Abstract
(1) Background: Advance directives (ADs) in Portugal have been legalized since 2012. What has been observed over time, from the few studies carried out, is that despite the positive attitudes in the population, there is a low level of adherence to ADs. To try to understand the reasons for these data, the current study aimed to explore and describe the experiences of the Portuguese population regarding AD. (2) Methods: For this exploratory and descriptive qualitative study, the researchers conducted open (unstructured) interviews with a convenience sample aged over 18 years until data saturation was achieved. (3) Results: A total of fifteen interviews were conducted—eight with women and seven with men. The following four categories emerged from the content analysis of the interviews: (1) AD literacy, (2) AD relevance, (3) AD attitudes, and (4) conditionalities for compiling the ADs. (4) Conclusions: The study pointed out the good receptivity of the participants to the ADs; however, literacy on this subject was low, and identifying the conditionalities in the development of ADs could contribute to improvements in implementation in the population. The data from this study suggest the need to implement measures to increase the literacy of the Portuguese population on ADs and review the legal framework for improving the accessibility of the citizen population. There is also a need to continue researching and obtain more evidence about the ways in which the Portuguese population perceives ADs; thus, in this way, a society can better respond to its citizens’ right to freely exercise their prospective autonomy at the end of their lives.
1. Introduction
The exercise of citizen autonomy in healthcare has been developing in recent years [1,2]. Currently, with the great developments in technology, there is an increasing number of therapeutic advances that have allowed us to increase the longevity and quality of life of the population. However, this framework of scientific and technological development is not without ethical problems, particularly in the field of end-of-life care [3,4,5,6,7]. Should all techniques and drugs be used to prolong human life under any circumstance? When should we withdraw or withhold a particular action to avoid medical futility and disrespect for the dignity of the human person? New challenges are posed to average citizens, who, on many occasions, must decide whether to consent or not to act in relation to healthcare. The current paradigm in the provision of healthcare requires respect for the autonomy of a person over the care provided to them, abandoning the paternalistic paradigm that prevailed for centuries [8,9]. In the 1960s, Luis Kutner, a lawyer from Chicago, initiated a new way to respect the autonomy of an individual in healthcare, not only in the present but also in the future [10,11]. Specifically, this refers to an advance directive (AD), a legal instrument that is commonly known as a living will. This instrument, which allows individuals to write their wishes to healthcare professionals, i.e., the care they wish to receive or refuse if they are unable to express their will autonomously in the future, has already been implemented by several countries, although with differing legal formats and characteristics [12,13,14]. Originally, ADs were simply a written document that presented the wishes of a person in terms of the healthcare that they did or did not want to receive, and later, they included greater reflection from the field of bioethics, and the figure of a healthcare power of attorney was also created, where a trusted person who knows the person’s values and desires and would be able to represent them. With evolution and bioethical consensus, it can be said that ADs take two formats: a living will and/or a healthcare power of attorney [15,16,17].
ADs in all legal frameworks in all countries are optional, i.e., a person is not required to prepare such a document. They can only be used to make an advance decision about end-of-life care, i.e., the individuals have the right to exercise prospective autonomy. On the other hand, some studies have revealed the advantages of this instrument in clinical practice, which include ensuring respect for the values and preferences of a patient, increasing the quality of life and comfort at the end of a patient’s life, and avoiding unnecessary medical procedures [18,19,20,21]. The relief of the burden to family members and caregivers in decision-making has also been noted [19,20,22]. Finally, there is an effect on the health professionals, where they are relieved of the anguish of ethical decision-making [23].
In Portugal, the possibility of citizens having this right enshrined had its genesis in the 21st century, more precisely, in 2001, with the Parliament’s ratification of the so-called Convention on Human Rights and Biomedicine of the Council of Europe [24]. This Convention, under Articles 5 and 9 (see below), allowed Portuguese citizens who were unable to communicate to have their previously expressed wishes (in writing or verbally to family members or caregivers) taken into account by healthcare professionals at the appropriate clinical time, as follows:
| Convention on Human Rights and Biomedicine of the Council of Europe |
| CHAPTER II |
| Consent |
| Article 5 |
| General rule |
| An intervention in the health field may only be carried out after the person concerned has given free and informed consent to it. |
| This person shall beforehand be given appropriate information as to the purpose and nature of the intervention as well as on its consequences and risks. |
| The person concerned may freely withdraw consent at any time. |
| (…) |
| Article 9 |
| Previously expressed wishes |
| The previously expressed wishes relating to a medical intervention by a patient who is not, at the time of the intervention, in a state to express his or her wishes shall be considered. |
This was the first step toward the legalization of ADs in the country, but the reflection and bioethical consensus on this matter were advanced in 2006 with the proposal to the Portuguese Parliament launched by the Portuguese Association of Bioethics for the legalization of ADs. It was only in 2012, after social discussion, that law 25/2012 [25], which established the AD as a tool for reinforcing self-determination of a person in healthcare, came into force.
However, more than a decade later, it was found that the Portuguese population’s knowledge and implementation rate of ADs was still very low [26,27,28].
Studies conducted in Portugal on ADs have focused mainly on health professionals [29,30,31,32]. However, few studies have addressed this approach among the general population [27,28,33,34]. The latter, as quantitative research, mainly sought to understand the attitudes and knowledge of the population on the subject. In addition to these data, it is essential to understand how the population perceives ADs. Research on the discourse of the population is essential for us to respond more clearly to the needs they present in this matter.
In view of the above limitations, it was relevant to understand the experiences of people regarding ADs. In this sense, this study was guided by the following research question: how do the Portuguese people deal with the reality of ADs? Therefore, in this study, we intended to explore and describe the experiences of the Portuguese population regarding ADs.
2. Materials and Methods
2.1. Study Design
This study fit into the qualitative research paradigm, as it was an exploratory, descriptive study that aimed to study the phenomenon in depth, highlighting the meaning that ADs have for individuals [35]. Based on the legal parameters established in Portuguese legislation [25] and the unquestionable respect for human autonomy in the bioethical field, we carried out this study [36].
Using open interviews with the participants, a content analysis was carried out according to Bardin [37], which sought to explore and describe the meaning of ADs for the study population. Furthermore, no software was used to manage the data. In addition, the study followed the guidelines of the Consolidated Criteria for Reporting Qualitative Research (CoreQ) [38].
2.2. Instruments, Participants, and Data Collection
It was decided to conduct open interviews to stimulate free thinking and, thus, explore in-depth the discourse of the participants [35].
The interviews followed a previously constructed script for this purpose and included sociodemographic data and the following question related to the subject of the study: would you like to talk to me openly about advance directives?
The study chose an accidental sample, selecting a street in a Portuguese city, going randomly to people’s homes, and inviting everyone over the age of 18 to take part in the study. The interview was pre-tested with a sample of four people. From the evaluation of the pre-test, it was evident that due to a lack of knowledge on the subject, people were unable to speak, which would allow us to carry out the survey. To overcome this problem, it was decided to perform a new pre-test with four other people; however, this time, the participants were given copies of the law 25/2012 [25] and the FAQs [39] so that within a few days, they could read the documentation and then schedule the interview. In this second test, it was verified that after reading the documents, people were able to talk about the subject.
Data collection took place from March to May 2023 by going door-to-door and asking the respondents about their interest in taking part in the research. If they showed interest, the documents mentioned above were handed over and an interview was scheduled for a date and time more convenient for the person and with enough time to read the documents. All the interviews were carried out face-to-face and at a location of their choice. An interview form was used with the socio-demographic data and a guiding question (Appendix A).
2.3. Formal and Ethical Procedures
The study was approved by the Ethics Committee of the Faculty of Medicine of the University of Porto (approval protocol n.° 59/CEFMUP/2022). All study procedures followed the recommendations of the Declaration of Helsinki and subsequent updates. Participant consent was obtained through a document in which they were informed in advance of the aims of the study, assured of the anonymity and confidentiality of any data they provided and had to agree to be interviewed by signing their voluntary participation form. They were also informed that they could withdraw from the study at any time without personal harm and that there was no financial or other reward for taking part in the study.
2.4. Data Analysis
The interviews were audio-recorded, immediately transcribed, and anonymized with an alphanumeric code (i.e., E1…E15). As these were open interviews, for clarification, the interviewers sometimes asked the participants to increase the depth of the discourse without inducing a response, which basically consisted of interventions such as “Tell me more about that…” or “What do you mean by that…”. For the qualitative analysis of the study, we used the theoretical framework of Bardin [37] and complied with the categorical typology. The data analysis followed three phases. First, the pre-analysis, which consisted of a phase of organizing the material to be analyzed to make it operational and to systematize ideas, corresponded to a period of intuitions that allowed us to guide a precise scheme for the development of the following phases. This was followed by the material exploration/coding phase, which consisted of the systematic transformation of the raw data and their aggregation into units that allowed the description of the characteristics relevant to the content of the text. This was a lengthy stage where the categories and their coding were defined, and the decisions made in the pre-analysis were carried out. Finally, the treatment phase of the results—inference and interpretation—consisted of processing the data to be significant and valid. The relationship between the data obtained and the theoretical foundation provided meaning to the interpretation performed. The treatment and analysis of the data favored an inductive approach, without the definition of a priori categories.
Two researchers (J.C.M. and E.M.) read and reread the interviews shortly after their transcription and independently categorized the discourses, ultimately reaching consensus on the categories and subcategories resulting from the analysis.
3. Results
In studies of this nature, the number of participants varies. Thus, the number of interviews ended when data saturation was reached through the data analysis [35,40]. In fact, a total of 15 people were interviewed (eight women and seven men). The youngest was 19 years old, and the oldest was 70 years old. Most of the respondents were married, Catholic, and had higher education. In professional terms, three were retired, two were students, and the remainder had different professional activities, three of which involved health professionals. Of the 15 interviewees, only two had prepared their ADs. The median interview length was 36 min (they ranged from 27 to 72 min). The detailed participant sociodemographic characteristics are provided in Table 1.

Table 1.
Participants’ sociodemographic characteristics (n = 15).
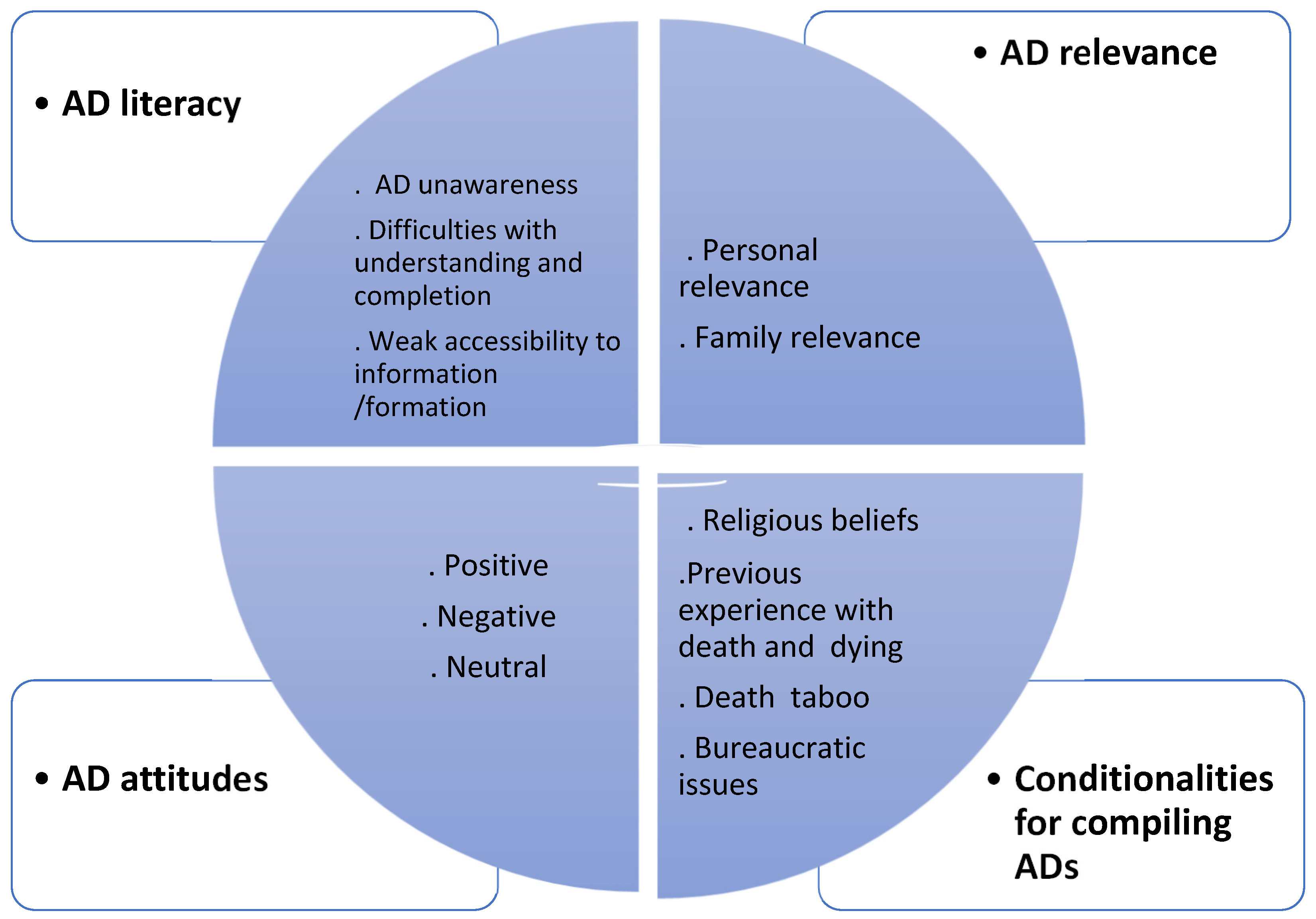
Four categories emerged from the content analysis of the interviews: AD literacy, AD relevance, AD attitudes, and conditionalities for compiling ADs. Additionally, 12 subcategories were extracted, as shown in Figure 1.
Figure 1.
General overview of the categories and subcategories identified from the interview analysis.
For the sake of clarity, Table 2 shows the categories, subcategories, and even some excerpts from the participant discourse.

Table 2.
Categories, subcategories, and context unit (verbatims).
3.1. AD Literacy
The category “AD literacy” emerged from the analysis of the interviews because in the speech, there was a lack of knowledge about a subject, difficulty understanding and completing an AD, and poor accessibility to information/training.
3.1.1. AD Unawareness
Indeed, most participants reported not having knowledge about the subject of ADs. It should be noted that, with the exception of the health professionals involved in the study, the remaining participants had never heard about the subject. This reconfirmed what the researchers found during the pre-test of the interview (see Section 2.2), where they had to send previous documentation to interviewees to be able to formulate some discourse on ADs.
3.1.2. Difficulties with Understanding and Completion
Another aspect that was of relevance was the recording of difficulties in understanding the documentation of a living will and the manifest difficulty in writing an AD. There were participants in the study who reported that the optional document for writing an AD was not understandable and the language was not accessible, and they were unable to write it without some help. There were references to the need to ask a health professional for help in order to develop an AD.
3.1.3. Weak Accessibility to Information/Formation
Another aspect that emerged from the speech was poor accessibility to information/training. In fact, only the health professionals had the opportunity to receive training on the subject. In addition to not having knowledge about the subject, as mentioned in Section 3.1.1 of the results, the remaining participants were also unable to identify access to information on ADs. There was one interviewee who referred to a memory during the initial phase of the process where there was some disclosure in the media and some debate in the community, and another interviewee remembered having seen a dissemination poster in a health unit.
3.2. AD Relevance
Another category that emerged from the discourse was AD relevance, and it took two forms: personal and family relevance.
3.2.1. Personal Relevance
A majority of the sample highly valued personal autonomy with regard to end-of-life care. The interviewees pointed to personal wills and the exercise of autonomy as fundamental elements of respect for a person. Thus, ADs assumed personal relevance because, in their words, they are fundamental instruments for respecting a person’s dignity at the end of their life.
3.2.2. Family Relevance
An awareness of the importance of having ADs for one’s family also emerged in the speech. The analyzed data allowed us to show that the interviewees did not want to be weights or burdens at the end of their lives, and they verbalized that having ADs would be elements that would not burden their families when they had to make decisions.
3.3. AD Attitudes
From the analysis of the interviews, a set of elements also emerged that allowed us to categorize attitudes toward ADs.
3.3.1. Positive
Most of the interviewees had positive attitudes, considered ADs important, and in some cases, intended to elaborate on ADs and considered it logical to have a law of this nature.
3.3.2. Negative
A negative attitude emerged in this sample, and it showed no advantages in implementing the ADs.
3.3.3. Neutral
Two attitudinal positions also emerged from the interviewees that were configured as neutral. Respondents considered that they ethically accepted the ADs but were indifferent (i.e., neither in favor of them nor against them).
3.4. Conditionalities for Compiling ADs
During the interviews, the researchers were also able to find important data relating to the constraints on the development of an AD.
3.4.1. Religious Beliefs
One of the constraints that was mentioned, in this case, as an impediment to developing an AD was religious belief. Participants of the sample, mostly Catholics, revealed that they believed in natural death without interference; therefore, drawing up a living will would interfere with this process. According to one participant, developing an AD did not seem to be in accordance with her religious beliefs or philosophy of life.
3.4.2. Previous Experience with Death and Dying
Another conditioning factor emerged for the elaboration of ADs, and it had to do with previous experience with death and dying. From the speech obtained, we were able to verify that the experience of monitoring or even caring for a family member at the end of their life is a motivator for developing an AD. The course of illness of the family member until death, especially for those with very disabling diseases, was a reason for reflection and constituted an impetus to think about the need to express wishes about end-of-life care.
3.4.3. Death Taboo
In the discourse of the interviewees, the taboo of death also emerged as an impediment to the elaboration of an AD. Indeed, some interviewees expressed their avoidance of talking about the subject and how uncomfortable it was for them. According to them, preparing for the end of life is something they do not think about; therefore, they will not seek to develop an AD.
3.4.4. Bureaucratic Issues
Another constraint also emerged which, according to the participants, was an obstacle to the elaboration of an AD, and it had more to do with the bureaucratic aspects of law enforcement. There was reference to the difficulties in understanding the technical language of the optional model that was placed online for citizens to fill out. Further, the renewal of an AD must be completed in-person after five years, and the participants questioned this period of validity for an AD and the need for renewal to require the person to go to the service with a new document. Participants considered the bureaucratic aspects to be constraints on the elaboration of ADs.
4. Discussion
To the best of our knowledge, this was the first study conducted in Portugal to explore and describe the experience of the Portuguese population with regard to ADs. The data found allowed us to develop a picture, although without generalizations, of how Portuguese citizens understood their right to exercise prospective autonomy in end-of-life care.
The results obtained in relation to literacy of the sample on the ADs, which revealed a lack of knowledge on the subject, were consistent with the findings of other studies [20,27,41,42,43,44,45,46,47,48,49]. A systematic review of the literature published from 1994 to 2016, revealed a low level of knowledge about ADs [19]. More recently, another review of literature published from 2018 to 2022 confirmed this fact [50]. As mentioned in the data collection section, it was only after reading the documents provided beforehand that some of the participants became aware of ADs. The Portuguese legislation on ADs dates back to 2012, and in 2017, the Portuguese parliament, realizing the low level of population adherence to ADs, asked the government to promote a publicity campaign [51]. Based on the data obtained thus far on the knowledge and level of adherence to ADs, it appears that the campaign did not have good results or that the dissemination strategies were not effective; therefore, there is still a need to promote the dissemination of ADs among the population [15,52,53].
In addition, only two participants in the sample had ADs, which was in agreement with the low level of adherence that existed at the national level. According to data from the Shared Services of the Ministry of Health, this rate was 0.51% of the population [26]. With the exception of the United States, where approximately one-third of the population has an AD [54,55], in European countries, the prevalence of ADs is lower, between 0.66% and 19% [41,43,56,57]. Another area identified in the context of literacy about ADs had to do with difficulties in understanding the AD documents and the wording of the ADs. These data likely explain the low adherence rates, constituting a barrier for citizens to exercise this right, as studies in other countries have shown [18,58,59]. Additionally, for this item, the participants mentioned the need for help in preparing ADs. Interestingly, this issue of citizens obtaining help with preparing their ADs has been expressed for some years in the United States through the Federal Patient Self-Determination Act of 1990, which forced health institutions to inform citizens of this right and provide counseling for its realization [60,61]. This aspect was particularly relevant, given the low level of literacy of the population in this area, due to both a lack of knowledge and an inability to understand what to write in an AD. It appeared that the need for counseling by health professionals, who are, in principle, more technically qualified, was a measure to be implemented to increase the ratio of ADs [53,62,63,64,65,66,67,68,69,70].
However, in this context, it turned out that there was scarce information and/or training on ADs in the population. It should be noted that within the sample, only health professionals had training on the subject. It appeared that accessibility to information/training was low, and furthermore, the Portuguese government’s publicizing of ADs to the Portuguese population at Parliament’s request [51], as mentioned in the introduction, did not have much effect. There was a need to increase access to training, especially for health professionals, to promote counseling, as mentioned above, and to increase access to community information in this digital age on social networks [71,72], support websites, or applications [73,74], as suggested by some studies.
Despite these aspects of literacy, the results of the study showed that attitudes toward ADs were mostly positive, which agreed with the findings of other studies [18,27,47,48,49,56,58,75,76,77]. However, there were also negative and even neutral attitudes. It is believed that this negative attitude may be associated with religious beliefs, that neutral positions were reported by younger participants, and that being confused about ADs demonstrated an uncommitted position.
Another interesting finding that emerged from the interviews was the relevance that the participants gave to the ADs. In addition to the positive attitudes, the participants attributed dual relevance to the ADs, as follows: they assumed the right to exercise their autonomy as fundamental in healthcare, and thus, in this way, ADs alleviated the burdens on their families for decision-making, given that these findings were in line with other empirical findings [19,23,54].
There is still much to be added to the findings of this study regarding the conditions for developing an AD. In this regard, religious beliefs likely play a role in hindering the development of ADs in the Portuguese context. Participants claimed that they did not want to interfere with the death process, and they felt that ADs interfered with this natural end-of-life process. Although these data need to be further investigated in terms of research, and bearing in mind that the majority of the sample was Catholic, it could be a notion of defense against natural death and the sacredness of life, which are ideas that are present in documents of the Catholic Church [78]. Curiously, in the United States, the Catholic Church informs and educates the faithful about ADs [79], but in Portugal, there has not been the same level of attention. This may determine this particularity and that it is still a subject that has not been reconciled with faith due to a lack of knowledge. Interestingly, some studies have shown that the more religious a population is, the less likely people are to think about the subject or develop an AD [80,81,82].
Previous experience and contact with death and dying were described as motivating individuals to develop ADs. Indeed, these data were in agreement with other studies that reaffirmed that experiencing the course of a disease in the death of a loved one can lead to introspection, identifying the values and care that one wants to receive or refuse at the end of their life, and thus, they seek to develop an AD [83,84].
In contrast to these results, it appeared to us that death was a barrier to the development of an AD, which was also what emerged in the discourse of some of the participants. Indeed, the disagreement in talking about death and even the denial of it could be assumed to be obstacles to discussing the planning of end-of-life care, as has been evidenced by some studies [76,77,85]. In this regard, there appears to be a need to introduce the themes of death and dying in the social discourse to demystify these subjects, reducing the fear, anxiety, and avoidance that are present when addressing end-of-life issues [86,87,88,89,90,91,92]. In recent years, the need for conversations about serious illness has been discussed and researched, and goals, values, fears, worries, desires, and hopes have been discussed on journeys through illnesses and the human experience of living with a serious illness has been explored, centered on people and their problems [93]. This could be a strategy for promoting end-of-life-care planning and ADs.
Despite the constraints in the elaboration of the ADs, some bureaucratic data have also emerged. The participants claimed that some items that are imposed by the AD law [25] may constitute obstacles in the implementation of ADs in a community and that they have to do with the need for renewal of an AD in-person and the five-year validity period. This aspect is relevant because the law is more than ten years old, and the data from this study point to the need to revisit the law and update it.
5. Limitations and Strengths
This qualitative study attempted to explore in-depth the experience of the Portuguese population regarding ADs; however, it had several limitations. First, it was not possible to make generalizations, and the convenience sample obtained may not have been able to encompass all the perceptions of the population regarding the subject under study. On the other hand, this sample had very specific characteristics, for example, more than half of the participants had higher education, which could also be a limiting element and not sufficiently comprehensive of the entire Portuguese population. Despite this, this study had its strengths in that it was the first study to be carried out with these characteristics in Portugal, providing a more concrete, albeit limited, understanding of how the Portuguese population deals with ADs.
Although the data obtained in this study cannot be generalized, the assumption of transferability is implicit in these studies, and it is understood as the possibility of observing the same result in other groups under similar social conditions, given the specificities of the new context [94]. Thus, it is necessary to continue investigating other samples and other types of investigations via focus groups to obtain additional evidence.
6. Conclusions
This study shed some light on the way Portuguese people deal with ADs. The data obtained indicated low levels of literacy, positive attitudes, and the special relevance of ADs for the Portuguese population. On the other hand, we identified some constraints that may facilitate or hinder the development of ADs in society.
As a result of this study, we developed the following implications for education: improving training programs for the general population and for health professionals, and it is also important that the curricula of students in health areas can, from the early stages, begin their training on end-of-life-care planning. On the other hand, there are also implications for the policy area because there is a need to change and improve the AD law. Finally, there is also a need to continue researching this topic to obtain additional data and to respond to society’s need more effectively for end-of-life-care planning. In this way, citizens can be given the chance to freely exercise their prospective autonomy.
Author Contributions
Conceptualization, J.C.M. and R.N.; methodology, J.C.M., E.M. and R.N.; validation, E.M. and R.N.; formal analysis, J.C.M. and E.M.; investigation, J.C.M.; resources, J.C.M.; data curation, J.C.M. and E.M.; writing—original draft preparation, J.C.M.; writing—review and editing, J.C.M., E.M. and R.N.; visualization, J.C.M., E.M. and R.N.; supervision, E.M. and R.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Faculty of Medicine of the University of Porto (approval protocol no. 59/CEFMUP/2022 of 29 July).
Informed Consent Statement
The subjects participated voluntarily and anonymously in the study. Informed consent was obtained from all participants involved in the study. They were required to provide consent before being interviewed. The participants received no compensation.
Data Availability Statement
All data generated or analyzed during this study are included in this article.
Acknowledgments
The authors would like to express their sincere thanks to all the participants who took part in the research.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A. Interview Sheet
- Code:___________ Duration:________________________Date: ___/____/_____
- Sociodemographic data
| Variable | |
| Age | 18–28 years old |
| 29–39 years old | |
| 40–50 years old | |
| 51–61 years old | |
| ≥62 years old | |
| Gender | Female |
| Male | |
| Other | |
| Marital status | Single |
| Married/living together | |
| Divorced/separated | |
| Widowed | |
| Religion | Catholic |
| Protestant | |
| Agnostic/atheist | |
| Level of education | Elementary education |
| Secondary education | |
| Bachelor’s degree | |
| Master’s degree | |
| Doctorate | |
| Occupation | |
| Have you got a living will? | Yes |
| No |
- Explanatory question:
- Thank you for agreeing to take part in this research.
- Would you like to talk to me openly about advance directives?
References
- Manda-Taylor, L.; Masiye, F.; Mfutso-Bengo, J. Autonomy. In Encyclopedia of Global Bioethics; ten Have, H., Ed.; Springer International Publishing: Cham, Switzerland, 2016; pp. 218–225. [Google Scholar] [CrossRef]
- Kühler, M.; Mitrović, V.L. (Eds.) Theories of the Self and Autonomy in Medical Ethics; The International Library of Bioethics; Springer International Publishing: Cham, Switzerland, 2020; Volume 83. [Google Scholar] [CrossRef]
- Martins-Branco, D.; Lopes, S.; Canario, R.; Freire, J.; Feio, M.; Ferraz-Goncalves, J.; Sousa, G.; Lunet, N.; Gomes, B. Factors Associated with the Aggressiveness of Care at the End of Life for Patients with Cancer Dying in Hospital: A Nationwide Retrospective Cohort Study in Mainland Portugal. ESMO Open 2020, 5, e000953. [Google Scholar] [CrossRef] [PubMed]
- Macedo, J.C. Bioethics Reflection on Life Prolongation in End-of-Life Care. Int. J. Clin. Stud. Med. Case Rep. 2022, 17, e1–e4. [Google Scholar] [CrossRef]
- Huynh, T.N.; Kleerup, E.C.; Wiley, J.F.; Savitsky, T.D.; Guse, D.; Garber, B.J.; Wenger, N.S. The Frequency and Cost of Treatment Perceived to Be Futile in Critical Care. JAMA Intern. Med. 2013, 173, 1887–1894. [Google Scholar] [CrossRef] [PubMed]
- Cheung, M.C.; Earle, C.C.; Rangrej, J.; Ho, T.H.; Liu, N.; Barbera, L.; Saskin, R.; Porter, J.; Seung, S.J.; Mittmann, N. Impact of Aggressive Management and Palliative Care on Cancer Costs in the Final Month of Life. Cancer 2015, 121, 3307–3315. [Google Scholar] [CrossRef] [PubMed]
- Togashi, S.; Masukawa, K.; Aoyama, M.; Sato, K.; Miyashita, M. Aggressive End-of-Life Treatments Among Inpatients with Cancer and Non-Cancer Diseases Using a Japanese National Claims Database. Am. J. Hosp. Palliat. Med. 2023, 10499091231216888. [Google Scholar] [CrossRef]
- Nunes, R. Bioética; Conselho Federal de Medicina/Faculdade de Medicina da Universidade do Porto: Brasília, Brazil, 2022. [Google Scholar]
- Simon, A. Ethical Issues Concerning Patient Autonomy in Clinical Practice. In Theories of the Self and Autonomy in Medical Ethics; Kühler, M., Mitrović, V.L., Eds.; Springer International Publishing: Cham, Switzerland, 2020; Volume 83, pp. 123–135. [Google Scholar] [CrossRef]
- Benzenhöfer, U.; Hack-Molitor, G. Luis Kutner and the Development of the Advance Directive (Living Will); Benzeenhöfer, O., Ed.; GWAB-Verlag: Wetzlar, Germany, 2009. [Google Scholar]
- Kutner, L. Due Process of Euthanasia: The Living Will, A Proposal. Indiana Law J. 1969, 44, 539–554. [Google Scholar]
- Veshi, D.; Neitzke, G. Advance Directives in Some Western European Countries: A Legal and Ethical Comparison. Eur. J. Health Law 2015, 22, 321–345. [Google Scholar] [CrossRef]
- Porcar Rodado, E.; Peral Sanchez, D.; Gisbert Grifo, M. Advance Directives. Comparison of Current Legislation within the European Union. Rev. Esp. Med. Leg. 2021, 47, 66–73. [Google Scholar] [CrossRef]
- Lack, P.; Biller-Andorno, N.; Brauer, S. (Eds.) Advance Directives; International Library of Ethics, Law, and the New Medicine; Springer: Dordrecht, The Netherlands, 2014. [Google Scholar] [CrossRef]
- Nunes, R. Directivas Anticipadas de Voluntad; Consejo Federal de Medicina: Brasília, Brazil, 2020. [Google Scholar]
- Andorno, R.; Biller-Andorno, N.; Brauer, S.; Biller-Andorno, N. Advance Health Care Directives: Towards a Coordinated European Policy? Eur. J. Health Law 2009, 16, 207–227. [Google Scholar] [CrossRef]
- Ten Have, H.; do Céu Patrão Neves, M. Advance Directives. In Dictionary of Global Bioethics; Springer International Publishing: Cham, Switzerland, 2021; p. 97. [Google Scholar] [CrossRef]
- Bar-Sela, G.; Bagon, S.; Mitnik, I.; Adi, S.; Baziliansky, S.; Bar-Sella, A.; Vornicova, O.; Tzuk-Shina, T. The Perception and Attitudes of Israeli Cancer Patients Regarding Advance Care Planning. J. Geriatr. Oncol. 2021, 12, 1181–1185. [Google Scholar] [CrossRef]
- Kermel-Schiffman, I.; Werner, P. Knowledge Regarding Advance Care Planning: A Systematic Review. Arch. Gerontol. Geriatr. 2017, 73, 133–142. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, Y.; Hong, Y.; Zeng, P.; Hu, Z.; Xu, X.; Wang, H. Advance Directives and End-of-Life Care: Knowledge and Preferences of Patients with Brain Tumours from Anhui, China. BMC Cancer 2021, 21, 25. [Google Scholar] [CrossRef] [PubMed]
- Dalmau-Bueno, A.; Saura-Lazaro, A.; Busquets, J.M.; Bullich-Marín, I.; García-Altés, A. Advance Directives and Real-World End-of-Life Clinical Practice: A Case-Control Study. BMJ Support. Palliat. Care 2021, 12, E337–E344. [Google Scholar] [CrossRef]
- Carbonneau, M.; Davyduke, T.; Spiers, J.; Brisebois, A.; Ismond, K.; Tandon, P. Patient Views on Advance Care Planning in Cirrhosis: A Qualitative Analysis. Can. J. Gastroenterol. Hepatol. 2018, 2018, 4040518. [Google Scholar] [CrossRef]
- Hemsley, B.; Meredith, J.; Bryant, L.; Wilson, N.J.; Higgins, I.; Georgiou, A.; Hill, S.; Balandin, S.; McCarthy, S. An Integrative Review of Stakeholder Views on Advance Care Directives (ACD): Barriers and Facilitators to Initiation, Documentation, Storage, and Implementation. Patient Educ. Couns. 2019, 102, 1067–1079. [Google Scholar] [CrossRef] [PubMed]
- Council of Europe. Convention for the Protection of Human Rights and Dignity of the Human Being with Regard to the Application of Biology and Medicine: Convention on Human Rights and Biomedicine; Republic Daily n.o 2/2001, Série I-A de 2001-01-03; Council of Europe: Strasbourg, France, 2001. [Google Scholar]
- Republic Assembly. Law 25/2012; Diário da República n.° 136/2012, Série I de 2012-07-16; Republic Assembly: Ljubljana, Slovenia, 2012; pp. 3728–3730. [Google Scholar]
- Serviços Partilhados do Ministério da Saúde. RENTEV—Registo Nacional do Testamento Vital. Available online: https://www.spms.min-saude.pt/2023/01/registo-de-testamentos-vitais-duplicou-em-2022/ (accessed on 17 March 2023).
- Laranjeira, C.; dos Anjos Dixe, M.; Gueifão, L.; Caetano, L.; Passadouro, R.; Querido, A. Awareness and Attitudes towards Advance Care Directives (ACDs): An Online Survey of Portuguese Adults. Healthcare 2021, 9, 648. [Google Scholar] [CrossRef] [PubMed]
- Capelas, M.L.V.; Coelho, S.P.F.; Silva, S.C.F.; Ferreira, C.M.D.; Pereira, C.M.F.; Alvarenga, M.I.S.F.; Freitas, M.S. Os Portugueses e o Testamento Vital. Cad. Saúde 2017, 9, 44–53. [Google Scholar] [CrossRef]
- Santos, L.; Cerqueira, M. Health Professionals’ Experiences in Complying with the Advance Directive of Will in Clinical Practice. Rev. Enferm. Ref. 2022, 6, e21153. [Google Scholar] [CrossRef]
- Barreto, A.L.F.; Capela, M.L.V. Conhecimento dos Profissionais de Saúde Sobre as Diretivas Antecipadas de Vontade. Cad. Saúde 2020, 12, 36–40. [Google Scholar] [CrossRef]
- Meireles, E.; Gonçalves, C.; Correia, C.; Carvalho, D.; Neves, S.; Macedo, E.; Macedo, J.C. Conhecimento dos Enfermeiros Sobre as Diretivas Antecipadas de Vontade. In Proceedings of the VI Congresso Ordem dos Enfermeiros, Braga, Portugal, 5–7 May 2022. [Google Scholar] [CrossRef]
- Pereira, S.M.; Fradique, E.; Fialho, R.; Cerqueira, M.; Pereira, A.; Sampaio, F. Advance Directives: Portuguese Palliative Care Professionals’ Views. Int. J. Palliat. Nurs. 2011, 17, 373–380. [Google Scholar] [CrossRef]
- Martins, C.S.; Nunes, R. Advanced Directives’ Knowledge among Portuguese Palliative Patients and Caregivers: Do the Sociodemographic Factors Influence It? A Cross-Sectional Survey. BMC Palliat. Care 2023, 22, 84. [Google Scholar] [CrossRef]
- Martins, C.S.; Sousa, I.; Barros, C.; Pires, A.; Castro, L.; da Costa Santos, C.; Nunes, R. Do Surrogates Predict Patient Preferences More Accurately after a Physician-Led Discussion about Advance Directives? A Randomized Controlled Trial. BMC Palliat. Care 2022, 21, 122. [Google Scholar] [CrossRef]
- Fortin, M.-F.; Gagnon, J. Fondements et Étapes du Processus de Recherche: Méthodes Quentitatives et Qualitatives; CHENELIERE MCGRAW-HILL: Montreal, QC, Canada, 2016. [Google Scholar]
- Beauchamp, T.L.; Childress, J.F. Principles of Biomedical Ethics, 8th ed.; Oxford University Press: Oxford, UK, 2019. [Google Scholar]
- Bardin, L. L’Analyse de Contenu; PUF: Paris, France, 2007. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Serviços Partilhados do Ministério da Saúde. Perguntas Frequentes FAQ´S—RENTEV Testamento Vital. Available online: https://www.spms.min-saude.pt/wp-content/uploads/2014/06/RENTEV_FAQ_20140519_v1.pdf (accessed on 17 November 2023).
- Ando, H.; Cousins, R.; Young, C. Achieving Saturation in Thematic Analysis: Development and Refinement of a Codebook. Compr. Psychol. 2014, 3, 03.CP.3.4. [Google Scholar] [CrossRef]
- Rurup, M.L.; Onwuteaka-Philipsen, B.D.; Van Der Heide, A.; Van Der Wal, G.; Deeg, D.J.H. Frequency and Determinants of Advance Directives Concerning End-of-Life Care in the Netherlands. Soc. Sci. Med. 2006, 62, 1552–1563. [Google Scholar] [CrossRef] [PubMed]
- Van Wijmen, M.P.S.; Rurup, M.L.; Pasman, H.R.W.; Kaspers, P.J.; Onwuteaka-Philipsen, B.D. Advance Directives in the Netherlands: An Empirical Contribution to the Exploration of a Cross-Cultural Perspective on Advance Directives. Bioethics 2010, 24, 118–126. [Google Scholar] [CrossRef] [PubMed]
- De Vleminck, A.; Pardon, K.; Houttekier, D.; Van Den Block, L.; Vander Stichele, R.; Deliens, L. The Prevalence in the General Population of Advance Directives on Euthanasia and Discussion of End-of-Life Wishes: A Nationwide Survey Ethics, Organization and Policy. BMC Palliat. Care 2015, 14, 71. [Google Scholar] [CrossRef] [PubMed]
- White, B.; Tilse, C.; Wilson, J.; Rosenman, L.; Strub, T.; Feeney, R.; Silvester, W. Prevalence and Predictors of Advance Directives in Australia. Intern. Med. J. 2014, 44, 975–980. [Google Scholar] [CrossRef] [PubMed]
- Chung, R.Y.-N.; Wong, E.L.-Y.; Kiang, N.; Chau, P.Y.-K.; Lau, J.Y.C.; Wong, S.Y.-S.; Yeoh, E.-K.; Woo, J.W. Knowledge, Attitudes, and Preferences of Advance Decisions, End-of-Life Care, and Place of Care and Death in Hong Kong. A Population-Based Telephone Survey of 1067 Adults. J. Am. Med. Dir. Assoc. 2017, 18, 367.e19–367.e27. [Google Scholar] [CrossRef]
- Ng, R.; Lip Hoe, K.; Lim, J.; Weifen, L. Advance Care Planning in Singapore: The Genesis and Evolution of a National Programme. Z. Evid. Fortbild. Qual. Gesundhwes 2023, 180, 99–102. [Google Scholar] [CrossRef]
- Lim, M.K.; Lai, P.S.M.; Lim, P.S.; Wong, P.S.; Othman, S.; Mydin, F.H.M. Knowledge, Attitude and Practice of Community-Dwelling Adults Regarding Advance Care Planning in Malaysia: A Cross-Sectional Study. BMJ Open 2022, 12, e048314. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Heo, S.; Woo Hong, S.; Shim, J.; Lee, J.-A. Correlates of Advance Directive Treatment Preferences among Community-Dwelling Older People with Chronic Diseases. Int. J. Older People Nurs. 2019, 14, e12229. [Google Scholar] [CrossRef]
- Hou, X.T.; Lu, Y.H.; Yang, H.; Guo, R.X.; Wang, Y.; Wen, L.H.; Zhang, Y.R.; Sun, H.Y. The Knowledge and Attitude towards Advance Care Planning among Chinese Patients with Advanced Cancer. J. Cancer Educ. 2021, 36, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Macedo, J.C.; Rego, F.; Nunes, R. Perceptions, Attitudes, and Knowledge toward Advance Directives: A Scoping Review. Healthcare 2023, 11, 2755. [Google Scholar] [CrossRef] [PubMed]
- Republic Assembly. Resolution of the Republic Assembly n.°1/2017; Diário da República n.° 1/2017, Série I de 2017-01-02; Republic Assembly: Ljubljana, Slovenia, 2017; p. 2. Available online: https://diariodarepublica.pt/dr/detalhe/resolucao-assembleia-republica/1-2017-105669745 (accessed on 24 August 2023).
- Altisent, R. Editorial- Planificación Anticipada de La Asistencia. Se Necesita Una Revolución Educativa. Aten. Primaria 2013, 45, 402–403. [Google Scholar] [CrossRef] [PubMed]
- Macedo, J.C. Contribution to Improve Advance Directives in Portugal. MOJ Gerontol. Geriatr. 2020, 5, 27–30. [Google Scholar] [CrossRef]
- Silveira, M.J.; Wiitala, W.; Piette, J. Advance Directive Completion by Elderly Americans: A Decade of Change. J. Am. Geriatr. Soc. 2014, 62, 706–710. [Google Scholar] [CrossRef]
- Yadav, K.N.; Gabler, N.B.; Cooney, E.; Kent, S.; Kim, J.; Herbst, N.; Mante, A.; Halpern, S.D.; Courtright, K.R. Approximately One in Three Us Adults Completes Any Type of Advance Directive for End-of-Life Care. Health Aff. 2017, 36, 1244–1251. [Google Scholar] [CrossRef]
- Kleiner, A.C.; Santos-Eggimann, B.; Fustinoni, S.; Dürst, A.V.; Haunreiter, K.; Rubli-Truchard, E.; Seematter-Bagnoud, L. Advance Care Planning Dispositions: The Relationship between Knowledge and Perception. BMC Geriatr. 2019, 19, 118. [Google Scholar] [CrossRef]
- Herreros, B.; Gella, P.; Valenti, E.; Márquez, O.; Moreno, B.; Velasco, T. Improving the Implementation of Advance Directives in Spain. Camb. Q. Healthc. Ethics 2023, 32, 270–275. [Google Scholar] [CrossRef]
- Schnur, K.; Radhakrishnan, K. Young Adult Knowledge and Readiness to Engage in Advance Care Planning Behaviors. J. Hosp. Palliat. Nurs. 2019, 21, 54–60. [Google Scholar] [CrossRef]
- Herreros, B.; Benito, M.; Gella, P.; Valenti, E.; Sánchez, B.; Velasco, T. Why Have Advance Directives Failed in Spain? BMC Med. Ethics 2020, 21, 113. [Google Scholar] [CrossRef]
- Hunsaker, A.E.; Mann, A. An Analysis of the Patient Self-Determination Act of 1990. J. Hum. Behav. Soc. Environ. 2013, 23, 841–848. [Google Scholar] [CrossRef]
- Inoue, M.; Tompkins, C.; Scruggs, K.; Robles, J. Advance Directives Information Delivery in Medicare/Medicaid-Funded Agencies: An Exploratory Study. J. Soc. Work. End. Life Palliat. Care 2018, 14, 177–193. [Google Scholar] [CrossRef] [PubMed]
- Hinderer, K.A.; Lee, M.C. Chinese Americans’ Attitudes toward Advance Directives: An Assessment of Outcomes Based on a Nursing-Led Intervention. Appl. Nurs. Res. 2019, 49, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Hinderer, K.A.; Lee, M.C. Assessing a Nurse-Led Advance Directive and Advance Care Planning Seminar. Appl. Nurs. Res. 2014, 27, 84–86. [Google Scholar] [CrossRef] [PubMed]
- Baker, E.F.; Marco, C.A. Advance Directives in the Emergency Department. J. Am. Coll. Emerg. Physicians Open 2020, 1, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Izumi, S. Advance Care Planning: The Nurse’s Role. Am. J. Nurs. 2017, 117, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Lum, H.D.; Sudore, R.L.; Bekelman, D.B. Advance Care Planning in the Elderly. Med. Clin. N. Am. 2015, 99, 391–403. [Google Scholar] [CrossRef]
- Porensky, E.K.; Carpenter, B.D. Knowledge and Perceptions in Advance Care Planning. J. Aging Health 2008, 20, 89–106. [Google Scholar] [CrossRef]
- Scholten, G.; Bourguignon, S.; Delanote, A.; Vermeulen, B.; Van Boxem, G.; Schoenmakers, B. Advance Directive: Does the GP Know and Address What the Patient Wants? Advance Directive in Primary Care. BMC Med. Ethics 2018, 19, 58. [Google Scholar] [CrossRef]
- Nauck, F.; Becker, M.; King, C.; Radbruch, L.; Voltz, R.; Jaspers, B. To What Extent Are the Wishes of a Signatory Reflected in Their Advance Directive: A Qualitative Analysis. BMC Med. Ethics 2014, 15, 52. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, J.; Waller, A.; Sanson-Fisher, R.; Clark, K.; Ball, J. Knowledge of, and Participation in, Advance Care Planning: A Cross-Sectional Study of Acute and Critical Care Nurses’ Perceptions. Int. J. Nurs. Stud. 2018, 86, 74–81. [Google Scholar] [CrossRef]
- Pei, Y.; Qi, X.; Zhu, Z.; Zhang, W.; Tsay, R.-M.; Wu, B. The Informal Discussion of Advance Care Planning among Chinese Older Adults: Do Education and Social Media Use Matter? Geriatr. Nurs. 2024, 55, 1–5. [Google Scholar] [CrossRef]
- Ortiz, A.C.; Rolnick, J.A. Cutting through the Noise: How Social Media Can Provide Insight into Advance Care Planning in the COVID-19 Pandemic. Chest 2022, 162, 35–36. [Google Scholar] [CrossRef] [PubMed]
- Biller, A.; Biller-Andorno, N. From Text to Interaction: The Digital Advance Directive Method for Advance Directives. Digit. Health 2023, 9, 20552076221147414. [Google Scholar] [CrossRef] [PubMed]
- Sudore, R.L.; Boscardin, J.; Feuz, M.A.; McMahan, R.D.; Katen, M.T.; Barnes, D.E. Effect of the Preparewebsite vs an Easy-to-Read Advance Directive on Advance Care Planning Documentation and Engagement among Veterans a Randomized Clinical Trial. JAMA Intern. Med. 2017, 177, 1102–1109. [Google Scholar] [CrossRef]
- Ugalde, A.; O’Callaghan, C.; Byard, C.; Brean, S.; MacKay, J.; Boltong, A.; Davoren, S.; Lawson, D.; Parente, P.; Michael, N.; et al. Does Implementation Matter If Comprehension Is Lacking? A Qualitative Investigation into Perceptions of Advance Care Planning in People with Cancer. Support. Care Cancer 2018, 26, 3765–3771. [Google Scholar] [CrossRef]
- Dhingra, L.; Cheung, W.; Breuer, B.; Huang, P.; Lam, K.; Chen, J.; Zhou, X.; Chang, V.; Chui, T.; Hicks, S.; et al. Attitudes and Beliefs toward Advance Care Planning among Underserved Chinese-American Immigrants. J. Pain Symptom Manag. 2020, 60, 588–594. [Google Scholar] [CrossRef]
- Yap, S.S.; Chen, K.; Detering, K.M.; Fraser, S.A. Exploring the Knowledge, Attitudes and Needs of Advance Care Planning in Older Chinese Australians. J. Clin. Nurs. 2018, 27, 3298–3306. [Google Scholar] [CrossRef]
- Congregation for the Doctrine of the Faith. Samaritanus Bonus on the Care of Persons in the Critical and Terminal Phases of Life; Congregation for the Doctrine of the Faith: Rome, Italy, 2020. [Google Scholar]
- Florida Conference of Catholic Bishops. End-of-Life Planning: A Catholic Introduction. Available online: https://flaccb.org/end-of-life-care (accessed on 8 December 2023).
- Johnson, S.; Butow, P.; Kerridge, I.; Tattersall, M. Advance Care Planning for Cancer Patients: A Systematic Review of Perceptions and Experiences of Patients, Families, and Healthcare Providers. Psychooncology 2016, 25, 362–386. [Google Scholar] [CrossRef]
- McDermott, E.; Selman, L.E. Cultural Factors Influencing Advance Care Planning in Progressive, Incurable Disease: A Systematic Review with Narrative Synthesis. J. Pain Symptom Manag. 2018, 56, 613–636. [Google Scholar] [CrossRef]
- True, G.; Phipps, E.J.; Braitman, L.E.; Harralson, T.; Harris, D.; Tester, W. Treatment Preferences and Advance Care Planning at End of Life: The Role of Ethnicity and Spiritual Coping in Cancer Patients. Ann. Behav. Med. 2005, 30, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Clem, S.; Rose, R.; Cagle, J.G. Exposure to a Loved One’s Death and Advance Care Planning: Moderating Effects of Age. Am. J. Hosp. Palliat. Med. 2023, 10499091231188689. [Google Scholar] [CrossRef] [PubMed]
- Carr, D. “I Don’t Want to Die like That …”: The Impact of Significant Others’ Death Quality on Advance Care Planning. Gerontologist 2012, 52, 770–781. [Google Scholar] [CrossRef] [PubMed]
- Graham-Wisener, L.; Nelson, A.; Byrne, A.; Islam, I.; Harrison, C.; Geddis, J.; Berry, E. Understanding Public Attitudes to Death Talk and Advance Care Planning in Northern Ireland Using Health Behaviour Change Theory: A Qualitative Study. BMC Public Health 2022, 22, 906. [Google Scholar] [CrossRef]
- Corradi, M.L.G.; Duim, E.; Rodrigues, C.I.S. Death and End of Life: Perceptions throughout the Career about Death, Palliative Care, and Educational Process. J. Palliat. Care 2021, 36, 243–247. [Google Scholar] [CrossRef]
- de la Herrán Gascón, A.; Herrero, P.R.; Peralta, I.R.; Rodríguez, J.J.M. The Pedagogy of Death and Special Needs Education. A Phenomenological Study. Eur. J. Spec. Needs Educ. 2022, 37, 747–760. [Google Scholar] [CrossRef]
- Macedo, J.C.G.M. An Approach to Death Education. MOJ Gerontol. Geriatr. 2019, 4. [Google Scholar] [CrossRef]
- Dadfar, M.; Lester, D. The Effectiveness of 8A Model Death Education on the Reduction of Death Depression: A Preliminary Study. Nurs. Open 2020, 7, 294–298. [Google Scholar] [CrossRef]
- McAfee, C.A.; Jordan, T.R.; Cegelka, D.; Polavarapu, M.; Wotring, A.; Wagner-Greene, V.R.; Hamdan, Z. COVID-19 Brings a New Urgency for Advance Care Planning: Implications of Death Education. Death Stud. 2022, 46, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Testoni, I.; Palazzo, L.; Calamarà, N.; Rossi, G.; Wieser, M.A. “Imagine You Have ALS”: Death Education to Prepare for Advance Treatment Directives. Behav. Sci. 2021, 11, 6. [Google Scholar] [CrossRef] [PubMed]
- OECD. Time for Better Care at the End of Life; OECD Health Policy Studies; OECD: Paris, France, 2023. [Google Scholar] [CrossRef]
- Baxter, R.; Pusa, S.; Andersson, S.; Fromme, E.K.; Paladino, J.; Sandgren, A. Core Elements of Serious Illness Conversations: An Integrative Systematic Review. BMJ Support. Palliat. Care 2023, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Martins, M.I.S.; Oliveira, F.A.; Alcântara, D.G.; Dias, P.R.G.; Vieira, E.P.; Sousa, F.S.; De Almeida, A.N.S.; Da Silva, J.P.F. Generalização e Transferibilidade: As Possibilidades da Pesquisa Qualitativa. REVISTA FOCO 2023, 16, e1157. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).