Are Malnourished Inpatients Treated by Dietitians Active Participants in Their Nutrition Care? Findings of an Exploratory Study of Patient-Reported Measures across Nine Australian Hospitals
Abstract
1. Introduction
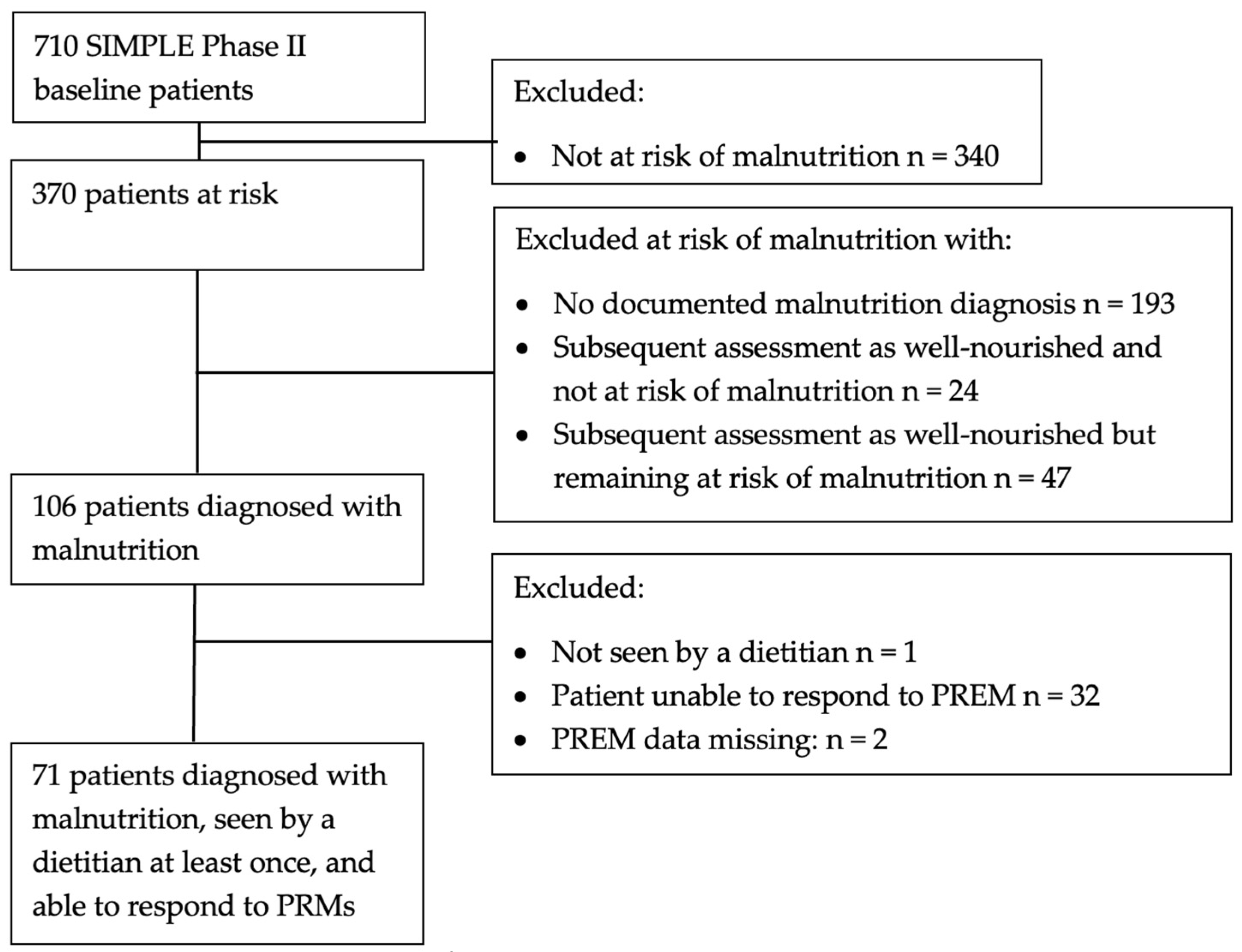
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bellanti, F.; Lo Buglio, A.; Quiete, S.; Vendemiale, G. Malnutrition in Hospitalized Old Patients: Screening and Diagnosis, Clinical Outcomes, and Management. Nutrients 2022, 14, 910. [Google Scholar] [CrossRef] [PubMed]
- Uhl, S.; Siddique, S.M.; McKeever, L.; Bloschichak, A.; D’Anci, K.; Leas, B.; Mull, N.K.; Tsou, A.Y. AHRQ Comparative Effectiveness Reviews. In Malnutrition in Hospitalized Adults: A Systematic Review; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2021. [Google Scholar] [CrossRef]
- Barker, L.A.; Gout, B.S.; Crowe, T.C. Hospital malnutrition: Prevalence, identification and impact on patients and the healthcare system. Int. J. Environ. Res. Public Health 2011, 8, 514–527. [Google Scholar] [CrossRef]
- Volkert, D.; Kiesswetter, E.; Cederholm, T.; Donini, L.M.; Eglseer, D.; Norman, K.; Schneider, S.M.; Ströbele-Benschop, N.; Torbahn, G.; Wirth, R.; et al. Development of a Model on Determinants of Malnutrition in Aged Persons: A MaNuEL Project. Gerontol. Geriatr. Med. 2019, 5, 2333721419858438. [Google Scholar] [CrossRef] [PubMed]
- O’Keeffe, M.; Kelly, M.; O’Herlihy, E.; O’Toole, P.W.; Kearney, P.M.; Timmons, S.; O’Shea, E.; Stanton, C.; Hickson, M.; Rolland, Y.; et al. Potentially modifiable determinants of malnutrition in older adults: A systematic review. Clin. Nutr. 2019, 38, 2477–2498. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.; Nisbett, N. The Basic Determinants of Malnutrition: Resources, Structures, Ideas and Power. Int. J. Health Policy Manag. 2021, 10, 817–827. [Google Scholar] [CrossRef]
- Young, A.M. Solving the wicked problem of hospital malnutrition. Nutr. Diet. 2015, 72, 200–204. [Google Scholar] [CrossRef]
- Norman, K.; Haß, U.; Pirlich, M. Malnutrition in Older Adults-Recent Advances and Remaining Challenges. Nutrients 2021, 13, 2764. [Google Scholar] [CrossRef]
- Swan, W.I.; Vivanti, A.; Hakel-Smith, N.A.; Hotson, B.; Orrevall, Y.; Trostler, N.; Beck Howarter, K.; Papoutsakis, C. Nutrition Care Process and Model Update: Toward Realizing People-Centered Care and Outcomes Management. J. Acad. Nutr. Diet. 2017, 117, 2003–2014. [Google Scholar] [CrossRef]
- Volkert, D.; Berner, Y.N.; Berry, E.; Cederholm, T.; Coti Bertrand, P.; Milne, A.; Palmblad, J.; Schneider, S.; Sobotka, L.; Stanga, Z.; et al. ESPEN Guidelines on Enteral Nutrition: Geriatrics. Clin. Nutr. 2006, 25, 330–360. [Google Scholar] [CrossRef]
- Druml, C.; Ballmer, P.E.; Druml, W.; Oehmichen, F.; Shenkin, A.; Singer, P.; Soeters, P.; Weimann, A.; Bischoff, S.C. ESPEN guideline on ethical aspects of artificial nutrition and hydration. Clin. Nutr. 2016, 35, 545–556. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.L.; Correia, M.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 38, 207–217. [Google Scholar] [CrossRef] [PubMed]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef] [PubMed]
- Dent, E.; Wright, O.R.L.; Woo, J.; Hoogendijk, E.O. Malnutrition in older adults. Lancet 2023, 401, 951–966. [Google Scholar] [CrossRef]
- Keller, H.; Koechl, J.M.; Laur, C.; Chen, H.; Curtis, L.; Dubin, J.A.; Gramlich, L.; Ray, S.; Valaitis, R.; Yang, Y.; et al. More-2-Eat implementation demonstrates that screening, assessment and treatment of malnourished patients can be spread and sustained in acute care; a multi-site, pretest post-test time series study. Clin. Nutr. 2021, 40, 2100–2108. [Google Scholar] [CrossRef]
- Bell, J.J.; Young, A.; Hill, J.; Banks, M.; Comans, T.; Barnes, R.; Keller, H.H. Rationale and developmental methodology for the SIMPLE approach: A Systematised, Interdisciplinary Malnutrition Pathway for impLementation and Evaluation in hospitals. Nutr. Diet. J. Dietit. Assoc. Aust. 2018, 75, 226–234. [Google Scholar] [CrossRef] [PubMed]
- Bell, J.J.; Young, A.M.; Hill, J.M.; Banks, M.D.; Comans, T.A.; Barnes, R.; Keller, H.H. Systematised, Interdisciplinary Malnutrition Program for impLementation and Evaluation delivers improved hospital nutrition care processes and patient reported experiences—An implementation study. Nutr. Diet. 2021, 78, 466–475. [Google Scholar] [CrossRef] [PubMed]
- Tappenden, K.A.; Quatrara, B.; Parkhurst, M.L.; Malone, A.M.; Fanjiang, G.; Ziegler, T.R. Critical Role of Nutrition in Improving Quality of Care: An Interdisciplinary Call to Action to Address Adult Hospital Malnutrition. J. Parenter. Enter. Nutr. 2013, 37, 482–497. [Google Scholar] [CrossRef]
- Bell, J.J.; Bauer, J.D.; Capra, S.; Pulle, R.C. Multidisciplinary, multi-modal nutritional care in acute hip fracture inpatients—Results of a pragmatic intervention. Clin. Nutr. 2014, 33, 1101–1107. [Google Scholar] [CrossRef]
- Rushton, A.; Edwards, A.; Bauer, J.; Bell, J.J. Dietitian assistant opportunities within the nutrition care process for patients with or at risk of malnutrition: A systematic review. Nutr. Diet. 2021, 78, 69–85. [Google Scholar] [CrossRef]
- ten Cate, D.; Ettema, R.G.A.; Huisman-de Waal, G.; Bell, J.J.; Verbrugge, R.; Schoonhoven, L.; Schuurmans, M.J.; Basic Care Revisited Group (BCR). Interventions to prevent and treat malnutrition in older adults to be carried out by nurses: A systematic review. J. Clin. Nurs. 2020, 29, 1883–1902. [Google Scholar] [CrossRef]
- Keller, H.; Laur, C.; Atkins, M.; Bernier, P.; Butterworth, D.; Davidson, B.; Hotson, B.; Nasser, R.; Laporte, M.; Marcell, C. Update on the Integrated Nutrition Pathway for Acute Care (INPAC): Post implementation tailoring and toolkit to support practice improvements. Nutr. J. 2018, 17, 2. [Google Scholar] [CrossRef]
- Keller, H.H.; Valaitis, R.; Laur, C.V.; McNicholl, T.; Xu, Y.; Dubin, J.A.; Curtis, L.; Obiorah, S.; Ray, S.; Bernier, P.; et al. Multi-site implementation of nutrition screening and diagnosis in medical care units: Success of the More-2-Eat project. Clin. Nutr. 2019, 38, 897–905. [Google Scholar] [CrossRef] [PubMed]
- Keller, H.H.; Xu, Y.; Dubin, J.A.; Curtis, L.; Laur, C.V.; Bell, J. Improving the standard of nutrition care in hospital: Mealtime barriers reduced with implementation of the Integrated Nutrition Pathway for Acute Care. Clin. Nutr. ESPEN 2018, 28, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Australian Commission on Safety and Quality in Healthcare. Comprehensive Care Standard. Available online: https://www.safetyandquality.gov.au/standards/nsqhs-standards/comprehensive-care-standard#background-to-this-standard (accessed on 17 February 2023).
- Australian Commission on Safety and Quality in Healthcare. Partnering with Consumers Standard. Available online: https://www.safetyandquality.gov.au/standards/nsqhs-standards/partnering-consumers-standard (accessed on 20 February 2023).
- Erickson, N.; Schinkoethe, T.; Eckhardt, C.; Storck, L.; Joos, A.; Liu, L.; Ballmer, P.E.; Mumm, F.; Fey, T.; Heinemann, V. Patient-reported outcome measures obtained via E-Health tools ease the assessment burden and encourage patient participation in cancer care (PaCC Study). Support Care Cancer 2021, 29, 7715–7724. [Google Scholar] [CrossRef]
- Kozica-Olenski, S.; Treleaven, E.; Hewitt, M.; McRae, P.; Young, A.; Walsh, Z.; Mudge, A. Patient-reported experiences of mealtime care and food access in acute and rehabilitation hospital settings: A cross-sectional survey. J. Hum. Nutr. Diet. Off. J. Br. Diet. Assoc. 2021, 34, 687–694. [Google Scholar] [CrossRef]
- Keller, H.; Allard, J.; Vesnaver, E.; Laporte, M.; Gramlich, L.; Bernier, P.; Davidson, B.; Duerksen, D.; Jeejeebhoy, K.; Payette, H. Barriers to food intake in acute care hospitals: A report of the Canadian Malnutrition Task Force. J. Hum. Nutr. Diet. Off. J. Br. Diet. Assoc. 2015, 28, 546–557. [Google Scholar] [CrossRef]
- Bell Jack, J.; Young Adrienne, M.; Hill, J.; Banks, M.D.; Comans, T.; Barnes, R. Allied Health Implementation Project Final Report: SIMPLE; Queensland Health: Brisbane, Australia, 2020. [Google Scholar]
- Wilkinson, S.A.; Bell, J.J.; Neaves, B.; McCray, S.J.; Campbell, K. Qualitative analysis of the implementation of a hospital room service in a large metropolitan hospital: Foundations for transformation. JBI Evid. Implement. 2022, 20, 199–208. [Google Scholar] [CrossRef]
- Neaves, B.; Bell, J.J.; McCray, S. Impact of room service on nutritional intake, plate and production waste, meal quality and patient satisfaction and meal costs: A single site pre-post evaluation. Nutr. Diet. 2022, 79, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Rushton, A.; Young, A.; Keller, H.; Bauer, J.; Bell, J. Delegation Opportunities for Malnutrition Care Activities to Dietitian Assistants—Findings of a Multi-Site Survey. Healthcare 2021, 9, 446. [Google Scholar] [CrossRef]
- Rushton, A.; Elmas, K.; Bauer, J.; Bell, J.J. Identifying Low Value Malnutrition Care Activities for De-Implementation and Systematised, Interdisciplinary Alternatives—A Multi-Site, Nominal Group Technique Approach. Nutrients 2021, 13, 2063. [Google Scholar] [CrossRef]
- Rushton, A.; Bauer, J.; Young, A.; Keller, H.; Bell, J. Barriers and Enablers to Delegating Malnutrition Care Activities to Dietitian Assistants. Nutrients 2022, 14, 1037. [Google Scholar] [CrossRef]
- Detsky, A.S.; McLaughlin, J.R.; Baker, J.P.; Johnston, N.; Whittaker, S.; Mendelson, R.A.; Jeejeebhoy, K.N. What is subjective global assessment of nutritional status? JPEN J. Parenter. Enter. Nutr. 1987, 11, 8–13. [Google Scholar] [CrossRef]
- National Centre for Classification in Health. The International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification (ICD-10-AM): Tabular List of Diseases, 5th ed.; Shannon Books: Sydney, Australia, 2006. [Google Scholar]
- Kaiser, M.J.; Bauer, J.M.; Ramsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.; Charlton, K.E.; Maggio, M.; et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): A practical tool for identification of nutritional status. J. Nutr. Health Aging 2009, 13, 782–788. [Google Scholar] [CrossRef]
- Young, A.; Keller, H.; Barnes, R.; Bell, J. Clinicians as novice facilitators: A SIMPLE case study. J. Health Organ. Manag. 2019, 33, 78–92. [Google Scholar] [CrossRef] [PubMed]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. IS 2009, 4, 50. [Google Scholar] [CrossRef] [PubMed]
- Bell, J.J.; Rossi, T.; Bauer, J.D.; Capra, S. Developing and evaluating interventions that are applicable and relevant to inpatients and those who care for them; a multiphase, pragmatic action research approach. BMC Med. Res. Methodol. 2014, 14, 98. [Google Scholar] [CrossRef]
- Curtis, L.J.; Bernier, P.; Jeejeebhoy, K.; Allard, J.; Duerksen, D.; Gramlich, L.; Laporte, M.; Keller, H.H. Costs of hospital malnutrition. Clin. Nutr. 2017, 36, 1391–1396. [Google Scholar] [CrossRef]
- Abizanda, P.; Sinclair, A.; Barcons, N.; Lizán, L.; Rodríguez-Mañas, L. Costs of Malnutrition in Institutionalized and Community-Dwelling Older Adults: A Systematic Review. J. Am. Med. Dir. Assoc. 2016, 17, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cruz-Jentoft, A.; Hooper, L.; Kiesswetter, E.; Maggio, M.; Raynaud-Simon, A.; Sieber, C.; Sobotka, L.; et al. ESPEN practical guideline: Clinical nutrition and hydration in geriatrics. Clin. Nutr. 2022, 41, 958–989. [Google Scholar] [CrossRef]
- Barry, M.J.; Edgman-Levitan, S. Shared Decision Making—The Pinnacle of Patient-Centered Care. N. Engl. J. Med. 2012, 366, 780–781. [Google Scholar] [CrossRef]
- Laur, C.; Curtis, L.; Dubin, J.; McNicholl, T.; Valaitis, R.; Douglas, P.; Bell, J.; Bernier, P.; Keller, H. Nutrition Care after Discharge from Hospital: An Exploratory Analysis from the More-2-Eat Study. Healthcare 2018, 6, 9. [Google Scholar] [CrossRef]
- Braithwaite, J. Changing how we think about healthcare improvement. BMJ 2018, 361, k2014. [Google Scholar] [CrossRef] [PubMed]
- Higgins, T.; Larson, E.; Schnall, R. Unraveling the meaning of patient engagement: A concept analysis. Patient Educ. Couns. 2017, 100, 30–36. [Google Scholar] [CrossRef]
- Bramer, G.R. International statistical classification of diseases and related health problems. Tenth revision. World Health Stat. Q. 1988, 41, 32–36. [Google Scholar]
- Burnes, D.; Sheppard, C.; Henderson, C.R., Jr.; Wassel, M.; Cope, R.; Barber, C.; Pillemer, K. Interventions to Reduce Ageism Against Older Adults: A Systematic Review and Meta-Analysis. Am. J. Public Health 2019, 109, e1–e9. [Google Scholar] [CrossRef] [PubMed]
- Ek, S. Gender differences in health information behaviour: A Finnish population-based survey. Health Promot. Int. 2013, 30, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Hooker, R.S.; Williams, J.H.; Papneja, J.; Sen, N.; Hogan, P. Dietetics supply and demand: 2010–2020. J. Acad. Nutr. Diet 2012, 112, S75–S91. [Google Scholar] [CrossRef]
- Joy, P.; Gheller, B.; Lordly, D. Men who are Dietitians: Deconstructing Gender within the Profession to Inform Recruitment. Can. J. Diet Pract. Res. 2019, 80, 209–212. [Google Scholar] [CrossRef]
- Geraghty, A.A.; Browne, S.; Reynolds, C.M.E.; Kennelly, S.; Kelly, L.; McCallum, K.; McBean, L.; Clyne, B.; Bury, G.; Bradley, C.; et al. Malnutrition: A Misunderstood Diagnosis by Primary Care Health Care Professionals and Community-Dwelling Older Adults in Ireland. J. Acad. Nutr. Diet 2021, 121, 2443–2453. [Google Scholar] [CrossRef]
- Verwijs, M.H.; Puijk-Hekman, S.; van der Heijden, E.; Vasse, E.; de Groot, L.; de van der Schueren, M.A.E. Interdisciplinary communication and collaboration as key to improved nutritional care of malnourished older adults across health-care settings—A qualitative study. Health Expect 2020, 23, 1096–1107. [Google Scholar] [CrossRef]
- Labouvie-Vief, G.; Medler, M. Affect optimization and affect complexity: Modes and styles of regulation in adulthood. Psychol. Aging 2002, 17, 571–588. [Google Scholar] [CrossRef] [PubMed]
- Kerac, M.; McGrath, M.; Connell, N.; Kompala, C.; Moore, W.H.; Bailey, J.; Bandsma, R.; Berkley, J.A.; Briend, A.; Collins, S.; et al. ‘Severe malnutrition’: Thinking deeplyS, communicating simply. BMJ Glob. Health 2020, 5, e00302. [Google Scholar] [CrossRef] [PubMed]
- Meloncelli, N.; Young, A.; Christoffersen, A.; Rushton, A.; Zhelnov, P.; Wilkinson, S.A.; Scott, A.M.; de Jersey, S. Co-designing nutrition interventions with consumers: A scoping review. J. Hum. Nutr. Diet. Off. J. Br. Diet. Assoc. 2022; Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
| Original SIMPLE Patient-Reported Measures | Revised Patient-Reported Measures | |
|---|---|---|
| PRM 1 | Our nutrition screening process indicates you are at risk of malnutrition. Has anybody made you aware of this already? | I am here today because you have been identified as at risk of malnutrition. This is because you have a medical condition that places you at an increased risk of being malnourished, or it might be because you told a staff member that you have lost some weight, had a poor appetite, or you weren’t sure if you had lost any weight. Has anybody discussed this with you? |
| PRM 2 | Have you seen or received any information or resources regarding nutrition? | Has someone provided you with any information about being at risk of malnutrition since you have been in hospital? |
| PRM 3 | Has anybody discussed whether you need ongoing nutrition care and monitoring in hospital or after you leave hospital | Do you have a plan for ongoing nutrition care (prompts: dietitian or GP follow up)? |
| Characteristic | ||
|---|---|---|
| Hospital location: n (%) | ||
| Metropolitan | 37 | (52.1) |
| Regional or rural a | 34 | (47.9) |
| Age in years: median (IQR) b | 81 | (15) |
| Sex: n (%) | ||
| Female | 46 | 64.8 |
| Male | 25 | 35.2 |
| Length of stay in days until time of audit: median (IQR) | 6 | (12) |
| Malnutrition severity: n (%) | ||
| Mild/moderate or unspecified a severity | 54 | 76.1 |
| Severe | 17 | 23.9 |
| Number of dietitian chart entries: median (IQR) | 2 | (2) |
| Documented nutrition support: n (%) | ||
| None or missing a | 3 | 4.2 |
| One or more nutrition support processes | 68 | 95.8 |
| Patient-Reported Measures | No n (%) | Yes n (%) |
|---|---|---|
| You have been identified as at risk of malnutrition. Has anybody discussed this with you? | 34 (47.9) | 37 (52.1) |
| Have you been provided with any information about being at risk of malnutrition? | 41 (57.7) | 30 (42.3) |
| Do you have an ongoing plan for nutrition care or follow-up? | 40 (56.3) | 31 (43.7) |
| Patient Characteristics | Reported Receiving Malnutrition Diagnosis, Receiving Information about Malnutrition, and Having a Plan for Ongoing Care or Follow-Up | |
|---|---|---|
| No (n = 56) | Yes (n = 15) | |
| Hospital location: n (%) | ||
| Metropolitan | 31 (55.4) | 6 (40.0) |
| Regional or rural | 25 (44.6) | 9 (60.0) |
| Age in years: median (IQR) a | 83 (13) | 72 (26) |
| Sex: n (%) | ||
| Female | 40 (71.4) | 6 (40.0) |
| Male | 16 (28.6) | 9 (60.0) |
| Length of stay in days until time of audit: median (IQR) | 6 (11) | 4 (16) |
| Malnutrition severity: n (%) | ||
| Mild/moderate or unspecified | 43 (76.8) | 11 (73.3) |
| Severe | 13 (23.2) | 4 (26.7) |
| Number of dietitian chart entries: median (IQR) | 2 (2) | 2 (3) |
| Documented nutrition support: n (%) | ||
| None or missing | 2 (3.6) | 1 (6.7) |
| One or more nutrition support processes | 54 (98.2) | 14 (93.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bell, J.J.; Rushton, A.; Elmas, K.; Banks, M.D.; Barnes, R.; Young, A.M. Are Malnourished Inpatients Treated by Dietitians Active Participants in Their Nutrition Care? Findings of an Exploratory Study of Patient-Reported Measures across Nine Australian Hospitals. Healthcare 2023, 11, 1172. https://doi.org/10.3390/healthcare11081172
Bell JJ, Rushton A, Elmas K, Banks MD, Barnes R, Young AM. Are Malnourished Inpatients Treated by Dietitians Active Participants in Their Nutrition Care? Findings of an Exploratory Study of Patient-Reported Measures across Nine Australian Hospitals. Healthcare. 2023; 11(8):1172. https://doi.org/10.3390/healthcare11081172
Chicago/Turabian StyleBell, Jack J., Alita Rushton, Kai Elmas, Merrilyn D. Banks, Rhiannon Barnes, and Adrienne M. Young. 2023. "Are Malnourished Inpatients Treated by Dietitians Active Participants in Their Nutrition Care? Findings of an Exploratory Study of Patient-Reported Measures across Nine Australian Hospitals" Healthcare 11, no. 8: 1172. https://doi.org/10.3390/healthcare11081172
APA StyleBell, J. J., Rushton, A., Elmas, K., Banks, M. D., Barnes, R., & Young, A. M. (2023). Are Malnourished Inpatients Treated by Dietitians Active Participants in Their Nutrition Care? Findings of an Exploratory Study of Patient-Reported Measures across Nine Australian Hospitals. Healthcare, 11(8), 1172. https://doi.org/10.3390/healthcare11081172






