Urodynamics Are Essential to Predict the Risk for Upper Urinary Tract Damage after Acute Spinal Cord Injury
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Neuro-Urological Evaluation and Management
2.3. Predictive Measures
2.4. Statistical Analyses
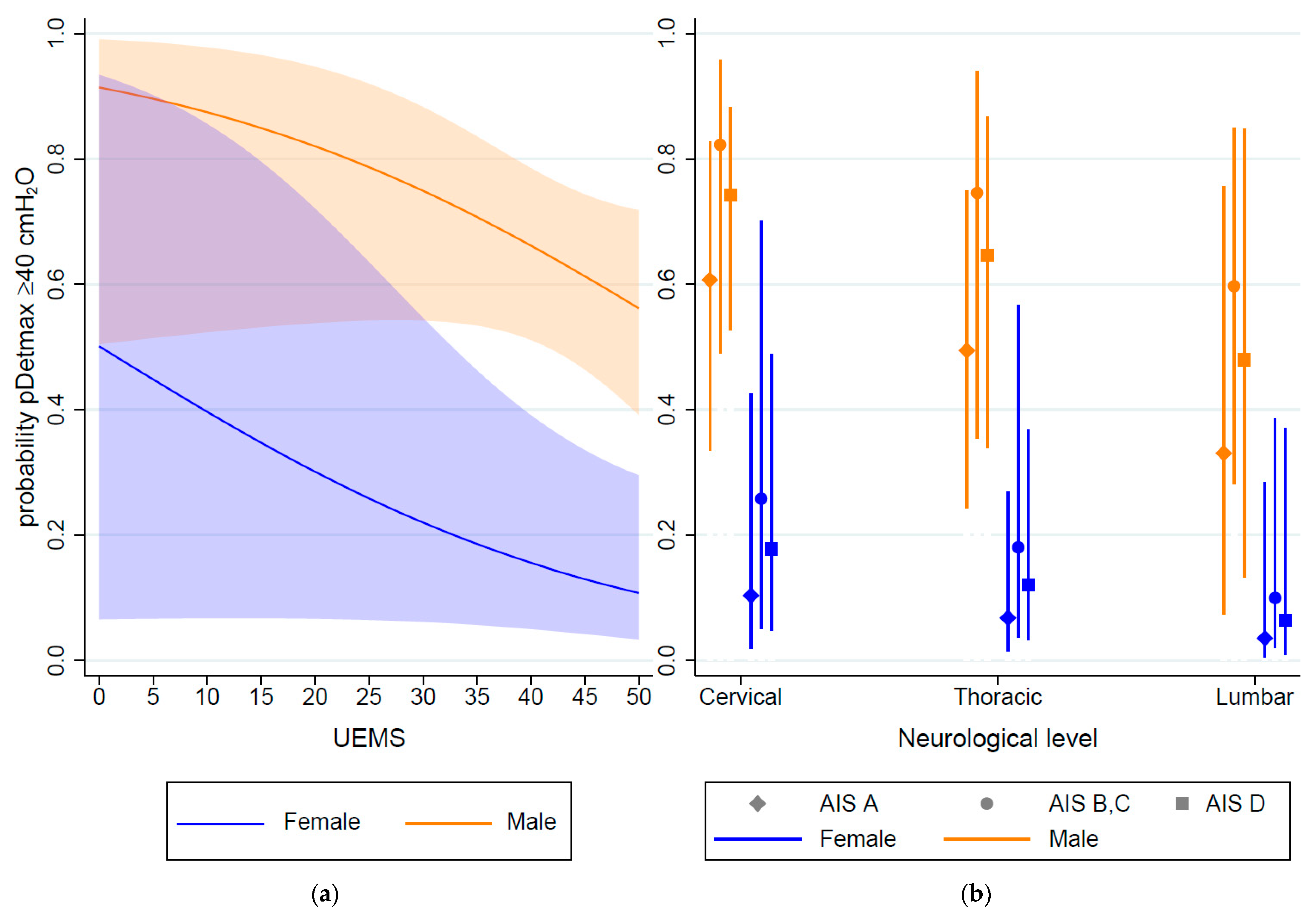
3. Results
3.1. Study Population and Prevalence of Unfavorable Urodynamic Parameters
3.2. Model Performance and Internal Validation
3.3. Sensitivity Analyses
4. Discussion
4.1. Main Findings
4.2. Findings in the Context of Existing Evidence
4.3. Implications—Practice
4.4. Implications—Research
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Panicker, J.N.; Fowler, C.J.; Kessler, T.M. Lower urinary tract dysfunction in the neurological patient: Clinical assessment and management. Lancet Neurol. 2015, 14, 720–732. [Google Scholar] [CrossRef]
- Groen, J.; Pannek, J.; Diaz, D.C.; Del Popolo, G.; Gross, T.; Hamid, R.; Karsenty, G.; Kessler, T.M.; Schneider, M.; Blok, B. Summary of European Association of Urology (EAU) guidelines on neuro-urology. Eur. Urol. 2016, 69, 324–333. [Google Scholar] [CrossRef]
- Ma, V.Y.; Chan, L.; Carruthers, K.J. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: Stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Arch. Phys. Med. Rehabil. 2014, 95, 986–995. [Google Scholar]
- Simpson, L.A.; Eng, J.J.; Hsieh, J.T.; Wolfe, D.L.; Spinal Cord Injury Rehabilitation Evidence Scire Research Team. The health and life priorities of individuals with spinal cord injury: A systematic review. J. Neurotrauma 2012, 29, 1548–1555. [Google Scholar]
- Welk, B.; Schneider, M.P.; Thavaseelan, J.; Traini, L.R.; Curt, A.; Kessler, T.M. Early urological care of patients with spinal cord injury. World J. Urol. 2018, 36, 1537–1544. [Google Scholar] [CrossRef]
- McGuire, E.J.; Woodside, J.R.; Borden, T.A.; Weiss, R.M. Prognostic value of urodynamic testing in myelodysplastic patients. J. Urol. 2002, 167 Pt 2, 1049–1053. [Google Scholar] [CrossRef]
- Shin, J.C.; Lee, Y.; Yang, H.; Kim, D.H. Clinical significance of urodynamic study parameters in maintenance of renal function in spinal cord injury patients. Ann. Rehabil. Med. 2014, 38, 353–359. [Google Scholar] [CrossRef]
- Shingleton, W.B.; Bodner, D.R. The development of urologic complications in relationship to bladder pressure in spinal cord injured patients. J. Am. Paraplegia Soc. 1993, 16, 14–17. [Google Scholar] [CrossRef]
- Lawrenson, R.; Wyndaele, J.J.; Vlachonikolis, I.; Farmer, C.; Glickman, S. Renal failure in patients with neurogenic lower urinary tract dysfunction. Neuroepidemiology 2001, 20, 138–143. [Google Scholar] [CrossRef]
- Ginsberg, D.A.; Boone, T.B.; Cameron, A.P.; Gousse, A.; Kaufman, M.R.; Keays, E.; Kennelly, M.J.; Lemack, G.E.; Rovner, E.S.; Souter, L.H.; et al. The AUA/SUFU guideline on adult neurogenic lower urinary tract dysfunction: Diagnosis and evaluation. J. Urol. 2021, 206, 1097–1105. [Google Scholar] [CrossRef]
- Abedi, A.; Sayegh, A.S.; Ha, N.T.; La Riva, A.; Perez, L.C.; Kohli, P.; Abedi, A.; Jen, R.P.; Ginsberg, D.A.; Kreydin, E.I. Health care economic burden of treatment and rehabilitation for neurogenic lower urinary tract dysfunction: A systematic review. J. Urol. 2022, 208, 773–783. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Moons, K.G.; van der Windt, D.A.; Hayden, J.A.; Perel, P.; Schroter, S.; Riley, R.D.; Hemingway, H.; Altman, D.G.; PROGRESS Group. Prognosis Research Strategy (PROGRESS) 3: Prognostic model research. PLoS Med. 2013, 10, e1001381. [Google Scholar] [CrossRef]
- Pavese, C.; Schneider, M.P.; Schubert, M.; Curt, A.; Scivoletto, G.; Finazzi-Agrò, E.; Mehnert, U.; Maier, D.; Abel, R.; Röhrich, F.; et al. Prediction of bladder outcomes after traumatic spinal cord injury: A longitudinal cohort study. PLoS Med. 2016, 13, e1002041. [Google Scholar] [CrossRef]
- Elliott, C.S.; Dallas, K.B.; Zlatev, D.; Comiter, C.V.; Crew, J.; Shem, K. Volitional voiding of the bladder after spinal cord injury: Validation of bilateral lower extremity motor function as a key predictor. J. Urol. 2018, 200, 154–160. [Google Scholar] [CrossRef]
- Kozomara, M.; Birkhäuser, V.; Anderson, C.E.; Bywater, M.; Gross, O.; Kiss, S.; Knüpfer, S.C.; Koschorke, M.; Leitner, L.; Mehnert, U.; et al. Neurogenic Lower Urinary Tract Dysfunction in the First Year After Spinal Cord Injury: A Descriptive Study of Urodynamic Findings. J. Urol. 2023, 209, 225–232. [Google Scholar] [CrossRef]
- Anderson, C.E.; Kozomara, M.; Birkhäuser, V.; Bywater, M.; Gross, O.; Kiss, S.; Knüpfer, S.C.; Koschorke, M.; Leitner, L.; Mehnert, U.; et al. Temporal development of unfavourable urodynamic parameters during the first year after spinal cord injury. BJU Int. 2023, 131, 503–512. [Google Scholar] [CrossRef]
- Rosier, P.F.; Schaefer, W.; Lose, G.; Goldman, H.B.; Guralnick, M.; Eustice, S.; Dickinson, T.; Hashim, H. International Continence Society good urodynamic practices and terms 2016: Urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol. Urodyn. 2017, 36, 1243–1260. [Google Scholar] [CrossRef]
- Gajewski, J.B.; Schurch, B.; Hamid, R.; Averbeck, M.; Sakakibara, R.; Agrò, E.F.; Dickinson, T.; Payne, C.K.; Drake, M.J.; Haylen, B.T. An International Continence Society (ICS) report on the terminology for adult neurogenic lower urinary tract dysfunction (ANLUTD). Neurourol. Urodyn. 2018, 37, 1152–1161. [Google Scholar] [CrossRef]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G.M. Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD): The TRIPOD Statement. Eur. Urol. 2015, 67, 1142–1151. [Google Scholar] [CrossRef]
- Krassioukov, A.; Biering-Sørensen, F.; Donovan, W.; Kennelly, M.; Kirshblum, S.; Krogh, K.; Alexander, M.S.; Vogel, L.; Wecht, J. International standards to document remaining autonomic function after spinal cord injury. J. Spinal. Cord. Med. 2012, 35, 201–210. [Google Scholar] [CrossRef]
- Catz, A.; Itzkovich, M.; Tesio, L.; Biering-Sorensen, F.; Weeks, C.; Laramee, M.T.; Craven, B.C.; Tonack, M.; Hitzig, S.L.; Glaser, E.; et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal. Cord. 2007, 45, 275–291. [Google Scholar] [CrossRef]
- Royston, P.; Sauerbrei, W. Multivariable Model-Building. A Pragmatic Approach to Regression Analysis Based on Fractional Polynomials for Modelling Continous Variables; Wiley Series in Probability and Statistics; Wiley: Chichester, UK, 2008. [Google Scholar]
- Fernandez-Felix, B.; García-Esquinas, E.; Muriel, A.; Royuela, A.; Zamora, J. Bootstrap internal validation command for predictive logistic regression models. Stata J. 2021, 21, 498–509. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Vickers, A.J.; Cook, N.R.; Gerds, T.; Gonen, M.; Obuchowski, N.; Pencina, M.J.; Kattan, M.W. Assessing the performance of prediction models: A framework for traditional and novel measures. Epidemiology 2010, 21, 128–138. [Google Scholar] [CrossRef]
- Sterne, J.A.; White, I.R.; Carlin, J.B.; Spratt, M.; Royston, P.; Kenward, M.G.; Wood, A.M.; Carpenter, J.R. Multiple imputation for missing data in epidemiological and clinical research: Potential and pitfalls. BMJ 2009, 338, b2393. [Google Scholar] [CrossRef]
- Spratt, M.; Carpenter, J.; Sterne, J.A.; Carlin, J.B.; Heron, J.; Henderson, J.; Tilling, K. Strategies for multiple imputation in longitudinal studies. Am. J. Epidemiol. 2010, 172, 478–487. [Google Scholar] [CrossRef]
- Sievert, K.D.; Amend, B.; Gakis, G.; Toomey, P.; Badke, A.; Kaps, H.P.; Stenzl, A. Early sacral neuromodulation prevents urinary incontinence after complete spinal cord injury. Ann. Neurol. 2010, 67, 74–84. [Google Scholar] [CrossRef]
- Stampas, A.; Gustafson, K.; Korupolu, R.; Smith, C.; Zhu, L.; Li, S. Bladder neuromodulation in acute spinal cord injury via transcutaneous tibial nerve stimulation: Cystometrogram and autonomic nervous system evidence from a randomized control pilot trial. Front. Neurosci. 2019, 13, 119. [Google Scholar] [CrossRef]
- Redshaw, J.D.; Lenherr, S.M.; Elliott, S.P.; Stoffel, J.T.; Rosenbluth, J.P.; Presson, A.P.; Myers, J.B. Protocol for a randomized clinical trial investigating early sacral nerve stimulation as an adjunct to standard neurogenic bladder management following acute spinal cord injury. BMC Urol. 2018, 18, 72. [Google Scholar] [CrossRef]
- Birkhäuser, V.; Liechti, M.D.; Anderson, C.E.; Bachmann, L.M.; Baumann, S.; Baumberger, M.; Birder, L.A.; Botter, S.M.; Büeler, S.; Cruz, C.D.; et al. TASCI-transcutaneous tibial nerve stimulation in patients with acute spinal cord injury to prevent neurogenic detrusor overactivity: Protocol for a nationwide, randomised., sham-controlled, double-blind clinical trial. BMJ Open 2020, 10, e039164. [Google Scholar] [CrossRef]
- Kreydin, E.; Welk, B.; Chung, D.; Clemens, Q.; Yang, C.; Danforth, T.; Gousse, A.; Kielb, S.; Kraus, S.; Mangera, A.; et al. Surveillance and management of urologic complications after spinal cord injury. World J. Urol. 2018, 36, 1545–1553. [Google Scholar] [CrossRef]
- Bywater, M.; Tornic, J.; Mehnert, U.; Kessler, T.M. Detrusor Acontractility after Acute Spinal Cord Injury-Myth or Reality? J. Urol. 2018, 199, 1565–1570. [Google Scholar] [CrossRef]
- Çetinel, B.; Önal, B.; Can, G.; Talat, Z.; Erhan, B.; Gündüz, B. Risk factors predicting upper urinary tract deterioration in patients with spinal cord injury: A retrospective study. Neurourol. Urodyn. 2017, 36, 653–658. [Google Scholar] [CrossRef]
- Swatesutipun, V.; Tangpaitoon, T. The safety cutoff storage pressure for preventing upper urinary tract damage in neurogenic bladder from spinal cord pathology and risk factor analysis. Neurourol. Urodyn. 2022, 41, 991–1001. [Google Scholar] [CrossRef]
- Hashim, H.; Ellis-Jones, J.; Swithinbank, L.; Woodward, M.; Small, D.; Frank, J.D.; Abrams, P. Trying to predict ‘dangerous’ bladders in children: The area under the curve concept. J. Pediatr. Urol. 2005, 1, 343–347. [Google Scholar] [CrossRef]

| Characteristic (% Missing) | Overall Population, N = 97 | 12-Month UDI Present, N = 73 | Missed 12-Month UDI, N = 24 | |
|---|---|---|---|---|
| Baseline continuous variables | Median (Q1–Q3) | Median (Q1–Q3) | Median (Q1–Q3) | p-value |
| Age at SCI (0) | 57 (42–69) | 56 (45–69) | 60 (40–72) | 0.56 |
| Lower extremity motor score (LEMS) (5) | 33 (1–48) | 32 (2–48) | 40 (0–47) | 0.98 |
| Upper extremity motor score (UEMS) (5) | 50 (38–50) | 50 (41–50) | 50 (27–50) | 0.69 |
| SCIM Score (2) | 36 (22–68) | 37 (22–74) | 31 (22–59) | 0.55 |
| SCIM Respiratory-Sphincter Subscale (2) | 15 (12–25) | 15 (15–25) | 14 (10–25) | 0.32 |
| Baseline categorical variables | n (%) | n (%) | n (%) | p-value |
| Sex (0) | 0.36 | |||
| Female | 33 (34) | 23 (32) | 10 (42) | |
| Male | 64 (66) | 50 (68) | 14 (58) | |
| Lesion etiology (0) | 0.17 | |||
| Traumatic spinal cord injury | 75 (77) | 54 (74) | 21 (87) | |
| Ischemic spinal cord injury | 22 (23) | 19 (26) | 3 (13) | |
| Neurological Level (5) a | 0.88 | |||
| Cervical (C1–C8) | 43 (44) | 33 (45) | 10 (41) | |
| Thoracic (T1–T12) | 37 (38) | 28 (38) | 9 (38) | |
| Lumbar (L1–L5) | 17 (18) | 12 (17) | 5 (21) | |
| SCI Severity (5) a | 0.64 | |||
| AIS A | 21 (22) | 18 (25) | 3 (13) | |
| AIS B | 10 (10) | 7 (10) | 3 (13) | |
| AIS C | 16 (16) | 12 (16) | 4 (16) | |
| AIS D | 50 (52) | 36 (49) | 14 (58) | |
| S3 light touch score (6) | 0.45 | |||
| Absent | 25 (26) | 21 (29) | 4 (17) | |
| Altered | 46 (47) | 33 (45) | 13 (54) | |
| Normal | 20 (21) | 14 (19) | 6 (25) | |
| Outcomevariables | n (%) | n (%) | n (%) | p-value |
| DO–DSD (0) b | <0.01 | |||
| No | 12 (12) | 5 (7) | 7 (29) | |
| Yes | 85 (88) | 68 (93) | 17 (71) | |
| pDetmax ≥ 40 cmH2O (0) b | <0.001 | |||
| No | 59 (61) | 39 (53) | 20 (83) | |
| Yes | 38 (39) | 34 (47) | 4 (17) | |
| Vesicoureteral reflux (1) b | 0.12 | |||
| No | 89 (92) | 66 (90) | 23 (96) | |
| Yes | 7 (7) | 7 (10) | 0 (0) | |
| Any unfavorable UDI parameter (1) b | <0.01 | |||
| No | 9 (9) | 3 (4) | 6 (25) | |
| Yes | 87 (90) | 70 (96) | 17 (71) |
| Characteristic (% Missing) | No DO–DSD | DO–DSD | No pDetmax ≥ 40 cmH2O | pDetmax ≥ 40 cmH2O | No VUR | VUR | No Unfavorable UDI Parameters | Unfavorable UDI Parameters | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | n = 5 | n = 85 | n = 39 | n = 38 | n = 66 | n = 7 | n = 3 | n = 87 | ||||
| Continuous variables | Median (Q1–Q3) | Median (Q1–Q3) | p-value | Median (Q1–Q3) | Median (Q1–Q3) | p-value | Median (Q1–Q3) | Median (Q1–Q3) | p-value | Median (Q1–Q3) | Median (Q1–Q3) | p-value |
| Age at SCI (0) | 35 (34–67) | 57 (47–71) | 0.36 | 55 (36–71) | 57 (45–66) | 0.73 | 56 (49–70) | 57 (32–69) | 0.90 | 35 (34–67) | 57 (45–71) | 0.32 |
| LEMS (5) | 28 (0–50) | 32 (2–47) | 0.96 | 32 (5–48) | 25 (0–50) | 0.67 | 33 (3–50) | 5 (0–16) | 0.054 | 50 (0–50) | 31 (2–47) | 0.41 |
| UEMS (5) | 48 (15–50) | 50 (36–50) | 0.46 | 50 (47–50) | 45 (21–50) | <0.01 | 50 (39–50) | 50 (20–50) | 0.92 | 50 (48–50) | 50 (35–50) | 0.43 |
| SCIM Respiratory-Sphincter subscale (2) | 62 (21–96) | 34 (22–59) | 0.42 | 38 (26–74) | 35 (14–68) | 0.26 | 38 (23–74) | 27 (20–45) | 0.45 | 92 (31–100) | 34 (21–58) | 0.091 |
| Categorical variables | n (%) | n (%) | p-value | n (%) | n (%) | p-value | n (%) | n (%) | p-value | n (%) | n (%) | p-value |
| Sex (0) | 0.65 | <0.0001 | 0.42 | >0.99 | ||||||||
| Female | 1 (20) | 31 (36) | 20 (51) | 3 (8) | 22 (33) | 1 (14) | 1 (33) | 31 (36) | ||||
| Male | 4 (80) | 54 (64) | 19 (49) | 35 (92) | 44 (67) | 6 (86) | 2 (67) | 56 (64) | ||||
| Lesion etiology (0) | >0.99 | 0.021 | 0.18 | >0.99 | ||||||||
| Traumatic spinal cord injury | 4 (80) | 64 (75) | 25 (64) | 33 (87) | 47 (71) | 7 (100) | 2 (67) | 66 (76) | ||||
| Ischemic spinal cord injury | 1 (20) | 21 (25) | 14 (36) | 5 (13) | 19 (29) | 0 (0) | 1 (33) | 21 (24) | ||||
| Neurological Level (5) a | 0.38 | 0.23 | 0.51 | >0.99 | ||||||||
| Cervical (C1–C8) | 4 (80) | 36 (42) | 14 (36) | 21 (55) | 31 (47) | 2 (29) | 2 (67) | 38 (44) | ||||
| Thoracic (T1–T12) | 1 (20) | 34 (40) | 17 (44) | 12 (32) | 25 (38) | 3 (42) | 1 (33) | 34 (39) | ||||
| Lumbar (L1–L5) | 0 (0) | 15 (18) | 8 (20) | 5 (13) | 10 (15) | 2 (29) | 0 (0) | 15 (17) | ||||
| SCI Severity (5) a | 0.10 | 0.40 | 0.10 | 0.61 | ||||||||
| AIS A | 3 (60) | 18 (21) | 10 (26) | 8 (21) | 15 (23) | 3 (43) | 1 (33) | 20 (23) | ||||
| AIS B/C | 0 (0) | 23 (27) | 8 (20) | 13 (34) | 16 (24) | 3 (43) | 0 (0) | 23 (26) | ||||
| AIS D | 2 (40) | 44 (52) | 21 (54) | 17 (45) | 35 (53) | 1 (14) | 2 (67) | 44 (51) | ||||
| S3 light touch score (6) | 0.27 | 0.60 | 0.13 | 0.065 | ||||||||
| Absent | 2 (40) | 23 (27) | 11 (28) | 10 (26) | 17 (26) | 1 (14) | 1 (33) | 24 (28) | ||||
| Altered | 1 (20) | 42 (49) | 20 (51) | 16 (42) | 32 (48) | 2 (29) | 0 (0) | 43 (49) | ||||
| Normal | 2 (40) | 15 (18) | 6 (15) | 9 (24) | 12 (18) | 0 (0) | 2 (67) | 15 (17) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Birkhäuser, V.; Anderson, C.E.; Kozomara, M.; Bywater, M.; Gross, O.; Kiss, S.; Knüpfer, S.C.; Koschorke, M.; Leitner, L.; Mehnert, U.; et al. Urodynamics Are Essential to Predict the Risk for Upper Urinary Tract Damage after Acute Spinal Cord Injury. Biomedicines 2023, 11, 1748. https://doi.org/10.3390/biomedicines11061748
Birkhäuser V, Anderson CE, Kozomara M, Bywater M, Gross O, Kiss S, Knüpfer SC, Koschorke M, Leitner L, Mehnert U, et al. Urodynamics Are Essential to Predict the Risk for Upper Urinary Tract Damage after Acute Spinal Cord Injury. Biomedicines. 2023; 11(6):1748. https://doi.org/10.3390/biomedicines11061748
Chicago/Turabian StyleBirkhäuser, Veronika, Collene E. Anderson, Marko Kozomara, Mirjam Bywater, Oliver Gross, Stephan Kiss, Stephanie C. Knüpfer, Miriam Koschorke, Lorenz Leitner, Ulrich Mehnert, and et al. 2023. "Urodynamics Are Essential to Predict the Risk for Upper Urinary Tract Damage after Acute Spinal Cord Injury" Biomedicines 11, no. 6: 1748. https://doi.org/10.3390/biomedicines11061748
APA StyleBirkhäuser, V., Anderson, C. E., Kozomara, M., Bywater, M., Gross, O., Kiss, S., Knüpfer, S. C., Koschorke, M., Leitner, L., Mehnert, U., Sadri, H., Sammer, U., Stächele, L., Tornic, J., Liechti, M. D., Brinkhof, M. W. G., & Kessler, T. M. (2023). Urodynamics Are Essential to Predict the Risk for Upper Urinary Tract Damage after Acute Spinal Cord Injury. Biomedicines, 11(6), 1748. https://doi.org/10.3390/biomedicines11061748







