Robotic Animal Use among Older Adults Enrolled in Palliative or Hospice Care: A Scoping Review and Framework for Future Research
Abstract
1. Introduction
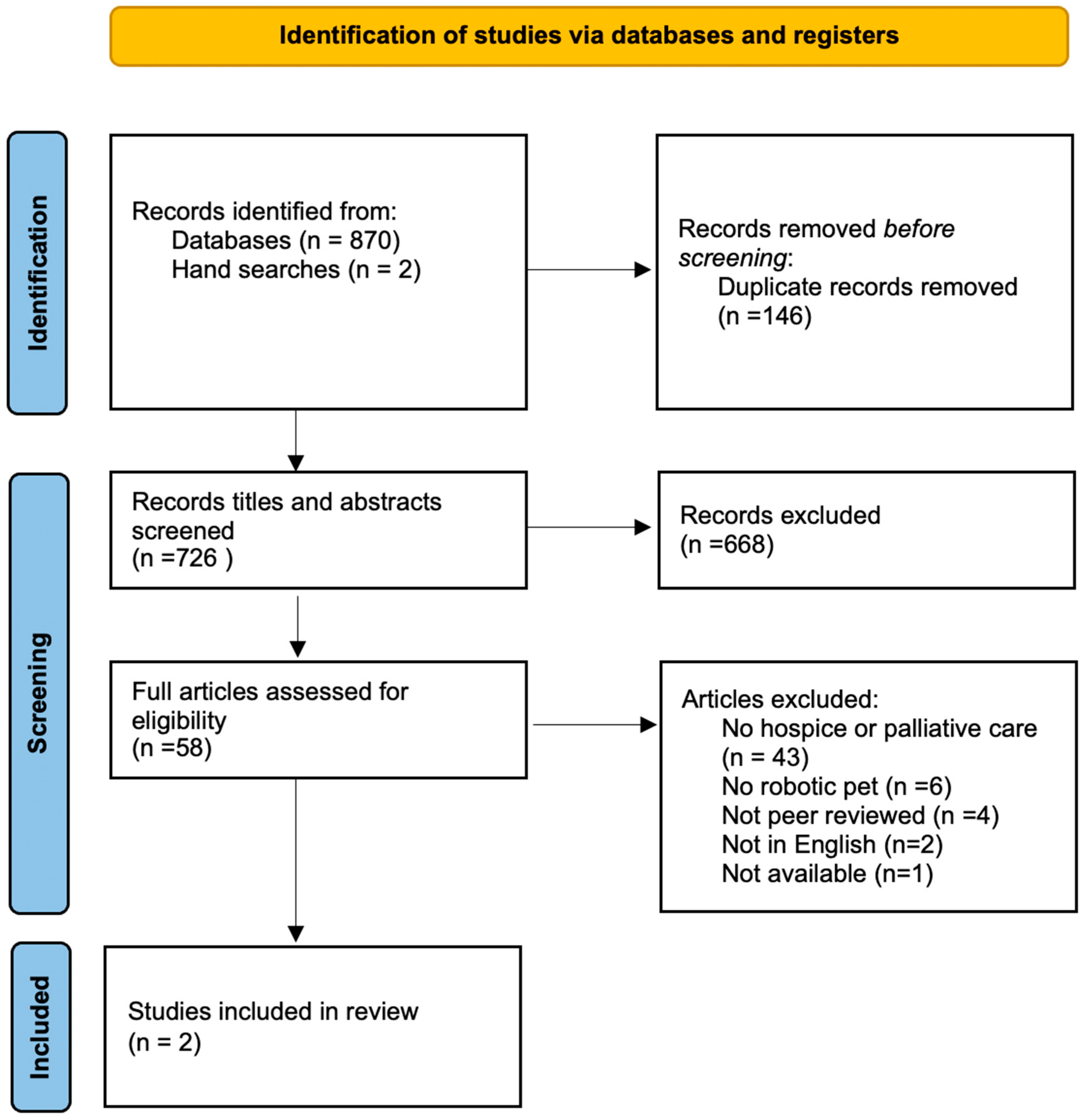
2. Methods
2.1. Types of Sources
2.2. Search Strategy
2.3. Study Selection
2.4. Data Extraction
3. Results
3.1. Participants and Study Settings
3.2. Study Design & Delivery
3.3. Perception of Robotic Pet
4. Outcomes
4.1. Decreased Need for Medication
4.2. Behavior Change
4.3. Emotional Benefit
5. Ethics
6. Discussion
7. Limitations and Strengths
8. Implications
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hui, D.; de la Cruz, M.; Mori, M.; Parsons, H.A.; Kwon, J.; Torres-Vigil, I.; Kim, S.H.; Dev, R.; Hutchins, R.; Liem, C.; et al. Concepts and definitions for “supportive care”, “best supportive care”, “palliative care”, and “hospice care” in the published literature, dictionaries, and textbooks. Support. Care Cancer 2012, 21, 659–685. [Google Scholar] [CrossRef] [PubMed]
- Krau, S.D. The difference between palliative care and end of life care: More than semantics. Nurs. Clin. 2016, 51, ix–x. [Google Scholar] [CrossRef]
- National Center for Health Statistics. Long-term Care Providers and Services Users in the United States. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Available online: https://www.cdc.gov/nchs/data/series/sr_03/sr03_43-508.pdf (accessed on 16 April 2024).
- Lupu, D.; Quigley, L.; Mehfoud, N.; Salsberg, E.S. The growing demand for hospice and palliative medicine physicians: Will the supply keep up? J. Pain Symptom Manag. 2018, 55, 1216–1223. [Google Scholar] [CrossRef] [PubMed]
- Mills, J.; Fox, J.; Damarell, R.; Tieman, J.; Yates, P. Palliative care providers’ use of digital health and perspectives on technological innovation: A national study. BMC Palliat. Care 2021, 20, 124. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Strategy on Digital Health. Available online: https://www.who.int/docs/defaultsource/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf (accessed on 16 April 2024).
- Novillo-Ortiz, D.; Dumit, E.M.; D’Agostino, M.; Becerra-Posada, F.; Kelley, E.T.; Torrent-Sellens, J.; Jiménez-Zarco, A.; Saigí-Rubió, F. Digital health in the Americas: Advances and challenges in connected health. BMJ Innov. 2018, 4, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Portz, J.D.; Cognetta, S.; Bekelman, D.B. Potential technological development in palliative care. J. Palliat. Med. 2021, 21, 899–900. [Google Scholar] [CrossRef]
- Nwosu, A.C.; Sturgeon, B.; McGlinchey, T.; Goodwin, C.D.; Behera, A.; Mason, S.; Stanley, S.; Payne, T.R. Robotic technology for palliative and supportive care: Strengths, weaknesses, opportunities, and threats. Palliat. Med. 2019, 33, 1106–1113. [Google Scholar] [CrossRef] [PubMed]
- Søraa, R.A.; Tøndel, G.; Kharas, M.W.; Serrano, J.A. What do Older Adults Want from Social Robots? A Qualitative Research Approach to Human-Robot Interaction (HRI) Studies. Int. J. Soc. Robot. 2023, 15, 411–424. [Google Scholar] [CrossRef]
- Petersen, S.; Houston, S.; Qin, H.; Tague, C.; Studley, J. The utilization of robotic pets in dementia care. J. Alzheimer’s Dis. 2017, 55, 569–574. [Google Scholar] [CrossRef]
- Saragih, I.D.; Tonapa, S.I.; Sun, T.L.; Chia-Ju, L.; Lee, B.O. Effects of robotic care interventions for dementia care: A systematic review and meta-analysis randomized controlled trials. J. Clin. Nurs. 2021, 30, 3139–3152. [Google Scholar] [CrossRef]
- Eachus, P. Pets, people, and robots: The role of companion animals and robopets in the promotion of health and well-being. Int. J. Health Promot. Educ. 2001, 39, 7–13. [Google Scholar] [CrossRef]
- Koh, W.Q.; Ang, F.X.H.; Casey, D. Impacts of Low-cost Robotic Pets for Older Adults and People with Dementia: Scoping Review. JMIR Rehabil. Assist. Technol. 2021, 8, e25340. [Google Scholar] [CrossRef]
- Abbott, R.; Orr, N.; McGill, P.; Whear, R.; Bethel, A.; Garside, R.; Stein, K.; Thompson-Coon, J. How do “robopets” impact the health and well-being of residents in care homes? A systematic review of qualitative and quantitative evidence. Int. J. Older People Nurs. 2019, 14, e12239. [Google Scholar] [CrossRef]
- Lu, L.-C.; Lan, S.-H.; Hsieh, Y.-P.; Lin, L.-Y.; Lan, S.-J.; Chen, J.-C. Effectiveness of Companion Robot Care for Dementia: A Systematic Review and Meta-Analysis. Innov. Aging 2021, 5, igab013. [Google Scholar] [CrossRef]
- Bates, M. Robotic Pets: A Senior’s Best Friend? IEEE Pulse 2019, 10, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Pu, L.; Moyle, W.; Jones, C. How people with dementia perceive a therapeutic robot called PARO in relation to their pain and mood: A qualitative study. J. Clin. Nurs. 2020, 29, 437–446. [Google Scholar] [CrossRef]
- Jones, C.; Moyle, W.; Murfield, J.; Draper, B.; Shum, D.; Beattie, E.; Thalib, L. Does cognitive impairment and agitation in dementia influence intervention effectiveness? Findings from a cluster-randomized-controlled trial with the therapeutic robot, PARO. J. Am. Med. Dir. Assoc. 2018, 19, 623–626. [Google Scholar] [CrossRef] [PubMed]
- Moyle, W.; Bramble, M.; Jones, C.; Murfield, J. Care staff perceptions of a social robot called Paro and a look-alike plush toy: A descriptive qualitative approach. Aging Ment. Health 2018, 22, 330–335. [Google Scholar] [CrossRef]
- Gustafsson, C.; Svanberg, C.; Müllersdorf, M. Using a robotic cat in dementia care: A pilot study. J. Gerontol. Nurs. 2015, 41, 46–56. [Google Scholar] [CrossRef]
- Yu, C.; Sommerlad, A.; Sakure, L.; Livingston, G. Socially assistive robots for people with dementia: Systematic review and meta-analysis of feasibility, acceptability and the effect on cognition, neuropsychiatric symptoms, and quality of life. Ageing Res. Rev. 2022, 78, 101633. [Google Scholar] [CrossRef]
- Persson, M. Introducing social robots in Swedish dementia care: Exploring the interaction between care workers, residents, and robotic cats. J. Sociol. Soc. Work 2020, 8, 8–18. [Google Scholar] [CrossRef]
- Ageless Innovation. Available online: https://agelessinnovation.com (accessed on 16 April 2024).
- Pike, J.; Picking, R.; Cunningham, S. Robot companion cats for people at home with dementia: A qualitative case study on companotics. Dementia 2021, 20, 1300–1318. [Google Scholar] [CrossRef] [PubMed]
- Gee, N.R.; Rodriguez, K.E.; Fine, A.H.; Trammell, J.P. Dogs supporting human health and well-being: A biopsychosocial approach. Front. Vet. Sci. 2021, 8, 630465. [Google Scholar] [CrossRef] [PubMed]
- Enders-Slegers, M.J.; Hediger, K. Pet ownership and human–animal interaction in an aging population: Rewards and challenges. Anthrozoös 2019, 32, 255–265. [Google Scholar] [CrossRef]
- Hudson, J.; Ungar, R.; Albright, L.; Tkatch, R.; Schaeffer, J.; Wicker, E.R. Robotic Pet Use among Community-Dwelling Older Adults. J. Gerontol. Ser. B 2020, 75, 2018–2028. [Google Scholar] [CrossRef] [PubMed]
- Guerra, S.; Rosa, C.; Sousa, L.; Neves, A.; Pestana, G.; Hernández, M.J.; Losada, R.; Pires, S.; Ribeiro, O. The use of robotic pets by community-dwelling older adults: A scoping review. Int. J. Soc. Robot. 2022, 14, 1481–1492. [Google Scholar] [CrossRef]
- Community Hospice and Palliative Care Receives Robotic Pets for Patients. Available online: https://www.communityhospice.com/about/media-room/community-hospice-palliative-care-receives-robotic-cats-and-dogs-for-patients (accessed on 1 May 2024).
- Robotic Companion Pets. Capital Caring. Available online: https://www.capitalcaring.org/get-help/our-services/robotic-companion-pets/ (accessed on 1 May 2024).
- Robotic Pets Donated to Hampton VA Medical Center Hospice. Available online: https://www.wavy.com/news/military/robotic-pets-donated-to-hampton-va-medical-center-hospice/ (accessed on 1 May 2024).
- Pham, M.T.; Rajić, A.; Greig, J.D.; Sargeant, J.M.; Papadopoulos, A.; McEwen, S.A. A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Res. Synth. Methods 2014, 5, 371–385. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Chapter 11: Scoping Reviews. In JBI Manual for Evidence Synthesis, 2020 version; Aromataris, E., Munn, Z., Eds.; JBI: Singapore, 2020. [Google Scholar]
- Bramer, W.M.; De Jonge, G.B.; Rethlefsen, M.L.; Mast, F.; Kleijnen, J. A systematic approach to searching: An efficient and complete method to develop literature searches. J. Med. Libr. Assoc. JMLA 2018, 106, 53. [Google Scholar] [CrossRef]
- University of Illinois Library. Available online: https://guides.library.illinois.edu/c.php?g=563215&p=3877584 (accessed on 1 May 2024).
- Covidence. Available online: https://www.covidence.org (accessed on 5 December 2022).
- Brecher, D.B. Use of a Robotic Cat to Treat Terminal Restlessness: A Case Study. J. Palliat. Med. 2020, 23, 432–434. [Google Scholar] [CrossRef]
- Birks, M.; Bodak, M.; Barlas, J.; Harwood, J.; Pether, M. Robotic Seals as Therapeutic Tools in an Aged Care Facility: A Qualitative Study. J. Aging Res. 2016, 2016, 8569602. [Google Scholar] [CrossRef] [PubMed]
- Jung, M.M.; Van der Leij, L.; Kelders, S.M. An exploration of the benefits of an animal like robot companion with more advanced touch interaction capabilities for dementia care. Front. ICT 2017, 4, 16. [Google Scholar] [CrossRef]
- Moyle, W.; Bramble, M.; Jones, C.J.; Murfield, J.E. “She had a smile on her face as wide as the great Australian bite”: A qualitative examination of family perceptions of a therapeutic robot and a plush toy. Gerontologist 2019, 59, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, I.; Koulouglioti, C.; Ali, S. Views of nurses and other health and social care workers on the use of assistive humanoid and animal-like robots in health and social care: A scoping review. Contemp. Nurse 2018, 54, 425–442. [Google Scholar] [CrossRef] [PubMed]
- Vandemeulebroucke, T.; de Casterlé, B.D.; Gastmans, C. How do older adults experience and perceive socially assistive robots in aged care: A systematic review of qualitative evidence. Aging Ment. Health 2018, 22, 149–167. [Google Scholar] [CrossRef]
- Cubanski, J.; Neuman, T. Prices Increased Faster than Inflation for Half of All Drugs Covered by Medicare in 2020. Kaiser Family Foundation. 2022. Available online: https://www.kff.org/medicare/issue-brief/prices-increased-faster-than-inflation-for-half-of-all-drugs-covered-by-medicare-in-2020/ (accessed on 1 May 2024).
- Cardoso, C.S.; Monteiro-Soares, M.; Matos, J.R.; Prazeres, F.; Martins, C.; Gomes, B. Protocol: Non-pharmacological interventions in primary care to improve the quality of life of older patients with palliative care needs: A systematic review protocol. BMJ Open 2022, 12, e060517. [Google Scholar] [CrossRef]
- Robins, L.M.; Lee, D.C.A.; Bell, J.S.; Srikanth, V.; Möhler, R.; Hill, K.D.; Haines, T.P. Definition, and measurement of physical and chemical restraint in long-term care: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 3639. [Google Scholar] [CrossRef]
- Jeyakuma, J.; Feuer, D. The care of dying men. Trends Urol. Men’s Health 2013, 4, 21–24. [Google Scholar] [CrossRef]
- Krauss, B.J.; Schlievert, M.A.; Wagner, B.K.; Deutsch, D.D.; Powell, R.J. A pilot study of nonpharmacological interventions for hospice patients with behavioral and psychological symptoms in dementia. J. Hosp. Palliat. Nurs. 2020, 22, 489–494. [Google Scholar] [CrossRef]
- Hui, D.; De La Rosa, A.; Wilson, A.; Nguyen, T.; Wu, J.; Delgado-Guay, M.; Azhar, A.; Arthur, J.; Epner, D.; Bruera, E.; et al. Neuroleptic strategies for terminal agitation in patients with cancer and delirium at an acute palliative care unit: A single-centre, double-blind, parallel-group, randomized trial. Lancet Oncol. 2020, 21, 989–998. [Google Scholar] [PubMed]
- Jøranson, N.; Pedersen, I.; Rokstad, A.; Ihlebæk, C. Effects on symptoms of agitation and depression in persons with dementia participating in robot-assisted activity: A cluster-randomized controlled trial. J. Am. Med. Dir. Assoc. 2015, 16, 867–873. [Google Scholar] [CrossRef] [PubMed]
- Shamsuddin, S.; Zulkifli, W.Z.; Thiam Hwee, L.; Yussof, H. Animal robot as augmentative strategy to elevate mood: A preliminary study for post-stroke depression. In Interactive Collaborative Robotics, Proceedings of the Second International Conference, ICR 2017, Hatfield, UK, 12–16 September 2017, Proceedings 2; Springer International Publishing: Berlin/Heidelberg, Germany, 2017; pp. 209–218. [Google Scholar] [CrossRef]
- Bovero, A.; Gottardo, F.; Botto, R.; Tosi, C.; Selvatico, M.; Torta, R. Definition of a good death, attitudes toward death, and feelings of interconnectedness among people taking care of terminally ill patients with cancer: An exploratory study. Am. J. Hosp. Palliat. Med. 2020, 37, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Fogelson, D.M.; Rutledge, C.; Zimbro, K.S. The impact of robotic companion pets on depression and loneliness for older adults with dementia during the COVID-19 pandemic. J. Holist. Nurs. 2022, 40, 397–409. [Google Scholar] [CrossRef] [PubMed]
- Bricout, J.; Greer, J.; Fields, N.; Xu, L.; Tamplain, P.; Doelling, K.; Sharma, B. The “humane in the loop”: Inclusive research design and policy approaches to foster capacity building assistive technologies in the COVID-19 era. Assist. Technol. 2022, 34, 644–652. [Google Scholar] [CrossRef] [PubMed]
- Fields, N.; Xu, L.; Greer, J.; Murphy, E. Shall I compare thee… to a robot? An exploratory pilot study using participatory arts and social robotics to improve psychological well-being in later life. Aging Ment. Health 2021, 25, 575–584. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Fields, N.L.; Greer, J.A.; Tamplain, P.M.; Bricout, J.C.; Sharma, B.; Doelling, K.L. Socially assistive robotics and older family caregivers of young adults with Intellectual and Developmental Disabilities (IDD): A pilot study exploring respite, acceptance, and usefulness. PLoS ONE 2022, 17, e0273479. [Google Scholar] [CrossRef] [PubMed]
- Bedaf, S.; Marti, P.; Amirabdollahian, F.; de Witte, L. A multi-perspective evaluation of a service robot for seniors: The voice of different stakeholders. Disabil. Rehabil. Assist. Technol. 2018, 13, 592–599. [Google Scholar] [CrossRef] [PubMed]
- Fiorini, L.; De Mul, M.; Fabbricotti, I.; Limosani, R.; Vitanza, A.; D’Onofrio, G.; Tsui, N.; Sancarlo, D.; Giuliani, F.; Greco, A.; et al. Assistive robots to improve the independent living of older persons: Results from a needs study. Disabil. Rehabil. Assist. Technol. 2021, 16, 92–102. [Google Scholar] [CrossRef]
- Lenca, M.; Kressig, R.W.; Jotterand, F.; Elger, B. Proactive ethical design for neuro-engineering, assistive and rehabilitation technologies: The Cybathlon. J. NeuroEng. Rehabil. 2017, 14, 115. [Google Scholar] [CrossRef]
- Chen, E.K.; Riffin, C.; Cary Reid, M.; Adelman, R.; Warmington, M.; Mehta, S.S.; Pillemer, K. Why is high-quality research on palliative care so hard to do? Barriers to improved research from a survey of palliative care researchers. J. Palliat. Med. 2014, 17, 782–787. [Google Scholar] [CrossRef] [PubMed]
- Center to Advance Palliative Care. Help CAPC Achieve “Palliative Care Everywhere”. Available online: https://www.capc.org/about/donate/?clickthrough_doc_id=core.contentpage.548&clickthrough_req_id=jtZGqs7oTUKb9bu8IAHu_w&clickthrough_query=Everywhere (accessed on 1 May 2024).
- Canadian Hospice Palliative Care Association. A Model to Guide Hospice Palliative Care. Available online: https://www.chpca.ca/wp-content/uploads/2019/12/norms-of-practice-eng-web.pdf (accessed on 1 May 2024).
- Jøranson, N.; Pedersen, I.; Rokstad, A.M.M.; Ihlebæk, C. Change in quality of life in older people with dementia participating in Paro-activity: A cluster-randomized controlled trial. J. Adv. Nurs. 2016, 72, 3020–3033. [Google Scholar] [CrossRef] [PubMed]
- Robinson, H.; MacDonald, B.; Broadbent, E. Physiological effects of a companion robot on blood pressure of older people in residential care facility: A pilot study. Australas. J. Ageing 2015, 34, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Moyle, W.; Cooke, M.; Beattie, E.; Jones, C.; Klein, B.; Cook, G.; Gray, C. Exploring the effect of companion robots on emotional expression in older adults with dementia: A pilot randomized controlled trial. J. Gerontol. Nurs. 2013, 39, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Tkatch, R.; Wu, L.; MacLeod, S.; Ungar, R.; Albright, L.; Russell, D.; Murphy, J.; Schaeffer, J.; Yeh, C.S. Reducing loneliness and improving well-being among older adults with animatronic pets. Aging Ment. Health 2021, 25, 1239–1245. [Google Scholar] [CrossRef] [PubMed]
- Robinson, H.; MacDonald, B.; Kerse, N.; Broadbent, E. The psychosocial effects of a companion robot: A randomized controlled trial. J. Am. Med. Dir. Assoc. 2013, 14, 661–667. [Google Scholar] [CrossRef] [PubMed]
- Liang, A.; Piroth, I.; Robinson, H.; MacDonald, B.; Fisher, N.U.M.; Skoluda, N.; Broadbent, E. A pilot randomized trial of a companion robot for people with dementia living in the community. J. Am. Med. Dir. Assoc. 2017, 10, 871–878. [Google Scholar] [CrossRef]
- Moyle, W.; Jones, C.J.; Murfield, J.E.; Thalib, L.; Beattie, E.R.; Shum, D.K.; O’Dwyer, S.T.; Mervin, M.C.; Draper, B.M. Use of a robotic seal as a therapeutic tool to improve dementia symptoms: A cluster-randomized controlled trial. J. Am. Med. Dir. Assoc. 2017, 18, 766–773. [Google Scholar] [CrossRef]
- Thodberg, K.; Sørensen, L.U.; Videbech, P.B.; Poulsen, P.H.; Houbak, B.; Damgaard, V.; Keseler, I.; Edwards, D.; Christensen, J.W. Behavioral responses of nursing home residents to visits from a person with a dog, a robot seal or a toy cat. Anthrozoös 2016, 29, 107–121. [Google Scholar] [CrossRef]
- Yuan, S.; Coghlan, S.; Lederman, R.; Waycott, J. Social robots in aged care: Care staff experiences and perspectives on robot benefits and challenges. Proc. ACM Hum. Comput. Interact. 2022, 6, 329. [Google Scholar] [CrossRef]
- Bemelmans, R.; Gelderblom, G.J.; Jonker, P.; de Witte, L. Effectiveness of robot Paro in intramural psychogeriatric care: A multicenter quasi-experimental study. J. Am. Med. Dir. Assoc. 2015, 16, 946–950. [Google Scholar] [CrossRef] [PubMed]
- Randall, N.; Bennett, C.C.; Šabanović, S.; Nagata, S.; Eldridge, L.; Collins, S.; Piatt, J.A. More than just friends: In-home use and design recommendations for sensing socially assistive robots (SARs) by older adults with depression. Paladyn J. Behav. Robot. 2019, 10, 237–255. [Google Scholar] [CrossRef]

| Database | Search Strategy |
|---|---|
| MEDLINE | Line 1: robo * Line 2: animal OR pet OR dog OR cat OR seal OR companion Line 3: hospice OR palliative OR “end of life” OR terminal * OR dying OR death OR end-stage |
| Title | Robotic Seals as Therapeutic Tools in an Aged Care Facility: A Qualitative Study. | Use of a Robotic Cat to Treat Terminal Restlessness: A Case Study |
|---|---|---|
| Lead Author | Birks, Melanie; Bodak, Marie; Barlas, Joanna; Harwood, June; Pether, Mary | Brecher, DB |
| Publication Year | 2016 | 2020 |
| Location | Australia | U.S.A |
| Setting | Aged care facility | Veterans Affairs Community Living Center |
| Population | Older adults | Veteran Age 90 |
| Sample | Therapists (n = 3) | Case study (n = 1) |
| Methods | Qualitative thematic analysis | Case study |
| Aim/Purpose | Identify, explore, and describe the impact of PARO. PARO is used daily as a diversional therapy with residents in an individual or group activity. Each therapy session lasted 30–40 min. During the sessions, residents were encouraged to engage with Paro. After approximately four months, interviews were conducted with the participants for about one hour each. | The case study examined the effectiveness of using a robotic cat to assist with the treatment of an older adult with terminal restlessness. |
| Type of Robot | Seal; PARO | Cat; Joy for All Ageless Innovation |
| Perception of Robot | Mixed views | Not clearly stated |
| Outcomes | Behavioral and emotional benefits | The use of robotic cats may enhance the older adult’s quality of life and their ability to interact with loved ones before entering the active dying process. In addition, robotic cats may have a role in decreasing terminal restlessness as they have positive physical and emotional effects which can be used to supplement pharmacological interventions. |
| Measures | Interviews with the three therapists who were asked to share their experiences and observations using PARO, data were transcribed and thematically analyzed | Minimizing pharmacological treatments for behaviors |
| Major Findings | Three major themes were identified from the analyses: “a therapeutic tool that’s not for everybody”, “every interaction is powerful”, and “keeping the momentum”. The findings support using PARO as a therapeutic tool, showing improvement in emotional state, reduction of challenging behaviors, and improvement in social connections. | The case study showed robotic cats can have a positive role in terminal restlessness as they can impact physical and emotional well-being and can be used to supplement pharmacological therapy. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miles, A.; Fields, N.L.; Bennett, M.; Xu, L.; Magruder, K.; Stringfellow, M.K.; Sesay, B.J.; Handique, S. Robotic Animal Use among Older Adults Enrolled in Palliative or Hospice Care: A Scoping Review and Framework for Future Research. Robotics 2024, 13, 92. https://doi.org/10.3390/robotics13060092
Miles A, Fields NL, Bennett M, Xu L, Magruder K, Stringfellow MK, Sesay BJ, Handique S. Robotic Animal Use among Older Adults Enrolled in Palliative or Hospice Care: A Scoping Review and Framework for Future Research. Robotics. 2024; 13(6):92. https://doi.org/10.3390/robotics13060092
Chicago/Turabian StyleMiles, Allyson, Noelle L. Fields, Michael Bennett, Ling Xu, Karen Magruder, Mary Kris Stringfellow, Benjamin J. Sesay, and Swasati Handique. 2024. "Robotic Animal Use among Older Adults Enrolled in Palliative or Hospice Care: A Scoping Review and Framework for Future Research" Robotics 13, no. 6: 92. https://doi.org/10.3390/robotics13060092
APA StyleMiles, A., Fields, N. L., Bennett, M., Xu, L., Magruder, K., Stringfellow, M. K., Sesay, B. J., & Handique, S. (2024). Robotic Animal Use among Older Adults Enrolled in Palliative or Hospice Care: A Scoping Review and Framework for Future Research. Robotics, 13(6), 92. https://doi.org/10.3390/robotics13060092







