Abstract
Background: Diabetic peripheral neuropathy (DPN) is one of the most common complications of type 2 diabetes mellitus. There is a gradual loss of protective sensation in the skin and the function of the foot joints, increasing the risk of injury as the disease progresses. The objective of this study was to verify whether socioeconomic factors, health risk factors, and self-care are associated with DPN. Methods: Observational cross-sectional with 228 individuals of ≥30 years in Family Health Strategies in a city in the eastern Amazon, in northern Brazil, using questionnaires containing socioeconomic information, clinical and laboratory parameters, the Summary of Diabetes Self-Care Activities Questionnaire, and the Michigan Neuropathy Screening Instrument. Results: The prevalence of DPN was 66.6%. The presence of neuropathy is associated with male gender, dyslipidemia, and increased microalbuminuria. Logistic regression analysis revealed male subjects’ increased BMI and altered HDL levels were associated with DPN. Conclusions: In men with altered BMI, and dysregulation in biochemical parameters, neuropathy is more prevalent.
1. Introduction
Type 2 diabetes mellitus (DM2) is the most common type of diabetes [1]. The high prevalence of DM2 is related to urbanization, epidemiological transition, nutritional transition, adoption of a sedentary lifestyle, population growth, and aging [2]. This disease can generate complications and aggravations, such as diabetic peripheral neuropathy (DPN), that can appear with disease progression if not treated and monitored.
DPN is characterized by peripheral nerve dysfunction that leads to a gradual loss of protective sensation in the lower limbs, especially in the feet, increasing the risk of injury [3]. In Brazil, the occurrence of “diabetic foot” as a result of DPN is frequent owing to poor glycemic control, lack of information, non-adherence to treatment, and economic difficulties, in addition to specific problems related to poor hygiene and inappropriate use of shoes [4]. In the early stages, motor deficits are uncommon, but symptoms such as pain, burning, and tingling are present in a third of patients diagnosed with neuropathy [5].
However, if there are injuries, individuals are more susceptible to infections, necrosis, and even limb amputations, which are responsible for the increase in the number of hospitalizations, generating an impact on health resources [6] with significant damage to quality of life, functionality, activities of daily living, family, and social dynamics [4]. The damage can decrease with the expansion of neuropathy screening and guidelines on foot care practices [7]. The risk factors are diverse but depend on the specifics of each region.
Developing countries concentrate on most cases with a tendency to increase in the coming decades and, consequently, the prospect of higher expenses due to complications and treatment of diabetes. In this context, Brazil is among the five countries with the highest number of people living with diabetes [1]. Few studies on DPN screening [8,9,10,11] and self-care for diabetes control using specific instruments in patients treated in primary healthcare in Brazil have been developed. This is especially true in the northern part of the country, the Amazon region, which has social, economic, and cultural issues. These characteristics can affect the self-care practices of these individuals.
The American Diabetes Association (2022) recommends performing DPN screening annually to identify risk factors for ulcers and amputation [12]. In Brazil, the Ministry of Health established, as a screening technique, the evaluation of tactile sensitivity using Semmes–Weinstein monofilament (10 g), vibratory sensitivity with a 128 Hz tuning fork, and Achilles tendon reflex through percussion [13]. However, DPN screening tools that assess signs and symptoms, as well as physical examination, are necessary to assess the damage to patients’ quality of life and map the progression of changes systematically and quantitatively, which is crucial for adequate therapy [14]. Knowing that the application of instruments for the early diagnosis of DPN can direct intervention strategies for the management of exposure to multiple risk factors, reduce the incidence, and delay the progression of DPN [15], this study emerged as a model for evaluating the implementation of the Family Health Strategy (FHS).
Therefore, this study aimed to verify whether socioeconomic status, health risk factors, and self-care were associated with DPN. In addition, the prevalence of diabetic neuropathy in individuals followed up in primary healthcare facilities was identified. Nevertheless, we analyzed whether these risk factors were associated with neuropathy. Our initial hypothesis was that diabetic neuropathy may be associated with socioeconomic and health risk factors. In addition, self-care may be a determinant of DPN in patients with type 2 diabetes.
2. Materials and Methods
2.1. Study Design
This was an observational cross-sectional study with descriptive and inferential analyses.
2.2. Setting and Period of Study
The study used data from the participants’ baseline assessment in the project “Amazon Amandaba: Culture Circles as a strategy to encourage self-care for DM in Primary Health Care,” carried out in November and December 2021. The study was conducted in November and December 2021 in the Family Health Strategy units of the two most populous administrative districts of Belém, Pará in the eastern Amazon. The study abided by the Ethics Committee of the Institute of Health Sciences of the Federal University of Pará (n. 4,693,984).
2.3. Population
The study population included individuals with type 2 diabetes mellitus aged 30 years or older (n = 2099).
2.4. Sampling
We used the simple random probability sampling method. In case of refusal, a new participant was selected by lot.
2.5. Sample Size
The sample size was calculated according to Bashar et al. (2021) [16]. The variable “Glycemic control (based on Hb1Ac)” was used as a reference. The values were: odds ratio (OR) = 0.28, proportion p2 = 0.55, error probability α = 0.05, β = 0.20, and allocation ratio N2/N1 = 1.38. The minimum sample size defined was 90 participants.
2.6. Sample
Initially, 2099 individuals were evaluated for eligibility and randomization. The initial sample consisted of 230 individuals; 228 participants were selected for analysis and grouped into individuals with (n = 76) or without (n = 152) diabetic neuropathy (Figure 1).
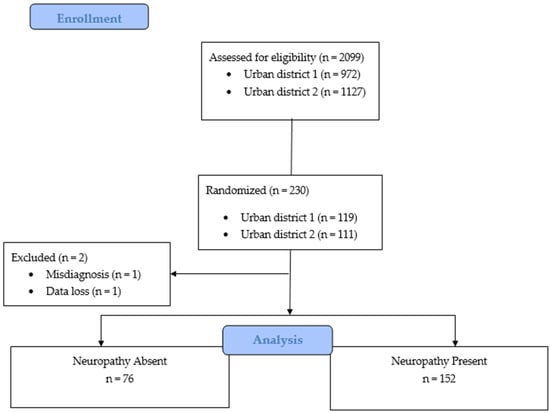
Figure 1.
Flow diagram of the selection and distribution of individuals in the groups.
2.7. Eligibility Criteria
Individuals aged ≥ 30 years, enrolled in the “Hipertensão e Diabetes” Program (HIPERDIA) assisted in the FHS units, who received the medical diagnosis of type 2 diabetes mellitus at least one year ago, were residents in the two most populous administrative districts, and agreed to participate, were selected for this study by lot. Exclusion criteria were: presenting the neurological diseases, including Alzheimer’s disease, spinal cord injury, stroke, and multiple sclerosis; individuals with complete or significant hearing loss that would interfere with communication during the study; and individuals who were bedridden.
2.8. Data Collection and Variables
Social data (age, sex, race/color, education (years), marital status, and income), health habits, clinical characteristics (DM2 diagnosis time (years)), perception of general health status, smoking, systolic arterial hypertension (SAH), and body mass index (BMI, kg/m2). In addition, biochemical parameters, including blood glucose (normal: 55–130; high: ≥130 mg/dL), triglycerides (normal: 36–149; high: ≥150 mg/dL), total cholesterol (normal: 87–189; high: ≥190 mg/dL), high-density lipoprotein—HDL (normal: 20–39; high: ≥40 mg/dL), low-density lipoprotein—LDL (normal: 15–99; ≥100 mg/dL), non high-density lipoprotein—NHDL (normal: 59–129; high: ≥130 mg/dL), HbA1c (normal: 4.8–6.9; high ≥7%), and microalbuminuria (normal: <30; micro: 30–300; macro: >300 mg/g), were obtained through laboratory tests.
To measure the perception of self-care, we used the Summary of Diabetes Self-Care Activities Questionnaire, which was translated and adapted to Portuguese [17]. This questionnaire is an instrument that identifies the performance and frequency of activities performed by people with diabetes related to their self-care in the seven days before the evaluation. The answers ranged from 0 to 7, and the scores indicated the performance of these self-care activities. The questionnaire assesses five aspects of the diabetes treatment regimen and groups them into six dimensions of 15 items (general diet, specific diet, exercise, blood glucose testing, foot care, and medication) [17].
Michigan Neuropathy Screening Instrument (MSNI)
The Michigan Neuropathy Screening Instrument (MNSI) is a low-cost, quick-to-use tool for evaluating, classifying, and diagnosing diabetic neuropathy. The instrument had two sections (A and B). The first section refers to the participant’s clinical history and contains 15 questions whose answers are summed to obtain the final score for this section. The second section refers to physical examination, starting with the inspection of the feet to observe skin dryness, callus formation, fissures, and the presence of ulcers or deformities. We then performed tests of vibration sensitivity of the hallux with a tuning fork of 128 Hz, in addition to a neurological ankle reflex, and a sensitivity test with a 10 g monofilament [18]. The total scores in Sections A and B were calculated. We assumed a score of 3 (total of 12 in section A) and 2 (total of 10 in section B) as the cutoffs. MSNI values ≤ 5 = no neuropathy, 5.5–10 = moderate neuropathy, and 16.5–22 = severe neuropathy [19].
2.9. Study Outcomes
The primary outcome was the presence or absence of diabetic foot neuropathy in patients with DM2.
2.10. Bias
Participants were recruited by direct contact after drawing, and if they did not agree to participate in the study, they were replaced by another randomly-selected individual. To minimize possible late-response biases, the benefit of returning the laboratory test results was offered to the research participants and to the health unit to which they were linked to encourage participation in the study.
2.11. Statistical Analysis
Descriptive statistical analysis was used to identify the frequency (absolute and relative), mean, standard deviation, and median with interquartile range. Categorical variables were analyzed using the chi-square test (χ2), and continuous variables were analyzed using the Mann–Whitney test (U). Binary logistic regression was used to identify independent variables that could be associated with diabetic peripheral neuropathy. The reference value adopted for entering these variables into the multivariate logistic regression model was p ≤ 0.25 [20], with no multicollinearity (tolerance > 0.10, variance inflation factor—VIF < 10). A p-value < 0.05 was considered statistically significant for the association between variables in this analysis.
3. Results
3.1. Prevalence of Diabetic Peripheral Neuropathy
The prevalence of diabetic neuropathy was 152 (66.6%), as determined by the combined score of the two parts of the MSNI, history of symptoms, and physical assessment of the feet.
3.2. Social Characteristics
In total, 228 participants were studied. The participant characteristics were as follows: female (52.6%), brown-skin (60.8%), > 61 years of age (57.4%), less than four years of schooling (35.1%), and married (48.2%). The monthly income survey participants lived on was less than one minimum wage (396.46 reais per family member) (Table 1).

Table 1.
Socioeconomic and clinical characteristics and health habits, biochemical parameters of the participants and perception of self-care in diabetes.
The differences between the groups with or without neuropathy showed that men were more frequently affected by neuropathy (p = 0.024). Other variables were not statistically significant.
3.3. Health-Related and Clinical Characteristics
The timing of the DM2 diagnosis was 10–19 years for the entire sample. Most of the participants were individuals with a smoking history (51.8%) and SAH (69.2%). Regarding participants’ self-perception of their general health, 47.3% considered their health to be regular. The participants had a mean BMI value of 28.87 kg/m2, indicating overweight (Table 1). There was no difference between these parameters in participants with and without neuropathy.
3.4. Biochemical Parameters
Based on established biochemical parameters, blood glucose (67.9%), triglycerides (62.2%), total cholesterol (51.3%), HDL (51.7%), LDL (62.7%), NHDL (64.9%), and HbA1c (82.8%) levels showed changes in the studied samples. Regarding the microalbuminuria parameters, 71.1% of the participants were within the adopted target values.
When comparing the parameters between individuals with and without neuropathy, altered triglyceride (Zcrit > 1.96), HDL (p = 0.031), and NHDL (p = 0.049) levels were more prevalent in individuals without neuropathy. However, altered microalbuminuria (p = 0.033) was associated with neuropathy.
3.5. Diabetes Self-Care Activities
The participants followed self-care practice 2.5 and 2.6 days a week for general and specific diet domains, respectively. The exercise and blood glucose testing domains were the least performed by the participants (0 days), while the foot care and medication domains were the practices most carried out by the participants during a week (4.0 and 4.6 days, respectively) (Table 1).
Participants’ perception of diabetes self-care did not show a statistically significant difference between the groups with or without neuropathy.
3.6. Associated Factors with Diabetic Peripheral Neuropathy
Variables that were significant in the univariate binary logistic regression analysis (p < 0.25) without multicollinearity (VIF > 10) were entered into the multivariate binary logistic regression model as independent variables, and the outcome (presence or absence of neuropathy) as a dependent variable. Thus, of the 11 variables selected, three were considered to be statistically significant associated with the prevalence of diabetic neuropathy (Table 2). The associated variables were sex, BMI, and HDL cholesterol levels. Male diabetic participants were less likely to develop neuropathy than female participants (OR, 0.50; 95% confidence interval [CI]: 0.26, 0.96, p = 0.03). Participants with high BMI were more likely to develop diabetic neuropathy (OR 1.05; 95% CI: 1.00, 1.10, 0.96, p = 0.05), and those with established non-standard HDL were more likely to develop neuropathy (OR 2.06; 95% CI: 1.07, 3.97, p = 0.03).

Table 2.
Univariate and multivariate binary regression analysis of variables (socioeconomic, clinical, health, and self-care habits) associated with diabetic neuropathy.
4. Discussion
This study sought to identify the prevalence of DPN and its relationship with socioeconomic determinants, health habits, biochemical parameters, and perception of self-care in 228 individuals with DM2, who were randomly selected in two administrative districts of a municipality in the northern region of Brazil.
The prevalence of diabetic peripheral neuropathy was 66.6%, with a significant difference according to sex. Men had a higher incidence of DPN (52.6%) compared to women (47.3%). This result was above the average prevalence reported in other studies (between 38% and 42%) in Jordan, Ethiopia, and India [6,16]. Studies in Latin American countries [21,22,23] have shown a prevalence of > 69%. This prevalence may be influenced by the characteristics of each location/region.
The participants, regardless of neuropathy, had a healthy diet, blood glucose monitoring, and less frequent physical activity. These findings are consistent with those of studies conducted in other regions of Brazil [24,25,26]. The use of drugs was a constant practice, which may be related to free access offered by the Unified Health System [27]. Foot care was also a common practice, differing from the average number of days reported in other studies [24,25,26,28].
Our data revealed a high adherence to medication and foot care. Other self-care practices were less frequent. This relationship between poor self-care practices in diabetes and neuropathy requires monitoring, even with high foot care.
High levels of triglycerides, HDL, NHDL, and microalbuminuria were frequent among patients with diabetic neuropathy. In agreement with other reports, it is possible that dyslipidemia is associated with the risk of developing DPN. Evidence supports that treatments for lowering cholesterol and triglycerides help reduce the progression of diabetes complications such as neuropathy [29,30,31]. The controlled levels of microalbuminuria in participants showed a significant association with the presence of neuropathy. Previous studies have demonstrated that DPN is associated with high levels of microalbuminuria [32,33].
Evidence suggests that treatments for lowering cholesterol and triglycerides help reduce the progression of diabetes complications, such as neuropathy [29,30,31]. The controlled levels of microalbuminuria in participants showed a significant association with the presence of neuropathy. Previous studies have demonstrated that DPN is associated with high levels of microalbuminuria [32,33].
The variables Identified as associated with neuropathy were male sex, high HDL levels, and high BMI. Hypercholesterolemia and obesity are significant risk factors for early diabetic neuropathy, independent of glycemic control [6,34,35,36]. HDL contains all atherogenic lipoproteins, which are important parameters for cardiovascular risk. Vascular risk factors are also risk factors for DPN in diabetic and non-diabetic populations [34]. The role of obesity in DPN seems to be related to the activation of inflammatory signaling pathways, given that the chronic inflammatory process seems to be important in the pathogenesis of this complication [37]. Obese patients with diabetes have higher levels of oxidative stress, which is also associated with DPN [38,39]. In relation to males, the differences in lifestyle and testosterone deficiency, which is common in men with diabetes [40], must be taken into account.
Type 2 DM has been associated with long-term macrovascular (atherosclerosis, coronary heart disease, cardiomyopathy, cerebrovascular disease, peripheral artery disease, and lower extremity amputations) and microvascular (retinopathy, nephropathy and neuropathy) complications. This dysfunction is related to an increase in circulating inflammatory factors (C-reactive protein, chemokines, and cytokines), and when associated with obesity-related insulin resistance it is related to worse outcomes [41]. In this study, we observed altered BMI in individuals with NPD. Therefore, the involvement of inflammation should be considered in future research, aiming to verify the role of these markers in the development of this dysfunction.
The limitations of this study are a cross-sectional design, and the sample size of the study is related to the population studied, which should not generalize the findings. Some variables associated with DPN have been identified; however, other structural and socioeconomic issues need to be considered. This affects the patterns that contribute to these risk factors, such as food choice, food insecurity, access to healthy food options, cultural factors, and the social determinants of health.
The use of screening instruments for DPN is low-cost and easily accessible, which prevents late diagnosis and poor prognosis. Knowing the associated aspects of DPN is necessary for developing well-targeted and individualized preventive strategies.
5. Conclusions
The prevalence of diabetic neuropathy in these individuals following primary healthcare was 66.6%. Male sex, biochemical parameters, such as triglyceride, HDL, NHDL, and microalbuminuria were associated with DPN. The variables associated with neuropathy were male sex, high BMI, and HDL. Early detection with screening tests and laboratory tests among people with DM is necessary for adequate follow-up.
Author Contributions
Conceptualization, A.L.d.F., M.d.S.C.-B.d.O.B. and J.S.d.M.-N.; Data curation, A.L.d.F., A.S.A.d.S., J.d.S.e.S. and V.B.T.; Formal analysis, and J.S.d.M.-N.; Methodology, A.L.d.F., A.S.A.d.S., V.B.T., M.d.S.C.-B.d.O.B. and J.S.d.M.-N.; Project administration, H.P.d.S., M.d.S.C.-B.d.O.B. and J.S.d.M.-N.; Supervision, M.d.S.C.-B.d.O.B. and J.S.d.M.-N.; Validation, H.P.d.S., M.d.S.C.-B.d.O.B. and J.S.d.M.-N.; Writing—original draft, A.L.d.F., V.B.T. and J.S.d.M.-N.; Writing—review and editing, all authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
All methods were carried out in accordance with relevant guidelines and regulations under Resolution 466/12 of the National Health Council of Brazil, and in accordance with the standards established in the Helsinki Declaration of 1975. The research was conducted after approval by the Research Local Ethics Committee of the (n. 4,693,984). Patient’s informed consent was performed prior to the start of the study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data not available due to ethical principles.
Conflicts of Interest
The authors declare no conflict of interest.
References
- International Diabetes Federation. IDF Diabetes Atlas, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021. [Google Scholar]
- Sociedade Brasileira de Diabetes. Diretrizes da Sociedade Brasileira de Diabetes 2019–2020; Editora Clanad: Sao Paulo, Brasil, 2019. [Google Scholar]
- Bodman, M.A.; Varacallo, M. Peripheral Diabetic Neuropathy; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Ministério da Saúde; Secretaria de Atenção à Saúde; Departamento de Atenção Básica. Estratégias para o Cuidado da Pessoa com Doença Crônica: Diabetes Mellitus; Ministério da Saúde; Secretaria de Atenção à Saúde; Departamento de Atenção Básica: Rio de Janeiro, Brasil, 2013. [Google Scholar]
- Tesfaye, S.; Selvarajah, D. Advances in the epidemiology, pathogenesis and management of diabetic peripheral neuropathy. Diab. Met. Res. Rev. 2012, 28, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Khawaja, N.; Abu-Shennar, J.; Saleh, M.; Dahbour, S.S.; Khader, Y.S.; Ajlouni, K.M. The prevalence and risk factors of peripheral neuropathy among patients with type 2 diabetes mellitus; the case of Jordan. Diabetol. Metab. Syndr. 2018, 10, 8. [Google Scholar] [CrossRef] [PubMed]
- Silva, F.M.; Viana, M.C.A.V.A.; Sousa, N.M.; Penha, A.A.G. Síntese de evidências para políticas de saúde: Prevenção e controle do pé diabético na atenção primária a saúde. Bis 2019, 20, 2–4. [Google Scholar] [CrossRef]
- Brinati, L.M.; Diogo, N.A.S.; Moreira, T.R.; Mendonça, E.T.; Amaro, M.O.F. Prevalência e fatores associados à neuropatia periférica em indivíduos com diabetes mellitus. Rev. Fund Care 2017, 9, 347–355. [Google Scholar] [CrossRef]
- Nascimento, J.W.A.; Silva, E.C.S.; Roque, G.S.L.; Ferreira Júnior, L.; Jesus, S.B. Correlação entre o tipo de calçado com alterações físicas em pés de diabéticos. Rev. Enferm. UFPI 2020, 9, e10189. [Google Scholar] [CrossRef]
- Borges, F.S.C.; Gama, H.S. Avaliação sensório-motora do tornozelo e pé entre idosos diabéticos e não diabéticos. Rev. Brasil Geri. Geront. 2010, 13, 93–102. [Google Scholar] [CrossRef]
- Gonçalves, I.E.S.; Reis, M.S.; Perez, V.C.; Silva, G.G.; Franciulli, P.M. Avaliação sensório motora de tornozelo e pé em pacientes diabéticos. Rev. Iberk-Am. Podol. 2020, 2, 101. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. Retinopathy, neuropathy, and foot care: Standards of Medical Care in Diabetes—2022. Diabetes Care 2022, 45, S185. [Google Scholar] [CrossRef]
- Ministério da Saúde; Secretaria de Atenção à Saúde; Departamento de Atenção Básica. Manual do pé diabético: Estratégias para o cuidado da pessoa com doença crônica; Departamento de Atenção Básica; Secretaria de Atenção à Saúde; Ministério da Saúde: Rio de Janeiro, Brasília, 2016. [Google Scholar]
- Sartor, C.D.; Oliveira, M.D.; Campos, V.; Ferreira, J.S.S.P.; Sacco, I.C.N. Cross-cultural adaptation and measurement properties of the Brazilian Version of the Michigan Neuropathy Screening Instrument. Bra. J. Phys. Ther. 2018, 22, 222–230. [Google Scholar] [CrossRef]
- Selvarajah, D.; Kar, D.; Khunti, K.; Davies, M.J.; Scott, A.R.; Walker, J.; Tesfaye, S. Diabetic peripheral neuropathy: Advances in diagnosis and strategies for screening and early intervention. Lancet Diabetes Endocrinol. 2019, 7, 938–948. [Google Scholar] [CrossRef]
- Bashar, M.D.A.; Verma, M. Prevalence and Determinants of Diabetic Peripheral Neuropathy/Foot Syndrome in the Rural Population of North India. Iberoam J. Med. 2021, 3, 18–25. [Google Scholar] [CrossRef]
- Michels, J.M.; Coral, M.H.C.; Sakae, T.M.; Damas, T.B.; Furlanetto, L.M. Questionário de Atividades de Autocuidado com o Diabetes: Tradução, adaptação e avaliação das propriedades psicométricas. Arq. Bras. De Endocrinol. Metabol. 2010, 54, 644–651. [Google Scholar] [CrossRef]
- Oliveira, F.B.; Botelho, K.K.P.; Bezerra, A.R.; Azevedo, D.I.O.; Paz, C.C.S.C.; Martins, E.F. Cross-cultural adaptation to Brazilian Portuguese of the Michigan Neuropathy Screening Instrument: MNSI-Brazil. Arq. Neuro-Psiquiatr. 2016, 74, 653–661. [Google Scholar] [CrossRef]
- Barbosa, M.; Saavedra, A.; Oliveira, S.; Reis, L.; Rodrigues, F.; Severo, M.; Sittl, R.; Maier, C.; Carvalho, D.M. Prevalence and Determinants of Painful and Painless Neuropathy in Type 1 Diabetes Mellitus. Front. Endocrinol. 2019, 10, 402. [Google Scholar] [CrossRef] [PubMed]
- Abdissa, D.; Sorsa, R.; Gerbi, A.; Hamba, N.; Banjaw, Z. Magnitude and associated factors of peripheral neuropathy among diabetes patients attending Jimma University Medical Center, Southwest Ethiopia. Heliyon 2021, 7, e08460. [Google Scholar] [CrossRef] [PubMed]
- Arellano-Longinos, S.A.; Godínez-Tamay, E.D.; Hernández-Miranda, M.B. Prevalencia de neuropatía diabética en pacientes con diabetes mellitus tipo 2 en una clínica regional del Estado de México. Aten. Fam. 2018, 25, 7–11. [Google Scholar] [CrossRef]
- Ibarra, C.T.R.; Rocha, J.J.L.; Hernández, R.O.; Nieves, R.E.R.; Leyva, R.J. Prevalencia de neuropatía periférica en diabéticos tipo 2 en el primer nivel de atención. Rev. Méd. Chile 2012, 140, 1126–1131. [Google Scholar] [CrossRef]
- Solís-Villanueva, J.; Michahelles-Barreno, C.; Rodríguez-Lay, E.G.; Farfán-García, J.; Anticona-Sayán, M.; Curo-Carrión, N.; Miranda-Montero, J.J.; Avilez, J.L.; Akehurst, H. Prevalencia y factores de riesgo de neuropatía diabética periférica en pacientes recientemente diagnosticados de diabetes mellitus tipo 2 en un hospital nacional. Rev. Soc. Peru Med. Int. 2019, 32, 4–8. [Google Scholar] [CrossRef]
- Freitas, S.S.; Silva, G.R.F.; Rezende Neta, D.S.; Silva, A.R.V. Analysis of the self-care of diabetics according to by the Summary of Diabetes Self-Care Activities Questionnaire (SDSCA). Acta Sci. Health Sci. 2014, 36, 73–81. [Google Scholar] [CrossRef]
- França, A.A.; Barbosa, J.A.G.; Guimaraes, F.P.; Guimarães, G.L.; Guimarães, J.B. Avaliação da adesão ao autocuidado em diabetes após intervenção educativa realizada com pacientes hospitalizados. Rev. Brasil. Ciênc. Saúde 2020, 24, 47260. [Google Scholar] [CrossRef]
- Imazu, M.F.M.; Faria, B.N.; Arruda, G.O.; Sales, C.A.; Marcon, S.S. Efetividade das intervenções individual e em grupo junto a pessoas com diabetes tipo 2 1. Rev. Lat. Americ. Enferm. 2015, 23, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Meiners, M.M.M.A.; Tavares, N.U.L.; Guimarães, L.S.P.; Bertoldi, A.D. Acesso e adesão a medicamentos entre pessoas com diabetes no Brasil: Evidências da PNAUM. Rev. Brasil. Epidem. 2017, 20, 445–459. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; Wu, T.; Hu, X.; Gao, L. Self-care activities among patients with type 2 diabetes mellitus: A cross-sectional study. Int. J. Nurs. Pract. 2021, 27, e12987. [Google Scholar] [CrossRef] [PubMed]
- Richardson, C.R.; Borgeson, J.R.; Van Harrison, R.; Wyckoff, J.A.; Yoo, A.S. Management of Type 2 Diabetes Mellitus; Michigan Medicine University of Michigan: Ann Arbor, MI, USA, 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK579413/ (accessed on 6 December 2022).
- Villegas-Rivera, G.; Román-Pintos, L.M.; Cardona-Muñoz, E.G.; Arias-Carvajal, O.; Rodríguez-Carrizalez, A.D.; Troyo-Sanromán, R.; Pacheco-Moisés, F.P.; Moreno-Ulloa, A.; Miranda-Díaz, A.G. Effects of Ezetimibe/Simvastatin and Rosuvastatin on Oxidative Stress in Diabetic Neuropathy: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Oxid. Med. Cell Longev. 2015, 2015, 756294. [Google Scholar] [CrossRef]
- Iqbal, Z.; Azmi, S.; Yadav, R.; Ferdousi, M.; Kumar, M.; Cuthbertson, D.J.; Lim, J.; Malik, R.A.; Alam, U. Diabetic Peripheral Neuropathy: Epidemiology, Diagnosis, and Pharmacotherapy. Clin. Ther. 2018, 40, 828–849. [Google Scholar] [CrossRef]
- Bariha, P.K.; Tudu, K.M.; Kujur, S.T. Correlation of microalbuminuria with neuropathy in type-II diabetes mellitus patients. Intern. J. Adv. Med. 2018, 5, 1143–1150. [Google Scholar] [CrossRef]
- Gæde, P.; Oellgaard, J.; Carstensen, B.; Rossing, P.; Lund-Andersen, H.; Parving, H.H.; Pedersen, O. Years of life gained by multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: 21 years follow-up on the Steno-2 randomised trial. Diabetologia 2016, 59, 2298–2307. [Google Scholar] [CrossRef]
- Smith, A.G.; Singleton, J.R. Obesity and hyperlipidemia are risk factors for early diabetic neuropathy. J. Diabetes Complicat. 2013, 27, 436–442. [Google Scholar] [CrossRef]
- Sendi, R.A.; Mahrus, A.M.; Saeed, R.M.; Mohammed, M.A.; Al-Dubai, S.A.R. Diabetic peripheral neuropathy among Saudi diabetic patients: A multicenter cross-sectional study at primary health care setting. J. Family Med. Prim. Care. 2020, 9, 197–201. [Google Scholar] [CrossRef]
- Perrin, B.M.; Allen, P.; Gardner, M.J.; Chappell, A.; Phillips, B.; Massey, C.; Skinner, I.; Skinner, T.C. The foot-health of people with diabetes in regional and rural Australia: Baseline results from an observational cohort study. J. Foot Ankle Res. 2019, 12, 56. [Google Scholar] [CrossRef]
- Ristikj-stomnaroska, D.; Risteska-Nejashmikj, V.; Papazova, M. Role of inflammation in the pathogenesis of diabetic peripheral neuropathy. Open Access Maced. J. Med. Sci. 2019, 7, 2267. [Google Scholar] [CrossRef] [PubMed]
- Gaman, M.A.; Epîngeac, M.E.; Diaconu, C.C.; Găman, A.M. Evaluation of oxidative stress levels in obesity and diabetes by the free oxygen radical test and free oxygen radical defence assays and correlations with anthropometric and laboratory parameters. World J. Diabetes 2020, 11, 193. [Google Scholar] [CrossRef] [PubMed]
- Mallet, M.L.; Hadjivassiliou, M.; Sarrigiannis, P.G.; Zis, P. The role of oxidative stress in peripheral neuropathy. J. Mol. Neurosci. 2020, 70, 1009–1017. [Google Scholar] [CrossRef] [PubMed]
- Yao, Q.M.; Wang, B.; An, X.F.; Zhang, J.A.; Ding, L. Testosterone level and risk of type 2 diabetes in men: A systematic review and meta-analysis. Endocr. Connect. 2018, 7, 220–231. [Google Scholar] [CrossRef] [PubMed]
- Velikova, T.V.; Kabakchieva, P.P.; Assyov, Y.S.; Georgiev, T.A. Targeting Inflammatory Cytokines to Improve Type 2 Diabetes Control. Biomed. Res. Int. 2021, 2021, 7297419. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).