The Impact of SARS-CoV-2 Infection on Youth Mental Health: A Narrative Review
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
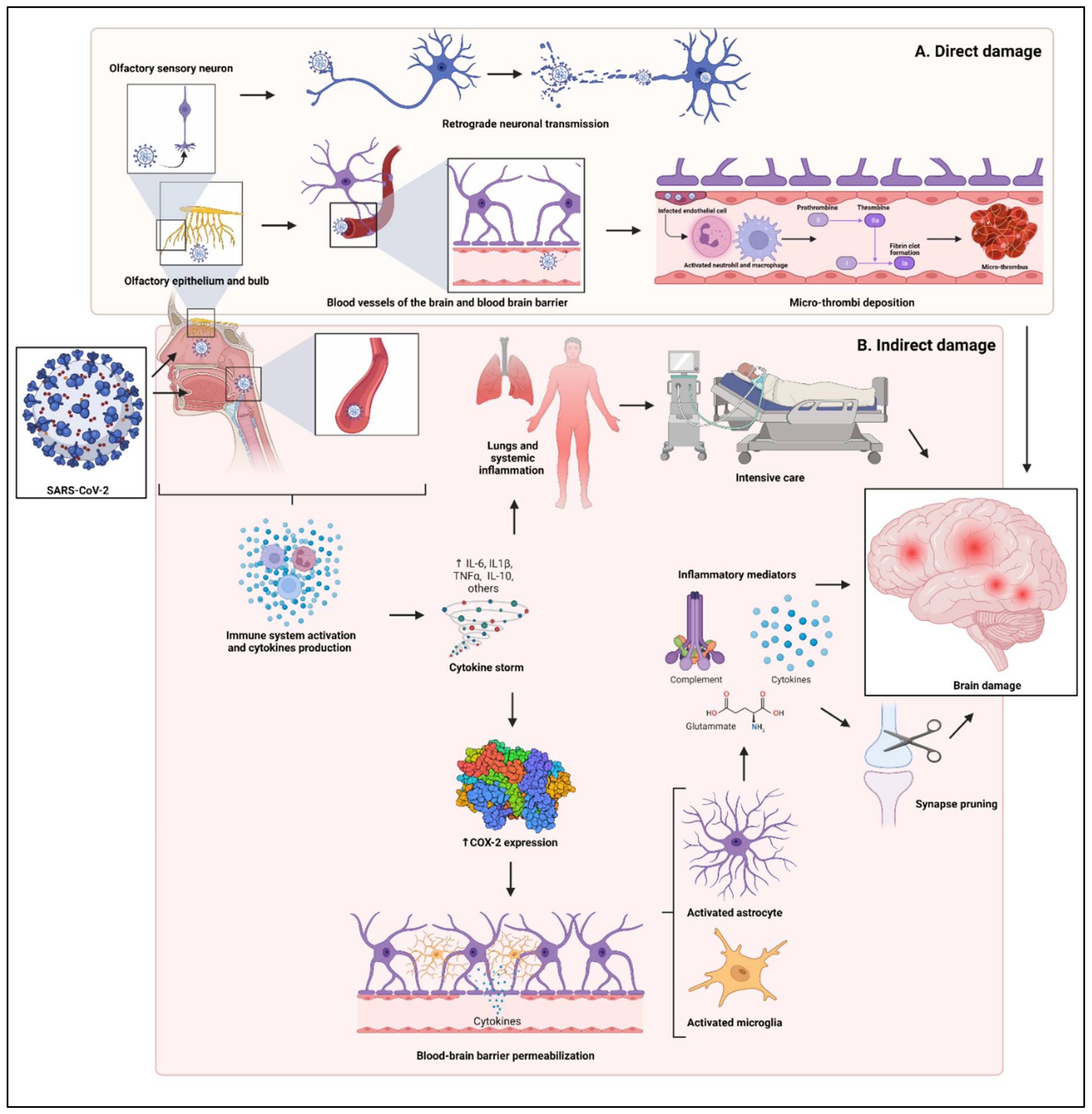
4.1. Biological Sequelae of the SARS-CoV-2 Infection on the CNS
4.1.1. Putative Biological Mechanism of Psychopathological Manifestations of SARS-CoV-2
4.1.2. Neuropsychiatric Symptoms in Youth during and after the SARS-CoV-2 Infection
4.2. The Role of COVID-19 Pandemic in the Mental Health of Young People: Onset of New Mental Disorders and Symptoms
4.2.1. Onset of New Symptoms or Signs Affecting the Mental Health of Non-Clinical Populations of Young People
Depressive Symptoms
Anxiety Symptoms
Distress
Post-Traumatic Stress Disorder Symptoms
Obsessive-Compulsive Symptoms
Eating Disorder Symptoms
Sleep Disturbances
Changes in Alcohol and Substance Use
4.2.2. Variation of the Incidence or Prevalence of Mental Disorders in the Populations of Young People after the Onset of the COVID-19 Pandemic
4.3. Suicide-Related Issues in the Youth during the COVID-19 Pandemic
4.3.1. Suicide Ideation
4.3.2. Suicide Attempt
4.3.3. Emergency Department Attendance
4.4. Role of Technology and Social Media
4.4.1. Impact of Web Technologies on the Mental Health of Young People during the COVID-19 Pandemic
4.4.2. The Role of Telemedicine for the Mental Health of Young People during the COVID-19 Pandemic
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- Dhama, K.; Patel, S.K.; Pathak, M.; Yatoo, M.I.; Tiwari, R.; Malik, Y.S.; Singh, R.; Sah, R.; Rabaan, A.A.; Bonilla-Aldana, D.K.; et al. An Update on SARS-CoV-2/COVID-19 with Particular Reference to Its Clinical Pathology, Pathogenesis, Immunopathology and Mitigation Strategies. Travel. Med. Infect. Dis. 2020, 37, 101755. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Gao, G.; Wang, S.; Chen, M.; Qian, F.; Tang, W.; Xu, Y.; Song, R.; Zhuang, L.; Ma, X.; et al. Clinical Characteristics and Risk Factors of Acute Respiratory Distress Syndrome (ARDS) in COVID-19 Patients in Beijing, China: A Retrospective Study. Med. Sci. Monit. 2020, 26, e925974-1–e925974-9. [Google Scholar] [CrossRef] [PubMed]
- Long, Q.-X.; Tang, X.-J.; Shi, Q.-L.; Li, Q.; Deng, H.-J.; Yuan, J.; Hu, J.-L.; Xu, W.; Zhang, Y.; Lv, F.-J.; et al. Clinical and Immunological Assessment of Asymptomatic SARS-CoV-2 Infections. Nat. Med. 2020, 26, 1200–1204. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Yuan, Z.; Yang, D.; Li, H.; Zhang, Y.; Gao, P.; Liu, X.; Zhao, W.; Xiao, T.; Duan, X. A Family Cluster of Severe Acute Respiratory Syndrome Coronavirus 2 Infections. Eur. J. Clin. Microbiol. Infect. Dis. 2020, 39, 1611–1615. [Google Scholar] [CrossRef] [PubMed]
- Vetter, P.; Eberhardt, C.S.; Meyer, B.; Murillo, P.A.M.; Torriani, G.; Pigny, F.; Lemeille, S.; Cordey, S.; Laubscher, F.; Vu, D.-L.; et al. Daily Viral Kinetics and Innate and Adaptive Immune Response Assessment in COVID-19: A Case Series. mSphere 2020, 5, e00827-20. [Google Scholar] [CrossRef]
- Ellul, M.A.; Benjamin, L.; Singh, B.; Lant, S.; Michael, B.D.; Easton, A.; Kneen, R.; Defres, S.; Sejvar, J.; Solomon, T. Neurological Associations of COVID-19. Lancet Neurol. 2020, 19, 767–783. [Google Scholar] [CrossRef]
- Varatharaj, A.; Thomas, N.; Ellul, M.A.; Davies, N.W.S.; Pollak, T.A.; Tenorio, E.L.; Sultan, M.; Easton, A.; Breen, G.; Zandi, M.; et al. Neurological and Neuropsychiatric Complications of COVID-19 in 153 Patients: A UK-Wide Surveillance Study. Lancet Psychiatry 2020, 7, 875–882. [Google Scholar] [CrossRef]
- Moldofsky, H.; Patcai, J. Chronic Widespread Musculoskeletal Pain, Fatigue, Depression and Disordered Sleep in Chronic Post-SARS Syndrome; a Case-Controlled Study. BMC Neurol. 2011, 11, 37. [Google Scholar] [CrossRef] [Green Version]
- Carfì, A.; Bernabei, R.; Landi, F. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-Acute COVID-19 Syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-Month Consequences of COVID-19 in Patients Discharged from Hospital: A Cohort Study. Lancet 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Solomon, I.H.; Normandin, E.; Bhattacharyya, S.; Mukerji, S.S.; Keller, K.; Ali, A.S.; Adams, G.; Hornick, J.L.; Padera, R.F.; Sabeti, P. Neuropathological Features of COVID-19. N. Engl. J. Med. 2020, 383, 989–992. [Google Scholar] [CrossRef] [PubMed]
- Hornuss, D.; Lange, B.; Schröter, N.; Rieg, S.; Kern, W.V.; Wagner, D. Anosmia in COVID-19 Patients. medRxiv 2020. [Google Scholar] [CrossRef] [PubMed]
- Reichard, R.R.; Kashani, K.B.; Boire, N.A.; Constantopoulos, E.; Guo, Y.; Lucchinetti, C.F. Neuropathology of COVID-19: A Spectrum of Vascular and Acute Disseminated Encephalomyelitis (ADEM)-like Pathology. Acta Neuropathol. 2020, 140, 1–6. [Google Scholar] [CrossRef]
- Moriguchi, T.; Harii, N.; Goto, J.; Harada, D.; Sugawara, H.; Takamino, J.; Ueno, M.; Sakata, H.; Kondo, K.; Myose, N.; et al. A First Case of Meningitis/Encephalitis Associated with SARS-Coronavirus-2. Int. J. Infect. Dis. Off. Publ. Int. Soc. Infect. Dis. 2020, 94, 55–58. [Google Scholar] [CrossRef]
- Helms, J.; Kremer, S.; Merdji, H.; Clere-Jehl, R.; Schenck, M.; Kummerlen, C.; Collange, O.; Boulay, C.; Fafi-Kremer, S.; Ohana, M.; et al. Neurologic Features in Severe SARS-CoV-2 Infection. N. Engl. J. Med. 2020, 382, 2268–2270. [Google Scholar] [CrossRef]
- Oxley, T.J.; Mocco, J.; Majidi, S.; Kellner, C.P.; Shoirah, H.; Singh, I.P.; De Leacy, R.A.; Shigematsu, T.; Ladner, T.R.; Yaeger, K.A.; et al. Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. N. Engl. J. Med. 2020, 382, e60. [Google Scholar] [CrossRef]
- Shimohata, T. Neuro-COVID-19. Clin. Exp. Neuroimmunol. 2021, 13, 17–23. [Google Scholar] [CrossRef]
- Couzin-Frankel, J. The Long Haul. Science 2020, 369, 614–617. [Google Scholar] [CrossRef]
- Hosp, J.A.; Dressing, A.; Blazhenets, G.; Bormann, T.; Rau, A.; Schwabenland, M.; Thurow, J.; Wagner, D.; Waller, C.; Niesen, W.D.; et al. Cognitive Impairment and Altered Cerebral Glucose Metabolism in the Subacute Stage of COVID-19. Brain J. Neurol. 2021, 144, 1263–1276. [Google Scholar] [CrossRef] [PubMed]
- Morin, L.; Savale, L.; Pham, T.; Colle, R.; Figueiredo, S.; Harrois, A.; Gasnier, M.; Lecoq, A.L.; Meyrignac, O.; Noel, N.; et al. Four-Month Clinical Status of a Cohort of Patients after Hospitalization for COVID-19. JAMA J. Am. Med. Assoc. 2021, 325, 1525–1534. [Google Scholar] [CrossRef]
- Blomberg, B.; Mohn, K.G.I.; Brokstad, K.A.; Zhou, F.; Linchausen, D.W.; Hansen, B.A.; Lartey, S.; Onyango, T.B.; Kuwelker, K.; Sævik, M.; et al. Long COVID in a Prospective Cohort of Home-Isolated Patients. Nat. Med. 2021, 27, 1607–1613. [Google Scholar] [CrossRef] [PubMed]
- WHO. Director-General’s Opening Remarks at the Media Briefing on COVID-19. 13 April 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19--13-april-2020 (accessed on 26 January 2022).
- WHO Announces COVID-19 Outbreak a Pandemic. 2020. Available online: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (accessed on 14 December 2021).
- Shrestha, N.; Shad, M.Y.; Ulvi, O.; Khan, M.H.; Karamehic-Muratovic, A.; Nguyen, U.S.D.T.; Baghbanzadeh, M.; Wardrup, R.; Aghamohammadi, N.; Cervantes, D.; et al. The Impact of COVID-19 on Globalization. One Health 2020, 11, 100180. [Google Scholar] [CrossRef]
- Xiang, S.; Rasool, S.; Hang, Y.; Javid, K.; Javed, T.; Artene, A.E. The Effect of COVID-19 Pandemic on Service Sector Sustainability and Growth. Front. Psychol. 2021, 12, 633597. [Google Scholar] [CrossRef]
- Horton, R. Offline: COVID-19 Is Not a Pandemic. Lancet 2020, 396, 874. [Google Scholar] [CrossRef]
- Cândido, E.L.; Gonçalves Júnior, J. COVID-19 Syndemic, Government, and Impact on Mental Health: A Brazilian Reality. Front. Psychiatry 2021, 12, 671449. [Google Scholar] [CrossRef]
- Fiorillo, A.; Frangou, S. European Psychiatry 2020: Moving Forward. Eur. Psychiatry 2020, 63, e1. [Google Scholar] [CrossRef] [Green Version]
- Cullen, W.; Gulati, G.; Kelly, B.D. Mental Health in the COVID-19 Pandemic. QJM Int. J. Med. 2020, 113, 311–312. [Google Scholar] [CrossRef]
- Serafini, G.; Parmigiani, B.; Amerio, A.; Aguglia, A.; Sher, L.; Amore, M. The Psychological Impact of COVID-19 on the Mental Health in the General Population. QJM Int. J. Med. 2020, 113, 531–537. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 Pandemic on Mental Health in the General Population: A Systematic Review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Vindegaard, N.; Benros, M.E. COVID-19 Pandemic and Mental Health Consequences: Systematic Review of the Current Evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Giallonardo, V.; Sampogna, G.; Del Vecchio, V.; Luciano, M.; Albert, U.; Carmassi, C.; Carrà, G.; Cirulli, F.; Dell’Osso, B.; Nanni, M.G.; et al. The Impact of Quarantine and Physical Distancing Following COVID-19 on Mental Health: Study Protocol of a Multicentric Italian Population Trial. Front. Psychiatry 2020, 11, 533. [Google Scholar] [CrossRef] [PubMed]
- Onchev, G. Changes in Psychopathology and Mental Health Resilience. Front. Psychiatry 2021, 12, 676492. [Google Scholar] [CrossRef] [PubMed]
- Veer, I.M.; Riepenhausen, A.; Zerban, M.; Wackerhagen, C.; Puhlmann, L.M.C.; Engen, H.; Köber, G.; Bögemann, S.A.; Weermeijer, J.; Uściłko, A.; et al. Psycho-Social Factors Associated with Mental Resilience in the Corona Lockdown. Transl. Psychiatry 2021, 11, 67. [Google Scholar] [CrossRef]
- Ellena, G.; Battaglia, S.; Làdavas, E. The Spatial Effect of Fearful Faces in the Autonomic Response. Exp. Brain Res. 2020, 238, 2009–2018. [Google Scholar] [CrossRef]
- Candini, M.; Battaglia, S.; Benassi, M.; di Pellegrino, G.; Frassinetti, F. The Physiological Correlates of Interpersonal Space. Sci. Rep. 2021, 11, 2611. [Google Scholar] [CrossRef]
- Blakemore, S.-J. Adolescence and Mental Health. Lancet 2019, 393, 2030–2031. [Google Scholar] [CrossRef]
- Whittaker, E.; Bamford, A.; Kenny, J.; Kaforou, M.; Jones, C.E.; Shah, P.; Ramnarayan, P.; Fraisse, A.; Miller, O.; Davies, P.; et al. Clinical Characteristics of 58 Children with a Pediatric Inflammatory Multisystem Syndrome Temporally Associated with SARS-CoV-2. JAMA 2020, 324, 259. [Google Scholar] [CrossRef]
- Swann, O.V.; Holden, K.A.; Turtle, L.; Pollock, L.; Fairfield, C.J.; Drake, T.M.; Seth, S.; Egan, C.; Hardwick, H.E.; Halpin, S.; et al. Clinical Characteristics of Children and Young People Admitted to Hospital with COVID-19 in United Kingdom: Prospective Multicentre Observational Cohort Study. BMJ 2020, 370, 5. [Google Scholar] [CrossRef]
- Hepburn, M.; Mullaguri, N.; George, P.; Hantus, S.; Punia, V.; Bhimraj, A.; Newey, C.R. Acute Symptomatic Seizures in Critically Ill Patients with COVID-19: Is There an Association? Neurocrit. Care 2021, 34, 1. [Google Scholar] [CrossRef] [PubMed]
- Desforges, M.; Le Coupanec, A.; Dubeau, P.; Bourgouin, A.; Lajoie, L.; Dubé, M.; Talbot, P.J. Human Coronaviruses and Other Respiratory Viruses: Underestimated Opportunistic Pathogens of the Central Nervous System? Viruses 2020, 12, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zubair, A.S.; McAlpine, L.S.; Gardin, T.; Farhadian, S.; Kuruvilla, D.E.; Spudich, S. Neuropathogenesis and Neurologic Manifestations of the Coronaviruses in the Age of Coronavirus Disease 2019: A Review. JAMA Neurol. 2020, 77, 1018–1027. [Google Scholar] [CrossRef]
- Swanson, P.A.; McGavern, D.B. Viral Diseases of the Central Nervous System. Curr. Opin. Virol. 2015, 11, 44–54. [Google Scholar] [CrossRef] [Green Version]
- Lemprière, S. SARS-CoV-2 Detected in Olfactory Neurons. Nat. Rev. Neurol. 2021, 17, 63. [Google Scholar] [CrossRef]
- Meinhardt, J.; Radke, J.; Dittmayer, C.; Franz, J.; Thomas, C.; Mothes, R.; Laue, M.; Schneider, J.; Brünink, S.; Greuel, S.; et al. Olfactory Transmucosal SARS-CoV-2 Invasion as a Port of Central Nervous System Entry in Individuals with COVID-19. Nat. Neurosci. 2021, 24, 168–175. [Google Scholar] [CrossRef]
- Song, E.; Zhang, C.; Israelow, B.; Lu-Culligan, A.; Prado, A.V.; Skriabine, S.; Lu, P.; Weizman, O.-E.; Liu, F.; Dai, Y.; et al. Neuroinvasion of SARS-CoV-2 in Human and Mouse Brain. J. Exp. Med. 2021, 218, e20202135. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.P.; Le Quesne, J.; Officer-Jones, L.; Teodòsio, A.; Thaventhiran, J.; Ficken, C.; Goddard, M.; Smith, C.; Menon, D.; Allinson, K.S.J. Neuropathological Findings in Two Patients with Fatal COVID-19. Neuropathol. Appl. Neurobiol. 2021, 47, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Schaller, T.; Hirschbühl, K.; Burkhardt, K.; Braun, G.; Trepel, M.; Märkl, B.; Claus, R. Postmortem Examination of Patients with COVID-19. JAMA 2020, 323, 2518–2520. [Google Scholar] [CrossRef]
- Boldrini, M.; Canoll, P.D.; Klein, R.S. How COVID-19 Affects the Brain. JAMA Psychiatry 2021, 78, 682. [Google Scholar] [CrossRef]
- Channappanavar, R.; Fehr, A.R.; Vijay, R.; Mack, M.; Zhao, J.; Meyerholz, D.K.; Perlman, S. Dysregulated Type I Interferon and Inflammatory Monocyte-Macrophage Responses Cause Lethal Pneumonia in SARS-CoV-Infected Mice. Cell Host Microbe 2016, 19, 181–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davidson, S.; Maini, M.K.; Wack, A. Disease-Promoting Effects of Type I Interferons in Viral, Bacterial, and Coinfections. J. Interferon Cytokine Res. 2015, 35, 252–264. [Google Scholar] [CrossRef] [PubMed]
- Daniels, B.P.; Holman, D.W.; Cruz-Orengo, L.; Jujjavarapu, H.; Durrant, D.M.; Klein, R.S. Viral Pathogen-Associated Molecular Patterns Regulate Blood-Brain Barrier Integrity via Competing Innate Cytokine Signals. mBio 2014, 5, e01476-14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meier, I.B.; Vieira Ligo Teixeira, C.; Tarnanas, I.; Mirza, F.; Rajendran, L. Neurological and Mental Health Consequences of COVID-19: Potential Implications for Well-Being and Labour Force. Brain Commun. 2021, 3, fcab012. [Google Scholar] [CrossRef] [PubMed]
- Maeng, S.H.; Hong, H. Inflammation as the Potential Basis in Depression. Int. Neurourol. J. 2019, 23, S63–S67. [Google Scholar] [CrossRef] [Green Version]
- Vasek, M.J.; Garber, C.; Dorsey, D.; Durrant, D.M.; Bollman, B.; Soung, A.; Yu, J.; Perez-Torres, C.; Frouin, A.; Wilton, D.K.; et al. A Complement–Microglial Axis Drives Synapse Loss during Virus-Induced Memory Impairment. Nature 2016, 534, 538–543. [Google Scholar] [CrossRef] [Green Version]
- Sarzi-Puttini, P.; Giorgi, V.; Sirotti, S.; Marotto, D.; Ardizzone, S.; Rizzardini, G.; Antinori, S.; Galli, M. COVID-19, Cytokines and Immunosuppression: What Can We Learn from Severe Acute Respiratory Syndrome? Clin. Exp. Rheumatol. 2020, 38, 337–342. [Google Scholar]
- Mangalmurti, N.; Hunter, C.A. Cytokine Storms: Understanding COVID-19. Immunity 2020, 53, 19–25. [Google Scholar] [CrossRef]
- Romero-Sánchez, C.M.; Díaz-Maroto, I.; Fernández-Díaz, E.; Sánchez-Larsen, Á.; Layos-Romero, A.; García-García, J.; González, E.; Redondo-Peñas, I.; Perona-Moratalla, A.B.; Del Valle-Pérez, J.A.; et al. Neurologic Manifestations in Hospitalized Patients with COVID-19: The ALBACOVID Registry. Neurology 2020, 95, e1060–e1070. [Google Scholar] [CrossRef]
- Rogers, J.P.; Chesney, E.; Oliver, D.; Pollak, T.A.; McGuire, P.; Fusar-Poli, P.; Zandi, M.S.; Lewis, G.; David, A.S. Psychiatric and Neuropsychiatric Presentations Associated with Severe Coronavirus Infections: A Systematic Review and Meta-Analysis with Comparison to the COVID-19 Pandemic. Lancet Psychiatry 2020, 7, 611–627. [Google Scholar] [CrossRef]
- Shaw, A.C.; Goldstein, D.R.; Montgomery, R.R. Age-Dependent Dysregulation of Innate Immunity. Nat. Rev. Immunol. 2013, 13, 875–887. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanaka, M.; Tóth, F.; Polyák, H.; Szabó, Á.; Mándi, Y.; Vécsei, L. Immune Influencers in Action: Metabolites and Enzymes of the Tryptophan-Kynurenine Metabolic Pathway. Biomedicines 2021, 9, 734. [Google Scholar] [CrossRef] [PubMed]
- Irwin, M.R.; Miller, A.H. Depressive Disorders and Immunity: 20 Years of Progress and Discovery. Brain Behav. Immun. 2007, 21, 374–383. [Google Scholar] [CrossRef] [PubMed]
- Dinan, T.G.; Dinan, T. Inflammatory Markers in Depression. Curr. Opin. Psychiatry 2009, 22, 32–36. [Google Scholar] [CrossRef]
- Miller, A.H.; Maletic, V.; Raison, C.L. Inflammation and Its Discontents: The Role of Cytokines in the Pathophysiology of Major Depression. Biol. Psychiatry 2009, 65, 732–741. [Google Scholar] [CrossRef] [Green Version]
- Maes, M.; Song, C.; Yirmiya, R. Targeting IL-1 in Depression. Expert Opin. Ther. Targets 2012, 16, 1097–1112. [Google Scholar] [CrossRef]
- Leonard, B.; Maes, M. Mechanistic Explanations How Cell-Mediated Immune Activation, Inflammation and Oxidative and Nitrosative Stress Pathways and Their Sequels and Concomitants Play a Role in the Pathophysiology of Unipolar Depression. Neurosci. Biobehav. Rev. 2012, 36, 764–785. [Google Scholar] [CrossRef]
- Maes, M. Depression Is an Inflammatory Disease, but Cell-Mediated Immune Activation Is the Key Component of Depression. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2011, 35, 664–675. [Google Scholar] [CrossRef]
- Slavich, G.M.; Irwin, M.R. From Stress to Inflammation and Major Depressive Disorder: A Social Signal Transduction Theory of Depression. Psychol. Bull. 2014, 140, 774–815. [Google Scholar] [CrossRef]
- Miller, A.H.; Raison, C.L. The Role of Inflammation in Depression: From Evolutionary Imperative to Modern Treatment Target. Nat. Rev. Immunol. 2016, 16, 22–34. [Google Scholar] [CrossRef] [Green Version]
- Watkins, C.C.; Andrews, S.R. Clinical Studies of Neuroinflammatory Mechanisms in Schizophrenia. Schizophr. Res. 2016, 176, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues-Amorim, D.; Rivera-Baltanás, T.; Spuch, C.; Caruncho, H.J.; González-Fernandez, Á.; Olivares, J.M.; Agís-Balboa, R.C. Cytokines Dysregulation in Schizophrenia: A Systematic Review of Psychoneuroimmune Relationship. Schizophr. Res. 2018, 197, 19–33. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Tian, B.; Han, H.-B. Serum Interleukin-6 in Schizophrenia: A System Review and Meta-Analysis. Cytokine 2021, 141, 155441. [Google Scholar] [CrossRef]
- Zakharyan, R.; Boyajyan, A. Inflammatory Cytokine Network in Schizophrenia. World J. Biol. Psychiatry 2014, 15, 174–187. [Google Scholar] [CrossRef]
- Saccaro, L.F.; Schilliger, Z.; Perroud, N.; Piguet, C. Inflammation, Anxiety, and Stress in Attention-Deficit/Hyperactivity Disorder. Biomedicines 2021, 9, 1313. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; Hu, X.; Ekumi, I.O.; Wang, J.; An, Y.; Li, Z.; Yuan, B. Psychological Distress and Its Correlates Among COVID-19 Survivors During Early Convalescence Across Age Groups. Am. J. Geriatr. Psychiatry 2020, 28, 1030–1039. [Google Scholar] [CrossRef]
- Blankenburg, J.; Wekenborg, M.K.; Reichert, J.; Kirsten, C.; Kahre, E.; Haag, L.; Schumm, L.; Czyborra, P.; Berner, R.; Armann, J.P. Mental Health of Adolescents in the Pandemic: Long-COVID-19 or Long-Pandemic Syndrome? SSRN Electron. J. 2021. [Google Scholar] [CrossRef]
- Hampshire, A.; Trender, W.; Chamberlain, S.R.; Jolly, A.E.; Grant, J.E.; Patrick, F.; Mazibuko, N.; Williams, S.C.; Barnby, J.M.; Hellyer, P.; et al. Cognitive Deficits in People Who Have Recovered from COVID-19. eClinicalMedicine 2021, 39, 101044. [Google Scholar] [CrossRef]
- Roge, I.; Smane, L.; Kivite-Urtane, A.; Pucuka, Z.; Racko, I.; Klavina, L.; Pavare, J. Comparison of Persistent Symptoms After COVID-19 and Other Non-SARS-CoV-2 Infections in Children. Front. Pediatr. 2021, 9, 752385. [Google Scholar] [CrossRef]
- Parola, A.; Rossi, A.; Tessitore, F.; Troisi, G.; Mannarini, S. Mental Health Through the COVID-19 Quarantine: A Growth Curve Analysis on Italian Young Adults. Front. Psychol. 2020, 11, 567484. [Google Scholar] [CrossRef]
- Akhtarul Islam, M.; Barna, S.D.; Raihan, H.; Nafiul Alam Khan, M.; Tanvir Hossain, M. Depression and Anxiety among University Students during the COVID-19 Pandemic in Bangladesh: A Web-Based Cross-Sectional Survey. PLoS ONE 2020, 15, e0238162. [Google Scholar] [CrossRef]
- Khan, A.H.; Sultana, M.S.; Hossain, S.; Hasan, M.T.; Ahmed, H.U.; Sikder, M.T. The Impact of COVID-19 Pandemic on Mental Health & Wellbeing among Home-Quarantined Bangladeshi Students: A Cross-Sectional Pilot Study. J. Affect. Disord. 2020, 277, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Wan Mohd Yunus, W.M.A.; Badri, S.K.Z.; Panatik, S.A.; Mukhtar, F. The Unprecedented Movement Control Order (Lockdown) and Factors Associated with the Negative Emotional Symptoms, Happiness, and Work-Life Balance of Malaysian University Students During the Coronavirus Disease (COVID-19) Pandemic. Front. Psychiatry 2021, 11, 566221. [Google Scholar] [CrossRef] [PubMed]
- Mekonen, E.G.; Workneh, B.S.; Ali, M.S.; Muluneh, N.Y. The Psychological Impact of COVID-19 Pandemic on Graduating Class Students at the University of Gondar, Northwest Ethiopia. Psychol. Res. Behav. Manag. 2021, 14, 109. [Google Scholar] [CrossRef] [PubMed]
- Padrón, I.; Fraga, I.; Vieitez, L.; Montes, C.; Romero, E. A Study on the Psychological Wound of COVID-19 in University Students. Front. Psychol. 2021, 12, 9. [Google Scholar] [CrossRef]
- Zhou, S.J.; Zhang, L.G.; Wang, L.L.; Guo, Z.C.; Wang, J.Q.; Chen, J.C.; Liu, M.; Chen, X.; Chen, J.X. Prevalence and Socio-Demographic Correlates of Psychological Health Problems in Chinese Adolescents during the Outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef]
- Seçer, İ.; Ulaş, S. An Investigation of the Effect of COVID-19 on OCD in Youth in the Context of Emotional Reactivity, Experiential Avoidance, Depression and Anxiety. Int. J. Ment. Health Addict. 2021, 19, 1. [Google Scholar] [CrossRef]
- Qi, M.; Zhou, S.J.; Guo, Z.C.; Zhang, L.G.; Min, H.J.; Li, X.M.; Chen, J.X. The Effect of Social Support on Mental Health in Chinese Adolescents During the Outbreak of COVID-19. J. Adolesc. Health 2020, 67, 514. [Google Scholar] [CrossRef]
- Tee, M.L.; Tee, C.A.; Anlacan, J.P.; Aligam, K.J.G.; Reyes, P.W.C.; Kuruchittham, V.; Ho, R.C. Psychological Impact of COVID-19 Pandemic in the Philippines. J. Affect. Disord. 2020, 277, 379–391. [Google Scholar] [CrossRef]
- Ellis, W.E.; Dumas, T.M.; Forbes, L.M. Physically Isolated but Socially Connected: Psychological Adjustment and Stress among Adolescents during the Initial COVID-19 Crisis. Can. J. Behav. Sci. Rev. Can. Sci. Comport. 2020, 52, 177. [Google Scholar] [CrossRef]
- Ma, Z.; Zhao, J.; Li, Y.; Chen, D.; Wang, T.; Zhang, Z.; Chen, Z.; Yu, Q.; Jiang, J.; Fan, F.; et al. Mental Health Problems and Correlates among 746,217 College Students during the Coronavirus Disease 2019 Outbreak in China. Epidemiol. Psychiatr. Sci. 2020, 29, e181. [Google Scholar] [CrossRef] [PubMed]
- Murata, S.; Rezeppa, T.; Thoma, B.; Marengo, L.; Krancevich, K.; Chiyka, E.; Hayes, B.; Goodfriend, E.; Deal, M.; Zhong, Y.; et al. The Psychiatric Sequelae of the COVID-19 Pandemic in Adolescents, Adults, and Health Care Workers. Depress. Anxiety 2021, 38, 233–246. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Zhang, E.; Wong, G.T.F.; Hyun, S.; Hahm, H. “Chris” Factors Associated with Depression, Anxiety, and PTSD Symptomatology during the COVID-19 Pandemic: Clinical Implications for U.S. Young Adult Mental Health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef] [PubMed]
- Essadek, A.; Rabeyron, T. Mental Health of French Students during the COVID-19 Pandemic. J. Affect. Disord. 2020, 277, 392–393. [Google Scholar] [CrossRef] [PubMed]
- Son, C.; Hegde, S.; Smith, A.; Wang, X.; Sasangohar, F. Effects of COVID-19 on College Students’ Mental Health in the United States: Interview Survey Study. J. Med. Internet Res. 2020, 22, e21279. [Google Scholar] [CrossRef]
- Sun, S.; Goldberg, S.B.; Lin, D.; Qiao, S.; Operario, D. Psychiatric Symptoms, Risk, and Protective Factors among University Students in Quarantine during the COVID-19 Pandemic in China. Glob. Health 2021, 17, 15. [Google Scholar] [CrossRef]
- Wang, X.; Hegde, S.; Son, C.; Keller, B.; Smith, A.; Sasangohar, F. Investigating Mental Health of US College Students during the COVID-19 Pandemic: Cross-Sectional Survey Study. J. Med. Internet Res. 2020, 22, e22817. [Google Scholar] [CrossRef]
- Glowacz, F.; Schmits, E. Psychological Distress during the COVID-19 Lockdown: The Young Adults Most at Risk. Psychiatry Res. 2020, 293, 113486. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The Psychological Impact of the COVID-19 Epidemic on College Students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Baloch, G.M.; Sundarasen, S.; Chinna, K.; Nurunnabi, M.; Kamaludin, K.; Khoshaim, H.B.; Hossain, S.F.A.; AlSukayt, A. COVID-19: Exploring Impacts of the Pandemic and Lockdown on Mental Health of Pakistani Students. PeerJ 2021, 9, e10612. [Google Scholar] [CrossRef]
- Bourion-Bédès, S.; Tarquinio, C.; Batt, M.; Tarquinio, P.; Lebreuilly, R.; Sorsana, C.; Legrand, K.; Rousseau, H.; Baumann, C. Psychological Impact of the COVID-19 Outbreak on Students in a French Region Severely Affected by the Disease: Results of the PIMS-CoV 19 Study. Psychiatry Res. 2021, 295, 113559. [Google Scholar] [CrossRef] [PubMed]
- Faize, F.A.; Husain, W. Students with Severe Anxiety during COVID-19 Lockdown—Exploring the Impact and Its Management. J. Ment. Health Train. Educ. Pract. 2021, 16, 153–163. [Google Scholar] [CrossRef]
- Jiang, R. Knowledge, Attitudes and Mental Health of University Students during the COVID-19 Pandemic in China. Child. Youth Serv. Rev. 2020, 119, 105494. [Google Scholar] [CrossRef] [PubMed]
- Baiano, C.; Zappullo, I.; Conson, M.; Di Mauro, G.; Petra, M.; Piacenti, M.; Rauso, B. Tendency to Worry and Fear of Mental Health during Italy’s COVID-19 Lockdown. Int. J. Environ. Res. Public Health 2020, 17, 5928. [Google Scholar] [CrossRef] [PubMed]
- Oosterhoff, B.; Palmer, C.A.; Wilson, J.; Shook, N. Adolescents’ Motivations to Engage in Social Distancing During the COVID-19 Pandemic: Associations with Mental and Social Health. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2020, 67, 179–185. [Google Scholar] [CrossRef]
- Yang, H.; Bin, P.; He, A.J. Opinions from the Epicenter: An Online Survey of University Students in Wuhan amidst the COVID-19 Outbreak11. J. Chin. Gov. 2020, 5, 234–248. [Google Scholar] [CrossRef] [Green Version]
- Luijten, M.A.J.; van Muilekom, M.M.; Teela, L.; Polderman, T.J.C.; Terwee, C.B.; Zijlmans, J.; Klaufus, L.; Popma, A.; Oostrom, K.J.; van Oers, H.A.; et al. The Impact of Lockdown during the COVID-19 Pandemic on Mental and Social Health of Children and Adolescents. Qual. Life Res. 2021, 30, 2795–2804. [Google Scholar] [CrossRef]
- Sundarasen, S.; Chinna, K.; Kamaludin, K.; Nurunnabi, M.; Baloch, G.M.; Khoshaim, H.B.; Hossain, S.F.A.; Sukayt, A. Psychological Impact of COVID-19 and Lockdown among University Students in Malaysia: Implications and Policy Recommendations. Int. J. Environ. Res. Public Health 2020, 17, 6206. [Google Scholar] [CrossRef]
- Liang, L.; Ren, H.; Cao, R.; Hu, Y.; Qin, Z.; Li, C.; Mei, S. The Effect of COVID-19 on Youth Mental Health. Psychiatr. Q. 2020, 91, 841–852. [Google Scholar] [CrossRef]
- Al-Musharaf, S. Prevalence and Predictors of Emotional Eating among Healthy Young Saudi Women during the COVID-19 Pandemic. Nutrients 2020, 12, 2923. [Google Scholar] [CrossRef]
- Buckley, G.L.; Hall, L.E.; Lassemillante, A.-C.M.; Belski, R. Disordered Eating & Body Image of Current and Former Athletes in a Pandemic; a Convergent Mixed Methods Study—What Can We Learn from COVID-19 to Support Athletes through Transitions? J. Eat. Disord. 2021, 9, 73. [Google Scholar] [CrossRef] [PubMed]
- Keel, P.K.; Gomez, M.M.; Harris, L.; Kennedy, G.A.; Ribeiro, J.; Joiner, T.E. Gaining “The Quarantine 15:” Perceived versus Observed Weight Changes in College Students in the Wake of COVID-19. Int. J. Eat. Disord. 2020, 53, 1801–1808. [Google Scholar] [CrossRef] [PubMed]
- Kohls, E.; Baldofski, S.; Moeller, R.; Klemm, S.L.; Rummel-Kluge, C. Mental Health, Social and Emotional Well-Being, and Perceived Burdens of University Students during COVID-19 Pandemic Lockdown in Germany. Front. Psychiatry 2021, 12, 441. [Google Scholar] [CrossRef] [PubMed]
- Puhl, R.M.; Lessard, L.M.; Larson, N.; Eisenberg, M.E.; Neumark-Stzainer, D. Weight Stigma as a Predictor of Distress and Maladaptive Eating Behaviors During COVID-19: Longitudinal Findings from the EAT Study. Ann. Behav. Med. 2020, 54, 738–746. [Google Scholar] [CrossRef]
- Scharmer, C.; Martinez, K.; Gorrell, S.; Reilly, E.E.; Donahue, J.M.; Anderson, D.A. Eating Disorder Pathology and Compulsive Exercise during the COVID-19 Public Health Emergency: Examining Risk Associated with COVID-19 Anxiety and Intolerance of Uncertainty. Int. J. Eat. Disord. 2020, 53, 2049–2054. [Google Scholar] [CrossRef]
- Simone, M.; Emery, R.L.; Hazzard, V.M.; Eisenberg, M.E.; Larson, N.; Neumark-Sztainer, D. Disordered Eating in a Population-Based Sample of Young Adults during the COVID-19 Outbreak. Int. J. Eat. Disord. 2021, 54, 1189–1201. [Google Scholar] [CrossRef]
- Trott, M.; Johnstone, J.; Pardhan, S.; Barnett, Y.; Smith, L. Changes in Body Dysmorphic Disorder, Eating Disorder, and Exercise Addiction Symptomology during the COVID-19 Pandemic: A Longitudinal Study of 319 Health Club Users. Psychiatry Res. 2021, 298, 113831. [Google Scholar] [CrossRef]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in Sleep Pattern, Sense of Time and Digital Media Use during COVID-19 Lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef]
- Dumas, T.M.; Ellis, W.; Litt, D.M. What Does Adolescent Substance Use Look Like During the COVID-19 Pandemic? Examining Changes in Frequency, Social Contexts, and Pandemic-Related Predictors. J. Adolesc. Health 2020, 67, 354. [Google Scholar] [CrossRef]
- Czeisler, M.É.; Wiley, J.F.; Facer-Childs, E.R.; Robbins, R.; Weaver, M.D.; Barger, L.K.; Czeisler, C.A.; Howard, M.E.; Rajaratnam, S.M.W. Mental Health, Substance Use, and Suicidal Ideation during a Prolonged COVID-19-Related Lockdown in a Region with Low SARS-CoV-2 Prevalence. J. Psychiatr. Res. 2021, 140, 533–544. [Google Scholar] [CrossRef]
- Wu, Z.; Liu, Z.; Zou, Z.; Wang, F.; Zhu, M.; Zhang, W.; Tao, H.; Ross, B.; Long, Y. Changes of Psychotic-like Experiences and Their Association with Anxiety/Depression among Young Adolescents before COVID-19 and after the Lockdown in China. Schizophr. Res. 2021, 237, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Esposito, C.M.; D’Agostino, A.; Dell Osso, B.; Fiorentini, A.; Prunas, C.; Callari, A.; Oldani, L.; Fontana, E.; Gargano, G.; Viscardi, B.; et al. Impact of the First COVID-19 Pandemic Wave on First Episode Psychosis in Milan, Italy. Psychiatry Res. 2021, 298, 113802. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhang, P.; Zhang, N. Adolescent Mental Health in China Requires More Attention. Lancet Public Health 2020, 5, e637. [Google Scholar] [CrossRef]
- Santomauro, D.F.; Herrera, A.M.M.; Shadid, J.; Zheng, P.; Ashbaugh, C.; Pigott, D.M.; Abbafati, C.; Adolph, C.; Amlag, J.O.; Aravkin, A.Y.; et al. Global Prevalence and Burden of Depressive and Anxiety Disorders in 204 Countries and Territories in 2020 Due to the COVID-19 Pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Taquet, M.; Geddes, J.R.; Luciano, S.; Harrison, P.J. Incidence and Outcomes of Eating Disorders during the COVID-19 Pandemic. Br. J. Psychiatry 2021, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Suicide Worldwide in 2019. Available online: https://www.who.int/publications-detail-redirect/9789240026643 (accessed on 27 January 2022).
- Yuodelis-Flores, C.; Ries, R.K. Addiction and Suicide: A Review. Am. J. Addict. 2015, 24, 98–104. [Google Scholar] [CrossRef]
- Barzilay, S.; Brunstein Klomek, A.; Apter, A.; Carli, V.; Wasserman, C.; Hadlaczky, G.; Hoven, C.W.; Sarchiapone, M.; Balazs, J.; Kereszteny, A.; et al. Bullying Victimization and Suicide Ideation and Behavior Among Adolescents in Europe: A 10-Country Study. J. Adolesc. Health 2017, 61, 179–186. [Google Scholar] [CrossRef]
- Kwok, S.Y.C.L.; Gu, M.; Cheung, A. A Longitudinal Study on the Relationship among Childhood Emotional Abuse, Gratitude, and Suicidal Ideation of Chinese Adolescents. Child. Abus. Neglect. 2019, 94, 104031. [Google Scholar] [CrossRef]
- Kim, K.M.; Kim, D.; Chung, U.S. Investigation of the Trend in Adolescent Mental Health and Its Related Social Factors: A Multi-Year Cross-Sectional Study For 13 Years. Int. J. Environ. Res. Public Health 2020, 17, 5405. [Google Scholar] [CrossRef]
- Wasserman, I.M. The Impact of Epidemic, War, Prohibition and Media on Suicide: United States, 1910–1920. Suicide Life Threat. Behav. 1992, 22, 240–254. [Google Scholar]
- Cheung, Y.T.; Chau, P.H.; Yip, P.S.F. A Revisit on Older Adults Suicides and Severe Acute Respiratory Syndrome (SARS) Epidemic in Hong Kong. Int. J. Geriatr. Psychiatry 2008, 23, 1231–1238. [Google Scholar] [CrossRef] [PubMed]
- Moutier, C. Suicide Prevention in the COVID-19 Era. JAMA Psychiatry 2021, 78, 433. [Google Scholar] [CrossRef] [PubMed]
- Isumi, A.; Doi, S.; Yamaoka, Y.; Takahashi, K.; Fujiwara, T. Do Suicide Rates in Children and Adolescents Change during School Closure in Japan? The Acute Effect of the First Wave of COVID-19 Pandemic on Child and Adolescent Mental Health. Child Abus. Negl. 2020, 110, 104680. [Google Scholar] [CrossRef] [PubMed]
- Burke, T.A.; Bettis, A.H.; Kudinova, A.; Thomas, S.A.; Nesi, J.; Erguder, L.; MacPherson, H.A.; Thompson, E.; Ammerman, B.A.; Wolff, J.C. COVID-19-Specific Suicidal Thoughts and Behaviors in Psychiatrically Hospitalized Adolescents. Child. Psychiatry Hum. Dev. 2021. [Google Scholar] [CrossRef]
- Carison, A.; Babl, F.E.; O’Donnell, S.M. Increased Paediatric Emergency Mental Health and Suicidality Presentations during COVID-19 Stay at Home Restrictions. Emerg. Med. Australas. 2022, 34, 85–91. [Google Scholar] [CrossRef]
- Chadi, N.; Spinoso-Di Piano, C.; Osmanlliu, E.; Gravel, J.; Drouin, O. Mental Health–Related Emergency Department Visits in Adolescents Before and During the COVID-19 Pandemic: A Multicentric Retrospective Study. J. Adolesc. Health 2021, 69, 847–850. [Google Scholar] [CrossRef]
- Cousien, A.; Acquaviva, E.; Kernéis, S.; Yazdanpanah, Y.; Delorme, R. Temporal Trends in Suicide Attempts Among Children in the Decade Before and During the COVID-19 Pandemic in Paris, France. JAMA Netw. Open 2021, 4, e2128611. [Google Scholar] [CrossRef]
- Davico, C.; Marcotulli, D.; Lux, C.; Calderoni, D.; Cammisa, L.; Bondone, C.; Rosa-Brusin, M.; Secci, I.; Porro, M.; Campanile, R.; et al. Impact of the COVID-19 Pandemic on Child and Adolescent Psychiatric Emergencies. J. Clin. Psychiatr. 2021, 6, 20m13467. [Google Scholar] [CrossRef]
- Ferrando, S.J.; Klepacz, L.; Lynch, S.; Shahar, S.; Dornbush, R.; Smiley, A.; Miller, I.; Tavakkoli, M.; Regan, J.; Bartell, A. Psychiatric Emergencies during the Height of the COVID-19 Pandemic in the Suburban New York City Area. J. Psychiatr. Res. 2021, 136, 552–559. [Google Scholar] [CrossRef]
- Gracia, R.; Pamias, M.; Mortier, P.; Alonso, J.; Pérez, V.; Palao, D. Is the COVID-19 Pandemic a Risk Factor for Suicide Attempts in Adolescent Girls? J. Affect. Disord. 2021, 292, 139–141. [Google Scholar] [CrossRef]
- Gratz, K.L.; Mann, A.J.D.; Tull, M.T. Suicidal Ideation among University Students during the COVID-19 Pandemic: Identifying at-Risk Subgroups. Psychiatry Res. 2021, 302, 114034. [Google Scholar] [CrossRef] [PubMed]
- Hill, R.M.; Rufino, K.; Kurian, S.; Saxena, J.; Saxena, K.; Williams, L. Suicide Ideation and Attempts in a Pediatric Emergency Department Before and During COVID-19. Pediatrics 2021, 147, e2020029280. [Google Scholar] [CrossRef] [PubMed]
- Leff, R.A.; Setzer, E.; Cicero, M.X.; Auerbach, M. Changes in Pediatric Emergency Department Visits for Mental Health during the COVID-19 Pandemic: A Cross-Sectional Study. Clin. Child Psychol. Psychiatry 2021, 26, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Mourouvaye, M.; Bottemanne, H.; Bonny, G.; Fourcade, L.; Angoulvant, F.; Cohen, J.F.; Ouss, L. Association between Suicide Behaviours in Children and Adolescents and the COVID-19 Lockdown in Paris, France: A Retrospective Observational Study. Arch. Dis. Child. 2021, 106, 918–919. [Google Scholar] [CrossRef]
- Odd, D.; Williams, T.; Appleby, L.; Gunnell, D.; Luyt, K. Child Suicide Rates during the COVID-19 Pandemic in England. J. Affect. Disord. Rep. 2021, 6, 100273. [Google Scholar] [CrossRef]
- Gonçalves-Pinho, M.; Mota, P.; Ribeiro, J.; Macedo, S.; Freitas, A. The Impact of COVID-19 Pandemic on Psychiatric Emergency Department Visits—A Descriptive Study. Psychiatr. Q. 2021, 92, 621–631. [Google Scholar] [CrossRef]
- Sokoloff, W.C.; Krief, W.I.; Giusto, K.A.; Mohaimin, T.; Murphy-Hockett, C.; Rocker, J.; Williamson, K.A. Pediatric Emergency Department Utilization during the COVID-19 Pandemic in New York City. Am. J. Emerg. Med. 2021, 45, 100–104. [Google Scholar] [CrossRef]
- Turner, B.J.; Robillard, C.L.; Ames, M.E.; Craig, S.G. Prevalence and Correlates of Suicidal Ideation and Deliberate Self-Harm in Canadian Adolescents during the Coronavirus Disease 2019 Pandemic. Can. J. Psychiatry 2021, 070674372110366. [Google Scholar] [CrossRef]
- Yalçın, M.; Baş, A.; Bilici, R.; Özdemir, Y.Ö.; Beştepe, E.E.; Kurnaz, S.; Güneş, M.; Kurt, V.; Koyu, E. Psychiatric Emergency Visit Trends and Characteristics in a Mental Health Epicenter in Istanbul during COVID-19 Lockdown. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 2299–2310. [Google Scholar] [CrossRef]
- Yard, E.; Radhakrishnan, L.; Ballesteros, M.F.; Sheppard, M.; Gates, A.; Stein, Z.; Hartnett, K.; Kite-Powell, A.; Rodgers, L.; Adjemian, J.; et al. Emergency Department Visits for Suspected Suicide Attempts Among Persons Aged 12–25 Years Before and During the COVID-19 Pandemic—United States, January 2019–May 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 888–894. [Google Scholar] [CrossRef]
- Zhu, S.; Zhuang, Y.; Lee, P.; Wong, P.W.C. The Changes of Suicidal Ideation Status among Young People in Hong Kong during COVID-19: A Longitudinal Survey. J. Affect. Disord. 2021, 294, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Leeb, R.T.; Bitsko, R.H.; Radhakrishnan, L.; Martinez, P.; Njai, R.; Holland, K.M. Mental health–related emergency department visits among children aged<18 years during the COVID-19 pandemic—United States, January 1–October 17, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1675. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Misirlis, N.; Zwaan, M.H.; Weber, D. International Students’ Loneliness, Depression and Stress Levels in COVID-19 Crisis. The Role of Social Media and the Host University. J. Contemp. Educ. Theory Res. 2020, 4, 20–25. [Google Scholar] [CrossRef]
- Zhao, N.; Zhou, G. Social Media Use and Mental Health during the COVID-19 Pandemic: Moderator Role of Disaster Stressor and Mediator Role of Negative Affect. Appl. Psychol. Health Well-Being 2020, 12, 1019–1038. [Google Scholar] [CrossRef]
- Brothwood, P.L.; Baudinet, J.; Stewart, C.S.; Simic, M. Moving Online: Young People and Parents’ Experiences of Adolescent Eating Disorder Day Programme Treatment during the COVID-19 Pandemic. J. Eat. Disord. 2021, 9, 62. [Google Scholar] [CrossRef]
- David, M.E.; Roberts, J.A. Smartphone Use during the COVID-19 Pandemic: Social versus Physical Distancing. Int. J. Environ. Res. Public Health 2021, 18, 1034. [Google Scholar] [CrossRef]
- De Pasquale, C.; Pistorio, M.L.; Sciacca, F.; Hichy, Z. Relationships Between Anxiety, Perceived Vulnerability to Disease, and Smartphone Use During Coronavirus Disease 2019 Pandemic in a Sample of Italian College Students. Front. Psychol. 2021, 12, 692503. [Google Scholar] [CrossRef]
- Fernandes, B.; Uzun, B.; Aydin, C.; Tan-Mansukhani, R.; Vallejo, A.; Saldaña-Gutierrez, A.; Nanda Biswas, U.; Essau, C.A. Internet Use during COVID-19 Lockdown among Young People in Low- and Middle-Income Countries: Role of Psychological Wellbeing. Addict. Behav. Rep. 2021, 14, 100379. [Google Scholar] [CrossRef]
- Li, Y.; Zhao, J.; Ma, Z.; McReynolds, L.S.; Lin, D.; Chen, Z.; Wang, T.; Wang, D.; Zhang, Y.; Zhang, J.; et al. Mental Health Among College Students During the COVID-19 Pandemic in China: A 2-Wave Longitudinal Survey. J. Affect. Disord. 2021, 281, 597–604. [Google Scholar] [CrossRef]
- Nicholas, J.; Bell, I.H.; Thompson, A.; Valentine, L.; Simsir, P.; Sheppard, H.; Adams, S. Implementation Lessons from the Transition to Telehealth during COVID-19: A Survey of Clinicians and Young People from Youth Mental Health Services. Psychiatry Res. 2021, 299, 113848. [Google Scholar] [CrossRef] [PubMed]
- Palinkas, L.A.; De Leon, J.; Salinas, E.; Chu, S.; Hunter, K.; Marshall, T.M.; Tadehara, E.; Strnad, C.M.; Purtle, J.; Horwitz, S.M.; et al. Impact of the COVID-19 Pandemic on Child and Adolescent Mental Health Policy and Practice Implementation. Int. J. Environ. Res. Public Health 2021, 18, 9622. [Google Scholar] [CrossRef]
- Rauschenberg, C.; Schick, A.; Goetzl, C.; Roehr, S.; Riedel-Heller, S.G.; Koppe, G.; Durstewitz, D.; Krumm, S.; Reininghaus, U. Social Isolation, Mental Health, and Use of Digital Interventions in Youth during the COVID-19 Pandemic: A Nationally Representative Survey. Eur. Psychiatry 2021, 64, e20. [Google Scholar] [CrossRef] [PubMed]
- Sewall, C.J.R.; Goldstein, T.R.; Rosen, D. Objectively Measured Digital Technology Use during the COVID-19 Pandemic: Impact on Depression, Anxiety, and Suicidal Ideation among Young Adults. J. Affect. Disord. 2021, 288, 145–147. [Google Scholar] [CrossRef]
- Shao, R.; Shi, Z.; Zhang, D. Social Media and Emotional Burnout Regulation during the COVID-19 Pandemic: Multilevel Approach. J. Med. Internet Res. 2021, 23, e27015. [Google Scholar] [CrossRef] [PubMed]
- Shaw, H.; Robertson, S.; Ranceva, N. What Was the Impact of a Global Pandemic (COVID-19) Lockdown Period on Experiences within an Eating Disorder Service? A Service Evaluation of the Views of Patients, Parents/Carers and Staff. J. Eat. Disord. 2021, 9, 14. [Google Scholar] [CrossRef]
- Stewart, C.; Konstantellou, A.; Kassamali, F.; McLaughlin, N.; Cutinha, D.; Bryant-Waugh, R.; Simic, M.; Eisler, I.; Baudinet, J. Is This the ‘new Normal’? A Mixed Method Investigation of Young Person, Parent and Clinician Experience of Online Eating Disorder Treatment during the COVID-19 Pandemic. J. Eat. Disord. 2021, 9, 78. [Google Scholar] [CrossRef]
- Wheaton, M.G.; Prikhidko, A.; Messner, G.R. Is Fear of COVID-19 Contagious? The Effects of Emotion Contagion and Social Media Use on Anxiety in Response to the Coronavirus Pandemic. Front. Psychol. 2021, 11, 567379. [Google Scholar] [CrossRef]
- Wood, S.M.; Pickel, J.; Phillips, A.W.; Baber, K.; Chuo, J.; Maleki, P.; Faust, H.L.; Petsis, D.; Apple, D.E.; Dowshen, N.; et al. Acceptability, Feasibility, and Quality of Telehealth for Adolescent Health Care Delivery During the COVID-19 Pandemic: Cross-Sectional Study of Patient and Family Experiences. JMIR Pediatr. Parent. 2021, 4, e32708. [Google Scholar] [CrossRef]
- Yang, X.; Yip, B.H.K.; Mak, A.D.P.; Zhang, D.; Lee, E.K.P.; Wong, S.Y.S. The Differential Effects of Social Media on Depressive Symptoms and Suicidal Ideation among the Younger and Older Adult Population in Hong Kong During the COVID-19 Pandemic: Population-Based Cross-Sectional Survey Study. JMIR Public Health Surveill. 2021, 7, e24623. [Google Scholar] [CrossRef]
- 290 Million Students out of School Due to COVID-19: UNESCO Releases First Global Numbers and Mobilizes Response. Available online: https://en.unesco.org/news/290-million-students-out-school-due-covid-19-unesco-releases-first-global-numbers-and-mobilizes (accessed on 30 November 2021).
- Subrahmanyam, K.; Smahel, D. Digital Youth; Springer: Cham, Switzerland, 2011; pp. 123–142. [Google Scholar] [CrossRef]
- Bartsch, M.; Subrahmanyam, K. Technology and Self-presentation. In The Wiley Handbook of Psychology, Technology, and Society; Rosen, L.D., Cheever, N.A., Carrier, L.M., Eds.; Wiley: Hoboken, NJ, USA, 2015; pp. 339–357. [Google Scholar]
- Van der Linden, S.; Roozenbeek, J.; Compton, J. Inoculating against Fake News about COVID-19. Front. Psychol. 2020, 11, 566790. [Google Scholar] [CrossRef] [PubMed]
- Zarocostas, J. How to Fight an Infodemic. Lancet 2020, 395, 676. [Google Scholar] [CrossRef]
- WHO. Novel Coronavirus (2019-NCoV): Situation Report-13; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Garfin, D.R.; Silver, R.C.; Holman, E.A. The Novel Coronavirus (COVID-2019) Outbreak: Amplification of Public Health Consequences by Media Exposure. Health Psychol. 2020, 39, 355–357. [Google Scholar] [CrossRef] [PubMed]
- Adelantado-Renau, M.; Moliner-Urdiales, D.; Cavero-Redondo, I.; Beltran-Valls, M.R.; Martínez-Vizcaíno, V.; Álvarez-Bueno, C. Association between Screen Media Use and Academic Performance among Children and Adolescents: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2019, 173, 1058–1067. [Google Scholar] [CrossRef]
- Ho, R.C.; Zhang, M.W.B.; Tsang, T.Y.; Toh, A.H.; Pan, F.; Lu, Y.; Cheng, C.; Yip, P.S.; Lam, L.T.; Lai, C.M.; et al. The Association between Internet Addiction and Psychiatric Co-Morbidity: A Meta-Analysis. BMC Psychiatry 2014, 14, 183. [Google Scholar] [CrossRef] [Green Version]
- Siomos, K.; Floros, G.; Makris, E.; Christou, G.; Hadjulis, M. Internet Addiction and Psychopathology in a Community before and during an Economic Crisis. Epidemiol. Psychiatr. Sci. 2014, 23, 301–310. [Google Scholar] [CrossRef]
- Schimmenti, A.; Passanisi, A.; Caretti, V.; La Marca, L.; Granieri, A.; Iacolino, C.; Gervasi, A.M.; Maganuco, N.R.; Billieux, J. Traumatic Experiences, Alexithymia, and Internet Addiction Symptoms among Late Adolescents: A Moderated Mediation Analysis. Addict. Behav. 2017, 64, 314–320. [Google Scholar] [CrossRef]
- Cui, X.; Chi, X. The Relationship between Social Support and Internet Addiction among Chinese Adolescents during the COVID-19 Pandemic: A Multiple Mediation Model of Resilience and Post-Traumatic Stress Disorder Symptoms. Psychol. Res. Behav. Manag. 2021, 14, 1665. [Google Scholar] [CrossRef]
- Wong, A.; Ho, S.; Olusanya, O.; Antonini, M.V.; Lyness, D. The Use of Social Media and Online Communications in Times of Pandemic COVID-19. J. Intensive Care Soc. 2021, 22, 255–260. [Google Scholar] [CrossRef]
- Ko, C.-H.; Yen, J.-Y. Impact of COVID-19 on Gaming Disorder: Monitoring and Prevention. J. Behav. Addict. 2020, 9, 187–189. [Google Scholar] [CrossRef]
- Balhara, Y.S.; Kattula, D.; Singh, S.; Chukkali, S.; Bhargava, R. Impact of Lockdown Following COVID-19 on the Gaming Behavior of College Students. Indian J. Public Health 2020, 64, 172. [Google Scholar] [CrossRef] [PubMed]
- King, D.L.; Delfabbro, P.H.; Billieux, J.; Potenza, M.N. Problematic Online Gaming and the COVID-19 Pandemic. J. Behav. Addict. 2020, 9, 184–186. [Google Scholar] [CrossRef] [PubMed]
- Anjum, S.; Ullah, R.; Suleman Rana, M.; Ali Khan, H.; Shabir Memon, F.; Ahmed, Y.; Jabeen, S.; Faryal, R. COVID-19 Pandemic: A Serious Threat for Public Mental Health Globally. Psychiatr. Danub. 2020, 32, 245–250. [Google Scholar] [CrossRef]
- Cosic, K.; Popovic, S.; Sarlija, M.; Kesedzic, I. Impact of Human Disasters and COVID-19 Pandemic on Mental Health: Potential of Digital Psychiatry. Psychiatr. Danub. 2020, 32, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Moreno, C.; Wykes, T.; Galderisi, S.; Nordentoft, M.; Crossley, N.; Jones, N.; Cannon, M.; Correll, C.U.; Byrne, L.; Carr, S.; et al. How Mental Health Care Should Change as a Consequence of the COVID-19 Pandemic. Lancet Psychiatry 2020, 7, 813–824. [Google Scholar] [CrossRef]
- Chen, I.H.; Chen, C.Y.; Pakpour, A.H.; Griffiths, M.D.; Lin, C.Y.; Li, X.D.; Tsang, H.W.H. Problematic Internet-Related Behaviors Mediate the Associations between Levels of Internet Engagement and Distress among Schoolchildren during COVID-19 Lockdown: A Longitudinal Structural Equation Modeling Study. J. Behav. Addict. 2021, 10, 135–148. [Google Scholar] [CrossRef]
- A Health Telematics Policy in Support of WHO’s Health-for-All Strategy for Global Health Development: Report of the WHO Group Consultation on Health Telematics, 11–16 December, Geneva. 1997. Available online: https://apps.who.int/iris/handle/10665/63857 (accessed on 28 January 2022).
- Chakrabarti, S. Usefulness of Telepsychiatry: A Critical Evaluation of Videoconferencing-Based Approaches. World J. Psychiatry 2015, 5, 286. [Google Scholar] [CrossRef]
- Dwyer, T.F. Telepsychiatry: Psychiatric Consultation by Interactive Television. Am. J. Psychiatry 2006, 130, 865–869. [Google Scholar] [CrossRef]
- Chipps, J.; Brysiewicz, P.; Mars, M. Effectiveness and Feasibility of Telepsychiatry in Resource Constrained Environments? A Systematic Review of the Evidence. Afr. J. Psychiatry 2012, 15, 235–243. [Google Scholar] [CrossRef] [Green Version]
- American Psychiatric Association. Telepsychiatry. Available online: https://www.psychiatry.org/psychiatrists/practice/telepsychiatry (accessed on 22 December 2021).
- Johnson, K.R.; Fuchs, E.; Horvath, K.J.; Scal, P. Distressed and Looking for Help: Internet Intervention Support for Arthritis Self-Management. J. Adolesc. Health 2015, 56, 666–671. [Google Scholar] [CrossRef]
- Davis, C.; Ng, K.C.; Oh, J.Y.; Baeg, A.; Rajasegaran, K.; Chew, C.S.E. Caring for Children and Adolescents with Eating Disorders in the Current Coronavirus 19 Pandemic: A Singapore Perspective. J. Adolesc. Health 2020, 67, 131–134. [Google Scholar] [CrossRef] [PubMed]
- Gordon, C.M.; Katzman, D.K. Lessons Learned in Caring for Adolescents with Eating Disorders: The Singapore Experience. J. Adolesc. Health 2020, 67, 5–6. [Google Scholar] [CrossRef] [PubMed]
- Datta, N.; Derenne, J.; Sanders, M.; Lock, J.D. Telehealth Transition in a Comprehensive Care Unit for Eating Disorders: Challenges and Long-Term Benefits. Int. J. Eat. Disord. 2020, 53, 1774–1779. [Google Scholar] [CrossRef] [PubMed]
| Authors | Study Design | States | Date of Data Collection | Sample Characteristics | Sampling Strategy/Data Collection Method | Outcomes |
|---|---|---|---|---|---|---|
| Cai et al., 2020 [78] | Longitudinal study | China | February–March 2020 | N = 126 COVID-19 survivors Mage = 45.7 | Online survey questionnaire | ↔ No significant difference between older COVID-19 survivors and the younger survivors for depression symptoms. ↑ Younger participants have more emotional reactivity to infection, more anxiety symptoms, and more stress reaction symptoms than older survivors. |
| Blankenburg et al., 2021 [79] | Cross-sectional study | Germany | March–April 2021 | N = 1560 students (Mage = 15 years) 1365 (88%) were seronegative, 188 (12%) were seropositive | Long-COVID19 survey questionnaire | ↑ of neurocognitive, pain, and mood symptoms in the surveyed group of adolescents, most reported symptoms were insomnia, pain, fatigue, and concentration difficulties. |
| Blom-berg et al., 2021 [23] | Longitudinal study | Norway | February–April 2020 | N = 312 COVID-19 survivors Mage = 46 years | Long term follow-up survey | 52% of home-isolated young adults, aged 16–30 years, had symptoms: loss of taste and/or smell (28%), fatigue (21%), dyspnea (13%), impaired concentration (13%), and memory problems (11%). |
| Hampshire et al., 2021 [80] | Cross-sectional study | United Kingdom | January–December 2020 | N = 81,337 participants (68,648 control) | Online questionnaire | Young adults as early as in their 20s showed large cognitive impairments in multiple domains particularly semantic problem solving, visual attention, and executive functions. |
| Roge et al., 2021 [81] | Longitudinal study | Latvia | 1 July 2020, and 30 April 2021 | N = 236 pediatric COVID-19 patients N = 142 comparison group patients | Clinical interview | 2/3 of patients reported at least one persistent symptom 53% had two or more concurrent symptoms. The prevalence of persistent fatigue and cognitive symptoms significantly ↑ according to the study’s age groups: the highest rates were found among teenagers (14.7%, 1–4-year-olds versus 37.0%, 15–18-year-olds). |
| Authors | Study Design | States | Date of Data Collection | Sample Characteristics | Sampling Strategy/Data Collection Method | Outcomes |
|---|---|---|---|---|---|---|
| Al-Musharaf et al., 2020 [112] | Cross- sectional study | Saudi Arabia | 18 May 2020 to 28 May 2020 | N = 638 women, ages 18–39 | Online survey | 47.2% reported low emotional eating, 40.4% moderate, and 12.4% high. The main emotional eating indicators/predictors were fat intake (p = 0.004), number of meals (p < 0.001), sugar consumption (p < 0.001), body mass index (p < 0.001), stress (p = 0.004), energy intake (p = 0.04), and fast food intake frequency (p < 0.01). EE score correlated negatively with increased family income (p = 0.049). |
| Baiano et al., 2020 [108] | Longitudinal study | Italy | T0: 4 November 2019–17 February 2020 T1: 26 April–30 April 2020. | N = 25 University students Mage = 23.84 | Online survey | ↑ worriers at pre-lockdown and during lockdown conditions, ↑ anxiety sensitivity, and fear of mental health. |
| Cao et al., 2020 [101] | Cross- sectional study | China | - | N = 7143 Undergraduate age College students | - | About 24.9% of respondents experienced anxiety because of the COVID-19 outbreak. Protective factors: family income stability, living with parents, and social support. Negative factors: having relatives infected with COVID-19, economic stressors, academic delay, and effects on daily life. |
| Cellini et al., 2020 [120] | Longitudinal study | Italy | March 2020 | N = 1310 University students and young workers aged 18–35 Mage = 23.91 | Online survey | ↓ sleep-wake rhythms markedly changed ↓ lower sleep quality. The decrease in sleep quality was stronger for people with a higher level of depression, anxiety, and stress symptomatology. |
| Dumas et al., 2020 [121] | Cross- sectional study | Canada | 4–13 April 2020 | N = 1054 14–18 years Mage = 16.68 | Online survey | ↑ in the frequency of both alcohol and cannabis use among adolescents. |
| Ellis et al., 2020 [92] | Longitudinal study | Canada | 4–16 April 2020 | N = 1054 Mage = 16.68 | Online survey | ↑ loneliness and depression, especially for adolescents who spend more time on social media. |
| Essadek et al., 2020 [96] | Cross- sectional study | France | 27 April to 30 April 2020 | N = 8004 University students Mage = 21.7 | Online survey | 43% of students suffered from depression (6.96% of severe level) 39.19% suffered from anxiety (20.7% of severe level) 42.94% from distress (16, 09% of severe level). Female scores were significantly higher than those of males. |
| Glowacz et al., 2020 [100] | Cross- sectional study | Belgium | 17 April to 1 May 2020 | N= 2871 adults 18–85 years (Mage = 33.67) | Online survey | ↓ of living space, occupational activity, social contact, and alcohol use. ↑ anxiety, depression, and uncertainty than older participants. |
| Islam et al., 2020 [83] | Cross- sectionalstudy | Bangladesh | March 2020 | N = 476 17 and older University students | Online survey | More than 2/3 of the students reported mild to severe depression (82.4%) and anxiety (87.7%). The prolonged unemployment, financial insecurity, and concern about academic performance were the most significant stressors. |
| Jiang et al., 2020 [105] | Cross- sectionalstudy | China | February 2020 | N = 472 University students (17–22 years old) | Online survey | ↑ levels in somatization, obsessive-compulsive disorder, interpersonal sensitivity, anxiety, phobic anxiety, paranoid ideation, and general severity index, during the pandemic. |
| Keel et al., 2020 [114] | Longitudinal study | USA | T1: 8–24 January 2020 T2: 15–24 April 2020 | N = 90 university students Mage: 19.45 at T1; 19.71 at T2. | Online survey | ↑ body weight, eating, screen time ↓ physical activity along with ↑ concerns about weight, shape, and eating since COVID-19. Longitudinal data indicated no significant change in weight, body mass index (BMI), or BMI category. |
| Khan et al., 2020 [84] | Cross- sectionalstudy | Bangladesh | April 2020 | N = 505 19 or less (12.67%) 20–24 (78.42%) 25 or more (8.91%) College and university students | Online survey | 28.5% of the respondents experienced stress, 33.3% anxiety, and 46.92% depression from mild to extremely severe. 69.31% had event-specific distress from mild to severe. Perceiving physical symptoms similar to the symptoms of COVID-19, fear of infection, financial uncertainty, inadequate food supply, no physical activity, and limited or no social activity had a significant association with stress, anxiety, depression, and post-traumatic symptoms. Excessive exposure to COVID-19 news in social and mass media had a significant association with depression, stress, psychological impact in terms of event-specific distress. |
| Liu et al., 2020 [97] | Cross- sectionalstudy | USA | 13 April to 19 May 2020 | N = 898 Aged 18–30 years | Online survey | ↑ levels of depression (43.3%, PHQ-8 scores ≥ 10), anxiety scores (45.4%, GAD-7 scores ≥ 10), and PTSD symptoms (31.8%, PCL-C scores ≥ 45). ↑ loneliness, COVID-19-specific worry, and ↓ distress tolerance were significantly associated with clinical levels of depression, anxiety, and PTSD symptoms. |
| Ma et al., 2020 [93] | Cross- sectional study | China | 3–10 February 2020 | N = 746,217 College students | Online survey | The prevalence rates of acute stress, depressive and anxiety symptoms were 34.9%, 21.1% and 11.0%. COVID-19 epidemic factors that were associated with increased risk of mental health problems were having relatives or friends being infected. Students with exposure to media coverage of the COVID-19 ≥ 3 h/day were 2.13 times more likely than students with media exposure < 1 h/day to have acute stress symptoms. |
| Oosterhoff et al., 2020 [107] | Cross- sectional study | USA | 28–29 March 2020 | N = 683 adolescents Mage = 16.35 | Online survey | 98.1% reported engaging in at least a little social distancing due to social responsibility and not wanting others to get sick. Specific motivations for social distancing were differentially associated with adolescents’ anxiety symptoms, depressive symptoms, burdensomeness, and belongingness. |
| Parola et al., 2020 [82] | Longitudinal study | Italy | March–April 2020 | N = 97 Young in a lockdown condition (aged 19–29). | Online survey | ↑ Internalising and externalising symptoms while the lockdown measures were in place. |
| Puhl et al., 2020 [116] | Longitudinal study | USA | T1: 2018 T2: 2020 | N = 584 participants T1 Mage = 21.9 years T2 Mage = 24.6 years | Online survey | Pre-pandemic experiences of weight stigma predicted higher levels of depressive symptoms (p < 0.001), stress (p = 0.001), eating as a coping strategy (p < 0.001), and an increased likelihood of binge eating (p < 0.001) among young adults during the COVID-19 pandemic but were unrelated to physical activity. |
| Qi et al., 2020 [90] | Cross- sectional study | China | 8–15 March 2020 | N = 7202 aged 14–18 years | Online survey | ↑ prevalence of depression symptoms and anxiety symptoms. Only 24.6% of adolescents reported high levels of social support. |
| Seçer et al., 2020 [89] | Cross- sectional study | Turkey | Data collected during 15 days, no other information reported | N = 568 aged 14–18 years mean age = 16.4 | Online survey | Fear of COVID-19 has a positive and significant effect on OCD. Considering possibilities, such as the speed of disease spread and the risk of death, it may be reasonable for adolescents to have washing and hoarding obsessions. |
| Scharmer et al., 2020 [117] | Cross- sectional study | USA | March–April 2020 | N= 295 University students Mage= 19.7 years | Online survey | ↑ ED pathology, but not compulsive exercise. Results from dependent samples t-tests indicated ↓ in exercise associated with COVID-19 (p < 0.001). Trait and COVID-19 intolerance of uncertainty moderated associations between COVID-19 anxiety and compulsive exercise and ED pathology. COVID-19 anxiety was more strongly related to compulsive exercise and ED pathology for individuals with lower intolerance of uncertainty. |
| Son et al., 2020 [97] | Cross- sectional study | USA | April–May 2020 | N = 195 university students Mage = 20.7 years | Online survey | 71% indicated ↑stress and anxiety 20% indicated it remained the same 9% mentioned ↓ stress and anxiety. Among those who perceived increased stress and anxiety, only 5% used mental health counselling services. |
| Tee et al., 2020 [91] | Cross- sectional study | Philippines | 28 March–12 April 2020 | N = 1879 Mage = 34.5 years | Online survey | 16.3% of respondents rated the psychological impact of the outbreak as moderate-to-severe; 16.9% reported moderate-to-severe depressive symptoms; 28.8% had moderate-to-severe anxiety levels; and 13.4% had moderate-to-severe stress levels. Females had higher rates of psychological distress, anxiety, and depression due to the pandemic. |
| Wan Mohd Yunus et al., 2020 [85] | Cross- sectional study | Malaysia | April 2020 | N = 1005 17 and older University students | Online survey | 22%, 34.3%, and 37.3% of the university students scored moderate to extremely severe levels of stress, anxiety, and depression symptoms, respectively. The levels of stress, anxiety, and depression were significantly different according to age: younger students experienced more stress, anxiety, and depression symptoms compared with older ones. |
| Wang et al., 2020 [125] | Cross- sectional study | USA | May 2020 | N = 2031 University students Mage = 22.88 | Online survey | 48.14% showed a moderate-to-severe level of depression, 38.48% showed a moderate- to-severe level of anxiety, and 18.04% had suicidal thoughts. |
| Yang et al., 2020 [108] | Cross- sectional study | China | 28–30 January 2020 | N = 8252 University students Mage = 17.9 | Online survey | 53.49% of the respondents were in a state of anxiety, while 46.83% were in a state of fear. |
| Zhou et al., 2020 [88] | Cross- sectional study | China | 8–15 March 2020 | N = 8072 students Mage= 16 range 12–18 years | Online survey | The prevalence of depressive symptoms, anxiety symptoms, and a combination of depressive and anxiety symptoms was 43.7%, 37.4%, and 31.3%, respectively |
| Baloch et al., 2021 [102] | Cross- sectional study | Pakistan | From 26 May to 6 June 2020 | N = 494 College and university students below 18 years (9.1%) 19–25 (77.3%) above 26 (13.5%) | Online survey | 41% of the respondents experienced minimal to moderate, marked to severe, and most extreme levels of anxiety. Female students were more anxious than male ones. The most prominent stressors are associated with online teaching, concerns about their academic performance, and completion of the current semester. |
| Bourion-Bédès et al., 2021 [103] | Cross- sectional study | France | May 2020 | N = 3928 College and University students Mage = 21.74 | Online survey | 61% of students experienced anxiety during the lockdown. Female gender, having relatives infected with COVID-19, conflicts at home, difficulties isolating themselves, noisy environments, no direct outside access, delay in final examinations, reduced time for learning, and increased tobacco consumption were the main risk factors for anxiety. |
| Buckley et al., 2021 [113] | Cross- sectional convergent mixed methods (CMM) design | Australia | April until May 2020 | N = 204 current (n = 93) and former (n = 111) athletes aged between 18 and 63 years Mage = 27.0 | Online survey | Eating disorders were reported by 21.1% of participants. There was a significant difference between males and females (p = 0.018, r = 0.17). 34.8% (n = 69) self-reported worsened body image. 32.8% (n = 65) self-reported a worsened food relationship directly from COVID-19. |
| Czeisler et al., 2021 [122] | Cross- sectional study | Australia | 15–24 September 2020 | N = 1531 ≥18 years | Online survey | Younger adults reported ↑ adverse mental or behavioural health conditions than older adults. |
| Esposito et al., 2021 [124] | Longitudinal study | Italy | 8 March–8 July 2020, versus the same period in 2019 | N = 62 35 first episode of psychosis) FEP patients were hospitalized in 2020 27 in 2019 | Clinical survey | ↑ 29.6% in psychiatric hospitalizations for incident psychosis cases were observed. Patients with FEP in 2020 were significantly older than patients with FEP in 2021 and presented with significantly ↓ fewer substances abuse. Interestingly, patients presenting with FEP in 2020 were significantly older than patients with FEP in 2019. |
| Faize et al., 2021 [104] | Cross- sectional study | Pakistan | - | N = 342 University students Undergraduate age | Online survey | 21.6% had mild, 9.4% had moderate and only 8.2% had severe anxiety. Students with severe anxiety reported psychological, social, and physical problems related to COVID-19, during the interview. |
| Kohls et al., 2021 [115] | Cross- sectional study | Germany | July– August 2020 | N = 3382 University students Mage = 23.98 | Online survey | 33.0% reported binge eating at least once per week, 3.5% reported vomiting as compensatory behaviors minimum once per week, 0.1% usage of laxative minimum once per week, 25% diet or calorie food minimum once per week, 28.0% reported excessive exercising minimum once per week, 45.8% reported weight changes during the COVID-19 lockdown, 26.2% reported weight gain, and 19.6% reported weight loss. Of those reporting any weight change, over 63% attributed this to the pandemic and lockdown. |
| Luijten et al., 2021 [109] | Longitudinal Study | The Netherlands | April 2020 versus 2018 | N = 2401 (2018) N = 844 (2020) 8–18 years | Online survey | During the lockdown, more patients reported severe Anxiety (RR = 1.95) and Sleep-Related Impairment (RR = 1.89) and fewer reported poor Global Health (RR = 0.36). |
| Mekonen et al., 2021 [86] | Cross- sectional study | Ethiopia | November 2020 | N = 350 20 and older University students Mage = 24.70 | Graduating class students available during the data collection period | The prevalence of stress, anxiety, and depression among graduating class students was 22.2%, 39.6%, and 40.2%, respectively. |
| Murata et al., 2021 [94] | Longitudinal study | USA | 27 April to 13 July 2020 | N = 4909 Mage = 40.3 Adolescents N = 583 Adults N = 4326 | Online survey | Adolescents were significantly more likely to report moderate to severe symptoms of depression (55% versus 29%; p < 0.001), anxiety (48% versus 29%; p < 0.001), PTSD (45% versus 33%; p < 0.001), suicidal ideation or behavior (38% versus 16%; p < 0.001), and sleep problems (69% versus 57%; p < 0.001) compared to adults. |
| Padrón et al., 2021 [87] | Cross sectional study | Spain | - | N = 932 University students 18 and older | Online survey | Results indicated that students experienced considerable psychological problems during the lockdown, with ↑ of emotional difficulties in females and younger students than in male and older students, respectively. |
| Simone et al., 2021 [118] | Longitudinal study | USA | T1: 2010–1018 T2: April–May 2020 | N = 720 Mage = 24.7 | Online survey | Low-stress management, food insecurity, higher depressive symptoms, and financial difficulties were significantly associated with a ↑ of extreme unhealthy weight control behaviors (UWCBs). were significantly associated with a ↑ of UWCBs. Higher stress and depressive symptoms were significantly associated with ↑ of binge eating. |
| Sun et al., 2021 [98] | Cross- sectional study | China | March–April 2020. | N = 1912 University students Mage = 20.28 | Online survey | 67.05% reported traumatic stress, 46.55% had depressive symptoms, and 34.73% reported anxiety symptoms. Further, 19.56% endorsed suicidal ideation. |
| Trott et al., 2021 [119] | Longitudinal study | United Kingdom | T1: April–July 2019 T2: August–September 2020 | N = 319 health club users Mage = 36.77 | Online survey | ↓ Exercise addiction scores (p = 0.034) ↑ Eating disorder symptomology scores (p = < 0.001) ↑ Leisure-time exercise (p = < 0.001) No differences in body dysmorphic disorder were found. |
| Wu et al., 2021 [123] | Longitudinal study | China | T0= 20 October 2019 T1 = 18 May 2020 | N = 1825 adolescents | Clinical survey | ↑ in adolescent Psychotic Like Experiences (PLEs) scores after the lockdown. We also found a positive correlation between changes in PLEs and changes in anxiety/depression. Furthermore, four PLEs trajectories were identified based on the report of PLEs at two time points: 60.4% with no PLEs, 9.3% remitted PLEs, 16.7% new PLEs, and 13.6% persistent PLEs. |
| Santomauro et al., 2021 [126] | Systematic review | - | 1 January 2020 and 29 January 2021 | N = 48 studies (46 studies met inclusion criteria for major depressive disorder and 27 for anxiety disorders) + additional 11 studies for major depressive disorder and seven studies for anxiety disorders | Systematic literature search | ↑ in the COVID-19 impact, index were associated with an ↑ in the prevalence of major depressive disorder and anxiety disorders. For both disorders, females were affected more than males, and younger age groups were affected more than older age groups. |
| Taquet et al., 2021 [127] | Ecological study | UK USA | 20 January 2020–19 January 2021 versus previous year | N = 5,186,451 patients Mage = 15.4 years | Electronic health records | ↑ 15.3% incidence of eating disorders in 2020 compared with previous years. ↑ of relative risk from March 2020 onwards exceeding 1.5 by the end of the year. This increase occurred solely in females, especially in teenagers. |
| Authors | Study Design | States | Date of Data Collection | Sample Characteristics | Sampling Strategy/Data Collection Method | Outcomes |
|---|---|---|---|---|---|---|
| Isumi et al., 2020 [136] | Ecological study | Japan | from March to May 2020 | Population < 20 years old | Statistics compiled by the Ministry of Health, Labor and Welfare | No significant change in suicide rates during school closure compared to previous years (IRR = 1.15, 95% CI: 0.81–1.64). |
| Burke et al., 2021 [137] | Cross- sectional study | USA | 13 March 2020, to 14 August 2020 | N = 143 psychiatrically hospitalized adolescents Mage = 15.13 | Participants were admitted to a psychiatric inpatient unit | COVID-specific suicidal ideation is common in high-risk youth and was associated with COVID-19-related negative emotions, elevated stress, and decreased public health guidance compliance. |
| Carison et al., 2021 [138] | Retrospective observational study | Australia | April– September 2020 versus the same period in 2019 | Patients younger than 18 years | Electronic medical record review of all emergency department patients with mental health discharge codes | 40% ↓ ED presentations 47% ↑ in MH presentations to ED during the study periods between 2019 and 2020. Suicidality presentation numbers were highest in June to September 2020 compared with 2019. Patients with a diagnosis of suicidality had a higher rate of re-presentation in 2020 compared to 2019. |
| Chadi et al., 2021 [139] | Retrospective observational study | Canada | January 2018 and December 2020 | Adolescent 12–17 years old | Electronic health records With mental health discharge codes | ↓ ED visits at the beginning of the pandemic followed by a significant ↑ in proportion of mental health related ED visits out of all adolescent ED visits. |
| Cousien et al., 2021 [140] | Cross- sectional study | France | 2010–2021 | Patients younger than 18 years | surveillance data | The number of suicide attempts among children ↓ from 12.2 at the lowest level (July to August) in 2019, to 7.8 during the first lockdown period (—36%). ↑ number of suicide attempts among children +116% before the second lockdown and +299%, early November to December 2020. |
| Czeisler et al., 2021 [122] | Cross- sectional study | USA | June 2020 | N = 5470 participants aged 18–24 years | Web-based surveys | 25% of the sample reported experiencing suicidal ideation related to the pandemic in the past 30 days, twice than in 2018. |
| Davico et al., 2021 [141] | Retrospective observational study | Italy | 7 weeks prior to 24 February 2020 and in the following 8 weeks of national lockdown versus 2019 | Patients < 18 years | Electronic medical record | 72.0% ↓ of all pediatric ED visits (3395) compared with the corresponding period in 2019 (12,128), with a 46.2% decrease in psychiatric visits (50 versus 93). |
| Ferrando et al., 2021 [142] | Longitudinal study | USA | 1 March–30 April 2020; N = 201) versus 1 January-28 February 2020 N = 355 | Emergency Psychiatric Evaluation (EPE) | Electronic medical record | The most common psychiatric diagnoses and presenting symptoms during both periods were depression and suicidal ideation. Comparing the Pre-COVID-19 and COVID-19 periods ↓ in emergency psychiatric volume was observed in children and adolescents, but not adults. |
| Gracia et al., 2021 [143] | Ecological study | Spain | March 2020 to March 2021 versus March 2019 to March 2020 | Adolescent 12–18 years old | Catalonia Suicide Risk Code (CRSC) | ↑ 25% suicide attempts among adolescents during the COVID-year and they noticed that the increase in girls was prominent in the starting school period in the COVID-year, where it reached 195%. |
| Gratz et al., 2021 [144] | Cross- sectional study | USA | Fall 2020 Fall 2014 Fall 2013 | N = 1700 university students | Screening questionnaires as part of the research requirement | Rates of suicide ideation were not significantly higher in Fall 2020 versus the earlier semesters.↑ Rates of suicidal ideation in Fall 2020 among sexual minority. |
| Hill et al., 2021 [145] | Cross- sectional study | USA | January–July 2020 | N = 9092 participants Mage 14.72 | Electronic health record of a large pediatric emergency department | ↑ suicide-related matched times when COVID-related stressors were intensified. |
| Leff et al., 2021 [146] | Cross-sectional study | USA | 10 March 2020, to 20 May 2020, versus the same period the year prior. | Patients younger than 18 years | Electronic medical record (EMR) system (EPIC™ 2010) | ↓ of 60.84% of patients presenting mental health-related diagnoses, compared to the pre-pandemic period. |
| Mourouvaye et al., 2021 [147] | Retrospective observational study | France | 1 January 2018 and 1 June 2020. | N = 234 Patients younger than 18 years | Patients were identified based on discharge codes | 50% ↓ in the incidence of admissions for suicide behaviour. |
| Odd et al., 2021 [148] | Ecological study | England | January 2020–May 2020 versus January 2019–May 2019 | Population under 18 years old | England’s National Child Mortality Database (NCMD) | No consistent evidence that child suicide deaths increased during the COVID-19 pandemic |
| Pinho et al., 2021 [149] | Retrospective observational study | Portugal | 19 March and 2 May 2019 versus 2020 | N = 2413 Adults admitted to the Psychiatric Unit of the emergency department | Administrative database that collects information of adult emergency department visits | 52·2% relative ↓ on the total number of psychiatric emergency visits between the two periods with a maximum decrease of 59·2% for the 18–30 years group. |
| Sokoloff et al., 2021 [150] | Retrospective observational study | USA | 7 March to 6 May 2020, and during the same period in 2018 and 2019. | PreCOVID n = 18,513; COVID n = 4068 Patients younger than 18 years | Data were collected Through routinely created hospital analytic reports | ↑ 100% Visits for suicidal ideation, suicide attempt, or self-harms (p < 0.001) ↓ 64% visits for psychiatric disorders. |
| Turner et al., 2021 [151] | Cross- sectional study | Canada | June and July 2020 | N = 809 participants aged 12–18 years Mage = 15.67 | Social media advertisements | 44% of adolescents experienced suicide ideation since the pandemic began, while 32% reported engaging in deliberate self-harm. SI and DSH were more common among youth who identified as transgender, gender fluid, or non-binary; who did not reside with both parents; and who reported frequent cannabis use or psychiatric concerns. |
| Yalçın et al., 2021 [152] | Longitudinal study | Turkey | 30 March–31 May 2020, versus the same period in 2019. | Patients younger than 18 years | Electronic medical records | ↓ 12% of PED visits and 41.6%, of hospitalizations in LP. ↑ anxiety and depressive disorders and bipolar disorders. |
| Yard et al., 2021 [153] | Retrospective observational study | USA | spring 2020; summer 2020; winter 2021 versus their corresponding reference periods in 2019. | Patients aged 12–25 years | Chief complaint terms and administrative discharge diagnosis codes. | ↑ 50.6% suspected suicide attempt ED visits among girls aged 12–17 years than 2019; ↑ 3.7% suspected suicide attempt ED visits among boys aged 12–17 years. ↑ among adults aged 18–25 years throughout the pandemic compared with that during 2019 |
| Zhu et al., 2021 [154] | Longitudinal study | Hong Kong | Baseline: 19 September; follow-up: 20 June | N = 1491 adolescents | A survey conducted in classrooms among volunteer participants | The prevalence of suicidal ideation was 24% and 21% among the participants before and during COVID-19, respectively. 65.0% remained non-suicidal, 14.0% recovered from being suicidal, 10.7% newly reported being suicidal, and 10.4% remained suicidal. |
| Authors | Study Design | States | Date of Data Collection | Sample Characteristics | Sampling Strategy/Data Collection Method | Outcomes |
|---|---|---|---|---|---|---|
| Misirlis et al., 2020 [157] | Cross-sectional study | The Nether-lands | 6 April– 6 May 2020 | N = 248 international university students | Online survey | Social media use has an inverse relationship with depressive symptoms and there was no statistically significant association between social media use and anxiety, loneliness, or the COVID-19 stressor (impact of events on student life). |
| Zhao et al., 2020 [158] | Cross-sectional study | China | 24 March– 1 April 2020 | N = 512 college students Mage = 22.12 | Online survey | A higher level of social media use was associated with worse mental health. More exposure to disaster news via social media ↑ depression for participants with high (but not low) levels of the disaster stressor. Path analysis showed negative affect mediated the relationship of social media use and mental health. |
| Brothwood et al., 2021 [159] | Cross-sectional study | United Kingdom | March and November 2020 | N = 14 young patients and N = 19 parents | Online survey | The experience of online Intensive Treatment Programme was rated positively. Parents rated it slightly higher (median = 8/10, IQR = 6.5–10) than young people (median = 6.5/10, IQR = 5–7).When online working was compared to face-to-face support responses were more varied. Young people generally found all online components of treatment less helpful than their parents. |
| David & Roberts, 2021 [160] | Cross-sectional study | USA | N = 400 university students Mage = 20 years | Online survey | Smartphones can mitigate the negative impact of social distancing on social connection and well-being | |
| De Pasquale et al., 2021 [161] | Cross-sectional study | Italy | September 2020–January 2021 | N = 194 University students Mage = 21.74 | Online survey | Both men and women showed a high risk of smartphone addiction in SAS-SV. University students showed moderate trait and state anxiety in STAI and moderate perceived vulnerability to disease in PVD. The results showed that fear of COVID-19 and trait anxiety appear to be the predictors of STAI and PVD but not the predictors of risk of smartphone addiction (SAS-SV). |
| Fernandes et al., 2021 [162] | Cross-sectional study | India, Malaysia, Mexico, and the UK | N = 185 participants Mage = 21.59 | Online survey | ↑ use of social media sites and streaming services. Compulsive internet use, gaming addiction, and social media use significantly predicted high scores of depression, loneliness, escapism, poor sleep quality, and anxiety related to the pandemic. | |
| Li et al., 2021 [163] | Longitudinal study | China | T1: 3 February–10 February 2020 T2: 24 March– 3 April 2020 | N = 68,685 University students | Online survey | Heavy social media use (>3 h/day) at T1 was found to be a significant predictor of acute stress and anxiety symptoms, but not of depressive symptoms. Heavy social media may have a negative influence on short- and long-term mental health. |
| Nicholas et al., 2021 [164] | Cross-sectional study | Australia | March–June 2020 | N = 308 participants (aged 12–25) + N = 92 clinicians | Online survey | Telehealth positively impacted service quality and was significantly more likely to rate telehealth positively than clinicians. |
| Palinkas et al., 2021 [165] | Quali-tative study | USA | November 2020–May 2021 | 29 State Mental Health Authorities (SMHA) | Online survey | Telehealth implementation ranged from 80% to 100%. Desire to continue the use of telehealth post-pandemic ranged from 60% to 100%. For both, the highest percentages were recorded in states with high rates of coronavirus positivity and high rates of unmet need. |
| Rauschenberg et al., 2021 [166] | Cross-sectional study | Germany | 5 May– 16 May 2020 | N = 666 participants aged 16–25 years Mage = 21.3 | Online survey | 8% of youth met the criteria for moderate or severe psychological distress. Social isolation worries and anxiety and objective risk indicators were associated with psychological distress. Psychological distress, worries, and anxiety were associated with a positive attitude toward using mental health interventions. |
| Sewall et al., 2021 [167] | Cross-sectional study | USA | August–November 2020 | N = 384 young adults Mage = 24.5 ± 5.1 | Online survey | None of the objectively-measured digital technology use variables were positively associated with depression, anxiety, or suicidal ideation at the within- or between-person levels. Pandemic-related impacts on mental health had by far the largest effects on depression, anxiety, and suicidal ideation. |
| Shao et al., 2021 [168] | Cross-sectional study | China | 7 February–18 February2020 | N = 528 Chinese citizens Mage = 35 | Online survey | Hyper-personal (social media-based) regulation strategies, such as disclosing and retweeting negative emotions, generate maladaptive effects: individuals who frequently disclose pandemic-related feelings and retweet negative emotions on social media reported less reappraisal of the stressful situation. |
| Shaw et al., 2021 [169] | Cross-sectional study | United Kingdom | March–July 2020 | N = 43 participants: 12 patients, 19 parents/carers, and 12 members of staff | Online survey | Patients, families, and staff all preferred face-to-face appointments over virtual options (e.g., telephone calls or video calls). There was no difference between the service satisfaction before and during COVID-19. |
| Stewart et al., 2021 [170] | Cross-sectional study | United Kingdom | 18 May–25 July 2020 | N = 53 young people with any eating disorder N = 75 parents N = 23 clinicians | Online survey | ↑ Satisfaction with treatment, good engagement, and ability to manage technology. Young people who had transitioned care, rather than started care virtually in lockdown, rated therapy as less effective. However, individual accounts of experience were more varied. |
| Wheaton et al., 2021 [171] | Cross-sectional study | USA | 5 April–13 May 2020 | N = 603 university students Mage = 22.92 | Online survey | Greater susceptibility to emotion contagion ↑ depression, anxiety, stress, and OCD symptoms. Consumption of media about COVID-19 predicted anxiety about COVID-19, though results were not moderated by emotion contagion. Emotion contagion did moderate the relationship between COVID-19-related media consumption and elevated OCD symptoms. |
| Wood et al., 2021 [172] | Cross-sectional study | USA | 16 March and 15 April 2020 | N = 55 patients (Mean Age = 18 years) + N = 123 caregivers (Mean age = 48 years) | Online survey | Telehealth as non-inferior to in-person visits with respect to communication, medication management, and mental health care for patients and caregivers. A higher proportion of patients compared to caregivers found telehealth inferior with respect to confidentiality (11/51, 22% versus 3/118, 2.5%, p < 0.001). One-quarter (14/55) of patients and 31.7% (39/123) of the caregivers reported technical difficulties. |
| Yang et al., 2021 [173] | Cross-sectional study | Hong Kong | May–June 2020 | N = 1070 participants | Telephone survey | Negative direct effect of social media use on depressive symptoms among older people (p = 0.04) but not among younger people (p = 0.55). The indirect effect via PTSD symptoms was significantly positive among both younger people (p = 0.02) and older people (p = 0.01). The indirect effect via social loneliness was significant among older people (p = 0.04) but not among younger people (p = 0.31). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brasso, C.; Bellino, S.; Blua, C.; Bozzatello, P.; Rocca, P. The Impact of SARS-CoV-2 Infection on Youth Mental Health: A Narrative Review. Biomedicines 2022, 10, 772. https://doi.org/10.3390/biomedicines10040772
Brasso C, Bellino S, Blua C, Bozzatello P, Rocca P. The Impact of SARS-CoV-2 Infection on Youth Mental Health: A Narrative Review. Biomedicines. 2022; 10(4):772. https://doi.org/10.3390/biomedicines10040772
Chicago/Turabian StyleBrasso, Claudio, Silvio Bellino, Cecilia Blua, Paola Bozzatello, and Paola Rocca. 2022. "The Impact of SARS-CoV-2 Infection on Youth Mental Health: A Narrative Review" Biomedicines 10, no. 4: 772. https://doi.org/10.3390/biomedicines10040772
APA StyleBrasso, C., Bellino, S., Blua, C., Bozzatello, P., & Rocca, P. (2022). The Impact of SARS-CoV-2 Infection on Youth Mental Health: A Narrative Review. Biomedicines, 10(4), 772. https://doi.org/10.3390/biomedicines10040772









