Implementation and User Satisfaction Analysis of an Electronic Medication Reconciliation Tool (ConciliaMed) in Patients Undergoing Elective Colorectal Surgery
Abstract
1. Introduction
2. Materials and Methods
2.1. Implementation of ConciliaMed
2.1.1. Setting and Study Design
2.1.2. Participants
- Polypharmacy, defined as the concomitant use of five or more chronic medications.
- Diabetes mellitus type 1 or 2.
- Advanced chronic conditions:
- c.1. Cardiovascular disease is defined as congestive heart failure with dyspnea on exertion or ischemic heart disease with acute coronary syndrome or undergoing catheterisation in the last 12 months.
- c.2. Chronic renal failure (filtration glomerular < 30 mL/min).
- c.3. Lung disease with dyspnea on exertion.
- c.4. Liver disease and cirrhosis (Child-Pugh B or C).
- c.5. Hypertension
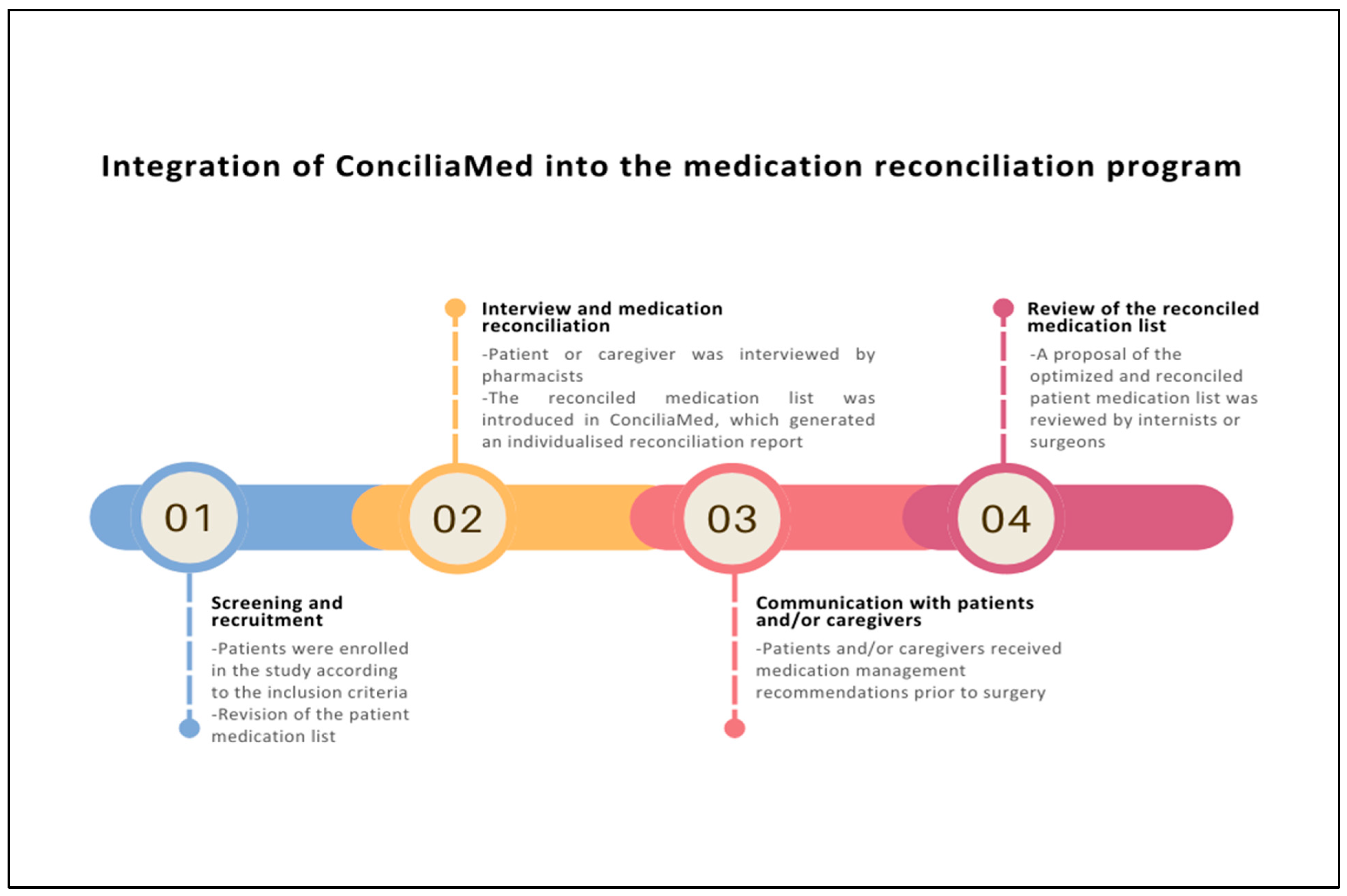
2.1.3. Intervention
2.1.4. Data Collection and Study Measures
- The total and the median number of reconciled medications per patient.
- The number and type of medication discrepancies between the medication list extracted from the EMRs and the reconciled medication list were recorded after the interview with patients or caregivers (discrepancies related to doses, frequency, route of administration, addition or discontinuation of medications). The percentage of patients with at least one discrepancy was recorded.
- Pharmacotherapeutic groups, according to the Anatomical Therapeutic Chemical Classification System (ATC) code, involved in the medication discrepancies and if there were any of these medications classified as “high-risk” according to the High-Alert Medications for patients with Chronic illnesses (HAMC) list [24].
- The number of interventions made optimising the reconciled medication list to the perioperative setting based on ConciliaMed and the anaesthesia reports related to stopping or replacing the patient’s chronic medication before surgery. The pharmacological groups commonly involved in these interventions were also evaluated.
- Conversed medications according to the equivalent doses of drugs included in the “Therapeutics equivalents” module of the tool.
- Number and type of changes related to dose, frequency, route of administration or discontinuation of medications made by physicians to the reconciled and optimised medication list proposed by pharmacists.
- The number of registered users in the app from the day the tool was released on Google Play Store (5 March 2024) to 31 December 2024. Sex, age and professional category of the users were also collected.
- The number of satisfaction surveys completed by users.
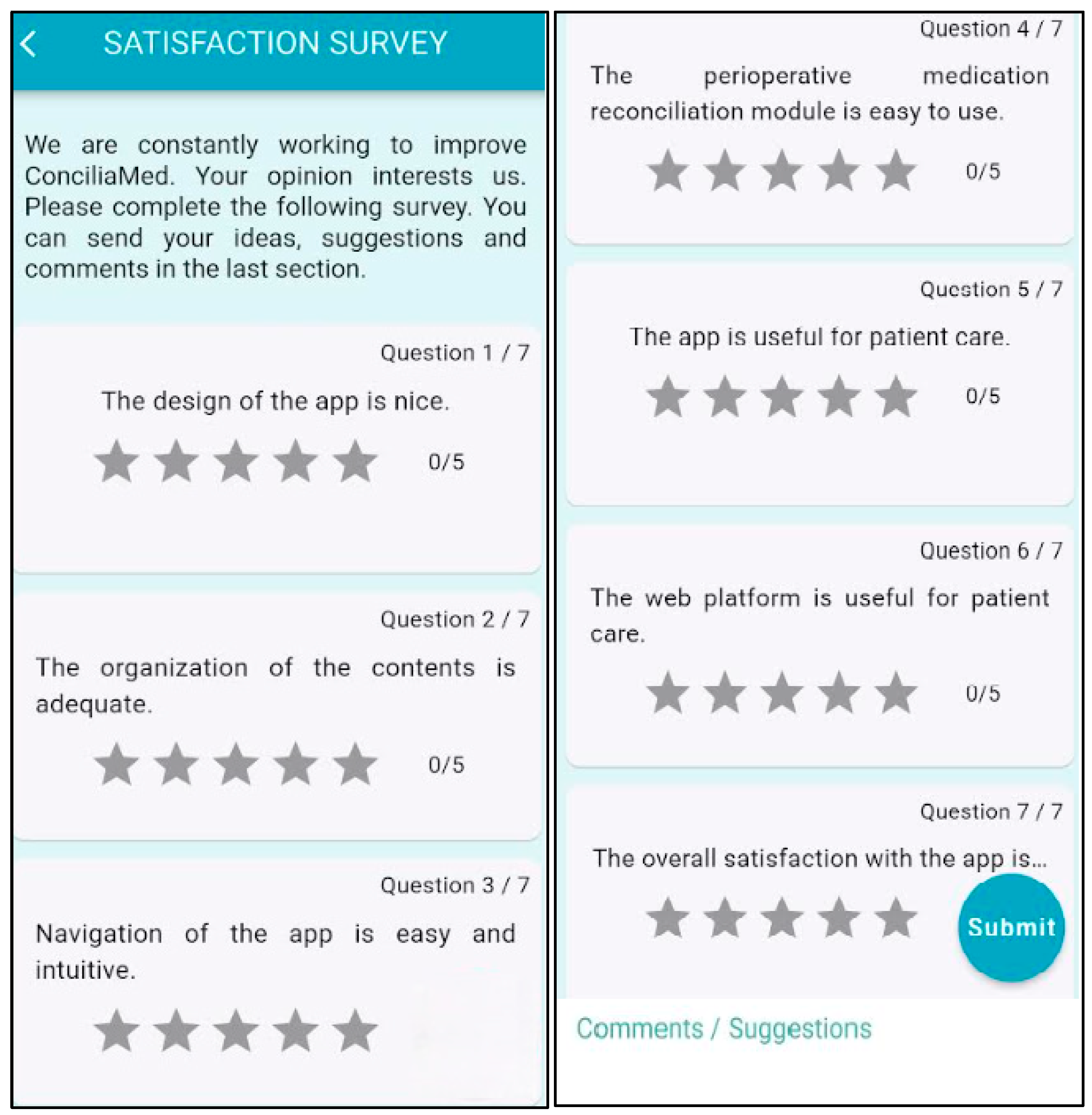
- The means score of a 7-question survey [Figure 2]. A Likert-type scale was used to rate each question from 1 to 5.
- Users’ comments to suggest changes to improve the app’s usability.
2.1.5. Statistical Analysis
2.1.6. Funding and Ethics Approval
3. Results
3.1. Implementation of ConciliaMed
3.2. User Satisfaction Analysis
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MedRec | Medication reconciliation |
| HCPs | Healthcare professionals |
| m-health apps | Mobile health applications |
| EMRs | Electronic medical records |
| BMI | Body mass index |
| ASA | American Society of Anesthesiologists |
| ATC | Anatomical Therapeutic Chemical Classification |
| HAMC | High-Alert Medications for Patients with Chronic Illnesses |
| SPSS | Statistical Package for the Social Sciences |
| SD | Standard deviation |
| IQR | Interquartile range |
| FAQs | Frequently asked questions |
| DOACs | Direct oral anticoagulants |
References
- Devalapalli, A.P.; Kashiwagi, D.T. Perioperative care of geriatric patients. Hosp. Pract. 2020, 48 (Suppl. S1), 26–36. [Google Scholar] [CrossRef] [PubMed]
- Zietlow, K.E.; Wong, S.; Heflin, M.T.; McDonald, S.R.; Sickeler, R.; Devinney, M.; Blitz, J.; Lagoo-Deenadayalan, S.; Berger, M. Geriatric Preoperative Optimization: A Review. Am. J. Med. 2022, 135, 39–48. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Abu Hammour, K.; Abu Farha, R.; Ya’acoub, R.; Salman, Z.; Basheti, I. Impact of Pharmacist-Directed Medication Reconciliation in Reducing Medication Discrepancies: A Randomized Controlled Trial. Can. J. Hosp. Pharm. 2022, 75, 169–177. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Renaudin, A.; Leguelinel-Blache, G.; Choukroun, C.; Lefauconnier, A.; Boisson, C.; Kinowski, J.M.; Cuvillon, P.; Richard, H. Impact of a preoperative pharmaceutical consultation in scheduled orthopedic surgery on admission: A prospective observational study. BMC Health Serv. Res. 2020, 20, 747. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- The Joint Commission. National Patient Safety Goals Effective. 2022. Available online: https://www.jointcommission.org/standards/national-patient-safety-goals/ (accessed on 31 January 2025).
- Medication Safety in Transitions of Care. World Health Organization. 2019. Available online: https://www.who.int/publications/i/item/WHO-UHC-SDS-2019.9 (accessed on 31 January 2025).
- Zheng, X.; Xiao, L.; Li, Y.; Qiu, F.; Huang, W.; Li, X. Improving safety and efficacy with pharmacist medication reconciliation in orthopedic joint surgery within an enhanced recovery after surgery program. BMC Health Serv. Res. 2022, 22, 448. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Anderson, R.; Ferguson, R. A nurse practitioner-led medication reconciliation process to reduce hospital readmissions from a skilled nursing facility. J. Am. Assoc. Nurse Pract. 2020, 32, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Park, B.; Baek, A.; Kim, Y.; Suh, Y.; Lee, J.; Lee, E.; Lee, J.Y.; Lee, E.; Lee, J.; Park, H.S.; et al. Clinical and economic impact of medication reconciliation by designated ward pharmacists in a hospitalist-managed acute medical unit. Res. Soc. Adm. Pharm. 2022, 18, 2683–2690. [Google Scholar] [CrossRef] [PubMed]
- Guisado-Gil, A.B.; Ramírez-Duque, N.; Barón-Franco, B.; Sánchez-Hidalgo, M.; De la Portilla, F.; Santos-Rubio, M.D. Impact of a multidisciplinary medication reconciliation program on clinical outcomes: A pre-post intervention study in surgical patients. Res. Soc. Adm. Pharm. 2021, 17, 1306–1312. [Google Scholar] [CrossRef] [PubMed]
- Marien, S.; Krug, B.; Spinewine, A. Electronic tools to support medication reconciliation: A systematic review. J. Am. Med. Inform. Assoc. 2017, 24, 227–240. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Naseralallah, L.; Koraysh, S.; Aboujabal, B.; Alasmar, M. Interventions and impact of pharmacist-delivered services in perioperative setting on clinically important outcomes: A systematic review and meta-analysis. Ther. Adv. Drug Saf. 2024, 15, 20420986241260169. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fatehi, F.; Samadbeik, M.; Kazemi, A. What is Digital Health? Review of Definitions. Stud. Health Technol. Inform. 2020, 275, 67–71. [Google Scholar] [CrossRef] [PubMed]
- An, Q.; Kelley, M.M.; Hanners, A.; Yen, P.Y. Sustainable Development for Mobile Health Apps Using the Human-Centered Design Process. JMIR Form. Res. 2023, 7, e45694. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Giebel, G.D.; Speckemeier, C.; Schrader, N.F.; Abels, C.; Plescher, F.; Hillerich, V.; Wiedemann, D.; Börchers, K.; Wasem, J.; Blase, N.; et al. Quality assessment of mHealth apps: A scoping review. Front. Health Serv. 2024, 4, 1372871. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Muro-Culebras, A.; Escriche-Escuder, A.; Martin-Martin, J.; Roldán-Jiménez, C.; De-Torres, I.; Ruiz-Muñoz, M.; Gonzalez-Sanchez, M.; Mayoral-Cleries, F.; Biró, A.; Tang, W.; et al. Tools for Evaluating the Content, Efficacy, and Usability of Mobile Health Apps According to the Consensus-Based Standards for the Selection of Health Measurement Instruments: Systematic Review. JMIR Mhealth Uhealth 2021, 9, e15433. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schnall, R.; Cho, H.; Liu, J. Health information technology usability evaluation scale (Health-ITUES) for usability assessment of mobile health technology: Validation study. JMIR Mhealth Uhealth 2018, 6, e4. [Google Scholar] [CrossRef]
- Terhorst, Y.; Philippi, P.; Sander, L.B.; Schultchen, D.; Paganini, S.; Bardus, M.; Santo, K.; Knitza, J.; Machado, G.C.; Schoeppe, S.; et al. Validation of the Mobile Application Rating Scale (MARS). PLoS ONE 2020, 15, e0241480. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shen, Y.; Wang, S.; Shen, Y.; Tan, S.; Dong, Y.; Qin, W.; Zhuang, Y. Evaluating the Usability of mHealth Apps: An Evaluation Model Based on Task Analysis Methods and Eye Movement Data. Healthcare 2024, 12, 1310. [Google Scholar] [CrossRef]
- Ribaut, J.; DeVito Dabbs, A.; Dobbels, F.; Teynor, A.; Mess, E.V.; Hoffmann, T.; De Geest, S. Developing a Comprehensive List of Criteria to Evaluate the Characteristics and Quality of eHealth Smartphone Apps: Systematic Review. JMIR Mhealth Uhealth 2024, 12, e48625. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Giménez-Manzorro, Á.; Romero-Jiménez, R.M.; Calleja-Hernández, M.Á.; Pla-Mestre, R.; Muñoz-Calero, A.; Sanjurjo-Sáez, M. Effectiveness of an electronic tool for medication reconciliation in a general surgery department. Int. J. Clin. Pharm. 2015, 37, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Tamblyn, R.; Abrahamowicz, M.; Buckeridge, D.L.; Bustillo, M.; Forster, A.J.; Girard, N.; Habib, B.; Hanley, J.; Huang, A.; Kurteva, S.; et al. Effect of an Electronic Medication Reconciliation Intervention on Adverse Drug Events: A Cluster Randomized Trial. JAMA Netw. Open 2019, 2, e1910756. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ciudad-Gutiérrez, P.; Suárez-Casillas, P.; Alfaro-Lara, E.R.; Santos-Rubio, M.D.; Santos-Ramos, B.; Guisado-Gil, A.B. ConciliaMed: An interactive mobile and web tool to reconcile chronic medications of patients undergoing elective surgery. BMJ Health Care Inform. 2025, 32, e101256. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Otero, M.J.; Moreno-Gómez, A.M.; Santos-Ramos, B.; Agra, Y. Developing a list of high-alert medications for patients with chronic diseases. Eur. J. Intern. Med. 2014, 25, 900–908. [Google Scholar]
- Capilla-Montes, C.; Casellas-Gilbert, M.; González-Ponce, C.M.; González Pérez, Y.; López Sánchez, P.; Padullés Zamora, N. Guideline About the Perioperative Management of Immunosuppressants and Biological Treatments. Sociedad Española de Farmacia Hospitalaria. 2024. Available online: https://www.sefh.es/bibliotecavirtual/guia_inmunosupresores/guia_perioperatorioV3.pdf?ts=20240612111853 (accessed on 31 January 2025).
- van der Nat, D.J.; Taks, M.; Huiskes, V.J.B.; van den Bemt, B.J.F.; van Onzenoort, H.A.W. Risk factors for clinically relevant deviations in patients’ medication lists reported by patients in personal health records: A prospective cohort study in a hospital setting. Int. J. Clin. Pharm. 2022, 44, 539–547. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Moges, T.A.; Akalu, T.Y.; Sema, F.D. Unintended medication discrepancies and associated factors upon patient admission to the internal medicine wards: Identified through medication reconciliation. BMC Health Serv. Res. 2022, 22, 1251. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Han, A.; Nguyen, N.Y.; Hung, N.; Kamalay, S. Efficacy of a Bariatric Surgery Clinic-Based Pharmacist. Obes. Surg. 2022, 32, 2618–2624. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Naseralallah, L.; Koraysh, S.; Alasmar, M.; Aboujabal, B. The role of pharmacists in mitigating medication errors in the perioperative setting: A systematic review. Syst. Rev. 2025, 14, 12. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ciudad-Gutiérrez, P.; Del Valle-Moreno, P.; Lora-Escobar, S.J.; Guisado-Gil, A.B.; Alfaro-Lara, E.R. Electronic Medication Reconciliation Tools Aimed at Healthcare Professionals to Support Medication Reconciliation: A Systematic Review. J. Med. Syst. 2023, 48, 2. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Plaisant, C.; Wu, J.; Hettinger, A.Z.; Powsner, S.; Shneiderman, B. Novel user interface design for medication reconciliation: An evaluation of Twinlist. J. Am. Med. Inform. Assoc. 2015, 22, 340–349. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Marien, S.; Legrand, D.; Ramdoyal, R.; Nsenga, J.; Ospina, G.; Ramon, V.; Spinewine, A. A User-Centered design and usability testing of a web-based medication reconciliation application integrated in an eHealth network. Int. J. Med. Inform. 2019, 126, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Gionfriddo, M.R.; Hu, Y.; Maddineni, B.; Kern, M.; Hayduk, V.; Kaledas, W.R.; Elder, N.; Border, J.; Frusciante, K.; Kobylinski, M.; et al. Evaluation of a Web-Based Medication Reconciliation Application Within a Primary Care Setting: Cluster-Randomized Controlled Trial. JMIR Form. Res. 2022, 6, e33488. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Characteristics | Intervention Group n = 73 |
|---|---|
| Sex, n (%) | |
| Male | 56 (76.7) |
| Female | 17 (23.3) |
| Age | |
| ≤75 years, n (%) | 36 (49.3) |
| >75 years, n (%) | 37 (50.7) |
| Body mass index, mean ± SD a | 29.3 ± 5.1 |
| Primary tumor location, n (%) | |
| Colon | 61 (83.6) |
| Rectum | 12 (16.4) |
| ASA b physical status classification, n (%) | |
| ASA I | 2 (2.7) |
| ASA II | 22 (30.1) |
| ASA III | 49 (67.1) |
| Polypharmacy, n (%) | 57 (78.1) |
| Diabetes, n (%) | 35 (47.9) |
| Advanced chronic conditions, n (%) | 14 (19.7) |
| Cardiovascular disease | 8 (8.7) |
| Lung disease | 0 (0) |
| Liver disease | 2 (2.7) |
| Kidney disease | 4 (5.5) |
| Hypertension, n (%) | 55 (76.0) |
| Medication discrepancies (n = 56) | Pharmacotherapeutic Groups (n) | “High-Risk” Medications (n) |
| A02. Drugs for acid-related disorders (2) | ||
| A06. Drugs for constipation (4) | ||
| A12. Mineral supplements (1) | ||
| B01. Antithrombotic agents (3) | Acetylsalicylic acid (2) Enoxaparin (1) | |
| B05. Blood substitutes and perfusion solutions (5) | ||
| C03. Diuretics (5) | Furosemide (3) Spironolactone (1) | |
| C05. Vasoprotectives (1) | ||
| C07. Beta blocking agents (4) | Bisoprolol (3) Atenolol (1) | |
| C08. Calcium channel blockers (1) | ||
| C09. Agents acting on the renin-angiotensin system (3) | ||
| C10. Lipid modifying agents (4) | ||
| J01. Antibacterials for systemic use (2) | ||
| M01. Anti-inflamatory and antirheumatic products (2) | Ibuprofen (2) | |
| N02. Analgesics (3) | Tramadol (1) | |
| N05. Psycholeptics (7) | Lorazepam (2) Diazepam (1) Alprazolam (1) Risperidone (1) | |
| N06. Psychoanaleptics (3) | ||
| R03. Drugs for obstructive airway diseases (3) | ||
| R05. Cough and cold preparations (1) | ||
| R06. Antihistamines for systemic use (2) |
| Items Evaluated | Mean Score ± SD 1 [Score: 1–5] | User’s Comments | Next Updates of ConciliaMed |
|---|---|---|---|
| Design and visualisation | 4.28 ± 1.04 | “New professional categories should be included in the tool to be selected during the registration process, for example, community pharmacists” “The FAQs module was useful in enabling direct communication with researchers in order to quickly resolve questions about the tool’s navigation or content” | More professional categories will be added in ConciliaMed according to the demand from healthcare professionals. |
| Organisation and content | 4.45 ± 0.89 | “It is desirable to expand the information about certain drugs which perioperative management recommendations are missing” “The guidelines about perioperative medication management included in the “Documents of interest” module was useful to consult some queries about certain information of medication management” | New sources of information are explored periodically by researchers to provide more information about the perioperative management of medications with limited data, such as monoclonal antibodies or immunosuppressants. |
| Navigation | 4.40 ± 0.91 | “It would be interesting to integrate a scanner into the app to automatically extract the information about the patient medication list from electronic health records” | Automatic data entry into the tool will be evaluated by researchers in the near future. |
| Easy-to-use of the perioperative medication management module | 4.38 ± 0.91 | “It would be necessary to select automatically an individualized perioperative management recommendation in certain medications, for example, DOACs, with a different perioperative management according to the type of surgery or patient risk factors” | A free text option is provided to be completed by healthcare professionals, especially for those medications with high variability in the perioperative management. |
| App usability | 4.31 ± 0.87 | “The development of an iOS version would enhance the rapid spread of the app” | ConciliaMed is developed for Android systems, but all users can also be registered via the web platform. The development of an iOS version will be taken into account by researchers in the next year. |
| Web platform usability | 4.35 ± 0.93 | “It would be helpful for users that the generation of reconciliation reports could be also made through the web platform” | All users will have access to the information included in the “Perioperative medication management” module in the web platform, which was not implemented up to date. The generation of reconciliation reports in the web platform will be explored by researchers in the future according to healthcare professionals’ needs. |
| Global satisfaction | 4.45 ± 0.80 | “It is an easy-to-use and intuitive tool to carry out the MedRec process, especially for those healthcare professionals who are working in the perioperative setting” |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciudad-Gutiérrez, P.; Suárez-Casillas, P.; Guisado-Gil, A.B.; Acosta-García, H.L.; Campano-Pérez, I.L.; Ramírez-Duque, N.; Alfaro-Lara, E.R. Implementation and User Satisfaction Analysis of an Electronic Medication Reconciliation Tool (ConciliaMed) in Patients Undergoing Elective Colorectal Surgery. Healthcare 2025, 13, 778. https://doi.org/10.3390/healthcare13070778
Ciudad-Gutiérrez P, Suárez-Casillas P, Guisado-Gil AB, Acosta-García HL, Campano-Pérez IL, Ramírez-Duque N, Alfaro-Lara ER. Implementation and User Satisfaction Analysis of an Electronic Medication Reconciliation Tool (ConciliaMed) in Patients Undergoing Elective Colorectal Surgery. Healthcare. 2025; 13(7):778. https://doi.org/10.3390/healthcare13070778
Chicago/Turabian StyleCiudad-Gutiérrez, Pablo, Paloma Suárez-Casillas, Ana Belén Guisado-Gil, Héctor Luis Acosta-García, Isabel Laura Campano-Pérez, Nieves Ramírez-Duque, and Eva Rocío Alfaro-Lara. 2025. "Implementation and User Satisfaction Analysis of an Electronic Medication Reconciliation Tool (ConciliaMed) in Patients Undergoing Elective Colorectal Surgery" Healthcare 13, no. 7: 778. https://doi.org/10.3390/healthcare13070778
APA StyleCiudad-Gutiérrez, P., Suárez-Casillas, P., Guisado-Gil, A. B., Acosta-García, H. L., Campano-Pérez, I. L., Ramírez-Duque, N., & Alfaro-Lara, E. R. (2025). Implementation and User Satisfaction Analysis of an Electronic Medication Reconciliation Tool (ConciliaMed) in Patients Undergoing Elective Colorectal Surgery. Healthcare, 13(7), 778. https://doi.org/10.3390/healthcare13070778






