Abstract
Background: Children generally face a higher incidence of airway management complications, intubation difficulties, and the risk of failed intubation. Currently, there is sufficient evidence in clinical practice for the use of videolaryngoscopes in pediatric airway management. However, there are a number of standard-blade videolaryngoscopes available for children. In addition, there is no clear recommendation on which videolaryngoscope is superior. The primary objective of this study is to compare the first pass success rate and the Percentage of Glottic Opening (POGO) scores with Cormack–Lehane (CML) scores obtained through direct and indirect laryngoscopy with HugeMed and McGrath Mac videolaryngoscopes in pediatric patients with an unanticipated, difficult airway. Materials and Methods: Following the Ethics Committee approval and written parental consents, a total of 40 elective surgical patients, aged 3 and under, with ASA 1–3 risk classification, and undergoing general anesthesia, were included in the study. After induction of general anesthesia, the first group of patients (Group McGrath, n = 20) was intubated with the McGrath Mac videolaryngoscope, and the second group (Group HugeMed, n = 20) with the HugeMed videolaryngoscope. Before intubation, CML and POGO scores were recorded for both groups using direct and indirect laryngoscopy with videolaryngoscopes. Intubation time, number of attempts, need for cricoid pressure, optimization maneuver requirement, and hemodynamic parameters were recorded for both groups. Results: There was no significant difference between groups in demographic data including age, gender, body mass index, ASA, and hemodynamic parameters. A significant improvement was observed in CML and POGO scores using indirect laryngoscopy (p < 0.001). CML scores obtained with the McGrath Mac were significantly lower than the HugeMed Group (p = 0.0034). The mean POGO value calculated with indirect laryngoscopy was significantly higher in the McGrath Group compared to the HugeMed Group (92.63 ± 6.09 vs. 88.75 ± 4.44, respectively). Conclusions: Videolaryngoscopes improved laryngeal visualization in children under 3 years old. Compared to HugeMed, in indirect laryngoscopy, the McGrath Mac videolaryngoscope was found to be superior, with better CML and POGO scores. However, number of tracheal intubation attempts, success rate, complication risk, and hemodynamic parameters did not show any significant difference between the groups. Clinical trial registration number was NCT06484517.
1. Introduction
Children are generally at a higher risk of airway management complications, intubation difficulties, and the risk of failed intubation [1]. These risks are associated with increased morbidity and mortality rates, increased frequency of intensive care admissions, and increased cardiovascular instability in children with difficult airway [2]. Currently, there is sufficient evidence to suggest the use of videolaryngoscopes (VLs) in pediatric airway management, and they are increasingly used in clinical practice [3]. The French guidelines for the management of a child’s airway under anesthesia recommend the use of a videolaryngoscopy as the first option in cases of anticipated difficult intubation [4]. The recently published joint guidelines on airway management in neonates and infants also recommended VLs as the first stage for both the clinically stable and unstable patients [5]. In particular, the COVID-19 pandemic has had a significant impact on VLs. Both the availability of videolaryngoscopes and their routine use in all cases have significantly increased [6]. It has been reported that standard blades are superior to non-standard blades in pediatric patients [7]. However, there are many standard bladed VLs available in the market for children. Therefore, a clear recommendation cannot be made regarding which VL is superior [8]. Many prospective comparative studies have been conducted in an attempt to find the “best” VL, but often conflicting results have been obtained [9]. McGrath Mac is a VL with a standard blade and a high-resolution camera at the tip [10]. A disposable plastic blade and a battery-contained handle are included [11]. As it has an external display monitor, there is no need for additional cable, screen, or power unit connections [12].
The HugeMed VL features a reusable Macintosh blade. It has a 3.5-inch HD screen at the top of the handle. The screen can rotate right-left and up-down. The camera at the tip of the blade has a field of view of 60 degrees [6]. Despite the frequent use of both McGrath Mac and HugeMed VL in pediatric patients in recent years, there is currently no prospective comparative study in the literature comparing the two VLs. The primary objective of this study was to compare first pass success rate and POGO scores reflecting the percentage of glottis opening in unexpected difficult pediatric airways using HugeMed and McGrath Mac VLs for both direct and indirect laryngoscopy. We aimed to compare Cormack Lehane scores as well. Our secondary objectives included the postoperative complication rate and their impact on hemodynamic response.
2. Materials and Methods
This is a randomized controlled trial, and Ethics Committee approval from the Institutional Review Board of our university hospital (09.2021.961) was obtained. The study was retrospectively registered on www.clinicaltrials.gov (Registration No: NCT06484517). A total of 40 elective surgical patients under the age of 3, classified as American Society of Anesthesiologists (ASA) 1–3 risk group, who underwent general anesthesia with predicted normal airways were included in the study. Patients were divided into two groups using a sealed envelope method as McGrath Group and HugeMed Group. The flow diagram is presented in Figure 1. After standard anesthesia monitoring to each group, general anesthesia was administered. Written informed consent was obtained from the parents of the patients.
Figure 1.
Flow diagram.
2.1. Exclusion Criteria
Patients who could not obtain parental consent, those classified as ASA 4 and above, individuals with serious cardiac and respiratory problems, patients undergoing laryngeal and oral surgery and anticipated to have a difficult airway were not included in the study.
2.2. General Anesthesia
Thirty minutes before anesthesia induction, all patients received premedication with intravenous 0.03 mg/kg midazolam. Standard monitoring before surgery included continuous ST-segment analysis with a 3-lead electrocardiogram (ECG), peripheral oxygen saturation (SpO2), and intermittent non-invasive blood pressure assessment. After three minutes of preoxygenation with 100% oxygen, general anesthesia was induced with intravenous propofol 3 mg/kg following the administration of fentanyl 2 µg/kg. Muscle relaxation was achieved in all patients with intravenous rocuronium 0.5 mg/kg.
2.3. Tracheal Intubation
A direct laryngoscopy provides a clear visualization of the larynx under direct vision. An indirect laryngoscopy uses a camera to visualize the larynx without a direct view. Both McGrath Mac and HugeMed laryngoscopes are devices with an attached camera system (Figure 2). When the camera is off, the device functions as a direct laryngoscope. When turned on, it operates as an indirect laryngoscope. In this way, they integrate the advantages of both direct laryngoscopy and indirect video laryngoscopy.
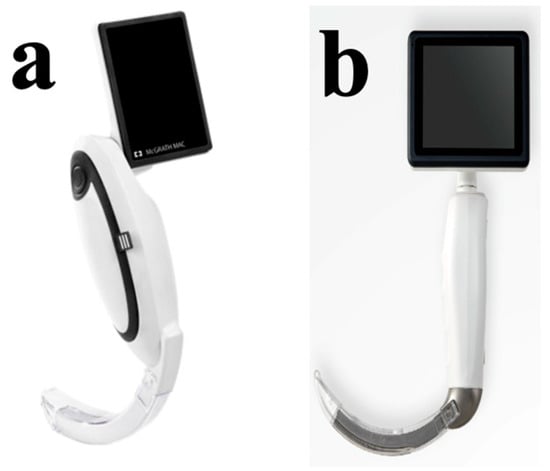
Figure 2.
MacGrath Mac (a) and HugeMed videolaryngoscope (b).
After general anesthesia induction, Group McGrath patients were intubated with the McGrath Mac VL (Medtronic, Minneapolis, MN, USA). Before intubation, CML and POGO scores were recorded by applying direct and indirect laryngoscopy. All tracheal intubations were performed by the same expert with over 10 years of experience in pediatric anesthesia. Rocuronium was administered at a dose of 0.6 mg/kg as a muscle relaxant for tracheal intubation during anesthesia induction. The train-of-four measurement was conducted every 10 s at a train frequency of 0.1 Hz after administering rocuronium. Laryngoscopy was performed once the count reached zero.
For the second group (Group HugeMed, n = 20), the HugeMed VL (Shenzhen HugeMed Medical Technical Development Co., Ltd., Shenzhen, China) was used. After the induction of general anesthesia, patients underwent direct and indirect laryngoscopy with HugeMed VL under the guidance of train-of-four monitoring. Patients were intubated using one of the appropriate Macintosh blades numbered 1, or 2, based on their height, weight, and age in both the McGrath and HugeMed groups. Hyperangulated blades were not used. The number of attempts, the need for cricoid pressure, optimization maneuvers, success rate, and hemodynamic parameters of both groups were recorded. The optimization maneuvers were used to enhance visualization of the glottis and improve intubation success rate during videolaryngoscopy. These maneuvers included blade tip manipulation for direct epiglottic lifting, withdrawal maneuver to pull back the blade, BURP Maneuver (Backward, Upward, Rightward Pressure) as an external laryngeal manipulation and rotating the tracheal tube 90° counterclockwise. Both VLs were initially used as direct laryngoscopes; the camera system was not activated, and CML and POGO scoring were performed. A second anesthetist other than the operator, took a photograph of the laryngeal view. Following the photo capture during direct laryngoscopy, patients were ventilated with a face mask and 100% oxygen for 1 min. Subsequently, indirect laryngoscopy was performed, and another photograph was taken from the image on the VL integrated camera. An iPhone X brand mobile phone camera (Apple Inc., Cupertino, CA, USA) was used for photographing. Another researcher, blinded to the type of VL used, conducted the CML and POGO scoring based on the photos. After the second photo shoot, children were intubated with an appropriately sized tracheal tube. Optimization maneuvers, including cricoid pressure and cricoid manipulation, were recorded to determine whether we had performed them.
2.4. POGO Classification
The POGO classification was based on a 100% scale, where a score of 100% indicated a full glottic opening from the anterior commissure to the posterior cartilage. The absence of a glottic opening was scored as 0.
Patient characteristics, including age, gender, body weight, Mallampati score, mouth opening, thyromental distance, ASA physical status classification, and intubation time, were recorded. Intubation time was defined as the time from the holding time of laryngoscope to the visualization of end-tidal carbon dioxide (EtCO2). Additionally, mean arterial pressure, heart rate, SpO2, and EtCO2 were recorded before anesthesia induction, after induction, and post-intubation. The number of intubation attempts and complications were also recorded for both groups including throat soreness, bronchospasm, laryngospasm, mucosal trauma, dental injury, arrhythmia, hemodynamic changes, pulmonary aspiration, and mortality.
2.5. Statistical Analysis
Data were analyzed using IBM SPSS V23. Normality was assessed using the Shapiro–Wilk test. Independent samples t-test was used for normally distributed data when comparing between two groups, and the Mann–Whitney U test was used for non-normally distributed data. Repeated measures analysis of variance (ANOVA) was used for normally distributed data within groups over time, with multiple comparisons assessed using the Bonferroni test. Friedman test was used for non-normally distributed quantitative data within groups over time, and multiple comparisons were assessed using the Dunn test. Wilcoxon test was used to compare non-normally distributed POGO values within groups for VL and DL. The Marginal Homogeneity Test was used to compare VL and DL Cormack–Lehane scores within groups. Chi-square test and Yates correction were used to compare categorical data between groups. Relationships between non-normally distributed variables were examined using Spearman’s rho correlation coefficient. The significance level was set at p < 0.050.
2.6. Sample Size Calculation
The sample size was calculated based on data from a similar comparative study [13]. As the primary outcomes were the comparison of first attempt success rate, CML, and POGO scores, a two-tailed effect size of 1.175 was calculated with alpha (α) set at 0.05 and beta (β) at 0.10 when we considered a significant decrease between the two groups. Accordingly, it was determined that 19 patients should be included in each group. Taking into account a potential 20% loss of patient data, we planned to include 20 patients in each group, totaling 40 patients.
3. Results
The mean age was 28.47 ± 7.83 months for McGrath Group and 23.43 ± 7.38 months for HugeMed Group (p = 0.054). In one patient, a postoperative severe airway edema, following an unexpectedly prolonged surgery, led to cardiac arrest after extubating. The child had a large cleft palate and did not respond to cardiopulmonary resuscitation and, unfortunately, did not survive. As a result, this case was excluded from the study. Data from a total of 39 patients were analyzed, and it is noteworthy that all patients were successfully intubated on the first attempt.
Ten of our patients were admitted to the orthopedic ward and underwent surgery for orthopedic reasons. Three of them had humerus fractures, one had debridement, four had tendon repairs, and two had plate removal surgeries. Nine patients were operated on by the neurosurgery team. Two of them had posterior fossa surgeries, four had extraventricular drain placements, and three had shunt surgeries. Six patients were operated on by the pediatric surgery team. One of them had stoma closure, two had circumcision, two had appendectomies, and one had a cystoscopy. Two patients underwent cleft palate surgery by the plastic surgery team. Thirteen patients underwent surgery by the ear, nose, and throat (ENT) team. Six of them had tonsillectomies, five had cochlear implants, and two had cochlear implant revisions. When comparing the demographic data, including age, gender, body mass index, and ASA classification, no significant differences were observed between the groups (p > 0.05, Table 1).

Table 1.
Comparison of demographic data and complications between groups.
As postoperative complications, sore throat was observed in 1 patient in the HugeMed Group and bronchospasm was observed in 1 patient in the McGrath group. Laryngospasm and minimal mucosal bleeding were noted in one patient in each group (Table 1). Minimal mucosal bleeding was observed in patients with a higher frequency of intubation attempts. These were identified upon seeing blood on the laryngoscope blade. Upon oral inspection in these patients, no actively bleeding focus was observed. After oral aspiration, pressure was applied with a sponge to the areas where minimal bleeding was observed for 1 min. Following extubating, the oral cavity was inspected again with the aid of light, and it was confirmed that there was no bleeding.
After the induction of anesthesia, the number of tracheal intubation attempts were similar in both groups (p = 0.788, Table 2). The mean tracheal intubation time for Group McGrath was 39.26 ± 21.88 s, while those for Group HugeMed were 48.07 ± 27.15 s. No significant difference was observed between the two groups (p > 0.05). The optimization maneuvers were performed in six patients from Group McGrath (30%). The maneuvers included tracheal tube rotation in three patients, lifting the epiglottis instead of tongue base in two patients, and a withdrawal maneuver in one patient. The HugeMed Group experienced optimization maneuvers in five patients (25%). There was no statistically significant difference between groups (p > 0.05). One patient required a BURP maneuver, while two patients required tracheal tube rotation. Epiglottis lifting was performed for two patients.

Table 2.
The comparison of the number of tracheal intubation attempts.
The comparison of successful tracheal intubation attempts did not show any significant difference between groups (χ2 = 0.022, p = 0.882, Table 3).

Table 3.
The comparison of a successful first tracheal intubation attempt.
The Modified Cormack–Lehane scores obtained from direct laryngoscopy before intubation were similar between the two groups (p = 0.462, Table 4). When comparing the CML scores from direct laryngoscopy with indirect laryngoscopy values, both groups showed a significant improvement in CML scores with indirect laryngoscopy (p < 0.001). The CML scores obtained with McGrath Mac VL were significantly lower than those in the HugeMed Group (p = 0.0034, Table 4). The mean difference was −0.5 (95% CI: −0.8 to −0.2), with a Cohen’s d of −0.65, indicating a medium effect size.

Table 4.
Comparison of Cormack–Lehane scores between and within groups.
The mean POGO values measured during direct laryngoscopy were similar between the McGrath and HugeMed groups (78.42 ± 12.48 and 80.75 ± 6.74, respectively). The mean POGO values calculated with indirect laryngoscopy using both VLs were significantly higher than those obtained from direct laryngoscopy (p < 0.001, Table 4). The mean POGO value calculated with indirect laryngoscopy in the McGrath Group was significantly higher than that in the HugeMed Group (92.63 ± 6.09 vs. 88.75 ± 4.44, respectively). The mean difference was 3.88 (95% CI: 1.12 to 6.64), with a Cohen’s d of 0.75, indicating a medium to large effect size. The success rate for the first intubation attempt was 52.6% in the McGrath group and 55.0% in the HugeMed group. The odds ratio for success in the McGrath group compared to the HugeMed group was 0.91 (95% CI: 0.45 to 1.85), indicating no significant difference.
There was no significant difference between and within groups in systolic, diastolic and mean arterial pressure, and heart rate immediately before induction, within two minutes after induction, and post-intubation period until the patient was discharged from the operating room (p > 0.05). There was no significant difference in the mean oxygen saturation values before induction, after induction, and post-intubation between the groups (p > 0.05). However, in the HugeMed Group, there was a significant difference in oxygen saturation values before induction and post-intubation (p = 0.014). In Group McGrath, no significant difference was observed in oxygen saturation values over time (p = 0.420). There was no difference in mean end-tidal carbon dioxide values before and after induction between the groups (p > 0.05). However, there was a significant difference in post-intubation end-tidal carbon dioxide values between the groups (p = 0.039). In Group HugeMed, the mean end-tidal carbon dioxide was 32.10 mmHg, while in Group McGrath, it was 35.74 mmHg. Additionally, in both Group HugeMed and Group McGrath, there was a significant difference between pre-induction end-tidal carbon dioxide values and post-intubation end-tidal carbon dioxide values (p < 0.001, Table 5). The box plot graphs of the SpO2 change over time in the groups are shown in Figure 3.

Table 5.
Comparison of inter and intragroup hemodynamic, SpO2 and etCO2 variables.
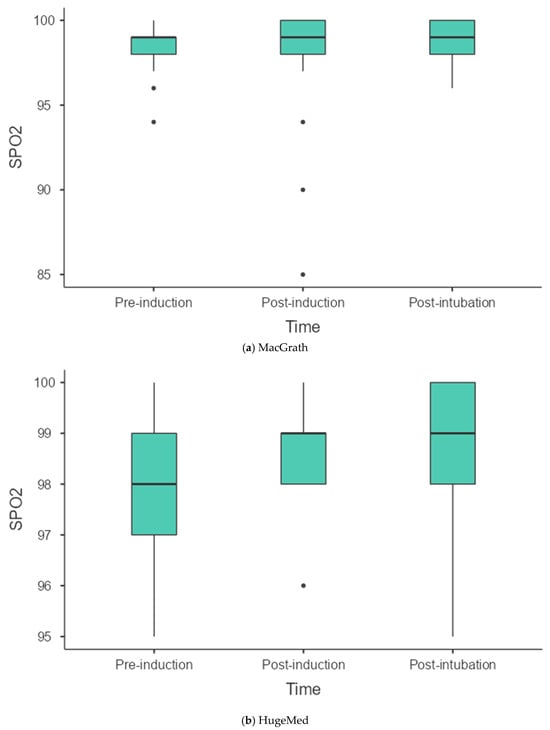
Figure 3.
Box plot graphs of the SpO2 change over time in the groups. Dots represent the outliers. (a) MacGrath. (b) HugeMed.
Within each group, no statistically significant relationship was found between the number of attempts and post-intubation systolic, diastolic, mean arterial pressure, heart rate, oxygen saturation, and end-tidal carbon dioxide values (p > 0.05, Table 6).

Table 6.
Examining the relationship between the number of attempts within groups and the parameters.
An insignificant positive relationship was observed between age and POGO scores with a VL and a negative relationship between POGO scores with a direct laryngoscopy in the McGrath Group. It was observed that, as the age increased, the POGO score with a direct laryngoscope decreased, while the POGO score with VL increased. In the HugeMed group, a positive insignificant relationship was observed between the age and POGO scores with VL and POGO with direct laryngoscopy. We observed that POGO scores with VL and direct laryngoscopy decreased as age increased (Table 7).

Table 7.
Correlation analysis.
4. Discussion
In this prospective randomized controlled study, data obtained through direct and indirect laryngoscopy with HugeMed and McGrath VLs were compared in children under 3 years of age undergoing elective surgery requiring tracheal intubation. Significant improvements in both CML and POGO scores were recorded with indirect laryngoscopy in both groups compared to direct laryngoscopy. The McGrath VL yielded higher POGO scores and lower CML values compared to HugeMed, however the number of intubation attempts, success and complication rates, or hemodynamic data did not differ.
In recent years, videolaryngoscopy has increasingly been regarded as a primary tool for airway management, rather than merely a backup for difficult intubations. However, it does not guarantee a 100% success rate in intubation [14]. Although videolaryngoscopy offers numerous benefits, there are potential challenges that can arise, many of which can be easily mitigated with proper knowledge and attention. Adequate training, consistent practice, and familiarity with device-specific tools are essential to ensure that the enhanced laryngeal view leads to successful tracheal intubation. Our study demonstrated that videolaryngoscopy improves laryngeal visualization, with the McGrath VL showing a particularly enhanced image. However, the clarity of vocal cord visibility did not influence either the rate of tracheal intubation attempts or the success of the first attempt. Various factors contribute to the number of intubation attempts, with the most critical being the ability to direct the tracheal tube. In our study, the anesthesiologists were experienced with both devices, which used a standard Macintosh-type blade. Despite the team’s expertise and group standardization, first-pass failure occurred in nine patients using both VLs. We believe that further practice and experience in this area will help reduce the number of intubation attempts.
The results from the PeDI Registry suggested that we still do not make accurate choices for pediatric airway management [15]. In the analysis of difficult airway cases in children, 46% of anesthetists chose direct laryngoscopy as the first-choice airway technique, with a success rate of 3%. Only 18% of anesthesia experts chose videolaryngoscopy, reporting a success rate of 55%. While the physiological changes in children’s airways and the associated risk of intubation difficulty are known, the superiority of VLs over direct laryngoscopy has been proven in many studies [16]. However, recent multicenter survey studies have revealed that 88% of direct laryngoscopes are routinely used in the intubation of children, with only 11% preferring VLs for all intubations [17].
One advantage of videolaryngoscopes is the ability to obtain both direct and indirect images. A meta-analysis from 2014 comparing pediatric videolaryngoscopes with direct laryngoscopes in 14 randomized controlled studies reported better visualization of the glottis with VLs [18]. Although the initial success rate and the associated complications were similar for both laryngoscope types, this meta-analysis reported a higher incidence of failure for VLs. It is evident that more experience with pediatric VLs has been gained over the years. A Cochrane meta-analysis in 2017, including 803 children, reported marked heterogeneity among studies on this topic and emphasized the difficulty in outcome analysis [19]. As reported in the Anaesthesia Practice In Children Observational Trial (APRICOT), prospective multicenter observational study, education, training, and research can improve perioperative care and reduce complication rates in these children [20]. Considering these factors, in this study, an anesthetist with over 10 years of pediatric anesthesia experience was dedicated to tracheal intubation. The results showed that not only were laryngeal structures better visualized with VLs, but the success rate of tracheal intubation was also 100% in experienced hands. Additionally, we observed only minor, manageable complications through this approach.
Our study demonstrated a significant improvement in both CML and POGO scores with indirect laryngoscopy. Standard-blade videolaryngoscopes resemble traditional direct laryngoscopes in shape and design, requiring less experience and being easy to learn [7]. However, non-standard blades should be used by experienced operators. Despite the recommendation for the use of standard-blade VLs, there is no clear suggestion in the literature regarding which standard-blade VLs can be used in pediatric patients.
Even though the operators in our study were experienced in pediatric anesthesia, we observed minor complications including sore throat, bronchospasm, and minimal mucosal bleeding. Postoperative sore throat was observed in one patient from the HugeMed Group. It was likely due to mechanical irritation from the laryngoscope blade. Despite using the same blade sizes, slight variations between laryngoscopes may have contributed to this outcome. Typically mild and self-limiting, it can still impact patient comfort and recovery. Therefore, operators should consider this possibility during tracheal intubation. Minimal mucosal injuries might occur due to minor trauma from laryngoscope insertion, particularly in difficult airways. Typically they are minor and self-resolving but could indicate excessive force or a suboptimal technique.
McGrath Mac VL, on the market since 2010, has had conflicting results in studies conducted in children. In a study involving 30 children aged 1–10 years undergoing surgical release of torticollis, McGrath Mac was compared with Macintosh direct laryngoscope [10]. The McGrath group reported a significantly prolonged intubation time: 31.4 ± 6.7 s vs. 26.1 ± 5.4 s. In another pediatric manikin study comparing McGrath Mac to direct laryngoscopy, the use of McGrath Mac VL increased intubation success in cases with a high probability of difficult intubation [1]. In another manikin study by Owada et al. [13] in 2017, the authors revealed that intubation with Airtraq was more successful than with McGrath Mac and Macintosh laryngoscopes. Intubations with Airtraq had lower CML scores, higher POGO scores, and less postoperative throat pain and dental trauma compared to intubations with the other two laryngoscopes.
In our study, tracheal intubation attempts were performed lifting the tongue base. Kucukoglu et al. [21] compared McGrath and Miller laryngoscopes when the direct lifting method of the epiglottis was used. Both laryngoscopes demonstrated comparable effectiveness in terms of POGO and CL scores. In a randomized controlled study, the McGrath Mac was compared with a direct Macintosh laryngoscope. Similarly, there were again no significant differences in the POGO scores between the two groups [22]. A unique aspect of our study was the comparison of both direct and indirect visualization methods. This approach allowed us to gain a clearer understanding of which method may be more beneficial for the pediatric population.
HugeMed is a recently introduced VL that offers adult and pediatric blade sizes, and its use has increased with the COVID-19 pandemic. To the best of our knowledge, this study is the first to investigate pediatric HugeMed VL. We chose McGrath Mac VL as the comparison group because it is easily accessible and we have experience with it. While the success rate and complication rate did not differ, the results of our study clearly demonstrated the superiority of McGrath Mac VL over HugeMed in visualizing pediatric laryngeal structures.
5. Limitations
Limitations of this study include its single-center nature and the low sample size. Despite the low sample size, meaningful results that can shed light on the use of VLs in our clinical practice have been obtained. However, it is clear that there is a need for further comparative multicenter studies. We performed a second exposure of glottis and the photos were recorded. This approach could increase the risk of a laryngeal edema and extended intubation time, which can lead to a lower peripheral oxygen saturation and decrease the patients benefit. However, no complication occurred. There was a time period of 1 min between the direct and indirect laryngoscopies. This could affect the POGO score and CML grade. Finally, we did not measure the ease of the tracheal tube passage. This can be a study parameter for the planned future studies.
6. Conclusions
In conclusion, VLs improved laryngeal visualization in elective surgical pediatric patients under 3 years old. McGrath Mac VL, compared to HugeMed in indirect laryngoscopy, was found to be superior with better CML and POGO scores. However, the number of tracheal intubation attempts, success rate, complication risk, and hemodynamic parameters did not show significant differences.
Author Contributions
Conceptualization: K.T.S. and A.S., data curation: G.T.C., R.A., E.G. and A.S., formal analysis: R.A., investigation: G.T.C., E.G. and A.S., methodology K.T.S., project administration, supervision: K.T.S. and A.S., writing—original draft: G.T.C., K.T.S., R.A., E.G. and A.S., writing—review and editing: G.T.C. and P.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Marmara University School of Medicine Clinical Researches Ethics Committee (09.2021.961) on 10 September 2021, protocol code 2018/515/124/9.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data can be shared upon request.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All authors have read and agreed to the published version of the manuscript
References
- Madziala, M.; Smereka, J.; Dabrowski, M.; Leung, S.; Ruetzler, K.; Szarpak, L. A comparison of McGrath MAC® and standard direct laryngoscopy in simulated immobilized cervical spine pediatric intubation: A manikin study. Eur. J. Pediatr. 2017, 176, 779–786. [Google Scholar] [PubMed]
- Klabusayová, E.; Klučka, J.; Kosinová, M.; Ťoukálková, M.; Štoudek, R.; Kratochvíl, M.; Mareček, L.; Svoboda, M.; Jabandžiev, P.; Urík, M.; et al. Videolaryngoscopy vs. Direct Laryngoscopy for Elective Airway Management in Paediatric Anaesthesia: A prospective randomised controlled trial. Eur. J. Anaesthesiol. 2021, 38, 1187–1193. [Google Scholar] [PubMed]
- Saracoglu, K.T.; Gunalp, B.; Çabaklı, G.T.; Saracoglu, A. Never-ending debate on pediatric airway: Laryngoscopy, blades and approaches. J. Clin. Anesth. 2022, 76, 110562. [Google Scholar] [PubMed]
- Dadure, C.; Sabourdin, N.; Veyckemans, F.; Babre, F.; Bourdaud, N.; Dahmani, S.; Queiroz, M.; Devys, J.M.; Dubois, M.C.; Kern, D.; et al. Management of the child’s airway under anaesthesia: The French guidelines. Anaesth. Crit. Care Pain. Med. 2019, 38, 681–693. [Google Scholar]
- Disma, N.; Asai, T.; Cools, E.; Cronin, A.; Engelhardt, T.; Fiadjoe, J.; Fuchs, A.; Garcia-Marcinkiewicz, A.; Habre, W.; Heath, C.; et al. Airway management in neonates and infants: European Society of Anaesthesiology and Intensive Care and British Journal of Anaesthesia joint guidelines. Br. J. Anaesth. 2024, 132, 124–144. [Google Scholar] [CrossRef]
- Saracoglu, A.; Saracoglu, K.; Sorbello, M.; Çakmak, G.; Greif, R. The influence of the COVID-19 pandemic on videolaryngoscopy: A cross-sectional before-and-after survey. Anaesthesiol. Intensive Ther. 2023, 55, 93–102. [Google Scholar]
- Peyton, J.; Park, R.; Staffa, S.J.; Sabato, S.; Templeton, T.W.; Stein, M.L.; Garcia-Marcinkiewicz, A.G.; Kiss, E.; Fiadjoe, J.E.; von Ungern-Sternberg, B.; et al. A comparison of videolaryngoscopy using standard blades or non-standard blades in children in the Paediatric Difficult Intubation Registry. Br. J. Anaesth. 2021, 126, 331–339. [Google Scholar]
- Saracoglu, K.T.; Eti, Z.; Kavas, A.D.; Umuroglu, T. Straight video blades are advantageous than curved blades in simulated pediatric difficult intubation. Paediatr. Anaesth. 2014, 24, 297–302. [Google Scholar]
- Norris, A.; Armstrong, J. Comparative videolaryngoscope performance in children: Data from the Pediatric Difficult Intubation Registry. Br. J. Anaesth. 2021, 126, 20–22. [Google Scholar]
- Kriege, M.; Lang, P.; Lang, C.; Schmidtmann, I.; Kunitz, O.; Roth, M.; Strate, M.; Schmutz, A.; Vits, E.; Balogh, O.; et al. A comparison of the McGrath videolaryngoscope with direct laryngoscopy for rapid sequence intubation in the operating theatre: A multicentre randomised controlled trial. Anaesthesia 2024. [Google Scholar] [CrossRef]
- Ho, C.H.; Chen, L.C.; Hsu, W.H.; Lin, T.Y.; Lee, M.; Lu, C.W. A Comparison of McGrath Videolaryngoscope versus Macintosh Laryngoscope for Nasotracheal Intubation: A Systematic Review and Meta-Analysis. J Clin Med. 2022, 11, 2499. [Google Scholar] [PubMed]
- Hoshijima, H.; Mihara, T.; Maruyama, K.; Denawa, Y.; Takahashi, M.; Shiga, T.; Nagasaka, H. McGrath videolaryngoscope versus Macintosh laryngoscope for tracheal intubation: A systematic review and meta-analysis with trial sequential analysis. J. Clin. Anesth. 2018, 46, 25–32. [Google Scholar] [PubMed]
- Owada, G.; Mihara, T.; Inagawa, G.; Asakura, A.; Goto, T.; Ka, K. A comparison of the Airtraq®, McGrath®, and Macintosh laryngoscopes for difficult paediatric intubation: A manikin study. PLoS ONE 2017, 12, e0171889. [Google Scholar] [CrossRef]
- Kelly, F.E.; Cook, T.M. Seeing is believing: Getting the best out of videolaryngoscopy. Br. J. Anaesth. 2016, 117 (Suppl. S1), i9–i13. [Google Scholar] [PubMed]
- Fiadjoe, J.E.; Nishisaki, A.; Jagannathan, N.; Hunyady, A.I.; Greenberg, R.S.; Reynolds, P.I.; Matuszczak, M.E.; Rehman, M.A.; Polaner, D.M.; Szmuk, P.; et al. Airway management complications in children with difficult tracheal intubation from the Pediatric Difficult Intubation (PeDI) registry: A prospective cohort analysis. Lancet Respir. Med. 2016, 4, 37–48. [Google Scholar]
- Macnair, D.; Baraclough, D.; Wilson, G.; Bloch, M.; Engelhardt, T. Pediatric airway management: Comparing the Berci-Kaplan video laryngoscope with direct laryngoscopy. Paediatr Anaesth 2009, 19, 577–580. [Google Scholar]
- Saracoglu, A.; Saracoglu, K.T.; Sorbello, M.; Kurdi, R.; Greif, R.; European Airway Management Society. A view on pediatric airway management: A cross sectional survey study. Minerva Anestesiol. 2022, 88, 982–993. [Google Scholar]
- Sun, Y.; Lu, Y.; Huang, Y.; Jiang, H. Pediatric video laryngoscope versus direct laryngoscope: A meta-analysis of randomized controlled trials. Paediatr. Anaesth. 2014, 24, 1056–1065. [Google Scholar]
- Abdelgadir, I.S.; Phillips, R.S.; Singh, D.; Moncreiff, M.P.; Lumsden, J.L. Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in children (excluding neonates). Cochrane Database Syst. Rev. 2017, 5, CD011413. [Google Scholar]
- Engelhardt, T.; Virag, K.; Veyckemans, F.; Habre, W.; APRICOT Group of the European Society of Anaesthesiology Clinical Trial Network. Airway management in paediatric anaesthesia in Europe-insights from APRICOT (Anaesthesia Practice In Children Observational Trial): A prospective multicentre observational study in 261 hospitals in Europe. Br. J. Anaesth. 2018, 121, 66–75. [Google Scholar]
- Küçükosman, G.; Bollucuoğlu, K.; Ava, M.; Ayoğlu, H. Comparison of the Effectiveness of the Miller Laryngoscope and the McGrath-MAC Video Laryngoscope in Direct Visualization of the Glottic Opening. Medicina 2023, 60, 62. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, Y.; Kimura, S.; Kuniyoshi, H.; Hiroe, T.; Terui, T.; Kase, Y. Novice residents’ endotracheal intubation skill retention on a simulated mannequin after rotating at an anaesthesiology department: A randomized controlled study. J. Int. Med. Res. 2023, 51, 3000605231206313. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).