Abstract
Ananindeua city, State of Pará, North of Brazil, is a hyperendemic area for tuberculosis (TB), with a cure rate below the recommendation by the Brazilian Ministry of Health. We aimed to describe: (I) the TB incidence coefficient of Ananindeua municipality comparatively against Brazilian data; (II) TB treatment outcomes; (III) to compare the socioeconomic and epidemiological characteristics of abandonment versus cure outcome; and (IV) to evaluate the risk factors associated with TB treatment abandonment in Ananindeua city, from 2017 to 2021. This is a retrospective, descriptive, and cross-sectional epidemiological study which used secondary TB entries. Data were analyzed by linear regression, descriptive statistics, and associations were made using the Chi-square test and G-test, followed by univariate and multivariate logistic regression analyses. Cure rates ranged from 28.7% to 70.1%, abandonment between 7.3% and 11.8%, deaths from the disease ranged from 0% to 1.6%, and drug-resistant tuberculosis (TB-DR) rates had frequencies from 0% to 0.9%. Patient transfer rates to other municipalities were between 4.9% and 12.5%. The multivariate analysis showed that alcohol is almost 2 times more likely to lead an individual to abandon treatment and use of illicit drugs was almost 3 times more likely. Individuals between 20 and 59 years of age were also more likely to abandon treatment almost twice as often. Finally, data obtained in the present report is of great relevance to strengthen epidemiological surveillance and minimize possible discrepancies between the information systems and the reality of public health in high endemicity areas.
1. Introduction
Tuberculosis (TB) is a curable disease in virtually all cases in individuals who have bacilli that are sensitive to anti-tuberculosis (anti-TB) drugs, if treatment is correctly instituted and maintained to eliminate the disease-causing agent [1]. Indeed, TB treatment interruption entails a series of problems for individuals and society, such as death, sequelae, outbreaks and antibiotic-resistant strains emergence, limitations for drug therapy, increase of health systems costs, and permanence of dissemination foci within community environments [2].
In Brazil, TB treatment adherence is associated with several biological and social factors, which may be closely linked to the patient themself, such as health, psychological, cognitive, behavioral, and belief issues; to the disease, such as condition severity; and to the treatment, including access to health services. Despite several advances in TB treatment, adult male individuals from low socioeconomic conditions, black-skinned people, as well as institutionalized patients are at higher risk of the disease [1,3,4,5].
In this context, it is estimated that the TB abandonment rate in Brazil is around 9% of cases, ranging from 2.8% to 15.9% among the states of the federation [6]. In the Northern Brazilian State of Pará, between 2016 and 2019, an average of 11.7% of individuals comprised the treatment abandonment rate [7]. These numbers are above the limit of 5% established as a parameter for this indicator by national and international health agencies [1,6,8,9,10].
Also, in 2021, the city of Ananindeua, State of Pará, had an incidence of 73.8 cases of tuberculosis per 100,000 inhabitants, an average higher than the state and national averages, which were 46.9% and 32.0% per 100,000 inhabitants, respectively [7]. A recent epidemiological study with data from 2018–2020 demonstrated that Ananindeua is a hyperendemic area for TB, harboring a cure rate of 60.31%, which was below the recommendation by the Brazilian Ministry of Health. The quality indicators showed many weaknesses (non-availability of smear microscopy, culture, and rapid molecular test (RMT) tests; and, among others, failure to fill in essential variables for TB surveillance [11]).
Data from the Brazilian Notifiable Diseases Information System (SINAN) has shown that TB incidence in Ananindeua municipality between 2017 and 2021 was between 61.3% and 93.9% per 100,000 inhabitants, and the treatment abandonment rate was between 7.3% and 11.8% of cases closed [12]. Based on that, we aimed to (i) describe the TB incidence coefficient of Ananindeua municipality comparatively against Brazilian data; (ii) to describe the TB treatment outcomes; (iii) to compare the socioeconomic and epidemiological characteristics of abandonment versus cure outcomes; and (iv) to evaluate the risk factors associated to the TB treatment abandonment in Ananindeua municipality from 2017 to 2021.
2. Materials and Methods
2.1. Study Design
This is a retrospective, descriptive, and cross-sectional epidemiological study which used secondary TB entries from the municipality of Ananindeua, State of Pará, Brazil, between January 2017 to December 2021. We followed the guidelines for reporting observational study recommendations based on the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement [13,14].
2.2. Study Scenario
The present study was conducted with data from the city of Ananindeua/PA and data provided by the Health Secretariat of the State of Pará (SESPA). This data is sent by each municipality/city to the state secretariats and, after consolidation, are sent to the Ministry of Health, and added to the National System of Diseases and Notifications (SINAN) of the Department of Informatics of the Unified Health System (DATASUS) of the Ministry of Health of Brazil. Ananindeua has an estimated population of 540,410 inhabitants with a territorial extension of 190,451 km, located in the 6th microregion of the state of Pará, bordering the municipality of Belém, the state capital, and the city of Marituba [15,16].
2.3. Selection Criteria and Data Collection
The data obtained refer to cases reported in the municipality between 2017 and 2021. The outcomes included in the statistical analyzes were treatment abandonment and cure. The other types of outcomes were only described. The total sample of entries with a closure status due to cure and abandonment was 1599 cases. However, some of these entries had no response for some of the variables of interest in the study, and therefore were not considered in the logistic regression analysis. The total number of entries with all fields of interest filled in was 1345 (used in the univariate and multivariate analyses). The data were collected in May 2022. The variables of interest analyzed were sex, age, race, education, participation in a social cash transfer program, type of entry, form, Directly Observed Treatment (DOT), alcoholism, smoking, use of illicit drugs, and HIV coinfection.
The definition of cure is when the patient presents two negative smears, one in any month of follow-up and another at the end of the treatment (5th or 6th month), for longer treatments the last two months are considered. Patients who completed the treatment with no evidence of failure and were discharged based on clinical and radiological criteria, due to the impossibility of performing bacilloscopy exams, were also discharged for cure. Abandonment, on the other hand, is defined as the use of medication for 30 days or more, followed by discontinuation for 30 consecutive days or more [1].
2.4. Statistics Analysis
The incidence coefficient is the parameter that allows comparing the number of new cases of a given disease between cities, states, and countries, as it estimates the number of people affected by a disease per 100,000 inhabitants.
The TB incidence coefficients were calculated using the population projections of the Statistical Yearbook of Pará 2021, the Projection of the population of Brazil released by the Fundação Amazônia de Amparo a Estudos e Pesquisas (FAPESPA) [15], and the Brazilian Institute of Geography and Statistics (IBGE) [16]. Linear regression analysis was performed to determine the tendency for growth or decrease in incidence between the years analyzed, with a significance level of p < 0.05.
Treatment abandonment and cure data were analyzed and are presented according to the absolute and relative frequency and associations were analyzed using the Chi-square test and G-test, with a significance level of p < 0.05. Variables that showed statistical significance were submitted for univariate and multivariate logistic regression analysis to identify risk factors associated with treatment dropout. For the uni- and multivariate regression analyses, only the 1345 entries that contained all the variables were considered. Some variables were categorized and dichotomized. All variables submitted for univariate logistic regression analysis with a p-value < 0.1 were considered eligible for multivariate analysis. The variable year of entry was included in the regression, using the year 2017 as a reference. Statistical tests were run using Bioestat software version 5.4 and Mnitab.
2.5. Ethics
Despite being a secondary data analysis database, with no direct contact with the researched individuals, the database contains personal information and therefore requires compliance with the ethical guidelines, established by law, and approved by the Research Ethics Committee of Evandro Chagas Research Institute, under standards 4.172.679 and CAEE 20821119.4.0000.0019.
3. Results
3.1. Number of New Reported Cases of Tuberculosis and Incidence Coefficient in Ananindeua, State of Pará and Brazil
The incidence of tuberculosis in Ananindeua has shown an increase, especially in 2019, which had the highest number of cases among the years studied. In 2021 there was a decrease in cases compared to the previous year, however, the number remains higher than in 2017 and 2018. The same is observed among the numbers of new cases reported in the state of Pará and in Brazil, with a high number of cases in 2019, followed by a slight decrease in the following years (Table 1).

Table 1.
Number of new TB cases notified in the municipality of Ananindeua, state of Pará and Brazil from 2017 to 2021.
The TB incidence in Ananindeua demonstrated rates higher than the state and national incidences throughout the period of this study, with a tendency for the trend to increase. The linear regression model adopted points to an increase of 2.99 cases per year per 100,000 inhabitants, however the coefficient of determination of the regression function shows that this trend was not representative (R2 = 0.1643), and the value of the test was not significant (p > 0.05). The TB incidence rate in Pará maintained a slight increase compared to that of Brazil, which showed a decrease. Both Ananindeua and the state of Pará and Brazil had the highest TB incidence rates in 2019 compared to other years, due to the increase in the number of cases for this year, as shown (Table 1, Figure 1).
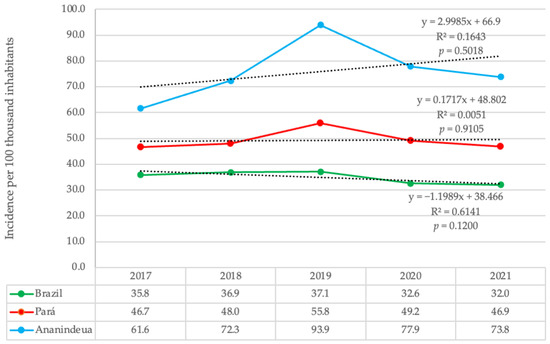
Figure 1.
Trend of TB incidence coefficient in the Municipality of Ananindeua, state of Pará and Brazil from 2017 to 2021. Trend line represented by the dashed line.
3.2. Tuberculosis Treatment Outcomes Reported in Ananindeua
Between the years 2017 and 2021, 2339 entries were found, of which 431 (18.4%) did not have the closure status field filled in. Of this number, 1599 entries were selected, of which 1369 (58.5%) were of people who were discharged from TB treatment having been cured and 230 (9.8%) of people who abandoned treatment. These are the two variables that make up the comparison groups of the study. The remaining cases refer to the other scenarios for termination, as described in Table 2.

Table 2.
Closure situation of tuberculosis cases in the municipality of Ananindeua-Pa from 2017 to 2021 (n = 2339).
Cure rates were between 28.7% and 70.1%, abandonment rates were between 7.3% and 11.8%, deaths from the disease ranged from 0% to 1.6% of cases, and rates of drug-induced tuberculosis resistance (DR-TB) presented frequencies from 0% to 0.9%, between the analyzed years. Transfer rates of patients to other municipalities were between 4.9% and 12.5%.
3.3. Socioeconomic Characteristics of Abandonment Cases and Cure Outcome
Cases reported as treatment abandonment or cure of the disease, the outcomes of interest in the study, totaled 1599 entries between 2017 and 2021. In the comparison between the two groups (abandonment and cure), there was a significant difference for gender and age group. Males showed the highest frequency, with 154 (67%) among those who abandoned treatment (p = 0.0395). The adult age group, 20 to 59 years old, was also more present among dropouts, with 194 (84.3%, p = 0.0062).
The predominant race in both groups was brown/pardo, with 174 (75.7%) of those who abandoned treatment and 1055 (77.1%) of those who were cured. As for education, individuals who had incomplete elementary school education (n = 95, 41.3%) were more associated with the abandonment outcome, while complete elementary school education (n = 44, 19.1%) and complete high school education (n = 339, 24.8%) were more associated with individuals who achieved a cure (p < 0.0001). The schooling variable was one of the most unfilled fields in the entries, with a percentage of 23.1% of cases without information; for this reason, we chose to exclude this variable from the logistic regression analyses (Table 3).

Table 3.
Socioeconomic characteristics of the cases with the Treatment abandonment outcome and Tuberculosis cure in Ananindeua from 2017 to 2021.
3.4. Epidemiological Characteristics of Abandonment Cases and Cure Outcome
As for the type of admission, a new case related to the cure group with 1203 (87.9%, p < 0.0001) individuals and re-entry after abandonment was statistically significant among the abandonment group 186 (80.9%, p < 0.0001). The disease form showed no significant difference between the groups (p > 0.05). Directly Observed Treatment (DOT) also showed no significant difference between the groups and was not performed in most cases (N = 142, 61.7%).
Alcoholism, smoking, and the use of illicit drugs were associated with cases of abandonment, respectively. HIV negative serology was significant for the cure group with 630 cases (46.0%, p < 0.0001). It is noteworthy that in 47.3% of cases, almost half of the total sample, HIV serology was not performed, making it impossible to measure. For this reason, it was also decided to exclude it from the logistic rlegression analysis, since removing the entries without this information would substantially compromise the size of the study population (n = 757) (Table 4).

Table 4.
Epidemiological characteristics of the cases with the Treatment abandonment outcome and Tuberculosis cure in Ananindeua from 2017 to 2021.
3.5. Risk Factors Associated with Treatment Abandonment
For the logistic regression analysis, only the entries that had all the variables filled out and that were significant in the Chi-square or G-test were considered. Of the 1599 entries, only 1345 were filled out. We chose to include the variable year, taking the year 2017 as a reference.
The results of the univariate analysis showed that age group (OR: 1.57; 95% CI: 1.04–2.38; p: 0.033), type of entry (OR: 0.49; 95% CI: 0.31–0.78; p: 0.002), alcoholism (OR: 2.72; 95% CI: 1.68–4.40; p < 0.001), smoking (OR: 3.33; 95% CI: 1.73–6.41; p < 0.001), drug use (OR: 4.23; 95% CI: 2.35–7.60; p < 0.001), and the year 2021 (OR: 1.47; 95% CI: 1.03–2.09; p: 0.032) were significantly associated with treatment dropout. In addition, multivariate analysis showed that the age group (OR: 1.55; 95% CI: 1.03–2.32; p: 0.035), alcoholism (OR: 1.74; 95% CI: 1.11–2.72; p: 0.016), illicit drug use (OR: 2.64; 95% CI 1.56–4.46; p < 0.001), and the year 2021 (OR: 1.45; 95% CI: 1.01–2.08; p: 0.043) are predictors associated with treatment abandonment (Table 5).

Table 5.
Results of the logistic analysis of risk factors for abandoning Tuberculosis treatment in Ananindeua from 2017 to 2021 (n = 1345).
4. Discussion
The city of Ananindeua has higher incidence rates than the state of Pará and Brazil and is therefore considered a hyperendemic region for TB [11]. The incidence of cases in the municipality of Ananindeua has followed the state and national trends that saw an increase in cases from 2017 to 2019 and a discrete decrease in the years 2020 and 2021. The epidemiological scenario brought on by the COVID-19 pandemic and the measures to contain virus transmission influenced the detection of new cases, causing probable underreporting, and interfered with the continuity of ongoing treatments [17,18].
The study shows that in all the years analyzed, the cure rates for TB each year remained below 85%, the minimum recommended by the Brazilian Ministry of Health. The World Health Organization (WHO) recommends at least a 90% cure of identified cases [8,9]. Dropout rates were above 5%, the maximum recommended by the Ministry of Health in Brazil [1,10].
The municipalities of the state of Pará along with municipalities from other states were grouped in a cluster formed by 163 municipalities at high risk for treatment abandonment in the years 2012 to 2018, in a study on the spatial-temporal distribution of TB treatment abandonment in Brazil. In these municipalities, the average proportion of abandonment was 16.85% [6].
Although 2021 had only a 28.1% cure rate, we emphasize that this number may represent the incompleteness of the data due to the delay in updating the information passed on to the surveillance system. The information is passed on by each notifying unit to the municipal departments and later to the state departments until it reaches the Ministry of Health, where the consolidated information is published and becomes public domain. This data is updated as new information is passed on.
Surveillance data from the Tuberculosis Special Treatments Information System (SITE-TB) that make up another database for monitoring drug-resistant tuberculosis (DR-TB) cases, shows a difference between the numbers of DR-TB presented. According to the system, 12 cases of DR-TB were reported in 2017, 14 cases in 2018, 8 cases in 2019, 5 cases in 2020, and 10 cases in 2021 [19].
The SITE-TB is a complementary system to the Information System for Notifiable Diseases (SINAN), and the main tool for surveillance and management of TB cases with indication of special schemes. This inconsistency between data shows a communication gap between the systems since every confirmed case of TB should be notified in SINAN, regardless of the type of treatment to be administered [20].
The cases of transfer of patients to other municipalities totaled an average of 8.5% between the years analyzed. According to the National Plan for the End of Tuberculosis as a Public Health Problem in Brazil, this indicator, together with the cases in which the outcome of the treatment was not informed, compromises the actions to combat the disease. Since there is no information, the analysis of cure and abandonment indicators are impaired [10].
Other important variables also neglected were education, which presented a total of 23.1% of the total cases of cure and abandonment and was not filled out information, and the performance of HIV serology throughout treatment, which was not done in almost half (47.3%) of the cases of cure and abandonment, going against the advice of the Brazilian Ministry of Health’s recommendation to offer HIV testing to all TB cases [1]. TB/HIV coinfection is already well documented in the literature, with people living with HIV who are not on treatment having a higher risk for developing the disease, including its extrapulmonary form, and a higher risk of death, if bought to people not living with the virus [21,22,23].
Regarding socioeconomic characteristics, our results show an association between males and the group with the abandonment outcome, however, in the regression analysis, there was no significant difference. This may be due to factors such as alcoholism and the use of illicit drugs, which in our study were shown to be risk factors for abandonment, and are behaviors more observed among males [24].
Different studies point to an association between treatment abandonment and certain factors. Sociodemographic factors, such as the use of licit or illicit drugs, age, sex, education, income, housing, access to information and health services and stigmas, clinical factors such as co-infection with the HIV, history of abandonment, extrapulmonary TB and comorbidities, and treatment-related factors, such as the stage of treatment (usually at the beginning), adverse drug effects, and improvement in disease symptoms are some of the commonly reported factors [3,25,26,27].
Our results show that individuals considered to be alcoholics are almost 2 times more likely to abandon treatment, while those who use illicit drugs are almost 3 times more likely. In Belém/PA, a survey of patients undergoing retreatment for the disease observed that the use of illicit drugs and alcoholic beverages were among the most cited reasons why patients decided to discontinue treatment [27].
In the state of Ceará, it was observed that alcoholism increased the chances of abandoning treatment by 50% [5]. Another study carried out, this time in the capital of Ceará, also showed that in addition to alcoholism, the use of illicit drugs significantly increased the chances of abandonment [3].
In a systematic review, alcohol use was associated with a 1.5- to 2-fold increase in the odds of poor treatment outcomes in drug-sensitive TB and DR-TB, relative to minimal or no alcohol exposure. Alcohol and TB treatment were associated with higher odds of poor treatment outcomes, i.e., death, treatment failure, and loss to follow-up, in studies of drug-sensitive (OR 1.99, 95% CI 1.57–2.51) and multidrug-resistant TB patients (OR 2.00, 95% CI 1.73–2.32) [28].
The age group which presented with an increased risk of treatment abandonment, with 1.5-fold higher chance were those aged between 20 and 59 years. Our criteria for determining this age group were based on the population considered economically active. These results are concordant with another study that identified a higher risk of abandonment among younger adults aged between 20 and 40 years [3].
As for the analysis of the year, the year 2021 presented odds of 1.45. We consider that this finding should be analyzed more carefully over time, since the data for the year 2021 were not yet complete and many entries were not yet closed, due to the delay between the closure of the case and the arrival of information to the surveillance agencies. It is worth remembering that the minimum time for the treatment of tuberculosis is six months, at best, while the time for the individual to be considered in the treatment give-up group is 30 days after the date of the last dispensation of the drug.
For this reason, there may be a difference in the proportion of cases of cure and treatment abandonment that does not reflect the totality of cases in the year, if we analyze each year separately, so a data analysis is necessary when this period has the most entries with status closed.
In this study, the type of entry and smoking was associated with treatment abandonment in the univariate regression analysis, but it was not significant in the multivariate analysis. Factors such as participation in a cash transfer program, form of the disease and DOT were not statistically significant. While ethnicity, the type of entry and smoking were associated in the Chi-square tests, the G-test or univariate regression analysis, however, did not show significance in the final regression model. This may be because many exposure factors are related to each other but are not always the direct cause of a problem.
Low education commonly associated with cases of tuberculosis, was not included in the logistic regression analyses because many entries did not inform this data. However, low education is related to alcohol abuse [29]. The absence of many responses to the HIV serology status also resulted in the non-inclusion of this variable in the regression model. This lack of information can compromise the findings and generate results which differ from reality. For this reason, it is important from the point of view to strengthen surveillance systems so that the information is properly filled out, because it is from these findings that health policies are formulated [30].
The problem of incomplete information in the entries was identified in research on the evaluation of TB surveillance data in Brazil and points to the need for the proper completion of surveillance instruments beyond a bureaucratic issue, and to allow an effective epidemiological analysis of TB in the country [31]. Information systems are essential for the epidemiological surveillance of any disease, because through them the information-decision-action process is triggered [32], and the quality of the data is important for the evaluation of services and decision-making in TB control actions [1].
The absence of information about some important variables for tuberculosis monitoring and its non-use in the logistic regression model can compromise the quality of the analysis. We chose to perform the model without considering such variables since excluding the number of entries without this information would considerably reduce the size of our sample and for this reason would be a limitation of our study. We suggest that further studies be done in order to consider these variables.
We also recommend that better attention be given to people at higher risk of abandoning TB treatment in Ananindeua, i.e., individuals with a history of alcoholism and illicit drug use. These cases should be prioritized within the local tuberculosis control program, including priority for the performance of the DOT, along with other priority groups such as homeless people, deprived of freedom and diabetics, as recommended by the Brazilian Ministry of Health [1]. For this, we also recommend the adoption of risk stratification for treatment abandonment and shared care with other services that meet the specific needs of each priority group, such as the stratification proposed by Navarro and collaborators that decreased by fifteen times the chances of abandonment of tuberculosis treatment [2].
5. Conclusions
The incidence of TB in Ananindeua showed a similar observation like that observed in the state of Pará and Brazil, although in higher numbers, with 2019 being the one with the highest number of cases and the highest coefficient. Cure outcomes are below the recommended minimum and the treatment abandonment rate is higher than recommended. In this study, alcoholism was almost 2 times more likely to lead the individual to abandon TB treatment and the use of illicit drugs was almost 3 times more likely. Individuals between 20 and 59 years of age were also more likely to abandon treatment almost twice as often. Factors such as ethnicity, and smoking were associated with risk factors for abandonment, but were not risk factors for the abandonment outcome according to the multivariate analysis. Participation in cash transfer program, disease form, and DOT were not statistically associated with dropout cases. It was not possible to estimate the impact of education level and HIV serology as risk factors for treatment abandonment in the proposed statistical model, given the number of reports in which these variables were ignored.
This study was conducted with secondary data provided by the state epidemiological surveillance, with lack of information on important indicators in some of the entries. For this reason, it is essential to strengthen the epidemiological surveillance so that the data from the entries are correctly filled out and minimize possible discrepancies between the information systems and the reality of public health and thus enable more accurate studies.
Author Contributions
Conceptualization, G.F.C., J.C.D.G. and K.V.B.L.; validation, G.F.C., J.C.D.G., A.L.d.S.F., J.A.A.A. and K.V.B.L.; formal analysis, G.F.C., J.C.D.G., W.M., A.L.d.S.F. and J.A.A.A.; investigation, G.F.C., J.C.D.G., W.M., A.L.d.S.F. and J.A.A.A.; resources, L.N.G.C.L. and K.V.B.L.; writing—original draft preparation, G.F.C., Y.C.R., L.N.G.C.L., E.C.C. and K.V.B.L.; writing—review and editing, G.F.C., Y.C.R., L.N.G.C.L., E.C.C. and K.V.B.L.; supervision, E.C.C., L.N.G.C.L. and K.V.B.L.; project administration, K.V.B.L.; funding acquisition, L.N.G.C.L. and K.V.B.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by funding from Evandro Chagas Institute (IEC), Secretariat for Science, Technology, Innovation and Strategic Health Inputs (SCTIE), Brazilian Ministry of Health (MS). Yan Corrêa Rodrigues scholarship is funded by PDPG—Pós-Doutorado Estratégico (PDPG-POSDOC), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES/Edital 16/2022).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Research Ethics Committee of Evandro Chagas Research Institute under opinion number 4.172.679 and CAEE 20821119.4.0000.0019 on 24 July 2020.
Informed Consent Statement
Patient consent was waived due to because it is analysis of secondary data in a database, without contact with the subjects or identification of these.
Data Availability Statement
All relevant data is presented within the manuscript.
Conflicts of Interest
The authors declare no conflict of interest regarding the publication of the present study, and the funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Brasil, Ministério da Saúde; Secretaria de Vigilância em Saúde; Departamento de Vigilância das Doenças Transmissíveis. Manual de Recomendações para o Controle da Tuberculose no Brasil; Ministério da Saúde: Brasília, Brazil, 2019; pp. 1–364. Available online: http://bvsms.saude.gov.br/bvs/publicacoes/manual_recomendacoes_controle_tuberculose_brasil_2_ed.pdf (accessed on 22 May 2022).
- De Navarro, P.D.; Haddad, J.P.A.; Rabelo, J.V.C.; Silva, C.H.D.L.E.; de Almeida, I.N.; Carvalho, W.D.S.; de Miranda, S.S. The impact of the stratification by degree of clinical severity and abandonment risk of tuberculosis treatment. J. Bras. Pneumol. 2021, 47, e20210018. [Google Scholar] [CrossRef] [PubMed]
- Harling, G.; Neto, A.S.L.; Sousa, G.S.; Machado, M.M.T.; Castro, M.C. Determinants of tuberculosis transmission and treatment abandonment in Fortaleza, Brazil. BMC Public Health 2017, 17, 508. [Google Scholar] [CrossRef] [PubMed]
- Soares, M.L.M.; Amaral, N.A.C.D.; Zacarias, A.C.P.; Ribeiro, L.K.D.N.P. Aspectos sociodemográficos e clínico-epidemiológicos do abandono do tratamento de tuberculose em Pernambuco, Brasil, 2001–2014. Epidemiol. Serviços Saúde 2017, 26, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Sousa, G.J.B.; Maranhão, T.A.; Leitão, T.D.M.J.S.; de Souza, J.T.; Moreira, T.M.M.; Pereira, M.L.D. Prevalência e fatores associados ao abandono do tratamento da tuberculose. Rev. Esc. Enferm. USP 2021, 55, e03767. [Google Scholar] [CrossRef] [PubMed]
- Soeiro, V.M.D.S.; Caldas, A.D.J.M.; Ferreira, T.F. Abandono do tratamento da tuberculose no Brasil, 2012–2018: Tendência e distribuição espaço-temporal. Cien. Saude Colet. 2022, 27, 825–836. [Google Scholar] [CrossRef] [PubMed]
- Pará, Governo do Estado do Pará; Secretaria de Estado de Saúde Pública; Sistema Único de Saúde; Diretoria de Vigilância em Saúde; Departamento de Controle de Doenças Transmissíveis. Coordenação do Programa de Controle da Tuberculose. II Boletim Epidemiológico da Tuberculose. 2022. Available online: http://www.saude.pa.gov.br/a-secretaria/diretorias/dvs/tuberculose/be-tuberculose/ (accessed on 13 June 2022).
- World Health Organization (WHO). Global Strategy and Targets for Tuberculosis Prevention, Care and Control after 2015—Report by the Secretariat. 2013. Available online: https://apps.who.int/iris/handle/10665/172828 (accessed on 14 May 2021).
- World Health Organization (WHO). The End TB Strategy. 2015. Available online: https://www.who.int/publications/i/item/WHO-HTM-TB-2015.19 (accessed on 14 May 2021).
- Brasil, Ministério da Saúde; Secretaria de Vigilância em Saúde; Departamento de Vigilância das Doenças Transmissíveis. Brasil Livre da Tuberculose: Plano Nacional pelo Fim da Tuberculose como Problema de Saúde Pública; Ministério da Saúde: Brasília, Brazil, 2017; pp. 1–52. Available online: https://www.saude.gov.br/images/pdf/2017/julho/05/af-miolo-plano-nac-tuberculose-29jun17-grafica.pdf (accessed on 27 June 2021).
- Garcez, J.C.D.; Sardinha, D.M.; Conceição, E.C.; Costa, G.F.; Sousa, I.F.R.; Mesquita, C.R.; Carmo, W.C.D.; Rodrigues, Y.C.; Lima, L.N.G.C.; Lima, K.V.B. Surveillance Quality Indicators Highlight the Need for Improving Tuberculosis Diagnostics and Monitoring in a Hyperendemic Area of the Brazilian Amazon Region. Trop. Med. Infect. Dis. 2022, 7, 165. [Google Scholar] [CrossRef] [PubMed]
- Brasil, Ministério da Saúde. Departamento de Informática do Sistema Único de Saúde. Sistema de Informação de Agravos de Notificação—Sinan. Casos de Tuberculose—Desde 2001. 2022. Available online: https://datasus.saude.gov.br/acesso-a-informacao/casos-de-tuberculose-desde-2001-sinan/ (accessed on 27 November 2022).
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef] [PubMed]
- Malta, M.; Cardoso, L.O.; Bastos, F.I.; Magnanini, M.M.F.; da Silva, C.M.F.P. Iniciativa STROBE: Subsídios para a comunicação de estudos observacionais. Rev. Saude Publica 2010, 44, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Fundação Amazônia de Amparo a Estudos e Pesquisa (FAPESPA). População Total e Estimativas Populacionais, Pará e municipios—2017 a 2021, Anuário Estatístico do Pará 2021. 2021. Available online: https://www.fapespa.pa.gov.br/sistemas/anuario2021/tabelas/demografia/tab-1.1-populacao-total-e-estimativas-populacionais-2017-a-2021.htm (accessed on 6 July 2022).
- Instituto Brasileiro de Geografia e Estatística (IBGE). Diretoria de Pesquisas. Coordenação de População e Indicadores Sociais. Gerência de Estudos e Análises da Dinâmica Demográfica. Projeção da população do Brasil e Unidades da Federação por sexo e idade para o período 2010–2060, 6 April 2020. Available online: https://www.ibge.gov.br/estatisticas/sociais/populacao/9109-projecao-da-populacao.html?=&t=resultados (accessed on 6 July 2022).
- Jain, V.K.; Iyengar, K.P.; Samy, D.A.; Vaishya, R. Tuberculosis in the era of COVID-19 in India. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1439–1443. [Google Scholar] [CrossRef]
- Maia1, C.M.F.; Martelli, D.R.B.; da Silveira, D.M.M.L.; Oliveira, E.A.; Júnior, H.M. Tuberculosis in Brazil: The impact of the COVID-19 pandemic. J. Bras. Pneumol. 2022, 48, e20220082. [Google Scholar] [CrossRef] [PubMed]
- Brasil, Ministério da Saúde; Departamento de Doenças, Condições Crônicas e Infecções Sexualmente Transmissíveis. Sistema de informação de tratamento especiais da tuberculose (Site-TB): Casos confirmados TB-DR, 1 November 2022. Available online: http://sitetb.saude.gov.br (accessed on 19 November 2022).
- Brasil, Ministério da Saúde; Departamento de Doenças de Condições Crônicas e Infecções Sexualmente Transmissíveis. Sistema de Informação de Tratamento Especiais da Tuberculose (Site-TB), 4 May 2022. Available online: https://www.gov.br/aids/pt-br/indicadores-epidemiologicos/sistemas-de-informacao/sitetb (accessed on 19 November 2022).
- Dorman, S.E. Diagnosis of HIV-associated tuberculosis. Curr. Opin. HIV AIDS 2018, 13, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Meintjes, G.; Brust, J.C.M.; Nuttall, J.; Maartens, G. Management of active tuberculosis in adults with HIV. Lancet HIV 2019, 6, e463–e474. [Google Scholar] [CrossRef] [PubMed]
- Natarajan, A.; Beena, P.; Devnikar, A.V.; Mali, S. A systemic review on tuberculosis. Indian J. Tuberc. 2020, 67, 295–311. [Google Scholar] [CrossRef] [PubMed]
- Scholze, A.R. Análise Espacial e Temporal da Tuberculose Entre Pessoas em uso Crônico de Álcool, Tabaco e ou Drogas Ilícitas no Estado do Paraná. Ph.D. Thesis, Universidade de São Paulo, Ribeirão Preto, Brazil, 2021. Available online: https://www.teses.usp.br/teses/disponiveis/22/22133/tde-22032022-151416/publico/ALESSANDROROLIMSCHOLZE.pdf (accessed on 10 July 2022).
- Bezerra, W.D.S.P.; Lemos, E.F.; Prado, T.N.D.; Kayano, L.T.; de Souza, S.Z.; Chaves, C.E.V.; Paniago, A.M.M.; de Souza, A.S.; de Oliveira, S.M.D.V.L. Risk Stratification and Factors Associated with Abandonment of Tuberculosis Treatment in a Secondary Referral Unit. Patient Prefer. Adherence 2020, 14, 2389–2397. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, M.R.L.; Bonfim, R.O.; Siqueira, T.C.; Orfão, N.H. Abandono do tratamento da tuberculose: Uma revisão integrativa. Rev. Enferm. Contemp. 2018, 7, 63–71. [Google Scholar] [CrossRef]
- Sá, A.M.M.; de Aquino Santiago, L.; Santos, N.V.; Monteiro, N.P.; Pinto, P.H.A.; de Lima, A.M.; Iwasaka-Neder, P.L. Reasons for treatment abandonment among tuberculosis patients. Rev. Soc. Bras. Clin. Med. 2017, 15, 155–160. Available online: https://www.sbcm.org.br/revistas/RBCM/RBCM-2017-03.pdf#page=12 (accessed on 9 July 2022).
- Ragan, E.J.; Kleinman, M.B.; Sweigart, B.; Gnatienko, N.; Parry, C.D.; Horsburgh, C.R.; LaValley, M.P.; Myers, B.; Jacobson, K.R. The impact of alcohol use on tuberculosis treatment outcomes: A systematic review and meta-analysis. Int. J. Tuberc. Lung Dis. 2020, 24, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, L.E.S.; Helman, B.; Silva, D.C.D.L.E.; de Aquino, C.; de Freitas, P.C.; Santos, R.D.O.; Brito, V.C.D.A.; Garcia, L.P.; Sardinha, L.M.V. Prevalência de consumo abusivo de bebidas alcoólicas na população adulta brasileira: Pesquisa Nacional de Saúde 2013 e 2019. Epidemiologia Serviços Saúde 2022, 31, 1–15. [Google Scholar] [CrossRef]
- Dos Santos, N.P.; Lírio, M.; Passos, L.A.R.; Dias, J.P.; Kritski, A.L.; Galvão-Castro, B.; Grassi, M.F.R. Completeness of tuberculosis reporting forms in five Brazilian capitals with a high incidence of the disease. J. Bras. Pneumol. 2013, 39, 221–225. [Google Scholar] [CrossRef]
- Da Silva, G.D.M.; Bartholomay, P.; Cruz, O.G.; García, L.P. Avaliação da qualidade dos dados, oportunidade e aceitabilidade da vigilância da tuberculose nas microrregiões do Brasil. Cien. Saude Colet. 2017, 22, 3307–3319. [Google Scholar] [CrossRef]
- Brasil, Ministério da Saúde; Secretaria de Vigilância em Saúde; Departamento de Vigilância Epidemiológica. Guia de Vigilância Epidemiológica, 7th ed.; Ministério da Saúde: Brasília, Brazil, 2009; pp. 1–816. Available online: https://bvsms.saude.gov.br/bvs/publicacoes/guia_vigilancia_epidemiologica_7ed.pdf (accessed on 25 September 2022).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).