Visualization of Medical Record with 3D Human Body Models
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature
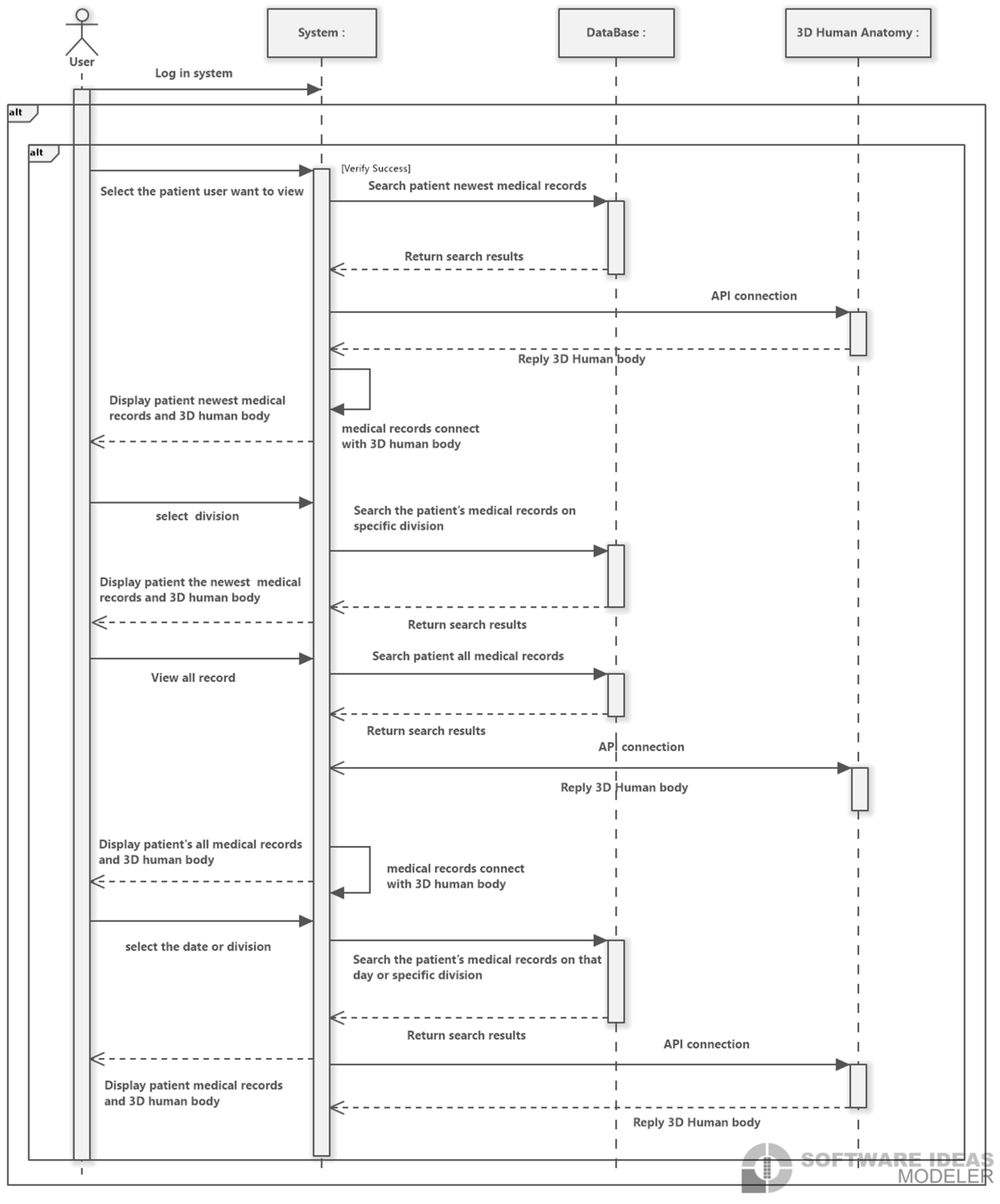
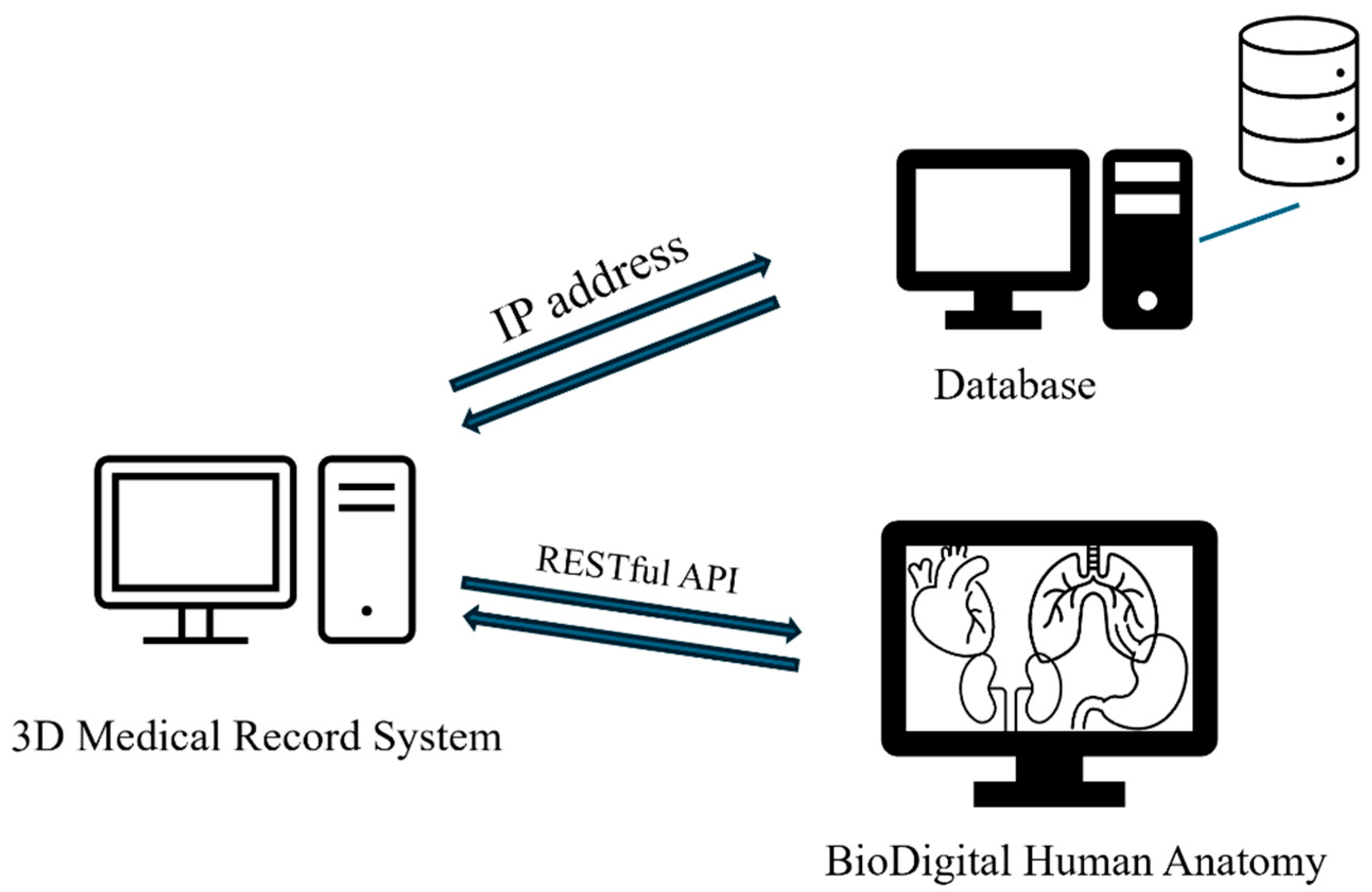
2.2. System Architecture and Backend Logic
3. Results and Experiment
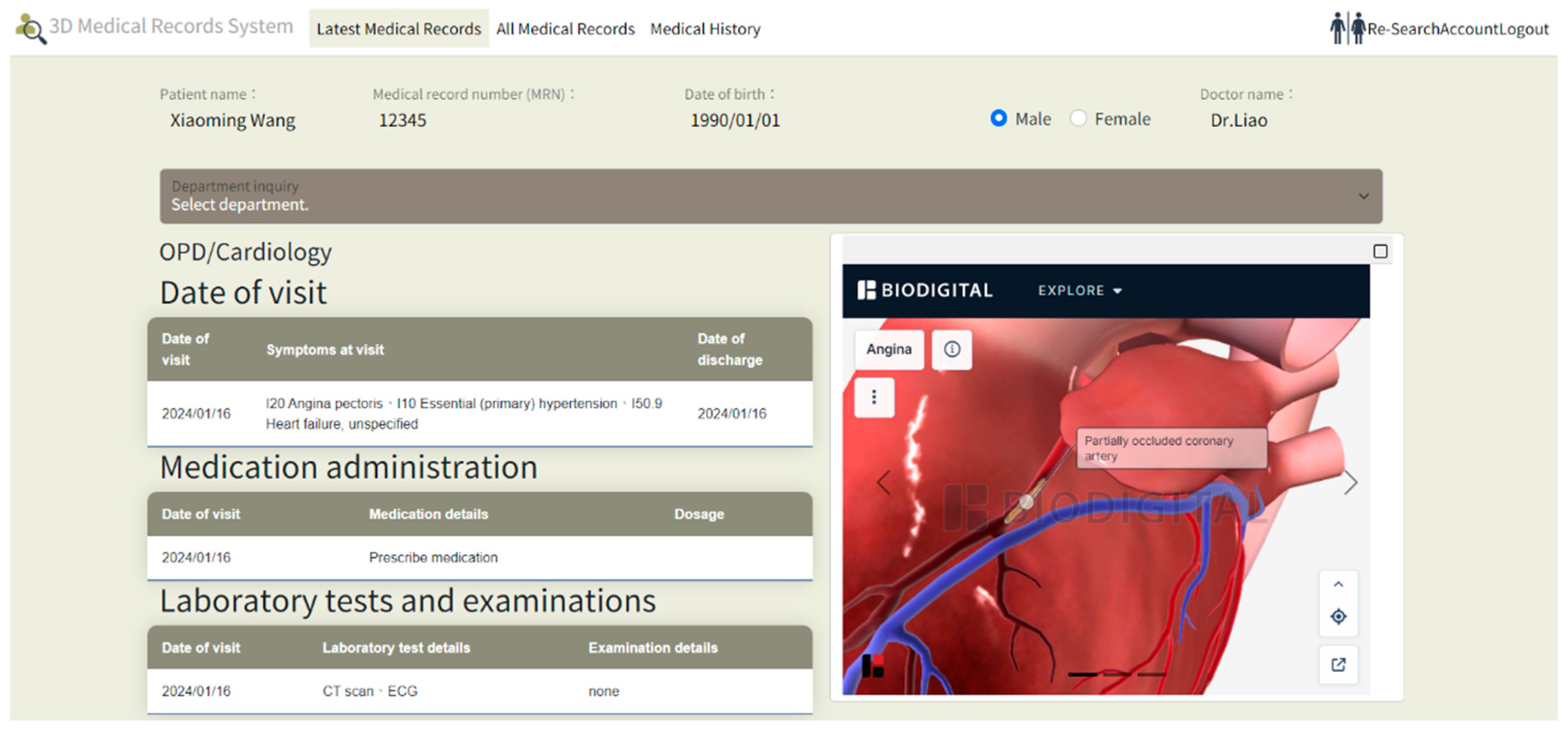
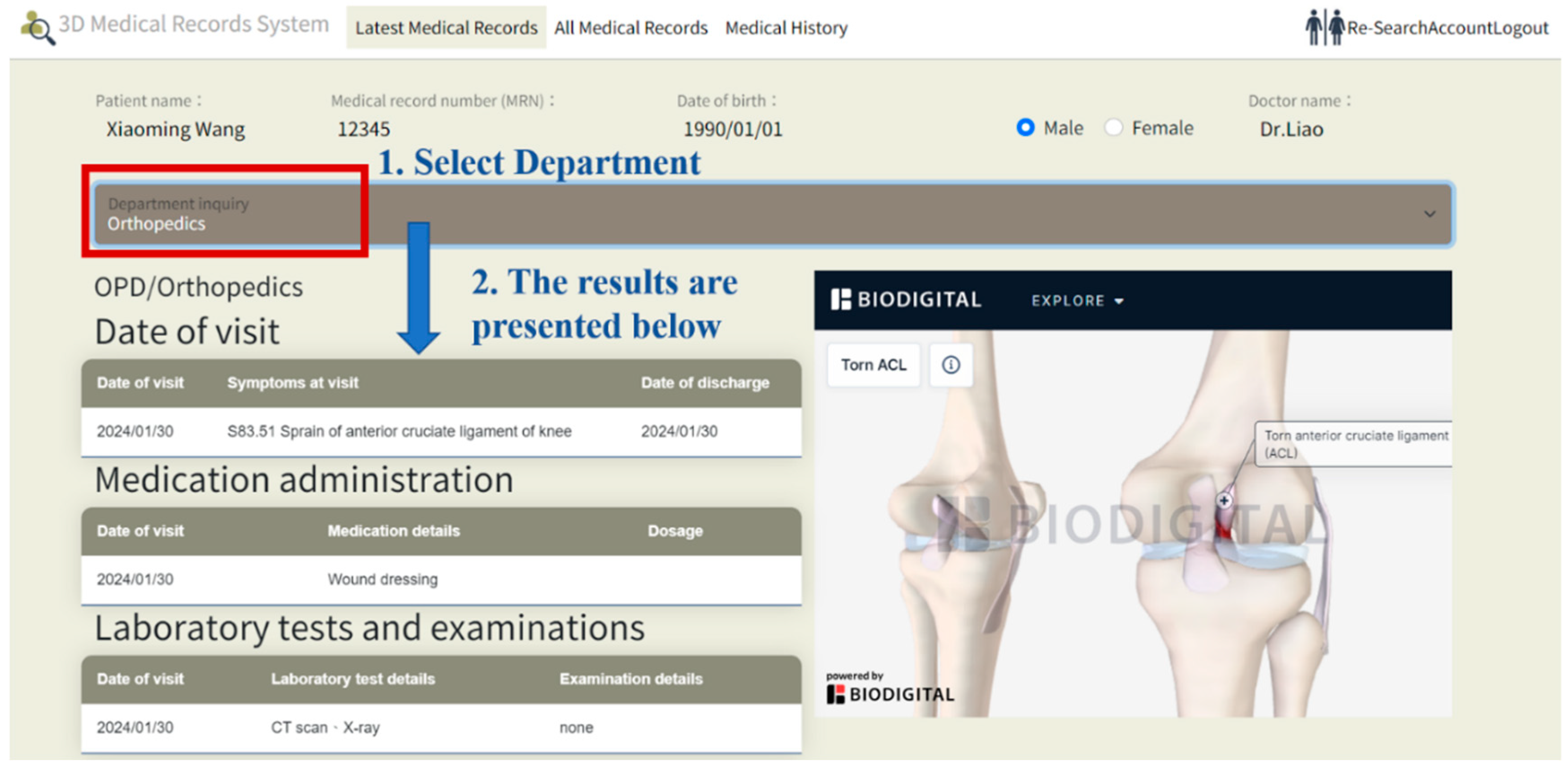
3.1. Results of Visualization Pipeline
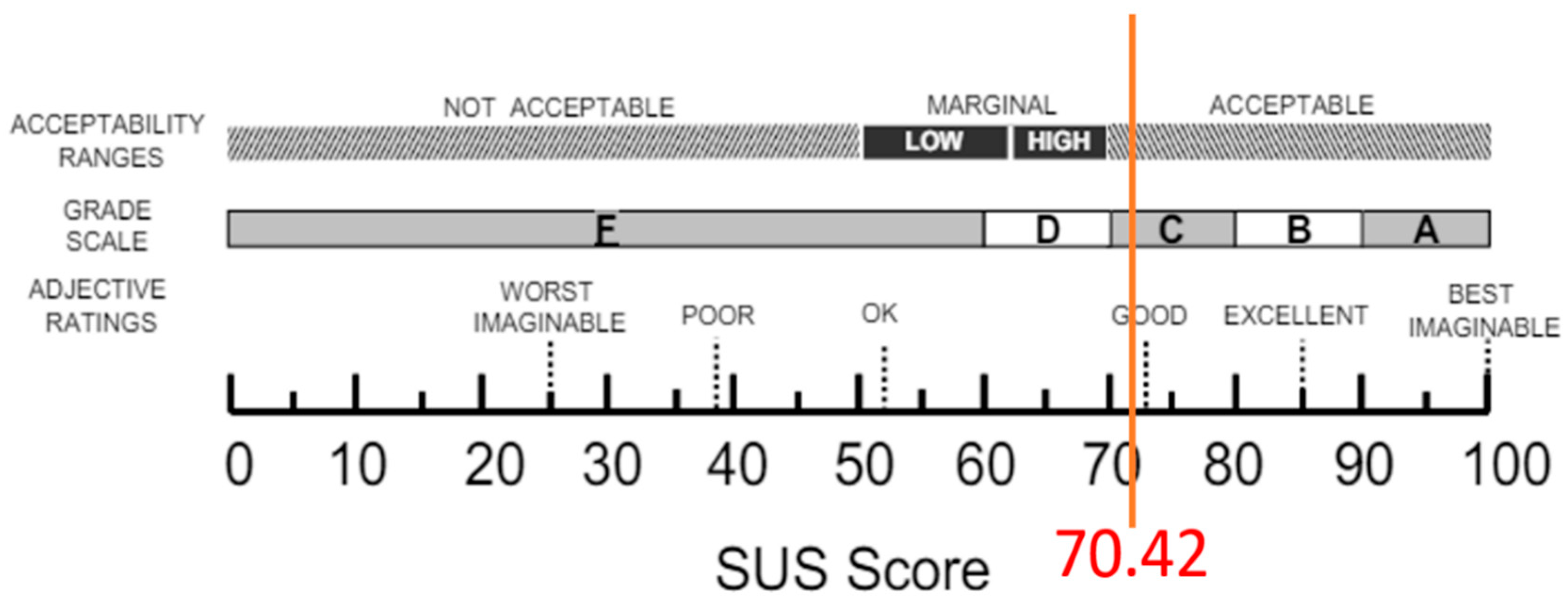
3.2. Usability Evaluation
- Usability: Assesses whether the design of the 3D visualization interface is intuitive, easy to navigate, and search;
- Convenience of Operation: Evaluates the ease with which users can view and interact with electronic medical records through the 3D models;
- Learnability: Measures the learning curve for first-time users, specifically how easy the system is to understand and use;
- Efficiency: Determines the speed of information retrieval, focusing on whether users can quickly locate the medical information they need within the 3D visualization system;
- Satisfaction: Gauges overall user satisfaction with the 3D human model EMR visualization system, including user experience and visual effects.
3.3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Demographic information The personal information will only be used for statistical analysis in this study and will not be used for any other purpose. Please feel free to answer the questions. | ||
| No | Content | Answer |
| 1 | Gender | □ Male □ Female |
| 2 | Ages | □ 20–29 □ 30–39 □ 40–49 □ 50–59 □ 60 and above |
| 3 | How many years have you been a doctor? | □ 1–10 years □ 10–20 years □ 20–30 years □ 30 years and above |
| No | Question | Strongly Disagree | Disagree | Not sure | Agree | Strongly Agree |
|---|---|---|---|---|---|---|
| 1 | I think that I would like to use this system frequently. | □ | □ | □ | □ | □ |
| 2 | I found the system unnecessarily complex. | □ | □ | □ | □ | □ |
| 3 | I thought the system was easy to use. | □ | □ | □ | □ | □ |
| 4 | I think that I would need the support of a technical person to be able to use this system. | □ | □ | □ | □ | □ |
| 5 | I found the various functions in this system were well integrated. | □ | □ | □ | □ | □ |
| 6 | I thought there was too much inconsistency in this system. | □ | □ | □ | □ | □ |
| 7 | I would imagine that most people would learn to use this system very quickly. | □ | □ | □ | □ | □ |
| 8 | I found the system very cumbersome to use. | □ | □ | □ | □ | □ |
| 9 | I felt very confident using the system. | □ | □ | □ | □ | □ |
| 10 | I needed to learn a lot of things before I could get going with this system. | □ | □ | □ | □ | □ |
References
- Holroyd-Leduc, J.M.; Lorenzetti, D.; Straus, S.E.; Sykes, L.; Quan, H. The impact of the electronic medical record on structure, process, and outcomes within primary care: A systematic review of the evidence. J. Am. Med. Inform. Assoc. 2011, 18, 732–737. [Google Scholar] [CrossRef]
- Rahal, R.M.; Mercer, J.; Kuziemsky, C.; Yaya, S. Factors affecting the mature use of electronic medical records by primary care physicians: A systematic review. BMC Med. Inform. Decis. Mak. 2021, 21, 67. [Google Scholar]
- Liu, R.; Gao, M.; Wang, L.; Wang, X.; Xiang, Y.; Zhang, A.; Xia, J.; Chen, Y.; Chen, S. Interactive extended reality techniques in information visualization. IEEE Trans. Hum.-Mach. Syst. 2022, 52, 1338–1351. [Google Scholar]
- Liu, Z.; Deng, L.; Wang, F.; Xiong, W.; Wu, T.; Demian, P.; Osmani, M. Building Information Modeling and Big Data in Sustainable Building Management: Research Developments and Thematic Trends via Data Visualization Analysis. Systems 2025, 13, 595. [Google Scholar] [CrossRef]
- West, V.L.; Borland, D.; Hammond, W.E. Innovative information visualization of electronic health record data: A systematic review. J. Am. Med. Inform. Assoc. 2015, 22, 330–339. [Google Scholar] [CrossRef]
- Ola, O.; Sedig, K. Beyond simple charts: Design of visualizations for big health data. Online J. Public Health Inform. 2016, 8, e195. [Google Scholar] [CrossRef] [PubMed]
- Żukowska, M.; Rad, M.A.; Górski, F. Additive manufacturing of 3D anatomical models—Review of processes, materials and applications. Materials 2023, 16, 880. [Google Scholar] [CrossRef] [PubMed]
- Abreu de Souza, M.; Alka Cordeiro, D.C.; Oliveira, J.D.; Oliveira, M.F.A.D.; Bonafini, B.L. 3D multi-modality medical imaging: Combining anatomical and infrared thermal images for 3D reconstruction. Sensors 2023, 23, 1610. [Google Scholar] [CrossRef] [PubMed]
- Bartoletti-Stella, A.; Gatta, V.; Mariani, G.A.; Gobbi, P.; Falconi, M.; Manzoli, L.; Faenza, I.; Salucci, S. Three-dimensional virtual anatomy as a new approach for medical student’s learning. Int. J. Environ. Res. Public Health 2021, 18, 13247. [Google Scholar]
- Sutherland, J.; Belec, J.; Sheikh, A.; Chepelev, L.; Althobaity, W.; Chow, B.J.; Mitsouras, D.; Christensen, A.; Rybicki, F.J.; La Russa, D.J. Applying modern virtual and augmented reality technologies to medical images and models. J. Digit. Imaging 2019, 32, 38–53. [Google Scholar] [CrossRef]
- Marro, A.; Bandukwala, T.; Mak, W. Three-dimensional printing and medical imaging: A review of the methods and applications. Curr. Probl. Diagn. Radiol. 2016, 45, 2–9. [Google Scholar] [CrossRef]
- Faisal, S.; Blandford, A.; Potts, H.W. Making sense of personal health information: Challenges for information visualization. Health Inform. J. 2013, 19, 198–217. [Google Scholar] [CrossRef]
- Ruan, W.; Appasani, N.; Kim, K.; Vincelli, J.; Kim, H.; Lee, W.S. Pictorial visualization of EMR summary interface and medical information extraction of clinical notes. In Proceedings of the 2018 IEEE International Conference on Computational Intelligence and Virtual Environments for Measurement Systems and Applications (CIVEMSA), Ottawa, ON, Canada, 12–13 June 2018; pp. 1–6. [Google Scholar]
- Angel, E.; Shreiner, D. Interactive Computer Graphics with WebGL; Addison-Wesley Professional: Boston, MA, USA, 2014. [Google Scholar]
- Bai, S.; Ma, C.; Wang, X.; Zhou, S.; Jiang, H.; Ma, L.; Jiang, H. Application of medical image 3D visualization web platform in auxiliary diagnosis and preoperative planning. J. Image Graph. 2023, 11, 32–39. [Google Scholar] [CrossRef]
- Jin, Y. Interactive Medical Record Visualization Based on Symptom Location in a 2D Human Body. Ph.D. Thesis, Université d’Ottawa/University of Ottawa, Ottawa, ON, Canada, 2016. [Google Scholar]
- Panayides, A.S.; Amini, A.; Filipovic, N.D.; Sharma, A.; Tsaftaris, S.A.; Young, A.; Foran, D.; Do, N.; Golemati, S.; Kurc, T.; et al. AI in medical imaging informatics: Current challenges and future directions. IEEE J. Biomed. Health Inform. 2020, 24, 1837–1857. [Google Scholar] [CrossRef]
- Zhang, Z.; Ahmed, F.; Mittal, A.; Ramakrishnan, I.V.; Zhao, R.; Viccellio, A.; Mueller, K. AnamneVis: A framework for the visualization of patient history and medical diagnostics chains. In IEEE Visual Analytics in Health Care (VAHC) Workshop; IEEE: Piscataway, NJ, USA, 2011. [Google Scholar]
- Florkow, M.C.; Willemsen, K.; Mascarenhas, V.V.; Oei, E.H.; van Stralen, M.; Seevinck, P.R. Magnetic resonance imaging versus computed tomography for Three-Dimensional bone imaging of musculoskeletal pathologies: A review. J. Magn. Reson. Imaging 2022, 56, 11–34. [Google Scholar] [CrossRef] [PubMed]
- Brenton, H.; Hernandez, J.; Bello, F.; Strutton, P.; Purkayastha, S.; Firth, T.; Darzi, A. Using multimedia and Web3D to enhance anatomy teaching. Comput. Educ. 2007, 49, 32–53. [Google Scholar] [CrossRef]
- Mamo, H.B.; Adamiak, M.; Kunwar, A. 3D printed biomedical devices and their applications: A review on state-of-the-art technologies, existing challenges, and future perspectives. J. Mech. Behav. Biomed. Mater. 2023, 143, 105930. [Google Scholar] [CrossRef] [PubMed]
- Bui, I.; Bhattacharya, A.; Wong, S.H.; Singh, H.R.; Agarwal, A. Role of three-dimensional visualization modalities in medical education. Front. Pediatr. 2021, 9, 760363. [Google Scholar] [CrossRef]
- Alper, B.; Hollerer, T.; Kuchera-Morin, J.; Forbes, A. Stereoscopic highlighting: 2d graph visualization on stereo displays. IEEE Trans. Vis. Comput. Graph. 2011, 17, 2325–2333. [Google Scholar] [CrossRef]
- Ganguli, A.; Pagan-Diaz, G.J.; Grant, L.; Cvetkovic, C.; Bramlet, M.; Vozenilek, J.; Kesavadas, T.; Bashir, R. 3D printing for preoperative planning and surgical training: A review. Biomed. Microdevices 2018, 20, 65. [Google Scholar] [CrossRef]
- Bozkurt, Y.; Karayel, E. 3D printing technology; methods, biomedical applications, future opportunities and trends. J. Mater. Res. Technol. 2021, 14, 1430–1450. [Google Scholar] [CrossRef]
- Meyer-Szary, J.; Luis, M.S.; Mikulski, S.; Patel, A.; Schulz, F.; Tretiakow, D.; Fercho, J.; Jaguszewska, K.; Frankiewicz, M.; Pawłowska, E.; et al. The role of 3D printing in planning complex medical procedures and training of medical professionals—Cross-sectional multispecialty review. Int. J. Environ. Res. Public Health 2022, 19, 3331. [Google Scholar] [CrossRef]
- Yeung, A.W.K.; Tosevska, A.; Klager, E.; Eibensteiner, F.; Laxar, D.; Stoyanov, J.; Glisic, M.; Zeiner, S.; Kulnik, S.T.; Crutzen, R.; et al. Virtual and augmented reality applications in medicine: Analysis of the scientific literature. J. Med. Internet Res. 2021, 23, e25499. [Google Scholar] [CrossRef]
- Bale, A.S.; Ghorpade, N.; Hashim, M.F.; Vaishnav, J.; Almaspoor, Z. A comprehensive study on metaverse and its impacts on humans. Adv. Hum.-Comput. Interact. 2022, 2022, 3247060. [Google Scholar] [CrossRef]
- Cravano, S.M.; Carmine, A.D.; De Maio, C.; Di Mitri, M.; Bisanti, C.; Collautti, E.; Libri, M.; D’Antonio, S.; Gargano, T.; Ciardini, E.; et al. Technical Skill Acquisition in Pediatric Minimally Invasive Surgery: Evaluation of a 3D-Printed Simulator for Thoracoscopic Esophageal Atresia Repair. Healthcare 2025, 13, 1720. [Google Scholar] [CrossRef]
- Qualter, J.; Sculli, F.; Oliker, A.; Napier, Z.; Lee, S.; Garcia, J.; Frenkel, S.; Harnik, V.; Triola, M. The biodigital human: A web-based 3D platform for medical visualization and education. Stud. Health Technol. Inform. 2012, 173, 359–361. [Google Scholar]
- Schwartzman, G.; Ramamurti, P. Visible body human anatomy atlas: Innovative anatomy learning. J. Digit. Imaging 2021, 34, 1328–1330. [Google Scholar] [CrossRef]
- Bobak, D.; Gabrisova, A.; Juricek, M.; Kulas, P.; Listvan, A.; Jelinek, A.; Kardosova, K.; Kvassay, M. Development of Online Anatomical Atlas for Biomedical Informatics. In Proceedings of the 2023 21st International Conference on Emerging eLearning Technologies and Applications (ICETA), Stary Smokovec, Slovakia, 26–27 October 2023; IEEE: Piscataway, NJ, USA, 2023; pp. 68–75. [Google Scholar]
- Stouthandel, M.E.; Van Beek, L.; Van de Velde, J.; Vangestel, C.; Van Hoof, T. A pilot study for the evaluation of 3D anatomy application ‘Complete Anatomy’as an additional non-mandatory study tool for the functional anatomy classes of first year physical therapy students. Anat. Sci. Educ. 2024, 17, 1336–1344. [Google Scholar] [CrossRef]
- Temkin, B.; Acosta, E.; Hatfield, P.; Onal, E.; Tong, A. Web-based three-dimensional virtual body structures: W3D-VBS. J. Am. Med. Inform. Assoc. 2002, 9, 425–436. [Google Scholar] [CrossRef]
- Sack, J.D. BioDigital: Powering the world’s understanding of the human body. Am. Biol. Teach. 2021, 83, 71. [Google Scholar] [CrossRef]
- Bangor, A.; Kortum, P.T.; Miller, J.T. An empirical evaluation of the system usability scale. Intl. J. Hum.-Comput. Interact. 2008, 24, 574–594. [Google Scholar] [CrossRef]
- Lewis, J.R. The system usability scale: Past, present, and future. Int. J. Hum.-Comput. Interact. 2018, 34, 577–590. [Google Scholar] [CrossRef]
- Fraenkel, J.R.; Wallen, N.E.; Hyun, H.H. How to Design and Evaluate Research in Education; Mac Graw Hill: New York, NY, USA, 2006. [Google Scholar]

| Function | The Proposed System | 2D Interactive Visual Electronic Medical Record System [16] | AnamneVis [18] |
|---|---|---|---|
| Human body model red dot | 3D with 360-degree rotation, zoom in, zoom out, and clickable | 2D with a clickable component | 2D with a clickable red dot |
| Physiological | system subdivided by department, mainly based on departments that are difficult to observe with the naked eye, such as cardiology, gastroenterology, and orthopedics | System subdivided into skeletal, muscular, cardiovascular, digestive, and neural parts. | single model without distinguishing physiological systems |
| Symptoms | Symptoms labeled in 3D model using ICD10 codes and corresponding English names | Symptoms color-coded in 2D model | Symptoms color-coded in 2D model |
| Historical patient records | Providing POMR and timeline | Providing timeline | Providing hierarchical ring, 5W1H, namely, Who, When, What, Where, Why, How |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, T.-J.; Lai, C.-Y.; Chiang, Y.-C. Visualization of Medical Record with 3D Human Body Models. Healthcare 2025, 13, 2393. https://doi.org/10.3390/healthcare13192393
Liu T-J, Lai C-Y, Chiang Y-C. Visualization of Medical Record with 3D Human Body Models. Healthcare. 2025; 13(19):2393. https://doi.org/10.3390/healthcare13192393
Chicago/Turabian StyleLiu, Tz-Jie, Chia-Yi Lai, and Yi-Cheng Chiang. 2025. "Visualization of Medical Record with 3D Human Body Models" Healthcare 13, no. 19: 2393. https://doi.org/10.3390/healthcare13192393
APA StyleLiu, T.-J., Lai, C.-Y., & Chiang, Y.-C. (2025). Visualization of Medical Record with 3D Human Body Models. Healthcare, 13(19), 2393. https://doi.org/10.3390/healthcare13192393






