Abstract
Purpose: The purpose of this study is to observe how preoperative sarcopenia and hypoalbuminemia affect the oncological outcome of nonmetastatic renal cell carcinoma (RCC) after partial or radical nephrectomy. Methods: This study retrospectively analyzes 288 Japanese patients with nonmetastatic RCC who underwent radical treatment at Kanazawa University Hospital between October 2007 and December 2018. Relationships between sarcopenia as indicated by the psoas muscle mass index and hypoalbuminemia (albumin ≤ 3.5 g/dL) with overall survival (OS) and metastasis-free survival (MFS) were determined. Results: The study found that 110 (38.2%) of the 288 patients were sarcopenic and 29 (10.1%) had hypoalbuminemia. The combination of sarcopenia and hypoalbuminemia was associated with a shorter OS and MFS (p for trend = 0.0007 and <0.0001, respectively), according to Kaplan–Meier curves. The concurrent presence of sarcopenia and hypoalbuminemia were found to be significant and independent predictors of poor MFS (hazard ratio (HR), 2.96; 95% confidence interval (95% CI), 1.05–8.39; p = 0.041) and poor OS (HR, 6.87; 95% CI, 1.75–26.94; p = 0.006), respectively. Conclusions: In Japanese patients with surgically treated nonmetastatic RCC, combined preoperative sarcopenia and hypoalbuminemia was a significant predictor of poor survival.
1. Introduction
Predictive tools to accurately assess the risk of mortality, recurrence, and postoperative complications are extremely useful in real-world clinical practice. At present, prognostic models, such as pathological tumor stages, tumor size, nuclear grade, and histologic tumor necrosis, are tumor-centric and require data derived from the final pathology specimen [1,2]. However, cancer prognosis is influenced not only by tumor characteristics, but also by a patient’s physical condition, with a particular emphasis on inflammatory and nutritional status. The development and validation of prognostic models that incorporate readily available baseline clinical data to inform decision making and treatment selection are gaining popularity.
Sarcopenia is a progressive and common skeletal muscle disease characterized by reduced skeletal muscle mass and function [3]. Sarcopenia pathogenesis is complex, and several mechanisms are thought to contribute to the phenotype, including hormone function, redistribution of muscle fiber, decreased number of motor units, decreased number and regenerative capacity of satellite cells, inflammatory pathways, and intracellular changes in proteostasis and mitochondrial function [4]. Several existing studies suggest that skeletal muscle mass more accurately represents body composition than body mass index (BMI), demonstrating that BMI is an inadequate surrogate for both muscle mass and adiposity, and is not consistently associated with survival in patients with several cancers [5,6]. In contrast, several recent studies have confirmed that the onset of sarcopenia is closely related to the treatment and prognosis of many cancers, including hepatocellular, pancreaticobiliary, gastroesophageal, colorectal, and urothelial carcinomas [7,8].
Serum albumin is a simple and inexpensive marker of systemic inflammation, as well as a surrogate for nutritional status and a strong prognostic factor in cancer patients [9,10]. Furthermore, albumin has been shown to be a prognostic factor and predictive marker of treatment response in many cancer types when combined with C-reactive protein (CRP), fibrinogen, globulin, and lymphocyte [11,12,13,14,15,16,17,18]. Malnutrition, routinely indicated by decreased in serum albumin and low BMI, is often comorbid with sarcopenia and may accelerate the process of muscle degeneration [19]. Although the independent association of sarcopenia and albumin with mortality in patients with renal cell carcinoma (RCC) is well known, there have been few studies on the relationship between sarcopenia and albumin status and RCC. Thus, this study retrospectively aims to investigate the potential associations between sarcopenia and hypoalbuminemia and oncological outcomes in Japanese patients with nonmetastatic RCC after curative surgery.
2. Patients and Methods
2.1. Patients
This retrospective study included patients with nonmetastatic RCC (T1–T4, N0, and M0), who underwent partial or radical nephrectomy at Kanazawa University Hospital between October 2007 and December 2018. According to our previous study [14], the inclusion and exclusion criteria were established. The inclusion criteria were set as follows: (I) age of 18 years or older; (II) confirmed imaging or histologic diagnosis of RCC; and (III) complete electronic medical records, including clinical laboratory tests within one month before surgery. We excluded patients who did not undergo surgical therapy. Furthermore, the Medical Ethics Committee of Kanazawa University (2018-116) approved this study [14]. All research was performed in accordance with relevant guidelines and regulations and the Declaration of Helsinki. The requirement for informed consent was waived by the Medical Ethics Committee of Kanazawa University due to the observational nature of the study using only existing data. Instead, information on this study will be posted on the Kanazawa University Hospital website, and patients are free to revoke their consent at any point.
2.2. Data Collection and Variable Definitions
Age, gender, BMI, psoas muscle mass index (PMI), Karnofsky performance status (KPS), Charlson comorbidity index (CCI), smoking history, medical conditions, such as hypertension and diabetes, and preoperative serum biomarkers, such as CRP and albumin concentration, were collected at the time of surgery. In addition, baseline oncological data were obtained, including pathological tumor stage and size, histological subtype, histological nuclear grade, and lymphovascular invasion. The pathological stage was determined using the Union for International Cancer Control’s (2017) tumor–node–metastasis (TNM) classification of malignant tumors (eighth edition).
Overall survival (OS) and metastasis-free survival (MFS) were calculated as the time from the date of surgery to death from any cause and the first detection of RCC metastasis, respectively.
2.3. Assessment of Sarcopenia and Hypoalbuminemia
The PMI is a straightforward method of expressing total body skeletal muscle mass that is often used to assess sarcopenia cases. The total psoas muscle cross-sectional area at the L3 vertebral level was manually measured by tracing preoperative computed tomography images, and PMI (mm2/m2) was calculated by multiplying the total psoas muscle area (mm2) by the square of the patient’s height (m2) [20]. In this study, the optimal cutoff value for PMI was determined by using the point closest to (0, 1) on the receiver operating curve (ROC) [21]. A 3.5 g/dL cutoff was used to distinguish between normal and low serum albumin levels according to a previous study [22]. Patients were divided into four groups to study the effects of sarcopenia and serum albumin together: non-sarcopenia and albumin > 3.5, sarcopenia and albumin > 3.5, non-sarcopenia and albumin ≤ 3.5, and sarcopenia and albumin ≤ 3.5.
2.4. Statistical Analysis
The chi-squared test and one-way analysis of variance (ANOVA) were used to compare differences in the patients’ characteristics. The Kaplan–Meier method was used to estimate OS and MFS, and the log-rank and log-rank trend tests were used to compare them. To assess the association of sarcopenia and albumin status with MFS and OS, univariate and multivariate analyses were performed using Cox proportional hazards models. Statistical analyses were performed using GraphPad Prism version 6.07 (GraphPad Software Inc., San Diego, CA, USA) and IBM SPSS Statistics version 25 (IBM Corp., Armonk, NY, USA). Statistical significance was indicated by a p-value of <0.05.
3. Results
3.1. Patient and Disease Characteristics
The data were extracted from 288 patients with T1–T4, N0, and M0 RCC who underwent partial or radical nephrectomies. Table 1 shows the demographics of all the patients. The study population’s median follow-up period was 4.38 yr (range, 0.02–14.71 yr). Most patients were males (72.2%) and the median age of the 288 patients was 63 yr (interquartile range (IQR), 55–71 yr), and 110 (38.2%) and 29 (10.1%) patients were diagnosed with sarcopenia and hypoalbuminemia (albumin ≤ 3.5 g/dL), respectively. The median BMI, PMI, serum albumin concentration, serum CRP level, and tumor size of the entire cohort were 23.7 kg/m2 (IQR, 21.7–26.4 kg/m2), 468.2 mm2/m2 (IQR, 352.9–571.7 mm2/m2), 4.2 g/dL (IQR, 3.9–4.5 g/dL), 0.1 mg/dL (IQR, 0.1–0.2 mg/dL), and 2.9 cm (IQR, 2.0–4.93 cm), respectively. Patients had a radical nephrectomy (50.3%), clear cell histology (85.1%), ≥pT3 (17.7%), nuclear grade ≥ 3 disease (17.0%), and lymphovascular invasion (47.9%).

Table 1.
Patient demographics (n = 288).
3.2. The Optimal Thresholds for PMI
The ROC analysis was used to determine the optimal cutoff value for PMI using OS as the end point. The ROC revealed that the optimal PMI cutoff value for males was 516.8 mm2/m2 (area under curve (AUC), 0.573; 95% CI, 0.457–0.688; p = 0.3081, with sensitivity of 61.1% and specificity of 53.8%) and 235.1 mm2/m2 for females (AUC, 0.686; 95% CI, 0.437–0.934; p = 0.2118, with sensitivity of 50%). Sarcopenia was defined as any measurement that was lower than each PMI value.
3.3. Association of Clinicopathological Parameters with Sarcopenia and Albumin
As shown in Table 2, patients were stratified into groups based on their sarcopenia and albumin status to investigate significant associations between covariates using ANOVA. The variables of age, gender, KPS, CCI, BMI, CRP, tumor size, pathological T-stage, nuclear grade, and lymphovascular invasion demonstrated significant associations within an integrated model considering both sarcopenia and hypoalbuminemia.

Table 2.
Summary of clinicopathological characteristics according to preoperative sarcopenia and albumin status.
3.4. Survival Rates and Prognostic Factors
During the study period, 42 patients developed metastatic recurrence and 21 patients died, eight of whom died from RCC. Figure 1 shows the results of the Kaplan–Meier analysis for OS and MFS in all patients stratified by sarcopenia and albumin status. There was a statistically significant difference in OS (p = 0.0011), and concurrent sarcopenia and hypoalbuminemia tended to worsen survival (p for trend = 0.0007, Figure 1a). The 5-year OS values for non-sarcopenia and albumin > 3.5, sarcopenia and albumin > 3.5, non-sarcopenia and albumin ≤ 3.5, and sarcopenia and albumin ≤ 3.5 groups were 96.4%, 93.7%, 82.5%, and 86.5%, respectively. Furthermore, the MFS varied significantly (p < 0.0001) between the four groups, and concurrent sarcopenia and hypoalbuminemia tended to increase metastasis (p for trend < 0.0001, Figure 1b). The 5-year MFS values for non-sarcopenia and albumin > 3.5, sarcopenia and albumin > 3.5, non-sarcopenia and albumin ≤ 3.5, and sarcopenia and albumin ≤ 3.5 groups were 90.9%, 81.3%, 58.3%, and 42.9%, respectively. Sarcopenia and albumin status were significantly associated with shorter MFS in the multivariate analysis of the prognostic factors (non-sarcopenia, albumin ≤ 3.5: hazard ratio (HR), 4.79; 95% CI, 1.44–15.89; p = 0.010; sarcopenia, albumin ≤ 3.5: HR, 2.96; 95% CI, 1.05–8.39; p = 0.041, Table 3). Furthermore, for the multivariate analysis, a stepwise increase in HRs and a decrease in p-values were observed with increasing risk in the OS composite prognostic models that included both sarcopenia and hypoalbuminemia (sarcopenia, albumin > 3.5: HR, 3.64; 95% CI, 1.21–10.90; p = 0.021; non-sarcopenia, albumin ≤ 3.5: HR, 5.87; 95% CI, 1.39–24.73; p = 0.016; sarcopenia, albumin ≤ 3.5: HR, 6.87; 95% CI, 1.75–26.94; p = 0.006, Table 4).
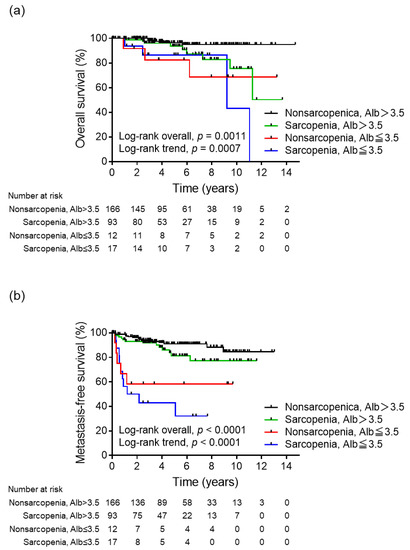
Figure 1.
Kaplan–Meier analyses for (a) overall survival and (b) metastasis-free survival based on the sarcopenia and albumin status, respectively.

Table 3.
Univariate and multivariate analyses of the association between clinicopathological characteristics and metastasis-free survival.

Table 4.
Univariate and multivariate analyses of the association between clinicopathological characteristics and overall survival.
4. Discussion
The need for better prognostic models based on preoperative parameters in localized RCC remains an important challenge. Previous research has demonstrated a significant association between sarcopenia and an elevated risk of mortality and recurrence following nephrectomy in both localized and metastatic RCCs [23,24,25,26,27]. Furthermore, a recent meta-analysis found that patients with malignant neoplasms, including RCC and sarcopenia, had worse clinical outcomes than those who did not [28]. Interestingly, recent research has shown that preoperative sarcopenia and elevated systemic inflammatory markers, such as the modified Glasgow Prognostic Score including both CRP and albumin levels, were associated with a decreased survival [29,30]. Furthermore, a recent retrospective study found that patients with localized RCC who had both sarcopenia and hypoalbuminemia prior to surgery had a two-to-three-fold reduction in OS and recurrence-free survival after nephrectomy in an American population [22]. Hypoalbuminemia, weight loss, and low BMI are commonly utilized indicators for evaluating nutritional deficiencies in patients with RCC [31]. Nevertheless, relying solely on BMI to elucidate changes in body mass may yield unreliable prognostic information, as it may not accurately capture specific shifts between lean and adipose tissues [32]. This is particularly significant in the case of patients with sarcopenic obesity, as the presence of stable or increased adiposity may camouflage detrimental alterations in skeletal muscle [6]. In contrast, sarcopenia has been consistently linked to nutritional deficiencies in both cancer and non-cancer patients [3]. Overall, assessing body composition and nutritional status prior to surgery may help urologists and oncologists make treatment decisions.
The present study examined the relationship between preoperative sarcopenia and albumin status, as well as postoperative survival outcomes in Japanese patients with nonmetastatic RCC who had nephrectomy. The findings confirm that the presence of sarcopenia, as indicated by low PMI, and hypoalbuminemia is not only associated with significantly worse MFS values, but also with decreased OS after radical surgery for nonmetastatic RCC, and that a combined model of sarcopenia and hypoalbuminemia is an independent poor prognostic factor for MFS and OS.
The correlation between sarcopenia and heightened mortality could potentially be attributed to the interplay between factors, such as low muscle mass, malnutrition, and systemic inflammation [22]. Accumulating evidence indicates that the nutritional and immune statuses are involved in the onset and advancement of cancer, consequently impacting survival outcomes [33]. Sarcopenia was found to be an independent predictor of OS (HR, 1.83; 95% CI, 1.41–2.37), cancer-specific survival (CSS) (HR, 1.78; 95% CI, 1.34–2.36), and progression-free survival (PFS) (HR, 1.98; 95% CI, 1.34–2.92) in a recent meta-analysis involving 3591 patients with RCC [34]. Furthermore, a recent umbrella review concluded that sarcopenia was significantly associated with multiple health-related outcomes, such as dysphagia, cognitive impairment, fractures, falls, and hospitalization in older populations, whether or not tumors were present [35]. Otherwise, in a prior investigation conducted at our institution, which encompassed 299 patients with surgically treated nonmetastatic RCC, we presented evidence indicating that sarcopenia served as a substantial indicator of unfavorable pathological outcomes and diminished survival prognosis [27]. Serum albumin, on the other hand, is an objective indicator of nutritional status and clinical inflammation, implying that its expression is reduced in inflammatory conditions [36]. Hypoalbuminemia has been linked to an increased in overall mortality in patients undergoing surgery for both localized and metastatic RCCs [31,37]. Furthermore, a recent meta-analysis involving 2863 patients with metastatic RCC treated with tyrosine kinase inhibitors showed that a lower pre-treatment serum albumin level was related to poorer OS (dichotomous: HR, 2.01; 95% CI, 1.64–2.46; p < 0.001; I2 = 28.8%; continuous: HR, 0.93; 95% CI, 0.86–1.00; p = 0.040; I2 = 67.5%) [38]. Interestingly, recent oncologic studies evaluating the utility of serum albumin in prognostic models have primarily evaluated it in combination with other biomarkers. The prognostic nutritional index (PNI), which integrates lymphocyte count and serum albumin levels, is widely regarded as a comprehensive measure reflecting the nutritional and immunological status related to cancer. As patients with a lower PNI may experience a compromised antitumor response and subsequently exhibit decreased survival rates, PNI serves as a valuable tool for clinicians to anticipate optimal preoperative medical interventions and determine the ideal timing for surgical procedures [33,39]. A decreased PNI was found to be a significant predictor of worse OS (HR, 2.00; 95% CI, 1.64–2.42; p < 0.001), CSS (HR, 2.54; 95% CI, 1.61–4.00; p < 0.001), and PFS (HR, 2.12; 95% CI, 1.82–2.46; p < 0.001) in a recent meta-analysis involving 7629 patients with RCC [40]. Otherwise, in a previous study at our institution involving 213 patients with nonmetastatic RCCs, we demonstrated that the combination of serum CRP and albumin is a predictor of postoperative recurrence [14].
Because sarcopenia and hypoalbuminemia strongly reflect nutritional status and systemic inflammation and are independently associated with poor treatment outcomes and survival in RCC, it stands to reason that this combined model can be used as a powerful prognostic marker in patients with nonmetastatic RCC. To our knowledge, this study represents the initial investigation into the biomarkers of sarcopenia and hypoalbuminemia, specifically in Japanese patients with nonmetastatic RCC. All the biomarkers assessed in this study are readily obtainable through routine blood tests or imaging studies, offering the potential for straightforward and replicable prognostic markers, distinct from the previous research. Thus, the pretreatment assessment of sarcopenia and measurement of albumin levels may be of great help in predicting prognosis after surgical treatment for patients with nonmetastatic RCC. Based on these findings, clinicians can contribute to the identification of patients with a compromised nutritional status and poor body composition who may potentially benefit from additional resources and interventions.
Early intervention with muscle-building exercise programs and nutritional supplements linked to both myoprotein synthesis and anti-inflammatory pathways has been shown to reduce mortality and improve muscle composition in cancer patients [29,41,42]. Interestingly, a recent study discovered that the dynamics in sarcopenia status from pre- to postoperative stages served as a substantial prognostic factor for survival outcomes, suggesting the significance of maintaining optimal nutritional status before and after surgery to enhance long-term survival in patients with RCC [43]. Nutritional interventions aim to maintain or improve dietary intake, skeletal muscle mass, and physical performance, and reduce metabolic abnormalities. To meet all nutrient and micronutrient requirements, cancer patients should consume a high-energy diet rich in high-density foods, including fats, and have a high-protein intake. Furthermore, artificial nutrition and antioxidant supplementation should be used as needed. Multimodal training (combining various methods of physical training, such as aerobic and strength exercises, with pharmacotherapy and nutritional supplementation) can be an interesting strategy for improving the results [44]. Thus, conducting preoperative assessments of body composition and nutritional status to identify patients with modifiable risk factors, along with implementing a multimodal approach to managing body composition throughout all stages of the disease, may play a crucial role in enhancing patient outcomes.
There were several limitations to this study. Manual tracing was used to collect PMI data; however, this study did not investigate the correlation between PMI and total skeletal muscle mass. Furthermore, it should be noted that the cutoff values for PMI varied among different racial populations, and specific cutoff values for each race were not established. Furthermore, because of the complex sequential treatment using various currently available agents, such as molecularly targeted drugs and immune checkpoint inhibitors, the systemic treatment of patients with recurrent metastatic RCC after radical surgery was not detailed in this study. Furthermore, recent significant advances in surgical treatment may have had an impact on these prognostic analyses. Finally, the sample size and observation period may be insufficient to precisely determine the statistical significance. The present study, on the other hand, confirmed that sarcopenia, defined here as low PMI, and hypoalbuminemia are both independent predictors of survival in patients surgically treated for nonmetastatic RCC. More large-scale studies are needed to confirm these findings.
5. Conclusions
According to the findings of this retrospective study, Japanese patients with nonmetastatic RCC and concurrent sarcopenia and hypoalbuminemia had a higher incidence of metastasis and poor prognosis. Evaluating body composition and albumin status may be useful for prognostic risk stratification in patients with nonmetastatic RCC who are undergoing surgical treatment, as well as for identifying patients who require early nutritional and exercise interventions aiming to maintain or improve food intake and skeletal muscle mass and function.
Author Contributions
Conceptualization, T.M.; methodology, T.M.; validation, T.M.; formal analysis, T.M.; investigation, T.M.; resources, T.M.; data curation, T.M.; writing—original draft preparation, T.M.; writing—review and editing, K.I., H.I. and S.K.; visualization, T.M.; supervision, A.M.; project administration, T.M. and K.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Medical Ethics Committee of Kanazawa University (2018-116).
Informed Consent Statement
Patient consent was waived by the Medical Ethics Committee of Kanazawa University due to an observational study using only existing information.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Klatte, T.; Rossi, S.H.; Stewart, G.D. Prognostic factors and prognostic models for renal cell carcinoma: A literature review. World J. Urol. 2018, 36, 1943–1952. [Google Scholar] [CrossRef] [PubMed]
- Parker, W.P.; Cheville, J.C.; Frank, I.; Zaid, H.B.; Lohse, C.M.; Boorjian, S.A.; Leibovich, B.C.; Thompson, R.H. Application of the Stage, Size, Grade, and Necrosis (SSIGN) Score for Clear Cell Renal Cell Carcinoma in Contemporary Patients. Eur. Urol. 2017, 71, 665–673. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyere, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Wiedmer, P.; Jung, T.; Castro, J.P.; Pomatto, L.C.D.; Sun, P.Y.; Davies, K.J.A.; Grune, T. Sarcopenia—Molecular mechanisms and open questions. Ageing Res. Rev. 2021, 65, 101200. [Google Scholar] [CrossRef]
- Caan, B.J.; Meyerhardt, J.A.; Kroenke, C.H.; Alexeeff, S.; Xiao, J.; Weltzien, E.; Feliciano, E.C.; Castillo, A.L.; Quesenberry, C.P.; Kwan, M.L.; et al. Explaining the Obesity Paradox: The Association between Body Composition and Colorectal Cancer Survival (C-SCANS Study). Cancer Epidemiol. Biomark. Prev. 2017, 26, 1008–1015. [Google Scholar] [CrossRef]
- Prado, C.M.; Lieffers, J.R.; McCargar, L.J.; Reiman, T.; Sawyer, M.B.; Martin, L.; Baracos, V.E. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: A population-based study. Lancet Oncol. 2008, 9, 629–635. [Google Scholar] [CrossRef] [PubMed]
- Joglekar, S.; Nau, P.N.; Mezhir, J.J. The impact of sarcopenia on survival and complications in surgical oncology: A review of the current literature. J. Surg. Oncol. 2015, 112, 503–509. [Google Scholar] [CrossRef]
- Shachar, S.S.; Williams, G.R.; Muss, H.B.; Nishijima, T.F. Prognostic value of sarcopenia in adults with solid tumours: A meta-analysis and systematic review. Eur. J. Cancer 2016, 57, 58–67. [Google Scholar] [CrossRef]
- Gupta, D.; Lis, C.G. Pretreatment serum albumin as a predictor of cancer survival: A systematic review of the epidemiological literature. Nutr. J. 2010, 9, 69. [Google Scholar] [CrossRef]
- Meyer, C.P.; Rios-Diaz, A.J.; Dalela, D.; Ravi, P.; Sood, A.; Hanske, J.; Chun, F.K.H.; Kibel, A.S.; Lipsitz, S.R.; Sun, M.; et al. The association of hypoalbuminemia with early perioperative outcomes—A comprehensive assessment across 16 major procedures. Am. J. Surg. 2017, 214, 871–883. [Google Scholar] [CrossRef]
- Proctor, M.J.; Morrison, D.S.; Talwar, D.; Balmer, S.M.; O’Reilly, D.S.; Foulis, A.K.; Horgan, P.G.; McMillan, D.C. An inflammation-based prognostic score (mGPS) predicts cancer survival independent of tumour site: A Glasgow Inflammation Outcome Study. Br. J. Cancer 2011, 104, 726–734. [Google Scholar] [CrossRef] [PubMed]
- Proctor, M.J.; Morrison, D.S.; Talwar, D.; Balmer, S.M.; Fletcher, C.D.; O’Reilly, D.S.; Foulis, A.K.; Horgan, P.G.; McMillan, D.C. A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow Inflammation Outcome Study. Eur. J. Cancer 2011, 47, 2633–2641. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Zhang, G.L. C-reactive protein to albumin ratio predicts the outcome in renal cell carcinoma: A meta-analysis. PLoS ONE 2019, 14, e0224266. [Google Scholar] [CrossRef] [PubMed]
- Makino, T.; Izumi, K.; Iwamoto, H.; Kadomoto, S.; Kadono, Y.; Mizokami, A. Comparison of the Prognostic Value of Inflammatory and Nutritional Indices in Nonmetastatic Renal Cell Carcinoma. Biomedicines 2023, 11, 533. [Google Scholar] [CrossRef]
- Sun, D.W.; An, L.; Lv, G.Y. Albumin-fibrinogen ratio and fibrinogen-prealbumin ratio as promising prognostic markers for cancers: An updated meta-analysis. World J. Surg. Oncol. 2020, 18, 9. [Google Scholar] [CrossRef]
- Xia, Z.; Fu, X.; Yuan, X.; Li, J.; Wang, H.; Sun, J.; Wu, J.; Tang, L. Serum albumin to globulin ratio prior to treatment as a potential non-invasive prognostic indicator for urological cancers. Front. Nutr. 2022, 9, 1012181. [Google Scholar] [CrossRef]
- Kim, S.I.; Kim, S.J.; Kim, S.J.; Cho, D.S. Prognostic nutritional index and prognosis in renal cell carcinoma: A systematic review and meta-analysis. Urol. Oncol. 2021, 39, 623–630. [Google Scholar] [CrossRef]
- Ni, L.; Huang, J.; Ding, J.; Kou, J.; Shao, T.; Li, J.; Gao, L.; Zheng, W.; Wu, Z. Prognostic Nutritional Index Predicts Response and Prognosis in Cancer Patients Treated with Immune Checkpoint Inhibitors: A Systematic Review and Meta-Analysis. Front. Nutr. 2022, 9, 823087. [Google Scholar] [CrossRef]
- Visser, M.; Kritchevsky, S.B.; Newman, A.B.; Goodpaster, B.H.; Tylavsky, F.A.; Nevitt, M.C.; Harris, T.B. Lower serum albumin concentration and change in muscle mass: The Health, Aging and Body Composition Study. Am. J. Clin. Nutr. 2005, 82, 531–537. [Google Scholar] [CrossRef]
- Hamaguchi, Y.; Kaido, T.; Okumura, S.; Kobayashi, A.; Hammad, A.; Tamai, Y.; Inagaki, N.; Uemoto, S. Proposal for new diagnostic criteria for low skeletal muscle mass based on computed tomography imaging in Asian adults. Nutrition 2016, 32, 1200–1205. [Google Scholar] [CrossRef]
- Akobeng, A.K. Understanding diagnostic tests 3: Receiver operating characteristic curves. Acta Paediatr. 2007, 96, 644–647. [Google Scholar] [CrossRef] [PubMed]
- Midenberg, E.; Higgins, M.I.; Schmeusser, B.N.; Patil, D.H.; Zaldumbide, J.; Martini, D.J.; Steele, S.; Williams, M.; Nabavizadeh, R.; Psutka, S.P.; et al. Prognostic Value of Sarcopenia and Albumin in the Surgical Management of Localized Renal Cell Carcinoma. Urol. Oncol. 2023, 41, 50.e19–50.e26. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Zargar-Shoshtari, K.; Caracciolo, J.T.; Fishman, M.; Poch, M.A.; Pow-Sang, J.; Sexton, W.J.; Spiess, P.E. Sarcopenia as a predictor of overall survival after cytoreductive nephrectomy for metastatic renal cell carcinoma. Urol. Oncol. 2015, 33, 339.e17–339.e23. [Google Scholar] [CrossRef] [PubMed]
- Psutka, S.P.; Boorjian, S.A.; Moynagh, M.R.; Schmit, G.D.; Costello, B.A.; Thompson, R.H.; Stewart-Merrill, S.B.; Lohse, C.M.; Cheville, J.C.; Leibovich, B.C.; et al. Decreased Skeletal Muscle Mass is Associated with an Increased Risk of Mortality after Radical Nephrectomy for Localized Renal Cell Cancer. J. Urol. 2016, 195, 270–276. [Google Scholar] [CrossRef]
- Fukushima, H.; Nakanishi, Y.; Kataoka, M.; Tobisu, K.; Koga, F. Prognostic Significance of Sarcopenia in Patients with Metastatic Renal Cell Carcinoma. J. Urol. 2016, 195, 26–32. [Google Scholar] [CrossRef]
- Mao, W.; Wang, K.; Zhang, H.; Lu, H.; Sun, S.; Tian, C.; Wu, Z.; Wu, J.; Xu, B.; Xu, H.; et al. Sarcopenia as a poor prognostic indicator for renal cell carcinoma patients undergoing nephrectomy in China: A multicenter study. Clin. Transl. Med. 2021, 11, e270. [Google Scholar] [CrossRef]
- Makino, T.; Izumi, K.; Iwamoto, H.; Kadomoto, S.; Kadono, Y.; Mizokami, A. Sarcopenia Is Associated with Aggressive Clinicopathological Outcomes and Is a Poor Prognostic Indicator for Non-metastatic Renal Cell Carcinoma. In Vivo 2023, 37, 1304–1311. [Google Scholar] [CrossRef]
- Li, S.; Wang, T.; Tong, G.; Li, X.; You, D.; Cong, M. Prognostic Impact of Sarcopenia on Clinical Outcomes in Malignancies Treated with Immune Checkpoint Inhibitors: A Systematic Review and Meta-Analysis. Front. Oncol. 2021, 11, 726257. [Google Scholar] [CrossRef]
- Higgins, M.I.; Martini, D.J.; Patil, D.H.; Nabavizadeh, R.; Steele, S.; Williams, M.; Joshi, S.S.; Narayan, V.M.; Sekhar, A.; Psutka, S.P.; et al. Sarcopenia and modified Glasgow Prognostic Score predict postsurgical outcomes in localized renal cell carcinoma. Cancer 2021, 127, 1974–1983. [Google Scholar] [CrossRef]
- Liu, Q.; Yang, J.; Chen, X.; Yang, J.; Zhao, X.; Huang, Y.; Lin, Y.; Pu, J. Prognostic significance of sarcopenia and systemic inflammation for patients with renal cell carcinoma following nephrectomy. Front. Oncol. 2022, 12, 1047515. [Google Scholar] [CrossRef]
- Morgan, T.M.; Tang, D.; Stratton, K.L.; Barocas, D.A.; Anderson, C.B.; Gregg, J.R.; Chang, S.S.; Cookson, M.S.; Herrell, S.D.; Smith, J.A., Jr.; et al. Preoperative nutritional status is an important predictor of survival in patients undergoing surgery for renal cell carcinoma. Eur. Urol. 2011, 59, 923–928. [Google Scholar] [CrossRef] [PubMed]
- Prado, C.M.; Heymsfield, S.B. Lean tissue imaging: A new era for nutritional assessment and intervention. JPEN J. Parenter. Enteral. Nutr. 2014, 38, 940–953. [Google Scholar] [CrossRef] [PubMed]
- Mantzorou, M.; Koutelidakis, A.; Theocharis, S.; Giaginis, C. Clinical Value of Nutritional Status in Cancer: What is its Impact and how it Affects Disease Progression and Prognosis? Nutr. Cancer 2017, 69, 1151–1176. [Google Scholar] [CrossRef] [PubMed]
- Yuxuan, L.; Junchao, L.; Wenya, L. The role of sarcopenia in treatment-related outcomes in patients with renal cell carcinoma: A systematic review and meta-analysis. Medicine 2022, 101, e31332. [Google Scholar] [CrossRef]
- Xia, L.; Zhao, R.; Wan, Q.; Wu, Y.; Zhou, Y.; Wang, Y.; Cui, Y.; Shen, X.; Wu, X. Sarcopenia and adverse health-related outcomes: An umbrella review of meta-analyses of observational studies. Cancer Med. 2020, 9, 7964–7978. [Google Scholar] [CrossRef]
- Caraceni, P.; Tufoni, M.; Bonavita, M.E. Clinical use of albumin. Blood Transfus. 2013, 11 (Suppl. S4), s18–s25. [Google Scholar] [CrossRef]
- Corcoran, A.T.; Kaffenberger, S.D.; Clark, P.E.; Walton, J.; Handorf, E.; Piotrowski, Z.; Tomaszewski, J.J.; Ginzburg, S.; Mehrazin, R.; Plimack, E.; et al. Hypoalbuminaemia is associated with mortality in patients undergoing cytoreductive nephrectomy. BJU Int. 2015, 116, 351–357. [Google Scholar] [CrossRef]
- Zhou, X.; Fu, G.; Zu, X.; Xu, Z.; Li, H.T.; D’Souza, A.; Tulpule, V.; Quinn, D.I.; Bhowmick, N.A.; Weisenberger, D.J.; et al. Albumin levels predict prognosis in advanced renal cell carcinoma treated with tyrosine kinase inhibitors: A systematic review and meta-analysis. Urol. Oncol. 2022, 40, 12.e13–12.e22. [Google Scholar] [CrossRef]
- Sun, K.; Chen, S.; Xu, J.; Li, G.; He, Y. The prognostic significance of the prognostic nutritional index in cancer: A systematic review and meta-analysis. J. Cancer Res. Clin. Oncol. 2014, 140, 1537–1549. [Google Scholar] [CrossRef]
- Peng, Q.; Liu, L.; Li, T.; Lei, C.; Wan, H. Prognostic impact of prognostic nutritional index on renal cell carcinoma: A meta-analysis of 7629 patients. PLoS ONE 2022, 17, e0265119. [Google Scholar] [CrossRef]
- Nascimento, W.; Ferrari, G.; Martins, C.B.; Rey-Lopez, J.P.; Izquierdo, M.; Lee, D.H.; Giovannucci, E.L.; Rezende, L.F.M. Muscle-strengthening activities and cancer incidence and mortality: A systematic review and meta-analysis of observational studies. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 69. [Google Scholar] [CrossRef] [PubMed]
- Rock, C.L.; Thomson, C.A.; Sullivan, K.R.; Howe, C.L.; Kushi, L.H.; Caan, B.J.; Neuhouser, M.L.; Bandera, E.V.; Wang, Y.; Robien, K.; et al. American Cancer Society nutrition and physical activity guideline for cancer survivors. CA Cancer J. Clin. 2022, 72, 230–262. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; He, T.; Sun, S.; Wu, J.; Xu, B.; Mao, W.; Chen, M. Prognostic Significance of Pre- to Postoperative Dynamics of Sarcopenia for Patients with Renal Cell Carcinoma Undergoing Laparoscopic Nephrectomy. Front. Surg. 2022, 9, 871731. [Google Scholar] [CrossRef] [PubMed]
- Clemente-Suarez, V.J.; Redondo-Florez, L.; Rubio-Zarapuz, A.; Martinez-Guardado, I.; Navarro-Jimenez, E.; Tornero-Aguilera, J.F. Nutritional and Exercise Interventions in Cancer-Related Cachexia: An Extensive Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 4604. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).