Abstract
Background: Providing complex care and support for people with technology dependence (PwTD) is challenging, even under routine conditions. During disasters, when health and power infrastructure are disrupted, the complex care of PwTD must be maintained under extreme conditions. This research aims to summarize the specific needs of PwTD in disasters and to describe how these needs are addressed in real-life events. Methods: We conducted a scoping review, searching four databases (CINAHL, MEDLINE, PsycInfo, SocINDEX) and the websites of relevant disaster relief organizations. A total of 43 of 2625 screened records were included. Content analysis was used to identify and cluster the needs of PwTD and the response to these needs. Results: Case reports were the most reported types of literature. It was repeatedly stated that PwTD have complex care needs that are often difficult to meet in disaster situations. The review identified three interdependent clusters of needs: clinical and supportive care needs, aids and supply needs, and access needs. The needs of patients and relatives were, as far as the situation allowed, met in accordance with existing plans and guidelines and, where these were found to be inadequate, through creative solutions devised by frontline nurses. Conclusions: We conclude that addressing the complex care needs of PwTD in disasters requires a strategy integrating structural preparedness, professional adaptability, and user participation. Nurses could play a key role in developing and implementing such strategies. This review provides a starting point to develop a more practice-oriented research agenda to achieve inclusive disaster risk management.
1. Introduction
People with technology dependence (PwTD) form a relatively small but diverse and challenging group of healthcare users. According to Brenner, et al. [1], technology dependence refers to “a wide range of clinical technology to support biological functioning across a dependency continuum, for a range of clinical conditions. They are initiated within a complex biopsychosocial context and have wide ranging sequelae for the child and family and health and social care delivery.” Other definitions, such as that of Spratling [2], highlight that “the terms technology and complex care should be included in the terminology and/or definition of all studies on children and adolescents who require technology”. Technology dependence can result from genetic and congenital disorders, complications related to prematurity and perinatal trauma, progressive illnesses like renal failure, neoplasia, and degenerative neurological conditions, as well as accidents [1]. Dependence can range from medical–technical support for respiration, cardiac function, nutrition, or dialysis to assistive devices for speech, vision, hearing, and mobility. The degree of dependence varies considerably and can extend from intermittent use of a single device to continuous dependence on multiple assistive devices over longer periods [1,2,3]. In general, PwTD rely on these technologies and assistive devices to sustain life and maintain independence.
Due to increased life expectancy and the growing availability and wider use of medical technology, the population of PwTD is growing [4]. Although the total number of this user group is difficult to determine and data on PwTD is not systematically recorded [5,6], trends in the literature suggest substantial growth [7,8]. For instance, an estimate of 2.6 million people worldwide received kidney replacement therapy in 2010, a number projected to increase to 5.4 million by 2030 due to population growth, improved survival of end-stage kidney disease, and better access to dialysis [8]. Overall trends show an estimation of 900 million people worldwide using assistive devices, excluding spectacles, with projections rising to 1.3 billion by 2050 [4].
PwTD have complex care needs encompassing clinical, psychosocial, and educational aspects. According to Spratling [2] complex care is a defining characteristic of the population of PwTD and “is associated with a high level of skilled nursing care”. Clinical needs include wound and line care, administration of medication (e.g., IV-therapy), suction management and oxygen therapy, clinical monitoring, and nutritional support [9]. Psychosocial needs concern the prevention or treatment of anxiety, depression, and post-traumatic stress disorder [1], as well as mitigating emotional and social burdens for family caregivers [10,11]. Education and information needs relate to managing medical technology [12], specific health conditions (e.g., renal failure), and self-management of care [13]. These overlapping needs illustrate the inherent complexity of care for PwTD, where clinical management, psychosocial stability, and patient education are tightly interrelated Comorbidities that are either related to the underlying cause of technology dependence or have other causes, as well as the variability and instability of the patients’ health and the associated uncertainty for all involved, add further complexity to the care situation [3,14].
Meeting these complex needs requires coordination across multiple care settings and professions. There are various professional groups that take on this coordination task, including doctors, paramedics, social workers and nurses [15]. The latter are considered particularly important because reliance on skilled nursing care is closely related to the complexity of care needs of PwTD [2]. Nurses are found across various health services. These services include all forms of home care such as home and community-based services (HCBS), hospital-at-home, and advanced home care, which allow PwTD to receive complex care in their own home [16]. Settings also include long-term care facilities and hospitals, as well as specialized care centers like dialysis centers or weaning facilities [13,16,17,18,19]. In all these settings, nurses from multiple specialties (e.g., nephrology, pneumology, neurology, intensive care) provide essential care, which may involve continuous monitoring depending on the severity of the health condition [2,20]. While PwTD need regular consultations with other healthcare professionals [9], such as specialized physicians, physical, occupational, and speech therapists, and social workers [21,22], nurses function as care coordinators or support other professions such as social workers in the interdisciplinary care coordination team, ensuring continuity of care for PwTD and supporting their families [15,23,24].
Even under everyday conditions, providing comprehensive care for PwTD places high demands on the care system and the service providers, which cannot always be met. As a result, PwTD often disproportionately experience access barriers and unmet needs compared to the general population [25]. Patient care is often inadequate and lacks a focus on results; safety issues are commonplace [20,26,27,28]. For example, PwTD often struggle to access nurses with specialized qualifications about their specific needs [29] and report availability and transportation barriers to healthcare [30,31]. Additionally, their families experience caregiver burden, especially when skilled care cannot be provided 24 h, PwTD living at home rely on family or informal caregivers [32].
These pre-existing challenges indicate that even under stable conditions, the care of PwTD is fragile, making it particularly vulnerable to disruption during disasters. As stated by the United Nations Office for Disaster Risk Reduction (UNDRR) a disaster constitutes a “serious disruption of the functioning of a community or a society at any scale due to hazardous events interacting with conditions of exposure, vulnerability and capacity, leading to one or more of the following: human, material, economic and environmental losses and impacts” [33]. They affect healthcare services and create cascading effects [34], including staff shortages when personnel are unable or unwilling to work [35], disruptions in power supply and medication or equipment supply chains [36,37], and facility evacuations or prolonged sheltering with limited resources [38,39]. Damaged or blocked roads can restrict access to care sites [40,41]. Some care sites may have been destroyed and others overwhelmed by patient surges [42]. Consequently, disasters pose particular challenges for care providers to maintain care for PwTD and adequately address their complex care needs under exceptional circumstances.
These challenges in providing continuous and needs-based care for PwTD during disasters have already been discussed in the literature [37,43,44,45]. Various guidelines state how this issue should be addressed [46,47,48,49,50] and what nursing competencies might be needed to maintain care during disasters [51]. However, only real-life disaster experiences can reveal which plans are actually feasible in practice and what other options are available to meet the complex needs of PwTD if the existing plans fall short. So far, no comprehensive overview exists outlining the evidence on specific care needs of PwTD during disasters, the resulting healthcare requirements arising from these needs, and how they are addressed under exceptional circumstances during real-life disaster conditions. Therefore, the aim of this study is twofold: (1) to identify the specific care needs of PwTD, the response to which is of existential importance to them, and (2) to describe how these specific care needs can be met even under exceptional circumstances. The results can inform more inclusive disaster management—taking into account the complex care needs of PwTD, supplement existing guidelines and disaster plans—and provide nurses with information on how to meet these specific needs creatively, even under extreme conditions.
2. Materials and Methods
2.1. Study Design
To achieve these aims, we used a scoping review methodology in accordance with the PRISMA-ScR guidelines and the methods recommended in the JBI Manual for Evidence Synthesis [52,53]. No protocol was preregistered due to the iterative and exploratory nature of this scoping review. Given the diversity of PwTD populations and disaster contexts, a scoping review is particularly suited to mapping the breadth of available knowledge and identify gaps.
2.2. Search Strategy
To identify peer-reviewed literature, we searched four relevant databases (MEDLINE, CINAHL, PsycInfo, SocINDEX) between November and December 2024. Terms commonly used to describe PwTD and their care in disasters were used to formulate search terms. For instance, as complex care for PwTD in literature is described to be closely related to skilled nursing care [2], this term was added to the concept of complex care needs. The search string was oriented on the PCC (population, concept, context) scheme [53] and combined Medical Subject Headings (MeSH 2022) with additional keywords in titles and abstracts (see Table 1 and Table A2). We adapted the search string for each database accordingly.

Table 1.
Search strategy with keywords and MeSH terms for Medline.
To capture relevant grey literature, we conducted a hand search in the reference lists of relevant publications as well as targeted searches on the websites of international disaster relief and humanitarian organizations such as the International Federation of Red Cross and Red Crescent Societies (IFRC), United Nations Office for Disaster Risk Reduction (UNDRR), and the Sphere Project for standards in humanitarian care [54] using terms from the original search string.
2.3. Eligibility Criteria
Publications were eligible if the full text was available in English or German and if they were either a peer-reviewed journal article, an empirical paper, or a report from a government agency or non-governmental organization (NGO). We restricted inclusion to publications after 2001 since the attention on the topic and research increased following the terror attacks on 11 September 2001.
We excluded publications if they were not set in a disaster context, did not address people with technology dependence, or did not provide information on the needs of PwTD. There were no restrictions on the quality of research. Editorials, blogs, letters, press releases, opinions, and commentaries, as well as systematic syntheses of evidence, including guidelines, were excluded as sources. However, the references of relevant systematic evidence syntheses were hand-searched for eligible studies.
2.4. Selection Process
After duplicate removal, two independent reviewers (AP, JB) screened titles and abstracts against the predefined inclusion and exclusion criteria, using agreed operational definitions for key concepts (e.g., “people with technology dependence”, “needs”). Full texts of records meeting initial criteria were acquired for further screening for eligibility independently by two researchers (AP, JB) with a focus on needs and challenges in care provision in the context of disasters. Conflicts in the eligibility decisions were discussed and resolved by a third researcher (MK).
2.5. Data Extraction and Synthesis
Two researchers (AP, JB) independently extracted data using an iterative process, according to the recommendations of Pollock et al. [55], and organized the information in a data extraction matrix, which included author (s), study design, country, and information on the population, use of assistive technology, type of disasters, and specific needs. To better analyze in which conditions the needs of people with technology dependence are met in disasters, we extracted context factors (e.g., care setting, attending care workers).
We applied a basic content analysis [55] to synthesize the extracted information. A deductive–inductive approach was used, utilizing the data extraction matrix as an initial framework and open coding the needs and identifying overarching clusters.
3. Results
3.1. Study Selection
Initially, the search yielded 3075 records. After removing duplicates and screening titles, keywords, and abstracts, 2450 records were excluded. Of the 168 full-text records retrieved, 125 were excluded for not meeting eligibility criteria. A total of 43 sources met the inclusion criteria, e.g., Table A1. The selection process is shown in Figure 1.
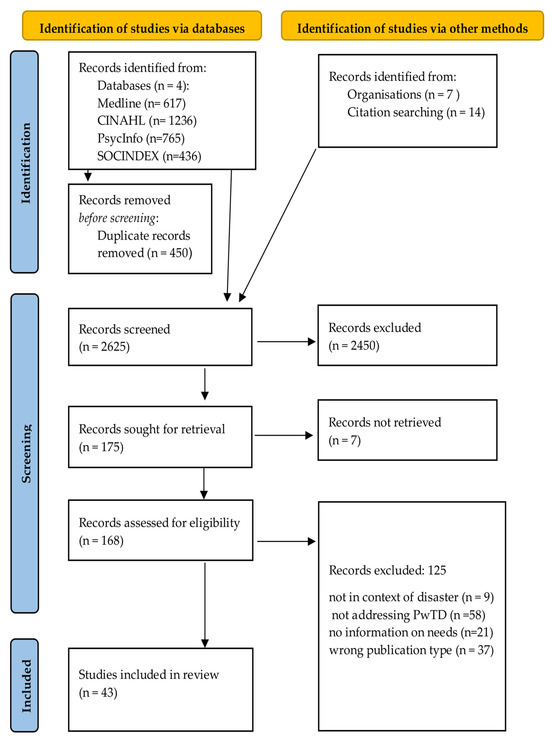
Figure 1.
PRISMA flowchart for the selection of records.
3.2. Identified Clusters of Needs of PwTDs and How They Were Addressed During Disasters
Across the included studies, we identified three overarching clusters of care needs, the response to which is of existential importance for PwTD: “clinical and supportive care needs”, “aids and supply needs”, and “access needs”. Each cluster contained distinct needs, as illustrated in Figure 2. Within these clusters, we synthesized the needs described in each case and how these needs were specifically addressed during disasters based on empirical evidence.
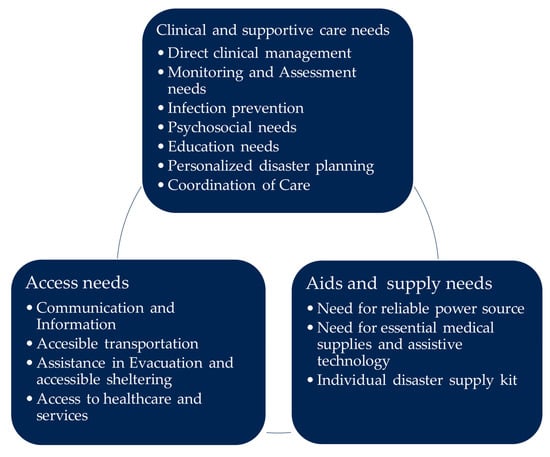
Figure 2.
Clusters of the needs of PwTD in disasters.
3.2.1. Clinical and Supportive Care Needs
Direct Clinical Management
Direct clinical management is a high priority for PwTD, encompassing strict medication, therapy, and dietary regimens [56,57,58,59,60,61] and routine clinical procedures like wound and line care, catheter management, and suction and oxygen management [62,63,64]. To address these clinical needs in disaster conditions, healthcare professionals were forced to adapt care provision to the available resources. These adaptations included changing continuous feeding with a pump to gravity flow or bolus feeding, maintaining ventilation with mechanical mask ventilation, or standardizing dialysis orders when individual prescriptions are unavailable [57,65]. For example, during hurricane Sandy, when specific formula was unavailable, a healthcare professional with expertise in enteral nutrition adapted an adult prescription using available infant nutrition and mixing instructions to meet adult calorie and protein requirements [66]. However, systemic challenges remained, as emergency food failed to meet dietary needs regarding dysphagia or other restrictions (specific nutrition formula and allergies) [56,61]. A lack of expertise and resources in disaster management organizations also compromised the safety of chronic wound care and other ongoing clinical interventions in the response and recovery phase [56,63,67].
Monitoring and Assessment Needs
Monitoring and assessment are essential for early detection of health deterioration of PwTD to enable immediate intervention, particularly given the instability of their health, regardless of whether they are in a care facility [57,68] or in a disaster shelter [69]. Disaster responses included initial screening by nurses to identify PwTD and assess their immediate care needs, health status, and functional ability [61,68]. In the case of particularly unstable PwTD, like preterm infants, expert monitoring of vital parameters by neonatal nurses was required, for example [57].
Infection Prevention
The crowded conditions in shelters combined with heightened susceptibility of PwTD and equipment contamination risks create a pressing need for infection prevention measures [70,71,72,73,74]. To respond to this need, measures included regular screening for infections, grouping symptomatic PwTD into cohorts [71,72,73,75,76], disinfecting assistive devices and contaminated equipment [65,74], and ensuring hygienic sheltering facilities [56].
Education Needs
PwTD and their families have information and education needs that are not always met by public disaster information [80]. These specific needs concern self-management and self-assessment of their health and the operation of assistive devices before, during, and after disasters [65,67,70,81]. In practice, the response to these information and education needs was often spontaneous, arising from the immediate challenges of the disaster context. Nurses and other providers were forced to provide targeted education in shelters and provisional care facilities, for instance, on non-dialytic management of end-stage kidney disease [73,75] and the use of alternative feeding methods (bolus, gravity bags) [66]. Educational topics also included the role of comorbidities in pandemics [71] and general disaster preparedness [65,82].
Personalized Disaster Planning
Personalized disaster and evacuation planning was recognized as a specific need for PwTD, as generic approaches are often insufficient for their individual requirements [57,59,83]. According to existing guidelines, individualized disaster plans should therefore be developed in anticipation of events with the support of nurses and other care providers [82,84]. However, evidence revealed gaps in such plans, often uncovered during real events or drills [85]. For instance, a cross-sectional study reported that PwTD and their families planned to go to the hospital in case of power failure but also reported that this plan was unlikely to work due to hospital lockdown and public transportation failure during an event [86].
Coordination of Care
Finally, the care provision attending to various needs must be coordinated to ensure safety and healthy recovery after the event. This includes coordinating essential services (e.g., dialysis) between shelters and alternative care facilities [87]. Evidence from case studies [60,75,87] and a prospective analysis [22] suggest that nurse-led coordination could be an effective response for improving care provision and recovery.
3.2.2. Aids Supply Needs
Reliable Power Sources
PwTD depend on reliable, continuous power sources to operate their assistive technology—a need that becomes more critical during indefinite power outages common in disasters [37,60,63,65,81,86]. Documented solutions to meet this need include the provision of diesel generators in specialized facilities [65,75], backup batteries provided by facilities or stockpiled in emergency kits [57], and rapid repairs by technical personnel [62,75]. For instance, nurses delivered back-up batteries for people relying on home parenteral nutrition (HPN) when devices could not be charged during hurricane Sandy [66].
Essential Medical Supplies and Assistive Technology
In addition, PwTD need essential medical supplies and assistive technology, including clean water, consumable food (e.g., nutrition formula), medical oxygen [59,62,65,85,88], and medication and assistive device replacement [58,64]. This need is exacerbated by disaster-related logistical challenges, such as the short shelf life and refrigeration requirements of many supplies, and the difficulty of sterilizing equipment for reuse. In response, creative adaptations documented in the literature include healthcare providers supporting PwTD and their families to stockpile supplies, using simple glucose solutions as emergency sustenance, and even improvising with sterilization equipment from a tattoo parlor [59,77].
Individual Disaster Supply Kit
In order to compensate for the indefinite disruption of supply chains for specialized equipment and consumables, PwTD also need individualized disaster supply kits [57,65,80,85]. The reported response to this need was inconsistent. Nurses in some healthcare facilities had packed and distributed kits or backpacks tailored for individual PwTD [65,85]. However, a study interviewing PwTD living at home found that, apart from a stockpile of medication, no emergency kit was available for them [77]. Nurses compensated for the lack of individualized disaster kits by adapting care to standardized prescriptions [65] or using available substitutions fitting individual needs [59,66].
3.2.3. Access Needs
Access to vital information and communication between providers, disaster management, and PwTD are essential. Adequate and accessible transportation, evacuation and sheltering, and access to essential healthcare services are also crucial in maintaining care for PwTD in disasters.
Communication and Information
Effective communication and access to reliable information are essential to maintain care for and independence of PwTD in disasters. PwTD need communication and information pathways to access care and make informed decisions during disasters [60,75,81,89,90]. These needs include maintaining communication with providers, receiving information on the availability of services [56,91], and overcoming disruptions to medical records and alarm systems that hinder care delivery [17,65,84]. In disaster response, emergency information cards were used containing information about medications, allergies, dialysis or nutrition prescriptions, emergency contacts, care providers, and medical history [58,59,60,75]. Physical records of care coordination also proved to be helpful in maintaining care when digital systems failed and data was lost [22].
Accessible Transportation
Beyond communication challenges, PwTD face access barriers related to transportation during disasters. Therefore, a critical need identified for PwTD during disasters is accessible transportation to reach shelters and alternate care sites [17,40,92] and for their home care nurses to reach them reliably. In disaster response, nurses adapted their schedules to account for long fuel lines and blocked roads, transported critical supplies themselves [66], and improvised transportation solutions, such as creating thermoregulated infant transport devices using blankets and plastic wrap material [57].
Evacuation and Accessible Sheltering
Additional access needs arise when PwTD have to evacuate or find appropriate shelter. PwTD need more time and assistance when forced to evacuate, and general population shelters often lack necessary accommodation for complex care needs [56,74,92,93,94]. Based on the literature, PwTD benefited from early evacuation due to their heightened vulnerability to service disruptions and power failures [40,75,84,94,95]. In disaster response, nurses and healthcare providers encouraged PwTD’s early evacuation and assisted them when care facilities were evacuated [57,66]. In some cases, specialized shelters for PwTD were established, providing reliable power, refrigeration, oxygen, and private care spaces and specialized nursing care [68,81,93]. Several sources highlight that these shelters were particularly useful when they took in not only PwTD but also their primary home care nurse or other familiar caregivers. This made it possible to maintain individualized care and relieve the burden on nurses responsible for the people in these shelters [56,68].
Access to Healthcare and Services
Finally, overall access to essential healthcare services might be compromised during disasters. Even in disaster situations, PwTD require continuity of care and unimpeded access to their essential healthcare contacts [70,79], including dialysis [60], home nursing [17,66], maintenance and repair of assistive devices [70,74], or emergency services if their condition deteriorates [37,90]. Their routine healthcare contacts might not be available during an event due to destroyed facilities, staff shortages, or face high patient surges [65]. Response strategies implemented by nurses included referring PwTD to outpatient dialysis facilities that operated during disasters [84], delivering care on adjusted schedules if they sheltered in place [66], or providing care in designated emergency shelters [67].
4. Discussion
This review set out to explore the specific care needs of PwTD in disasters and to describe how these needs can be met even under exceptional circumstances. The synthesis of the literature documents the range and complexity of these needs of PwTD, clustered in the areas of “clinical and supportive care”, “aids supply”, and “access to care”. The included sources mentioned numerous disaster scenarios in which formal guidelines and existing disaster plans for addressing these needs were inadequate or could only be implemented partially in practice. At the same time, however, they outlined how these challenges were overcome to meet the complex care needs of PwTD during disasters.
Developing disaster care guidelines and preparedness plans that are tailored for answering the complex care needs not only for PwTD but for the broad spectrum of so-called CMIST populations (communication, maintaining health, independence, support, safety and self-determination, transportation) with functional impairments and access problems [48,96] is of utmost importance. They are an essential first step towards a more inclusive disaster risk management and emergency response system, as has been called for by the United Nations and other international organizations for some time [50,97,98]. However, our analysis of the literature has shown that developing such inclusive disaster care guidelines and preparedness plans alone is insufficient. They must also be regularly tested, evaluated, and implemented in ways that reflect the realities of disasters. For instance, although existing guidelines propose measures like individualized stockpiles or emergency kits [47] and specialized shelter facilities for PwTD and others within a needs-based framework [48], the included studies indicate that these are only partially realized [85]. Evidence suggests that PwTD in home care settings tend to have less comprehensive stockpiles and supplies in alternate care sites do not match individual prescriptions [59,77]. Similarly, reports from real-life events point to challenges with screening and the provision of specialized sheltering, which can result in PwTD being housed in general shelters without appropriate facilities and personnel [56]. Although some countries have begun expanding civil protection and disaster control to individuals with complex care needs [48,81], their implementation and evaluation still seem to receive little attention. In addition, it would be appropriate to place greater emphasis on these guidelines and planning processes to ensure that people with complex problems are increasingly accommodated and cared for in community-based and home settings. As the literature shows, the prevailing conditions in these settings in the event of a disaster prove to be particularly challenging, which is why protecting those in need of complex care in their homes and communities deserves special attention in this endeavor.
When disaster response guidelines and emergency plans fell short and gaps in the care of PwTD emerged in disaster situations, these were often filled by spontaneous or improvised measures taken by qualified and experienced nurses [57,65]. For instance, nurses across settings used their expertise to improvise solutions when information or supplies were insufficient [66]. In other cases, nurses with clinical expertise were able to ensure patient safety even in unusual locations when their health deteriorated suddenly and evacuation was not possible, or no other care options were available [87]. This observed capacity for improvisation and immediate action appears to align with the core competencies of disaster nursing [51], emphasizing flexibility and decision making under constrained conditions. However, creativity must never go so far as to jeopardize the safety and health of the nurses themselves or the persons entrusted to their care. Differing from recommended care protocols should be a last resort and guided by ensuring quality of care and patient safety despite dire conditions. Frameworks regarding the standards of care in crisis and disasters could help to inform such efforts [99]. In order to identify risks for themselves or other helpers, the patients, and their relatives and to be able to control or avert these risks proactively, nurses require sound medical and nursing knowledge, sufficient clinical experience, and a high degree of professionalism [67]. This is even more important given that nurses in emergency and disaster care often have to respond spontaneously to unpredictable circumstances and act without being able to rely on the immediate support of colleagues or other clinical experts. The targeted deployment of skilled nurses in disaster risk management and emergency response appears to be one of the most promising measures for meeting the needs of people with complex needs during disasters and for maintaining their well-being even under difficult conditions, especially for PwTD.
The literature offers interesting insights into how providers respond to crises and disasters and how they sometimes deal with the challenges arising in exceptional situations in highly creative ways. However, the voices and perspectives of people with complex care needs and those in their social environment remain largely unconsidered. In many cases, the literature is characterized by a paternalistic attitude in which experts and other outsiders decide on patients’ needs and how to respond to them [49]. Examples of this are a primary focus on the technical aspect of care and vulnerabilities resulting from disruptions [62] or a focus on organizational challenges in disaster management [92]. The burden placed on family caregivers, especially in extreme situations, was also not addressed in the included literature. Even though, across the OECD countries, home care for complex care situations is promoted, it can lead to an increased reliance on family caregivers, especially when skilled care is not adequately funded [32]. Only a few studies focused on the lived experience of PwTD in disasters; these studies found that PwTD and their families considered their own disaster preparedness to be inadequate and were not familiar with guidelines from experts [77,80]. Sometimes they experienced problems during and after a disaster, they were not prepared for by their healthcare providers, like exacerbations arising from the access loss to regular dialysis and wound care [63]. It is extremely important to address this issue of user participation and actively involve people in emergency and disaster planning considerations. A sensitive, person-centered approach can help to alleviate irrational fears, enable needs-based precautions to be taken, and, above all, allow the specific experience of those most affected to be incorporated in the planning process. Often, PwTD and other patients with complex care needs have already gained experience with crises and exceptional situations during their long-term care. This could be put to work and actively taken up, for example, by the nurses who work with them to co-develop individual disaster plans. Including PwTD voices in preparedness planning and research could provide valuable insights into the feasibility of emergency and disaster response measures and, additionally, strengthen the person-centeredness of disaster preparedness and risk management.
Limitations
While this study provides valuable insights, several limitations must be considered when interpreting the results.
First, the search strategy may have inadvertently missed relevant publications. While the terminology focused on PwTD and general descriptors of the population, it did not include specific diagnostic terms associated with technology dependence. As a result, studies focusing on particular diagnostic groups may have been overlooked.
Second, the found literature shows a dominance of reports regarding renal replacement therapy, leading to an underrepresentation of other PwTD such as children with special healthcare needs or those relying on enteral nutrition, oxygen therapy or mechanical ventilators, and their specific care needs in disasters.
Only publications in English and German language were included for pragmatic reasons. As a result, studies published in native languages, particularly those from the disaster-prone region of Asia, may have been overlooked. Additionally, the specifications of the search regarding nursing care may have led to underrepresentation of interdisciplinary care provided or care given by medical or public healthcare providers.
Third, the geographic distribution of included publications is skewed, with many of the studies originating from the United States. Therefore, the findings are influenced by the terminologies and frameworks used within the US context and may have limited transferability to other national contexts. For instance, as reported by the OECD [32], care systems differ greatly between nations regarding organization and financing systems. Some are tax-based, like the UK or Australia, while others have a health insurance-based system with a big private sector like the United States. Countries like Germany or Japan even have an insurance dedicated to long-term care [100]. In addition, there is a lack of insight into the extent to which measures have already been taken in other countries for inclusive disaster risk management for PwTD, what effects these measures are having, and what role nurses play in their implementation.
Finally, the nature of the evidence base presents a constraint. The body of literature is primarily composed of retrospective case studies and empirical analyses. While case studies can provide in-depth insights into specific contexts, the generalizability of their findings is limited. Similarly, the dominance of retrospective designs is a common challenge in disaster research due to the unpredictable nature of such events, which restricts the ability to collect data prospectively. The sole prospective study identified was incidentally affected by a disaster rather than designed for one, underscoring this methodological gap [22].
5. Conclusions
In order to be able to answer the complex care needs of PwTD and comparable patient groups during disasters, a complementary strategy that combines structural preparedness, professional adaptability, and user participation—including PwTD and their families—is required. Clinicians with dedicated disaster response roles within a multidisciplinary disaster management team and clinical expertise in emergency, critical care, or disaster nursing are a promising factor in the development, implementation, and evaluation of needs-based disaster response plans for people with complex care needs. As nurses play an important role in care delivery for PwTD across settings, their involvement can help mitigate care gaps for PwTD and prevent safety issues for these patients when existing plans fall short in the event of a disaster.
To further strengthen the evidence base, future studies should go beyond descriptive or retrospective designs and employ study designs that allow for both empirical depth and practical transferability. To create a more comprehensive body of research regarding the needs of PwTD in disasters, underrepresented subgroups (such as people relying on tube feeding, an allergy-specific diet, infusion therapy or respiration assistance) should be studied, and the benefits of multidisciplinary teams caring for people with complex needs in extreme conditions should be explored.
Future studies can build on the findings of this review to examine how the identified needs can be operationalized in disaster preparedness and response, particularly regarding the role of nurses within a multidisciplinary disaster management team, intersectoral and interdisciplinary cooperation (e.g., partnerships with home-care agencies, disaster management and utility companies), and organizational structures in different national contexts. Empirical studies extending this work could help to assess how far PwTD and their families are already integrated into disaster planning and what measures effectively sustain nursing care under disaster conditions. This review thus provides a foundation for a broader practice-oriented research agenda aimed at strengthening inclusive, needs-based, and person-centred disaster risk management.
Author Contributions
Conceptualization, A.P. and M.E.; methodology, A.P., M.E. and J.B.; validation, A.P., J.B. and M.K.; analysis, A.P., J.B. and M.K.; writing—original draft preparation, A.P.; writing—review and editing, A.P., M.E., M.K. and J.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| PwTD | People with technology dependence |
| MeSH | Medical subject headings |
| IFRC | International Federation of Red Cross and Red Crescent Societies |
| UNDRR | United Nations Office for Disaster Risk Reduction |
| CMIST | Communication, maintaining health, independence, support, safety and self-determination, transportation |
Appendix A

Table A1.
Overview of the included studies.
Table A1.
Overview of the included studies.
| Author, Year Country | Aim and Study Design | Population |
|---|---|---|
| Al Amin, Morrison, Kabir and Sajib [71], Bangladesh | Short report using routine data summarizing strategies to mitigate the sufferings of non-COVID patients with chronic kidney disease. | People suffering from chronic kidney disease using dialysis during the COVID-19 pandemic |
| Arichi, Cadwgan, McDonald, Patel, Turner, Barkey, Lumsden and Fairhurst [79], USA | Cross-sectional survey highlighting the impact of the initial pandemic response on health, education, and social care for children and young people with severe physical neurodisability and multiple comorbidities. | Children or young people with severe neurodisabilities |
| Baker and Baker [80], USA | Cross-sectional baseline study within a larger longitudinal study to explore disaster preparedness levels among families with children with special healthcare needs (CSHCN) and educate on preparedness for this population. | Family caregivers of children with special healthcare needs |
| Baker, Baker and Flagg [82], USA | Quasi-experimental pretest/posttest intervention study to determine the short-term effectiveness of a brief patient education intervention in increasing disaster preparedness among families of CSHCN. | Family caregivers of children with special healthcare needs |
| Benigno, Kleinitz, Calina, Alcido, Gohy and Hall [89],Philippines | Report outlining needs assessments and activities conducted by WHO and other specialists to improve access to rehabilitation and services for people with disabilities and injuries after the Haiyan typhoon. | People with disabilities relying on various assistive technology. |
| Berry, Soltau, Richmond, Kieltyka, Tran and Williams [22], USA | Prospective study to evaluate the ability of nurse care coordinators to enhance a pediatric clinic’s ability to meet medical home objectives and improve service receipt for families of children with special healthcare needs before and after a hurricane. | Family caregivers of children with special healthcare needs |
| Cary and Schroeder [65], USA | Case study on the lessons learned from caring for patients on kidney dialysis in a disaster in the renal care group in Baton Rouge during Hurricane Katrina. | Nurses caring for patients receiving hemodialysis |
| Davis, O’Shea and Beach [62], USA | Hazard vulnerability analysis exploring the risks and specific needs that VAD patients could face in a disaster situation. | People with ventricular assist devices |
| Deal, Fountain, Russell-Broaddus and Stanley-Hermanns [67], USA | Case study discussing challenges and opportunities encountered by nurses volunteering in special-needs shelters. | Nurses caring for people in special-needs shelters |
| Fannin, Brannen, Howell and Martin [69], USA | Quasi-experimental study evaluating Medical Reserve Corps volunteers and public health workers in conducting chronic care triage by use of a rubric prior to sheltering to connect survivors with services. | Medical Reserve Corps volunteers, public health workers, and personal care assistants |
| Finkelstein and Finkelstein [77], Israel | Qualitative interview aimed at understanding how people with disabilities perceive emergencies and their needs in preparing for such situations. | People with disabilities using wheelchairs and ventilators |
| Gershon, Muska, Zhi and Kraus [92], USA | Cross-sectional study assessing disaster planning of local offices of emergency management with respect to people with disabilities. | Local disaster planning offices planning for people with disabilities using mobility and respiratory assistive devices |
| Goodhue, Demeter, Burke, Toor, Upperman and Merritt [59], USA | Mixed-methods pilot study evaluating disaster preparedness of families with children dependent on enteral or parenteral nutrition. | Families of children relying on EN/PN |
| Hoffman, Fagan, Casas-Melley, Wei and Hebra [68], USA | Case study on the measures taken to protect children with special healthcare needs during hurricane Irma in a children’s hospital in Florida. | Children with special healthcare needs using ventilators and other assistive technologies |
| Holmes, Williams, Wong, Smith, Bandzuh and Uejio [56], USA | Case study presenting an evaluation framework to assess factors influencing the emergency response and management of the Special Needs Shelter Program in Monroe County, Florida during Hurricane Irma in 2017. | People in a special needs shelter using various assistive devices |
| Kelman, Finne, Bogdanov, Worrall, Margolis, Rising, MaCurdy and Lurie [90], USA | Retrospective cohort study using Medicare/Medicaid claims data to analyze care patterns and mortality of kidney disease patients in areas most affected by Hurricane Sandy, aiming to inform disaster preparedness and mitigate adverse outcomes for this population. | People with end-stage renal disease (ESRD) relying on dialysis |
| Khorram-Manesh, Yttermyr, Sörensson and Carlström [17], Sweden | Cross-sectional study assessing the overall risks that influence advanced care at home patients in Sweden. | People receiving advanced care at home |
| Kleinpeter [91], USA | Case study reviewing ESRD patients and services before and after Hurricanes Katrina and Rita, covering disaster preparation, recovery, mitigation activities, and health policy recommendations for patients, healthcare professionals, and services relevant to other natural disasters. | People with ESRD relying on dialysis |
| Kolwaite, Hlady, Simon, Cadwell, Daley, Fleischauer, May and Thoroughman [88], USA | Cross-sectional study conducted through community assessment for public health emergency response following severe weather events, assessing household health status, preparedness, and shelter needs for future planning. | Randomly selected households in Pike Country, Kentucky |
| Kopp, Ball, Cohen, Kenney, Lempert, Miller, Muntner, Qureshi and Yelton [84], USA | Retrospective Case report of disaster response following the 2005 hurricane season and the Kashmir earthquake, assessing the severe impact on dialysis patient care and facility operations. | People with ESRD relying on dialysis |
| Koyama, Fuse, Hagiwara, Matsumoto, Shiraishi, Masuno, Miyauchi, Kawai and Yokota [40], Japan | Case study describing difficulties in delivering medical supplies, providing medical care and evacuating patients in a hospital after the earthquake and nuclear disaster in Fukushima. | Hospital staff and patients relying on ventilators or dialysis |
| Löfqvist, Oskarsson, Brändström, Vuorio and Haney [83], Sweden | Cross sectional study assessing ICU evacuation preparedness for fire in all hospitals within Sweden’s national public healthcare system. | Staff and patients in intensive care units in Sweden |
| Lukowsky, Dobalian, Goldfarb, Kalantar-Zadeh and Der-Martirosian [72], USA | Retrospective longitudinal cohort study examining dialysis and healthcare service utilization by ESRD patients in Manhattan receiving hemodialysis pre- and post- Hurricane Sandy. | Patients with ESRD relying on dialysis |
| Ma, Cohen and Lee [85], USA | Qualitative interview study exploring how NICU personnel in California hospitals managed neonatal transfers during recent wildfires, with the goal of sharing lessons learned to enhance disaster preparedness for healthcare teams. | Staff and pediatric patients in a neonatal intensive care unit during wildfires |
| McKinney, McKinney and Swartz [78], South Africa | Case study exploring challenges people with disabilities experience accessing healthcare facilities during the COVID-19 pandemic. | People with disabilities relying on wheelchairs or/and ventilators |
| Mellgard, Abramson, Okamura and Weerahandi [63], USA | Case study exploring Hurricane Marias impact on a resident of Puerto Rico with chronic health problems seeking healthcare in New York. | Person with multiple chronic conditions relying on dialysis |
| Molinari, Chen, Krishna and Morris [37], USA | Secondary data analysis focused on estimating the national prevalence of individuals relying on electricity-dependent technology at home and who are at risk during a power outage. | People depending on electrically powered technology |
| Motoki, Mori, Kaji, Nonami, Fukano, Kayano, Kawada, Kimura, Yasui, Ueki and Ugai [70], Japan | Qualitative interview study aimed at developing pamphlets to help patients with diabetes, rheumatic diseases, and chronic respiratory disease, and those undergoing dialysis, to manage their conditions during disasters. | People suffering from diabetes, rheumatic disease, chronic respiratory disease or needing dialysis and being affected by an Earthquake or typhoon |
| Naghavi, Faramarzi, Abbasi and Badakhshiyan [74], Iran | Qualitative interview study explored the challenges Iranian assistive technology users faced in accessing health information and care during the COVID-19 pandemic. | People using assistive devices |
| Nakayama, Tanaka, Uematsu, Kikuchi, Hino-Fukuyo, Morimoto, Sakamoto, Tsuchiya and Kure [81], Japan | Case study examining the impact of the 2011 Eastern Japan earthquake and subsequent blackout on pediatric patients using medical devices. | Children using assistive technology |
| Orlando, Bernard and Mathews [57], USA | Case study exploring nursing care challenges and lessons from neonatal units in New Orleans during and after Hurricane Katrina, offering guidance to support disaster education for neonatal nurses. | Staff and Patients in NICUs |
| Rauch, Baumberger, Moise, von Elm and Reinhardt [64], Haiti | Pilot study using an ICF-based tool to assess rehabilitation needs in person with spinal cord injuries following the 2010 earthquake in Haiti. | People with spinal cord injuries needing assistive technology |
| Sakashita, Matthews and Yamamoto [86], USA | Cross-sectional survey of caregivers for children with technology dependence with special healthcare needs, assessing household preparedness for electrical power failures, device backup power availability, and emergency contingency planning. | Children with special healthcare needs |
| Sekkarie, Zanabli, Rifai, Murad and Al-Makki [73], Syria | Case study on the impact of the conflict in Syria on the hemodialysis system and ESRD patients focusing on the collapsed healthcare in Aleppo, Idlib and Homs. | Patients with end-stage renal disease (ESRD) |
| Shakour, Mithani, Kopp, Shepherd, Nogueira, Espinel and Shultz [75], USA | Case study on lessons learned from dialysis providers disaster response in providing patient support during Hurricane Ian in Florida. | People with ESRD relying on dialysis |
| Shapira, Aharonson-Daniel, Clarfield and Feder-Bubis [58], Israel | Mixed-methods study exploring the perceptions and needs of community-dwelling medically vulnerable individuals in Israel to inform future preparedness efforts. | Medically vulnerable relying on dialysis and other technologies |
| Skewes [87], Australia | Case study reporting on the challenges in maintaining renal dialysis services during the Toowoomba flood disaster. | Staff and patients of a dialysis facility |
| Tashiro, Kawakami, Oka, Liu, Nishimura, Ogawa, Hagai, Yamamoto, Yazawa and Liu [61], Japan | Cross-sectional study estimating the number of community-dwelling elderly care recipients who require specific food preparations. | Community-dwelling elderly recipients of long-term care |
| Tatsuki [93], Japan | Case study exploring challenges for people with functional needs following the 2011 Great East Japan Earthquake. | People with functional needs |
| Trento and Allen [66], USA | Retrospective case report analyzing the impact of Hurricane Sandy on home parenteral and enteral nutrition consumers. | People relying on EN/PN |
| Tuglular, Luyckx, Vanholder, Skoberne, Wiecek, Nistor, Pawlowicz-Szlarska, Shroff, Ivanov, Eckardt, Noruisiene, Gallego, Loboda and Sever [60], Ukraine | Case study summarizing major challenges and lessons learned by the renal disaster task force during the conflict in Ukraine. | People with ESRD relying on dialysis |
| United Nations Office for Disaster Risk Reduction [94], Switzerland | Report assessing disaster preparedness, evacuation and assistance planning for people with disabilities and to evaluate the accessibility of early warning and risk information and determining if disaster risk reduction plans include their specific needs. | People with disabilities using various assistive technology |
| United Nations Office for Disaster Risk Reduction [95], Switzerland | Scoping report exploring how linking disaster risk reduction (DRR) with the Convention on the Rights of Persons with Disabilities (CRPD) can strengthen protections for people with disabilities in disasters. | People with disabilities using various assistive technology |

Table A2.
Complete Search String for MEDLINE.
Table A2.
Complete Search String for MEDLINE.
| Search | Search Term |
|---|---|
| 1. | “medically fragile”.ab,ti. |
| 2. | “technology depend *”.ab,ti. |
| 3. | “technology assist *”.ab,ti. |
| 4. | “medically complex”.ab,ti. |
| 5. | “complex chronic health”.ab,ti. |
| 6. | “complex care need?”.ab,ti. |
| 7. | “special healthcare need?”.ab,ti. |
| 8. | “special need?”.ab,ti. |
| 9. | “at-risk”.ab,ti. |
| 10. | CMIST.ab,ti. |
| 11. | Respiration, Artificial/ |
| 12. | Renal Dialysis/ |
| 13. | Enteral Nutrition/ |
| 14. | Parenteral Nutrition/ |
| 15. | Heart-Assist Devices/ |
| 16. | Vulnerable Populations/ |
| 17. | Disabled Persons/ |
| 18. | Nursing Care/ |
| 19. | Nursing/ |
| 20. | “Health Services Needs and Demand”/ |
| 21. | “Health Services for Persons with Disabilities”/ |
| 22. | Health Resources/ |
| 23. | Patient Care/ |
| 24. | “functional need?”.ab,ti. |
| 25. | “techn * need?”.ab,ti. |
| 26. | “nursing care”.ab,ti. |
| 27. | “access”.ab,ti. |
| 28. | Disasters/ |
| 29. | “cris?s”.ab,ti. |
| 30. | disaster?.ab,ti. |
| 31. | “public health emergency”.ab,ti. |
| 32. | 1. OR 2. OR 3. OR 4. OR 5. OR 6. OR 7. OR 8. OR 9. OR 10. OR 11. OR 12. OR 13. OR14. OR 15. OR 16. OR 17. |
| 33. | 18. OR 19. OR 20. OR 21. OR 22. OR 23 OR 24. OR 25. OR 26. OR 27. |
| 34. | 28. OR 29. OR 30. OR 31. |
| 35. | 32. AND 33. AND 34. |
| 36. | Limit 35 to year 2001—current |
| 37. | Limit 36 to language: English, German |
* wildcard operator to find all variations with different endings.
References
- Brenner, M.; Alexander, D.; Quirke, M.B.; Eustace-Cook, J.; Leroy, P.; Berry, J.; Healy, M.; Doyle, C.; Masterson, K. A systematic concept analysis of ‘technology dependent’: Challenging the terminology. Eur. J. Pediatr. 2021, 180, 1–12. [Google Scholar] [CrossRef]
- Spratling, R. Defining technology dependence in children and adolescents. West. J. Nurs. Res. 2015, 37, 634–651. [Google Scholar] [CrossRef] [PubMed]
- Gallo, M.; Agostiniani, R.; Pintus, R.; Fanos, V. The child with medical complexity. Ital. J. Pediatr. 2021, 47, 1. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Report on Assistive Technology; World Health Organization: Geneva, Switzerland, 2022; ISBN 978-92-4-004945-1. [Google Scholar]
- Buhl, N.D.; Bourry, J.; Seguy, D.; Lescut, D. Epidemiology of home enteral and parenteral nutrition in adults: Comprehensive national data. Clin. Nutr. ESPEN 2024, 60, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Stark, S.; Ewers, M. Healthcare needs of vulnerable patient groups: Available data and existing gaps in Germany with respect to long-term mechanical ventilation. Z. Gesundh. Wiss 2020, 28, 139–146. [Google Scholar] [CrossRef]
- Ferrari, A.J.; Santomauro, D.F.; Aali, A.; Abate, Y.H.; Abbafati, C.; Abbastabar, H.; Abd ElHafeez, S.; Abdelmasseh, M.; Abd-Elsalam, S.; Abdollahi, A.; et al. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2133–2161. [Google Scholar] [CrossRef]
- Thurlow, J.S.; Joshi, M.; Yan, G.; Norris, K.C.; Agodoa, L.Y.; Yuan, C.M.; Nee, R. Global Epidemiology of End-Stage Kidney Disease and Disparities in Kidney Replacement Therapy. Am. J. Nephrol. 2021, 52, 98–107. [Google Scholar] [CrossRef]
- Elias, E.R.; Murphy, N.A.; Liptak, G.S.; Adams, R.C.; Burke, R.; Friedman, S.L.; Houtrow, A.; Kalichman, M.; Kuo, D.; Levy, S.E.; et al. Home Care of Children and Youth With Complex Health Care Needs and Technology Dependencies. Pediatrics 2012, 129, 996–1005. [Google Scholar] [CrossRef]
- Sobotka, S.A.; Lynch, E.; Peek, M.E.; Graham, R.J. Readmission drivers for children with medical complexity: Home nursing shortages cause health crises. Pediatr. Pulmonol. 2020, 55, 1474–1480. [Google Scholar] [CrossRef]
- Sobotka, S.A.; Lynch, E.; Quinn, M.T.; Awadalla, S.S.; Agrawal, R.K.; Peek, M.E. Unmet Respite Needs of Children with Medical Technology Dependence. Clin. Pediatr. 2019, 58, 1175–1186. [Google Scholar] [CrossRef]
- Pitch, N.; Shahil, A.; Mekhuri, S.; Ambreen, M.; Chu, S.; Keilty, K.; Cohen, E.; Orkin, J.; Amin, R. Caring for children with new medical technology at home: Parental perspectives. BMJ Paediatr. Open 2023, 7, e002062. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.T.; Blankestijn, P.J.; Dember, L.M.; Gallieni, M.; Harris, D.C.H.; Lok, C.E.; Mehrotra, R.; Stevens, P.E.; Wang, A.Y.-M.; Cheung, M.; et al. Dialysis initiation, modality choice, access, and prescription: Conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019, 96, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Kentischer, F.; Kleinknecht-Dolf, M.; Spirig, R.; Frei, I.A.; Huber, E. Patient-related complexity of care: A challenge or overwhelming burden for nurses—A qualitative study. Scand. J. Caring Sci. 2018, 32, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Lindeke, L.L.; Leonard, B.J.; Presler, B.; Garwick, A. Family-centered care coordination for children with special needs across multiple settings. J. Pediatr. Health Care 2002, 16, 290–297. [Google Scholar] [CrossRef]
- Al-Hamad, A.; Yasin, Y.M.; Metersky, K.; Kokorelias, K.M.; Yasin, L.; Afzal, F. Home Healthcare Services and Interventions for Older Adults: An Umbrella Review of Systematic Reviews and Meta-Analyses. J. Ageing Longev. 2025, 5, 25. [Google Scholar] [CrossRef]
- Khorram-Manesh, A.; Yttermyr, J.; Sörensson, J.; Carlström, E. The impact of disasters and major incidents on vulnerable groups: Risk and medical assessment of Swedish patients with advanced care at home. Home Health Care Manag. Pract. 2017, 29, 183–190. [Google Scholar] [CrossRef]
- Sump, C.; Riddle, S.W.; Levine, D.M. Hospital at Home for Children—An Emerging Model of Acute Care. Hosp. Pediatr. 2024, 14, e110–e112. [Google Scholar] [CrossRef]
- Windisch, W.; Dreher, M.; Geiseler, J.; Siemon, K.; Brambring, J.; Dellweg, D.; Grolle, B.; Hirschfeld, S.; Kohnlein, T.; Mellies, U.; et al. Guidelines for Non-Invasive and Invasive Home Mechanical Ventilation for Treatment of Chronic Respiratory Failure—Update 2017. Pneumologie 2017, 71, 722–795. [Google Scholar] [CrossRef]
- Stark, S.; Lehmann, Y. “Ensuring patient safety is one of our primary responsibilities.”—Results of a qualitative study on maintaining safety in ventilation-associated technical aid supply. Z. Evid. Fortbild. Qual. Gesundhwes 2023, 182–183, 53–62. [Google Scholar] [CrossRef]
- Currie, G.; Materula, D.; Gall, N.; Lachuk, G.; Richard, C.; Yohemas, M.; Dewan, T.; Gibbard, W.B.; Zwicker, J. Care coordination of children with neurodevelopmental disabilities and medical complexity during the COVID-19 pandemic: Caregiver experiences. Child Care Health Dev. 2023, 49, 834–845. [Google Scholar] [CrossRef]
- Berry, S.; Soltau, E.; Richmond, N.; Kieltyka, R.; Tran, T.; Williams, A. Care Coordination in a Medical Home in Post-Katrina New Orleans: Lessons Learned. Matern. Child Health J. 2011, 15, 782–793. [Google Scholar] [CrossRef] [PubMed]
- Mantler, T.; Jackson, K.T.; Baer, J.; White, J.; Ache, B.; Shillington, K.; Ncube, N. Changes in Care-A Systematic Scoping Review of Transitions for Children with Medical Complexities. Curr. Pediatr. Rev. 2020, 16, 165–175. [Google Scholar] [CrossRef]
- Sobotka, S.A.; Lynch, E.; Agrawal, R. The Role of Care Coordinators for Children with Respiratory Technologies and Home Nursing. Pediatr. Allergy Immunol. Pulmonol. 2022, 35, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.; Ryan, N.P.; Byrne, L.K.; Hendrieckx, C.; White, V. Unmet supportive care needs of families of children with chronic illness: A systematic review. J. Clin. Nurs. 2023, 32, 7101–7124. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, Y.; Stark, S. Supply of Medical Aids in home Mechanical Ventilation: Needs-Based and Safe?—The Views of Stakeholders Related to the Care Process on the Current Status and Perspectives. Gesundheitswesen 2024, 86, 200–207. [Google Scholar] [CrossRef]
- Nawaz, R.F.; Page, B.; Harrop, E.; Vincent, C.A. Analysis of paediatric long-term ventilation incidents in the community. Arch. Dis. Child. 2020, 105, 446–451. [Google Scholar] [CrossRef]
- Mauskar, S.; Ngo, T.; Haskell, H.; Mallick, N.; Mercer, A.N.; Baird, J.; Bardsley, K.; Berry, J.G.; Copp, K.; Humphrey, K.; et al. In their own words: Safety and quality perspectives from families of hospitalized children with medical complexity. J. Hosp. Med. 2023, 18, 777–786. [Google Scholar] [CrossRef]
- International Council of Nurses (ICN). Guidelines on Advanced Practice Nursing; International Council of Nurses: Geneva, Switzerland, 2020; ISBN 978-92-95099-71-5. [Google Scholar]
- Graaf, G.; Baiden, P.; Boyd, G.; Keyes, L. Barriers to Respite Care for Children with Special Health Care Needs. J. Dev. Behav. Pediatr. 2022, 43, 117–129. [Google Scholar] [CrossRef]
- Graaf, G.; Gigli, K. Care coordination and unmet need for specialised health services among children with special healthcare needs in the USA: Results from a cross-sectional analysis of the national survey of children with special healthcare needs. BMJ Open 2022, 12, e063373. [Google Scholar] [CrossRef]
- OECD. The Economic Benefit of Promoting Healthy Ageing and Community Care; OECD Publishing: Paris, France, 2025. [Google Scholar]
- United Nations Office for Disaster Risk Reduction (UNDRR). Report of the Open-Ended Intergovernmental Expert Working Group on Indicators and Terminology Relating to Disaster Risk Reduction; United Nations Office for Disaster Risk Reduction (UNDRR): New York, NY, USA, 2016. [Google Scholar]
- Cuschieri, S.; Mamo, J. Taking care of the ordinary in extraordinary times—Delayed routine care means more morbidity and pre-mature mortality. Eur. J. Public Health 2021, 31, iv27–iv30. [Google Scholar] [CrossRef]
- Leão, T.; Duarte, G.; Gonçalves, G. Preparedness in a public health emergency: Determinants of willingness and readiness to respond in the onset of the COVID-19 pandemic. Public Health 2022, 203, 43–46. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, and Medicine; Policy and Global Affairs; Office of Special Projects; Committee on Building Adaptable and Resilient Supply Chains After Hurricanes Harvey, Irma, and Maria. Overview of Supply Chain Impacts from the 2017 Hurricanes. In Strengthening Post-Hurricane Supply Chain Resilience: Observations from Hurricanes Harvey, Irma, and Maria; National Academies Press (US): Washington, DC, USA, 2020. [Google Scholar]
- Molinari, N.A.M.; Chen, B.; Krishna, N.; Morris, T. Who’s at Risk When the Power Goes Out? The At-home Electricity-Dependent Population in the United States, 2012. J. Public Health Manag. Pract. 2017, 23, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Shimada, Y.; Nomura, S.; Ozaki, A.; Higuchi, A.; Hori, A.; Sonoda, Y.; Yamamoto, K.; Yoshida, I.; Tsubokura, M. Balancing the risk of the evacuation and sheltering-in-place options: A survival study following Japan’s 2011 Fukushima nuclear incident. BMJ Open 2018, 8, e021482. [Google Scholar] [CrossRef] [PubMed]
- Dosa, D.; Hyer, K.; Thomas, K.; Swaminathan, S.; Feng, Z.; Brown, L.; Mor, V. To evacuate or shelter in place: Implications of universal hurricane evacuation policies on nursing home residents. J. Am. Med. Dir. Assoc. 2012, 13, 190.e191–197. [Google Scholar] [CrossRef]
- Koyama, A.; Fuse, A.; Hagiwara, J.; Matsumoto, G.; Shiraishi, S.; Masuno, T.; Miyauchi, M.; Kawai, M.; Yokota, H. Medical relief activities, medical resourcing, and inpatient evacuation conducted by Nippon Medical School due to the Fukushima Daiichi Nuclear Power Plant accident following the Great East Japan Earthquake 2011. J. Nippon Med. Sch. = Nippon Ika Daigaku Zasshi 2011, 78, 393–396. [Google Scholar] [CrossRef]
- Smith, R.S.; Zucker, R.J.; Frasso, R. Natural Disasters in the Americas, Dialysis Patients, and Implications for Emergency Planning: A Systematic Review. Prev. Chronic Dis. 2020, 17, E42. [Google Scholar] [CrossRef]
- Hasan, M.K.; Nasrullah, S.M.; Quattrocchi, A.; Arcos González, P.; Castro Delgado, R. Hospital Surge Capacity Preparedness in Disasters and Emergencies: Protocol for a Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 13437. [Google Scholar] [CrossRef]
- Hua, C.L.; Patel, S.; Thomas, K.S.; Peterson, L.J.; Andel, R.; Gordon, L.; Jester, D.J.; Dosa, D.M. The relationship between exposure to Hurricane Harvey and mortality among nursing home residents. J. Am. Geriatr. Soc. 2023, 71, 888–894. [Google Scholar] [CrossRef]
- Dosa, D.M.; Skarha, J.; Peterson, L.J.; Jester, D.J.; Sakib, N.; Ogarek, J.; Thomas, K.S.; Andel, R.; Hyer, K. Association Between Exposure to Hurricane Irma and Mortality and Hospitalization in Florida Nursing Home Residents. JAMA Netw. Open 2020, 3, e2019460. [Google Scholar] [CrossRef]
- Skarha, J.; Gordon, L.; Sakib, N.; June, J.; Jester, D.J.; Peterson, L.J.; Andel, R.; Dosa, D.M. Association of Power Outage with Mortality and Hospitalizations Among Florida Nursing Home Residents After Hurricane Irma. JAMA Health Forum 2021, 2, e213900. [Google Scholar] [CrossRef]
- Dries, D.; Reed, M.J.; Kissoon, N.; Christian, M.D.; Dichter, J.R.; Devereaux, A.V.; Upperman, J.S. Task Force for Mass Critical Care. Special populations: Care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest 2014, 146, e75S–e86S. [Google Scholar] [CrossRef] [PubMed]
- Ireton-Jones, C.; Nishikawa, K.; Nishikawa, R. Home Parenteral and Enteral Nutrition During Natural Disasters: A Guide for Clinicians and Consumers. Nutr. Clin. Pract. 2019, 34, 216–219. [Google Scholar] [CrossRef] [PubMed]
- Mace, S.E.; Doyle, C.J.; Askew, K.; Bradin, S.; Baker, M.; Joseph, M.M.; Sorrentino, A. Planning considerations for persons with access and functional needs in a disaster-Part 3: Medical CMIST and recommendations. Am. J. Disaster Med. 2018, 13, 207–220. [Google Scholar] [CrossRef] [PubMed]
- Lempert, K.D.; Kopp, J.B. Renal Failure Patients in Disasters. Disaster Med. Public Health Prep. 2019, 13, 782–790. [Google Scholar] [CrossRef]
- United Nations. Convention on the Rights of Persons with Disabilities (CPRD); United Nations: New York, NY, USA, 2007. [Google Scholar]
- International Council of Nurses. Core Competencies in Disaster Nursing Version 2.0; International Council of Nurses: Geneva, Switzerland, 2019; ISBN 978-92-95099-68-5. [Google Scholar]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Scoping reviews. In JBI Manual for Evidence Synthesis; JBI: Adelaide, Australia, 2024. [Google Scholar] [CrossRef]
- Aromataris, E.; Lockwood, C.; Porritt, K.; Pilla, B.; Jordan, Z. JBI Manual for Evidence Synthesis; JBI: Adelaide, Australia, 2024. [Google Scholar]
- Sphere Association. The Sphere Handbook: Humanitarian Charter and Minimum Standards in Humanitarian Response, 4th ed.; Sphere Association: Geneva, Switzerland, 2018. [Google Scholar]
- Pollock, D.; Peters, M.D.J.; Khalil, H.; McInerney, P.; Alexander, L.; Tricco, A.C.; Evans, C.; de Moraes, É.B.; Godfrey, C.M.; Pieper, D.; et al. Recommendations for the extraction, analysis, and presentation of results in scoping reviews. JBI Evid. Synth. 2023, 21, 520–532. [Google Scholar] [CrossRef]
- Holmes, T.J.; Williams, P.C.; Wong, S.; Smith, K.; Bandzuh, J.T.; Uejio, C.K. Assessment of an evacuation shelter program for people with access and functional needs in Monroe County, Florida during Hurricane Irma. Soc. Sci. Med. 2022, 306, 115108. [Google Scholar] [CrossRef]
- Orlando, S.; Bernard, M.L.; Mathews, P. Neonatal nursing care issues following a natural disaster: Lessons learned from the Katrina experience. J. Perinat. Neonatal Nurs. 2008, 22, 147–153. [Google Scholar] [CrossRef]
- Shapira, S.; Aharonson-Daniel, L.; Clarfield, A.M.; Feder-Bubis, P. Giving a voice to medically vulnerable populations: A mixed-methods investigation of their unique perceptions and needs in emergency situations. Health Soc. Care Community 2020, 28, 811–822. [Google Scholar] [CrossRef]
- Goodhue, C.J.; Demeter, N.E.; Burke, R.V.; Toor, K.T.; Upperman, J.S.; Merritt, R.J. Mixed-Methods Pilot Study: Disaster Preparedness of Families With Children Followed in an Intestinal Rehabilitation Clinic. Nutr. Clin. Pract. Off. Publ. Am. Soc. Parenter. Enter. Nutr. 2016, 31, 257–265. [Google Scholar] [CrossRef]
- Tuglular, S.; Luyckx, V.; Vanholder, R.; Skoberne, A.; Wiecek, A.; Nistor, I.; Pawlowicz-Szlarska, E.; Shroff, R.; Ivanov, D.; Eckardt, K.-U.; et al. Lessons learned during the war in Ukraine: A report from the Renal Disaster Relief Task Force of the ERA. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Ren. Assoc. 2023, 38, 1960–1968. [Google Scholar] [CrossRef]
- Tashiro, S.; Kawakami, M.; Oka, A.; Liu, F.; Nishimura, A.; Ogawa, C.; Hagai, F.; Yamamoto, S.; Yazawa, M.; Liu, M. Estimating nutrition intake status of community-dwelling elderly people requiring care in disaster settings: A preliminary cross-sectional survey. J. Rehabil. Med. 2019, 51, 312–316. [Google Scholar] [CrossRef]
- Davis, K.J.; O’Shea, G.; Beach, M. Assessment of Risks Posed to VAD Patients During Disasters. Prehosp. Disaster Med. 2017, 32, 457–461. [Google Scholar] [CrossRef] [PubMed]
- Mellgard, G.; Abramson, D.; Okamura, C.; Weerahandi, H. Hurricanes and healthcare: A case report on the influences of Hurricane Maria and managed Medicare in treating a Puerto Rican resident. BMC Health Serv. Res. 2019, 19, 818. [Google Scholar] [CrossRef] [PubMed]
- Rauch, A.; Baumberger, M.; Moise, F.G.; von Elm, E.; Reinhardt, J.D. Rehabilitation needs assessment in persons with spinal cord injury following the 2010 earthquake in Haiti: A pilot study using an ICF-based tool. J. Rehabil. Med. 2011, 43, 969–975. [Google Scholar] [CrossRef] [PubMed]
- Cary, S.; Schroeder, K. Caring for patients on kidney dialysis in a disaster. Am. J. Nurs. 2008, 108, 26–32. [Google Scholar] [CrossRef]
- Trento, L.; Allen, S. Hurricane Sandy nutrition support during disasters. Nutr. Clin. Pract. 2014, 29, 576–584. [Google Scholar] [CrossRef]
- Deal, B.J.; Fountain, R.A.; Russell-Broaddus, C.A.; Stanley-Hermanns, M. Challenges and opportunities of nursing care in special-needs shelters. Disaster Manag. Response 2006, 4, 100–105. [Google Scholar] [CrossRef]
- Hoffman, A.; Fagan, H.; Casas-Melley, A.; Wei, J.; Hebra, A. Hurricane Irma Impact on the Inpatient Population at a Tertiary Children’s Hospital in Florida. Am. Surg. 2018, 84, 1395–1400. [Google Scholar] [CrossRef]
- Fannin, A.; Brannen, D.E.; Howell, M.; Martin, S. Using Functional Needs and Personal Care Assistance Rather Than Disability Status During Chronic Care Triage in Community Mass Care. Disaster Med. Public Health Prep. 2015, 9, 265–274. [Google Scholar] [CrossRef]
- Motoki, E.; Mori, K.; Kaji, H.; Nonami, Y.; Fukano, C.; Kayano, T.; Kawada, T.; Kimura, Y.; Yasui, K.; Ueki, H.; et al. Development of disaster pamphlets based on health needs of patients with chronic illnesses. Prehosp. Disaster Med. 2010, 25, 354–360. [Google Scholar] [CrossRef]
- Al Amin, S.; Morrison, S.D.; Kabir, M.; Sajib, M.R.U.-Z. Challenges for Non-COVID Patients with Chronic Kidney Disease in Bangladesh: An Observation during Coronavirus Disease Pandemic. Inquiry 2021, 58, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Lukowsky, L.R.; Dobalian, A.; Goldfarb, D.S.; Kalantar-Zadeh, K.; Der-Martirosian, C. Access to Care for VA Dialysis Patients During Superstorm Sandy. J. Prim. Care Community Health 2019, 10, 2150132719863599. [Google Scholar] [CrossRef] [PubMed]
- Sekkarie, M.A.; Zanabli, A.R.; Rifai, A.O.; Murad, L.B.; Al-Makki, A.A. The Syrian conflict: Assessment of the ESRD system and response to hemodialysis needs during a humanitarian and medical crisis. Kidney Int. 2015, 87, 262–265. [Google Scholar] [CrossRef] [PubMed]
- Naghavi, A.; Faramarzi, S.; Abbasi, A.; Badakhshiyan, S.-S. COVID-19 and challenges of assistive technology use in Iran. Disabil. Rehabil. Assist. Technol. 2022, 17, 268–274. [Google Scholar] [CrossRef]
- Shakour, R.L.; Mithani, Z.; Kopp, J.B.; Shepherd, J.M.; Nogueira, L.M.; Espinel, Z.; Shultz, J.M. Safeguarding Patients with End-Stage Kidney Disease From Climate-driven Extreme Heat and Hurricanes. Disaster Med. Public Health Prep. 2024, 18, e124. [Google Scholar] [CrossRef]
- Truong, T.; Dittmar, M.; Ghaffari, A.; Lin, E. Policy and Pandemic: The Changing Practice of Nephrology During the Coronavirus Disease-2019 Outbreak. Adv. Chronic Kidney Dis. 2020, 27, 390–396. [Google Scholar] [CrossRef]
- Finkelstein, A.; Finkelstein, I. Emergency preparedness—The perceptions and experiences of people with disabilities. Disabil. Rehabil. 2020, 42, 2056–2066. [Google Scholar] [CrossRef]
- McKinney, E.L.; McKinney, V.; Swartz, L. Access to healthcare for people with disabilities in South Africa: Bad at any time, worse during COVID-19? S. Afr. Fam. Pract. 2021, 63, 1–5. [Google Scholar] [CrossRef]
- Arichi, T.; Cadwgan, J.; McDonald, A.; Patel, A.; Turner, S.; Barkey, S.; Lumsden, D.E.; Fairhurst, C. Neurodisability care in the time of COVID-19. Child Care Health Dev. 2022, 48, 901–905. [Google Scholar] [CrossRef]
- Baker, L.R.; Baker, M.D. Disaster preparedness among families of children with special health care needs. Disaster Med. Public Health Prep. 2010, 4, 240–245. [Google Scholar] [CrossRef]
- Nakayama, T.; Tanaka, S.; Uematsu, M.; Kikuchi, A.; Hino-Fukuyo, N.; Morimoto, T.; Sakamoto, O.; Tsuchiya, S.; Kure, S. Effect of a blackout in pediatric patients with home medical devices during the 2011 eastern Japan earthquake. Brain Dev. 2014, 36, 143–147. [Google Scholar] [CrossRef]
- Baker, M.D.; Baker, L.R.; Flagg, L.A. Preparing families of children with special health care needs for disasters: An education intervention. Soc. Work Health Care 2012, 51, 417–429. [Google Scholar] [CrossRef]
- Löfqvist, E.; Oskarsson, Å.; Brändström, H.; Vuorio, A.; Haney, M. Evacuation Preparedness in the Event of Fire in Intensive Care Units in Sweden: More is Needed. Prehosp. Disaster Med. 2017, 32, 317–320. [Google Scholar] [CrossRef]
- Kopp, J.B.; Ball, L.K.; Cohen, A.; Kenney, R.J.; Lempert, K.D.; Miller, P.E.; Muntner, P.; Qureshi, N.; Yelton, S.A. Kidney patient care in disasters: Lessons from the hurricanes and earthquake of 2005. Clin. J. Am. Soc. Nephrol. 2007, 2, 814–824. [Google Scholar] [CrossRef] [PubMed]
- Ma, A.L.; Cohen, R.S.; Lee, H.C. Learning from Wildfire Disaster Experience in California NICUs. Children 2020, 7, 155. [Google Scholar] [CrossRef] [PubMed]
- Sakashita, K.; Matthews, W.J.; Yamamoto, L.G. Disaster preparedness for technology and electricity-dependent children and youth with special health care needs. Clin. Pediatr. 2013, 52, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Skewes, J. The Toowoomba flood disaster: Maintaining renal dialvsis services. Ren. Soc. Australas. J. 2011, 7, 61–62. [Google Scholar]
- Kolwaite, A.R.; Hlady, W.G.; Simon, M.C.; Cadwell, B.L.; Daley, W.R.; Fleischauer, A.T.; May, Z.; Thoroughman, D. Assessing functional needs sheltering in Pike County, Kentucky: Using a community assessment for public health emergency response. Disaster Med. Public Health Prep. 2013, 7, 597–602. [Google Scholar] [CrossRef]
- Benigno, M.R.; Kleinitz, P.; Calina, L.; Alcido, M.R.; Gohy, B.; Hall, J.L. Responding to the health and rehabilitation needs of people with disabilities post-Haiyan. West. Pac. Surveill. Response J. WPSAR 2015, 6, 53–59. [Google Scholar] [CrossRef]
- Kelman, J.; Finne, K.; Bogdanov, A.; Worrall, C.; Margolis, G.; Rising, K.; MaCurdy, T.E.; Lurie, N. Dialysis care and death following Hurricane Sandy. Am. J. Kidney Dis. 2015, 65, 109–115. [Google Scholar] [CrossRef]
- Kleinpeter, M.A. Shifts in dialysis patients from natural disasters in 2005. Hemodial. Int. 2007, 11, S33–S37. [Google Scholar] [CrossRef]
- Gershon, R.R.; Muska, M.A.; Zhi, Q.; Kraus, L.E. Are local offices of emergency management prepared for people with disabilities? Results from the FEMA Region 9 Survey. J. Emerg. Manag. 2021, 19, 7–20. [Google Scholar] [CrossRef]
- Tatsuki, S. Challenges in Counter-disaster Measures for People with Functional Needs in Times of Disaster Following the Great East Japan Earthquake. Int. J. Jpn. Sociol. 2012, 21, 12–20. [Google Scholar] [CrossRef]
- United Nations Office for Disaster Risk Reduction (UNDRR). Global Survey Report on Persons with Disabilities and Disasters 2023; United Nations Office for Disaster Risk Reduction (UNDRR): New York, NY, USA, 2023. [Google Scholar]
- United Nations Office for Disaster Risk Reduction (UNDRR). Persons with Disabilities in Situations of Risk: A Scoping Study on Article 11 of the Convention on the Rights of Persons with Disabilities; United Nations Office for Disaster Risk Reduction (UNDRR): New York, NY, USA, 2022. [Google Scholar]
- Kailes, J.I. Defining Functional Needs—Updating CMIST. The Partnership for Inclusive Disaster Strategies. Available online: https://disasterstrategies.org/blog-post/defining-functional-needs-updating-cmist-by-june-isaacson-kailes-disability-policy-consultant/ (accessed on 4 June 2025).
- Collaborating4Inclusion. Disability Inclusive Disaster Risk Reduction (DIDRR) Framework and Toolkit for Collaborative Action; University of Sydney: Sydney, Australia, 2024. [Google Scholar]
- Inter-Agency Standing Comittee (IASC). Guidelines Inclusion of Persons with Disabilities in Humanitatarian Action; Inter-Agency Standing Comittee (IASC): New York, NY, USA, 2019. [Google Scholar]
- Institute of Medicine (IoM). Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. In Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response; National Academies Press (US): Washington, DC, USA, 2012. [Google Scholar]
- Lee, S.-H.; Chon, Y.; Kim, Y.-Y. Comparative Analysis of Long-Term Care in OECD Countries: Focusing on Long-Term Care Financing Type. Healthcare 2023, 11, 206. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).