Effectiveness of Implementing Hospital Wastewater Treatment Systems as a Measure to Mitigate the Microbial and Antimicrobial Burden on the Environment
Abstract
1. Introduction
2. Materials and Methods
2.1. Hospital Wastewater
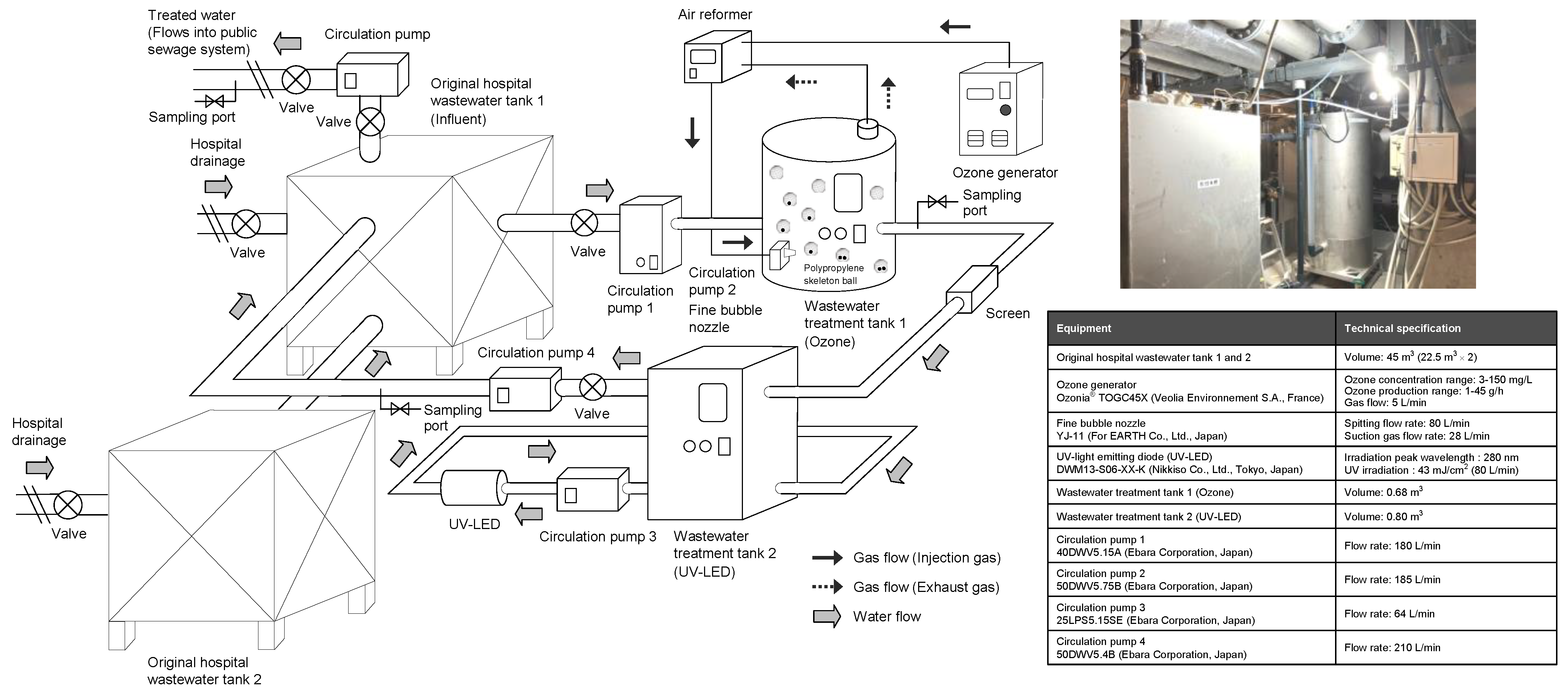
2.2. Hospital Wastewater Treatment by Ozone and UV with Continuous-Flow System
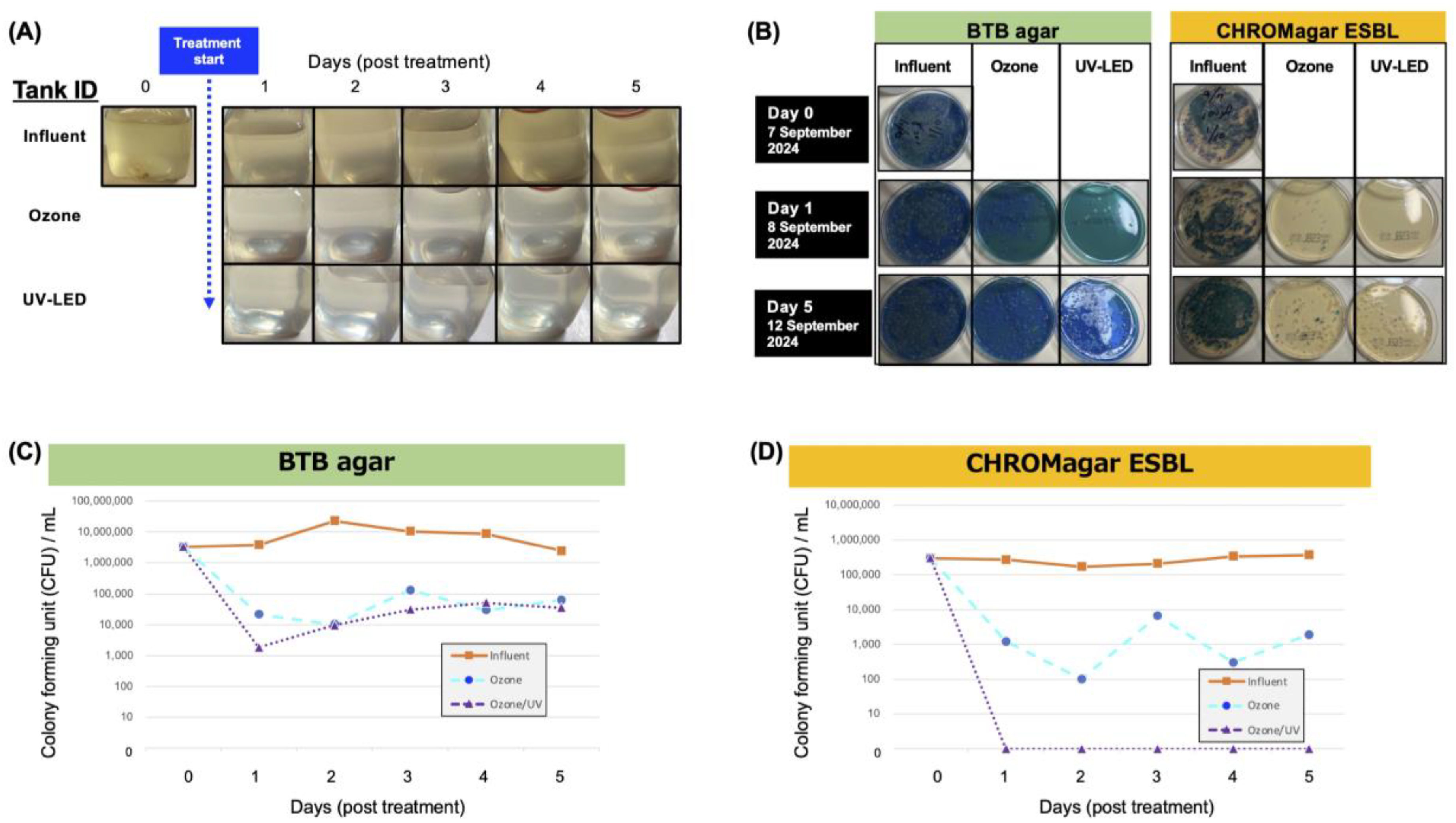
2.3. Viable Bacterial Counting of Wastewater Samples
2.4. Metagenomic DNA-Seq Analysis of Wastewater Samples
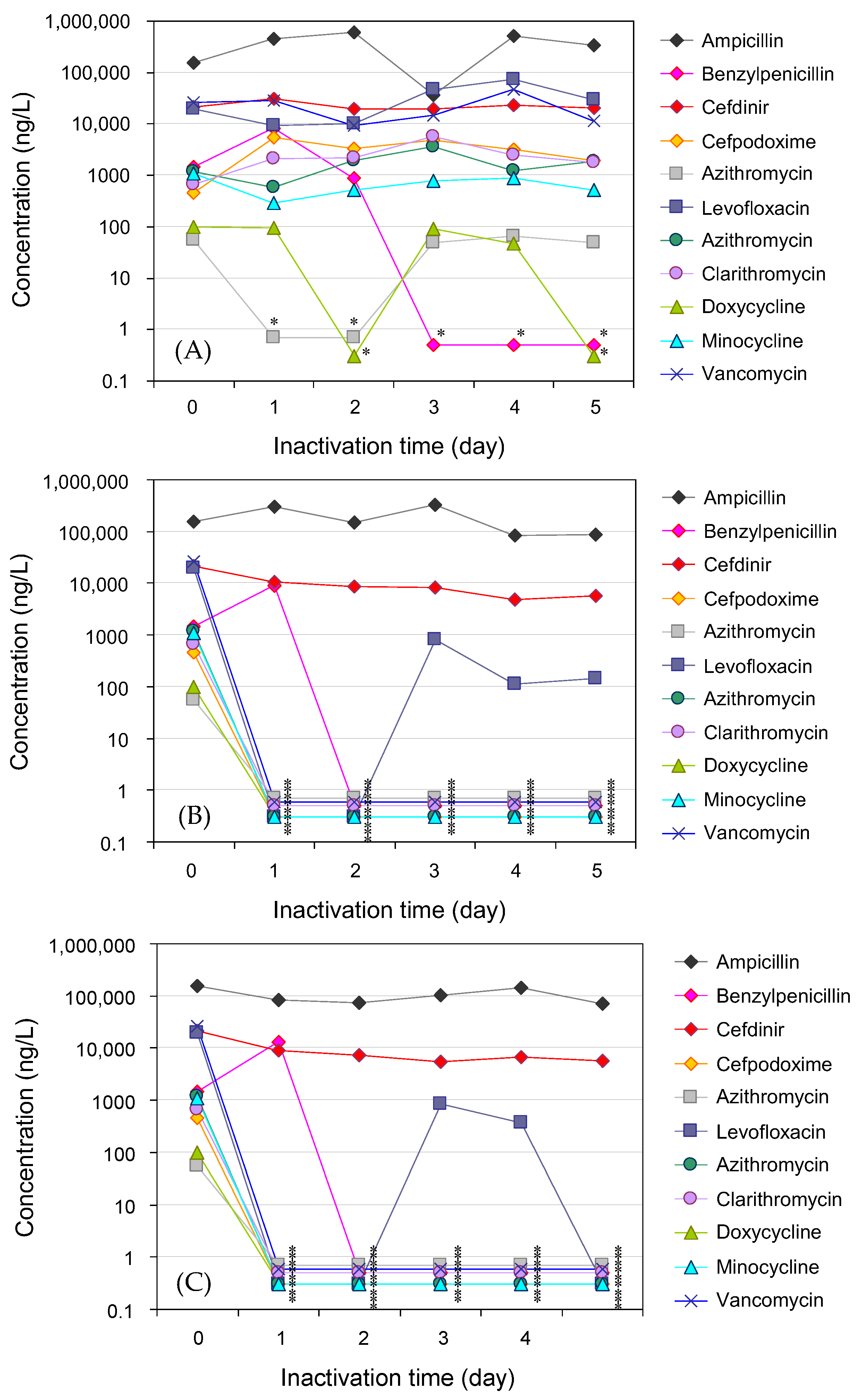
2.5. Antimicrobial Analysis in Hospital Wastewater Samples
3. Results
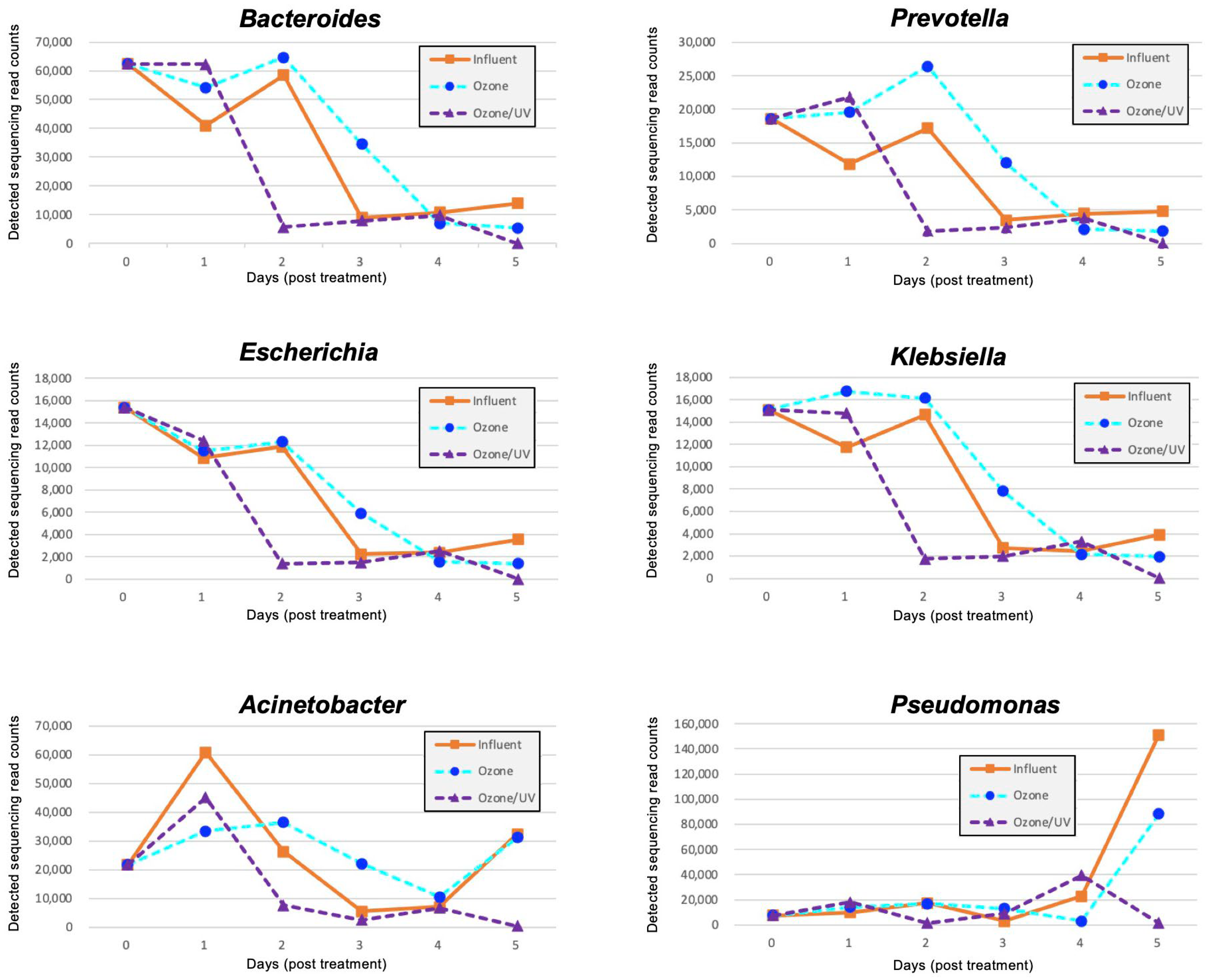
3.1. Proportion of Bacteria in Hospital Wastewater
3.2. Resistome Analysis in Hospital Wastewater
3.3. Removal of Antimicrobials in Hospital Wastewater
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jim, O.N. Tackling drug-resistant infections globally: Final report and recommendations. Rev. Antimicrob. Resist. 2016, 1–80. [Google Scholar]
- Murray, C.J.L.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Robles Aguilar, G.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef] [PubMed]
- Naghavi, M.; Vollset, S.E.; Ikuta, K.S.; Swetschinski, L.R.; Gray, A.P.; Wool, E.E.; Robles Aguilar, G.; Mestrovic, T.; Smith, G.; Han, C.; et al. Global burden of bacterial antimicrobial resistance 1990–2021: A systematic analysis with forecasts to 2050. Lancet 2024, 404, 1199–1226. [Google Scholar] [CrossRef] [PubMed]
- Siri, Y.; Precha, N.; Sirikanchana, K.; Haramoto, E.; Makkaew, P. Antimicrobial resistance in southeast asian water environments: A systematic review of current evidence and future research directions. Sci. Total Environ. 2023, 896, 165229. [Google Scholar] [CrossRef] [PubMed]
- Larsson, D.G.J.; Flach, C.F. Antibiotic resistance in the environment. Nat. Rev. Microbiol. 2022, 20, 257–269. [Google Scholar] [CrossRef]
- Calero-Cáceres, W.; de Almeida Kumlien, A.C.M.; Balcázar, J.L. Advances and challenges in assessing antimicrobial resistance in environmental settings. Curr. Opin. Environ. Sci. Health 2024, 41, 100571. [Google Scholar] [CrossRef]
- Feng, G.; Huang, H.; Chen, Y. Effects of emerging pollutants on the occurrence and transfer of antibiotic resistance genes: A review. J. Hazard. Mater. 2021, 420, 126602. [Google Scholar] [CrossRef]
- Wang, Y.; Han, Y.; Li, L.; Liu, J.; Yan, X. Distribution, sources, and potential risks of antibiotic resistance genes in wastewater treatment plant: A review. Environ. Pollut. 2022, 310, 119870. [Google Scholar] [CrossRef]
- Goh, S.G.; Haller, L.; Ng, C.; Charles, F.R.; Jitxin, L.; Chen, H.; He, Y.; Gin, K.Y.H. Assessing the additional health burden of antibiotic resistant enterobacteriaceae in surface waters through an integrated QMRA and DALY approach. J. Hazard. Mater. 2023, 458, 132058. [Google Scholar] [CrossRef]
- Thibodeau, A.J.; Barret, M.; Mouchet, F.; Nguyen, V.X.; Pinelli, E. The potential contribution of aquatic wildlife to antibiotic resistance dissemination in freshwater ecosystems: A review. Environ. Pollut. 2024, 350, 123894. [Google Scholar] [CrossRef]
- Herraiz-Carboné, M.; Cotillas, S.; Lacasa, E.; Sainz de Baranda, C.; Riquelme, E.; Cañizares, P.; Rodrigo, M.A.; Sáez, C. A review on disinfection technologies for controlling the antibiotic resistance spread. Sci. Total Environ. 2021, 797, 149150. [Google Scholar] [CrossRef]
- Pant, A.; Shahadat, M.; Ali, S.W.; Ahammad, S.Z. Removal of antimicrobial resistance from secondary treated wastewater—A review. J. Hazard. Mater. Adv. 2022, 8, 100189. [Google Scholar] [CrossRef]
- Foroughi, M.; Arzehgar, A.; Seyedhasani, S.N.; Nadali, A.; Zoroufchi Benis, K. Application of machine learning for antibiotic resistance in water and wastewater: A systematic review. Chemosphere 2024, 358, 142223. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Global Action Plan on Antimicrobial Resistance Resistance; World Health Organization: Geneva, Switzerland, 2015; pp. 1–19. [Google Scholar]
- Willemsen, A.; Reid, S.; Assefa, Y. A review of national action plans on antimicrobial resistance: Strengths and weaknesses. Antimicrob. Resist. Infect. Control 2022, 11, 90. [Google Scholar] [CrossRef]
- Dias, M.F.; da Rocha Fernandes, G.; Cristina de Paiva, M.; Christina de Matos Salim, A.; Santos, A.B.; Amaral Nascimento, A.M. Exploring the resistome, virulome and microbiome of drinking water in environmental and clinical settings. Water Res. 2020, 174, 115630. [Google Scholar] [CrossRef] [PubMed]
- Cui, C.Y.; Li, X.J.; Chen, C.; Wu, X.T.; He, Q.; Jia, Q.L.; Zhang, X.J.; Lin, Z.Y.; Li, C.; Fang, L.X.; et al. Comprehensive analysis of plasmid-mediated tet(X4)-positive Escherichia coli isolates from clinical settings revealed a high correlation with animals and environments-derived strains. Sci. Total Environ. 2022, 806, 150687. [Google Scholar] [CrossRef]
- Li, Y.; Li, R.; Hou, J.; Sun, X.; Wang, Y.; Li, L.; Yang, F.; Yao, Y.; An, Y. Mobile genetic elements affect the dissemination of antibiotic resistance genes (ARGs) of clinical importance in the environment. Environ. Res. 2024, 243, 117801. [Google Scholar] [CrossRef] [PubMed]
- Savin, M.; Sib, E.; Heinemann, C.; Eichel, V.M.; Nurjadi, D.; Klose, M.; Andre Hammerl, J.; Binsker, U.; Mutters, N.T. Tracing clinically-relevant antimicrobial resistances in Acinetobacter baumannii-calcoaceticus complex across diverse environments: A study spanning clinical, livestock, and wastewater treatment settings. Environ. Int. 2024, 186, 108603. [Google Scholar] [CrossRef]
- Sekizuka, T.; Inamine, Y.; Segawa, T.; Kuroda, M. Characterization of NDM-5- and CTX-M-55-coproducing Escherichia coli GSH8M-2 isolated from the effluent of a wastewater treatment plant in Tokyo Bay. Infect. Drug Resist. 2019, 12, 2243–2249. [Google Scholar] [CrossRef]
- Sekizuka, T.; Itokawa, K.; Tanaka, R.; Hashino, M.; Yatsu, K.; Kuroda, M. Metagenomic analysis of urban wastewater treatment plant effluents in Tokyo. Infect. Drug Resist. 2022, 15, 4763–4777. [Google Scholar] [CrossRef]
- Sekizuka, T.; Tanaka, R.; Hashino, M.; Yatsu, K.; Kuroda, M. Comprehensive genome and plasmidome analysis of antimicrobial resistant bacteria in wastewater treatment plant effluent of Tokyo. Antibiotics 2022, 11, 1283. [Google Scholar] [CrossRef]
- Fatimazahra, S.; Latifa, M.; Laila, S.; Monsif, K. Review of hospital effluents: Special emphasis on characterization, impact, and treatment of pollutants and antibiotic resistance. Environ. Monit. Assess. 2023, 195, 393. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Yuan, L.; Shuai, X.Y.; Lin, Z.J.; Sun, Y.J.; Zhou, Z.C.; Meng, L.X.; Ju, F.; Chen, H. Deciphering basic and key traits of antibiotic resistome in influent and effluent of hospital wastewater treatment systems. Water Res. 2023, 231, 119614. [Google Scholar] [CrossRef]
- Męcik, M.; Stefaniak, K.; Harnisz, M.; Korzeniewska, E. Hospital and municipal wastewater as a source of carbapenem-resistant Acinetobacter baumannii and Pseudomonas aeruginosa in the environment: A review. Environ. Sci. Pollut. Res. 2024, 31, 48813–48838. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.T.; Shah, I.A.; Ihsanullah, I.; Naushad, M.; Ali, S.; Shah, S.H.A.; Mohammad, A.W. Hospital wastewater as a source of environmental contamination: An overview of management practices, environmental risks, and treatment processes. J. Water Proc. Eng. 2021, 41, 101990. [Google Scholar] [CrossRef]
- Verlicchi, P. Trends, new insights and perspectives in the treatment of hospital effluents. Curr. Opin. Environ. Sci. Health 2021, 19, 100217. [Google Scholar] [CrossRef]
- Zou, H.; Zhou, Z.; Berglund, B.; Zheng, B.; Meng, M.; Zhao, L.; Zhang, H.; Wang, Z.; Wu, T.; Li, Q.; et al. Persistent transmission of carbapenem-resistant, hypervirulent Klebsiella pneumoniae between a hospital and urban aquatic environments. Water Res. 2023, 242, 120263. [Google Scholar] [CrossRef]
- Weissbrodt, D.; Kovalova, L.; Ort, C.; Pazhepurackel, V.; Moser, R.; Hollender, J.; Siegrist, H.; McArdell, C.S. Mass flows of X-ray contrast media and cytostatics in hospital wastewater. Environ. Sci. Technol. 2009, 43, 4810–4817. [Google Scholar] [CrossRef]
- Santos, L.H.M.L.M.; Gros, M.; Rodriguez-Mozaz, S.; Delerue-Matos, C.; Pena, A.; Barceló, D.; Montenegro, M.C.B.S.M. Contribution of hospital effluents to the load of pharmaceuticals in urban wastewaters: Identification of ecologically relevant pharmaceuticals. Sci. Total Environ. 2013, 461–462, 302–316. [Google Scholar] [CrossRef]
- Aydin, S.; Aydin, M.E.; Ulvi, A.; Kilic, H. Antibiotics in hospital effluents: Occurrence, contribution to urban wastewater, removal in a wastewater treatment plant, and environmental risk assessment. Environmen. Sci. Pollut. Res. 2019, 26, 544–558. [Google Scholar] [CrossRef]
- Afsa, S.; Hamden, K.; Lara Martin, P.A.; Mansour, H.B. Occurrence of 40 pharmaceutically active compounds in hospital and urban wastewaters and their contribution to mahdia coastal seawater contamination. Environ. Sci. Pollut. Res. 2020, 27, 1941–1955. [Google Scholar] [CrossRef]
- Xu, C.; Hu, C.; Li, F.; Liu, W.; Xu, Y.; Shi, D. Antibiotic resistance genes risks in relation to host pathogenicity and mobility in a typical hospital wastewater treatment process. Environ. Res. 2024, 259, 119554. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Bou, L.; Rosa-Masegosa, A.; Vilchez-Vargas, R.; Link, A.; Gonzalez-Martinez, A.; Gonzalez-Lopez, J.; Muñoz-Palazon, B. Treatment of hospital wastewater using aerobic granular sludge technology: Removal performance and microbial dynamics. J. Water Proc. Eng. 2024, 60, 105206. [Google Scholar] [CrossRef]
- Xu, C.; Zhang, Y.; Hu, C.; Shen, C.; Li, F.; Xu, Y.; Liu, W.; Shi, D. From disinfection to pathogenicity: Occurrence, resistome risks and assembly mechanism of biocide and metal resistance genes in hospital wastewaters. Environ. Pollut. 2024, 349, 123910. [Google Scholar] [CrossRef] [PubMed]
- Vorontsov, A.V. Advancing fenton and photo-Fenton water treatment through the catalyst design. J. Hazard. Mater. 2019, 372, 103–112. [Google Scholar] [CrossRef]
- Ahmed, Y.; Zhong, J.; Yuan, Z.; Guo, J. Simultaneous removal of antibiotic resistant bacteria, antibiotic resistance genes, and micropollutants by a modified photo-Fenton process. Water Res. 2021, 197, 117075. [Google Scholar] [CrossRef]
- Yang, S.Q.; Cui, Y.H.; Li, J.Y.; Lv, X.D.; Liu, Z.Q. Determination methods for steady-state concentrations of HO• and SO4•− in electrochemical advanced oxidation processes. Chemosphere 2020, 261, 127658. [Google Scholar] [CrossRef]
- Di Paola, A.; García-López, E.; Marcì, G.; Palmisano, L. A survey of photocatalytic materials for environmental remediation. J. Hazard. Mater. 2012, 211–212, 3–29. [Google Scholar] [CrossRef]
- Zhang, R.; Wang, X.; Zhou, L.; Liu, Z.; Crump, D. The impact of dissolved oxygen on sulfate radical-induced oxidation of organic micro-pollutants: A theoretical study. Water Res. 2018, 135, 144–154. [Google Scholar] [CrossRef]
- Chan, P.Y.; Gamal El-Din, M.; Bolton, J.R. A solar-driven UV/Chlorine advanced oxidation process. Water Res. 2012, 46, 5672–5682. [Google Scholar] [CrossRef]
- Yu, G.; Wang, Y.; Cao, H.; Zhao, H.; Xie, Y. Reactive oxygen species and catalytic active sites in heterogeneous catalytic ozonation for water purification. Environ. Sci. Technol. 2020, 54, 5931–5946. [Google Scholar] [CrossRef]
- Loeb, B.L. Forty years of advances in ozone technology. A review of Ozone: Science & Engineering. Ozone Sci. Eng. 2018, 40, 3–20. [Google Scholar]
- Rekhate, C.V.; Srivastava, J.K. Recent advances in ozone-based advanced oxidation processes for treatment of wastewater—A review. Chem. Eng. J. Adv. 2020, 3, 100031. [Google Scholar] [CrossRef]
- Lim, S.; Shi, J.L.; von Gunten, U.; McCurry, D.L. Ozonation of organic compounds in water and wastewater: A critical review. Water Res. 2022, 213, 118053. [Google Scholar] [CrossRef] [PubMed]
- Aleksić, S.; Žgajnar Gotvajn, A.; Premzl, K.; Kolar, M.; Turk, S.Š. Ozonation of amoxicillin and ciprofloxacin in model hospital wastewater to increase biotreatability. Antibiotics 2021, 10, 1407. [Google Scholar] [CrossRef]
- Azuma, T.; Hayashi, T. Disinfection of antibiotic-resistant bacteria in sewage and hospital effluent by ozonation. Ozone Sci. Eng. 2021, 43, 413–426. [Google Scholar] [CrossRef]
- Czekalski, N.; Imminger, S.; Salhi, E.; Veljkovic, M.; Kleffel, K.; Drissner, D.; Hammes, F.; Bürgmann, H.; von Gunten, U. Inactivation of antibiotic resistant bacteria and resistance genes by ozone: From laboratory experiments to full-scale wastewater treatment. Environ. Sci. Technol. 2016, 50, 11862–11871. [Google Scholar] [CrossRef]
- Basturk, I.; Varank, G.; Murat-Hocaoglu, S.; Yazici-Guvenc, S.; Oktem-Olgun, E.E.; Canli, O. Characterization and treatment of medical laboratory wastewater by ozonation: Optimization of toxicity removal by central composite design. Ozone Sci. Eng. 2021, 43, 213–227. [Google Scholar] [CrossRef]
- Simazaki, D.; Kubota, R.; Suzuki, T.; Akiba, M.; Nishimura, T.; Kunikane, S. Occurrence of selected pharmaceuticals at drinking water purification plants in japan and implications for human health. Water Res. 2015, 76, 187–200. [Google Scholar] [CrossRef]
- Japan Sewage Works Association. Statistics of Sewerage; Japan Sewage Works Association: Tokyo, Japan, 2024. (In Japanese) [Google Scholar]
- Azuma, T.; Usui, M.; Hayashi, T. Inactivation of antibiotic-resistant bacteria in wastewater by ozone-based advanced water treatment processes. Antibiotics 2022, 11, 210. [Google Scholar] [CrossRef]
- Azuma, T.; Katagiri, M.; Sasaki, N.; Kuroda, M.; Watanabe, M. Performance of a pilot-scale continuous flow ozone-based hospital wastewater treatment system. Antibiotics 2023, 12, 932. [Google Scholar] [CrossRef]
- Rajabi, A.; Farajzadeh, D.; Dehghanzadeh, R.; Aslani, H.; Mosaferi, M.; Mousavi, S.; Shanehbandi, D.; Asghari, F.B. Optimizing ozone dose and contact time for removal of antibiotic-resistant P. aeruginosa, A. baumannii, E. coli, and associated resistant genes in effluent of an activated sludge process in a municipal WWTP. Environ. Sci. Pollut. Res. 2023, 30, 55569–55581. [Google Scholar] [CrossRef]
- Zhang, X.Y.; Liu, T.S.; Hu, J.Y. Antibiotics removal and antimicrobial resistance control by ozone/peroxymonosulfate-biological activated carbon: A novel treatment process. Water Res. 2024, 261, 122069. [Google Scholar] [CrossRef]
- Yamada, S.; Amano, T.; Minagawa, H. A study for distribution of microbubbles and effects of oxygen supplying into water. Trans. Jpn. Soc. Mech. Eng. B 2005, 71, 1301–1306. [Google Scholar] [CrossRef]
- Hashimoto, K.; Kubota, N.; Okuda, T.; Nakai, S.; Nishijima, W.; Motoshige, H. Reduction of ozone dosage by using ozone in ultrafine bubbles to reduce sludge volume. Chemosphere 2021, 274, 129922. [Google Scholar] [CrossRef] [PubMed]
- Yin, X.; Jiang, X.T.; Chai, B.; Li, L.; Yang, Y.; Cole, J.R.; Tiedje, J.M.; Zhang, T. ARGs-OAP v2.0 with an expanded sarg database and hidden markov models for enhancement characterization and quantification of antibiotic resistance genes in environmental metagenomes. Bioinformatics 2018, 34, 2263–2270. [Google Scholar] [CrossRef] [PubMed]
- Yin, X.; Zheng, X.; Li, L.; Zhang, A.N.; Jiang, X.T.; Zhang, T. ARGs-OAP v3.0: Antibiotic-resistance gene database curation and analysis pipeline optimization. Engineering 2023, 27, 234–241. [Google Scholar] [CrossRef]
- Chaturvedi, P.; Shukla, P.; Giri, B.S.; Chowdhary, P.; Chandra, R.; Gupta, P.; Pandey, A. Prevalence and hazardous impact of pharmaceutical and personal care products and antibiotics in environment: A review on emerging contaminants. Environ. Res. 2021, 194, 110664. [Google Scholar] [CrossRef]
- Wang, J.; Xu, S.; Zhao, K.; Song, G.; Zhao, S.; Liu, R. Risk control of antibiotics, antibiotic resistance genes (ARGs) and antibiotic resistant bacteria (ARB) during sewage sludge treatment and disposal: A review. Sci. Total Environ. 2023, 877, 162772. [Google Scholar] [CrossRef]
- Ministry of Health Labour and Welfare (Japan). Ministry of Health Labour and Welfare, Japan. Japan Nosocomial Infections Surveillance (JANIS), Nosocomial Infections Surveillance for Antimicrobial-Resistant Bacteria. Available online: https://janis.mhlw.go.jp/english/index.asp (accessed on 17 July 2025).
- Ministry of Health Labour and Welfare (Japan). Annual Report on Statistics of Production by Pharmaceutical Industry in 2021. Available online: https://www.mhlw.go.jp/toukei/list/105-1.html (accessed on 17 July 2025). (In Japanese).
- Azuma, T.; Nakano, T.; Koizumi, R.; Matsunaga, N.; Ohmagari, N.; Hayashi, T. Evaluation of the correspondence between the concentration of antimicrobials entering sewage treatment plant influent and the predicted concentration of antimicrobials using annual sales, shipping, and prescriptions data. Antibiotics 2022, 11, 472. [Google Scholar] [CrossRef]
- Azuma, T.; Usui, M.; Hayashi, T. Inactivation of antibiotic-resistant bacteria in hospital wastewater by ozone-based advanced water treatment processes. Sci. Total Environ. 2024, 906, 167432. [Google Scholar] [CrossRef]
- Daughton, C.G. Pharmaceuticals and the Environment (PIE): Evolution and impact of the published literature revealed by bibliometric analysis. Sci. Total Environ. 2016, 562, 391–426. [Google Scholar] [CrossRef] [PubMed]
- Kim, L.; Lee, D.; Cho, H.K.; Choi, S.D. Review of the quechers method for the analysis of organic pollutants: Persistent organic pollutants, polycyclic aromatic hydrocarbons, and pharmaceuticals. Trends Environ. Anal. Chem. 2019, 22, e00063. [Google Scholar] [CrossRef]
- Oliveira, T.S.; Murphy, M.; Mendola, N.; Wong, V.; Carlson, D.; Waring, L. Characterization of pharmaceuticals and personal care products in hospital effluent and waste water influent/effluent by direct-injection LC-MS-MS. Sci. Total Environ. 2015, 518–519, 459–478. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M.; Tang, S.; Bao, Y.; Daniels, K.D.; How, Z.T.; El-Din, M.G.; Wang, J.; Tang, L. Fully-automated SPE coupled to uhplc-ms/ms method for multiresidue analysis of 26 trace antibiotics in environmental waters: SPE optimization and method validation. Environ. Sci. Pollut. Res. 2022, 29, 16973–16987. [Google Scholar] [CrossRef]
- Petrović, M.; Škrbić, B.; Živančev, J.; Ferrando-Climent, L.; Barcelo, D. Determination of 81 pharmaceutical drugs by high performance liquid chromatography coupled to mass spectrometry with hybrid triple quadrupole-linear ion trap in different types of water in serbia. Sci. Total Environ. 2014, 468–469, 415–428. [Google Scholar] [CrossRef]
- Wu, D.; Sui, Q.; Yu, X.; Zhao, W.; Li, Q.; Fatta-Kassinos, D.; Lyu, S. Identification of indicator PPCPs in landfill leachates and livestock wastewaters using multi-residue analysis of 70 PPCPs: Analytical method development and application in Yangtze River Delta, China. Sci. Total Environ. 2021, 753, 141653. [Google Scholar] [CrossRef]
- Azuma, T.; Otomo, K.; Kunitou, M.; Shimizu, M.; Hosomaru, K.; Mikata, S.; Ishida, M.; Hisamatsu, K.; Yunoki, A.; Mino, Y.; et al. Environmental fate of pharmaceutical compounds and antimicrobial-resistant bacteria in hospital effluents, and contributions to pollutant loads in the surface waters in japan. Sci. Total Environ. 2019, 657, 476–484. [Google Scholar] [CrossRef]
- Liu, J.; Ge, S.; Shao, P.; Wang, J.; Liu, Y.; Wei, W.; He, C.; Zhang, L. Occurrence and removal rate of typical pharmaceuticals and personal care products (PPCPs) in an urban wastewater treatment plant in Beijing, China. Chemosphere 2023, 339, 139644. [Google Scholar] [CrossRef]
- Heida, A.; Hamilton, M.T.; Gambino, J.; Sanderson, K.; Schoen, M.E.; Jahne, M.A.; Garland, J.; Ramirez, L.; Quon, H.; Lopatkin, A.J.; et al. Population ecology-quantitative microbial risk assessment (QMRA) model for antibiotic-resistant and susceptible E. coli in recreational water. Environ. Sci. Technol. 2025, 59, 4266–4281. [Google Scholar] [CrossRef]
- Wan, W.D.; Ma, J.X.; Lai, T.N.; Yan, Y.T.; Ali, W.; Hu, Z.; Li, X.; Tang, Z.R.; Wang, C.Y.; Yan, C. Quantitative microbial risk assessment for on-site employees in a wastewater treatment plant and implicated surrounding residents exposed to S. aureus bioaerosols. Environ. Pollut. 2025, 371, 125892. [Google Scholar] [CrossRef]
- Yuan, S.; Jin, G.; Cui, R.; Wang, X.; Wang, M.; Chen, Z. Transmission and control strategies of antimicrobial resistance from the environment to the clinic: A holistic review. Sci. Total Environ. 2024, 957, 177461. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Wang, B.; Wang, T.; Li, J.; Qi, J.; Luo, J.; Zhang, T.; Xu, X.; Hou, L.A. A review of antibiotic resistance genes in major river basins in china: Distribution, drivers, and risk. Environ. Pollut. 2025, 371, 125920. [Google Scholar] [CrossRef] [PubMed]
- Zheng, W.; Huyan, J.; Tian, Z.; Zhang, Y.; Wen, X. Clinical class 1 integron-integrase gene—A promising indicator to monitor the abundance and elimination of antibiotic resistance genes in an urban wastewater treatment plant. Environ. Int. 2020, 135, 105372. [Google Scholar] [CrossRef] [PubMed]
- Corno, G.; Ghaly, T.; Sabatino, R.; Eckert, E.M.; Galafassi, S.; Gillings, M.R.; Di Cesare, A. Class 1 integron and related antimicrobial resistance gene dynamics along a complex freshwater system affected by different anthropogenic pressures. Environ. Pollut. 2023, 316, 120601. [Google Scholar] [CrossRef]
- Sangwan, N.; Ahmed, Y.M.; Blatchley, E.R. III. Dose distribution scaling and validation of ultraviolet photoreactors using dimensional analysis. Environ. Sci. Technol. 2023, 57, 16707–16717. [Google Scholar] [CrossRef]
- Sun, W.; Ao, X.; Lu, D.; Zhang, Y.; Xue, Y.; He, S.; Zhang, X.; Mao, T. Ultraviolet technology application in urban water supply and wastewater treatment in china: Issues, challenges and future directions. Water Res. X 2024, 23, 100225. [Google Scholar] [CrossRef]
- Saravanan, A.; Deivayanai, V.C.; Kumar, P.S.; Rangasamy, G.; Hemavathy, R.V.; Harshana, T.; Gayathri, N.; Alagumalai, K. A detailed review on advanced oxidation process in treatment of wastewater: Mechanism, challenges and future outlook. Chemosphere 2022, 308, 136524. [Google Scholar] [CrossRef]
- Martín-Sómer, M.; Pablos, C.; Adán, C.; van Grieken, R.; Marugán, J. A review on led technology in water photodisinfection. Sci. Total Environ. 2023, 885, 163963. [Google Scholar] [CrossRef]
- Norte, T.H.d.O.; Marcelino, R.B.P.; Medeiros, F.H.A.; Moreira, R.P.L.; Amorim, C.C.; Lago, R.M. Ozone oxidation of β-lactam antibiotic molecules and toxicity decrease in aqueous solution and industrial wastewaters heavily contaminated. Ozone Sci. Eng. 2018, 40, 385–391. [Google Scholar] [CrossRef]
- Tufail, A.; Price, W.E.; Mohseni, M.; Pramanik, B.K.; Hai, F.I. A critical review of advanced oxidation processes for emerging trace organic contaminant degradation: Mechanisms, factors, degradation products, and effluent toxicity. J. Water Proc. Eng. 2021, 40, 101778. [Google Scholar] [CrossRef]
- Ike, I.A.; Karanfil, T.; Cho, J.; Hur, J. Oxidation byproducts from the degradation of dissolved organic matter by advanced oxidation processes—A critical review. Water Res. 2019, 164, 114929. [Google Scholar] [CrossRef] [PubMed]
- Tufail, A.; Price, W.E.; Hai, F.I. A critical review on advanced oxidation processes for the removal of trace organic contaminants: A voyage from individual to integrated processes. Chemosphere 2020, 260, 127460. [Google Scholar] [CrossRef] [PubMed]
- Magdeburg, A.; Stalter, D.; Oehlmann, J. Whole effluent toxicity assessment at a wastewater treatment plant upgraded with a full-scale post-ozonation using aquatic key species. Chemosphere 2012, 88, 1008–1014. [Google Scholar] [CrossRef]
- Díaz-Garduño, B.; Pintado-Herrera, M.G.; Biel-Maeso, M.; Rueda-Márquez, J.J.; Lara-Martín, P.A.; Perales, J.A.; Manzano, M.A.; Garrido-Pérez, C.; Martín-Díaz, M.L. Environmental risk assessment of effluents as a whole emerging contaminant: Efficiency of alternative tertiary treatments for wastewater depuration. Water Res. 2017, 119, 136–149. [Google Scholar] [CrossRef]
- Loeb, B.L. Ozone: A valuable tool for addressing today’s environmental issues. A review of forty-five years of Ozone: Science & Engineering. Ozone Sci. Eng. 2024, 46, 2–25. [Google Scholar]
- Zhang, H.; Li, S.; Zhang, C.; Ren, X.; Zhou, M. A critical review of ozone-based electrochemical advanced oxidation processes for water treatment: Fundamentals, stability evaluation, and application. Chemosphere 2024, 365, 143330. [Google Scholar] [CrossRef]
- Liang, J.; Fei, Y.; Yin, Y.; Han, Q.; Liu, Y.; Feng, L.; Zhang, L. Advancements in wastewater treatment: A comprehensive review of ozone microbubbles technology. Environ. Res. 2025, 266, 120469. [Google Scholar] [CrossRef]
- Ministry of the Environment (Japan). Energy Consumption in the Home in 2022. Available online: https://www.env.go.jp/earth/ondanka/kateico2tokei/energy/detail/01/ (accessed on 17 July 2025). (In Japanese).
- Khilar, R.; Suba, G.M.; Kumar, T.S.; Samson Isaac, J.; Shinde, S.K.; Ramya, S.; Prabhu, V.; Erko, K.G. Improving the efficiency of photovoltaic panels using machine learning approach. Int. J. Photoener. 2022, 2022, 4921153. [Google Scholar] [CrossRef]
- Divya, A.; Adish, T.; Kaustubh, P.; Zade, P.S. Review on recycling of solar modules/panels. Sol. Ener. Mater. Sol. Cells 2023, 253, 112151. [Google Scholar] [CrossRef]
- Amin, N.; Foster, T.; Shimki, N.T.; Willetts, J. Hospital wastewater (HWW) treatment in low- and middle-income countries: A systematic review of microbial treatment efficacy. Sci. Total Environ. 2024, 921, 170994. [Google Scholar] [CrossRef]
- Silvester, R.; Perry, W.B.; Webster, G.; Rushton, L.; Baldwin, A.; Pass, D.A.; Byrnes, N.A.; Farkas, K.; Heginbothom, M.; Craine, N.; et al. Metagenomic profiling of hospital wastewater: A comprehensive national scale analysis of antimicrobial resistance genes and opportunistic pathogens. J. Infect. 2025, 90, 106503. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Li, J.; Lai, J.; Zhang, Q.; Zhao, Z.; Li, B. Transfer dynamics of intracellular and extracellular last-resort antibiotic resistome in hospital wastewater. Water Res. 2025, 283, 123833. [Google Scholar] [CrossRef]
- The Ministry of Health, Labour and Welfare (MHLW). National Action Plan on Antimicrobial Resistance (AMR) (2016–2020); The Government of Japan: Tokyo, Japan, 2016; pp. 1–69. [Google Scholar]
- The Ministry of Health, Labour and Welfare (MHLW). National Action Plan on Antimicrobial Resistance (AMR) (2023–2027); The Government of Japan: Tokyo, Japan, 2023; pp. 1–90. [Google Scholar]
- Ajala, O.J.; Tijani, J.O.; Salau, R.B.; Abdulkareem, A.S.; Aremu, O.S. A review of emerging micro-pollutants in hospital wastewater: Environmental fate and remediation options. Results Eng. 2022, 16, 100671. [Google Scholar] [CrossRef]
- Bhandari, G.; Chaudhary, P.; Gangola, S.; Gupta, S.; Gupta, A.; Rafatullah, M.; Chen, S. A review on hospital wastewater treatment technologies: Current management practices and future prospects. J. Water Proc. Eng. 2023, 56, 104516. [Google Scholar] [CrossRef]
- Amaya-Santos, G.; Boelee, N.; Paulillo, A.; Lettieri, P. Life cycle assessment and life cycle costing of full-scale ozonation for micropollutants removal from wastewater. Case Study in the Netherlands. Sci. Total Environ. 2025, 961, 178259. [Google Scholar] [CrossRef] [PubMed]
| Tank ID | Days (Post Treatment) | Total ARGs | Detected RPM (Reads Per Million) of Antimicrobial Resistance Genes (ARGs) by ARGs_OAP Search * | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sulfonamide sul1 | Sulfonamide sul2 | Multidrug qacEdelta1 | β-Lactam GES-15 | β-Lactam GES-20 | β-Lactam OXA-1 | Aminoglycoside AAC(6′)-31 | Aminoglycoside aadS | Aminoglycoside APH(3″)-Ib | Aminoglycoside APH(6)-Id | Tetracycline tet(36) | Tetracycline tet(Q) | |||
| Original storage tank (Influent) | 0 | 2598 | 315 | 42 | 181 | 228 | 41 | 137 | 130 | 72 | 40 | 65 | 70 | 60 |
| 1 | 2527 | 396 | 32 | 76 | 137 | 15 | 80 | 216 | 76 | 76 | 0 | 103 | 34 | |
| 2 | 2723 | 333 | 52 | 187 | 237 | 44 | 81 | 99 | 12 | 24 | 6 | 53 | 42 | |
| 3 | 2241 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 379 | 0 | 158 | 158 | |
| 4 | 811 | 281 | 0 | 0 | 0 | 0 | 0 | 470 | 0 | 0 | 0 | 0 | 0 | |
| 5 | 1066 | 471 | 0 | 0 | 0 | 0 | 0 | 234 | 0 | 0 | 0 | 0 | 0 | |
| Wastewater treatment tank 1 (ozone) | 0 | 2598 | 315 | 42 | 181 | 228 | 41 | 137 | 130 | 72 | 40 | 65 | 70 | 60 |
| 1 | 2701 | 340 | 13 | 62 | 124 | 25 | 331 | 99 | 12 | 75 | 129 | 50 | 50 | |
| 2 | 2821 | 480 | 16 | 263 | 226 | 30 | 103 | 47 | 60 | 69 | 33 | 67 | 40 | |
| 3 | 3529 | 803 | 0 | 275 | 221 | 0 | 311 | 172 | 0 | 313 | 114 | 99 | 49 | |
| 4 | 6330 | 944 | 0 | 2980 | 398 | 0 | 0 | 0 | 0 | 428 | 0 | 0 | 0 | |
| 5 | 1561 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Wastewater treatment tank 2 (UV-LED) | 0 | 2598 | 315 | 42 | 181 | 228 | 41 | 137 | 130 | 72 | 40 | 65 | 70 | 60 |
| 1 | 2270 | 196 | 0 | 70 | 310 | 0 | 136 | 89 | 14 | 65 | 44 | 32 | 82 | |
| 2 | 2075 | 1754 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 3 | 3055 | 554 | 0 | 0 | 1077 | 0 | 1345 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 4 | 760 | 0 | 321 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Classification | Antimicrobials | Inactivation Time (day) | |||||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | ||
| (A) | |||||||
| β-lactams | Ampicillin | 157,128 | 462,024 | 614,340 | 37,108 | 525,180 | 337,424 |
| Benzylpenicillin | 1454 | 8402 | 871 | N.D. | N.D. | N.D. | |
| Cefdinir | 21,138 | 30,469 | 19,496 | 19,659 | 23,451 | 20,793 | |
| Cefpodoxime | 466 | 5551 | 3293 | 4865 | 3223 | 1929 | |
| Cefpodoxime proxetil | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Ceftiofur | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| New quinolones | Ciprofloxacin | 57 | N.D. | N.D. | 49 | 65 | 49 |
| Enrofloxacin | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Levofloxacin | 19,404 | 9250 | 10,096 | 47,668 | 74,311 | 30,386 | |
| Macrolides | Azithromycin | 1178 | 579 | 1925 | 3575 | 1245 | 1871 |
| Clarithromycin | 676 | 2087 | 2190 | 5689 | 2453 | 1792 | |
| Tetracyclines | Chlortetracycline | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. |
| Doxycycline | 101 | 96 | N.D. | 92 | 48 | N.D. | |
| Minocycline | 1077 | 293 | 522 | 793 | 893 | 516 | |
| Oxytetracycline | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Tetracycline | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Glycopeptides | Vancomycin | 26,587 | 28,503 | 9563 | 14,733 | 46,503 | 11,753 |
| (B) | |||||||
| β-lactams | Ampicillin | 157,128 | 297,428 | 148,632 | 329,932 | 84,192 | 87,156 |
| Benzylpenicillin | 1454 | 9098 | N.D. | N.D. | N.D. | N.D. | |
| Cefdinir | 21,138 | 10,644 | 8701 | 8234 | 4874 | 5662 | |
| Cefpodoxime | 466 | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Cefpodoxime proxetil | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Ceftiofur | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| New quinolones | Ciprofloxacin | 57 | N.D. | N.D. | N.D. | N.D. | N.D. |
| Enrofloxacin | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Levofloxacin | 19,404 | N.D. | N.D. | 832 | 114 | 144 | |
| Macrolides | Azithromycin | 1178 | N.D. | N.D. | N.D. | N.D. | N.D. |
| Clarithromycin | 676 | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Tetracyclines | Chlortetracycline | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. |
| Doxycycline | 101 | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Minocycline | 1077 | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Oxytetracycline | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Tetracycline | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Glycopeptides | Vancomycin | 26,587 | N.D. | N.D. | N.D. | N.D. | N.D. |
| (C) | |||||||
| β-lactams | Ampicillin | 157,128 | 85,295 | 75,486 | 104,616 | 144,181 | 71,242 |
| Benzylpenicillin | 1454 | 12,853 | N.D. | N.D. | N.D. | N.D. | |
| Cefdinir | 21,138 | 9179 | 7220 | 5449 | 6747 | 5592 | |
| Cefpodoxime | 466 | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Cefpodoxime proxetil | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Ceftiofur | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| New quinolones | Ciprofloxacin | 57 | N.D. | N.D. | N.D. | N.D. | N.D. |
| Enrofloxacin | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Levofloxacin | 19,404 | N.D. | N.D. | 865 | 371 | N.D. | |
| Macrolides | Azithromycin | 1178 | N.D. | N.D. | N.D. | N.D. | N.D. |
| Clarithromycin | 676 | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Tetracyclines | Chlortetracycline | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. |
| Doxycycline | 101 | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Minocycline | 1077 | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Oxytetracycline | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Tetracycline | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| Glycopeptides | Vancomycin | 26,587 | N.D. | N.D. | N.D. | N.D. | N.D. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Azuma, T.; Katagiri, M.; Yamamoto, T.; Kuroda, M.; Watanabe, M. Effectiveness of Implementing Hospital Wastewater Treatment Systems as a Measure to Mitigate the Microbial and Antimicrobial Burden on the Environment. Antibiotics 2025, 14, 807. https://doi.org/10.3390/antibiotics14080807
Azuma T, Katagiri M, Yamamoto T, Kuroda M, Watanabe M. Effectiveness of Implementing Hospital Wastewater Treatment Systems as a Measure to Mitigate the Microbial and Antimicrobial Burden on the Environment. Antibiotics. 2025; 14(8):807. https://doi.org/10.3390/antibiotics14080807
Chicago/Turabian StyleAzuma, Takashi, Miwa Katagiri, Takatoshi Yamamoto, Makoto Kuroda, and Manabu Watanabe. 2025. "Effectiveness of Implementing Hospital Wastewater Treatment Systems as a Measure to Mitigate the Microbial and Antimicrobial Burden on the Environment" Antibiotics 14, no. 8: 807. https://doi.org/10.3390/antibiotics14080807
APA StyleAzuma, T., Katagiri, M., Yamamoto, T., Kuroda, M., & Watanabe, M. (2025). Effectiveness of Implementing Hospital Wastewater Treatment Systems as a Measure to Mitigate the Microbial and Antimicrobial Burden on the Environment. Antibiotics, 14(8), 807. https://doi.org/10.3390/antibiotics14080807







