Abstract
Background: Alexithymia has been recognised as a predictor of negative outcomes in various chronic conditions, including type 2 diabetes mellitus (T2DM). However, evidence concerning its role in type 1 diabetes mellitus (T1DM) remains limited. This systematic review aims to explore the relationship between alexithymia and T1DM. Methods: In June 2025, following PRISMA guidelines, a systematic review was conducted using Scopus, PubMed, and Web of Science databases. Studies specifically addressing the relationship between alexithymia and type 1 diabetes mellitus were analysed. The search strategy included the keywords “Alexithymia” AND (“Type 1 Diabetes Mellitus” OR “T1DM”). The NIH Study Quality Assessment Tool was employed to evaluate the methodological quality of the selected studies. Results: Fifteen studies met the inclusion criteria. The systematic analysis of the literature highlighted three dominant themes: alexithymia was found to be associated with patients’ health status concerning weight and obesity, glycaemic control, and psychopathological symptoms. Moreover, alexithymia emerged as a potential predictor of adverse outcomes in T1DM self-management. Conclusions: Available evidence suggests that alexithymia has a clinically relevant impact on the management of T1DM. However, further research involving larger samples and longitudinal designs is needed to bridge the gap with other chronic conditions. Promoting evidence-based research in this area is aligned with the need for targeted psychological assessment, specific interventions, and improved care strategies.
1. Introduction
Type 1 Diabetes Mellitus (T1DM) is a chronic condition resulting from the autoimmune destruction of pancreatic β-cells producing insulin, whose absolute deficiency leads to significant clinical consequences [1,2]. As the most common chronic disease in youths [3], its overall impact is substantial [4,5]. Strategies and solutions to reduce the burden and increase perceived quality of life are therefore essential [6]. The interplay between chronic conditions and psychological factors currently represents a promising field of scientific investigation [7,8,9,10,11,12,13,14,15,16]. Identifying specific psychological mechanisms that worsen patients’ health and hinder disease management constitutes a significant advance in clinical research.
Notably, reduced quality of life has been widely reported in patients with T1DM [17,18,19], although the underlying psychological contributors remain insufficiently explored. Psychological functioning and health-related quality of life have emerged as key facets for T1DM [20,21,22]. These elements are identified as influencing disease course and management, often representing a serious risk for patients [20]. It is well established that psychopathology emphasises patients’ experience as both a predictor and a consequence of type 1 diabetes mellitus (T1DM) [23,24,25]. A strong link has been observed between psychological distress, general psychopathological dimensions, and diabetes, although most studies refer to Type 2 Diabetes Mellitus (T2DM) [26,27,28,29,30,31,32,33,34,35,36]. However, specific contributions directly related to T1DM remain limited.
The consequences of such psychological factors are especially evident in maladaptive responses that further complicate patients’ adjustment to the disease. Obesity and weight difficulties are strongly related to psychological functioning [37,38,39,40,41,42,43]. Lesions, insulin resistance and negative outcomes directly deriving from hyperglycaemia in obese patients with T1DM represent a major clinical concern. In this regard, glycaemic control represents a fundamental factor, and psychological influences on it must be carefully monitored [44,45,46].
Among the most influential factors for chronic conditions, alexithymia is gaining great attention. Alexithymia can be defined as difficulties or impossibility in identifying and describing affective manifestations such as emotions, feelings and mood correlates [47,48,49,50]. Its relationship with obesity, psychopathology and glycaemic control was evidenced with greater reference to T2DM [27,51,52]. A substantial body of evidence has demonstrated the impact of alexithymia on physical and psychological functioning across diverse clinical contexts, providing a solid scientific basis for its relevance in diagnosis and treatment [53,54,55,56,57,58,59,60,61,62]. The origins of the study of the impact of alexithymia on physical health are not recent [63]. A substantial number of contributions highlighted its role in terms of somatization [64,65]. In particular, it is known that phenomena linked to the amplification of bodily sensations with consequent variation in physiological responses to stress, the dysregulation of the autonomic nervous system with consequent increase in the risk of developing somatic disorders, play a fundamental role [66,67,68,69]. These phenomena are of particular relevance in the field of diabetes, where glycaemic variations are consistently influenced by affective functioning.
Given the clinical significance of alexithymia and the potential risks associated with its lack of assessment, a consistent analysis of the state of the art should precede future actions. This systematic review was aimed at portraying the state of the art regarding alexithymia in patients suffering from T1DM. A comprehensive understanding of emerging findings may serve as a strong foundation for future research and clinical interventions.
2. Materials and Methods
The present systematic review was performed in line with the Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) guidelines provided by Liberati, Moher and colleagues [70,71] and PRISMA 2020 Checklist [72]. This systematic review was not registered in a public database such as PROSPERO. At the time of the protocol development, registration was not mandatory for submission to this Journal. Nevertheless, the review was conducted in accordance with PRISMA guidelines to ensure methodological rigour and transparency.
2.1. Information Sources and Search Strategy
Scopus, PubMed, and Web of Science databases were systematically searched to retrieve relevant publications in June 2025. The search query consisted of the following terms: “Type 1 Diabetes Mellitus” OR “T1DM” OR “T1D” AND “Alexithymia” (see Table 1). No time restrictions were applied in any of the included databases, while only English published research items were considered eligible.

Table 1.
List of terms entered in the database search.
2.2. Eligibility Criteria
Inclusion criteria were full-text articles fully published in English in peer-reviewed journals, confirmed diagnosis of T1DM, and use of validated and standardised psychodiagnostic instruments for the assessment of alexithymia. Exclusion criteria included conference abstracts, literature reviews of any kind, qualitative studies, case reports, studies lacking a clear report of T1DM diagnosis, studies without a transparent description of the inclusion process and studies involving mixed diagnostic groups.
2.3. Selection Process and Data Collection
A thorough screening process was conducted by E.M.M and G.M. before proceeding to the subsequent steps. The initial analysis allowed for the removal of duplicates. Then, titles and abstracts were examined, and only studies meeting the inclusion criteria were selected. A detailed overview of the study selection process is presented in Figure 1 (PRISMA Flow Diagram, see Results).
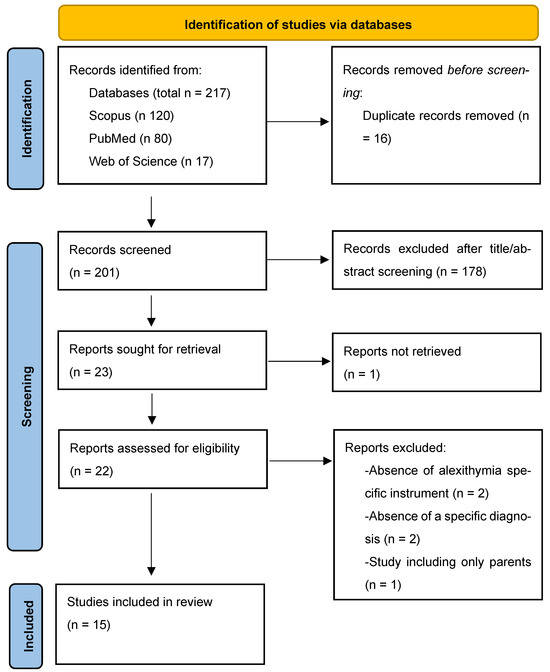
Figure 1.
Prisma Flow Diagram.
2.4. Assessment of the Methodological Quality of the Finally Extracted Studies
The NIH Study Quality Assessment Tool was employed to conduct a comprehensive evaluation of the methodological quality of the selected studies. All included studies ranked from fair to good.
3. Results
As reported in Figure 1, the PRISMA flow diagram highlights the results of the search strategy. In the initial step, 217 articles were identified as potentially eligible. Sixteen duplicates were removed, leaving 201 studies, which were screened based on title and abstract to assess their potential relevance. A total of 179 articles were excluded for not being pertinent to the study aim. Of the 23 remaining articles, 1 was excluded due to the unavailability of the full text. The remaining 22 reports were assessed in full, and 7 were excluded for specific methodological reasons. Ultimately, 15 studies met the inclusion criteria and are summarised in Table 2.

Table 2.
Included studies and main characteristics.
3.1. Characteristics of the Included Studies
From the analyses of the included contributions, twelve were cross-sectional studies [73,75,77,78,79,80,81,82,83,85,86,87], one was longitudinal [76] and two were case–control study [74,84]. Thirteen studies used the Toronto alexithymia scale (TAS-20) [74,76,77,78,79,80,81,82,83,84,85,86,87], one study employed the Children’s Alexithymia Measure (CAM) [73] and another one the Alexithymia Questionnaire for Children (AQC) [75]. Eleven studies included only T1DM participants [73,75,76,77,78,80,81,82,83,85,87], two studies also involved T2DM [79,84], two studies involved healthy controls [74,84], while one study distinguished between T1DM and brittle T1DM patients [86].
Concerning participants’ age groups, nine studies included adult patients [74,76,77,78,79,80,81,85,86]. One study involved a wide age range (15–58 years old) including both adolescents and adults [87]. Among the remaining studies, three focused specifically on adolescents [82,83,84] and two investigated children [73,75].
3.2. Weight and Risk for Obesity
Weight control, obesity risk, and related complications are increasingly recognised as Key issues in the clinical management of T1DM, since obesity is nowadays a frequent finding in T1DM patients, although with some sex- and age-related differences. Five included studies addressed this important theme. Considering the high value of studying the relationship between physical status and alexithymia, Ahmed and colleagues [73] recently highlighted the predictive role of IBM on alexithymia. Sleep disturbances were present in 59.3% of the patients, and a significant relationship emerged between overweight status and sleep disorders. Thus, a diminished quality of life was associated with higher obesity rates. Although the association between BMI and alexithymia was not directly analysed, the co-occurrence of obesity and emotional processing difficulties in the sleep-disturbed subgroup represents a noteworthy relationship that warrants attention.
The risks associated with obesity are well recognised in the scientific community. According to Melin and colleagues [78], the prevalence of abdominal overweight was 17%, with a considerable presence of physical inactivity and alexithymia directly associated. The subdimension Difficulty Identifying Feelings (DIF) was significantly associated with abdominal obesity (p = 0.011), and in a gender-stratified model, DIF remained statistically significant among male participants (p = 0.004). In female patients, abdominal obesity was associated with antidepressant use (p = 0.022) and reduced physical activity (p = 0.037). These findings suggest an indirect pathway linking alexithymia to cardiovascular complications, mediated by abdominal adiposity, and highlight the need for further investigation using longitudinal models. According to a subsequent study Melin and colleagues [80], the prevalence of abdominal obesity was triple in women. the prevalence of abdominal obesity in women was three times higher than in men (24% vs. 8%, p = 0.002). Alexithymia was associated with abdominal obesity in men (p = 0.041), further supporting its role as a relevant psychological risk factor. Moreover, according to previous results [77], and confirmed by recent data [81] the association between obesity and alexithymia appears consistent. Consequently, addressing alexithymia and related emotional dysregulation may contribute to reducing the risk of metabolic and cardiovascular complications in patients with T1DM.
3.3. Glycaemic Control
Glycaemic control is a key component in the management of T1DM, as it plays a central role in preventing negative outcomes. According to Chatzi and colleagues [74], alexithymia was more prevalent in T1DM patients (22%) compared to healthy controls (7.6%), even after adjusting for depressive symptoms. Higher alexithymia scores were positively correlated with illness duration and negatively with treatment intensification. Although no direct relationship with glycaemic control was observed, these findings suggest that alexithymia may influence glycaemic control through behavioural pathways, affecting disease management. According to Housiaux and colleagues [75], alexithymia represents a concrete risk for poor glycaemic control, with the subdimension Difficulty Describing Feelings (DDF) identified as a significant predictor of elevated HbA1c levels (β = 0.34, p = 0.01). Screening for alexithymia in children may provide a reliable basis for early preventive strategies. In adult patients, Luminet and colleagues [76] identified DDF as a significant predictor of poor glucose control, with higher scores associated with elevated glycated haemoglobin at admission and greater HbA1 reduction following treatment. These effects were consistent across both type 1 and type 2 diabetes, and the predictive value of DDF exceeded that of anxiety and depression, further confirming the role of alexithymia in glycaemic regulation and disease progression. A cross-sectional study also indicated an indirect link between alexithymia and glycaemic control, mediated by its association with depressive symptoms, which were independently related to elevated HbA1c levels [77]. T1DM patients with alexithymia were identified by Mnif and colleagues [84] as more exposed to fasting blood sugar than non-alexithymic ones (p = 0.021). These findings are further supported by evidence from adolescent populations. Shayeghian and collaborators [87] observed that DIF significantly predicted higher HbA1c levels in girls with T1DM (β = 0.15, p = 0.03), confirming a gender-specific vulnerability. This study also suggested that alexithymia affect self-care activities, underscoring its detrimental role in diabetes management. Measuring psychological traits and states would increase interventions efficiency and patients’ quality of life.
3.4. General Psychopathology
Psychopathology can be defined as a highly prevalent and heterogeneous set of factors resulting from altered mental functioning. Its role in affecting subjects’ quality of life is widely recognised. In the context of T1DM, several studies highlighted its impact, particularly concerning the predictive role of alexithymia.
According to Mellin et al. [79], T1DM patients were predominantly affected by melancholic depression, with a greater risk of misdiagnosis among alexithymic individuals. The associations between anxiety, depression and alexithymia were described as clinically significant. In a subsequent study [81], the authors reported that depression rates were higher among alexithymic patients, thus confusing the association between depression and alexithymia. A recent study by Merlo and colleagues [82] reported high rates of anxiety, depression and somatic symptoms, with alexithymia strongly linked not only to these conditions but also to intolerance of uncertainty. Building on these findings, a subsequent study confirmed their presence and further indicated that age, gender and education significantly predicted both alexithymia and intolerance to uncertainty [83]. Mnif and collaborators [84] observed that T1DM patients were more frequently alexithymic than those with T2DM. Moreover, in T1DM patients, erectile dysfunction, a common complication of diabetes, was associated with Difficulties Identifying Feelings (DIF). Finally, depression was found to be a predictor of alexithymia.
The study by Naito and colleagues [85] was the only one to examine personality traits alongside alexithymia. Their findings showed that these psychological factors negatively affected awareness of hypoglycaemia in adult T1DM patients. Cognitive barriers, including alexithymia and perfectionism, were identified as contributing factors, and maladaptive health beliefs emerged as threats to both disease progression and effective diabetes management. In line with these results, greater attention should be given to the role of psychopathology and its clear associations with alexithymia in patients with T1DM.
4. Discussion
T1DM is among the most challenging chronic conditions to manage on a daily basis. Constant blood sugar monitoring, fear of hyperglycemia and hypoglycemia, multiple insulin administrations, fear of the potentially debilitating complications, social stigma, and daily life obstacles are just some of the difficulties faced by patients living with T1DM and their families.
This systematic review identified several key psychological and behavioural factors which significantly influence the course of T1DM and the patient’s perceived quality of life. Compared to the abundant literature on T2DM, relatively few studies have examined psychological factors specifically affecting the T1DM trajectory. Thus, analysing the current state of the art to identify influential psychological variables is both timely and necessary. The difficulties associated with T1DM are wide-ranging, covering factors from metabolic regulation to emotional well-being. Among these, diagnostic delays and the failure to consider patients’ psychological functioning represent major clinical risks that may compromise both adaptation and disease management.
Obesity may act both as a risk factor for diabetes onset and as an aggravating element in pre-existing conditions [38,88,89,90,91,92]. However, in the case of T1DM, specific pathophysiological mechanisms must be considered [1,93]. Identifying individual psychological predictors, such as alexithymia, and their associations with other mental health dimensions could represent a significant advancement. The relationship between alexithymia and obesity has been documented [94,95,96], but the case of T1DM is qualitatively distinct due to its intrinsic risks.
According to the evidence presented, physical inactivity, sleep disturbances, direct associations between alexithymia and abdominal obesity, and the predictive value of alexithymia constitutes robust findings. In this context, interventions should be preceded by validated assessment procedures. Given the potentially severe outcomes of T1DM, this interrelated risk factor cannot be overlooked. The connections observed reflect well-established research domains [55,97,98] that must be specifically contextualised within T1DM.
Glycaemic control also emerges as a central determinant in the clinical course of T1DM [99,100,101]. In this domain as well, alexithymia represents a serious concern. Its associations and predictive value are consistent with current findings in the literature [45,102]. While emotional distress has recently been considered a treatment target in T1DM [103], alexithymia remains underexplored. Notably, studies specifically centred on the role of alexithymia in T1DM are lacking.
Alexithymia has been identified as a precursor of maladaptive beliefs, as confirmed by a recent systematic review and meta-analysis [104], although no direct reference to diabetes was made. This highlights the need for future studies that include this clinical population. As previously noted, eating behaviours play a critical role, and conditions such as diabulimia have been recognised as highly influential [105]. Given the impact of alexithymia on individuals’ health status and quality of life [55,57], together with the importance of glycaemic control, these factors must be systematically addressed.
Although alexithymia is not classified as a form of psychopathology, its associations with psychiatric conditions are well documented [106,107,108,109]. According to the findings of this review, a clear link between psychopathology and alexithymia was evident. Given the impact of affective disorders on diabetic patients and their well-being [110,111], closer clinical attention is warranted. Moreover, the risk of missed diagnosis due to alexithymia and its influence on illness-related beliefs has emerged as a relevant issue. This is consistent with the difficulty that alexithymic individuals have in identifying and describing affective states.
As a psychological vulnerability factor [56,112,113], alexithymia may contribute to the onset of psychopathology and worsen existing illness conditions. Conversely, the chronic nature of T1DM can itself trigger reactive psychopathological responses, leading to decreased quality of life and the emergence of typical clinical features. Somatisation disorders may also arise as a direct expression of alexithymic functioning. However, aside from the studies included in this review, data specifically addressing T1DM are still lacking. Therefore, psychopathology should be understood as a multifaceted construct, both influenced by and influencing alexithymia, with important implications for clinical outcomes. As such, clinical pathways must not ignore their presence and potential impact.
T1DM is a serious chronic illness with potentially severe consequences. The fact that most existing research on alexithymia focuses on T2DM represents a major limitation in the current scientific literature. The psychological dimensions of T1DM remain significantly underexplored. In light of what has emerged, alexithymia must not remain a neglected factor. Although it is still necessary to study its impact in the field of T1DM, the results obtained from chronic diseases must serve as a solid basis for further research. In particular, when it comes to chronic conditions that accompany the patient throughout life, the role of these psychological factors is fundamental. As previously reported, pathological outcomes linked to poor management of the disease can be serious [114,115]. In this case, affective dysregulation, the use of inadequate defences and coping has a profound impact on adherence to treatments. In addition to the scarcity of studies, there is a clear need for research designs capable of capturing the dynamic evolution of psychological and physical factors over time.
Through this systematic review, it was possible to highlight these shortcomings and the limitations of the current body of evidence. However, acknowledging these gaps offers a valuable opportunity to advance research and improve knowledge in the field of T1DM.
5. Strengths and Limitations
This review was aimed at portraying the relationship between alexithymia and T1DM. Based on the findings, alexithymia emerges as a clinically relevant risk factor that should be systematically assessed to prevent negative outcomes. However, this review also presents several limitations.
Although all included studies employed quantitative methodologies, the majority adopted a cross-sectional design. The lack of longitudinal data and the limited capacity to detect changes over time, especially in response to psychological or behavioural interventions, may reduce the interpretability and clinical generalisability of the results. Furthermore, considerable heterogeneity was observed in the age groups of participants, ranging from childhood to adulthood. This demographic variability may limit the comparability of findings across studies, although it also highlights the potential burden of alexithymia across different stages of life.
Most of the studies utilised the same assessment instrument for alexithymia, which, while contributing to methodological consistency, limited the possibility of convergent validation with alternative measures. Furthermore, all included studies’ design was quantitative. Qualitative research considering subjective experience could have enriched the panorama. Additionally, the reliance on self-report questionnaires may represent a weakness, as these instruments are susceptible to reporting biases and may not fully capture the clinical complexity of emotional dysregulation. Thus, since most of the results emerged in European contexts, this may limit generalisability.
Despite these limitations, to the best of our knowledge, this is the first systematic review specifically focused on the role of alexithymia in the context of T1DM. The substantial gap in the literature that motivated this review should be addressed through rigorous, longitudinal research capable of generating evidence-based insights and guiding future clinical practice.
6. Conclusions
Through this systematic review, relevant evidence emerged supporting the association between alexithymia and T1DM. The main domains identified were obesity and weight-related difficulties, psychopathology, and glycaemic control.
About obesity, alexithymia was found to influence patients’ weight status, emerging as a potential predictor of obesity. Given the specific metabolic and behavioural dynamics of T1DM, this association raises particular concern.
In the area of psychopathology, alexithymia showed strong associations with anxiety, depression, and somatisation. Across most of the included studies, a clear relationship was observed between alexithymia and general psychopathological burden. Beyond its predictive value, alexithymia was shown to negatively affect patients’ psychological adjustment, overall health status, and the effectiveness of disease management.
Furthermore, glycaemic control, crucial for the long-term prognosis of T1DM, was consistently reported as being adversely influenced by alexithymia. This suggests that alexithymia may represent an emotional barrier to effective diabetes self-management.
These findings should inform clinical practice, encouraging the routine assessment of alexithymia and the implementation of targeted psychological interventions aimed at mitigating its impact on T1DM outcomes.
Author Contributions
Conceptualisation, E.M.M. and G.M.; Methodology, E.M.M. and G.M.; Formal Analysis, E.M.M. and G.M.; Writing—original draft preparation, E.M.M., L.A.M.M., O.S., D.R., G.T.R., G.S. and G.M.; writing—review and editing, E.M.M., L.A.M.M., O.S. and G.M.; Supervision, G.T.R., G.S. and G.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| T2DM | Type 2 Diabetes Mellitus |
| T1DM | Type 1 Diabetes Mellitus |
| T1M | Type 1 Diabetes |
| TAS-20 | Toronto Alexithymia Scale-20 |
| DIF | Difficulty Identifying Feelings |
| DDF | Difficulty Describing Feelings |
| EOT | Externally Oriented Thinking |
| CAM | Children’s Alexithymia Scale |
| AQC | Alexithymia Questionnaire for Children |
| HbA1 | Haemoglobin A1 |
| HbA1c | Haemoglobin A1c |
References
- Quattrin, T.; Mastrandrea, L.D.; Walker, L.S.K. Type 1 diabetes. Lancet 2023, 401, 2149–2162. [Google Scholar] [CrossRef]
- Bazile, C.; Abdel Malik, M.M.; Ackeifi, C.; Anderson, R.L.; Beck, R.W.; Donath, M.Y.; Dutta, S.; Hedrick, J.A.; Karpen, S.R.; Kay, T.W.H.; et al. TNF-alpha inhibitors for type 1 diabetes: Exploring the path to a pivotal clinical trial. Front. Immunol. 2024, 15, 1470677. [Google Scholar] [CrossRef] [PubMed]
- Mastrandrea, L.D.; Quattrin, T. Preventing type 1 diabetes development and preserving beta-cell function. Curr. Opin. Endocrinol. Diabetes Obes. 2022, 29, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Gong, B.; Yang, W.; Xing, Y.; Lai, Y.; Shan, Z. Global, regional, and national burden of type 1 diabetes in adolescents and young adults. Pediatr. Res. 2025, 97, 568–576. [Google Scholar] [CrossRef] [PubMed]
- Tomic, D.; Shaw, J.E.; Magliano, D.J. The burden and risks of emerging complications of diabetes mellitus. Nat. Rev. Endocrinol. 2022, 18, 525–539. [Google Scholar] [CrossRef]
- Powers, A.C. Type 1 diabetes mellitus: Much progress, many opportunities. J. Clin. Investig. 2021, 131, e142242. [Google Scholar] [CrossRef]
- Martino, G.; Di Giuseppe, M.; Silvestro, O.; Vicario, C.M.; Giorgianni, C.M.; Ruggeri, P.; Sparacino, G.; Juli, M.R.; Schwarz, P.; Lingiardi, V.; et al. Defense mechanisms in immune-mediated diseases: A cross-sectional study focusing on Severe Allergic Asthma and Hymenoptera Venom Anaphylaxis patients. Front. Psychol. 2025, 16, 1608335. [Google Scholar] [CrossRef]
- Caputo, A.; Vicario, C.M.; Cazzato, V.; Martino, G. Editorial: Psychological Factors as Determinants of Medical Conditions, Volume II. Front. Psychol. 2022, 13, 865235. [Google Scholar] [CrossRef]
- Conversano, C. Common Psychological Factors in Chronic Diseases. Front. Psychol. 2019, 10, 2727. [Google Scholar] [CrossRef]
- Perrin, J.M.; Gnanasekaran, S.; Delahaye, J. Psychological aspects of chronic health conditions. Pediatr. Rev. 2012, 33, 99–109. [Google Scholar] [CrossRef]
- Stanton, A.L.; Revenson, T.A.; Tennen, H. Health psychology: Psychological adjustment to chronic disease. Annu. Rev. Psychol. 2007, 58, 565–592. [Google Scholar] [CrossRef]
- Enyinnaya Calistus, J.; Joshua Oluwasegun, A.; Oluwaseun, I.; Lucy Oluebubechi, K.; Anjolaoluwa Joy, O.; Kaosara Temitope, A.; Mary Oluwasayo, T. Psychosocial factors in chronic disease management: Implications for health psychology. Int. J. Sci. Res. Arch. 2024, 12, 117–128. [Google Scholar] [CrossRef]
- Fisher, L.; Dickinson, W.P. Psychology and primary care: New collaborations for providing effective care for adults with chronic health conditions. Am. Psychol. 2014, 69, 355–363. [Google Scholar] [CrossRef]
- Helgeson, V.S.; Zajdel, M. Adjusting to Chronic Health Conditions. Annu. Rev. Psychol. 2017, 68, 545–571. [Google Scholar] [CrossRef] [PubMed]
- Silvestro, O.; Vicario, C.M.; Costa, L.; Sparacino, G.; Lund-Jacobsen, T.; Spatola, C.A.M.; Merlo, E.M.; Viola, A.; Giorgianni, C.M.; Catalano, A.; et al. Defense mechanisms and inflammatory bowel diseases: A narrative review. Res. Psychother. 2025, 28, 854. [Google Scholar] [CrossRef] [PubMed]
- Merlo, E.M.; Myles, L.A.; Martino, G. On the Critical Nature of Psychosomatics in Clinical Practice. Clin. Psychol. Eur. 2025, 7, 1–3. [Google Scholar] [CrossRef]
- Nieuwesteeg, A.; Pouwer, F.; van der Kamp, R.; van Bakel, H.; Aanstoot, H.J.; Hartman, E. Quality of life of children with type 1 diabetes: A systematic review. Curr. Diabetes Rev. 2012, 8, 434–443. [Google Scholar] [CrossRef]
- Rosner, B.; Roman-Urrestarazu, A. Health-related quality of life in paediatric patients with Type 1 diabetes mellitus using insulin infusion systems. A systematic review and meta-analysis. PLoS ONE 2019, 14, e0217655. [Google Scholar] [CrossRef]
- Novato Tde, S.; Grossi, S.A. Factors associated to the quality of life of adolescents with type 1 diabetes mellitus. Rev. Esc. Enferm. USP 2011, 45, 770–776. [Google Scholar] [CrossRef]
- Turin, A.; Drobnic Radobuljac, M. Psychosocial factors affecting the etiology and management of type 1 diabetes mellitus: A narrative review. World J. Diabetes 2021, 12, 1518–1529. [Google Scholar] [CrossRef]
- Martinez, K.; Frazer, S.F.; Dempster, M.; Hamill, A.; Fleming, H.; McCorry, N.K. Psychological factors associated with diabetes self-management among adolescents with Type 1 diabetes: A systematic review. J. Health Psychol. 2018, 23, 1749–1765. [Google Scholar] [CrossRef]
- Sharif, K.; Watad, A.; Coplan, L.; Amital, H.; Shoenfeld, Y.; Afek, A. Psychological stress and type 1 diabetes mellitus: What is the link? Expert Rev. Clin. Immunol. 2018, 14, 1081–1088. [Google Scholar] [CrossRef]
- Akbarizadeh, M.; Naderi Far, M.; Ghaljaei, F. Prevalence of depression and anxiety among children with type 1 and type 2 diabetes: A systematic review and meta-analysis. World J. Pediatr. 2022, 18, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Stene, L.C.; Norris, J.M.; Rewers, M.J. Risk factors for type 1 diabetes. In National Institute of Diabetes & Digestive & Kidney Diseases Pamphlets (NIDDK); National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, ML, USA, 2023. [Google Scholar]
- Sivertsen, B.; Petrie, K.J.; Wilhelmsen-Langeland, A.; Hysing, M. Mental health in adolescents with Type 1 diabetes: Results from a large population-based study. BMC Endocr. Disord. 2014, 14, 83. [Google Scholar] [CrossRef]
- Marchini, F.; Langher, V.; Napoli, A.; Balonan, J.T.; Fedele, F.; Martino, G.; Amorosi, F.R.; Caputo, A. Unconscious loss processing in diabetes: Associations with medication adherence and quality of care. Psychoanal. Psychother. 2021, 35, 5–23. [Google Scholar] [CrossRef]
- Martino, G.; Bellone, F.; Langher, V.; Caputo, A.; Catalano, A.; Quattropani, M.C.; Morabito, N. Alexithymia and psychological distress affect perceived quality of life in patients with type 2 diabetes mellitus. Mediterr. J. Clin. Psychol. 2019, 7, 1–15. [Google Scholar] [CrossRef]
- Moroianu, L.A.; Motofei, I.G.; Cecilia, C.; Barbu, R.E.; Toma, A. The impact of anxiety and depression on the pediatric patients with diabetes. Mediterr. J. Clin. Psychol. 2020, 8. [Google Scholar] [CrossRef]
- Pușcașu, A.; Bolocan, A.; Păduraru, D.N.; Salmen, T.; Bica, C.; Andronic, O. The implications of chronic psychological stress in the development of diabetes mellitus type 2. Mediterr. J. Clin. Psychol. 2022, 10, 1–14. [Google Scholar]
- Ademoyegun, A.B.; Afolabi, O.E.; Aghedo, I.A.; Adelowokan, O.I.; Mbada, C.E.; Awotidebe, T.O. The mediating role of sedentary behaviour in the relationship between social support and depression among individuals with diabetes. Mediterr. J. Clin. Psychol. 2022, 10, 1–26. [Google Scholar] [CrossRef]
- Ingrosso, D.M.F.; Primavera, M.; Samvelyan, S.; Tagi, V.M.; Chiarelli, F. Stress and Diabetes Mellitus: Pathogenetic Mechanisms and Clinical Outcome. Horm. Res. Paediatr. 2023, 96, 34–43. [Google Scholar] [CrossRef]
- Theofilou, P.; Vlastos, D.D. The Psychological Burden of Families with Diabetic Children: A Literature Review Focusing on Quality of Life and Stress. Children 2023, 10, 937. [Google Scholar] [CrossRef] [PubMed]
- Gondek, T.M.; Kiejna, A.; Cichoń, E.; Kokoszka, A.; Bobrov, A.; de Girolamo, G.; Lecic-Tosevski, D.; Mankovsky, B.; Müssig, K.; Wölwer, W. Anxiety disorders as predictors of suicidality in people with type 2 diabetes mellitus: Findings of a study in six European countries. Psychiatr. Pol. 2024, 58, 7–24. [Google Scholar] [CrossRef] [PubMed]
- Łukasiewicz, A.; Kiejna, A.; Cichoń, E.; Jodko-Modlińska, A.; Obrębski, M.; Kokoszka, A. Relations of well-being, coping styles, perception of self-influence on the diabetes course and sociodemographic characteristics with HbA1c and BMI among people with advanced type 2 diabetes mellitus. Diabetes Metab. Syndr. Obes. Targets Ther. 2022, 15, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Łukasiewicz, A.; Cichoń, E.; Kostecka, B.; Kiejna, A.; Jodko-Modlińska, A.; Obrębski, M.; Kokoszka, A. Association of higher rates of type 2 diabetes (T2DM) complications with psychological and demographic variables: Results of a cross-sectional study. Diabetes Metab. Syndr. Obes. Targets Ther. 2022, 15, 3303–3317. [Google Scholar] [CrossRef]
- Lloyd, C.; Sartorius, N.; Ahmed, H.; Alvarez, A.; Bahendeka, S.; Bobrov, A.; Burti, L.; Chaturvedi, S.; Gaebel, W.; De Girolamo, G. Factors associated with the onset of major depressive disorder in adults with type 2 diabetes living in 12 different countries: Results from the INTERPRET-DD prospective study. Epidemiol. Psychiatr. Sci. 2020, 29, e134. [Google Scholar] [CrossRef]
- Vilarrasa, N.; San Jose, P.; Rubio, M.A.; Lecube, A. Obesity in Patients with Type 1 Diabetes: Links, Risks and Management Challenges. Diabetes Metab. Syndr. Obes. 2021, 14, 2807–2827. [Google Scholar] [CrossRef]
- Van der Schueren, B.; Ellis, D.; Faradji, R.N.; Al-Ozairi, E.; Rosen, J.; Mathieu, C. Obesity in people living with type 1 diabetes. Lancet Diabetes Endocrinol. 2021, 9, 776–785. [Google Scholar] [CrossRef]
- Steptoe, A.; Frank, P. Obesity and psychological distress. Phil. Trans. R. Soc. B Biol. Sci. 2023, 378, 20220225. [Google Scholar] [CrossRef]
- de la Portilla Maya, S.R.; de la Portilla Maya, D.A.; Londoño, D.M.M.; Martínez, D.A.L. Association Between Obesity, Executive Functions, and Affective States: An Analysis of Patients from an Endocrinology Clinic. Mediterr. J. Clin. Psychol. 2025, 13, 1–24. [Google Scholar] [CrossRef]
- Batt, E.; Asif-Malik, A. A narrative review of the current literature into the impacts of fasting on levels of impulsivity and psychological stress. Mediterr. J. Clin. Psychol. 2025, 13, 1–15. [Google Scholar] [CrossRef]
- Klanduchova, E.; Adamovska, L. Emotion and Stress Related Eating and Personality Dimensions Predict Food Addiction: Implications for Personalized Weight Management and Primary Prevention. Mediterr. J. Clin. Psychol. 2025, 13, 1–20. [Google Scholar] [CrossRef]
- Lucifora, C.; Martino, G.; Grasso, G.; Mucciardi, M.; Magnano, P.; Massimino, S.; Craparo, G.; Vicario, C.M. Does Fasting Make Us All Equal? Evidence on the Influence of Appetite on Implicit Sexual Prejudice. Mediterr. J. Clin. Psychol. 2025, 13, 1–22. [Google Scholar] [CrossRef]
- Khadilkar, A.; Oza, C. Glycaemic Control in Youth and Young Adults: Challenges and Solutions. Diabetes Metab. Syndr. Obes. 2022, 15, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Bitew, Z.W.; Alemu, A.; Jember, D.A.; Tadesse, E.; Getaneh, F.B.; Sied, A.; Weldeyonnes, M. Prevalence of Glycemic Control and Factors Associated With Poor Glycemic Control: A Systematic Review and Meta-analysis. Inquiry 2023, 60, 469580231155716. [Google Scholar] [CrossRef]
- Bashir, T.; Morrissey, H.; Ball, P. Systematic Review of Psychological and Educational Interventions Used to Improving Adherence in Diabetes and Depression Patients. Arch. Pharm. Pract. 2021, 12, 1–11. [Google Scholar] [CrossRef]
- Preece, D.A.; Gross, J.J. Conceptualizing alexithymia. Personal. Individ. Differ. 2023, 215, 112375. [Google Scholar] [CrossRef]
- Lesser, I.M. A review of the alexithymia concept. Psychosom. Med. 1981, 43, 531–543. [Google Scholar] [CrossRef]
- Timoney, L.R.; Holder, M.D.; Timoney, L.R.; Holder, M.D. Definition of alexithymia. In Emotional Processing Deficits and Happiness: Assessing the Measurement, Correlates, and Well-Being of People with Alexithymia; Springer: Berlin/Heidelberg, Germany, 2013; pp. 1–6. [Google Scholar] [CrossRef]
- Taylor, G.J. Alexithymia: 25 years of theory and research. In Emotional Expression and Health: Advances in Theory, Assessment and Clinical Applications; Taylor & Francis Group: Oxfordshire, UK, 2004; pp. 137–153. [Google Scholar]
- Martino, G.; Caputo, A.; Vicario, C.M.; Catalano, A.; Schwarz, P.; Quattropani, M.C. The Relationship Between Alexithymia and Type 2 Diabetes: A Systematic Review. Front. Psychol. 2020, 11, 2026. [Google Scholar] [CrossRef]
- Pei, J.H.; Wei, Y.T.; Tao, H.X.; Yang, Q.X.; Zhang, G.L.; Guo, X.J.; Guo, J.L.; Yan, F.H.; HanPh, D.L. The prevalence and characteristics of alexithymia in patients with type 2 diabetes mellitus: A systematic review and meta-analysis. J. Psychosom. Res. 2022, 162, 111018. [Google Scholar] [CrossRef]
- Silvestro, O.; Ricciardi, L.; Catalano, A.; Vicario, C.M.; Tomaiuolo, F.; Pioggia, G.; Squadrito, G.; Schwarz, P.; Gangemi, S.; Martino, G. Alexithymia and asthma: A systematic review. Front. Psychol. 2023, 14, 1221648. [Google Scholar] [CrossRef]
- Lumley, M.A.; Beyer, J.; Radcliffe, A. Alexithymia and physical health problems: A critique of potential pathways and a research agenda. In Emotion Regulation: Conceptual and Clinical Issues; Springer: Berlin/Heidelberg, Germany, 2008; pp. 43–68. [Google Scholar] [CrossRef]
- Lumley, M.A.; Stettner, L.; Wehmer, F. How are alexithymia and physical illness linked? A review and critique of pathways. J. Psychosom. Res. 1996, 41, 505–518. [Google Scholar] [CrossRef] [PubMed]
- Kojima, M. Alexithymia as a prognostic risk factor for health problems: A brief review of epidemiological studies. Biopsychosoc. Med. 2012, 6, 21. [Google Scholar] [CrossRef] [PubMed]
- Kano, M.; Fukudo, S. The alexithymic brain: The neural pathways linking alexithymia to physical disorders. Biopsychosoc. Med. 2013, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Luminet, O.; Nielson, K.A. Alexithymia: Toward an Experimental, Processual Affective Science with Effective Interventions. Annu. Rev. Psychol. 2025, 76, 741–769. [Google Scholar] [CrossRef]
- Gangemi, S.; Ricciardi, L.; Caputo, A.; Giorgianni, C.; Furci, F.; Spatari, G.; Martino, G. Alexithymia in an unconventional sample of Forestry Officers: A clinical psychological study with surprising results. Mediterr. J. Clin. Psychol. 2021, 9, 1–18. [Google Scholar] [CrossRef]
- Ricciardi, L.; Spatari, G.; Vicario, C.M.; Liotta, M.; Cazzato, V.; Gangemi, S.; Martino, G. Clinical Psychology and Clinical Immunology: Is there a link between Alexithymia and severe Asthma? Mediterr. J. Clin. Psychol. 2023, 11, 1–18. [Google Scholar] [CrossRef]
- Di Giuseppe, M.; Conversano, C. Psychological components of chronic diseases: The link between defense mechanisms and alexithymia. Mediterr. J. Clin. Psychol. 2022, 10, 1–11. [Google Scholar] [CrossRef]
- Giorgianni, C.M.; Martino, G.; Brunetto, S.; Buta, F.; Lund-Jacobsen, T.; Tonacci, A.; Gangemi, S.; Ricciardi, L. Allergic Sensitization and psychosomatic involvement in outdoor and indoor workers: A preliminary and explorative survey of motorway toll collectors and office employees. Healthcare 2024, 12, 1429. [Google Scholar] [CrossRef]
- Rady, A.; Alamrawy, R.; Ramadan, I.; Elmissiry, M. Alexithymia among patients with unexplained physical symptoms. Eur. Psychiatry 2021, 64, S249–S250. [Google Scholar] [CrossRef]
- Tsubaki, K.; Shimizu, E. Psychological Treatments for Alexithymia: A Systematic Review. Behav. Sci. 2024, 14, 1173. [Google Scholar] [CrossRef]
- Luminet, O.; Bagby, R.M.; Taylor, G.J. Alexithymia: Advances in Research, Theory, and Clinical Practice; Cambridge University Press: Cambridge, UK, 2018. [Google Scholar] [CrossRef]
- Meza-Concha, N.; Arancibia, M.; Salas, F.; Behar, R.; Salas, G.; Silva, H.; Escobar, R. Towards a neurobiological understanding of alexithymia. Medwave 2017, 17, e6960. [Google Scholar] [CrossRef]
- Lumley, M.A.; Neely, L.C.; Burger, A.J. The assessment of alexithymia in medical settings: Implications for understanding and treating health problems. J. Personal. Assess. 2007, 89, 230–246. [Google Scholar] [CrossRef] [PubMed]
- Donges, U.-S.; Suslow, T. Alexithymia and automatic processing of emotional stimuli: A systematic review. Rev. Neurosci. 2017, 28, 247–264. [Google Scholar] [CrossRef]
- Panayiotou, G.; Panteli, M.; Vlemincx, E. Adaptive and maladaptive emotion processing and regulation, and the case of alexithymia. Cogn. Emot. 2021, 35, 488–499. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ahmed, G.K.; Hasaballa, E.I.; Abdalla, A.A.; Refaee, A.; Nofal, M.; Shaban, M.; Abdurrahman, E.A.M.; Shehata, S.; Alsaied, R. Relationship between sleep disturbances, alexithymia, psychiatric problems, and clinical variables in children with type 1 diabetes mellitus. Middle East Curr. Psychiatry 2024, 31, 101. [Google Scholar] [CrossRef]
- Chatzi, L.; Bitsios, P.; Solidaki, E.; Christou, I.; Kyrlaki, E.; Sfakianaki, M.; Kogevinas, M.; Kefalogiannis, N.; Pappas, A. Type 1 diabetes is associated with alexithymia in nondepressed, non-mentally ill diabetic patients: A case-control study. J. Psychosom. Res. 2009, 67, 307–313. [Google Scholar] [CrossRef]
- Housiaux, M.; Luminet, O.; Van Broeck, N.; Dorchy, H. Alexithymia is associated with glycaemic control of children with type 1 diabetes. Diabetes Metab. 2010, 36, 455–462. [Google Scholar] [CrossRef]
- Luminet, O.; de Timary, P.; Buysschaert, M.; Luts, A. The role of alexithymia factors in glucose control of persons with type 1 diabetes: A pilot study. Diabetes Metab. 2006, 32, 417–424. [Google Scholar] [CrossRef]
- Melin, E.O.; Thunander, M.; Svensson, R.; Landin-Olsson, M.; Thulesius, H.O. Depression, obesity, and smoking were independently associated with inadequate glycemic control in patients with type 1 diabetes. Eur. J. Endocrinol. 2013, 168, 861–869. [Google Scholar] [CrossRef]
- Melin, E.O.; Svensson, R.; Thunander, M.; Hillman, M.; Thulesius, H.O.; Landin-Olsson, M. Gender, alexithymia and physical inactivity associated with abdominal obesity in type 1 diabetes mellitus: A cross sectional study at a secondary care hospital diabetes clinic. BMC Obes. 2017, 4, 21. [Google Scholar] [CrossRef] [PubMed]
- Melin, E.O.; Thunander, M.; Landin-Olsson, M.; Hillman, M.; Thulesius, H.O. Depression differed by midnight cortisol secretion, alexithymia and anxiety between diabetes types: A cross sectional comparison. BMC Psychiatry 2017, 17, 335. [Google Scholar] [CrossRef] [PubMed]
- Melin, E.O.; Hillman, M.; Thunander, M.; Landin-Olsson, M. Midnight salivary cortisol secretion and the use of antidepressants were associated with abdominal obesity in women with type 1 diabetes: A cross sectional study. Diabetol. Metab. Syndr. 2019, 11, 88. [Google Scholar] [CrossRef] [PubMed]
- Melin, E.O.; Svensson, R.; Dereke, J.; Hillman, M. Galectin-3 Binding Protein, Depression, and Younger Age Were Independently Associated With Alexithymia in Adult Patients With Type 1 Diabetes. Front. Psychiatry 2021, 12, 672931. [Google Scholar] [CrossRef] [PubMed]
- Merlo, E.M.; Tutino, R.; Myles, L.A.M.; Lia, M.C.; Minasi, D. Alexithymia, intolerance to uncertainty and mental health difficulties in adolescents with Type 1 diabetes mellitus. Ital. J. Pediatr. 2024, 50, 99. [Google Scholar] [CrossRef]
- Merlo, E.M.; Tutino, R.; Myles, L.A.M.; Alibrandi, A.; Lia, M.C.; Minasi, D. Type 1 Diabetes Mellitus, Psychopathology, Uncertainty and Alexithymia: A Clinical and Differential Exploratory Study. Healthcare 2024, 12, 257. [Google Scholar] [CrossRef]
- Mnif, L.; Damak, R.; Mnif, F.; Ouanes, S.; Abid, M.; Jaoua, A.; Masmoudi, J. Alexithymia impact on type 1 and type 2 diabetes: A case-control study. Ann. Endocrinol. 2014, 75, 213–219. [Google Scholar] [CrossRef]
- Naito, A.; Nwokolo, M.; Smith, E.L.; de Zoysa, N.; Garrett, C.; Choudhary, P.; Amiel, S.A. Personality traits of alexithymia and perfectionism in impaired awareness of hypoglycemia in adults with type 1 diabetes—An exploratory study. J. Psychosom. Res. 2021, 150, 110634. [Google Scholar] [CrossRef]
- Pelizza, L.; Pupo, S. Alexithymia in adults with brittle type 1 diabetes. Acta Biomed. 2019, 90, 279–287. [Google Scholar] [CrossRef]
- Shayeghian, Z.; Moeineslam, M.; Hajati, E.; Karimi, M.; Amirshekari, G.; Amiri, P. The relation of alexithymia and attachment with type 1 diabetes management in adolescents: A gender-specific analysis. BMC Psychol. 2020, 8, 30. [Google Scholar] [CrossRef] [PubMed]
- Boutari, C.; DeMarsilis, A.; Mantzoros, C.S. Obesity and diabetes. Diabetes Res. Clin. Pract. 2023, 202, 110773. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.; Gastaldelli, A.; Yki-Jarvinen, H.; Scherer, P.E. Why does obesity cause diabetes? Cell Metab. 2022, 34, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Rohm, T.V.; Meier, D.T.; Olefsky, J.M.; Donath, M.Y. Inflammation in obesity, diabetes, and related disorders. Immunity 2022, 55, 31–55. [Google Scholar] [CrossRef]
- Giandalia, A.; Russo, G.T.; Ruggeri, P.; Giancaterini, A.; Brun, E.; Cristofaro, M.; Bogazzi, A.; Rossi, M.C.; Lucisano, G.; Rocca, A. The burden of obesity in type 1 diabetic subjects: A sex-specific analysis from the AMD annals initiative. J. Clin. Endocrinol. Metab. 2023, 108, e1224–e1235. [Google Scholar] [CrossRef]
- Kueh, M.T.; Chew, N.W.; Al-Ozairi, E.; le Roux, C.W. The emergence of obesity in type 1 diabetes. Int. J. Obes. 2024, 48, 289–301. [Google Scholar] [CrossRef]
- Syed, F.Z. Type 1 Diabetes Mellitus. Ann. Intern. Med. 2022, 175, ITC33–ITC48. [Google Scholar] [CrossRef]
- Fanton, S.; Azevedo, L.C.; Vargas, D.M. Alexithymia in obese adolescents is associated with severe obesity and binge eating behavior. J. Pediatr. 2022, 98, 264–269. [Google Scholar] [CrossRef]
- Karukivi, M.; Jula, A.; Hutri-Kahonen, N.; Juonala, M.; Raitakari, O. Is alexithymia associated with metabolic syndrome? A study in a healthy adult population. Psychiatry Res. 2016, 236, 58–63. [Google Scholar] [CrossRef]
- Koyuncu, Z.; Kadak, M.T.; Tarakcioglu, M.C.; Bingol Caglayan, R.H.; Dogangun, B.; Ercan, O. Eating behaviors and alexithymic features of obese and overweight adolescents. Pediatr. Int. 2022, 64, e15008. [Google Scholar] [CrossRef] [PubMed]
- Alimoradi, Z.; Majd, N.R.; Brostrom, A.; Tsang, H.W.H.; Singh, P.; Ohayon, M.M.; Lin, C.Y.; Pakpour, A.H. Is alexithymia associated with sleep problems? A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2022, 133, 104513. [Google Scholar] [CrossRef] [PubMed]
- Conti, C.; Di Francesco, G.; Severo, M.; Lanzara, R.; Richards, K.; Guagnano, M.T.; Porcelli, P. Alexithymia and metabolic syndrome: The mediating role of binge eating. Eat. Weight Disord. 2021, 26, 1813–1823. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.J.; Wang, W.; Lim, S.T.; Wu, V.X. Factors associated with glycaemic control in patients with diabetes mellitus: A systematic literature review. J. Clin. Nurs. 2019, 28, 1433–1450. [Google Scholar] [CrossRef]
- McKnight, J.A.; Wild, S.H.; Lamb, M.J.; Cooper, M.N.; Jones, T.W.; Davis, E.A.; Hofer, S.; Fritsch, M.; Schober, E.; Svensson, J.; et al. Glycaemic control of Type 1 diabetes in clinical practice early in the 21st century: An international comparison. Diabet. Med. 2015, 32, 1036–1050. [Google Scholar] [CrossRef]
- Perkins, B.A.; Sherr, J.L.; Mathieu, C. Type 1 diabetes glycemic management: Insulin therapy, glucose monitoring, and automation. Science 2021, 373, 522–527. [Google Scholar] [CrossRef]
- Costa, V.; Pereira, B.; Patton, S.R.; Brandao, T. Parental Psychosocial Variables and Glycemic Control in T1D Pediatric Age: A Systematic Review. Curr. Diabetes Rep. 2024, 25, 11. [Google Scholar] [CrossRef]
- Franc, S.; Charpentier, G. Emotional distress as a therapeutic target against persistent poor glycaemic control in subjects with type 1 diabetes: A systematic review. Diabetes Obes. Metab. 2025, 27, 4662–4673. [Google Scholar] [CrossRef]
- Pilkington, P.D.; Karantzas, G.C.; Faustino, B.; Pizarro-Campagna, E. Early maladaptive schemas, emotion regulation difficulties and alexithymia: A systematic review and meta-analysis. Clin. Psychol. Psychother. 2024, 31, e2914. [Google Scholar] [CrossRef]
- Yahya, A.S.; Khawaja, S.; Naguib, M. ‘Diabulimia’: Current insights into type 1 diabetes and bulimia nervosa. Prog. Neurol. Psychiatry 2023, 27, 44–49. [Google Scholar] [CrossRef]
- Grabe, H.J.; Spitzer, C.; Freyberger, H.J. Alexithymia and personality in relation to dimensions of psychopathology. Am. J. Psychiatry 2004, 161, 1299–1301. [Google Scholar] [CrossRef]
- Hemming, L.; Haddock, G.; Shaw, J.; Pratt, D. Alexithymia and Its Associations With Depression, Suicidality, and Aggression: An Overview of the Literature. Front. Psychiatry 2019, 10, 203. [Google Scholar] [CrossRef] [PubMed]
- Sagar, R.; Talwar, S.; Desai, G.; Chaturvedi, S.K. Relationship between alexithymia and depression: A narrative review. Indian. J. Psychiatry 2021, 63, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Taylor, G.J.; Bagby, R.M. New trends in alexithymia research. Psychother. Psychosom. 2004, 73, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Deniz-Garcia, A.; Diaz-Artiles, A.; Saavedra, P.; Alvarado-Martel, D.; Wagner, A.M.; Boronat, M. Impact of anxiety, depression and disease-related distress on long-term glycaemic variability among subjects with Type 1 diabetes mellitus. BMC Endocr. Disord. 2022, 22, 122. [Google Scholar] [CrossRef]
- Navas Moreno, V.; Sager La Ganga, C.; Tapia Sanchiz, M.S.; Lopez Ruano, M.; Del Carmen Martinez Otero, M.; Carrillo Lopez, E.; Raposo Lopez, J.J.; Amar, S.; Gonzalez Castanar, S.; Marazuela, M.; et al. Impact of psychiatric disorders on the risk of diabetic ketoacidosis in adults with type 1 diabetes mellitus: A propensity score matching case-control study. Endocrine 2025, 88, 127–134. [Google Scholar] [CrossRef]
- Baiardini, I.; Abba, S.; Ballauri, M.; Vuillermoz, G.; Braido, F. Alexithymia and chronic diseases: The state of the art. G. Ital. Med. Lav. Ergon. 2011, 33, A47–A52. [Google Scholar]
- Wen, J.; Wu, Y.; Peng, L.; Chen, S.; Yuan, J.; Wang, W.; Cong, L. Constructing and Verifying an Alexithymia Risk-Prediction Model for Older Adults with Chronic Diseases Living in Nursing Homes: A Cross-Sectional Study in China. Geriatrics 2022, 7, 139. [Google Scholar] [CrossRef]
- Galletti, B.; Freni, F.; Meduri, A.; Oliverio, G.W.; Signorino, G.A.; Perroni, P.; Galletti, C.; Aragona, P.; Galletti, F. Rhi-no-Orbito-Cerebral Mucormycosis in Diabetic Disease Mucormycosis in Diabetic Disease. J. Craniofacial Surg. 2020, 31, e321–e324. [Google Scholar] [CrossRef]
- Oliverio, G.W.; Meduri, A.; De Salvo, G.; Trombetta, L.; Aragona, P. OCT Angiography Features in Diabetes Mellitus Type 1 and 2. Diagnostics 2022, 12, 2942. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).