Abstract
Background/Objectives: In recent years, Narrative Medicine (NM) has gained prominence in the context of neurodegenerative diseases, such as dementia, offering tools to understand the subjective experience of illness and to improve the care relationship. Methods: This scoping review, conducted following the PRISMA guidelines, analyzed the scientific literature from PubMed, PsycInfo, Web of Science, and Medline, encompassing 10 contributions focused on NM and patients with dementia or Alzheimer’s disease. Results: The analysis identified three main themes: 1) narrative, memory, and personal identity, highlighting the role of narrative in preserving a sense of self; 2) personalization of care, oriented towards person-centeredness; 3) the use of narrative in a formative and reflective function as a tool to promote empathy, clinical awareness, and observation skills in the training of health professionals. Conclusions: NM confirms itself as a relational and reflexive paradigm, capable of humanizing care and promoting therapeutic pathways that are more inclusive and sensitive to the patient’s subjectivity.
1. Introduction
Narrative Medicine (NM) represents a clinical intervention methodology that considers narrative as a fundamental instrument for comprehending the multiplicity of perspectives involved in a patient’s illness event. This approach encompasses not only the patient’s experience and narrative but also those of caregivers (both formal and informal), healthcare professionals, and other individuals engaged in the person’s care. NM advances clinical practice through the development of narrative competence, which enables practitioners to recognize, interpret, and be moved by stories of illness, thereby supporting physicians, nurses, social workers, and therapists in enhancing the effectiveness of care pathways [1,2,3]. An appropriately collected illness story, including the personal dimensions of the subject, facilitates the formulation and implementation of a more effective, suitable, and collaborative care pathway. The primary objective of applying NM is to construct a personalized care narrative that fosters a therapeutic alliance between the patient (or their family or caregiver) and the healthcare team [4,5,6]. Narrating the illness experience accentuates critical aspects of the patient’s journey, not only as a recollection of the clinical process but also as a resource to enrich the affective, relational, and subjective domains. This methodology emphasizes the importance of communicative and ethical considerations, thereby advancing patient care and facilitating effective dialog with family members and caregivers [7,8]. Consequently, NM emerges as a promising tool for addressing ethical, relational, and care-related challenges associated with various pathologies, as well as for integrating the human dimension into care pathways. It is essential to distinguish NM from therapeutic narrative interventions. While narrative practices within clinical encounters may confer beneficial effects and support patients’ overall well-being, narrative therapy seeks explicitly therapeutic objectives aimed at alleviating psychological distress or mental disorders [9,10]. These objectives significantly diverge from those guiding the management of chronic or neurodegenerative conditions. Therefore, a clear distinction must be made: narrative therapy constitutes a psychotherapeutic intervention with direct clinical aims, whereas NM is a clinical methodology centered on listening, understanding, and integrating patients’ illness narratives into care. Any therapeutic advantages derived from NM should be regarded as secondary or indirect relative to its primary communicative and relational purposes.
Over the past two decades, NM has garnered increasing interest from both the national and international scientific communities, and substantial contributions to its effectiveness in addressing multiple clinical conditions are now documented [11,12,13,14,15,16]. Regarding the older adult population, NM has also demonstrated potential as a beneficial approach [17,18], particularly in the context of dementia and Alzheimer’s disease. Dementia is a chronic, degenerative condition frequently observed in older adults, characterized by a progressive and irreversible decline in functional capacity and autonomy, with significant implications for care and familial relationships [19]. Among various forms of dementia, Alzheimer’s disease is a specific neuropathological condition and represents the most prevalent cause of dementia. The different nosological subtypes of dementia extend beyond short-term memory impairment, involving a gradual and irreversible deterioration of primary cognitive and behavioral functions [20]. Dementia is commonly described as a ‘family’ disease, not solely because of a genetic component, but due to the profound impact it has on the relational dynamics and emotional systems within families [21]. In this context, in addition to pharmacological treatments, it is crucial to implement consistent, effective, and needs-centered communication strategies with family members, who often assume the role of caregivers early in the disease course and become key interlocutors in the care process for individuals with dementia [22].
However, to date, no literature reviews have summarized whether and to what extent NM has been applied in the context of dementia, particularly Alzheimer’s disease. Given the complexity and multidimensional impact of dementia, there is a strong need for methodological tools that can enhance communication, improve care quality, and facilitate the sharing of care pathways. Due to its potential to address the complexity of dementia care, NM emerges as a promising and meaningful approach. Accordingly, we conducted a scoping review with the following objectives: (1) to identify and analyze scientific articles dealing with the application of NM in the care settings of dementia and Alzheimer’s disease; (2) to analyze how NM is cited and used in the selected contributions, assessing its role, function, and impact in clinical and care practices.
2. Materials and Methods
2.1. Study Design
This scoping review was conducted in accordance with the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) guidelines. As this study is a review of previously published literature, ethical approval was not required.
2.2. Research Question and Conceptual Framework
The research question was structured using the PICo framework (Person, Intervention, Concepts, Context): Person (individuals with dementia and Alzheimer’s disease, their caregivers, and health professionals); Intervention (applications of NM approach or tools); Concepts (NM perspectives and co-construction of care narratives); Context (clinical–assistential settings for people with dementia and Alzheimer’s disease).
2.3. Search Strategy
The search was conducted in October 2024 across four databases: PubMed, PsycInfo, Web of Science, and MEDLINE. Search strategies were customized for each database by combining keywords related to ‘dementia’ (dementia OR Alzheimer’s OR cognitive impairment OR memory loss) with keywords related to ‘narrative medicine’ (narrative medicine OR narrative approach OR narrative-based medicine) (Table 1). No time limits were applied to the search, allowing for the inclusion of all relevant publications to date. The search targeted titles and abstracts. Filters were applied to include English-language publications and peer-reviewed or formally published academic sources. In PsycInfo, filters included peer-reviewed journals and the English language, while other publication types (e.g., articles, reviews, case studies, editorials, letters, conference abstracts, book chapters) were included through search strategy design rather than automatic database limits.

Table 1.
Database Search Strategy.
2.4. Eligibility Criteria
A wide range of publication types was considered to ensure a comprehensive overview, including qualitative and quantitative research articles, review articles, case studies, study protocols, brief reports, commentaries, letters, editorials, conference abstracts, posters, and book chapters. Gray literature was excluded because the review focused exclusively on peer-reviewed or formally published academic sources. Publications not available in English were excluded.
2.5. Study Selection
Two researchers independently screened abstracts and retrieved relevant full texts (VC; AM). If abstract information was insufficient, the full text was read. The quality of data extraction was checked by randomly selecting 20% of the abstracts for a second, blinded review by two other researchers (MAV; ACS). Each reviewer classified studies as excluded, eligible, or ambiguous. Eligible or ambiguous full texts were analyzed, with 10% double-checked independently by two reviewers. Discrepancies and disagreements were resolved by discussion. Results were synthesized narratively and supported by tables to map key characteristics and findings across included studies.
2.6. Data Extraction and Synthesis
Data were extracted using a structured form designed to capture key study characteristics and findings. Results were synthesized narratively and supported with tables that mapped methodological features, narrative components, and the primary results reported across included studies.
3. Results
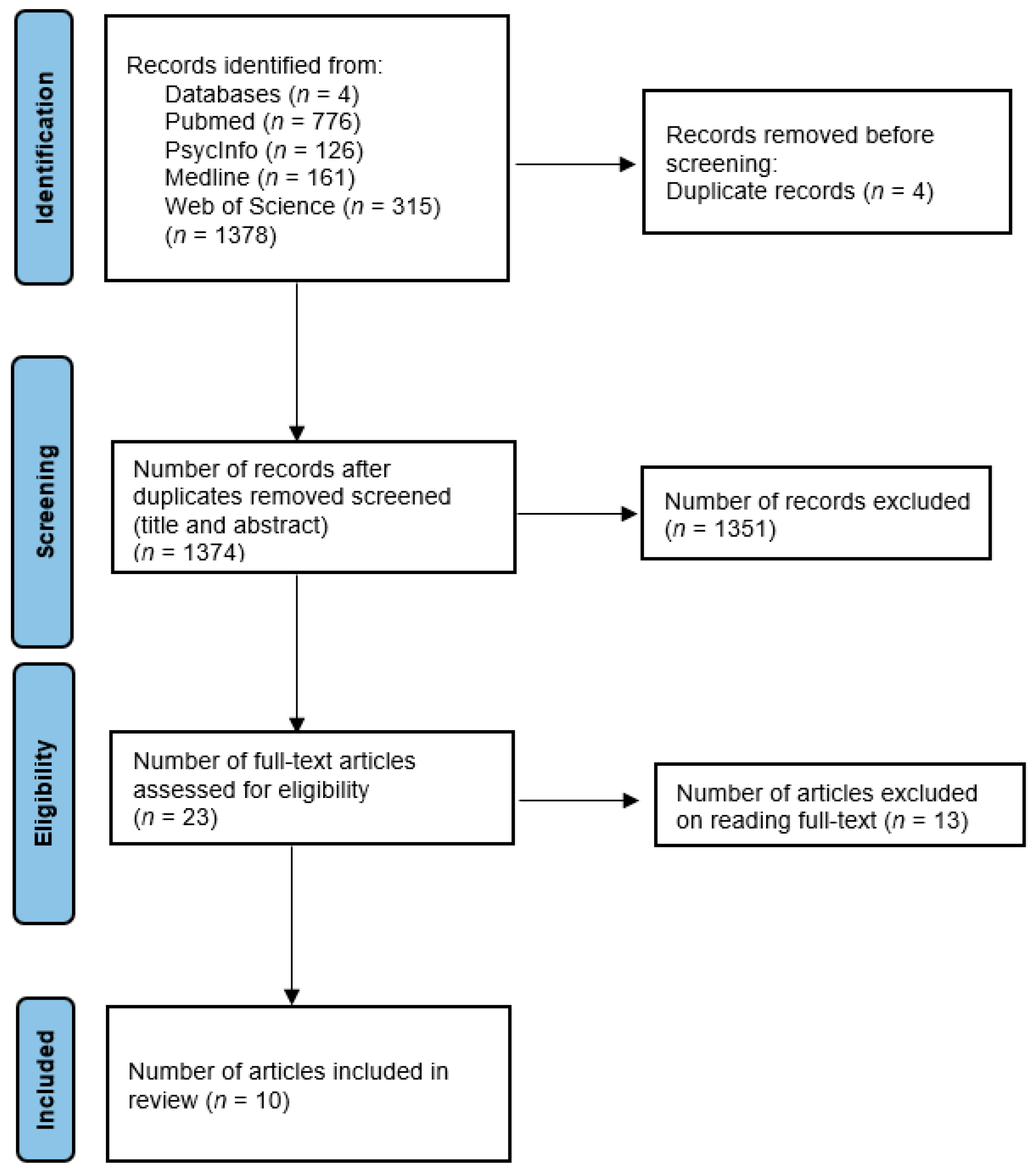
After searching all four bibliometric databases, we identified 1378 records. After duplicates had been removed (N = 4), a total of 1374 records were screened, 23 full texts were read, and 10 studies were included, as shown in Figure 1. Studies were excluded if they were not available or did not address the topic of the present scoping review. A total of 1351 studies were excluded because the keyword “narrative” retrieved numerous literature reviews not directly related to this review’s focus. Additionally, many studies did not address the target population of people with dementia and Alzheimer’s disease. Furthermore, several excluded studies involved narrative approaches unrelated to NM, such as narrative therapy interventions. These exclusion criteria ensured that the review retained only studies specifically addressing the application of NM in the care of people living with dementia, thereby preserving its relevance and focus.
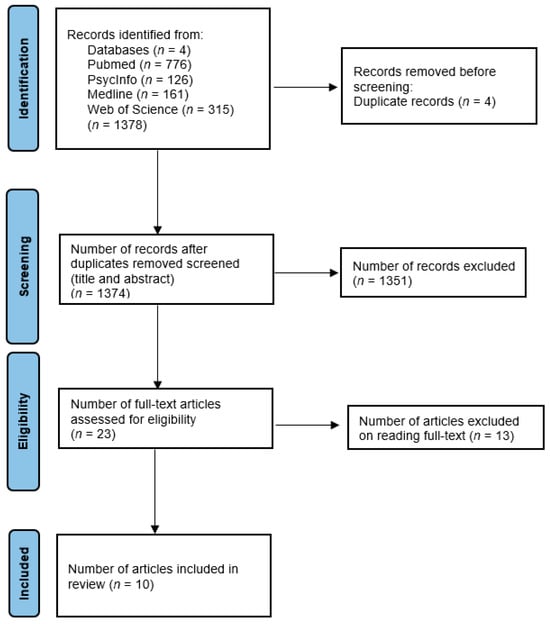
Figure 1.
Flowchart of study selection.
Table 2 delineates the principal characteristics of the studies included and summarizes the application of NM in care environments for individuals with dementia and Alzheimer’s disease. The reviewed literature predominantly originates from the United States [23,24,25,26,27,28], with additional contributions from Italy [29,30], Canada [31], and Poland [32]. The primary focus groups consist of individuals diagnosed with dementia or Alzheimer’s disease, alongside others involved in their care, such as caregivers, family members, and healthcare professionals. In certain instances, the focus also encompasses comorbid conditions such as breast cancer [23] or post-operative cognitive decline [25]. An illustrative example is the educational experience of a medical student engaged in home-based palliative care [24]. Participant data are not consistently available; however, two studies [26,30] report substantial sample sizes. Overall, the participant composition underscores the centrality of the person with dementia while also acknowledging the relational and institutional contexts in which care is administered.

Table 2.
Summary of Studies on Narrative Medicine in Dementia and Alzheimer’s Disease.
Table 3 delineates the application of NM within the retrieved publications, emphasizing its purpose, employed instruments, and resulting outcomes. Several studies explicitly mention NM in their titles, abstracts, or keywords [23,26,30], whereas in other instances, the reference remains implicit or is confined to the introductory sections [27]. Lawrence [23] underscores the therapeutic benefits of group narratives, including the enhancement of empathy, the encouragement of introspection, and the promotion of personal development. Similarly, Cerasoli et al. [29] reported utilizing diaries as narrative tools to monitor neuropsychiatric symptoms in patients with dementia, actively involving caregivers in the process. An innovative approach, as described by Lingler et al. [26], involves the use of culturally adapted narratives aimed at increasing confidence and participation among African American adults in Alzheimer’s research. The study conducted by Puto et al. [32] highlights the role of storytelling in affirming the identity of older adults, thereby augmenting their sense of uniqueness and personal biography. Furthermore, Merrilees [27] integrates oral history techniques with personal narratives to foster dignity, empathy, and social inclusion. Joo, Li, and Whitlock [25] emphasize how the integration of narratives with clinical data facilitates a more profound understanding of postoperative cognitive decline, thereby overcoming the limitations associated with quantitative evidence alone. Tsai [24] offers a formative account that highlights clinical sensitivity towards patients with end-stage Alzheimer’s disease. Solomon and Lawlor [28] investigate ‘wandering’ in individuals with dementia through a phenomenological-narrative approach. Caza [31] underscores the benefits of autobiographical reminiscence. Lastly, Guidi [30] presents a particularly relevant application by illustrating the systematic incorporation of narratives into hospital communication protocols using the Calgary–Cambridge Guide, a tool designed to facilitate effective communication between healthcare professionals and patients.

Table 3.
Narrative Medicine Approaches: Aims, Tools, and Outcomes in Dementia Care Studies.
4. Discussion
The analysis of the selected contributions confirms the growing interest in applying NM to dementia, particularly Alzheimer’s disease. Despite the heterogeneity of contexts, methodologies, and tools, it is possible to identify standard guidelines that enhance narrative as a clinical, educational, and relational resource. The first recurring area concerns the function of illness narrative collection in promoting the patient’s personal identity. In neurodegenerative conditions characterized by the progressive loss of cognitive functions, the possibility of telling one’s own story—or of seeing it said by others—represents a fundamental means of preserving the continuity of the self and the dignity of the individual [31,32]. Narrative practices, in this sense, are not limited to an expressive purpose but take on a therapeutic significance, insofar as they counteract processes of identity disintegration, often accentuated by stigmatization and social isolation [27]. A second interpretative axis is the personalization of care, a theme that is particularly evident in the contributions that apply narrative tools in care pathways. The diary proposed by Cerasoli et al. [29] is a practice that enables accurate assessment of neuropsychiatric symptoms, facilitates identification of triggering factors, and encourages caregivers to be actively involved in the patient’s daily management. In a similar vein, Guidi [30] systematically integrates illness narratives into clinical communication using the Calgary–Cambridge grid, facilitating the co-construction of meaning along the care pathway among caregivers, patients, and family members. The third thematic core concerns the use of narrative in a formative and reflective function, as demonstrated by Tsai’s [24] contribution, which recounts the experience of a medical student involved in a home visit to an Alzheimer’s patient in palliative care. Storytelling becomes a pedagogical tool to promote empathy, clinical awareness, and observation skills in the training of health professionals.
Furthermore, some studies highlight the potential of illness narrative collection to promote equity and inclusion in clinical research, as illustrated by Lingler et al. [26], who demonstrate that culturally adapted narratives can enhance the confidence and participation of African American individuals in Alzheimer’s studies. Such an approach proves crucial in a field like geriatrics, where minority groups are often underrepresented. Finally, contributions such as Lawrence’s [23] and Solomon & Lawlor’s [28] explore deeper, more philosophical dimensions of narrative, highlighting its capacity to foster interpersonal connections, process complex emotional experiences, and offer symbolic resistance to the fragmentation of experience caused by illness.
Despite the points of convergence, the studies differ in their areas of application, methodological tools, and cultural references. Merrilees et al. [27] and Puto et al. [32] valorize oral histories to promote dignity and reduce stigma, while other works, such as those by Tsai [24] and Joo, Li, and Whitlock [25], illustrate the integration of storytelling in home care or post-operative care settings. Finally, some studies explicitly address ethnic–cultural diversity in participation in care [26] and social biases in the management of behavioral symptoms [28].
Overall, the results show how NM, although still poorly systematized in the field of dementia, represents a versatile resource to enhance the quality of care, facilitate communication with caregivers, personalize patient biographies, and support caregivers in their clinical and human roles. However, further empirical research is needed to assess its effectiveness rigorously and to consolidate its integration into care protocols. Despite these promising findings, this review has some limitations. The selected contributions were heterogeneous, lacked formal criteria for assessing methodological quality, and varied in the explicitness of the narrative approach. Additionally, most studies were predominantly descriptive, preventing a systematic analysis of NM’s effectiveness in the examined clinical practices.
Future research should aim to clarify how NM might influence the care process, the health outcomes of adult patients with dementia or Alzheimer’s disease, the caregivers’ experience with care burdens, and communication dynamics among healthcare professionals, patients, and caregivers. There is a growing need for more methodologically rigorous research, such as controlled studies, longitudinal research, and mixed-methods approaches, to evaluate the effectiveness of narrative-based interventions across different stages of dementia and various care settings [33]. Further research should investigate, for example, how the various narrative tools discussed in this review can be incorporated into care pathways for these patients, assessing their feasibility and sustainability in real-world settings. The development of standardized narrative protocols could help incorporate NM into clinical guidelines and dementia care training programs.
5. Conclusions
This review emphasizes that NM offers an innovative, cross-disciplinary approach to dementia care, integrating clinical, relational, and cultural aspects. Despite varied application areas and methodological tools, all contributions acknowledge the importance of illness narratives in enhancing patient well-being, maintaining personal identity, and supporting more ethical, shared decision-making. Listening to individual stories helps reduce ineffective interventions and promotes personalized treatment plans. The ‘care story,’ co-created by patients, caregivers, and the team, serves not only as a clinical tool but also as a means to foster greater humanization, continuity of care, and alignment between expressed needs and therapeutic responses.
Author Contributions
Conceptualization, V.C., M.F. and A.M.; Methodology, V.C., M.F. and A.M.; Data collection and analysis, V.C., A.M. and A.C.S.; Interpretation of results, V.C., A.M. and M.A.V.; writing—original draft preparation, V.C. and M.A.V.; writing—review and editing, V.C. and M.A.V.; supervision, V.C.; funding acquisition, V.C. and M.F. All authors have read and agreed to the published version of the manuscript.
Funding
This literature review is part of the research project entitled “Aesthetics and Therapeia,” supported by the Italian Ministry of University and Research (MUR) under the PRIN 2022 PNRR programme [project code P2022R3X8B; CUP: H53D23009300001].
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviation
The following abbreviation is used in this manuscript:
| NM | Narrative Medicine |
References
- Charon, R. Narrative medicine: A model for empathy, reflection, profession, and trust. JAMA 2001, 286, 1897–1902. [Google Scholar] [CrossRef]
- Milota, M.M.; Van Thiel, G.J.; Van Delden, J.J. Narrative medicine as a medical education tool: A systematic review. Med. Teach. 2019, 41, 802–810. [Google Scholar]
- Kirmayer, L.J.; Gómez-Carrillo, A.; Sukhanova, E.; Garrido, E. Narrative Medicine. In Person Centered Medicine; Springer: Cham, Switzerland, 2023. [Google Scholar] [CrossRef]
- Greenhalgh, T. Patient and public involvement in chronic illness: Beyond the expert patient. BMJ 2009, 338, b49. [Google Scholar] [CrossRef] [PubMed]
- Zaharias, G. What is narrative-based medicine?: Narrative-based medicine 1. Can. Fam. Physician 2018, 64, 176–180. [Google Scholar]
- Marini, M.G. Narrative Medicine. In Bridging the Gap Between Evidence-Based Care and Medical Humanities; Springer: Cham, Switzerland, 2016. [Google Scholar]
- Testa, M.; Cappuccio, A.; Latella, M.; Napolitano, S.; Milli, M.; Volpe, M.; Marini, M.G.; TRUST Participants. The emotional and social burden of heart failure: Integrating physicians’, patients’, and caregivers’ perspectives through narrative medicine. BMC Cardiovasc. Disord. 2020, 20, 522. [Google Scholar] [CrossRef] [PubMed]
- Tonini, M.C.; Fiorencis, A.; Iannacchero, R.; Zampolini, M.; Cappuccio, A.; Raddino, R.; Grillo, E.; Albanese, M.; Allais, G.; Bassano, M.A.; et al. Narrative Medicine to integrate patients’, caregivers’ and clinicians’ migraine experiences: The DRONE multicentre project. Neurol. Sci. 2021, 42, 5277–5288. [Google Scholar] [CrossRef]
- Wallis, J.; Burns, J.; Capdevila, R. What Is Narrative Therapy and What Is It Not? The Usefulness of Q Methodology to Explore Accounts of White and Epston’s (1990) Approach to Narrative Therapy. Clin. Psychol. Psychother. 2011, 18, 486–497. [Google Scholar] [CrossRef] [PubMed]
- CNMR (Centro Nazionale Malattie Rare). Conferenza Linee di Indirizzo per l’Utilizzo della Medicina Narrativa in Ambito Clinico-Assistenziale, per le Malattie Rare e Cronico-Degenerative (Conference Guidelines for the Use of Narrative Medicine in Clinical and Care Settings for Rare and Chronic Degenerative Diseases); Collana ‘I Quaderni di Medicina’ de Il Sole24Ore Sanità: Rome, Italy, 2015. [Google Scholar]
- Fioretti, C.; Mazzocco, K.; Riva, S.; Oliveri, S.; Masiero, M.; Pravettoni, G. Research studies on patients’ illness experience using the Narrative Medicine approach: A systematic review. BMJ Open 2016, 6, e011220. [Google Scholar] [CrossRef]
- Palla, G.; Turchetti, S.; Polvani, S. Narrative Medicine: Theory, clinical practice and education—A scoping review. BMC Health Serv. Res. 2024, 24, 1116. [Google Scholar] [CrossRef]
- Cepeda, M.S.; Chapman, C.R.; Miranda, N.; Sanchez, R.; Rodriguez, C.H.; Restrepo, A.E.; Ferrer, L.M.; Linares, R.A.; Carr, D.B. Emotional disclosure through patient narrative may improve pain and wellbeing: Results of a randomized controlled trial in patients with cancer pain. J. Pain Symptom Manag. 2008, 35, 623–631. [Google Scholar] [CrossRef]
- Banfi, P.; Cappuccio, A.; Latella, M.E.; Reale, L.; Muscianisi, E.; Marini, M.G. Narrative medicine to improve the management and quality of life of patients with COPD: The first experience applying parallel chart in Italy. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 287–297. [Google Scholar] [CrossRef] [PubMed]
- Cercato, M.C.; Colella, E.; Fabi, A.; Bertazzi, I.; Giardina, B.G.; Di Ridolfi, P.; Mondati, M.; Petitti, P.; Bigiarini, L.; Scarinci, V.; et al. Narrative medicine: Feasibility of a digital narrative diary application in oncology. J. Int. Med. Res. 2022, 50, 03000605211045507. [Google Scholar] [CrossRef] [PubMed]
- Covelli, V.; Figini, L.; Santagelo, A.; Memini, F.; Bonforte, G. A narrative medicine pilot study using the McGill Illness Narrative Interview (MINI) with patients suffering from nephropathy and on dialysis. J. Soc. Sci. Humanit. 2019, 2, 62–65. [Google Scholar]
- Cenci, C. Narrative medicine and the personalisation of treatment for elderly patients. Eur. J. Intern. Med. 2016, 32, 22–25. [Google Scholar] [CrossRef]
- Covelli, V. Importance of narrative medicine to elderly patients (L’importanza della medicina narrativa con il paziente anziano). Ric. Di Psicol. 2018, 41, 77–90. [Google Scholar] [CrossRef]
- Bhattacharyya, K.K. Aging and Dementia. In Rethinking the Aging Transition; Springer: Cham, Switzerland, 2021. [Google Scholar] [CrossRef]
- Tampi, R.R.; Jeste, D.V. Dementia is more than memory loss: Neuropsychiatric symptoms of dementia and their nonpharmacological and pharmacological management. Am. J. Psychiatry 2022, 179, 528–543. [Google Scholar] [CrossRef]
- Taddei, R.N.; Cankaya, S.; Dhaliwal, S.; Chaudhuri, K. Management of psychosis in Parkinson’s disease: Emphasizing clinical subtypes and pathophysiological mechanisms of the condition. Park. Dis. 2017, 2017, 3256542. [Google Scholar] [CrossRef]
- Goto, Y.; Morita, K.; Suematsu, M.; Imaizumi, T.; Suzuki, Y. Caregiver burdens, health risks, coping and interventions among caregivers of dementia patients: A review of the literature. Intern. Med. 2023, 62, 3277–3282. [Google Scholar] [CrossRef]
- Lawrence, L.S. The group, the photograph, the wound, and the writing: How a social worker uses narrative medicine to facilitate groups. Smith Coll. Stud. Soc. Work. 2016, 86, 45–57. [Google Scholar] [CrossRef]
- Tsai, J. The Forgotten. Am. J. Hosp. Palliat. Med. 2019, 36, 1155–1156. [Google Scholar] [CrossRef]
- Joo, H.; Li, L.Y.; Whitlock, E.L. Long-term cognitive outcomes after surgery and anesthesia: What we find depends on where we look. Curr. Anesthesiol. Rep. 2024, 14, 8–14. [Google Scholar] [CrossRef]
- Lingler, J.H.; Ren, D.; Tamres, L.K.; Knox, M.L.; Mbawuike, U.; Williams, I.C.; Robinson, R.A.S.; Cameron, J.L.; Terry, M.H.; Garrett, M. Mechanisms by which cultural-centric narrative influences interest in ADRD research among African American adults. Gerontologist 2023, 63, 1060–1066. [Google Scholar] [CrossRef]
- Merrilees, J.; Mayotte, C.; Vong, E.; Matice, M.; Prioleau, C. Using personal narrative to promote person-centered values in aging, dementia, and caregiving. Front. Neurol. 2023, 14, 1167895. [Google Scholar] [CrossRef]
- Solomon, O.; Lawlor, M.C. Beyond V40.31: Narrative phenomenology of wandering in autism and dementia. Cult. Med. Psychiatry 2018, 42, 206–243. [Google Scholar] [CrossRef] [PubMed]
- Cerasoli, B.; Canevelli, M.; Vellucci, L.; Rossi, P.D.; Bruno, G.; Cesari, M. Adopting a diary to support an ecological assessment of neuropsychiatric symptoms of dementia. J. Nutr. Health Aging 2019, 23, 614–616. [Google Scholar] [CrossRef] [PubMed]
- Medicina Narrativa e Paziente Geriatrico con Demenza: Una Nuova Frontiera (Narrative Medicine and Geriatric Patients with Dementia: A New Frontier). Available online: https://www.seres-odv.it/riviste%20menti%20attive/2019/Rivista%20n1%202019%20v3.pdf (accessed on 1 November 2025).
- Caza, N. Se souvenir pour mieux vieillir. Gériatrie Psychol. Neuropsychiatr. Du Vieil. 2013, 11, 82–86. [Google Scholar] [CrossRef]
- Puto, G.; Zurzycka, P.; Musiał, Z.; Muszalik, M. Narrative in older people care—Concepts and issues in patients with dementia. Healthcare 2022, 10, 889. [Google Scholar] [CrossRef] [PubMed]
- Covelli, V. Medicina Narrativa e Ricerca. Riflessioni Teorico-Metodologiche per la Raccolta e l’Analisi delle Narrazioni (Narrative Medicine and Research. Theoretical-Methodological Reflections for the Collection and Analysis of Narratives); Libellula Edizioni: Bari, Italy, 2017. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).