Abstract
Lentiviral vectors (LVs) play an important role in gene therapy and have proven successful in clinical trials. LVs are capable of integrating specific genetic materials into the target cells and allow for long-term expression of the cDNA of interest. The use of non-integrating LVs (NILVs) reduces insertional mutagenesis and the risk of malignant cell transformation over integrating lentiviral vectors. NILVs enable transient expression or sustained episomal expression, especially in non-dividing cells. Important modifications have been made to the basic human immunodeficiency virus (HIV) structures to improve the safety and efficacy of LVs. NILV-aided transient expression has led to more pre-clinical studies on primary immunodeficiencies, cytotoxic cancer therapies, and hemoglobinopathies. Recently, the third generation of self-inactivating LVs was applied in clinical trials for recombinant protein production, vaccines, gene therapy, cell imaging, and induced pluripotent stem cell (iPSC) generation. This review discusses the basic lentiviral biology and the four systems used for generating NILV designs. Mutations or modifications in LVs and their safety are addressed with reference to pre-clinical studies. The detailed application of NILVs in promising pre-clinical studies is also discussed.
1. Introduction
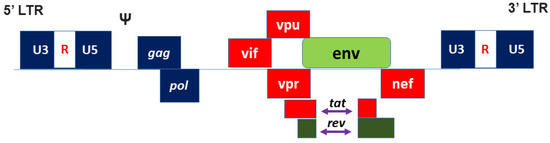
Lentiviruses are a genus of retroviruses that include human immunodeficiency virus (HIV), simian immunodeficiency virus (SIV), bovine immunodeficiency virus (BIV), feline immunodeficiency virus (FIV), puma lentiviruses, and equine infectious anaemia virus (EIAV). Among these viruses, HIV is widely used and has become the standard for lentiviral vectors (LVs) to facilitate the delivery of genetic material (DNA or RNA) into target cells [1,2]. HIV-1 derived LV is well known for its efficient and stable transduction in dividing and non-dividing cells. It integrates the desired transgene into the target cell genome using a viral integrase enzyme. In addition, LVs have the advantage of broad cell tropism and target-specific cell types through pseudotypes.
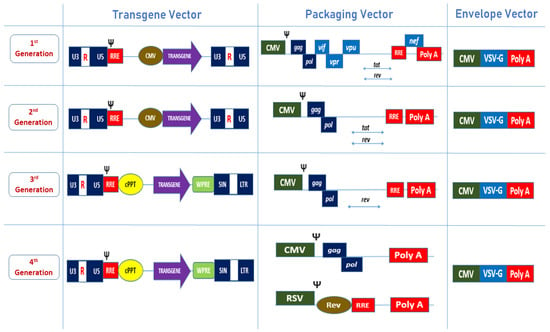
LVs can be stably integrated into the target cell genomes as proviruses. The three generations of LV-packaging systems are safer and are suited for the production with HEK293T cell line, while several studies reported increased vector production by utilising SV40 T-antigen [3,4]. Vectors yielded at 48 and 72 h post-transfection can be harvested from the supernatant. Further purification and concentration protocols should be performed to produce debris-free LVs. Due to the integration of provirus at the random site of a target genome, LVs may induce potential DNA mutations and detrimental side effects such as tumour formation [5,6]. LV-infected cells can become cancerous either by oncogene activation or tumour suppressor gene inactivation. It is also possible for insertional mutagenesis to occur due to gene dysregulation at the LV integration site within or near a coding region of the host genome [6]. In 2005, one study reported a high incidence of lentiviral-vector-associated tumorigenesis following in utero and neonatal gene transfer in mice [7]. Decreasing the efficiency of the integrase enzyme by inducing mutations in IN enzyme will impair the provirus formation, although vector DNA will exist as non-replicating episomes in the transduced cells. Thus, dividing cells gradually lose the episomal DNA, while the insertional mutagenesis is reduced. Alternatively, non-integrating LV (NILVs) can be designed by introducing mutations in the LV integrase or Δatt (LTR integrase attachment) site [8,9]. NILVs were optimised and modified to increase the transgene expression and to improvise the safety profile [10]. NILVs were developed to aid in gene transfer and deliver advancements in clinical applications, especially in cellular reprogramming and genetic therapy. Transient gene expression in NILVs is the ideal choice for cytotoxic-cancer therapies, protective NILV immunisation and episomal expression [11]. In this review, we first describe the biology of different LVs, the design of NILVs, and their limitations with respective to the possible solutions, which will be described. Next, the clinical applications of NILVs in different areas such as vaccination, cell-type differentiation, site-directed integration, and gene therapy will be reviewed.
4. Clinical Application of NILVs
LVs are among the most efficient gene transfer tools for dividing and non-dividing cells. However, insertional mutagenesis has been found in clinical trials with lentiviral vectors, prompting a detailed study of genotoxicity assays of all integrated vectors [76,77]. Avoiding integration is the most direct approach to overcome this problem for many clinical applications. This can be facilitated through extensive studies of the integrating mechanisms of lentiviruses, as discussed earlier. NILVs have been studied for the treatment of infectious and genetic diseases, in addition to being great cell mediators for reprogramming. From our point of view, the transient expression of NILVs over stable expression is also highly preferable for vaccinations, cell type differentiation, site-directed integration, and persistent episomal expression. This is due to the progressive loss of the transgenes expressed from these non-integrated proviral forms.
4.1. Vaccination
Transient expression of NILVs is required for vaccine development, as it shows sustained immune responses against various diseases in pre-clinical models, as shown in Table 5. Apart from cellular and humoral immunity, NILVs have also been proven successful for sustaining anti-tumour immunity. Dendritic cells (DC) are the most common targets for vaccines. They represent a safe and efficacious vaccination platform for the development of prophylactic vaccines. Many studies used dendritic cells as targets for malaria, thymoma, hepatitis B virus (HBV), and many more infectious agents that can be treated with NILVs. In a pre-clinical study, a single immunisation of NILVs encoded in a secreted form of the envelope of a virulent strain of West Nile virus (WNV) induced a strong B cell response, and a single immunisation was also sufficient to induce early and long-lasting protective immunity [78,79]. On the other hand, one in vivo study involving the H5 influenza A virus (IAV) demonstrated that the monoclonal antibody (mAb) administered through NILVs did not persist for longer time points [80]. However, this could be studied further to make it an effective strategy for rapid protection against infectious diseases in the future. Vaccinia virus [81], Zika virus [82], and human cytomegalovirus [83] have also been investigated in pre-clinical studies to test their immune responses.

Table 5.
Summary of elements used in developing non-integrating lentiviral vectors (NILVs) for vaccinations in pre-clinical studies conducted by the cited research teams. The first column lists the integrase mutations with subsequent columns categorizing the related diseases, target cells, and transgenes chosen for the mutations to be applied.
Additionally, the injection of the DC-directed IDLV encoding OVA has shown promising immune responses in C57BL/6 mice and complete protection against a thymoma tumour expressing a delivered ovalbumin (OVA) antigen in mice [87]. This shows that the IDLV system represents a promising and efficient vector platform for the future development of DC-based immunotherapy. Furthermore, cancer cell vaccines were also developed as an alternative approach to DC, since cancer cells express tumour antigens of interest and show robust improvements. Human immunodeficiency virus (HIV-1), human papillomavirus (HPV), and hepatitis C virus (HCV) were tested with cancer vaccines targeting the antigen-presenting cells [23]. Developing a strong cellular immunity among HIV patients has been the aim of several clinical studies. Therefore, several studies have suggested working on SIV-based NILVs to evaluate the induction of transgene-specific immune responses against sensibly designed structural HIV antigens, as proven in BALB/c mice [88,89]. This could be very efficient for studying the T cell immunogens for the development of long-lasting and effective HIV vaccines. A study showed that NILVs injected intramuscularly express systemic CD8+ T cells and antibody responses to the secreted hepatitis B virus (HBV) surface antigen and have also been proven as a great tumour therapy [90].
As a cancer immunotherapy candidate, NILVs delivering the tumour antigen NY-ESO-1 to the human dendritic cells in vivo have shown promising clinical results by showing sustained CD8+ T cells within 14 days post-immunisation and anti-tumour responses [91,92]. In 2020, this vaccine was improved with a heterologous boost by priming it with a recombinant protein, adenoviral vector, or self-replicating RNA boost. This resulted in increased efficacy of ZVex as a cancer vaccine. Improving the existing vaccines is a better option compared to developing new vaccines [86].
Another exciting study involved the application of NILVs to generate a vaccine candidate against coronavirus disease 2019 (COVID-19). Golden hamsters, which are naturally tolerant to SARS-CoV-2 replication and closely mimic human COVID-19 physiopathology, showed significant vaccination effectiveness and could limit lung deleterious damage by utilising the NILV approach [85]. These findings showed that NILV-based intranasal vaccination against SARS-CoV-2 has a significant prophylactic effect and is a viable option against COVID-19.
4.2. Cell-Type Differentiation
Regenerative medicine involving pluripotent stem cells has become an ideal goal for many researchers. Cellular reprogramming is another great application of NILVs via transient expression, as shown in Table 6. Additionally, iPSC production and differentiation into the lineage of interest is an alternative approach to the use of embryonic stem cells (ESCs). Furthermore, iPSCs can be an outstanding alternative to embryonic stem cells, although have several limitations and ethical concerns. Additionally, iPSCs also have similar pluripotency ability to human ESCs. As such, iPSC technology could be the desired application method for NILVs, as fewer genomic abnormalities are expected.

Table 6.
Summary of elements used in developing non-integrating lentiviral vectors (NILVs) for cell-type differentiation in pre-clinical studies conducted by the cited research teams. Important components of vector systems are provided in the table.
Successful transformation of human somatic cells into iPSCs was first carried out in 2007 using a lentiviral system [95]. Since then, multiple approaches were taken by other researchers worldwide in generating iPSCs with additional transcription factors, such as Oct4, Sox2, KLF4, and C-myc (OSKM) [96], while concentrating on higher safety profiles in clinical settings. Certain transcription factors are known as oncogenes and possible side effects are foreseeable [97]. Nonetheless, reprogramming without viral integration with plasmids or direct reprogramming protein delivery assays can solve this issue [98,99]. Additionally, several more recent technologies and approaches have been suggested for producing iPSCs without transgene integration that can cause possible mutagenesis, such as non-integrating viral vectors, RNA virions, RNA replicons, non-integrating replicating episomal plasmids, minicircles, Cre-loxP excision of transgenes, excisable transposon, protein transduction, RNA transfection, microRNA transfection, polycistron, and pre-integration of inducible reprogramming factors [42,100]. Polycistronic technology reduces the requirement for multiple viral vectors to deliver four different transcription factors, cutting this down to a single-stem cell cassette [101]. A study by Awe et al. compared the reprogramming efficiency of the polycistronic stem cell cassette (STEMCCA) to other integration-free approaches [102]. A similar polycistron approach was slightly modified using the Cre-Lox method. Another study was performed [103], whereby the integrated transgenes were excised from the reprogrammed genomes using the Cre-Lox method first and a single plasmid containing the four reprogramming factors was linked by the 2A sequence.
This type of advanced technology involving minimising genomic integrations can be used for potential human clinical trials with safer profiles. More studies are working on enhancing the iPSC reprogramming efficiency, such as by adding SV40 large T antigen (T) by 23–70-fold from human fibroblasts [104]. A recent study conducted a DNA methylation landscape assessment for isogenic iPSCs to compare different reprogramming methods, which could also be a way of proving the safety of iPSC lines generated by reading any significant changes in DNA methylation profiles [105].
Various platforms can be used to generate iPSCs through non-integrating methods, such as by transient transfection, EBV episomal plasmids, synthetic mRNA, adenoviral vectors, microRNA mimics, minicircles, and SeV vectors. However, all of these methods have low re-programming efficiency, except the Sendai viral vector [100]. NILV-based iPSCs can be used to study stem cell biology, as a cellular platform for pharmacological and toxicological studies, and can be considered as a possible source of autologous stem cells for use in regenerative medicine. Additionally, iPSCs have a great advantage in replacing human tissues or cells for disease modelling, drug screening (toxicity and efficacy), and cell-based therapy, especially for cardiovascular diseases [106].
However, most studies have used other non-integrated approaches, as discussed earlier, and only a few studies have used the NILV approach to produce iPSCs. In a previous study, purified integrase-deficient LV facilitated the generation of a population of purified hESC-derived hepatic progenitors that were devoid of integrated viral DNA. The ESCs could be differentiated into specific progenitor cells. For example, human embryonic stem cells (hESCs) encoding for green fluorescent protein (GFP) driven by the liver-specific apolipoprotein A-II (APOA-II) promoter can be differentiated into hepatic progenitors at day 16. Surprisingly, 99% of these APOA-II-GFP-positive cells expressed the hepatoblast markers, such as α-fetoprotein and cytokeratin-19, and were further cultured into more mature cells that resembled the hepatocytes [93]. This approach can be used in cell therapy and in in vitro applications, such as drug screening. The reprogramming efficiency of NILV has not been well-explored or compared with the SeV approach in vitro. Therefore, evidence is needed in the future of the dynamic effects on genomic stability.
To the best of our knowledge, iPSCs in clinical trials mostly involve neurological and cardiovascular disease treatments (such as for Parkinson’s disease) via iPSC-derived HSCs and cardiac cell injury via iPSC-derived cardiomyocytes. Japan started the world’s first iPSC-based clinical study in 2013, whereby a macular degeneration patient received a transplant of iPSC-based retinal cells; however, the patient showed no improvement [107]. Another study at Kyoto University focused on dopaminergic precursor cells that were differentiated from iPSCs injected into the brain of a patient with Parkinson’s disease. This boosted the dopamine levels and improved the patient’s symptoms [108,109].
4.3. Site-Directed Integration
NILV is also used as a template for site-directed integration systems. A variety of systems are available for direct integration into genomic “safe sites” or for gene-specific correction to minimise the dysregulation of gene expression, as listed in Table 7. One approach involves combining a recombinase or transposase transiently with an NILV to facilitate integration at specific sites. The most recent example involved the use of the sleeping beauty (SB) transposon and transposase expression cassette. NILVs were able to facilitate transient transposase expression to the target cells. Several studies using NILVs have shown similar integration to the SB cassette without viral element integration, thereby reducing the insertional mutagenesis [110]. An HIV-1/SB hybrid vector facilitated by the hyperactive SB100X transposase that allows efficient DNA transposition in primary human cells could be a valuable tool for therapeutic gene transfer, as it could be inserted into actively transcribed genomic regions. Another study explained that non-viral yeast Flpx9 recombinase produced by NILV can enter the circular viral recombination substrates and facilitate the site-directed genomic insertion [111].

Table 7.
A summary of the elements used in developing non-integrating lentiviral vectors (NILVs) for site-directed integration in pre-clinical studies. Different approaches for direct integration or site-specific modifications of safe genomic loci in different studies are listed with attached references.
Moreover, NILVs can be designed to promote site-specific homologous recombination (HR). This includes NILVs combined with a rare cutting nuclease for targeted recombination at specific sites by HR. This will lead to successful targeted gene correction. For example, an NILV encoding a repair template was co-transported with an I-SceI nuclease expression vector to rescue a defective enhanced green fluorescent protein (EGFP) gene. Expression of the nuclease created a double-strand break (DSB) within the targeted locus and stimulated stable gene correction at the end of the process [21]. Adding to this, calmegin (clgn) targets the neomycin-resistant transgene cassette that generates ES cells via transgene insertion. However, this method is unbeatable against the traditional electroporation method, which allows for more efficient gene transfer [116]. Thus, better modifications and changes are the main concerns of many researchers. NILVs can also be used as templates for HR along with engineered zinc finger nucleases (ZFNs) [117,118] and transcription activator-like effector nucleases (TALENs) [115] to induce successful gene correction at the target gene locus with less off-target integration. Recently, the development of regularly clustered, interspaced, short palindromic repeat and CRISPR-associated protein 9 (CRISPR/Cas9) technology has made NILVs ideal tools. CRISPR/Cas9 and a guide RNA targeting the cytochrome b-245 heavy chain can correct the defects in hematopoietic cells [119]. Another study also utilised CRISPR/Cas9-mediated, homology-directed repair via an ex vivo approach to conduct gene correction for recessive dystrophic epidermolysis bullosa [120].
4.4. Gene Therapy
From our viewpoint, the use of NILVs in gene transfer or gene therapy is a promising strategy for delivering therapeutic genes for genetic diseases such as cancer, macular degenerations, heart disease, diabetes, haemophilia, AIDS, and most blood-related disorders that is equal to the use of LVs. The LV-based gene therapies known as Zynteglo [121] and Libmedly [122] have been announced as treatments for β-thalassemia and metachromatic leukodystrophy (MLD), respectively, by the European Medicines Agency (EMA). However, this may to indicate a certain level of uncertainty related to future products, which may further delay the success and approval of LV-based therapies. Therefore, NILVs as alternatives with proven success in gene therapy can also be approved to meet the ultimate goal of treating genetic disorders without detrimental risks. Researchers have been replacing mutated and defective genes and making diseased cells more evident to the immune system. Gene transfer is a challenging process, as poorly studied unsuccessful steps can lead to adverse immune system reactions, incorrect cell targeting, infections caused by the virus, and tumour growth. For example, SCID-X1 patients who received HSCs transduced with murine leukaemia virus (MLV) developed abnormal T cell proliferation due to the insertion of a retroviral vector near the LMO2 proto-oncogene [123,124]. In another study, a successful dopamine replacement gene therapy in patients with Parkinson’s disease performed by targeting important genes for dopamine synthesis regulated the dopamine concentration, proving that gene therapy can be successful [125]. Therefore, gene therapy involving NILVs also needs to be assessed in order to bring this method into clinical application, since it has been proven to be better and more successful than other gene delivery methods, as listed in Table 8.

Table 8.
Summary of integrase mutations with added elements used in developing non-integrating lentiviral vectors (NILVs) for gene therapy in pre-clinical studies with specifically targeted organs.
NILVs encoding for in vivo expression of GFP have been reported in organs such as the brain, liver, and spinal cord via stable gene transfer for longer periods (up to months) in several studies [22,73,131,132,133,134]. In another study, hepatocytes that target NILVs with coagulation factor IX (FIX) in haemophilic mice induced an immune tolerance [135]. A similar study using FIX transgenes carrying an R338L amino acid substitution associated with clotting hyperactivity and thrombophilia showed increased gene therapy efficacy but also less efficiency in hepatic transgene expression of NILVs [136]. Recently, another study demonstrated that the NILV approach can overcome immune rejection and allow for the growth of transduced cells in an immunocompetent host by producing CRISPR-modified murine cell lines using mutated integrase vectors [137]. In addition to the advantages of the CRISPR/Cas9 system, another study proved that a Cas9 protein delivery system with NILVs encoding both guide RNA and donor DNA resulted in efficient DNA breakage, one-time genome correction of the sickle cell disease (SCD) mutation, and long-term engraftment of HSCs [126]. These studies explained the use of combined NILV approaches for a safer, long-lasting, and fruitful outcome in future research. Gene therapy has been given more importance compared to other clinical applications in treating many genetic disorders that are highly disruptive to human health. The latest research has also demonstrated a successful combination gene therapy strategy for HIV using a two-vector system design, which uses an integrating LV to transduce the cells sequentially and a non-integrating lentiviral LV to insert the conditional suicide gene, with knockout of CCR5, and transient expression of GFP to enrich the modified cells [128].
5. Future Directions and Challenges
From the frame of reference of this review, the integration-free capability of NILV is highly desirable for gene therapy and could be the gold option for vaccination and cell immunisations studies with long-lasting immune responses. However, very limited or less studies have chosen NILVs as a gene delivery method to generate iPSCs, although this approach has potential. The earlier iPSC reprogramming work utilised the viral vector system to express the advantages of OKSM with a highly successful rate. This opened up new possibilities in regenerative medicine, especially for the development of disease-specific models, including in drug toxicity studies. However, this viral vector also causes multiple potentially harmful integrations of the transgenes into the host genome, which lead to tumour formation. Although non-viral methods such as protein transduction [138], MiRNA expression [60], and mini circle vector expression [48] have been introduced to eliminate this harmful effect, the efficiency of generating functional iPSCs using the viral system means it is still favoured. Therefore, the effort to refine and develop alternative approaches is being continued, including the use of non-integrating systems to deliver the reprogramming genes.
In addition, a study published a decade ago showed for the first time the successful reprogramming of blood cells using non-integrative SeV as an efficient integration-free gene delivery method [139]. The high reprogramming efficiency without genomic integration of the SeV vector was also demonstrated commercially [140]. Since iPSCs have not been generated using the NILV approach, the same concept can be expected to be applied using NILVs with a similar safety profile and with a slight possibility of transgene integration into the host in the future. This increases the hope of working more on NILVs by setting SeV vectors as an ideal example to generate successful high-clinical-grade iPSCs. In conclusion, research is still ongoing at every step of therapeutic application for NILVs in the hope of achieving better curative options in the future.
The major drawback of NILVs are their reduced transgene expression and gradual loss of episomal vectors, especially in dividing cells, which eventually reduce the therapeutic effect and mean it does not have long-lasting persistence. Some important improvements that can be further explored in NILV systems are the introduction of multiple mutation sites of the integrase sequence gene. This approach could help to increase the episomal gene expression, as reported in a previous study where different mutation sites of the integrase plasmid resulted in different gene expression levels [75]. Another suggestion is to use a different type of promoter to drive the expression of the pluripotent genes, as the current promoter, the CMV promoter, is likely to be highly methylated during prolonged expression and might not be suitable or efficient for episomal expression due to the high replication rate of the transduced cells [141,142]. Only targeted methylation-induced gene silencing could be reversed via the addition of 5-aza-2′-deoxycytidine. Alternatively, another option is to consider introducing a transduction domain at the 3′-5′ exonuclease of the transcription gene, which could boost and enhance the gene expression, thereby increasing the reprogramming efficiency using NILVs.
Additionally, as NILVs have been used as the best option for non-invasive gene-based imaging only in non-dividing cells [143], highly proliferating cells should be considered for use with this approach in the future by merging OriP plasmid technology from EBV into NILV episomes that can retain the plasmids. Apart from the SNIL vector, incorporating the simian virus 40 (SV40) into NILVs could maintain the episomal DNA in dividing cells. One concern in merging or modifying the original vector to fix these limitations is the abnormal mutations and infections, which could multiply the existing limitations. Thus, careful epigenetic studies and DNA methylation profiles are needed prior to successfully applying the NILV approach in clinical settings.
In a nutshell, NILVs have emerged as an important tool in biomedical research as a therapeutic option. Future studies are needed with more advanced human clinical trials to achieve improvements and for optimisation in order to increase the safety and reduce illegitimate integration. The application of NILVs in the pre-clinical trials of recombinant protein production, vaccines, gene therapy, cell imaging, and induced pluripotent stem cell (iPSC) generation should be explored further to bring about even more advancements in the future.
Author Contributions
N.G. and G.J.T. collected the data and conducted the literature review. F.N., M.H.N. and W.S.W.K.Z. contributed to the design and outline of the review and provided supporting data. N.G., F.N. and G.J.T. wrote this manuscript and were involved in the proofreading. All authors have read and agreed to the published version of the manuscript.
Funding
The study was supported by the Ministry of Higher Education Malaysia (MOHE) through the awarded grant FRGS/1/2020/SKK06/UKM/03/4 and Universiti Kebangsaan Malaysia through a Faculty of Medicine grant (FF-2020-327). This funding body accepted the study as proposed.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analysed in this study. Data sharing does not apply to this article.
Acknowledgments
We would like to thank the members of Centre for Tissue Engineering and Regenerative Medicine (CTERM), UKM Medical Centre (UKMMC), for their support and assistance. Additionally, we thank Universiti Kebangsaan Malaysia (UKM) for the support and approval to conduct this study (ethic approval code UKM PPI/111/8/JEP-2021-347).
Conflicts of Interest
The authors report no conflict of interest in this work.
References
- Delviks-Frankenberry, K.A.; Ackerman, D.; Timberlake, N.D.; Hamscher, M.; Nikolaitchik, O.A.; Hu, W.-S.; Torbett, B.E.; Pathak, V.K. Development of Lentiviral Vectors for HIV-1 Gene Therapy with Vif-Resistant APOBEC3G. Mol. Ther.-Nucleic Acids 2019, 18, 1023–1038. [Google Scholar] [CrossRef]
- Milone, M.C.; O’Doherty, U. Clinical use of lentiviral vectors. Leukemia 2018, 32, 1529–1541. [Google Scholar] [CrossRef] [PubMed]
- Gama-Norton, L.; Botezatu, L.; Herrmann, S.; Schweizer, M.; Alves, P.; Hauser, H.; Wirth, D. Lentivirus Production Is Influenced by SV40 Large T-Antigen and Chromosomal Integration of the Vector in HEK293 Cells. Hum. Gene Ther. 2011, 22, 1269–1279. [Google Scholar] [CrossRef] [PubMed]
- Merten, O.-W.; Hebben, M.; Bovolenta, C. Production of lentiviral vectors. Mol. Ther.-Methods Clin. Dev. 2016, 3, 16017. [Google Scholar] [CrossRef]
- Rothe, M.; Modlich, U.; Schambach, A. Biosafety challenges for use of lentiviral vectors in gene therapy. Curr. Gene Ther. 2014, 13, 453–468. [Google Scholar] [CrossRef] [PubMed]
- Schlimgen, R.; Howard, J.; Wooley, D.; Thompson, M.; Baden, L.R.; Yang, O.O.; Christiani, D.C.; Mostoslavsky, G.; Diamond, D.V.; Duane, E.G.; et al. Risks Associated with Lentiviral Vector Exposures and Prevention Strategies. J. Occup. Environ. Med. 2016, 58, 1159–1166. [Google Scholar] [CrossRef] [PubMed]
- Themis, M.; Waddington, S.N.; Schmidt, M.; von Kalle, C.; Wang, Y.; Al-Allaf, F.; Gregory, L.G.; Nivsarkar, M.; Themis, M.; Holder, M.V.; et al. Oncogenesis Following Delivery of a Nonprimate Lentiviral Gene Therapy Vector to Fetal and Neonatal Mice. Mol. Ther. 2005, 12, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Engelman, A.; Englund, G.; Orenstein, J.M.; Martin, A.M.; Craigie, R. Multiple effects of mutations in human immunodeficiency virus type 1 integrase on viral replication. J. Virol. 1995, 69, 2729–2736. [Google Scholar] [CrossRef]
- Shaw, A.; Cornetta, K. Design and potential of non-integrating lentiviral vectors. Biomedicines 2014, 2, 14–35. [Google Scholar] [CrossRef]
- Luis, A. The old and the new: Prospects for non-integrating lentiviral vector technology. Viruses 2020, 12, 1103. [Google Scholar]
- Nordin, F.; Hamid, Z.A.; Chan, L.; Farzaneh, F.; Hamid, M.K.A.A. Transient Expression of Green Fluorescent Protein in Integrase-Defective Lentiviral Vector-Transduced 293T Cell Line. In Methods in Molecular Biology; Humana Press: New York, NY, USA, 2016; Volume 1448, pp. 159–173. Available online: https://pubmed.ncbi.nlm.nih.gov/27317180/ (accessed on 19 February 2021).
- Zynteglo|European Medicines Agency. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/zynteglo#overview-section (accessed on 6 December 2021).
- Zufferey, R.; Dull, T.; Mandel, R.J.; Bukovsky, A.; Quiroz, D.; Naldini, L.; Trono, D. Self-Inactivating Lentivirus Vector for Safe and Efficient In Vivo Gene Delivery. J. Virol. 1998, 72, 9873–9880. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Wakefield, J.K.; Liu, H.; Xiao, H.; Kralovics, R.; Prchal, J.T.; Kappes, J.C. Development of a Novel Trans-Lentiviral Vector That Affords Predictable Safety. Mol. Ther. 2000, 2, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Dull, T.; Zufferey, R.; Kelly, M.; Mandel, R.J.; Nguyen, M.; Trono, D.; Naldini, L. A Third-Generation Lentivirus Vector with a Conditional Packaging System. J. Virol. 1998, 72, 8463–8471. [Google Scholar] [CrossRef] [PubMed]
- Cornetta, K.; Yao, J.; Jasti, A.; Koop, S.; Douglas, M.; Hsu, D.; Couture, A.L.; Hawkins, T.; Duffy, L. Replication-competent Lentivirus Analysis of Clinical Grade Vector Products. Mol. Ther. 2011, 19, 557–566. [Google Scholar] [CrossRef]
- Cornetta, K.; Duffy, L.; Turtle, C.J.; Jensen, M.; Forman, S.; Binder-Scholl, G.; Fry, T.; Chew, A.; Maloney, D.G.; June, C.H. Absence of Replication-Competent Lentivirus in the Clinic: Analysis of Infused T Cell Products. Mol. Ther. 2018, 26, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Craigie, R.; Fujiwara, T.; Bushman, F. The IN protein of Moloney murine leukemia virus processes the viral DNA ends and accomplishes their integration in vitro. Cell 1990, 62, 829–837. [Google Scholar] [CrossRef]
- Katz, R.A.; Merkel, G.; Kulkosky, J.; Leis, J.; Skalka, A.M. The avian retroviral IN protein is both necessary and sufficient for integrative recombination in vitro. Cell 1990, 63, 87–95. [Google Scholar] [CrossRef]
- Apolonia, L.; Waddington, S.; Fernandes, C.; Ward, N.J.; Bouma, G.; Blundell, M.; Thrasher, A.J.; Collins, M.K.; Philpott, N.J. Stable Gene Transfer to Muscle Using Non-integrating Lentiviral Vectors. Mol. Ther. 2007, 15, 1947–1954. [Google Scholar] [CrossRef] [PubMed]
- Cornu, I.; Cathomen, T. Targeted Genome Modifications Using Integrase-deficient Lentiviral Vectors. Mol. Ther. 2007, 15, 2107–2113. [Google Scholar] [CrossRef] [PubMed]
- Yáñez-Muñoz, R.J.; Balaggan, K.S.; MacNeil, A.; Howe, S.J.; Schmidt, M.; Smith, A.J.; Buch, P.; MacLaren, R.; Anderson, P.N.; Barker, E.S.; et al. Effective gene therapy with nonintegrating lentiviral vectors. Nat. Med. 2006, 12, 348–353. [Google Scholar] [CrossRef]
- Negri, D.; Michelini, Z.; Baroncelli, S.; Spada, M.; Vendetti, S.; Buffa, V.; Bona, R.; Leone, P.; Klotman, E.M.; Cara, A. Successful Immunization with a Single Injection of Non-integrating Lentiviral Vector. Mol. Ther. 2007, 15, 1716–1723. [Google Scholar] [CrossRef] [PubMed]
- Vargas, J., Jr.; Gusella, G.L.; Najfeld, V.; Klotman, M.E.; Cara, A. Novel Integrase-Defective Lentiviral Episomal Vectors for Gene Transfer. Hum. Gene Ther. 2004, 15, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Banasik, M.B.; McCray, P.B. Integrase-defective lentiviral vectors: Progress and applications. Gene Ther. 2010, 17, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Goubin, G.; Hill, M. Monomer and multimer covalently closed circular forms of Rous sarcoma virus DNA. J. Virol. 1979, 29, 799–804. [Google Scholar] [CrossRef]
- Engelman, A.; Craigie, R. Identification of conserved amino acid residues critical for human immunodeficiency virus type 1 integrase function in vitro. J. Virol. 1992, 66, 6361–6369. [Google Scholar] [CrossRef] [PubMed]
- Shibagaki, Y.H.; Chow, S.A. Central Core Domain of Retroviral Integrase Is Responsible for Target Site Selection. J. Biol. Chem. 1997, 272, 8361–8369. [Google Scholar] [CrossRef] [PubMed]
- Leavitt, A.D.; Robles, G.; Alesandro, N.; Varmus, E.H. Human immunodeficiency virus type 1 integrase mutants retain in vitro integrase activity yet fail to integrate viral DNA efficiently during infection. J. Virol. 1996, 70, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Nightingale, S.J.; Hollis, R.P.; Pepper, K.A.; Petersen, D.; Yu, X.J.; Yang, C.; Bahner, I.; Kohn, D.B. Transient Gene Expression by Nonintegrating Lentiviral Vectors. Mol. Ther. 2006, 13, 1121–1132. [Google Scholar] [CrossRef]
- Nishimura, K.; Sano, M.; Ohtaka, M.; Furuta, B.; Umemura, Y.; Nakajima, Y.; Ikehara, Y.; Kobayashi, T.; Segawa, H.; Takayasu, S.; et al. Development of Defective and Persistent Sendai Virus Vector: A Unique gene delivery/expression system ideal for cell reprogramming. J. Biol. Chem. 2011, 286, 4760. [Google Scholar] [CrossRef] [PubMed]
- Sano, M.; Nakasu, A.; Ohtaka, M.; Nakanishi, M. A Sendai Virus-Based Cytoplasmic RNA Vector as a Novel Platform for Long-Term Expression of MicroRNAs. Mol. Ther.-Methods Clin. Dev. 2019, 15, 371–382. [Google Scholar] [CrossRef]
- Seki, T.; Yuasa, S.; Fukuda, K. Generation of induced pluripotent stem cells from a small amount of human peripheral blood using a combination of activated T cells and Sendai virus. Nat. Protoc. 2012, 7, 718–728. [Google Scholar] [CrossRef] [PubMed]
- Yamaki, Y.; Fukushima, T.; Yoshida, N.; Nishimura, K.; Fukuda, A.; Hisatake, K.; Aso, M.; Sakasai, T.; Kijima-Tanaka, J.; Miwa, Y.; et al. Utilization of a novel Sendai virus vector in ex vivo gene therapy for hemophilia A. Int. J. Hematol. 2021, 113, 493–499. [Google Scholar] [CrossRef]
- Mardanova, E.S.; Blokhina, E.A.; Tsybalova, L.M.; Peyret, H.; Lomonossoff, G.P.; Ravin, N.V. Efficient Transient Expression of Recombinant Proteins in Plants by the Novel pEff Vector Based on the Genome of Potato Virus X. Front. Plant Sci. 2017, 8, 247. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.; Neises, A.; Su, R.-J.; Payne, K.; Ritter, L.; Gridley, D.S.; Wang, J.; Sheng, M.; Lau, K.-H.; Baylink, D.J.; et al. Efficient Reprogramming of Human Cord Blood CD34+ Cells into Induced Pluripotent Stem Cells with OCT4 and SOX2 Alone. Mol. Ther. 2012, 20, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Hoshikawa, K.; Ezura, K.; Okazawa, R.; Fujita, S.; Takaoka, M.; Mason, H.S.; Ezura, H.; Miura, K. Improvement of the transient expression system for production of recombinant proteins in plants. Sci. Rep. 2018, 8, 4755. [Google Scholar] [CrossRef] [PubMed]
- Chou, B.K.; Mali, P.; Huang, X.; Ye, Z.; Dowey, S.N.; Resar, L.M.; Zou, C.; Zhang, Y.A.; Tong, J.; Cheng, L. Efficient human iPS cell derivation by a non-integrating plasmid from blood cells with unique epigenetic and gene expression signatures. Cell Res. 2011, 21, 518–529. [Google Scholar] [CrossRef]
- Chen, G.; Gulbranson, D.R.; Hou, Z.; Bolin, J.M.; Ruotti, V.; Probasco, M.D.; Smuga-Otto, K.; Howden, S.E.; Diol, N.R.; Propson, N.E.; et al. Chemically defined conditions for human iPSC derivation and culture. Nat. Methods 2011, 8, 424–429. [Google Scholar] [CrossRef]
- Yu, J.; Chau, K.F.; Vodyanik, M.A.; Jiang, J.; Jiang, Y. Efficient Feeder-Free Episomal Reprogramming with Small Molecules. PLoS ONE 2011, 6, e17557. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Hu, K.; Smuga-Otto, K.; Tian, S.; Stewart, R.; Slukvin, I.I.; Thomson, J.A. Human induced pluripotent stem cells free of vector and transgene sequences. Science 2009, 324, 797–801. [Google Scholar] [CrossRef]
- Hu, K.; Yu, J.; Suknuntha, K.; Tian, S.; Montgomery, K.; Choi, K.D.; Stewart, R.; Thomson, J.A.; Slukvin, I.I. Efficient generation of transgene-free induced pluripotent stem cells from normal and neoplastic bone marrow and cord blood mononuclear cells. Blood 2011, 117, e109–e119. [Google Scholar] [CrossRef]
- Marchetto, M.C.N.; Yeo, G.W.; Kainohana, O.; Marsala, M.; Gage, F.H.; Muotri, A.R. Transcriptional Signature and Memory Retention of Human-Induced Pluripotent Stem Cells. PLoS ONE 2009, 4, e7076. [Google Scholar] [CrossRef] [PubMed]
- Sherpa, C.; Le Grice, S.F. Adeno-Associated Viral Vector Mediated Expression of Broadly-Neutralizing Antibodies against HIV-Hitting a Fast-Moving Target. Curr. HIV Res. 2020, 18, 114–131. [Google Scholar] [CrossRef]
- Slon-Campos, J.L.; Poggianella, M.; Zentilin, L.; Burrone, O.R. Use of Adeno-associated viral vectors to improve delivery of a DNA vaccine against dengue virus. J. Gen. Virol. 2020, 101, 73–78. [Google Scholar] [CrossRef]
- Senís, E.; Mosteiro, L.; Wilkening, S.; Wiedtke, E.; Nowrouzi, A.; Afzal, S.; Fronza, R.; Landerer, H.; Abad, M.; Niopek, D.; et al. AAV vector-mediated in vivo reprogramming into pluripotency. Nat. Commun. 2018, 9, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, Y.; Yoshii, T.; Iyori, M.; Yoshida, K.; Mizukami, H.; Fukumoto, S.; Yamamoto, D.S.; Alam, A.; Bin Emran, T.; Amelia, F.; et al. Adeno-Associated Virus as an Effective Malaria Booster Vaccine Following Adenovirus Priming. Front. Immunol. 2019, 10, 730. [Google Scholar] [CrossRef] [PubMed]
- Jia, F.; Wilson, K.D.; Sun, N.; Gupta, D.M.; Huang, M.; Li, Z.; Panetta, N.J.; Chen, Z.Y.; Robbins, R.C.; Kay, M.A.; et al. A nonviral minicircle vector for deriving human iPS cells. Nat. Methods 2010, 7, 197–199. [Google Scholar] [CrossRef] [PubMed]
- Gallego, I.; Villate-Beitia, I.; Martínez-Navarrete, G.; Menéndez, M.; López-Méndez, T.; Soto-Sánchez, C.; Zárate, J.; Puras, G.; Fernández, E.; Pedraz, J.L. Non-viral vectors based on cationic niosomes and minicircle DNA technology enhance gene delivery efficiency for biomedical applications in retinal disorders. Nanomed. Nanotechnol. Biol. Med. 2019, 17, 308–318. [Google Scholar] [CrossRef]
- Narsinh, K.H.; Jia, F.; Robbins, R.C.; Kay, M.A.; Longaker, M.T.; Wu, J.C. Generation of adult human induced pluripotent stem cells using nonviral minicircle DNA vectors. Nat. Protoc. 2011, 6, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Schleef, M.; Schirmbeck, R.; Reiser, M.; Michel, M.L.; Schmeer, M. Minicircle: Next Generation DNA Vectors for Vaccination. Methods Mol. Biol. 2015, 1317, 327–339. [Google Scholar] [PubMed]
- Monjezi, R.; Miskey, C.; Gogishvili, T.; Schleef, M.; Schmeer, M.; Einsele, H.; Ivics, Z.; Hudecek, M. Enhanced CAR T-cell engineering using non-viral Sleeping Beauty transposition from minicircle vectors. Leukemia 2017, 31, 186–194. [Google Scholar] [CrossRef]
- Gaspar, V.; Melo-Diogo, D.D.; Costa, E.; Moreira, A.; Queiroz, J.; Pichon, C.; Correia, I.; Sousa, F. Minicircle DNA vectors for gene therapy: Advances and applications. Expert Opin. Biol. Ther. 2015, 15, 353–379. [Google Scholar] [CrossRef] [PubMed]
- Rohani, L.; Fabian, C.; Holland, H.; Naaldijk, Y.; Dressel, R.; Löffler-Wirth, H.; Binder, H.; Arnold, A.; Stolzing, A. Generation of human induced pluripotent stem cells using non-synthetic mRNA. Stem Cell Res. 2016, 16, 662–672. [Google Scholar] [CrossRef] [PubMed]
- Warren, L.; Lin, C. mRNA-Based Genetic Reprogramming. Mol. Ther. J. Am. Soc. Gene Ther. 2019, 27, 729–734. [Google Scholar] [CrossRef]
- Oh, S.; Kessler, J.A. Design, Assembly, Production, and Transfection of Synthetic Modified mRNA. Methods 2018, 133, 29–43. [Google Scholar] [CrossRef] [PubMed]
- Yoshioka, N.; Gros, E.; Li, H.R.; Kumar, S.; Deacon, D.C.; Maron, C.; Muotri, A.R.; Chi, N.C.; Fu, X.-D.; Yu, B.D.; et al. Efficient Generation of Human iPS Cells by a Synthetic Self-Replicative RNA. Cell Stem Cell 2013, 13, 246–254. [Google Scholar] [CrossRef] [PubMed]
- Henry, J.C.; Azevedo-Pouly AC, P.; Schmittgen, T.D. MicroRNA replacement therapy for cancer. Pharm. Res. 2011, 28, 3030–3042. [Google Scholar] [CrossRef]
- Costard, L.S.; Kelly, D.C.; Power, R.N.; Hobbs, C.; Jaskaniec, S.; Nicolosi, V.; Cavanagh, B.L.; Curtin, C.M.; O’Brien, F. Layered Double Hydroxide as a Potent Non-viral Vector for Nucleic Acid Delivery Using Gene-Activated Scaffolds for Tissue Regeneration Applications. Pharmaceutics 2020, 12, 1219. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi, N.; Ishii, H.; Nagano, H.; Haraguchi, N.; Dewi, D.L.; Kano, Y.; Nishikawa, S.; Tanemura, M.; Mimori, K.; Tanaka, F.; et al. Reprogramming of mouse and human cells to pluripotency using mature microRNAs. Cell Stem Cell 2011, 8, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Bian, W.S.; Shi, P.X.; Mi, X.F.; Sun, Y.Y.; Yang, D.D.; Gao, B.F. MiR-210 protects cardiomyocytes from OGD/R injury by inhibiting E2F3. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 743–749. [Google Scholar] [PubMed]
- Khan, N.; Cheemadan, S.; Saxena, H.; Bammidi, S.; Jayandharan, G.R. MicroRNA-based recombinant AAV vector assembly improves efficiency of suicide gene transfer in a murine model of lymphoma. Cancer Med. 2020, 9, 3188–3201. [Google Scholar] [CrossRef] [PubMed]
- Fusaki, N.; Ban, H.; Nishiyama, A.; Saeki, K.; Hasegawa, M. Efficient induction of transgene-free human pluripotent stem cells using a vector based on Sendai virus, an RNA virus that does not integrate into the host genome. Proc. Jpn. Acad. Ser. B 2009, 85, 348–362. [Google Scholar] [CrossRef] [PubMed]
- Nakanishi, M.; Otsu, M. Development of Sendai Virus Vectors and their Potential Applications in Gene Therapy and Regenerative Medicine. Curr. Gene Ther. 2012, 12, 410. [Google Scholar] [CrossRef] [PubMed]
- Hung, S.C.; Kang, M.-S.; Kieff, E. Maintenance of Epstein–Barr virus (EBV) oriP-based episomes requires EBV-encoded nuclear antigen-1 chromosome-binding domains, which can be replaced by high-mobility group-I or histone H1. Proc. Natl. Acad. Sci. USA 2001, 98, 1865–1870. [Google Scholar] [CrossRef] [PubMed]
- Howard, D.; Powers, K.; Wang, Y.; Harvey, B.K. Tropism and toxicity of adeno-associated viral vector serotypes 1, 2, 5, 6, 7, 8, and 9 in rat neurons and glia in vitro. Virology 2008, 372, 24–34. [Google Scholar] [CrossRef]
- Karra, D.; Dahm, R. Transfection Techniques for Neuronal Cells. J. Neurosci. 2010, 30, 6171–6177. [Google Scholar] [CrossRef] [PubMed]
- Kiyosue, K.; Miwa, Y. Epstein-Barr virus-derived vector suitable for long-term expression in neurons. Heliyon 2020, 6, e03504. [Google Scholar] [CrossRef]
- Xu, Z.; Chen, F.; Zhang, L.; Lu, J.; Xu, P.; Liu, G.; Xie, X.; Mu, W.; Wang, Y.; Liu, D. Non-integrating lentiviral vectors based on the minimal S/MAR sequence retain transgene expression in dividing cells. Sci. China Life Sci. 2016, 59, 1024–1033. [Google Scholar] [CrossRef]
- Schambach, A.; Zychlinski, D.; Ehrnstroem, B.; Baum, C. Biosafety features of lentiviral vectors. Hum. Gene Ther. 2013, 24, 132–142. [Google Scholar] [CrossRef]
- Zhou, S.; Mody, D.; DeRavin, S.S.; Hauer, J.; Lu, T.; Ma, Z.; Abina, S.H.-B.; Gray, J.T.; Greene, M.R.; Cavazzana-Calvo, M.; et al. A self-inactivating lentiviral vector for SCID-X1 gene therapy that does not activate LMO2 expression in human T cells. Blood 2010, 116, 900–908. [Google Scholar] [CrossRef] [PubMed]
- Zychlinski, D.; Schambach, A.; Modlich, U.; Maetzig, T.; Meyer, J.; Grassman, E.; Mishra, A.; Baum, C. Physiological promoters reduce the genotoxic risk of integrating gene vectors. Mol. Ther. 2008, 16, 718–725. [Google Scholar] [CrossRef]
- Bayer, M.; Kantor, B.; Cockrell, A.; Ma, H.; Zeithaml, B.; Li, X.; McCown, T.; Kafri, T. A Large U3 Deletion Causes Increased In Vivo Expression from a Nonintegrating Lentiviral Vector. Mol. Ther. 2008, 16, 1968–1976. [Google Scholar] [CrossRef]
- Poon, B.; Chen, I.S.Y. Human Immunodeficiency Virus Type 1 (HIV-1) Vpr Enhances Expression from Unintegrated HIV-1 DNA. J. Virol. 2003, 77, 3962–3972. [Google Scholar] [CrossRef]
- Wanisch, K.; Yáñez-Muñoz, R.J. Integration-deficient Lentiviral Vectors: A Slow Coming of Age. Mol. Ther. 2009, 17, 1316–1332. [Google Scholar] [CrossRef] [PubMed]
- Ranzani, M.; Annunziato, S.; Calabria, A.; Brasca, S.; Benedicenti, F.; Gallina, P.; Naldini, L.; Montini, E. Lentiviral Vector-based Insertional Mutagenesis Identifies Genes Involved in the Resistance to Targeted Anticancer Therapies. Mol. Ther. 2014, 22, 2056–2068. [Google Scholar] [CrossRef] [PubMed]
- Bokhoven, M.; Stephen, S.L.; Knight, S.; Gevers, E.F.; Robinson, I.C.; Takeuchi, Y.; Collins, M.K. Insertional Gene Activation by Lentiviral and Gammaretroviral Vectors. J. Virol. 2009, 83, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Coutant, F.; Frenkiel, M.-P.; Despres, P.; Charneau, P. Protective Antiviral Immunity Conferred by a Nonintegrative Lentiviral Vector-Based Vaccine. PLoS ONE 2008, 3, e3973. [Google Scholar] [CrossRef]
- Coutant, F.; Sanchez David, R.Y.; Félix, T.; Boulay, A.; Caleechurn, L.; Souque, P.; Thouvenot, C.; Bourgouin, C.; Beignon, A.-S.; Charneau, P. A Nonintegrative Lentiviral Vector-Based Vaccine Provides Long-Term Sterile Protection against Malaria. PLoS ONE 2012, 7, e48644. [Google Scholar] [CrossRef]
- Michelini, Z.; Minkoff, J.; Yang, J.; Negri, D.; Cara, A.; Hanson, B.; Salvatore, M. Integrase-Defective Lentiviral Vectors for Delivery of Monoclonal Antibodies against Influenza. Viruses 2020, 12, 1460. [Google Scholar] [CrossRef]
- Odegard, J.M.; Kelley-Clarke, B.; Tareen, S.U.; Campbell, D.J.; Flynn, P.A.; Nicolai, C.J.; Slough, M.M.; Vin, C.D.; McGowan, P.J.; Nelson, L.T.; et al. Virological and Preclinical Characterization of a Dendritic Cell Targeting, Integration-deficient Lentiviral Vector for Cancer Immunotherapy. J. Immunother. 2015, 38, 41–53. [Google Scholar] [CrossRef]
- Ku, M.W.; Anna, F.; Souque, P.; Petres, S.; Prot, M.; Simon-Loriere, E.; Charneau, P.; Bourgine, M. A Single Dose of NILV-Based Vaccine Provides Rapid and Durable Protection against Zika Virus. Mol. Ther. 2020, 28, 1772–1782. [Google Scholar] [CrossRef]
- Deng, Y.; Guan, J.; Wen, B.; Zhu, N.; Chen, H.; Song, J.; Yang, Y.; Wang, Y.; Tan, W. Induction of Broadly Neutralising HCV Antibodies in Mice by Integration-Deficient Lentiviral Vector-Based Pseudotyped Particles. PLoS ONE 2013, 8, e62684. [Google Scholar] [CrossRef]
- Gallinaro, A.; Borghi, M.; Bona, R.; Grasso, F.; Calzoletti, L.; Palladino, L.; Cecchetti, S.; Vescio, M.F.; Macchia, D.; Morante, V.; et al. Integrase Defective Lentiviral Vector as a Vaccine Platform for Delivering Influenza Antigens. Front. Immunol. 2018, 9, 171. [Google Scholar] [CrossRef] [PubMed]
- Ku, M.W.; Bourgine, M.; Authié, P.; Lopez, J.; Nemirov, K.; Moncoq, F.; Noirat, A.; Vesin, B.; Nevo, F.; Blanc, C.; et al. Intranasal vaccination with a lentiviral vector protects against SARS-CoV-2 in preclinical animal models. Cell Host Microbe 2021, 29, 236–249.e6. [Google Scholar] [CrossRef]
- LeLeux, J.A.; Albershardt, T.C.; Parsons, A.J.; Ter Meulen, J.; Berglund, P. ZVex™, a dendritic-cell-tropic lentivector, primes protective antitumor T cell responses that are significantly boosted using heterologous vaccine modalities. Vaccine 2020, 38, 6367–6373. [Google Scholar] [CrossRef]
- Hu, B.; Dai, B.; Wang, P. Vaccines delivered by integration-deficient lentiviral vectors targeting dendritic cells induces strong antigen-specific immunity. Vaccine 2010, 28, 6675–6683. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gallinaro, A.; Borghi, M.; Pirillo, M.F.; Cecchetti, S.; Bona, R.; Canitano, A.; Michelini, Z.; Di Virgilio, A.; Olvera, A.; Brander, C.; et al. Development and Preclinical Evaluation of an Integrase Defective Lentiviral Vector Vaccine Expressing the HIVACAT T Cell Immunogen in Mice. Mol. Ther.-Methods Clin. Dev. 2020, 17, 418–428. [Google Scholar] [CrossRef]
- Michelini, Z.; Negri, D.R.; Baroncelli, S.; Spada, M.; Leone, P.; Bona, R.; Klotman, M.E.; Cara, A. Development and use of SIV-based Integrase defective lentiviral vector for immunization. Vaccine 2009, 27, 4622–4629. [Google Scholar] [CrossRef]
- Karwacz, K.; Mukherjee, S.; Apolonia, L.; Blundell, M.; Bouma, G.; Escors, D.; Collins, M.K.; Thrasher, A.J. Nonintegrating Lentivector Vaccines Stimulate Prolonged T-Cell and Antibody Responses and Are Effective in Tumor Therapy. J. Virol. 2009, 83, 3094–3103. [Google Scholar] [CrossRef] [PubMed]
- Albershardt, T.C.; Campbell, D.J.; Parsons, A.J.; Slough, M.M.; ter Meulen, J.; Berglund, P. LV305, a dendritic cell-targeting integration-deficient ZVex TM -based lentiviral vector encoding NY-ESO-1, induces potent anti-tumor immune response. Mol. Ther.-Oncolytics 2016, 3, 16010. [Google Scholar] [CrossRef]
- Pollack, S.M. The potential of the CMB305 vaccine regimen to target NY-ESO-1 and improve outcomes for synovial sarcoma and myxoid/round cell liposarcoma patients. Expert Rev. Vaccines 2018, 17, 107–114. [Google Scholar] [CrossRef]
- Yang, G.; Si-Tayeb, K.; Corbineau, S.; Vernet, R.; Gayon, R.; Dianat, N.; Martinet, C.; Clay, D.; Goulinet-Mainot, S.; Tachdjian, G.; et al. Integration-deficient lentivectors: An effective strategy to purify and differentiate human embryonic stem cell-derived hepatic progenitors. BMC Biol. 2013, 11, 86. [Google Scholar] [CrossRef]
- Papapetrou, E.P.; Sadelain, M. Generation of transgene-free human induced pluripotent stem cells with an excisable single polycistronic vector. Nat. Protoc. 2011, 6, 1251–1273. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Vodyanik, M.A.; Smuga-Otto, K.; Antosiewicz-Bourget, J.; Frane, J.L.; Tian, S.; Nie, J.; Jonsdottir, G.A.; Ruotti, V.; Stewart, R.; et al. Induced pluripotent stem cell lines derived from human somatic cells. Science 2007, 318, 1917–1920. [Google Scholar] [CrossRef] [PubMed]
- Papapetrou, E.P.; Tomishima, M.J.; Chambers, S.M.; Mica, Y.; Reed, E.; Menon, J.; Tabar, V.; Mo, Q.; Studer, L.; Sadelain, M. Stoichiometric and temporal requirements of Oct4, Sox2, Klf4, and c-Myc expression for efficient human iPSC induction and differentiation. Proc. Natl. Acad. Sci. USA 2009, 106, 12759–12764. [Google Scholar] [CrossRef]
- Takahashi, K.; Yamanaka, S. Induction of Pluripotent Stem Cells from Mouse Embryonic and Adult Fibroblast Cultures by Defined Factors. Cell 2006, 126, 663–676. [Google Scholar] [CrossRef] [PubMed]
- Kiskinis, E.; Eggan, K. Progress toward the clinical application of patient-specific pluripotent stem cells. J. Clin. Investig. 2010, 120, 51–59. [Google Scholar] [CrossRef]
- Saha, K.; Jaenisch, R. Technical Challenges in Using Human Induced Pluripotent Stem Cells to Model Disease. Cell Stem Cell 2009, 5, 584–595. [Google Scholar] [CrossRef]
- Hu, K. All Roads Lead to Induced Pluripotent Stem Cells: The Technologies of iPSC Generation. Stem Cells Dev. 2014, 23, 1285–1300. [Google Scholar] [CrossRef]
- Sommer, C.A.; Stadtfeld, M.; Murphy, G.J.; Hochedlinger, K.; Kotton, D.N.; Mostoslavsky, G. Induced Pluripotent Stem Cell Generation Using a Single Lentiviral Stem Cell Cassette. Stem Cells 2009, 27, 543–549. [Google Scholar] [CrossRef]
- Awe, J.P.; Lee, P.C.; Ramathal, C.; Vega-Crespo, A.; Durruthy-Durruthy, J.; Cooper, A.; Karumbayaram, S.; Lowry, E.W.; Clark, A.T.; Zack, A.J.; et al. Generation and characterization of transgene-free human induced pluripotent stem cells and conversion to putative clinical-grade status. Stem Cell Res. Ther. 2013, 4, 87. [Google Scholar] [CrossRef]
- Kaji, K.; Norrby, K.; Paca, A.; Mileikovsky, M.; Mohseni, P.; Woltjen, K. Virus-free induction of pluripotency and subsequent excision of reprogramming factors. Nature 2009, 458, 771–775. [Google Scholar] [CrossRef]
- Mali, P.; Ye, Z.; Hommond, H.H.; Yu, X.; Lin, J.; Chen, G.; Zou, J.; Cheng, L. Improved Efficiency and Pace of Generating Induced Pluripotent Stem Cells from Human Adult and Fetal Fibroblasts. Stem Cells 2008, 26, 1998–2005. [Google Scholar] [CrossRef] [PubMed]
- Sultanov, R.; Lebedeva, O.; Arapidi, G.; Lagarkova, M.; Kiselev, S. Methylation profile of induced pluripotent stem cells generated by integration and integration-free approaches. Data Brief 2018, 17, 662–666. [Google Scholar] [CrossRef]
- Lian, Q.; Chow, Y.; Esteban, M.A.; Pei, D.; Tse, H.-F. Future perspective of induced pluripotent stem cells for diagnosis, drug screening and treatment of human diseases. Thromb. Haemost. 2010, 104, 39–44. [Google Scholar] [CrossRef]
- Cyranoski, D. Japanese man is first to receive ‘reprogrammed’ stem cells from another person. Nat. Cell Biol. 2017. [Google Scholar] [CrossRef]
- Takahashi, J. iPS cell-based therapy for Parkinson’s disease: A Kyoto trial. Regen. Ther. 2020, 13, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Schweitzer, J.S.; Song, B.; Herrington, T.M.; Park, T.-Y.; Lee, N.; Ko, S.; Jeon, J.; Cha, Y.; Kim, K.; Li, Q.; et al. Personalized iPSC-Derived Dopamine Progenitor Cells for Parkinson’s Disease. N. Engl. J. Med. 2020, 382, 1926–1932. [Google Scholar] [CrossRef] [PubMed]
- Staunstrup, N.; Moldt, B.; Mátés, L.; Villesen, P.; Jakobsen, M.; Ivics, Z.; Izsvák, Z.; Mikkelsen, J.G. Hybrid Lentivirus-transposon Vectors with a Random Integration Profile in Human Cells. Mol. Ther. 2009, 17, 1205–1214. [Google Scholar] [CrossRef]
- Moldt, B.; Staunstrup, N.H.; Jakobsen, M.; Yáñez-Muñoz, R.J.; Mikkelsen, J.G. Genomic insertion of lentiviral DNA circles directed by the yeast Flp recombinase. BMC Biotechnol. 2008, 8, 60. [Google Scholar] [CrossRef]
- Shariati, L.; Modarressi, M.H.; Tabatabaiefar, M.A.; Kouhpayeh, S.; Hejazi, Z.; Shahbazi, M.; Sabzehei, F.; Salehi, M.; Khanahmad, H. Engineered zinc-finger nuclease to generate site-directed modification in the KLF1 gene for fetal hemoglobin induction. J. Cell. Biochem. 2019, 120, 8438–8446. [Google Scholar] [CrossRef]
- Sadeghi, M.M.; Shariati, L.; Hejazi, Z.; Shahbazi, M.; Tabatabaiefar, M.A.; Khanahmad, H. Inducing indel mutation in the SOX6 gene by zinc finger nuclease for gamma reactivation: An approach towards gene therapy of beta thalassemia. J. Cell. Biochem. 2018, 119, 2512–2519. [Google Scholar] [CrossRef]
- Rio, P.; Baños, R.; Lombardo, A.L.; Quintana-Bustamante, O.; Alvarez, L.; Garate, Z.; Genovese, P.; Almarza, E.; Valeri, A.; Díez, B.; et al. Targeted gene therapy and cell reprogramming in F anconi anemia. EMBO Mol. Med. 2014, 6, 835–848. [Google Scholar] [CrossRef]
- Osborn, M.J.; Starker, C.; McElroy, A.N.; Webber, B.R.; Riddle, M.J.; Xia, L.; DeFeo, A.P.; Gabriel, R.; Schmidt, M.; Von Kalle, C.; et al. TALEN-based Gene Correction for Epidermolysis Bullosa. Mol. Ther. 2013, 21, 1151–1159. [Google Scholar] [CrossRef]
- Okada, Y.; Ueshin, Y.; Hasuwa, H.; Takumi, K.; Okabe, M.; Ikawa, M. Targeted gene modification in mouse ES cells using integrase-defective lentiviral vectors. Genesis 2009, 47, 217–223. [Google Scholar] [CrossRef]
- Joglekar, A.V.; Hollis, R.P.; Kuftinec, G.; Senadheera, S.; Chan, R.; Kohn, D.B. Integrase-defective lentiviral vectors as a delivery platform for targeted modification of adenosine deaminase locus. Mol. Ther. 2013, 21, 1705–1717. [Google Scholar] [CrossRef]
- Lombardo, A.; Genovese, P.; Beausejour, C.M.; Colleoni, S.; Lee, Y.L.; Kim, K.A.; Ando, D.; Urnov, F.D.; Galli, C.; Gregory, P.D.; et al. Gene editing in human stem cells using zinc finger nucleases and integrase-defective lentiviral vector delivery. Nat. Biotechnol. 2007, 25, 1298–1306. [Google Scholar] [CrossRef]
- Sürün, D.; Schwäble, J.; Tomasovic, A.; Ehling, R.; Stein, S.; Kurrle, N.; von Melchner, H.; Schnütgen, F. High Efficiency Gene Correction in Hematopoietic Cells by Donor-Template-Free CRISPR/Cas9 Genome Editing. Mol. Ther.-Nucleic Acids 2018, 10, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Izmiryan, A.; Ganier, C.; Bovolenta, M.; Schmitt, A.; Mavilio, F.; Hovnanian, A. Ex Vivo COL7A1 Correction for Recessive Dystrophic Epidermolysis Bullosa Using CRISPR/Cas9 and Homology-Directed Repair. Mol. Ther.-Nucleic Acids 2018, 12, 554–567. [Google Scholar] [CrossRef] [PubMed]
- Schuessler-Lenz, M.; Enzmann, H.; Vamvakas, S. Regulators’ Advice Can Make a Difference: European Medicines Agency Approval of Zynteglo for Beta Thalassemia. Clin. Pharmacol. Ther. 2020, 107, 492–494. [Google Scholar] [CrossRef] [PubMed]
- Aiuti, A.; Roncarolo, M.G.; Naldini, L. Gene therapy for ADA-SCID, the first marketing approval of an ex vivo gene therapy in Europe: Paving the road for the next generation of advanced therapy medicinal products. EMBO Mol. Med. 2017, 9, 737–740. [Google Scholar] [CrossRef] [PubMed]
- Hacein-Bey-Abina, S.; Von Kalle, C.; Schmidt, M.; McCormack, M.P.; Wulffraat, N.; Leboulch, P.; Lim, A.; Osborne, C.S.; Pawliuk, R.; Morillon, E.; et al. LMO2-Associated Clonal T Cell Proliferation in Two Patients after Gene Therapy for SCID-X1. Science 2003, 302, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Hacein-Bey-Abina, S.; Garrigue, A.; Wang, G.P.; Soulier, J.; Lim, A.; Morillon, E.; Clappier, E.; Caccavelli, L.; Delabesse, E.; Beldjord, K.; et al. Insertional oncogenesis in 4 patients after retrovirus-mediated gene therapy of SCID-X1. J. Clin. Investig. 2008, 118, 3132–3142. [Google Scholar] [CrossRef]
- Jarraya, B.; Boulet, S.; Ralph, G.S.; Jan, C.; Bonvento, G.; Azzouz, M.; Miskin, J.E.; Shin, M.; Delzescaux, T.; Drouot, X.; et al. Dopamine Gene Therapy for Parkinson’s Disease in a Nonhuman Primate Without Associated Dyskinesia. Sci. Transl. Med. 2009, 1, 2ra4. [Google Scholar] [CrossRef] [PubMed]
- Uchida, N.; Drysdale, C.M.; Nassehi, T.; Gamer, J.; Yapundich, M.; DiNicola, J.; Shibata, Y.; Hinds, M.; Gudmundsdottir, B.; Haro-Mora, J.J.; et al. Cas9 protein delivery non-integrating lentiviral vectors for gene correction in sickle cell disease. Mol. Ther.-Methods Clin. Dev. 2021, 21, 121–132. [Google Scholar] [CrossRef]
- Chen, F.; Qi, X.; Zhang, R.; Wu, Z.-Y.; Yan, C.-E.; Li, J.; Liu, Q.-Y.; Qi, J. Episomal lentiviral vectors confer erythropoietin expression in dividing cells. Plasmid 2017, 90, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Mehmetoglu-Gurbuz, T.; Yeh, R.; Garg, H.; Joshi, A. Combination gene therapy for HIV using a conditional suicidal gene with CCR5 knockout. Virol. J. 2021, 18, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Piras, F.; Riba, M.; Petrillo, C.; Lazarevič, D.; Cuccovillo, I.; Bartolaccini, S.; Stupka, E.; Gentner, B.; Cittaro, D.; Naldini, L.; et al. Lentiviral vectors escape innate sensing but trigger p53 in human hematopoietic stem and progenitor cells. EMBO Mol. Med. 2017, 9, 1198–1211. [Google Scholar] [CrossRef]
- Kampik, D.; Basche, M.; Luhmann, O.U.F.; Nishiguchi, K.M.; Williams, A.E.J.; Greenwood, J.; Moss, E.S.; Han, H.; Azam, S.; Duran, Y.; et al. In situ regeneration of retinal pigment epithelium by gene transfer of E2F2: A potential strategy for treatment of macular degenerations. Gene Ther. 2017, 24, 810–818. [Google Scholar] [CrossRef]
- Kantor, B.; Bayer, M.; Ma, H.; Samulski, J.; Li, C.; McCown, T.; Kafri, T. Notable Reduction in Illegitimate Integration Mediated by a PPT-deleted, Nonintegrating Lentiviral Vector. Mol. Ther. 2011, 19, 547–556. [Google Scholar] [CrossRef]
- Peluffo, H.; Foster, E.; Ahmed, S.G.; Lago, N.; Hutson, T.H.; Moon, L.; Yip, P.; Wanisch, K.; Caraballo-Miralles, V.; Olmos, G.; et al. Efficient gene expression from integration-deficient lentiviral vectors in the spinal cord. Gene Ther. 2012, 20, 645–657. [Google Scholar] [CrossRef]
- Philippe, S.; Sarkis, C.; Barkats, M.; Mammeri, H.; Ladroue, C.; Petit, C.; Mallet, J.; Serguera, C. Lentiviral vectors with a defective integrase allow efficient and sustained transgene expression in vitro and in vivo. Proc. Natl. Acad. Sci. USA 2006, 103, 17684–17689. [Google Scholar] [CrossRef] [PubMed]
- Rahim, A.A.; Wong, A.M.S.; Howe, S.J.; Buckley, S.M.K.; Acosta-Saltos, A.D.; Elston, E.K.; Ward, N.J.; Philpott, N.J.; Cooper, J.; Anderson, P.N.; et al. Efficient gene delivery to the adult and fetal CNS using pseudotyped non-integrating lentiviral vectors. Gene Ther. 2009, 16, 509–520. [Google Scholar] [CrossRef]
- Mátrai, J.; Cantore, A.; Bartholomae, C.C.; Annoni, A.; Wang, W.; Acosta-Sanchez, A.; Samara-Kuko, E.; De Waele, L.; Ma, L.; Genovese, P.; et al. Hepatocyte-targeted expression by integrase-defective lentiviral vectors induces antigen-specific tolerance in mice with low genotoxic risk. Hepatology 2011, 53, 1696–1707. [Google Scholar] [CrossRef] [PubMed]
- Cantore, A.; Nair, N.; Della Valle, P.; Di Matteo, M.; Màtrai, J.; Sanvito, F.; Brombin, C.; Di Serio, C.; D’Angelo, A.; Chuah, M.; et al. Hyperfunctional coagulation factor IX improves the efficacy of gene therapy in hemophilic mice. Blood 2012, 120, 4517–4520. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Schokrpur, S.; Archang, M.; Hermann, K.; Sharrow, A.C.; Khanna, P.; Novak, J.; Signoretti, S.; Bhatt, R.S.; Knudsen, B.S.; et al. A Non-integrating Lentiviral Approach Overcomes Cas9-Induced Immune Rejection to Establish an Immunocompetent Metastatic Renal Cancer Model. Mol. Ther.-Methods Clin. Dev. 2018, 9, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Kim, C.H.; Moon, J.I.; Chung, Y.G.; Chang, M.Y.; Han, B.S.; Ko, S.; Yang, E.; Cha, K.Y.; Lanza, R.; et al. Generation of human induced pluripotent stem cells by direct delivery of reprogramming proteins. Cell Stem Cell 2009, 4, 472–476. [Google Scholar] [CrossRef]
- Seki, T.; Yuasa, S.; Oda, M.; Egashira, T.; Yae, K.; Kusumoto, D.; Nakata, H.; Tohyama, S.; Hashimoto, H.; Kodaira, M.; et al. Generation of induced pluripotent stem cells from human terminally differentiated circulating T cells. Cell Stem Cell 2010, 7, 11–14. [Google Scholar] [CrossRef]
- Bhutani, K.; Nazor, K.L.; Williams, R.; Tran, H.; Dai, H.; Džakula, Ž.; Cho, E.; Pang, A.W.C.; Rao, M.; Cao, H.; et al. Whole-genome mutational burden analysis of three pluripotency induction methods. Nat. Commun. 2016, 7, 10536. [Google Scholar] [CrossRef]
- Hsu, C.C.; Li, H.P.; Hung, Y.H.; Leu, Y.W.; Wu, W.H.; Wang, F.S.; Lee, K.-D.; Chang, P.-J.; Wu, C.-S.; Lu, Y.-J.; et al. Targeted methylation of CMV and E1A viral promoters. Biochem. Biophys. Res. Commun. 2010, 402, 228–234. [Google Scholar] [CrossRef] [PubMed]
- Osterlehner, A.; Simmeth, S.; Göpfert, U. Promoter methylation and transgene copy numbers predict unstable protein production in recombinant Chinese hamster ovary cell lines. Biotechnol. Bioeng. 2011, 108, 2670–2681. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, A.M.; Foster, P.J.; Ronald, J. Evaluating Nonintegrating Lentiviruses as Safe Vectors for Noninvasive Reporter-Based Molecular Imaging of Multipotent Mesenchymal Stem Cells. Hum. Gene Ther. 2018, 29, 1213–1225. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).