Abstract
This study investigates the role of modern small-scale cities in addressing public health challenges through the lens of spatial justice, using the city of Tartu, Estonia, as a case study. Tartu has been recognized for its progressive public health initiatives, including the Tartu Health Care College, Mental Health Centre, Smoke-Free Tartu campaign, Health Trail network, Healthy School Program, and an expanding smart bike-sharing system. By employing Geographic Information Systems (GIS), we map and analyze the spatial distribution and accessibility of health-promoting infrastructure, such as healthcare facilities, green and blue spaces, health trails, and mobility services, across the urban landscape. A population-weighted accessibility assessment indicates that, although Tartu’s central districts (e.g., Kesklinn (HRI: 0.972)) are well-served, peripheral and densely populated districts such as Annelinn (HRI: 0.351) and Ropka (HRI: 0.377) exhibit notable deficits in health-related infrastructure. However, access to green infrastructure and mobility services is more evenly distributed citywide, reflecting a relatively equitable provision of non-clinical health assets. These findings highlight both the strengths and spatial gaps in Tartu’s health-oriented urban design, emphasizing the need for targeted investment in underserved areas. The study contributes to emerging studies on health-justice planning in small-scale urban contexts and demonstrates how spatial analytics can be guided to advance distributional justice in the provision of public health infrastructure. Ultimately, this research indicates the essential role of spatial analysis in guiding inclusive and data-informed health planning in urban environments.
1. Introduction
Health justice, the principle that everyone should have a fair and just opportunity to attain their full health potential, has moved from the margins of public health discourse to the center of urban planning debates [,]. Recent shifts in planning theory have placed renewed emphasis on spatial and distributional justice, moving beyond infrastructure provision to questions of who benefits, where and under what conditions [,]. Scholars of spatial justice emphasize that it is inherently spatial because where one is born, lives or works fundamentally shapes access to health-promoting resources [,]. Accordingly, the built environment functions both as a social determinant of health and as a moral arena in which planners negotiate competing claims to land, services and well-being [,].
Over the past three decades, Geographic Information Systems (GIS) have become necessary for translating abstract notions of fairness into measurable spatial relations such as distance, travel time and service catchments [,]. Methodological innovations now allow researchers to compare alternative distance-decay functions, assess service availability and spatial mismatch between population needs and resource allocation, integrate environmental-risk models with health outcomes and visualize real-time distributions of public amenities [,,].
Despite these achievements, empirical inquiry remains geographically uneven because much of the evidence base concentrates on megacities and global urban regions where data are richly available and inequalities are dramatic [,]. Small and medium-sized cities, which accommodate roughly one-third of Europe’s urban population [,], present a critical and understudied arena for health-justice planning. They differ from large cities in terms of their population, density, and resource allocation. Their urban forms, shorter travel distances, and more agile governance structures offer unique potential to rapidly prototype and implement justice-oriented planning [,]. These urban areas serve as critical experimental grounds for urban planning paradigms such as the 15-Minute City, which emphasizes the spatial reorganization of essential services including healthcare, green space, and mobility to prioritize accessibility and proximity within a short walk or bike ride for all residents [,]. This paper contributes to this emerging field by examining the city of Tartu, Estonia, a small-scale, digitally forward city that has invested heavily in health-supportive infrastructure and participatory urban strategies []. Tartu has implemented initiatives ranging from the Smoke-Free Tartu campaign and Health Trail network to smart mobility systems and mental health services. However, the extent to which these amenities are equitably distributed and accessible to all residents remains an open question. This research aims to critically evaluate whether health-promoting infrastructure in Tartu aligns spatially with the population’s distribution and need, a core principle of distributional justice [,].
This paper argues that advancing spatial health equity in small cities like Tartu has dual significance: it provides scalable methodological insights transferable to other compact urban systems and contributes to the comparative understanding of how urban scale shapes health infrastructure distribution. By demonstrating the applicability of composite accessibility tools at small-city scales, this research offers dissemination value for cities lacking the data capacity of large metropolitan areas.
Drawing on GIS and accessibility analysis, this study maps healthcare infrastructure, green and blue spaces, and public health initiatives across Tartu. It introduces a composite Health Resource Index (HRI) and applies a population-weighted accessibility analysis to explore how well Tartu’s health-promoting infrastructure serves its diverse districts and identifies areas of equity gap. By doing so, it builds on established spatial health methodologies [,,] while advancing a justice-oriented framework for health planning in small-scale cities.
The objectives of this paper are to (i) map and assess the spatial distribution of public health infrastructure in Tartu, including healthcare facilities, green and blue spaces, and mobility systems, (ii) identify inequities in access based on catchment analysis and population-weighted metrics, and (iii) reflect on the implications of these patterns for health-oriented spatial justice in small-scale cities. Therefore, the central argument of this paper is that health-oriented spatial analysis offers a critical tool for cities like Tartu to identify where infrastructure is located, and where it is most needed. By aligning spatial data with population demand, this approach reframes urban planning as an instrument for advancing equity, inclusivity, and long-term public health in small-scale urban contexts.
2. Literature Review
2.1. Spatial Justice and Health in Urban Theory
The concept of spatial justice has evolved from a radical critique of uneven development into a foundational lens through which urban space is increasingly analyzed and planned. Rooted in Henri Lefebvre’s (1991) notion of the “right to the city”, a claim for urban resources and participation in their shaping, spatial justice emphasizes the socially constructed nature of spatial arrangements and the embeddedness of power relations in urban form [,]. Building on Lefebvre, Edward Soja advanced the argument that justice is not only a legal or economic matter, but also “a locational and geographical one”, making spatial distribution central to urban inequality [].
Susan Fainstein translated these theoretical understandings into planning ethics, proposing a framework for “The Just City” that includes equity, diversity, and democratic participation as guiding principles []. Her work particularly critiques the technocratic tendencies of modern urbanism, insisting that justice, not merely efficiency or growth, must be at the core of planning practice.
When applied to health, spatial justice intersects with the social determinants of health, the conditions in which people are born, live, and age, which the World Health Organization identifies as central to health outcomes []. These determinants are often spatially distributed and deeply unequal, ranging from access to healthcare facilities and clean environments to public transportation and social infrastructure. Geographies of health literature have reinforced this link, arguing that spatial configurations, such as segregated urban development, fragmented green space, or environmental burdens, translate directly into disparities in morbidity and mortality [,]. Thus, a justice-oriented spatial analysis of health infrastructure must move beyond presence or absence to investigate who benefits, who is excluded, and how those patterns are reproduced in space.
The current study builds on this intersection, translating spatial justice theory into a practical geospatial diagnostic that small cities can adapt using open-source data and standard GIS techniques.
2.2. Planning for Health in Small Cities
Despite growing interest in the intersection of public health and urban planning, the majority of spatial health justice research continues to focus on megacities or large metropolitan areas [,,], often overlooking the unique conditions of small and mid-sized cities [,]. This focus has resulted in a systemic underrepresentation of small-scale urban contexts in both academic and policy literature, particularly regarding spatial analysis of health-promoting infrastructure []. Recent research in Nordic and Baltic contexts [] has shown that compact urban forms can support higher health accessibility when spatial planning aligns with community-scale service delivery. Similarly, work in Central Europe and Southeast Asia demonstrates that small cities, despite their scale, face infrastructure concentration and equity challenges similar to those of larger metropolitan regions [,].
As urban health justice frameworks increase, they are frequently shaped around the infrastructure capacities, governance scales, and data availability of larger cities, leaving smaller municipalities without appropriate tools for health planning []. Small cities present distinct opportunities. Their urban forms, shorter travel distances, and more cohesive institutional ecosystems make them ideal settings to operationalize justice-based planning models []. Cities like Tartu, Estonia, recognized for their progressive and localized health initiatives, exemplify how small-scale governance structures can enable integrated, citizen-responsive approaches. Moreover, data availability is improving even in smaller contexts, enabling the use of open-access spatial data and modeling tools to analyze intra-urban disparities with increasing precision [,,].
2.3. The 15-Minute City and Distributional Justice
The 15-Minute City concept, proposed by Carlos Moreno [], has gained global attention as a planning framework emphasizing proximity, accessibility, and temporal equity. Its core promise is that all residents should be able to reach essential services including healthcare, education and recreation within a 15-min walk or cycle [,]. Though frequently applied in large cities like Paris or Melbourne, the model is especially well-suited to small cities due to their natural spatial coherence and reduced travel times [,]. In this respect, the concept aligns closely with distributional justice, which evaluates just access and the fairness of spatial resource allocation relative to population need.
To operationalize this idea, methodologies and techniques such as catchment area analysis and population-weighted accessibility modeling, now widely used in GIS-based health research [,], allow researchers to quantify who can actually reach health resources, at what cost, and with what intensity of service. Recent literature also calls for composite indices like the HRI, which incorporate multiple dimensions of access (e.g., proximity, facility density) into a unified spatial equity metric [,]. By setting these tools in the analysis of Tartu, this study links the normative ambitions of the 15-Minute City with empirical techniques for measuring justice-oriented health access in small urban systems.
3. Materials and Methods
3.1. Study Area: Tartu, Estonia
Tartu, the second-largest city in Estonia (Figure 1) with a population of approximately 100,000 residents [], represents a model of modern small-scale urbanism. It functions as the intellectual and health capital of the country, hosting major institutions like the University of Tartu, University of Life Science, and the Tartu University Hospital. Tartu provided a wide range of public health initiatives and is recognized for its emphasis on digital innovation, sustainability, and inclusive urban policy []. Tartu’s urban form, relatively flat terrain, well-developed transportation network, extensive public health programs, and high digital literacy position it as a model small-scale urban system for implementing and evaluating health-supportive spatial strategies.
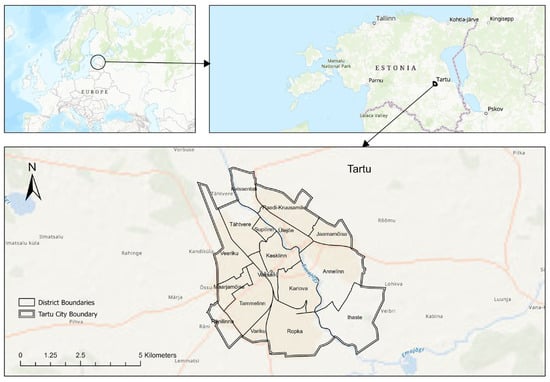
Figure 1.
Study Area: Tartu, Estonia (showing district boundaries).
To structure the analysis, we introduce a Three-Pillar Health Infrastructure Framework (Figure 2) to assess the city’s health-promoting systems, including:

Figure 2.
Three-Pillar Health Infrastructure of Tartu.
Health Services and Institutions: This pillar encompasses fixed-location clinical facilities such as the Tartu University Hospital Complex, Tartu Health Care College, and the Tartu Mental Health Centre. These represent the backbone of clinical care and professional training in the city.
Public Health and Community Programs: Representing community-based health initiatives and behavior-promoting amenities, including the Tartu Health Trail (a recreational path integrated into urban green spaces and through the city), Tartu Smart Bike Share (offering app-based short-term bicycle rentals at numerous urban docking points), and hobby services distributed throughout the city.
Environmental and Urban Health Factors: These represent broader determinants and non-clinical health-relevant urban features of public health, including green and blue infrastructure, mobility pathways (e.g., pedestrian and bicycle routes), and environmental quality metrics (air and noise pollution).
3.2. Data Layers
To assess the spatial distribution and accessibility of health-promoting assets in Tartu, we integrated the following data layers into a GIS environment (Table 1). Datasets were obtained from Tartu city government geoportal, OpenStreetMap, Estonian Topographic Database (ETAK), World Air Quality Historical Database, and the Estonian Environmental Agency. The data were projected to the same coordinate reference system (Lambert Conformal Conic projection = Estonian national grid of 1997, EPSG 3301), cleaned for accuracy, and processed for spatial consistency.

Table 1.
Data types, description and sources.
3.3. Spatial Analysis Techniques
The methodological framework combines network-based accessibility analysis, spatial statistics, spatial overlay mapping, and equity-weighted composite indexing. All spatial processing was performed using ArcGIS Pro (Version 3.5) and ArcMap (Version 10.8.2) software.
- (a)
- Infrastructure Mapping and Environmental Profiling
Each health-related layer including healthcare, green and blue spaces, mobility paths, and environmental exposures, was mapped independently to assess spatial distribution. These layers were analyzed for clustering and concentration patterns.
- (b)
- Catchment Area and Proximity Analysis
To assess the pedestrian accessibility of health-promoting infrastructure, we applied network-based service area buffers for healthcare facilities, fitness and hobby services, green and blue infrastructure, bike-share routes and stations, and health trails at radii of 400 m, 800 m, and 1200 m. This catchment-based accessibility model was selected due to its interpretability and compatibility with municipal-scale decision-making. These distances approximate 5-, 10-, and 15-min walking distances, respectively [], serving as benchmarks to determine whether urban amenities fall within reasonable reach of residents, suitable for the distributional justice analysis.
The accessibility analysis was conducted using pedestrian networks. While the 15-min city concept includes cycling, this study focuses on walking accessibility as the most universal mode of active transport, ensuring the baseline equity assessment is not influenced by variations in bicycle ownership or cycling propensity. The inclusion of cycling networks is a recommended avenue for future research to provide a more comprehensive assessment.
- (c)
- Composite Health Resource Hotspot Mapping
A composite Health Resource Hotspot Map was generated to identify spatial clusters of health-promoting infrastructure. We employed kernel density estimation (KDE) analysis. These spatial statistics identify zones of convergence where multiple amenities are co-located and likely to support cumulative health benefits.
- (d)
- Health Resource Index (HRI)
We developed a composite HRI to quantify and compare the spatial availability of health-supportive features across city. The four dimensions of the HRI were derived from the World Health Organization’s Social Determinants of Health (SDH) framework [] and the Healthy Cities approach []. These dimensions collectively represent both the service provision and environmental quality components of urban health systems. In addition, they operationalize our Three-Pillar Health Infrastructure Framework and capture key social determinants of health. (1) Proximity to healthcare facilities and public health amenities (Pillar 1), (2) access to green and blue infrastructure (Pillar 3), (3) availability of active mobility services (e.g., bike-share, pedestrian networks, and fitness trails) (Pillar 2) are well-established health-promoting factors. Conversely, environmental burdens (air and noise pollution (Pillar 3)) represent a critical health-depreciating factor, making their inclusion as a negative component essential for a holistic equity assessment.
To construct the HRI, four dimensions of health-promoting infrastructure were calculated for each 100 m2 hexagonal cell:
- 1.
- Healthcare Access (): Measured as the network distance from the cell centroid to the nearest healthcare facility (hospital, clinic, or mental health center). Shorter distances received higher scores.
- 2.
- Green and Blue Space Access (): Measured as the total area (m2) of green and blue spaces within an 800 m network buffer from the cell centroid. Larger areas received higher scores.
- 3.
- Mobility Service Availability (): A composite score based on (a) network distance to the nearest bike-share station and (b) the total length (m) of dedicated pedestrian and bicycle paths within an 800 m network buffer.
- 4.
- Environmental Burden (: A composite score based on standardized values of PM2.5 concentration and noise pollution levels assigned to each cell. Higher pollution levels received higher negative scores. The inclusion of environmental burden indicators as inverse weights is grounded in the concept of distributional environmental justice, which posits that exposure to pollution and noise constitutes negative health determinants that can offset the benefits of access to infrastructure.
Each of these component scores was standardized to a 0–1 scale (min-max normalization) to ensure comparability before combination.
In the absence of empirically established weightings and stakeholder-derived prioritizations, equal weighting was applied across all dimensions. This approach aligns with standard practice in exploratory spatial composite indices where all dimensions are assumed to contribute equally to the overall construct of interest [,]. While the equal-weight approach provides a neutral and replicable baseline, it is a study limitation. It assumes that proximity to a hospital is equally as important as access to a park, which may not reflect community preferences or the differential health impacts of various resources. Therefore, future research could refine this model using weighted multicriteria decision analysis (MCDA) or participatory weighting from community health priorities.
Final index was calculated as Equation (1):
or
where refers to healthcare access score, is green and blue space access score, , is the mobility infrastructure score, is environmental burden. shows weights (equal weights assumed in baseline model).
- (e)
- Population-Weighted Equity Analysis
To evaluate distributional justice from an equity perspective, we computed a population-weighted HRI for each district (see Equation (2)). This metric represents the average level of health resource access experienced by a typical resident in that district, giving more weight to hexagons with higher populations. A low population-weighted HRI indicates a district where many people have poor access.
where represents each 100 m2 hexagon within the district, is the Health Resource Index of that hexagon, and is its population. is the total number of hexagons in the district.
This allowed for a citywide comparison of infrastructure quality relative to actual demographic demand, highlighting spatial equity gaps. Then extracted the information based on each district, so high population and low HRI zones were explored as priority intervention areas.
To assess the applicability and precision of the Health Resource Index (HRI), a series of internal validation checks were conducted. First, the spatial consistency of HRI outputs was compared against observed service area distributions for healthcare and green infrastructure layers to ensure that high composite scores aligned with visually identifiable infrastructure clusters. Second, the population-weighted HRI was statistically correlated (Pearson’s r = 0.71) with individual accessibility indicators (e.g., proximity to health facilities), confirming internal coherence among the components.
While the model relies on open municipal and environmental data, which may introduce positional uncertainty and temporal variability, these limitations were minimized by harmonizing datasets to a unified 100 m spatial grid and normalizing all variables to standard scores before integration. Given its transparency and reproducibility, the HRI provides an adaptable tool for evaluating health-related spatial equity in small cities.
Figure 3 represents the Spatial health justice assessment framework applied in this study. This framework outlines the methodological structure used to evaluate the spatial equity of health-promoting infrastructure in Tartu.
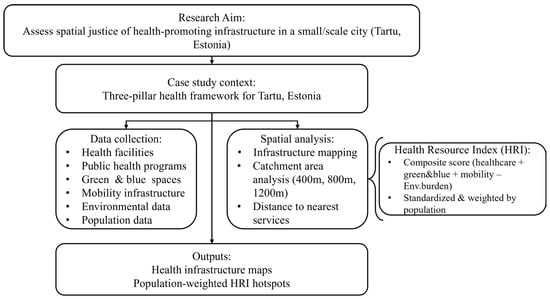
Figure 3.
Spatial health justice assessment framework.
4. Results
This section presents the spatial analysis of health-promoting infrastructure across Tartu, Estonia, based on the three-pillar framework: (1) health services and institutions, (2) public health and community programs, and (3) environmental and urban health factors. The analysis integrates point-level and polygon data with catchment area analysis and a composite population-weighted HRI.
4.1. Three-Pillar Health Infrastructure Distribution
4.1.1. Health Services and Institutions
The spatial distribution of Tartu’s formal healthcare facilities including hospitals, clinics and mental health centers is represented in Figure 4.
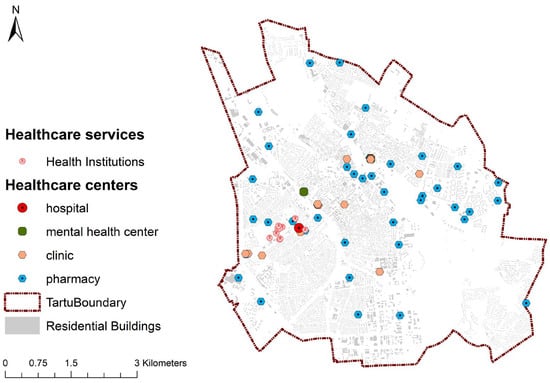
Figure 4.
Map of Health Facilities (categorized by facility type).
4.1.2. Public Health and Community Programs
The spatial distribution of bike-share system lanes with stations, and hobby services, which include sport and fitness facilities, is represented in Figure 5a, and the Tartu Health Trail is represented in Figure 5b.
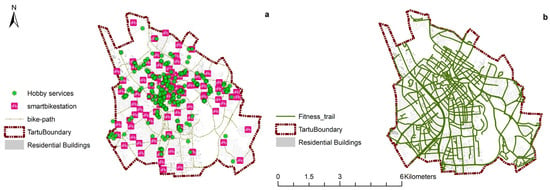
Figure 5.
Distribution of Public Health and Community Programs; Bike-share system lanes with stations, and hobby services (a), and Tartu Health Trail (b).
4.1.3. Environmental and Urban Health Factors
The network of pedestrian and bicycle paths and smart-Bick stations is represented in Figure 6a. Tartu benefits from a strong ecological integration, with the Emajõgi River serving as a central blue infrastructure axis. Numerous smaller lakes and green spaces are distributed throughout the urban fabric (Figure 6b). Air quality data, including PM2.5 and PM10 measurements (0–75 µg/m3), confirm that Tartu maintains excellent overall air quality over years (Figure 6c,e). It should be noted that due to minimal spatial variation in air quality across the city, this dimension contributed little to the spatial patterns observed in the final HRI. Noise pollution levels across Tartu generally remain within acceptable thresholds, with most residential areas registering between 40–55 dB. Moderate noise zones are concentrated along major arterial roads (Figure 6d).
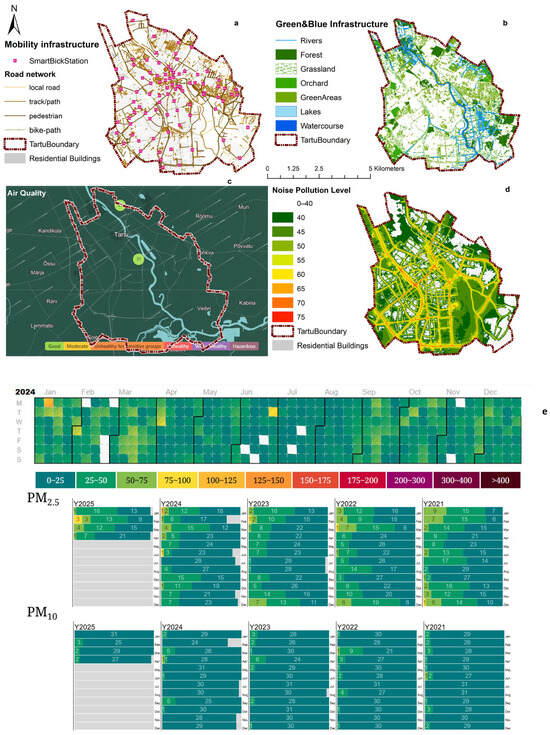
Figure 6.
Environmental and Urban Health Factors; Mobility infrastructure (a), Green & blue infrastructure (b), Air quality surface (c), Noise pollution level (d), Air quality over years (e).
4.2. Catchment Area and Accessibility Analysis Results
Catchment areas were generated at 400 m, 800 m, and 1200 m around key health-related infrastructure across Tartu to assess spatial accessibility within walking distances of approximately 5, 10, and 15 min. The catchment analysis of formal healthcare services (including hospitals and clinics) presented in Figure 7a. Hobby services (Figure 7b) and Fitness trails (Figure 7c) buffers intersect several residential districts. Central districts show denser service zones overlapping compared to peripheral areas. Catchment analysis for smart bike-share stations (Figure 7d) shows coverage in most urban districts within a 400 m–800 m walking range. Outer districts have fewer stations and correspondingly lower buffer coverage. Green (Figure 7e) and blue (Figure 7f) infrastructure catchments, including urban parks, forested areas, and proximity to the Emajõgi River and other small lakes, show a more dispersed pattern, while coverage is continuous along the river corridor and in peripheral park systems.
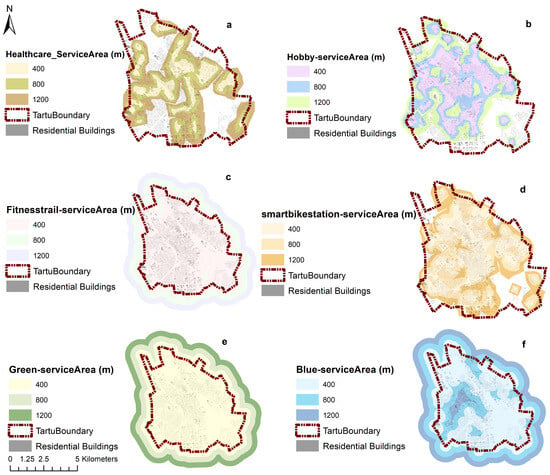
Figure 7.
Catchment Maps; healthcare (a), hobby services (b), fitness trails (c), bike-share stations (d), green infrastructure (e) and blue infrastructure (f), each shown with 400 m, 800 m, and 1200 m service area buffers.
4.3. Health Resource Index (HRI) Assessment
A composite KDE analysis was conducted to identify spatial concentrations of health-promoting infrastructure across Tartu. This analysis integrated the spatial locations of healthcare facilities, public health programs (e.g., bike-share stations, hobby services, fitness trails), green and blue spaces, and environmental quality layers. Hotspot zones were generated using spatial density estimation and overlaid to visualize multi-resource convergence (Figure 8). The results show that clusters of high infrastructure density are located in the central and near-central urban districts. These areas exhibit the greatest concentration of health-promoting resources in aggregate. Peripheral zones, particularly Annelinn, Ropka, Ihaste, and Ränilinn, show lower overall infrastructure density and less convergence across categories.
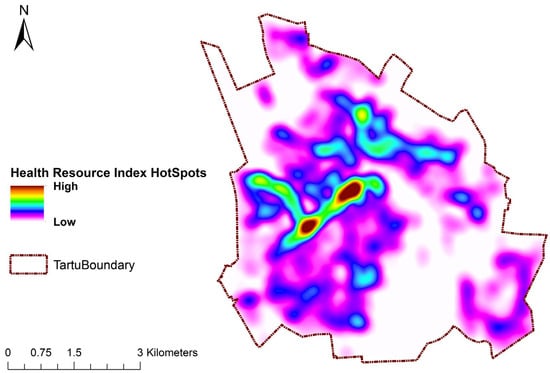
Figure 8.
Kernel Density Estimation (KDE) analysis of Health-Promoting Infrastructure.
To quantify spatial equity in access to health-promoting infrastructure across Tartu, a composite population-weighted HRI was calculated for each 100 m2 hexagonal cell and aggregated at the district level (Figure 9). The population-weighted HRI incorporates four dimensions: (i) proximity to healthcare infrastructure, (ii) accessibility to green and blue spaces, (iii) availability of mobility and public health services, and (iv) environmental burden from air and noise pollution, which was factored as a negative weight. Each variable was standardized, and the resulting index values were weighted by population calculated at a 100 m resolution to produce a population-weighted HRI score for each spatial unit.
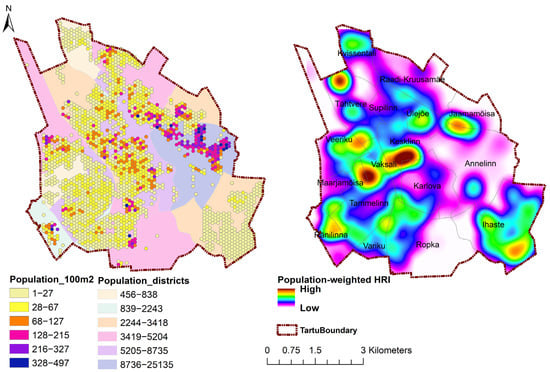
Figure 9.
Population in 100 m2 cells and districts (left) and population-weighted HRI in 100 m2 cells (right).
The index results represented in Table 2. display significant spatial variation. Kesklinn (city center) recorded the highest population-weighted HRI score (0.972), followed by Ülejõe (0.694) and Maarjamõisa (0.591), indicating strong alignment between infrastructure availability and population distribution. These districts are characterized by high concentrations of healthcare services, green areas, and multimodal mobility nodes. In contrast, Annelinn, Tartu’s most populous district with 25,135 residents, scored only 0.351, ranking 7th among 17 districts. Several other high-population or moderately dense districts, including Tammelinn (0.396), Ropka (0.377), and Veeriku (0.385), also returned medium HRI values, indicating a relative spatial mismatch between infrastructure distribution and demand. Districts such as Ihaste (0.097), Kvissentali (0.037), Variku (0.054), and Ränilinn (0.097) showed the lowest population-weighted HRI scores overall, though these are relatively low-population districts. Despite having smaller residential bases, these areas demonstrate minimal accessibility to health-related infrastructure.

Table 2.
Health Resource Index (HRI) Scores by District.
To support targeted interpretation of the HRI results, districts were categorized into three equity gap priority levels based on their population-weighted HRI scores. Districts with an HRI value of 0.00 to 0.20 were classified as “High Priority”, indicating a significant spatial mismatch between population density and access to health-promoting infrastructure; these include Jaamamõisa, Supilinn, Ränilinn, Ihaste, Variku, and Kvissentali. Scores between 0.20 and 0.50 were classified as “Medium Priority”, reflecting moderate infrastructure alignment, which consists of Tammelinn, Veeriku, Karlova, Raadi-Kruusamäe, Vaksali, Tähtvere, Ropka and Annelinn. Districts with scores above 0.50 were assigned “Low Priority”, denoting relatively equitable and sufficient spatial access to health-related amenities including Kesklinn, Ülejõe and Maarjamõisa. This classification scheme reflects relative thresholds of infrastructure equity within Tartu and enables a simple but evidence-based prioritization model for planning interventions. The thresholds were derived using a combination of quantile distribution and observed breaks in HRI clustering, ensuring both internal comparability and alignment with spatial justice principles that prioritize equity based on differentiated need rather than uniform provision [,].
Spatially, the HRI map indicates a central-peripheral gradient, where Kesklinn and Ülejõe exhibit the highest accessibility due to their concentration of health and educational institutions. Conversely, peripheral districts such as Annelinn, Ropka, and Ränilinn register low composite scores despite high residential densities, indicating a spatial mismatch between population needs and infrastructure supply. This asymmetry corresponds with historical urban expansion patterns, where newer residential zones developed faster than accompanying health infrastructure provision. The medium-accessibility belt (Karlova–Tähtvere–Raadi) reflects areas with balanced mobility networks and mixed land use, representing the link between urban form, connectivity, and health access.
5. Discussion
This study assessed the spatial justice of health-promoting infrastructure in Tartu, Estonia, using a combination of GIS, service catchment analysis, and a population-weighted HRI. As a digitally progressive small-scale city, Tartu provides a relevant case for examining how spatial planning frameworks, typically applied to larger urban areas, function at smaller scales. The findings demonstrate both strengths and spatial imbalances in the distribution of healthcare services, public health programs, and environmental resources. Here, the results are contextualized within broader academic and policy debates around spatial justice, accessibility, and the operationalization of the 15-Minute City. Drawing from existing literature and recent policy frameworks, we discuss the implications of the observed spatial patterns for urban health equity in small-city contexts, and outline strategies for addressing persistent gaps.
5.1. Spatial Distribution and Health Justice in a Small-Scale Urban Context
This study confirms that even in a small-scale city like Tartu, where health-promoting infrastructure is relatively well-developed, significant intra-urban disparities exist in terms of spatial justice. The central districts of Tartu demonstrate a high degree of co-location among healthcare facilities and mobility infrastructure. However, the green and blue infrastructures are evenly distributed. In contrast, peripheral districts such as Annelinn and Ropka, despite having some of the highest population densities, show consistently lower values in catchment access, facility clustering, and composite HRI. These findings reinforce the argument that spatial equity in health infrastructure cannot be assumed based on city size, population scale, or the nominal presence of health infrastructure services [,].
While small-scale cities are often viewed as inherently more equitable due to their form, shorter travel distances and lower population densities [], in the case of Tartu, despite its relatively modest population, it exhibits a polycentric and dispersed urban form [], with significant distances between core services and peripheral residential areas such as Annelinn and Ropka. This spatial dispersion limits access to centralized healthcare facilities and undermines the presumed advantages of small-city environments.
Prior studies have similarly cautioned against scaling down megacity frameworks without accounting for intra-urban form and service clustering [,]. In the context of Tartu, the uneven spatial alignment of population and infrastructure indicates that equity gaps are not necessarily a function of urban scale, but of how services are distributed in relation to actual settlement patterns. As Obeidat and Alourd [] demonstrate in their analysis of Irbid, Jordan, even modest-sized cities can maintain deep structural inequities when planning fails to reflect spatial-demographic realities.
Moreover, when evaluated through a population-weighted HRI, these resources appear [,] insufficient in precisely the areas where demand is greatest. This supports Fainstein’s [] and Soja’s [] argument that justice must be measured not just by availability but by accessibility and alignment with need. The Tartu case demonstrates that even well-resourced small cities must actively confront spatial mismatches between infrastructure and population, and that GIS-based methods can illuminate these often-overlooked gradients. This also challenges the planning idea of equating decentralization with accessibility. It illustrates that without deliberate spatial coordination, well-resourced and progressive small cities can reproduce invisible geographies of exclusion, where physical infrastructure is present but not equitably reachable by all communities [,]. The findings show that urban scale alone does not guarantee spatial justice; distribution, proximity, and population-weighted alignment are equally critical in ensuring that public health benefits are delivered inclusively.
Our population-weighted HRI approach offers a methodologically grounded alternative to simple service inventories. This reflects broader debates in urban planning around distributional justice, concerned with the fair spatial allocation of resources relative to need [,]. In this sense, Tartu’s spatial health landscape echoes broader patterns of urban inequality documented in large cities, but with local-specific manifestations that are equally consequential [,]. As the WHO [] emphasizes, spatially uneven access to health infrastructure can entrench disparities in outcomes, particularly when layered with environmental burdens like traffic-related noise or particulate exposure, even in generally “healthy” cities.
5.2. Integrating the 15-Minute City and GIS-Based Accessibility Planning
In this study, catchment areas were constructed at 400 m, 800 m, and 1200 m thresholds, representing approximately 5-, 10-, and 15-min walking distances, to analyze access to a range of health-promoting infrastructure in Tartu. This method directly reflects the time-distance metrics central to Moreno’s framework of the 15-Minute City concept, which emphasizes temporal proximity and daily access to essential services [].
The findings from Tartu show that while green and blue infrastructures and public health and community program amenities are relatively well distributed, healthcare facilities remain spatially concentrated, limiting accessibility in outer districts. This spatial mismatch suggests that even in cities with manageable geographic footprints, accessibility must be actively planned rather than presumed []. This is consistent with other studies showing that decentralization of services is often overlooked even in walkability-focused cities, leaving peripheral districts underserved [,].
Furthermore, GIS-based methods such as catchment analysis, hotspot mapping, and population-weighted equity indices offer strong tools for operationalizing spatial justice at the neighborhood scale [,,], while advancing the 15-Minute City beyond conceptual idealism. These tools allow planners to move beyond normative calls for equity and develop measurable, reproducible indicators that can guide infrastructure expansion and health policy design. As previous studies have shown, combining spatial accessibility with demographic weighting is essential to account for the “who” as well as the “where” of urban services [,,]. The WHO [] and Barton [] have long emphasized the importance of equity in urban health systems, and methods such as the HRI enable such principles to be translated into operational planning metrics.
The composite HRI used in this study contributes to this growing body of spatial health equity metrics. It captures the availability and co-location of health-relevant resources and adjusts these values relative to residential demand, aligning with WHO’s social determinants of health framework []. As Tiwari and Rushton [] argue, scalable spatial analysis systems offer a critical bridge between environmental health objectives and local planning capacity. When combined with accessibility models grounded in daily lived experiences, such as those proposed by Moreno, small cities like Tartu can prototype contextual, just implementations of the 15-Minute City at scale.
5.3. Policy Implications and Pathways for Small-Scale Cities
The spatial equity findings from Tartu offer important implications for health-oriented urban planning, particularly within the context of small-scale cities. While urban health policy and smart city technologies are often discussed in relation to large metropolitan areas [,], smaller cities face unique planning constraints and opportunities []. The findings of this study demonstrate how a data-driven, spatially explicit approach can guide equity-focused investment, promote distributed infrastructure planning, and institutionalize justice metrics into everyday decision-making.
The HRI developed in this study identifies districts where health-promoting infrastructure is misaligned with population density, a common issue in cities transitioning from centralization to more polycentric forms []. In Tartu, strategic interventions should prioritize high-population, medium- and low-HRI districts such as Annelinn and Ropka, where disparities between need and infrastructure availability are most acute. This could involve establishing a new community health clinic in Annelinn, expanding the bike-share network to ensure 400 m coverage in Ropka, and creating new pocket parks in these densely populated areas. These results align with broader findings in urban equity literature, which show that access to health infrastructure often does not correlate spatially with where health needs are greatest [,].
Strategic policy action should prioritize resource allocation based on population-weighted accessibility scores. This means extending clinical services, public health programs, and restorative environments (e.g., parks, fitness trails) into zones identified as underserved. Rather than equal distribution, the goal should be a just distribution, a key distinction in spatial justice theory [,,]. By doing so, small cities can establish their limited budgets more effectively while reducing health disparities that are spatial.
Active mobility systems, bicycle networks, pedestrian paths, and micro-transit, offer a cost-efficient means of improving access to health resources, especially in cities with flat geographies. In Tartu, accessibility to bike-share stations was generally strong. As seen in the literature [,,], co-location and connectivity between transit and health-promoting services enhances system-wide accessibility and encourages health-supportive behaviors.
Urban design policies should therefore incorporate mobility-health integration as a formal planning objective. For instance, the placement of health facilities along primary active mobility corridors or near green infrastructure can enhance both functional access and environmental quality. The integration of mobility and health can be operationalized by mandating that new health facilities are located along primary active mobility corridors and within 800 m of bike-share stations. This principle is also reflected in the 15-Minute City concept, where the clustering of amenities within short travel distances creates both efficiency and equity [,].
The composite HRI used in this study serves as a scalable tool for spatial justice in local planning workflows. While urban planners have long used distance-to-service indicators [,], composite indices that integrate population density, environmental quality, and service co-location [,,] provide a more comprehensive lens for monitoring infrastructure equity. By adopting open-source geospatial platforms and community-based participatory data collection, small cities can institutionalize real-time health equity monitoring without large administrative overheads [,]. Moreover, they can collaborate with regional or international networks of small urban systems to develop shared toolkits, knowledge repositories, and participatory frameworks that support distributed innovation and policy experimentation.
5.4. Limitations and Future Research
This study has several limitations that also present opportunities for future research. First, the HRI used equal weighting for its components; future studies could employ participatory methods like Analytic Hierarchy Process (AHP) to establish preference-based weights. Second, the analysis captured spatial accessibility but could not account for non-spatial barriers such as cost, cultural acceptability, or individual mobility constraints related to age, income, or disability. Third, as noted in the methods, the accessibility analysis was based on pedestrian travel; incorporating cycling and public transport networks would provide a more complete picture. Finally, the treatment of environmental burdens was necessarily simplistic, and future work could integrate exposure thresholds and population vulnerability metrics.
6. Conclusions
This study has examined the distributional justice of health-promoting infrastructure in Tartu, Estonia, offering a critical perspective on how small-scale cities can operationalize public health goals through urban design and spatial analysis. Using a three-pillar framework, comprising healthcare services, public health programs, and environmental health factors, the research employed GIS-based techniques including catchment analysis, composite hotspot mapping, and a population-weighted HRI to evaluate both infrastructure distribution and accessibility.
The results indicate that while Tartu demonstrates a strong foundation in green and blue infrastructure and community health programs, disparities persist in access to healthcare services, particularly in peripheral districts such as Annelinn and Ropka. The spatial patterning of these disparities underscores the importance of moving beyond total infrastructure counts to incorporate population-weighted equity indicators. The composite HRI introduced in this study serves as a replicable and scalable tool for such assessments.
The findings also highlight the relevance of the 15-Minute City concept for small-scale urban systems. By aligning catchment-based analysis with accessibility and mobility planning, cities like Tartu can design more equitable and resilient health environments. Importantly, this research demonstrates that small cities possess unique institutional flexibility to integrate open-source GIS tools, community data, and participatory planning practices into health policy and infrastructure decisions.
Future research could expand this work by incorporating real-time health outcomes, behavioral mobility data and community participation, and comparative analyses across small-scale cities. In doing so, planners and researchers can continue to develop context-sensitive models of spatial justice, ensuring that health infrastructure serves not only where people are, but also who they are.
Funding
This research received no external funding.
Data Availability Statement
The original contributions presented in this study are included in the article.
Conflicts of Interest
The author declares no conflicts of interest.
References
- Commission on the Social Determinants of Health. Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Marmot, M.; Bell, R. Fair society, healthy lives. Public Health 2012, 126 (Suppl. 1), S4–S10. [Google Scholar] [CrossRef]
- Soja, E.W. The city and spatial justice. Spat. Justice 2009, 1, 1–5. [Google Scholar]
- Fainstein, S.S. The just city. Int. J. Urban Sci. 2014, 18, 1–18. [Google Scholar] [CrossRef]
- Braveman, P.; Gruskin, S. Defining equity in health. J. Epidemiol. Community Health 2003, 57, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Barton, H. A health map for urban planners: Towards a conceptual model for healthy, sustainable settlements. Built Environ. 2005, 31, 339–355. [Google Scholar] [CrossRef]
- Giles-Corti, B.; Vernez-Moudon, A.; Reis, R.; Turrell, G.; Dannenberg, A.L.; Badland, H.; Foster, S.; Lowe, M.; Sallis, J.F.; Stevenson, M.; et al. City planning and population health: A global challenge. Lancet 2016, 388, 2912–2924. [Google Scholar] [CrossRef]
- Higgs, G. A literature review of the use of GIS-based measures of access to health care services. Health Serv. Outcomes Res. Methodol. 2004, 5, 119–139. [Google Scholar] [CrossRef]
- Cromley, E.K.; McLafferty, S.L. GIS and Public Health, 2nd ed.; Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Apparicio, P.; Abdelmajid, M.; Riva, M.; Shearmur, R. Comparing alternative approaches to measuring the geographical accessibility of urban health services: Distance types and aggregation-error issues. Int. J. Health Geogr. 2008, 7, 7. [Google Scholar] [CrossRef]
- Tiwari, C.; Rushton, G. A Spatial analysis system for integrating data, methods and models on environmental risks and Health outcomes. Trans. GIS 2010, 14 (Suppl. 1), 177–195. [Google Scholar] [CrossRef]
- Hashtarkhani, S.; Schwartz, D.L.; Shaban-Nejad, A. Enhancing Health Care Accessibility and Equity Through a Geoprocessing Toolbox for Spatial Accessibility Analysis: Development and Case Study. JMIR Form. Res. 2024, 8, e51727. [Google Scholar] [CrossRef]
- Ding, C.; He, X.; Zhu, Y. Megacity Growth, City System and Urban Strategy. Chin. J. Urban Environ. Stud. 2022, 10, 2250005. [Google Scholar] [CrossRef]
- Yang, H.; Chen, T.; Zeng, Z.; Mi, F. Does urban green space justly improve public health and well-being? A case study of Tianjin, a megacity in China. J. Clean. Prod. 2022, 380, 134920. [Google Scholar] [CrossRef]
- ESPON. Small and Medium-Sized Towns and Cities; Policies Strengthening Their Role in Achieving Active, Inclusive, and Functional Territories; ESPON EGTC: Kirchberg, Luxembourg, 2023. [Google Scholar]
- OECD; European Commission. Cities in the World: A New Perspective on Urbanisation; OECD Publishing: Paris, France, 2020. [Google Scholar] [CrossRef]
- Boelaert, M.; Arbyn, M.; der Stuyft, V. Editorial: Geographical information systems (GIS), gimmick or tool for health district management? Trop. Med. Int. Health 1998, 3, 163–165. [Google Scholar] [CrossRef] [PubMed]
- Allam, Z.; Bibri, S.E.; Chabaud, D.; Moreno, C. The Theoretical, Practical, and Technological Foundations of the 15-Minute City Model: Proximity and Its Environmental, Social and Economic Benefits for Sustainability. Energies 2022, 15, 6042. [Google Scholar] [CrossRef]
- Moreno, C.; Allam, Z.; Chabaud, D.; Gall, C.; Pratlong, F. Introducing the “15-minute city”: Sustainability, resilience and place identity in future post-pandemic cities. Smart Cities 2021, 4, 93–111. [Google Scholar] [CrossRef]
- Tartu City Government. Tartu 2030. 2006. Available online: https://www.riigiteataja.ee/akt/1034548.pdf (accessed on 22 January 2025).
- King, L. Henri Lefebvre and the right to the city. In The Routledge Handbook of Philosophy of the City; Routledge: Abingdon, UK, 2019; pp. 76–86. [Google Scholar] [CrossRef]
- Lefebvre, H.; Kofman, E.; Lebas, E. Writings on Cities; Wiley: Hoboken, NJ, USA, 1996; Available online: https://books.google.ee/books?id=RmiKMy3ICaYC (accessed on 13 March 2025).
- Jafri, S.H.; Gandhi, S.; Osei, E. Physician Deserts: Navigating the Texas Terrain of Provider Supply and Demand with GIS Mapping. Healthcare 2024, 12, 2397. [Google Scholar] [CrossRef]
- Takano, T.; Nakamura, K.; Watanabe, M. Urban residential environments and senior citizens’ longevity in megacity areas: The importance of walkable green spaces. J. Epidemiol. Community Health 2002, 56, 913–918. [Google Scholar] [CrossRef]
- Corburn, J. Healthy City Planning: From Neighbourhood to National Health Equity; Routledge: Abingdon, UK, 2013; pp. 1–182. [Google Scholar] [CrossRef]
- Luo, J.; Chan, E.H.W.; Du, J.; Feng, L.; Jiang, P.; Xu, Y. Developing a Health-Spatial Indicator System for a Healthy City in Small and Midsized Cities. Int. J. Environ. Res. Public Health 2022, 19, 3294. [Google Scholar] [CrossRef]
- Leão, A.L.F.; Banda, B.; Xing, E.; Gudapati, S.; Ahmad, A.; Lin, J.; Sastry, S.; Jacobs, N.; Reis, R.S. Applications of artificial intelligence in public health: Analyzing the built environment and addressing spatial inequities. J. Public Health 2025, 1–11. [Google Scholar] [CrossRef]
- Sunding, A.; Randrup, T.B.; Nordh, H.; Sang, Å.O.; Nilsson, K. Descriptions of the relationship between human health and green infrastructure in six Nordic comprehensive plans. Cities 2024, 146, 104746. [Google Scholar] [CrossRef]
- Obeidat, B.; Alourd, S. Healthcare equity in focus: Bridging gaps through a spatial analysis of healthcare facilities in Irbid, Jordan. Int. J. Equity Health 2024, 23, 52. [Google Scholar] [CrossRef] [PubMed]
- Servillo, L.; Atkinson, R.; Hamdouch, A. Small and Medium-Sized Towns in Europe: Conceptual, Methodological and Policy Issues. Tijdschr. Voor Econ. Soc. Geogr. 2017, 108, 365–379. [Google Scholar] [CrossRef]
- Rojas-Rueda, D.; Norberciak, M.; Morales-Zamora, E. Advancing Health Equity through 15-min Cities and Chrono-urbanism. J. Urban Health 2024, 101, 483–496. [Google Scholar] [CrossRef] [PubMed]
- Song, G.; He, X.; Kong, Y.; Li, K.; Song, H.; Zhai, S.; Luo, J. Improving the Spatial Accessibility of Community-Level Healthcare Service toward the ‘15-Minute City’ Goal in China. ISPRS Int. J. Geo-Inf. 2022, 11, 436. [Google Scholar] [CrossRef]
- Zhao, J.; Yang, Y.; Ogasawara, K. Measuring the Inequalities in the Distribution of Public Healthcare Resources by the HRDI (Health Resources Density Index): Data Analysis from 2010 to 2019. Healthcare 2022, 10, 1401. [Google Scholar] [CrossRef]
- Wang, T.; Zhou, T.; Zhou, L.; He, Y.; Wang, J.; Wang, Y.; Huang, L. Equity and efficiency of health resource allocation in the Chengdu–Chongqing Economic Circle of China. Front. Public Health 2024, 12, 1369568. [Google Scholar] [CrossRef] [PubMed]
- Statistical Database, Statistics Estonia. Available online: https://andmed.stat.ee/en/stat/rahvastik__rahvastikunaitajad-ja-koosseis__demograafilised-pehinaitajad/RV032 (accessed on 18 October 2024).
- de Sousa Silva, C.; Viegas, I.; Panagopoulos, T.; Bell, S. Environmental justice in accessibility to green infrastructure in two European Cities. Land 2018, 7, 134. [Google Scholar] [CrossRef]
- Mozaffaree Pour, N.; Partanen, J. Planning for the urban future: Two-level spatial analysis to discover 15-Minute City potential in urban area and expansion in Tallinn, Estonia. J. Comput. Soc. Sci. 2024, 7, 777–807. [Google Scholar] [CrossRef]
- Kizielewicz, B.; Tomczyk, T.; Gandor, M.; Sałabun, W. Subjective weight determination methods in multi-criteria decision-making: A systematic review. Procedia Comput. Sci. 2024, 246, 5396–5407. [Google Scholar] [CrossRef]
- Mozaffaree Pour, N. Urban Expansion in Estonia: Monitoring, Analysis, and Modeling; University of Tartu Press: Tartu, Estonia, 2022; Available online: http://dspace.ut.ee/handle/10062/83106 (accessed on 16 November 2024).
- Zhang, R.; Peng, S.; Sun, F.; Deng, L.; Che, Y. Assessing the social equity of urban parks: An improved index integrating multiple quality dimensions and service accessibility. Cities 2021, 129, 103839. [Google Scholar] [CrossRef]
- Pearce, J.; Witten, K.; Bartie, P. Neighbourhoods and health: A GIS approach to measuring community resource accessibility. J. Epidemiol. Community Health 2006, 60, 389–395. [Google Scholar] [CrossRef]
- Soja, E.W. Seeking spatial justice. Contemp. Polit. Theory 2013, 12, e16–e18. [Google Scholar] [CrossRef]
- Feitosa, F.O.; Wolf, J.H.; Marques, J.L. Operationalizing spatial justice in urban planning: Bridging theory with practice. Urban Res. Pract. 2024, 17, 720–736. [Google Scholar] [CrossRef]
- Lowe, M.; Adlakha, D.; Sallis, J.F.; Salvo, D.; Cerin, E.; Moudon, A.V.; Higgs, C.; Hinckson, E.; Arundel, J.; Boeing, G.; et al. City planning policies to support health and sustainability: An international comparison of policy indicators for 25 cities. Lancet Glob. Health 2022, 10, e882–e894. [Google Scholar] [CrossRef]
- Chen, Y.; Jia, S.; Xu, Q.; Xiao, Z.; Zhang, S. Measuring the dynamic accessibility to COVID-19 testing sites in the 15-min city: A focus on service congestion and mobility difference. J. Transp. Geogr. 2023, 111, 103670. [Google Scholar] [CrossRef]
- Haque, N.; Sharifi, A. Justice in access to urban ecosystem services: A critical review of the literature. Ecosyst. Serv. 2023, 67, 101617. [Google Scholar] [CrossRef]
- Moreno-Jiménez, A.; Cañada-Torrecilla, R.; Vidal-Domínguez, M.J.; Palacios-García, A.; Martínez-Suárez, P. Assessing environmental justice through potential exposure to air pollution: A socio-spatial analysis in Madrid and Barcelona, Spain. Geoforum 2016, 69, 117–131. [Google Scholar] [CrossRef]
- McLafferty, S.L. GIS and Health Care. Annu. Rev. Public Health 2003, 24, 25–42. [Google Scholar] [CrossRef]
- Glazener, A.; Sanchez, K.; Ramani, T.; Zietsman, J.; Nieuwenhuijsen, M.J.; Mindell, J.S.; Fox, M.; Khreis, H. Fourteen pathways between urban transportation and health: A conceptual model and literature review. J. Transp. Health 2021, 21, 101070. [Google Scholar] [CrossRef]
- Zhang, F.; Song, T.; Cheng, X.; Li, T.; Yang, Z. Transportation Infrastructure, Population Mobility, and Public Health. Int. J. Environ. Res. Public Health 2022, 20, 751. [Google Scholar] [CrossRef]
- Michel, S.; Banwell, N.; Senn, N. Mobility Infrastructures and Health: Scoping Review of studies in Europe. Public Health Rev. 2024, 45, 1606862. [Google Scholar] [CrossRef] [PubMed]
- Choperena-Aguilar, D.; Ramirez-Santiago, A.; Díaz, M.C.A. Measuring geospatial healthcare access to primary level facilities in Mexico: A gis-based diagnosis analysis. Cienc. Saude Coletiva 2021, 26, 2471–2482. [Google Scholar] [CrossRef] [PubMed]
- Gligorić, K.; Kamath, C.; Weiss, D.J.; Bavadekar, S.; Liu, Y.; Shekel, T.; Schulman, K.; Gabrilovich, E. Revealed versus potential spatial accessibility of healthcare and changing patterns during the COVID-19 pandemic. Commun. Med. 2023, 3, 157. [Google Scholar] [CrossRef] [PubMed]
- Brousmiche, D.; Occelli, F.; Genin, M.; Cuny, D.; Deram, A.; Lanier, C. Spatialized composite indices to evaluate environmental health inequalities: Meeting the challenge of selecting relevant variables. Ecol. Indic. 2020, 111, 106023. [Google Scholar] [CrossRef]
- Hyder, A.A.; Puvanachandra, P.; Morrow, R.H. Measuring the health of populations: Explaining composite indicators. J. Public Health Res. 2012, 1, 222–228. [Google Scholar] [CrossRef]
- Saib, M.-S.; Caudeville, J.; Beauchamp, M.; Carré, F.; Ganry, O.; Trugeon, A.; Cicolella, A. Building spatial composite indicators to analyze environmental health inequalities on a regional scale. Environ. Health 2015, 14, 68. [Google Scholar] [CrossRef]
- Mitropoulos, L.; Karolemeas, C.; Tsigdinos, S.; Vassi, A.; Bakogiannis, E. A composite index for assessing accessibility in urban areas: A case study in Central Athens, Greece. J. Transp. Geogr. 2023, 108, 103566. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Published by MDPI on behalf of the International Society for Photogrammetry and Remote Sensing. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).