Macrophage Migration Inhibitory Factor—An Innovative Indicator for Free Flap Ischemia after Microsurgical Reconstruction
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Methods
2.3. Statistics
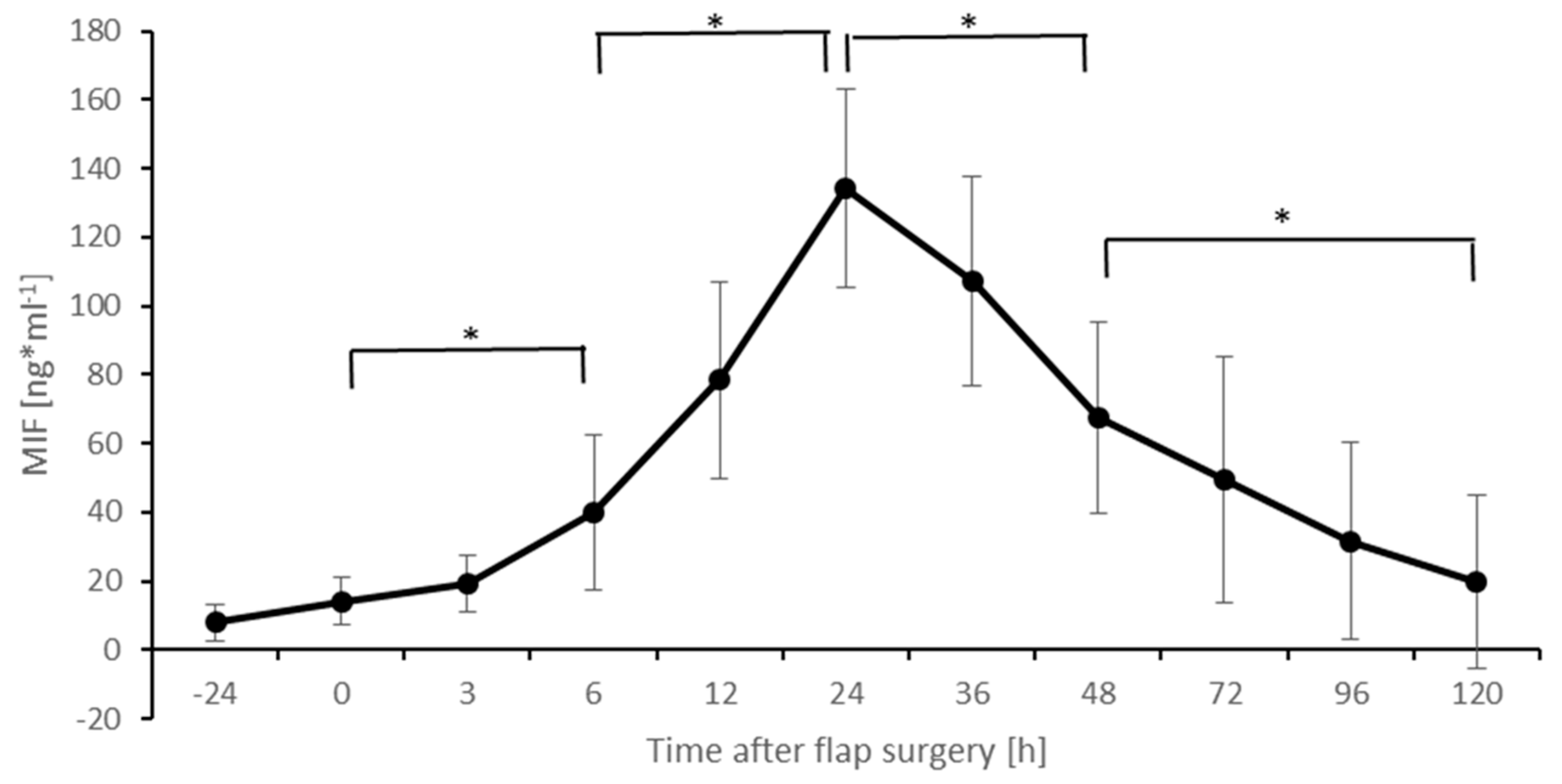
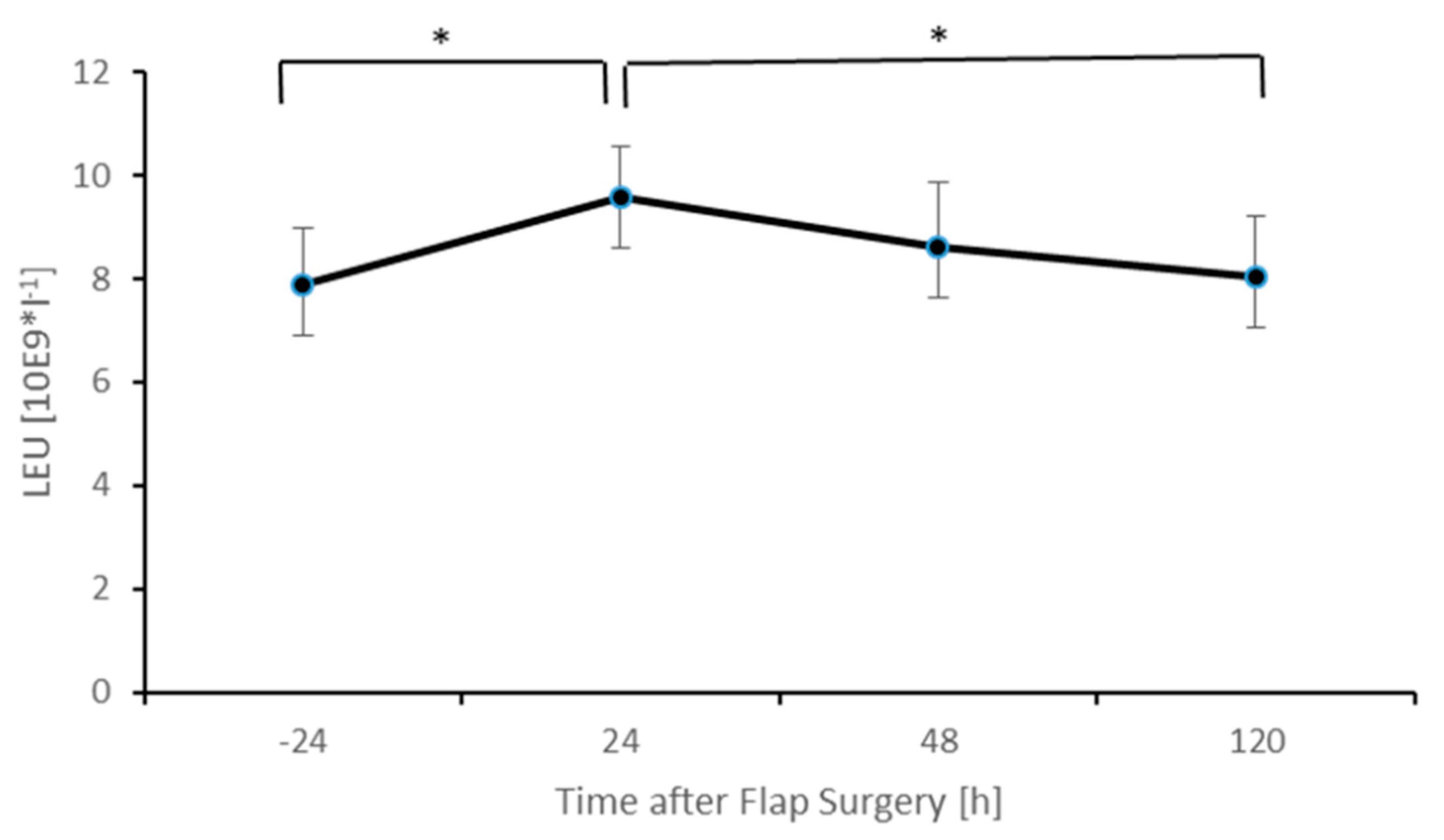
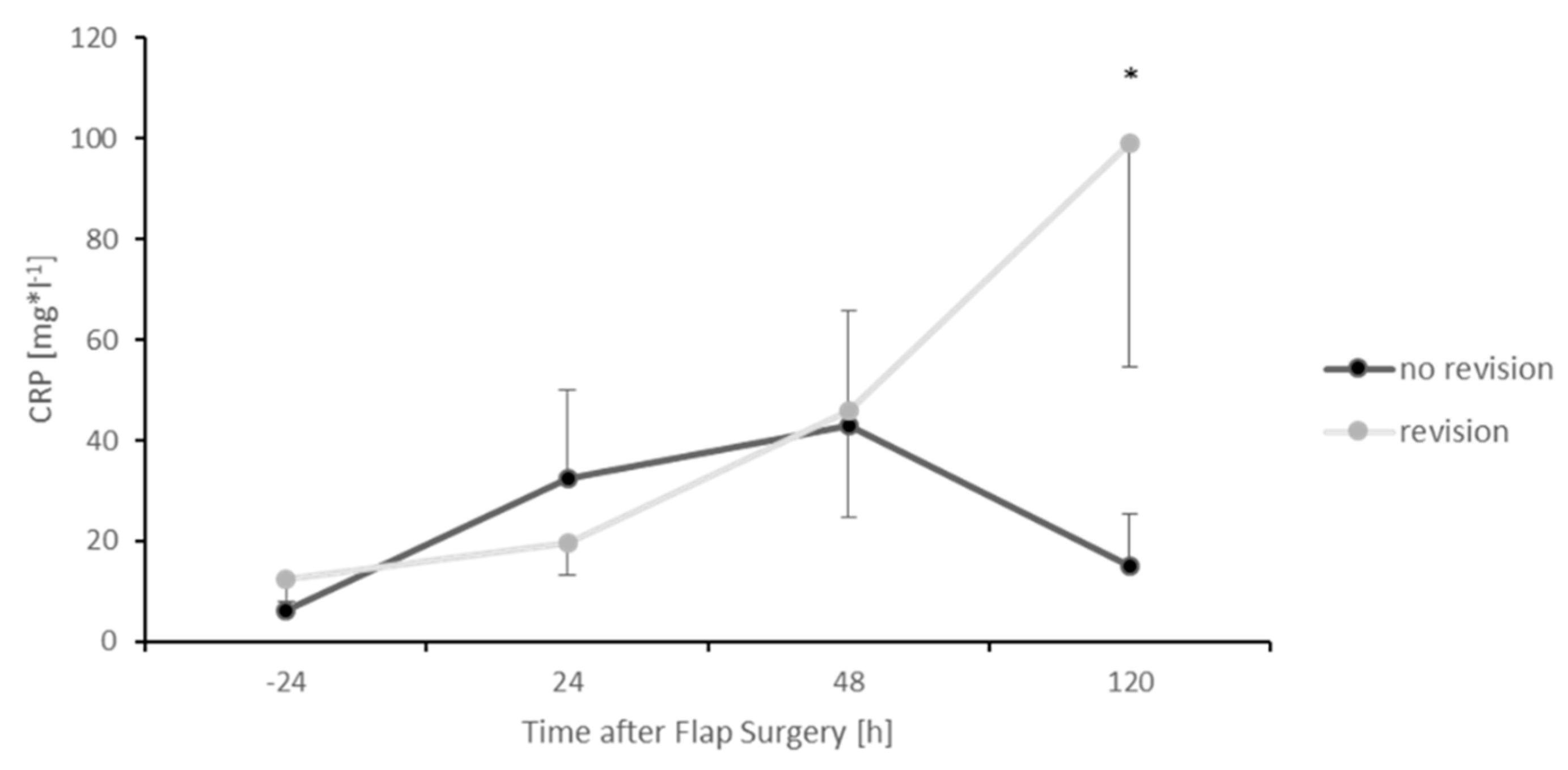
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Whitaker, I.S.; Rozen, W.M.; Chubb, D.; Acosta, R.; Kiil, B.J.; Birke-Sorensen, H.; Grinsell, D.; Ashton, M.W. Postoperative moni-toring of free flaps in autologous breast reconstruction: A multicenter comparison of 398 flaps using clinical monitoring, mi-crodialysis, and the implantable Doppler probe. J. Reconstr. Microsurg. 2010, 26, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Calandra, T.; Roger, T. Macrophage migration inhibitory factor: A regulator of innate immunity. Nat. Rev. Immunol. 2003, 3, 791–800. [Google Scholar] [CrossRef]
- Kang, I.; Bucala, R. The immunobiology of MIF: Function, genetics and prospects for precision medicine. Nat. Rev. Rheumatol. 2019, 15, 427–437. [Google Scholar] [CrossRef] [PubMed]
- Kapurniotu, A.; Gokce, O.; Bernhagen, J. The Multitasking Potential of Alarmins and Atypical Chemokines. Front. Med. 2019, 6, 3. [Google Scholar] [CrossRef] [PubMed]
- Bernhagen, J.; Krohn, R.; Lue, H.; Gregory, J.L.; Zernecke, A.; Koenen, R.R.; Dewor, M.; Georgiev, I.; Schober, A.; Leng, L.; et al. MIF is a noncognate ligand of CXC chemokine receptors in inflammatory and atherogenic cell recruitment. Nat. Med. 2007, 13, 587–596. [Google Scholar] [CrossRef]
- Weber, C.; Kraemer, S.; Drechsler, M.; Lue, H.; Koenen, R.R.; Kapurniotu, A.; Zernecke, A.; Bernhagen, J. Structural determi-nants of MIF functions in CXCR2-mediated inflammatory and atherogenic leukocyte recruitment. Proc. Natl. Acad. Sci. USA 2008, 105, 16278–16283. [Google Scholar] [CrossRef]
- Burger-Kentischer, A.; Goebel, H.; Seiler, R.; Fraedrich, G.; Schaefer, H.E.; Dimmeler, S.; Kleemann, R.; Bernhagen, J.; Ihling, C. Expression of Macrophage Migration Inhibitory Factor in Different Stages of Human Atherosclerosis. Circulation 2002, 105, 1561–1566. [Google Scholar] [CrossRef]
- Grieb, G.; Piątkowski, A.; Simons, D.; Hörmann, N.; Dewor, M.; Steffens, G.; Bernhagen, J.; Pallua, N. Macrophage migration inhibitory factor is a potential inducer of endothelial progenitor cell mobilization after flap operation. Surgery 2012, 151, 268–277.e1. [Google Scholar] [CrossRef]
- Kim, B.-S.; Breuer, B.; Arnke, K.; Ruhl, T.; Hofer, T.; Simons, D.; Knobe, M.; Ganse, B.; Guidi, M.; Beier, J.P.; et al. The effect of the macrophage migration inhibitory factor (MIF) on excisional wound healing in vivo. J. Plast. Surg. Hand Surg. 2020, 54, 137–144. [Google Scholar] [CrossRef]
- Grieb, G.; Kim, B.-S.; Simons, D.; Bernhagen, J.; Pallua, N. MIF and CD74-suitability as clinical biomarkers. Mini Rev. Med. Chem. 2014, 14, 1125–1131. [Google Scholar] [CrossRef]
- Hertelendy, J.; Reumuth, G.; Simons, D.; Stoppe, C.; Kim, B.-S.; Stromps, J.-P.; Fuchs, P.C.; Bernhagen, J.; Pallua, N.; Grieb, G. Macrophage Migration Inhibitory Factor-A Favorable Marker in Inflammatory Diseases? Curr. Med. Chem. 2018, 25, 601–605. [Google Scholar] [CrossRef] [PubMed]
- Flieger, O.; Engling, A.; Bucala, R.; Lue, H.; Nickel, W.; Bernhagen, J. Regulated secretion of macrophage migration inhibi-tory factor is mediated by a non-classical pathway involving an ABC transporter. FEBS Lett. 2003, 551, 78–86. [Google Scholar] [CrossRef]
- Grieb, G.; Simons, D.; Piatkowski, A.; Bernhagen, J.; Steffens, G.; Pallua, N. Macrophage migration inhibitory factor-A po-tential diagnostic tool in severe burn injuries? Burns 2010, 36, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Swartz, W.M.; Izquierdo, R.; Miller, M.J. Implantable venous Doppler microvascular monitoring: Laboratory investigation and clinical results. Plast Reconstr. Surg. 1994, 93, 152–163. [Google Scholar] [CrossRef]
- Paprottka, F.J.; Klimas, D.; Krezdorn, N.; Schlarb, D.; Trevatt, A.E.J.; Hebebrand, D. Cook-Swartz Doppler Probe Surveillance for Free Flaps-Defining Pros and Cons. Surg. J. 2019, 6, e42–e46. [Google Scholar] [CrossRef]
- Schmulder, A.; Gur, E.; Zaretski, A. Eight-year experience of the Cook-Swartz Doppler in free-flap operations: Microsur-gical and reexploration results with regard to a wide spectrum of surgeries. Microsurgery 2011, 31, 1–6. [Google Scholar] [CrossRef]
- Fox, P.M.; Zeidler, K.; Carey, J.; Lee, G.K. White light spectroscopy for free flap monitoring. Microsurgery 2012, 33, 198–202. [Google Scholar] [CrossRef]
- Salgado, C.J.; Moran, S.L.; Mardini, S. Flap Monitoring and Patient Management. Plast. Reconstr. Surg. 2009, 124, e295–e302. [Google Scholar] [CrossRef]
- Smit, J.M.; Zeebregts, C.J.; Acosta, R.; Werker, P.M.N. Advancements in free flap monitoring in the last decade: A critical re-view. Plast Reconstr. Surg. 2010, 125, 177–185. [Google Scholar] [CrossRef]
- Salgarello, M.; Pagliara, D.; Rossi, M.; Visconti, G.; Barone-Adesi, L. Postoperative Monitoring of Free DIEP Flap in Breast Reconstruction with Near-Infrared Spectroscopy: Variables Affecting the Regional Oxygen Saturation. J. Reconstr. Microsurg. 2018, 34, 383–388. [Google Scholar] [CrossRef]
- Ibrahim, M.M.; Patel, P.S.; Wu, Z.J.; Chien, J.S.; Wisniewski, N.A.; Mohammed, M.M.; Klitzman, B. Detection of flap tissue is-chemia in a rat model: Real-time monitoring of changes in oxygenation and perfusion through injectable biosensors. Surgery 2020, 168, 926–934. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.J.; Nguyen, M.-D.; Chen, C.; Colakoglu, S.; Curtis, M.S.; Tobias, A.M.; Lee, B.T. Tissue oximetry monitoring in microsurgi-cal breast reconstruction decreases flap loss and improves rate of flap salvage. Plast Reconstr. Surg. 2011, 127, 1080–1085. [Google Scholar] [CrossRef] [PubMed]
- Patel, U.A.; Hernandez, D.; Shnayder, Y.; Wax, M.K.; Hanasono, M.M.; Hornig, J.; Ghanem, T.A.; Old, M.; Jackson, R.S.; Ledgerwood, L.G.; et al. Free Flap Reconstruction Monitoring Techniques and Frequency in the Era of Restricted Resident Work Hours. JAMA Otolaryngol. Neck Surg. 2017, 143, 803–809. [Google Scholar] [CrossRef]
- Karinja, S.J.; Lee, B.T. Advances in flap monitoring and impact of enhanced recovery protocols. J. Surg. Oncol. 2018, 118, 758–767. [Google Scholar] [CrossRef]
- Cervenka, B.; Bewley, A.F. Free flap monitoring: A review of the recent literature. Curr. Opin. Otolaryngol Head Neck Surg. 2015, 23, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Luu, Q.; Farwell, D.G. Advances in free flap monitoring: Have we gone too far? Curr. Opin. Otolaryngol Head Neck Surg. 2009, 17, 267–269. [Google Scholar] [CrossRef] [PubMed]
- Frohwitter, G.; Nobis, C.-P.; Weber, M.; Oetter, N.; Rau, A.; Kesting, M.R.; Lutz, R. Thermal Imaging in a Clinically Non-assessable Free Flap Reconstruction of the Face. Plast. Reconstr. Surg.-Glob. Open 2021, 9, e3440. [Google Scholar] [CrossRef] [PubMed]
- Shen, A.Y.; Lonie, S.; Lim, K.; Farthing, H.; Hunter-Smith, D.J.; Rozen, W.M. Free Flap Monitoring, Salvage, and Failure Tim-ing: A Systematic Review. J. Reconstr. Microsurg. 2021, 37, 300–308. [Google Scholar]
- Koerdt, S.; Rommel, N.; Rohleder, N.; Sandig, S.; Frohwitter, G.; Steiner, T.; Wolff, K.; Kesting, M. Perioperative serum levels of procalcitonin, C-reactive protein, and leukocytes in head and neck free flaps. Int. J. Oral Maxillofac. Surg. 2017, 46, 699–705. [Google Scholar] [CrossRef]
- Du, W.; Wu, P.-F.; Qing, L.-M.; Wang, C.-Y.; Liang, J.-Y.; Yu, F.; Tang, J.-Y. Systemic and Flap Inflammatory Response Associates with Thrombosis in Flap Venous Crisis. Inflammation 2014, 38, 298–304. [Google Scholar] [CrossRef]
- Hill, J.B.; Patel, A.; Del Corral, G.A.; Sexton, K.W.; Ehrenfeld, J.M.; Guillamondegui, O.D.; Shack, R.B. Preoperative anemia pre-dicts thrombosis and free flap failure in microvascular reconstruction. Ann. Plast Surg. 2012, 69, 364–367. [Google Scholar] [CrossRef] [PubMed]
- Kloeters, O.; Vasilic, D.; Hupkens, P.; Ulrich, D. Markers of blood coagulation and fibrinolysis in patients with early and delayed microsurgical reconstructions in the lower extremities. J. Plast. Surg. Hand Surg. 2017, 51, 420–426. [Google Scholar] [CrossRef]
- Koga, K.; Kenessey, A.; Powell, S.R.; Sison, C.P.; Miller, E.J.; Ojamaa, K. Macrophage migration inhibitory factor provides cardioprotection during ischemia/reperfusion by reducing oxidative stress. Antioxid Redox Signal. 2011, 14, 1191–1202. [Google Scholar] [CrossRef] [PubMed]
- Wright, E.; Khan, U. Serum complement-reactive protein (CRP) trends following local and free-tissue reconstructions for traumatic injuries or chronic wounds of the lower limb. J. Plast. Reconstr. Aesthetic Surg. 2010, 63, 1519–1522. [Google Scholar] [CrossRef] [PubMed]



| Patients | Age | Sex | Region of Skin/Soft Tissue Defect | Free Flap Procedure | Revision Necessary | Total Flap Loss |
|---|---|---|---|---|---|---|
| (M/F) | (y/n) | (y/n) | ||||
| Patient 1 | 66 | M | elbow | antero lateral thigh flap | n | n |
| Patient 2 | 41 | M | hand | antero lateral thigh flap | n | n |
| Patient 3 | 53 | M | abdomen | latissimus dorsi flap | n | n |
| Patient 4 | 42 | F | lower leg | radial forearm flap | n | n |
| Patient 5 | 55 | M | foot | latissimus dorsi flap | n | n |
| Patient 6 | 19 | M | hand | parascapular | n | n |
| Patient 7 | 50 | M | lower leg | latissimus dorsi flap | n | n |
| Patient 8 | 25 | M | face | gracilis flap | n | n |
| Patient 9 | 27 | M | lower leg | latissimus dorsi flap | n | n |
| Patient 10 | 50 | M | lower leg | antero lateral thigh flap | n | n |
| Patient 11 | 53 | M | lower leg | gracilis flap | n | n |
| Patient 12 | 46 | F | breast | diep flap | n | n |
| Patient 13 | 71 | F | lower leg | radial forearm flap | n | n |
| Patient 14 | 59 | M | lower leg | antero lateral thigh flap | y | n |
| Patient 15 | 66 | M | lower leg | gracilis flap | y | n |
| Patient 16 | 63 | F | breast | diep flap | n | n |
| Patient 17 | 71 | F | lower leg | gracilis flap | n | n |
| Patient 18 | 51 | F | breast | diep flap | n | n |
| Patient 19 | 59 | M | foot | antero lateral thigh flap | n | n |
| Patient 20 | 48 | F | breast | diep flap | n | n |
| Patient 21 | 29 | M | knee | gracilis flap | y | y |
| Patient 22 | 52 | F | breast | diep flap | n | n |
| Patient 23 | 26 | M | axilla | antero lateral thigh flap | n | n |
| Patient 24 | 30 | M | lower leg | antero lateral thigh flap | y | y |
| Patient 25 | 42 | F | breast | diep flap | y | n |
| Patient 26 | 51 | F | breast | diep flap | n | n |
| Age | ||||||
| Mean | 47.885 | |||||
| Range | 19 to 71 | |||||
| Median | 50.5 | |||||
| SD | 14.72 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Megas, I.-F.; Simons, D.; Kim, B.-S.; Stoppe, C.; Piatkowski, A.; Fikatas, P.; Fuchs, P.C.; Bastiaanse, J.; Pallua, N.; Bernhagen, J.; et al. Macrophage Migration Inhibitory Factor—An Innovative Indicator for Free Flap Ischemia after Microsurgical Reconstruction. Healthcare 2021, 9, 616. https://doi.org/10.3390/healthcare9060616
Megas I-F, Simons D, Kim B-S, Stoppe C, Piatkowski A, Fikatas P, Fuchs PC, Bastiaanse J, Pallua N, Bernhagen J, et al. Macrophage Migration Inhibitory Factor—An Innovative Indicator for Free Flap Ischemia after Microsurgical Reconstruction. Healthcare. 2021; 9(6):616. https://doi.org/10.3390/healthcare9060616
Chicago/Turabian StyleMegas, Ioannis-Fivos, David Simons, Bong-Sung Kim, Christian Stoppe, Andrzej Piatkowski, Panagiotis Fikatas, Paul Christian Fuchs, Jacqueline Bastiaanse, Norbert Pallua, Jürgen Bernhagen, and et al. 2021. "Macrophage Migration Inhibitory Factor—An Innovative Indicator for Free Flap Ischemia after Microsurgical Reconstruction" Healthcare 9, no. 6: 616. https://doi.org/10.3390/healthcare9060616
APA StyleMegas, I.-F., Simons, D., Kim, B.-S., Stoppe, C., Piatkowski, A., Fikatas, P., Fuchs, P. C., Bastiaanse, J., Pallua, N., Bernhagen, J., & Grieb, G. (2021). Macrophage Migration Inhibitory Factor—An Innovative Indicator for Free Flap Ischemia after Microsurgical Reconstruction. Healthcare, 9(6), 616. https://doi.org/10.3390/healthcare9060616








