Abstract
Women frequently suffer from urinary incontinence due to atrophic changes in the urogenital tract. Recommended conservative treatment includes evaluation of pelvic-floor strength and the functional use of pelvic-floor-muscle (PFM) training. Following the PRISMA 2020 guidelines, a search was conducted in the electronic databases PubMed, Web of Science, and Scopus for articles with at least one group performing PFM exercises in post-menopausal women with urinary incontinence. Eight articles were included, and each study had at least one group of PFM exercise-based intervention alone or combined. The volume or duration, frequency, and number of sessions were heterogeneous. All the studies reported significant differences in favor of PFM exercise in strength, quality of life, and/or severity of urinary incontinence. PFM exercise is a highly recommended intervention to treat urinary incontinence in postmenopausal women. However, more research is needed to establish specific factors such as dose–response relationships and to standardize methods for measuring effects.
1. Introduction
Urinary incontinence was defined in 2003 as the complaint of any involuntary leakage of urine [1]. This condition is associated with risk factors such as pelvic-floor-muscle (PFM) deficits, pelvic surgery, prolapse, urinary-tract infections, obesity, smoking, constipation, diabetes mellitus, high-impact physical exercise, being female, increasing age, parity, and menopause [2,3].
Postmenopausal women frequently suffer from urinary incontinence as a result of increased intra-abdominal pressure, such as sneezing, coughing, jumping, laughing, or sexual relations [4]. Estrogen deficiency at this stage of the life cycle generates atrophic changes in the urogenital tract and vaginal and periurethral tissues [5], and has been associated with involuntary urine loss due to stress and increased urinary urgency and frequency [6]. Despite this association, there has been no evidence of improvement with hormonal management [7].
Among the options based on non-invasive and non-pharmacological intervention are therapeutic targeted exercise such as PFM training, which focuses on improving the function, muscle tone, strength, coordination, and endurance of the pelvic-floor musculature [8]. Other active treatment techniques are Kegel exercises, which focus on enhancing the strength and improving the function of the PFM [9], or pelvic-floor contraction exercises coupled with coactivation of the trunk-stabilizing muscles [10].
Conservative treatment, recommended as first line by the International Continence Society, includes assessment of pelvic-floor strength and functional use of PFM training [11]. The success of this intervention lies in the achievement of increased contraction and holding strength, coordination, speed, and endurance of the pelvic-floor musculature to keep the bladder elevated during demanding activities. Likewise, PFM training allows adequate urethral closure pressure to be maintained and supports and stabilizes the pelvic organs [12]. For postmenopausal women who receive regular supervision, it has been observed that they are more likely to comply and report a decrease in urinary incontinence than women who perform PFM training with little or no supervision [13].
Other systematic reviews related to exercise in this population can be found in the literature; however, they focused on determining the effects of exercise on quality of life or on comparing different interventions with this type of training on multiple variables associated with the pathology [14,15]. Therefore, the aim of the present review was to perform a systematic review of randomized controlled clinical trials that evaluated the effect of targeted PFM exercise in postmenopausal women for the treatment of urinary incontinence.
2. Materials and Methods
This systematic review was performed following the guidelines of the PRISMA statement (Preferred Reporting Items for Systematic reviews and Meta-Analysis) [16]. The pre-specified protocol was registered in PROSPERO under the code CRD42022373488.
2.1. Eligibility Criteria
Articles were selected according to the following criteria: clinical trial, randomized control trial with objective measures of urinary incontinence before and after an exercise-based intervention in postmenopausal women. Regarding the intervention, articles in which the PFM training method was used for the treatment of urinary incontinence during the postmenopausal period were included.
2.2. Information Sources
Data collection took place from October to November 2022 by consulting the following databases: Pubmed (MEDLINE), Scopus, and Web of Science.
2.3. Search Strategy
The keywords used were (“postmenopausal period” OR “postmenopausal” OR “postmenopausal women”) AND (“diurnal enuresis” OR “enuresis” OR “daytime wetting” OR “daytime urinary incontinence” OR “urinary incontinence”) AND (“pelvic floor muscle training” OR “pelvic floor exercises” OR “pelvic floor muscle exercise” OR “pelvic floor muscles”) AND (“severity” OR “frequency of urination” OR “urinary frequency” OR “urination behaviors” OR “frequency of micturition” OR “micturition” OR “quality of life” OR “mental health” OR “depression” OR “sexual activity”).
2.4. Selection Process
The search results were exported to the Rayyan QCRI application (https://rayyan.qcri.org/welcome accessed on 15 November 2021) [17]. Two blinded independent researchers conducted the literature review and decided on the inclusion of the articles separately. The pre-selection of the studies was performed based on reading of the title and abstract. Subsequently, the pre-selected articles were read in full text and the articles that met the criteria were included. In case of discrepancies, a third author resolved them.
2.5. Data-Collection Process
The main variable of this review was the objective measurement of urinary incontinence, mainly in terms of strength, quality of life, and severity of the incontinence. We included information on the authors, the year of publication, the country of publication, and the country in which the study was conducted; likewise, we collected the type, duration or volume, frequency, number of sessions, and number of weeks of the interventions performed, as well as the follow-up time and the results obtained in each measurement.
2.6. Assessment of Methodological Quality
The methodological quality of the articles included in this review was assessed using the PEDro scale [18], with a maximum score of 10 points, as the first item (“eligibility criteria”) is not used in the final score calculation. Each item can be answered as either “Yes” (1 point) or “No” (0 points) [19]. A score between 0 and 3 was considered “Poor” quality, 4–5 “Fair,” 6–8 “Good,” and >9 “Excellent” [20]. The scores were consulted in the PEDro database; when scores were not found, two authors evaluated the methodological quality of articles, and in situations where a discrepancy was generated, it was resolved by a third author.
3. Results
3.1. Selection of the Studies
The database search resulted in a total of 91 articles, which were revised to identify duplicates, discarding 35 and leaving 56 unique articles. After a title-and-abstract screen, 11 potentially eligible articles remained. Finally, only eight articles [21,22,23,24,25,26,27,28] met the eligibility criteria established for this review (Figure 1).
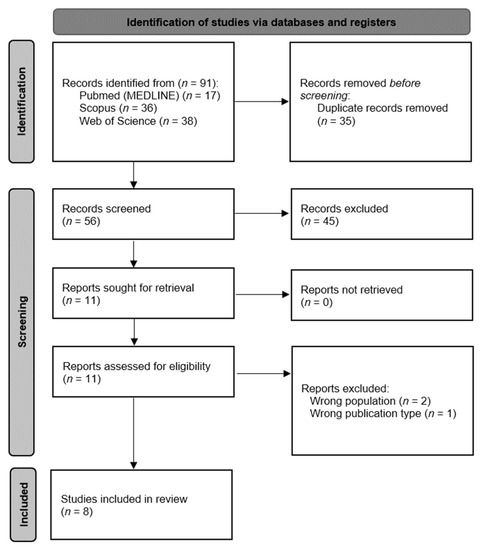
Figure 1.
Flow diagram of the study-selection process.
3.2. Methodological Quality
Methodological quality was assessed using the PEDro scale. The scores of seven of the articles [21,22,23,24,25,26,27] were obtained from the PEDro website, whereas the remaining article [28] was calculated manually. Seven of the articles [22,23,24,25,26,27,28] included in this review presented ”Good” methodological quality, and only one [21] had “Fair” methodological quality (Table 1).

Table 1.
Methodological quality of the articles included.
3.3. Characteristics of the Studies
The articles included in this systematic review were all randomized controlled clinical trials published in Switzerland [21,25], the United Kingdom [22,23,24], the United States [26,27], and Poland [28]; however, the studies were conducted in countries other than those in which they were published, such as Turkey [21], Australia [22], Brazil [23,24,25,27], Canada [26], and Egypt [28].
A total of 376 postmenopausal women aged 60.31 ± 6.73 years participated in the included studies. Out of the overall population, 196 postmenopausal women were part of the groups that received PFM exercise-based treatments (Table 2).

Table 2.
Characteristics of the included studies.
3.4. Study Intervention
Every study [21,22,23,24,25,26,27,28] included at least one group with a PFM exercise-based intervention. Six studies [21,22,23,24,25,27] performed PFM exercise-based interventions only, whereas Sran et al. [26] combined it with physiotherapy and Ghoniem et al. [28] with Pilates.
Although all the interventions included PFM exercises, the prescription of the volume or duration, frequency, and number of sessions was heterogeneous. Regarding frequency, one study proposed an intervention program with only one intervention per week [26], five studies proposed two sessions per week [23,24,25,27,28], one study maintained three sessions per day but did not specify the number of days per week [21], and one study did not specify either sessions per day or per week. The number of sessions ranged from 8 [27] to 12 [23,24,26] to 24 [25,28]; however, two studies did not specify the number of sessions [21,22].
Concerning the volume or duration of the exercises, four of the studies [23,24,26,27] dosed the exercises based on time, with sessions lasting from 20 min to 60 min. On the other hand, three studies [21,25,28] dosed the exercise based on the number of contractions and positions used, ranging from 10 contractions and one single position [21], to four positions and 10 contractions in each [25], and to positions with up to 52 contractions after the adaptation period [28].
3.5. Study Results
All the articles found a significant difference in favor of the PFM-exercise intervention in at least one variable related to the strength of this musculature, severity of incontinence, and/or quality of life [21,22,23,24,25,26,27,28]. In addition, when PFM exercises were applied in combination with other interventions, no significant differences were observed with the groups that did PFM exercises alone [28].
Similarly, to the interventions, the outcomes measured remained heterogeneous. Statistically significant changes (p < 0.05) were observed in the 1 h pad test [21,26], perineometry [21], PFM strength with digital palpation [21], incontinence frequency [21], stress test [22], urinary leakage [23,24], PFM pressure [23,24], incontinence impact [23,24], gravity measures [23,24], urinary-incontinence severity [25], number of leakage episodes [26], Urogenital Distress Inventory total score [26], precontraction [27], initial electromyographic baseline [27], duration of endurance contraction [27], maximum voluntary contraction [27], International Consultation Incontinence Questionnaire—Short Form [27], squeeze vaginal pressure [28], and the Urinary Incontinence Scale [28].
4. Discussion
The present systematic review aimed to determine the effects of PFM exercises in the treatment of urinary incontinence in postmenopausal women. The review included eight randomized controlled trials that met the selection criteria [21,22,23,24,25,26,27,28]. After analysis of the studies, scientific evidence was found to support the use of PFM training as an effective intervention for incontinence in the studied population.
Several risk factors predispose to the development of urinary incontinence in women, such as high parity, history of vaginal deliveries, and menopause [29,30,31]. In addition, obesity and aging are also important variables for the development of urinary incontinence independent of sex [32]. Within the eight articles included in this review, six studied overweight postmenopausal women (BMI > 25 Kg/m2–<30 Kg/m2) [22,23,24,25,27,28], one included postmenopausal women with normal weight [26], and finally, one article did not report BMI [21]. However, regardless of the BMI of the participants, the effects were statistically significant in all studies, which is in agreement with the systematic review made by Woodley et al. [33], who also conducted studies with varied BMI populations and observed favorable effects in all articles.
From the eight articles included in this review, 5 = five [21,22,23,27,28] focused on stress urinary incontinence only, two [24,25] included patients with stress or urgency urinary incontinence, and just one [26] of the articles included patients with stress, urgency, or mixed urinary incontinence; however, the effects of PFM training were statistically significant irrespective of this factor.
All studies used different measurement techniques to assess strength, quality of life, and the severity and prevalence of the urinary incontinence. Regarding strength, six articles [21,23,24,25,27] found statistically significant favorable changes in all of them. This is congruent with the findings of Alouini et al. [34], who reported similar results regarding the improvement of strength through PFM exercises in women. Strength production is mainly due to two factors: muscle-fiber trophism and motor-unit recruitment capacity. Current evidence suggests that changes in strength, at least during the first 8 weeks of a training protocol, are mainly caused by an increase in motor-unit recruitment capacity [35,36]. The protocols included in this review that found favorable results in terms of strength ranged from 6 to 12 weeks, finding in neural adaptations an explanation for their results. Additionally, one study evaluated the long-term effects [24], reporting that after 6 months, the strength gain decreased, however the change was not large enough to reach baseline.
The prevalence and severity of urinary incontinence was evaluated in seven of the studies [21,22,23,24,25,26,28], with statistically significant changes observed, both acutely and chronically, in favor of the groups that performed PFM exercise. The most prevalent ways to measure this variable were the pad test [21,26] and the amount or number of urinary leakages [23,24,26]. These results are similar to those obtained by other authors who determined the effects of PFM training in other population groups [33,37,38,39].
Quality of life was assessed in six [21,23,24,25,26,27] out of the eight studies included in this review, using different instruments such as the Social Activity Index [21], the International Consultation Incontinence Questionnaire—Short Form [25,27], the Incontinence Impact Questionnaire [26], and three domains (general health, incontinence impact, and gravity) of the King’s Health Questionnaire [23,24]. Only one of the studies [25] did not show statistically significant changes in this variable, mainly because the population of the intervention and control groups were not balanced from baseline (intergroup difference at baseline p = 0.03). Usually, patients with urinary incontinence present discomfort, low self-esteem, mood deterioration, and a feeling of helplessness, which generates an important psychological impact that ends up affecting the quality of life of the patient [37,40,41,42]. This is why interventions that generate a decrease in urinary incontinence are associated with an improvement in quality of life [43].
This systematic review is the first to evaluate the effects of PFM exercises in postmenopausal women with urinary incontinence; however, it has several limitations, and the results should be interpreted with discretion. The great heterogeneity in the exercise prescription does not allow an optimal prescription of the intervention to be established. In addition, no study was carried out in a European population; hence, a geographic bias was observed. Finally, it was not possible to calculate the size of the effects through a meta-analysis due to the great variety in the variables and the instruments and measurement techniques used by the different authors.
5. Conclusions
PFM exercise is a highly recommended intervention for treating urinary incontinence in postmenopausal women, whether it is applied alone or in combination with other interventions. Although the studies included in this review suggest that PFM training is effective regardless of the type of urinary incontinence, the current evidence is insufficient to be certain. Additionally, it is necessary to establish specific criteria for prescribing PFM exercises and measuring their results. More research in this field is needed, focused mainly on establishing the dose–response relationship of this intervention and on standardizing the methods of measuring the effects.
Author Contributions
Conceptualization, M.P.L.-P., C.R.-L. and Y.R.-C.; methodology, A.A.-A., F.H.-C. and M.d.C.C.-F.; writing—original draft preparation, M.P.L.-P., D.F.A.-R. and Y.C.-C.; writing—review and editing, Y.R.-C., M.d.C.C.-F., A.A.-A. and C.R.-L.; supervision, D.F.A.-R., Y.C.-C. and F.H.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Abrams, P.; Cardozo, L.; Fall, M.; Griffiths, D.; Rosier, P.; Ulmsten, U.; Van Kerrebroeck, P.; Victor, A.; Wein, A. The standardisation of terminology in lower urinary tract function: Report from the standardisation sub-committee of the international continence society. Urology 2003, 61, 37–49. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care. Risk Factors for Pelvic Floor Dysfunction; National Institute for Health and Care: London, UK, 2021.
- Robles, J.E. La incontinencia urinaria %j anales del sistema sanitario de navarra. An. Sis San Navar. 2006, 29, 219–231. Available online: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1137-66272006000300006&nrm=iso (accessed on 8 October 2022).
- Tubaro, A. Defining overactive bladder: Epidemiology and burden of disease. Urology 2004, 64, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Robinson, D.; Cardozo, L.D. The role of estrogens in female lower urinary tract dysfunction. Urology 2003, 62, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Seyyedi, F. Comparison of the effects of vaginal royal jelly and vaginal estrogen on quality of life, sexual and urinary function in postmenopausal women. J. Clin. Diagn. Res. 2016, 10, Qc01-5. [Google Scholar] [CrossRef]
- Ces, J.; Lago, I.; Liceras, J. Menopausia e incontinencia urinaria femenina: Acerca del posible efecto de la terapia hormonal sustitutiva. Clínica E Investig. En Ginecol. Y Obstet. 2007, 34, 224–229. [Google Scholar] [CrossRef]
- Dumoulin, C.; Cacciari, L.P.; Hay-Smith, E.J.C. Pelvic Floor Muscle Training Versus no Treatment, or Inactive Control Treatments, for Urinary Incontinence in Women. Available online: https://pubmed.ncbi.nlm.nih.gov/30288727/ (accessed on 8 October 2022).
- Arañó, P.; Rebollo, P.; Alsina, D.G.-S. Afectación de la calidad de vida relacionada con la salud en mujeres con incontinencia urinaria mixta. Actas Urológicas Españolas 2009, 33, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Hay-Smith, E.J.C.; Herderschee, R.; Dumoulin, C.; Herbison, G.P. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women. Cochrane Database Syst. Rev. 2011, 2011, CD009508. [Google Scholar] [CrossRef] [PubMed]
- Chamochumbi, C.C.M.; Nunes, F.R.; Guirro, R.R.D.J.; Guirro, E.C.D.O. Comparison of active and passive forces of the pelvic floor muscles in women with and without stress urinary incontinence. Rev. Bras Fisioter. 2012, 16, 314–319. [Google Scholar] [CrossRef] [PubMed]
- Berghmans; Hendriks; Bø; Smith, H.; Bie, D.; Van Doorn, V.W. Conservative treatment of stress urinary incontinence in women: A systematic review of randomized clinical trials. Br. J. Urol. 1998, 82, 181–191. [Google Scholar] [CrossRef]
- Wu, C.; Newman, D.; Schwartz, T.A.; Zou, B.; Miller, J.; Palmer, M.H. Effects of unsupervised behavioral and pelvic floor muscle training programs on nocturia, urinary urgency, and urinary frequency in postmenopausal women: Secondary analysis of a randomized, two-arm, parallel design, superiority trial (tulip study). Maturitas 2021, 146, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Malinauskas, A.P.; Bressan, E.F.M.; de Melo, A.M.Z.R.P.; Brasil, C.A.; Lordêlo, P.; Torelli, L. Efficacy of pelvic floor physiotherapy intervention for stress urinary incontinence in postmenopausal women: Systematic review. Arch. Gynecol. Obstet. 2022. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.M.; Do, T.T.T.; Tran, T.N.; Kim, J.H. Exercise and quality of life in women with menopausal symptoms: A systematic review and meta-analysis of randomized controlled trials. Int. J. Environ. Res. Public Health 2020, 17, 7049. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The prisma 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 105906. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Macedo, L.G.; Elkins, M.R.; Maher, C.G.; Moseley, A.M.; Herbert, R.D.; Sherrington, C. There was evidence of convergent and construct validity of physiotherapy evidence database quality scale for physiotherapy trials. J. Clin. Epidemiol. 2010, 63, 920–925. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Pitance, L.; Singh, V.; Neto, F.; Thie, N.; Michelotti, A. Effectiveness of manual therapy and therapeutic exercise for temporomandibular disorders: Systematic review and meta-analysis. Phys. Ther. 2016, 96, 9–25. [Google Scholar] [CrossRef]
- Rivas-Campo, Y.; García-Garro, P.A.; Aibar-Almazán, A.; Martínez-Amat, A.; Vega-Ávila, G.C.; Afanador-Restrepo, D.F.; León-Morillas, F.; Hita-Contreras, F. The effects of high-intensity functional training on cognition in older adults with cognitive impairment: A systematic review. Healthcare 2022, 10, 670. [Google Scholar] [CrossRef]
- Aksac, B.; Aki, S.; Karan, A.; Yalcin, O.; Isikoglu, M.; Eskiyurt, N. Biofeedback and pelvic floor exercises for the rehabilitation of urinary stress incontinence. Gynecol. Obs. Investig. 2003, 56, 23–27. [Google Scholar] [CrossRef]
- Sherburn, M.; Bird, M.; Carey, M.; Bø, K.; Galea, M.P. Incontinence improves in older women after intensive pelvic floor muscle training: An assessor-blinded randomized controlled trial. Neurourol. Urodyn. 2011, 30, 317–324. [Google Scholar] [CrossRef]
- Pereira, V.S.; De Melo, M.V.; Correia, G.N.; Driusso, P. Vaginal cone for postmenopausal women with stress urinary incontinence: Randomized, controlled trial. Climacteric 2012, 15, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Pereira, V.S.; de Melo, M.V.; Correia, G.N.; Driusso, P. Long-term effects of pelvic floor muscle training with vaginal cone in post-menopausal women with urinary incontinence: A randomized controlled trial. Neurourol. Urodyn. 2013, 32, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Antônio, F.I.; Herbert, R.D.; Bø, K.; Rosa-E-Silva, A.C.J.S.; Lara, L.A.S.; Franco, M.D.M.; Ferreira, C.H.J. Pelvic floor muscle training increases pelvic floor muscle strength more in post-menopausal women who are not using hormone therapy than in women who are using hormone therapy: A randomised trial. J. Physiother. 2018, 64, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Sran, M.; Mercier, J.; Wilson, P.; Lieblich, P.; Dumoulin, C. Physical therapy for urinary incontinence in postmenopausal women with osteoporosis or low bone density: A randomized controlled trial. Menopause 2016, 23, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Bertotto, A.; Schvartzman, R.; Uchôa, S.; Wender, M. Effect of electromyographic biofeedback as an add-on to pelvic floor muscle exercises on neuromuscular outcomes and quality of life in postmenopausal women with stress urinary incontinence: A randomized controlled trial. Neurourol. Urodyn. 2017, 36, 2142–2147. [Google Scholar] [CrossRef]
- Ghoniem, W.M.; Youssef, A.M.; Mohamed, S.A.; Elinin, M.F.A.; Hasanin, M.E. Effect of pilates exercises on stress urinary incontinence in post menopausal women: A randomized control trial. Fizjoterapia Pol. 2022, 22, 82–87. Available online: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85133327931&partnerID=40&md5=4d91ebea1b9969fe4f72be6c7407f97f (accessed on 28 October 2022).
- MacArthur, C.; Lewis, M.; Bick, D. Stress incontinence after childbirth. Br. J. Midwifery 1993, 1, 207–215. [Google Scholar] [CrossRef]
- Wilson, P.D.; Herbison, R.M.; Herbison, G.P. Obstetric practice and the prevalence of urinary incontinence three months after delivery. BJOG Int. J. Obstet. Gynaecol. 1996, 103, 154–161. [Google Scholar] [CrossRef]
- Thom, D.H.; Eeden, S.K.V.D.; Brown, J.S. Evaluation of parturition and other reproductive variables as risk factors for urinary incontinence in later life. Obstet. Gynecol. 1997, 90, 983–989. [Google Scholar] [CrossRef]
- Irwin, G.M. Urinary incontinence. Prim Care 2019, 46, 233–242. [Google Scholar] [CrossRef]
- Woodley, S.J.; Boyle, R.; Cody, J.D.; Mørkved, S.; Hay-Smith, E.J.C. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst. Rev. 2017, 12, Cd007471. [Google Scholar] [CrossRef] [PubMed]
- Alouini, S.; Memic, S.; Couillandre, A. Pelvic floor muscle training for urinary incontinence with or without biofeedback or electrostimulation in women: A systematic review. Int. J. Environ. Res. Public Health 2022, 19, 2789. [Google Scholar] [CrossRef]
- Škarabot, J.; Brownstein, C.G.; Casolo, A.; Del Vecchio, A.; Ansdell, P. The knowns and unknowns of neural adaptations to resistance training. Eur. J. Appl. Physiol. 2021, 121, 675–685. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, D.A.; Kamen, G.; Frost, G. Neural adaptations to resistive exercise: Mechanisms and recommendations for training practices. Sport. Med. 2006, 36, 133–149. [Google Scholar] [CrossRef] [PubMed]
- Radzimińska, A.; Strączyńska, A.; Weber-Rajek, M.; Styczyńska, H.; Strojek, K.; Piekorz, Z. The impact of pelvic floor muscle training on the quality of life of women with urinary incontinence: A systematic literature review. Clin. Interv. Aging. 2018, 13, 957–965. [Google Scholar] [CrossRef] [PubMed]
- Hagen, S.; Elders, A.; Stratton, S.; Sergenson, N.; Bugge, C.; Dean, S.; Hay-Smith, J.; Kilonzo, M.; Dimitrova, M.; Abdel-Fattah, M.; et al. Effectiveness of pelvic floor muscle training with and without electromyographic biofeedback for urinary incontinence in women: Multicentre randomised controlled trial. BMJ 2020, 371, m3719. [Google Scholar] [CrossRef]
- Sayılan, A.A.; Özbaş, A. The effect of pelvic floor muscle training on incontinence problems after radical prostatectomy. Am. J. Mens Health 2018, 12, 1007–1015. [Google Scholar] [CrossRef] [PubMed]
- Melville, J.L.; Fan, M.-Y.; Rau, H.; Nygaard, I.E.; Katon, W.J. Major depression and urinary incontinence in women: Temporal associations in an epidemiologic sample. Am. J. Obs. Gynecol. 2009, 201, 490.e1–490.e7. [Google Scholar] [CrossRef]
- Felde, G.; Bjelland, I.; Hunskaar, S. Anxiety and depression associated with incontinence in middle-aged women: A large norwegian cross-sectional study. Int. Urogynecol. J. 2012, 23, 299–306. [Google Scholar] [CrossRef]
- Tettamanti, G.; Altman, D.; Iliadou, A.N.; Bellocco, R.; Pedersen, N.L. Depression, neuroticism, and urinary incontinence in premenopausal women: A nationwide twin study. Twin Res. Hum. Genet. 2013, 16, 977–984. [Google Scholar] [CrossRef]
- Gordon, S.; Ruivo, D.B.; Viscardi, L.G.A.; de Oliveira, A.S. Effects of the pilates method isolated and associated with manual therapy in women with urinary incontinence. Man. Ther. Posturol. Rehabil. J. 2020, 18, 1–6. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).