role for complement-dependent pathways in allograft damage. These results highlight the importance of early detection and potential therapeutic interventions targeting the complement to improve graft outcomes in kidney-transplant recipients, which can be translated into clinical practice by using complement-binding donor-specific anti-HLA antibodies as a risk-stratification tool to identify high-risk patients and implement early interventions.
Song et al. [] analyzed 69 biopsy samples of renal allografts to investigate the clinical relevance of KIM-1 as a biomarker for tissue damage. They found that KIM-1 expression was highly positive in the chronic active antibody-mediated rejection group, but weakly positive in the normal group without acute rejection or immunosuppressant toxicity. The results suggest that KIM-1 expression in renal-allograft-biopsy samples is closely related to markers of tissue damage and rejection, and it may serve as an early marker of rejection injury and graft survival in renal transplantation. Furthermore, KIM-1 shows potential as an early diagnostic biomarker for acute kidney injury (AKI) and chronic kidney disease (CKD), offering valuable insights for timely intervention and management in clinical settings.
Roshdy et al. [] conducted a study to determine the association between CRP levels and the early identification of renal-allograft rejection. They monitored 91 renal-transplant recipients for a median follow-up of 8 weeks and discovered that individuals who experienced allograft rejection had significantly higher CRP levels before and after transplantation than those who did not. Hence, the association between CRP levels and early identification of renal-allograft rejection seems significant. Some studies propose CRP estimation as a simple and effective method for detecting rejection and predicting rejection-prone patients. However, other studies suggest the need for considering confounding factors and further research to determine CRP’s reliability as a marker for rejection.
DeVos et al. [] studied the impact of HLA-DQ donor-specific antibodies on renal-transplantation outcomes. They followed 347 patients for three years and found that 62 patients developed new donor-specific antibodies, with 48 of them having HLA-DQ antibodies either by themselves or in conjunction with other HLA antibodies.
In conclusion, some studies [,] reveal promising novel biomarkers for detecting AMR and acute rejection, respectively. Nevertheless, further validation in larger and diverse populations, along with functional experiments, is crucial before clinical implementation. The identified lncRNAs demonstrate strong diagnostic accuracy and predictive value for acute rejection compared to traditional clinical markers, but additional validation and comprehensive clinical parameters are necessary for clinical translation. The urinary Q-Score offers advantages over traditional markers, enabling early detection and personalized immunosuppressive therapy. However, challenges in timing and potential influences on metabolite analysis need to be addressed. The biomarker combination of fractalkine, IP-10, and IFN-γ shows promise for predicting early acute renal-allograft rejection, but requires multicenter validation and investigation into different rejection scenarios for broader clinical utility (Table 2).

Table 2.
A review of the existing literature regarding clinical markers used to anticipate acute rejection in patients.
Various studies have been conducted to identify and evaluate different biomarkers for diagnosing acute and antibody-mediated rejection in renal allografts [,,,]. The biomarkers that were evaluated include proteins, metabolites, long noncoding RNAs, and mRNA. Heidari et al. [] and Zhang et al. [] used protein markers, while Banas et al. [] and Zheng et al. [] evaluated metabolite markers. Nolan et al. [] used QSant biomarkers, while Chen et al. [] examined urinary CXCL13 levels. Xu et al. [] and Galichon et al. [] examined a combination of markers, including fractalkine, IP-10, IFN-γ, and IP-10 mRNA. Viglietti et al. [] monitored donor-specific antibodies (DSAs), and Venner et al. [] examined the expression of transcripts. Lastly, Shabir et al. [] examined a combination of protein and gene markers. These studies have found promising clinical and combined markers for identifying and predicting acute and antibody-mediated rejection in renal allografts [,,], which could lead to improved diagnosis and treatment outcomes for patients.
4. Genetic Markers
Genetic markers have become increasingly important in identifying and managing renal rejection. They provide valuable information about the genetic factors that influence the likelihood of rejection and the response to treatment. Potential confounding factors influencing the association between genetic markers and renal rejection include different gene-expression-analysis technologies (microarray vs. RNAseq), obtaining extra biopsy cores for profiling, and variability in blood tacrolimus concentrations affecting transplant outcomes and AR risk []. One of the most critical genetic markers for renal rejection is the HLA mismatch, which refers to differences in human leukocyte antigen between the donor and recipient [,]. The HLA system plays a crucial role in presenting antigens to the immune system and is involved in the recognition and rejection of foreign tissues. In addition to the HLA mismatch, single nucleotide polymorphisms (SNPs) in certain genes related to the immune response have been implicated in renal rejection []. The presence of specific SNPs in genes involved in immune response can increase the probability of rejection and affect the response to therapy. Gene-expression patterns are another type of genetic marker that has been investigated as a potential indicator of renal rejection []. These markers can provide valuable information about the molecular changes that occur during rejection and could be used to develop more targeted treatments. Overall, genetic markers offer significant insights into the mechanisms of renal rejection and provide opportunities for developing personalized treatments [,,].
Wisniewskaa et al. [] investigated the association between variations in the VAV1 gene and renal-allograft function. The study found that possessing more T alleles of the VAV1 rs2546133 variant may have a protective effect against acute rejection in kidney-transplant recipients. This conclusion was drawn from a multivariate regression analysis of 270 patients.
Sommerer et al. [] aimed to investigate whether monitoring the expression of genes controlled by NFAT could serve as an indicator for identifying individuals who are susceptible to developing acute rejection or infections following renal-allograft transplantation. In the study, blood samples from 64 newly transplanted renal-allograft recipients were collected at various intervals after transplantation and subjected to analysis. The findings suggest that individuals with a high level of remaining gene expression are more vulnerable to experiencing acute rejection, whereas those with a low level of remaining gene expression are more susceptible to viral complications, such as the replication of cytomegalovirus and BK virus. Klager et al. [] examined the diagnostic potential of DARC immunohistochemistry for ABMR by analyzing 82 biopsies from patients who tested positive for donor-specific antibodies (DSAs) and had gene-expression data that could be analyzed. The study revealed a significant association between DARC positivity and ABMR diagnosis, as well as a correlation between DARC gene-expression levels and DARC positivity. However, there was no noticeable difference in graft survival between ABMR cases that were DARC-positive and those that were DARC-negative.
A study conducted by Han et al. [] investigated the possible connection between dmtDNA levels and antibody-mediated rejection (ABMR) in 323 kidney-transplant recipients. The study found that patients who experienced acute rejection had significantly higher levels of dmtDNA compared to the control group. Multivariate logistic regression analysis demonstrated a significant link between dmtDNA levels and acute rejection. Therefore, measuring the levels of dmtDNA could be a valuable method for predicting acute rejection in individuals who have undergone kidney transplantation. In a study by Groeneweg et al. [], the influence of acute rejection (AR) on local vascular integrity was examined in 47 kidney-transplant recipients by analyzing kidney biopsies. The researchers observed a reduction in capillary density during AR. Elevated concentrations of LNC-EPHA6 were also identified in the bloodstream during AR, which returned to normal after one year. Furthermore, there was a significant association between the quantities of LNC-RPS24, LNC-EPHA6, and LIPCAR and the marker of vascular damage, soluble thrombomodulin.
Shaw et al. [] aimed to develop a gene signature capable of tracking acute rejection in kidney transplantation by comparing gene-expression profiles in kidney biopsy and peripheral blood samples from patients experiencing acute rejection (AR) with those of stable patients. They identified a signature of 90 probes, focusing on 76 genes, that could differentiate between stable patients and those experiencing AR. Moreover, they identified a group of eight genes with a unique link to AR. Kim et al. [] investigated the association between single nucleotide polymorphisms (SNPs) in the genes EGF or EGFR and the occurrence of end-stage renal disease (ESRD) and acute renal-allograft rejection (AR). Their study included 347 individuals who had received kidney transplants, consisting of 63 patients with AR and 289 healthy individuals. They found that certain SNPs in the genes EGF and EGFR were significantly associated with increased susceptibility to both ESRD and AR.
Sharbafi et al. [] investigated mRNA expressions of TLR-4, TLR-2, and MyD88 in PBMCs and biopsy samples of renal-transplant recipients with various types of rejection. The results revealed elevated TLR4 expression in both chronic and acute T-cell-mediated rejection, whereas TLR2 expression was only increased in acute T-cell-mediated rejection. MyD88 expression was elevated in all types of rejection and could be differentiated from stable grafts. In another study, Guberina et al. [] examined the correlation between HLA-E expression and the survival of renal allografts in the occurrence of acute cellular rejection (ACR). The research outcomes indicated that HLA-E expression increased in biopsies with ACR and had a positive correlation with mismatches in HLA-class I leader peptides and the presence of infiltrating cells such as CD8+ and CD56+. The study found that high HLA-E expression was linked to reduced allograft survival.
Ge et al. [] investigated the diagnostic potential of long noncoding RNAs (lncRNAs) by analyzing their expression patterns in peripheral blood samples from 150 renal-transplant recipients. The study identified 23 lncRNAs with differential expression in both adult and pediatric cohorts, which were able to distinguish between recipients with acute rejection (AR) and those without AR. These findings indicate that these lncRNAs can serve as effective diagnostic markers for AR in renal-transplant patients. Qiu et al. [] examined the role of lncRNA-ATB in acute kidney injury (AKI) in renal-transplant patients receiving immunosuppressive therapy. Their study found that lncRNA-ATB levels were significantly higher in patients with acute rejection (n = 72) compared to the control group. Additionally, their research suggested that lncRNA-ATB may affect the characteristics of kidney cells and the toxicity of immunosuppressive medications.
In their study, Liu et al. [] used next-generation sequencing to detect miRNA expression variations in 15 kidney allografts with acute rejection and normal allografts. Among the 75 dysregulated miRNAs, miR-10b had the most significant downregulation in rejected allografts. Inducing a decrease in miR-10b expression in human renal glomerular endothelial cells resulted in characteristics similar to those observed in acute allograft rejection. Pawlik et al. [,] conducted two separate studies to investigate the association between genetic variations and renal-allograft performance. Using TaqMan genotyping assays and enrolling 270 Caucasian kidney-allograft recipients, the first study did not find any correlation between the Glu37Asp polymorphism in the renalase gene and allograft functioning. In contrast, the second study showed that the IVS3 + 17T/C polymorphism in the CD28 gene could have an association with acute rejection, although it did not correlate with delayed graft function or chronic allograft nephropathy.
Kim et al. [] investigated the relationship between TLR9 gene polymorphisms and the success of kidney allografts in 342 renal-transplant patients using direct sequencing. They discovered that some alleles of the TLR9 gene were protective against acute rejection, and two TLR9 SNPs were linked to the risk of acute rejection in renal transplantation. In a separate study, Suthanthiran et al. [] developed a noninvasive technique using urine cells to identify acute rejection in kidney transplants. They collected urine samples from 485 kidney-graft patients and analyzed mRNA levels in urinary cells to identify a three-gene signature that could differentiate biopsy specimens with acute cellular rejection from those without it. The estimated AUC from cross-validation was 0.83, indicating good diagnostic accuracy for the three-gene signature in distinguishing biopsy specimens with acute cellular rejection from those without.
The genetic markers related to renal rejection have been validated in some large-scale studies with significant sample sizes, enhancing their robustness and reliability [,,]. These findings hold the potential to transform clinical practice by enabling personalized treatment strategies and improving graft outcomes in kidney-transplant recipients. However, gene-expression patterns as indicators of renal rejection have limitations, and their reliability and consistency across different patients and populations can vary due to genetic diversity and technological differences [,]. While the findings from different studies regarding genetic markers for renal rejection align in some areas [,], they also present contradictions, with certain markers consistently associated with renal rejection risk, and others showing variable diagnostic potential. Factors such as patient populations, sample sizes, methodologies, and immune response complexity contribute to these discrepancies. Alongside genetic markers, alternative approaches, such as monitoring NFAT-controlled genes, investigating lncRNAs, and analyzing urinary mRNA levels, offer valuable insights for renal-rejection management. Implementing genetic markers in routine clinical practice faces challenges, including technological differences and the complexity of immune responses, necessitating further research and validation through larger studies for successful integration into transplant management (Table 3).

Table 3.
A review of the existing literature regarding genomic markers used to anticipate acute rejection in patients.
Several studies investigated the association between genetic markers and the types of rejection in kidney-transplant recipients [,,]. The markers used in these studies vary, including genes (VAV1, NFAT, EGF, EGFR), mitochondrial DNA (dmtDNA), long noncoding RNAs (lncRNAs), and messenger RNA (mRNA). Despite the variation in the markers, the studies show some common findings. Firstly, they demonstrate that measuring the levels of genetic markers can predict acute rejection in individuals who have undergone kidney transplantation [,,,]. Secondly, the studies suggest that elevated levels of certain genetic markers are associated with acute rejection, while low levels are associated with viral complications [,,]. Thirdly, the studies reveal that measuring the expression of certain genetic markers can serve as an indicator for identifying individuals who are susceptible to developing acute rejection or infections following renal-allograft transplantation [,,]. Lastly, the studies by Ge et al. and Qiu et al. [,] showed that genetic markers, especially IncRNA, can serve as a noninvasive marker for identifying acute rejection in renal-transplant patients.
5. Limitations and Strengths
This survey contributes to identifying potential biomarkers and improving diagnostic techniques for acute rejection in kidney transplantation. Some studies have limitations in sample size and diversity, highlighting the need for further validation in extensive and diverse patient populations. However, the studies utilize innovative approaches, such as urine-based tests and T-cytotoxic memory cells, showing promise for personalized medicine and better patient outcomes. These insights can lead to more effective monitoring and management for acute rejection in kidney-transplant recipients. Overcoming limitations requires longitudinal data, optimal monitoring timing, and consideration of confounding variables such as comorbidities and immunosuppressive therapies. Standardizing sample collection methods enhances generalizability. Despite limitations, these studies offer promising efforts to improve acute-rejection monitoring, laying the groundwork for future research. Future studies should focus on validating and exploring clinical, genetic, and histopathological markers for improved kidney-transplant outcomes. Noninvasive early detection markers, specific biomarkers for different rejection types, and personalized immunosuppressive therapies show potential. Validation, standardization, and longitudinal studies are essential to address knowledge gaps and enhance patient care. Collaboration and ongoing research are vital to overcome immune rejection challenges. Moreover, widespread implementation of these markers in clinical practice may require further validation and replication studies to ensure their reliability and reproducibility across different populations and healthcare settings. Additionally, the adoption of histopathological markers for renal-transplant rejection may also depend on the availability and expertise of pathology resources in various medical centers. To increase the clinical applicability of these markers, ongoing research and collaboration between researchers, clinicians, and pathologists are essential.
6. Conclusions
In conclusion, various histopathological, clinical, and genetic markers have been identified as important indicators for identifying different types of renal rejection in kidney-transplant recipients. T-cell-mediated rejection (TCMR) and antibody-mediated rejection (ABMR) were found to be common in acute rejection, and detecting and treating acute rejection was found to be critical in improving treatment outcomes. Biomarkers, including proteins, metabolites, long noncoding RNAs, and mRNA, have been evaluated to diagnose acute and antibody-mediated rejection in renal allografts, showing promising results in improving diagnosis and treatment outcomes. Genetic markers, including genes, mitochondrial DNA, long noncoding RNAs, and messenger RNA, were also found to be important in predicting acute rejection in kidney-transplant patients and identifying individuals susceptible to developing acute rejection or infections following renal-allograft transplantation. Measuring the expression of certain genetic markers, especially IncRNA, has been identified as a noninvasive marker for identifying acute rejection in renal-transplant patients. The evaluation of these markers provides valuable insights into the mechanisms underlying kidney-transplant rejection and may lead to improved treatment outcomes for kidney-transplant patients.
Author Contributions
Conceptualization, I.S., A.A. and A.E.-B.; investigation, M.G., D.G. and A.E.-B.; Methodology, I.S., A.A., M.E. and A.E.-B.; project administration, M.A.E.-G., M.G. and A.E.-B.; supervision, A.E.-B.; visualization, I.S.; writing—original draft, I.S. and M.E.; writing—review and editing, I.S., A.A., M.A.E.-G., M.G., D.G. and A.E.-B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
Ghazal acknowledges the support from Abu Dhabi University’s Office of Research and Sponsored Programs (Grant \#19300792).
Conflicts of Interest
The authors declare no conflict of interest.
References
- How Successful Is the Kidney Transplant Procedure? Available online: https://www.healthline.com/health/kidney-transplant-success-rates#:~:text=People%20with%20end%20stage%20kidney,for%20at%20least%201%20year (accessed on 24 July 2023).
- Naik, R.H.; Shawar, S.H. Renal transplantation rejection. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- The Immune Response and Its Role in Renal Transplant Rejection. Available online: https://www.lakeforest.edu/news/the-immune-response-and-its-role-in-renal-transplant-rejection (accessed on 24 July 2023).
- LaRosa, D.F.; Rahman, A.H.; Turka, L.A. The innate immune system in allograft rejection and tolerance. J. Immunol. 2007, 178, 7503–7509. [Google Scholar] [CrossRef]
- Kidney Transplantation Services at Stony Brook Medicine. Available online: https://www.stonybrookmedicine.edu/patientcare/transplant/rejection#:~:text=Hyperacute%20rejection%20is%20extremely%20rare,completely%20destroys%20the%20kidney%20transplant (accessed on 24 July 2023).
- CDRG: Kidney Transplant Cost. Available online: https://health.costhelper.com/kidney-transplant.html (accessed on 10 May 2023).
- CDRG: WHAT IS TRANSPLANT REJECTION? Available online: https://www.kidney.org.uk/what-is-transplant-rejection (accessed on 10 May 2023).
- Lo, D.J.; Kaplan, B.; Kirk, A.D. Biomarkers for kidney transplant rejection. Nat. Rev. Nephrol. 2014, 10, 215–225. [Google Scholar] [CrossRef]
- Rogulska, K.; Wojciechowska-Koszko, I.; Dołe˛gowska, B.; Kwiatkowska, E.; Roszkowska, P.; Kapczuk, P.; Kosik-Bogacka, D. The most promising biomarkers of allogeneic kidney transplant rejection. J. Immunol. Res. 2022, 2022, 6572338. [Google Scholar] [CrossRef]
- Jeong, H.J. Diagnosis of renal transplant rejection: Banff classification and beyond. Kidney Res. Clin. Pract. 2020, 39, 17. [Google Scholar] [CrossRef]
- Wu, T.; Abu-Elmagd, K.; Bond, G.; Nalesnik, M.A.; Randhawa, P.; Demetris, A.J. A schema for histologic grading of small intestine allograft acute rejection. Transplantation 2003, 75, 1241–1248. [Google Scholar] [CrossRef]
- Racusen, L.C.; Colvin, R.B.; Solez, K.; Mihatsch, M.J.; Halloran, P.F.; Campbell, P.M.; Cecka, M.J.; Cosyns, J.P.; Demetris, A.J.; Fishbein, M.C.; et al. Antibody-mediated rejection criteria–an addition to the Banff’ 97 classification of renal allograft rejection. Am. J. Transplant. 2003, 3, 708–714. [Google Scholar] [CrossRef]
- Arai, T.; Oguchi, H.; Shinoda, K.; Sakurabayashi, K.; Mikami, T.; Itabashi, Y.; Sakai, K. Clinicopathological Analysis of Acute/Active Antibody-Mediated Rejection in Renal Allografts According to the Banff 2013 Classification. Nephron 2020, 144, 18–27. [Google Scholar] [CrossRef]
- García-Covarrubias, L.; Cedillo, J.S.; Morales, L.; Fonseca-Sanchez, M.A.; García-Covarrubias, A.; Villanueva-Ortega, E.; Hernández, C.; Diliz, H.; Reding-Bernal, A.; Soto, V.; et al. Interleukin 8 Is Overexpressed in Acute Rejection in Kidney Transplant Patients. Transplant. Proc. 2020, 52, 1127–1131. [Google Scholar] [CrossRef]
- Eiamsitrakoon, T.; Tharabenjasin, P.; Pabalan, N.; Tasanarong, A. Influence of Interferon Gamma+ 874 T> A (rs2430561) Polymorphism on Renal Allograft Rejection: A Meta-analysis. Transplant. Proc. 2021, 53, 897–905. [Google Scholar] [CrossRef]
- Rohan, V.S.; Soliman, K.M.; Alqassieh, A.; Alkhader, D.; Patel, N.; Nadig, S.N. Renal allograft surveillance with allospecific T-cytotoxic memory cells. Ren. Fail. 2020, 42, 1152–1156. [Google Scholar] [CrossRef]
- Shimizu, T. Clinical and Pathological Analyses of Borderline Changes Cases after Kidney Transplantation. Nephron 2020, 144, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, Q.; Li, H.; Yu, M.; Peng, B.; Liu, S.; Luo, M.; Stefano, G.B.; Kream, R.M.; Ming, Y. Profiles of B-cell subsets in immunologically stable renal allograft recipients and end-stage renal disease patients. Transpl. Immunol. 2020, 58, 101249. [Google Scholar] [CrossRef]
- Mueller, F.B.; Yang, H.; Lubetzky, M.; Verma, A.; Lee, J.R.; Dadhania, D.M.; Xiang, J.Z.; Salvatore, S.P.; Seshan, S.V.; Sharma, V.K.; et al. Landscape of innate immune system transcriptome and acute T cell–mediated rejection of human kidney allografts. JCI Insight 2019, 4, e128014. [Google Scholar] [CrossRef]
- Nowan´ska, K.; Donizy, P.; Kos´cielska-Kasprzak, K.; Kamin´ska, D.; Krajewska, M.; Mazanowska, O.; Madziarska, K.; Zmonarski, S.; Chudoba, P.; Małkiewicz, B.; et al. Endothelin A receptors expressed in renal blood vessels of renal transplant patients are connected with acute tubular necrosis or antibody-mediated rejection. Transplant. Proc. 2018, 50, 1760–1764. [Google Scholar] [CrossRef] [PubMed]
- de Leur, K.; Clahsen-van Groningen, M.; van den Bosch, T.; de Graav, G.; Hesselink, D.; Samsom, J.; Baan, C.; Boer, K. Characterization of ectopic lymphoid structures in different types of acute renal allograft rejection. Clin. Exp. Immunol. 2018, 192, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Malone, A.F.; Donnelly, E.L.; Kirita, Y.; Uchimura, K.; Ramakrishnan, S.M.; Gaut, J.P.; Humphreys, B.D. Single-cell transcriptomics of a human kidney allograft biopsy specimen defines a diverse inflammatory response. J. Am. Soc. Nephrol. 2018, 29, 2069–2080. [Google Scholar] [CrossRef]
- McRae, J.L.; Chia, J.S.; Pommey, S.A.; Dwyer, K.M. Evaluation of CD4+ CD25+/- CD39+ T-cell populations in peripheral blood of patients following kidney transplantation and during acute allograft rejection. Nephrology 2017, 22, 505–512. [Google Scholar] [CrossRef]
- Jiang, Y.; Wang, R.; Wang, H.; Huang, H.; Peng, W.; Qiu, W.; Zhou, J.; Chen, J. The effect of histological CD20-positive B cell infiltration in acute cellular rejection on kidney transplant allograft survival. J. Immunol. Res. 2016, 2016, 7473239. [Google Scholar] [CrossRef]
- Sentís, A.; Kers, J.; Yapici, U.; Claessen, N.; Roelofs, J.J.; Bemelman, F.J.; Ten Berge, I.J.; Florquin, S. The prognostic significance of glomerular infiltrating leukocytes during acute renal allograft rejection. Transpl. Immunol. 2015, 33, 168–175. [Google Scholar] [CrossRef]
- Matignon, M.; Aissat, A.; Canoui-Poitrine, F.; Grondin, C.; Pilon, C.; Desvaux, D.; Saadoun, D.; Barathon, Q.; Garrido, M.; Audard, V.; et al. TH-17 alloimmune responses in renal allograft biopsies from recipients of kidney transplants using extended criteria donors during acute T cell–mediated rejection. Am. J. Transplant. 2015, 15, 2718–2725. [Google Scholar] [CrossRef]
- Visona, I.; Sementilli, A.; Kuschnaroff, L.M.; Franco, M.F. Medullary nephritis in the diagnosis of acute cellular rejection. Pathol.-Res. Pract. 2015, 211, 811–815. [Google Scholar] [CrossRef]
- Lee, H.; Kim, J.I.; Moon, I.S.; Chung, B.H.; Yang, C.W.; Kim, Y.; Han, K.; Oh, E.J. Investigation of serum angiotensin II type 1 receptor antibodies at the time of renal allograft rejection. Ann. Lab. Med. 2015, 35, 314. [Google Scholar] [CrossRef]
- Crespo, M.; Yelamos, J.; Redondo, D.; Muntasell, A.; Perez-Saéz, M.; López-Montañés, M.; García, C.; Torio, A.; Mir, M.; Hernández, J.; et al. Circulating NK-cell subsets in renal allograft recipients with anti-HLA donor-specific antibodies. Am. J. Transplant. 2015, 15, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Bhat, Z.Y.; Bostwick, D.G.; Hossain, D.; Zeng, X. Participation of functionally active plasma cells in acute rejection and response to therapy in renal allografts. DNA Cell Biol. 2014, 33, 448–454. [Google Scholar] [CrossRef] [PubMed]
- DeVos, J.M.; Gaber, A.O.; Teeter, L.D.; Graviss, E.A.; Patel, S.J.; Land, G.A.; Moore, L.W.; Knight, R.J. Intermediate-term graft loss after renal transplantation is associated with both donor-specific antibody and acute rejection. Transplantation 2014, 97, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Wang, L.; Yang, C.; Zhao, T.; Li, L.; Hu, L.; Wu, D.; Rong, R.; Xu, M.; Zhu, T. Soluble FGL2 induced by tumor necrosis factor-α and interferon-γ in CD4+ T cells through MAPK pathway in human renal allograft acute rejection. J. Surg. Res. 2013, 184, 1114–1122. [Google Scholar] [CrossRef]
- Ge, Y.Z.; Wu, R.; Jia, R.P.; Liu, H.; Yu, P.; Zhao, Y.; Feng, Y.M. Association between interferon gamma+ 874 T> A polymorphism and acute renal allograft rejection: Evidence from published studies. Mol. Biol. Rep. 2013, 40, 6043–6051. [Google Scholar] [CrossRef]
- Li, X.; Sun, Q.; Chen, J.; Ji, S.; Wen, J.; Cheng, D.; Liu, Z. Immunophenotyping in BK virus allograft nephropathy distinct from acute rejection. Clin. Dev. Immunol. 2013, 2013, 412902. [Google Scholar] [CrossRef]
- Xu, Y.; Jin, J.; Wang, H.; Shou, Z.; Wu, J.; Han, F.; He, Q.; Zhao, J.; Bi, Y.; Chen, J. The regulatory/cytotoxic infiltrating T cells in early renal surveillance biopsies predicts acute rejection and survival. Nephrol. Dial. Transplant. 2012, 27, 2958–2965. [Google Scholar] [CrossRef]
- Chang, A.; Moore, J.M.; Cowan, M.L.; Josephson, M.A.; Chon, W.J.; Sciammas, R.; Du, Z.; Marino, S.R.; Meehan, S.M.; Millis, M.; et al. Plasma cell densities and glomerular filtration rates predict renal allograft outcomes following acute rejection. Transpl. Int. 2012, 25, 1050–1058. [Google Scholar] [CrossRef][Green Version]
- Vaidya, V.S.; Ferguson, M.A.; Bonventre, J.V. Biomarkers of acute kidney injury. Annu. Rev. Pharmacol. Toxicol. 2008, 48, 463–493. [Google Scholar] [CrossRef] [PubMed]
- AKI. Available online: https://emedicine.medscape.com/article/777845-overview#:~:text=Acute%20kidney%20injury%20(AKI)%2C,course%20of%20hours%20to%20weeks (accessed on 17 February 2023).
- Edelstein, C.L. Biomarkers of Acute Kidney Injury. Adv. Chronic Kidney Dis. 2008, 15, 222–234. [Google Scholar] [CrossRef]
- Gorriz, J.L.; Martinez-Castelao, A. Proteinuria: Detection and role in native renal disease progression. Transplant. Rev. 2012, 26, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.; Hossain, D.; Bostwick, D.G.; Herrera, G.A.; Zhang, P.L. Urinary 2-Microglobulin Is a Good Indicator of Proximal Tubule Injury: A Correlative Study with Renal Biopsies. J. Biomark. 2014, 2014, 492838. [Google Scholar] [CrossRef] [PubMed]
- Aldea, P.L.; Rachisan, A.L.; Stanciu, B.I.; Picos, A.; Picos, A.M.; Delean, D.I.; Stroescu, R.; Starcea, M.I.; Borzan, C.M.; Elec, F.I. The Perspectives of Biomarkers in Predicting the Survival of the Renal Graft. Front. Pediatr. 2022, 10, 869628. [Google Scholar] [CrossRef]
- Heidari, S.S.; Nafar, M.; Kalantari, S.; Tavilani, H.; Karimi, J.; Foster, L.; Moon, K.M.; Khodadadi, I. Urinary epidermal growth factor is a novel biomarker for early diagnosis of antibody mediated kidney allograft rejection: A urinary proteomics analysis. J. Proteom. 2021, 240, 104208. [Google Scholar] [CrossRef]
- Zhang, Z.; Tang, Y.; Zhuang, H.; Lin, E.; Xie, L.; Feng, X.; Zeng, J.; Liu, Y.; Liu, J.; Yu, Y.; et al. Identifying 4 novel lncRNAs as potential biomarkers for acute rejection and graft loss of renal allograft. J. Immunol. Res. 2020, 2020, 2415374. [Google Scholar] [CrossRef]
- Nolan, N.; Valdivieso, K.; Mani, R.; Yang, J.Y.; Sarwal, R.D.; Katzenbach, P.; Chalasani, K.; Hongo, D.; Lugtu, G.; Mark, C.; et al. Clinical and analytical validation of a novel urine-based test for the detection of allograft rejection in renal transplant patients. J. Clin. Med. 2020, 9, 2325. [Google Scholar] [CrossRef]
- Banas, M.C.; Neumann, S.; Pagel, P.; Putz, F.J.; Krämer, B.K.; Böhmig, G.A.; Eiglsperger, J.; Schiffer, E.; Ruemmele, P.; Banas, B. A urinary metabolite constellation to detect acute rejection in kidney allografts. eBioMedicine 2019, 48, 505–512. [Google Scholar] [CrossRef]
- Chen, D.; Zhang, J.; Peng, W.; Weng, C.; Chen, J. Urinary C-X-C motif chemokine 13 is a noninvasive biomarker of antibody-mediated renal allograft rejection. Mol. Med. Rep. 2018, 18, 2399–2406. [Google Scholar]
- Xu, C.X.; Shi, B.Y.; Jin, Z.K.; Hao, J.J.; Duan, W.L.; Han, F.; Zhao, Y.L.; Ding, C.G.; Xue, W.J.; Ding, X.M.; et al. Multiple-biomarkers provide powerful prediction of early acute renal allograft rejection by combination of serum fractalkine, IFN-γ and IP-10. Transpl. Immunol. 2018, 50, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Zheng, L.; Wang, J.; Gao, W.; Hu, C.; Wang, S.; Rong, R.; Guo, Y.; Zhu, T.; Zhu, D. GC/MS-based urine metabolomics analysis of renal allograft recipients with acute rejection. J. Transl. Med. 2018, 16, 202. [Google Scholar] [CrossRef] [PubMed]
- Seibert, F.S.; Rosenberger, C.; Mathia, S.; Arndt, R.; Arns, W.; Andrea, H.; Pagonas, N.; Bauer, F.; Zidek, W.; Westhoff, T.H. Urinary calprotectin differentiates between prerenal and intrinsic acute renal allograft failure. Transplantation 2017, 101, 387–394. [Google Scholar] [CrossRef]
- Viglietti, D.; Loupy, A.; Vernerey, D.; Bentlejewski, C.; Gosset, C.; Aubert, O.; van Huyen, J.P.D.; Jouven, X.; Legendre, C.; Glotz, D.; et al. Value of donor–specific anti–HLA antibody monitoring and characterization for risk stratification of kidney allograft loss. J. Am. Soc. Nephrol. 2017, 28, 702–715. [Google Scholar] [CrossRef] [PubMed]
- Galichon, P.; Amrouche, L.; Hertig, A.; Brocheriou, I.; Rabant, M.; Xu-Dubois, Y.C.; Ouali, N.; Dahan, K.; Morin, L.; Terzi, F.; et al. Urinary mRNA for the diagnosis of renal allograft rejection: The issue of normalization. Am. J. Transplant. 2016, 16, 3033–3040. [Google Scholar] [CrossRef] [PubMed]
- Venner, J.; Hidalgo, L.; Famulski, K.; Chang, J.; Halloran, P. The molecular landscape of antibody-mediated kidney transplant rejection: Evidence for NK involvement through CD16a Fc receptors. Am. J. Transplant. 2015, 15, 1336–1348. [Google Scholar] [CrossRef]
- Shabir, S.; Girdlestone, J.; Briggs, D.; Kaul, B.; Smith, H.; Daga, S.; Chand, S.; Jham, S.; Navarrete, C.; Harper, L.; et al. Transitional B lymphocytes are associated with protection from kidney allograft rejection: A prospective study. Am. J. Transplant. 2015, 15, 1384–1391. [Google Scholar] [CrossRef]
- Sigdel, T.K.; Salomonis, N.; Nicora, C.D.; Ryu, S.; He, J.; Dinh, V.; Orton, D.J.; Moore, R.J.; Hsieh, S.C.; Dai, H.; et al. The identification of novel potential injury mechanisms and candidate biomarkers in renal allograft rejection by quantitative proteomics. Mol. Cell. Proteom. 2014, 13, 621–631. [Google Scholar] [CrossRef]
- Freitas, M.C.S.; Rebellato, L.M.; Ozawa, M.; Nguyen, A.; Sasaki, N.; Everly, M.; Briley, K.P.; Haisch, C.E.; Bolin, P.; Parker, K.; et al. The role of immunoglobulin-G subclasses and C1q in de novo HLA-DQ donor-specific antibody kidney transplantation outcomes. Transplantation 2013, 95, 1113–1119. [Google Scholar] [CrossRef]
- Banasik, M.; Boratyn´ska, M.; Kos´cielska-Kasprzak, K.; Mazanowska, O.; Krajewska, M.; Zabin´ska, M.; Bartoszek, D.; Myszka, M.; Nowakowska, B.; Dawiskiba, T.; et al. The impact of de novo donor-specific anti-human leukocyte antigen antibodies on 5-year renal transplant outcome. Transplant. Proc. 2013, 45, 1449–1452. [Google Scholar] [CrossRef]
- Loupy, A.; Lefaucheur, C.; Vernerey, D.; Prugger, C.; van Huyen, J.P.D.; Mooney, N.; Suberbielle, C.; Frémeaux-Bacchi, V.; Méjean, A.; Desgrandchamps, F.; et al. Complement-binding anti-HLA antibodies and kidney-allograft survival. N. Engl. J. Med. 2013, 369, 1215–1226. [Google Scholar] [CrossRef] [PubMed]
- Song, L.; Xue, L.; Yu, J.; Zhao, J.; Zhang, W.; Fu, Y. Kidney injury molecule-1 expression is closely associated with renal allograft damage. Bosn. J. Basic Med. Sci. 2013, 13, 170. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Roshdy, A.; El-Khatib, M.M.; Rizk, M.N.; El-Shehaby, A.M. CRP and acute renal rejection: A marker to the point. Int. Urol. Nephrol. 2012, 44, 1251–1255. [Google Scholar] [CrossRef] [PubMed]
- DeVos, J.M.; Gaber, A.O.; Knight, R.J.; Land, G.A.; Suki, W.N.; Gaber, L.W.; Patel, S.J. Donor-specific HLA-DQ antibodies may contribute to poor graft outcome after renal transplantation. Kidney Int. 2012, 82, 598–604. [Google Scholar] [CrossRef]
- Dorr, C.R.; Oetting, W.S.; Jacobson, P.A.; Israni, A.K. Genetics of acute rejection after kidney transplantation. Transpl. Int. 2018, 31, 263–277. [Google Scholar] [CrossRef]
- Zanoni, F.; Kiryluk, K. Genetic Background and Transplantation Outcomes: Insights from GWAS. Curr. Opin. Organ Transplant. 2020, 25, 35. [Google Scholar] [CrossRef]
- Jethwani, P.; Rao, A.; Bow, L.; Menon, M.C. Donor–Recipient Non-HLA Variants, Mismatches and Renal Allograft Outcomes: Evolving Paradigms. Front. Immunol. 2022, 13, 822353. [Google Scholar] [CrossRef]
- Roedder, S.; Vitalone, M.; Khatri, P.; Sarwal, M.M. Biomarkers in solid organ transplantation: Establishing personalized transplantation medicine. Genome Med. 2011, 3, 37. [Google Scholar] [CrossRef]
- Wisniewska, M.; Banach, B.; Malinowski, D.; Domanski, L.; Sroczynski, T.; Dziedziejko, V.; Safranow, K.; Pawlik, A. VAV1 Gene Polymorphism is Associated with Kidney Allograft Rejection. Transplant. Proc. 2021, 53, 1528–1531. [Google Scholar] [CrossRef]
- Sommerer, C.; Brunet, M.; Budde, K.; Millán, O.; Guirado Perich, L.; Glander, P.; Meuer, S.; Zeier, M.; Giese, T. Monitoring of gene expression in tacrolimus-treated de novo renal allograft recipients facilitates individualized immunosuppression: Results of the IMAGEN study. Br. J. Clin. Pharmacol. 2021, 87, 3851–3862. [Google Scholar] [CrossRef]
- Kläger, J.; Eskandary, F.; Böhmig, G.A.; Kozakowski, N.; Kainz, A.; Colin Aronovicz, Y.; Cartron, J.P.; Segerer, S.; Regele, H. Renal allograft DARCness in subclinical acute and chronic active ABMR. Transpl. Int. 2021, 34, 1494–1505. [Google Scholar] [CrossRef] [PubMed]
- Han, F.; Sun, Q.; Huang, Z.; Li, H.; Ma, M.; Liao, T.; Luo, Z.; Zheng, L.; Zhang, N.; Chen, N.; et al. Donor plasma mitochondrial DNA is associated with antibody-mediated rejection in renal allograft recipients. Aging 2021, 13, 8440. [Google Scholar] [CrossRef] [PubMed]
- Groeneweg, K.E.; Duijs, J.M.; Florijn, B.W.; van Kooten, C.; de Fijter, J.W.; van Zonneveld, A.J.; Reinders, M.E.; Bijkerk, R. Circulating long noncoding RNA LNC-EPHA6 associates with acute rejection after kidney transplantation. Int. J. Mol. Sci. 2020, 21, 5616. [Google Scholar] [CrossRef] [PubMed]
- Shaw, B.I.; Cheng, D.K.; Acharya, C.R.; Ettenger, R.B.; Lyerly, H.K.; Cheng, Q.; Kirk, A.D.; Chambers, E.T. An age-independent gene signature for monitoring acute rejection in kidney transplantation. Theranostics 2020, 10, 6977. [Google Scholar] [CrossRef]
- Kim, B.W.; Kim, S.K.; Heo, K.W.; Bae, K.B.; Jeong, K.H.; Lee, S.H.; Kim, T.H.; Kim, Y.H.; Kang, S.W. Association between epidermal growth factor (EGF) and EGF receptor gene polymorphisms and end-stage renal disease and acute renal allograft rejection in a Korean population. Ren. Fail. 2020, 42, 98–106. [Google Scholar] [CrossRef]
- Sharbafi, M.H.; Assadiasl, S.; Pour-Reza-Gholi, F.; Barzegari, S.; Mohammadi Torbati, P.; Samavat, S.; Nicknam, M.H.; Amirzargar, A. TLR-2, TLR-4 and MyD88 genes expression in renal transplant acute and chronic rejections. Int. J. Immunogenet. 2019, 46, 427–436. [Google Scholar] [CrossRef]
- Guberina, H.; Rebmann, V.; Wagner, B.; da Silva Nardi, F.; Dziallas, P.; Dolff, S.; Bienholz, A.; Wohlschlaeger, J.; Bankfalvi, A.; Heinemann, F.M.; et al. Association of high HLA-E expression during acute cellular rejection and numbers of HLA class I leader peptide mismatches with reduced renal allograft survival. Immunobiology 2017, 222, 536–543. [Google Scholar] [CrossRef]
- Ge, Y.Z.; Xu, T.; Cao, W.J.; Wu, R.; Yao, W.T.; Zhou, C.C.; Wang, M.; Xu, L.W.; Lu, T.Z.; Zhao, Y.C.; et al. A molecular signature of two long non-coding RNAs in peripheral blood predicts acute renal allograft rejection. Cell. Physiol. Biochem. 2017, 44, 1213–1223. [Google Scholar] [CrossRef]
- Qiu, J.; Chen, Y.; Huang, G.; Zhang, Z.; Chen, L.; Na, N. Transforming growth factor-β activated long non-coding RNA ATB plays an important role in acute rejection of renal allografts and may impacts the postoperative pharmaceutical immunosuppression therapy. Nephrology 2017, 22, 796–803. [Google Scholar] [CrossRef]
- Liu, X.; Dong, C.; Jiang, Z.; Wu, W.K.; Chan, M.T.; Zhang, J.; Li, H.; Qin, K.; Sun, X. MicroRNA-10b downregulation mediates acute rejection of renal allografts by derepressing BCL2L11. Exp. Cell Res. 2015, 333, 155–163. [Google Scholar] [CrossRef]
- Pawlik, A.; Serdynska, M.; Dabrowska-Zamojcin, E.; Dziedziejko, V.; Safranow, K.; Domanski, L.; Ciechanowski, K. Renalase gene polymorphism in patients after renal allograft transplantation. Kidney Blood Press. Res. 2014, 39, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Pawlik, A.; Dabrowska-Zamojcin, E.; Dziedziejko, V.; Safranow, K.; Domanski, L. Association between IVS3+ 17T/C CD28 gene polymorphism and the acute kidney allograft rejection. Transpl. Immunol. 2014, 30, 84–87. [Google Scholar] [CrossRef]
- Kim, T.; Jeong, K.H.; Kim, S.; Lee, S.; Ihm, C.; Lee, T.; Moon, J.; Yoon, Y.; Chung, J.H.; Park, S.; et al. TLR9 gene polymorphism (rs187084, rs352140): Association with acute rejection and estimated glomerular filtration rate in renal transplant recipients. Int. J. Immunogenet. 2013, 40, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Suthanthiran, M.; Schwartz, J.E.; Ding, R.; Abecassis, M.; Dadhania, D.; Samstein, B.; Knechtle, S.J.; Friedewald, J.; Becker, Y.T.; Sharma, V.K.; et al. Urinary-cell mRNA profile and acute cellular rejection in kidney allografts. N. Engl. J. Med. 2013, 369, 20–31. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).