Abstract
Mycoplasma genitalium is recognized as a remarkable pathogen since azithromycin-resistant strains and treatment failure have been increasingly reported. Nevertheless, international guidelines still recommend azithromycin as a first-line treatment and moxifloxacin as a second-line treatment. We performed a systematic review and meta-analysis to validate the efficacy and safety of both drugs in the initial treatment of M. genitalium. We systematically searched the EMBASE, PubMed, Scopus, Ichushi, and CINAHL databases up to December 2021. We defined efficacy as clinical and microbiologic cure, and safety as persistent diarrhea. Overall, four studies met the inclusion criteria: one showed clinical cure (azithromycin treatment, n = 32; moxifloxacin treatment, n = 6), four showed microbiologic cure (n = 516; n = 99), and one showed safety (n = 63; n = 84). Moxifloxacin improved the microbiologic cure rate compared with azithromycin (odds ratio [OR] 2.79, 95% confidence interval [CI], 1.06–7.35). Clinical cure and safety did not show a significant difference between azithromycin and moxifloxacin treatments (OR 4.51, 95% CI 0.23–88.3; OR 0.63, 95% CI 0.21–1.83). Our meta-analysis showed that moxifloxacin was more effective than azithromycin at eradicating M. genitalium infections and supports its preferential use as a first-line treatment.
1. Introduction
Mycoplasma genitalium is a small bacterium belonging to the Mycoplasmataceae family and is implicated in the etiology of nongonococcal urethritis in men and cervicitis in women [1,2,3]. Although the prevalence of M. genitalium in a general population-based study of young adults is low (1%) [4], its prevalence in sexual health clinics is substantially higher, ranging from 10% to 20% [5,6,7]. Since M. genitalium does not have peptidoglycan-containing cell walls, treatment options are limited to antibiotics that disrupt protein synthesis (macrolides such as azithromycin, and tetracyclines such as doxycycline) or DNA replication (quinolones such as moxifloxacin). Clinical trials reported superior efficacy of azithromycin with a failure rate of 16% compared with doxycycline [8]. Moreover, it has been reported that the efficacy of moxifloxacin in patients with azithromycin treatment failure was 100%, with high in vitro susceptibility [9]. Therefore, international guidelines recommend azithromycin as a first-line treatment and moxifloxacin as a second-line treatment [10,11]. However, resistance to both antibiotics and treatment failure have recently been reported.
The eradication of M. genitalium is hampered by increased antibiotic resistance. Besides intrinsic resistance to all β-lactams, macrolide resistance has been reported in over 50% of M. genitalium isolates from patients with urethritis and cervicitis in many countries [12,13,14]. Moreover, azithromycin treatment fails in at least 10% of susceptible isolates, leading to the selection of strains with macrolide resistance-associated mutations (MRMs) at positions 2058 or 2059 in the 23S ribosomal RNA gene [15,16]. Quinolones are used as alternative agents against treatment failure in patients treated with azithromycin. However, a meta-analysis showed a decrease in the cure rate for moxifloxacin from 100% in studies until 2010 to 89% in studies from 2010 onward [17].
The Centers for Disease Control and Prevention (CDC) have developed a watch list of bacteria that show antibiotic-resistant threats with the potential to spread or become a challenge in the United States [18] and M. genitalium is included as a public health issue on that list. However, antibiotic resistance associated with treatment failure with azithromycin and moxifloxacin has not been reflected in the treatment strategy. We performed a systematic review and meta-analysis to validate the efficacy and safety of azithromycin and moxifloxacin as initial treatments for M. genitalium infections.
2. Results
2.1. Systematic Review
Data extracted from the electronic databases retrieved 865 potentially relevant articles. After removing duplicates, the titles and abstracts of 795 articles were screened. A full-text review of 19 articles was performed. Figure 1 depicts a full list of reasons for exclusion. Consequently, four studies met the inclusion criteria [9,19,20,21].
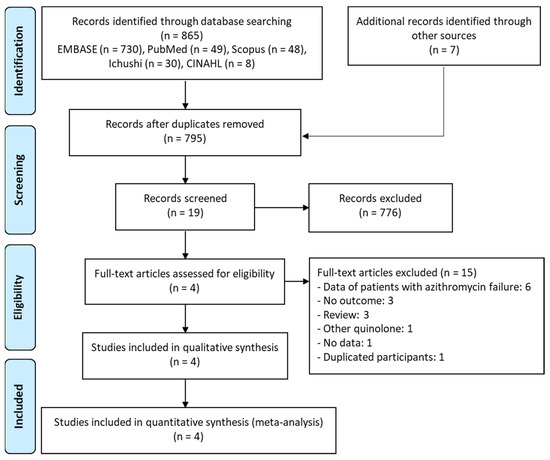
Figure 1.
PRISMA flow diagram for the selection of eligible studies.
The characteristics of these studies are summarized in Table 1. One was a case-control study and the others were cohort studies. All studies were conducted in a single center; two in Australia [9,21], one in Norway [19] and one in Japan [20]. All participants reported by Bradshaw [9] and Terada [20] were patients with urethritis and cervicitis, respectively. The participants reported by Jernberg [19] and Gundevia [21] were patients with either urethritis or cervicitis. Although three of the four studies were conducted among patients aged 15–57 years old [9,20,21], the other study did not report the age of the patients included [19]. The susceptibility of the isolated M. genitalium was not reported in the four studies included in this review. A total of 516 patients were treated with azithromycin, while 99 were treated with moxifloxacin. The dosage regimens of azithromycin were as follows: 1 g single dose; 1 g weekly for 3 doses; 1 g single dose day 1, repeated after 5–7 days; 500 mg single dose day 1, 250 mg single dose for the following 4 days, 2 g single dose, 1 g single dose day 1, 500 mg single dose for the following 4 days. The moxifloxacin dosage regimen was 400 mg every 24 h, and the treatment duration was 7–14 days. Assessment of the risk-of-bias is shown in Table 1. The Newcastle–Ottawa Quality Assessment Scale score was 6.

Table 1.
Characteristics of the studies included in the meta-analysis.
2.2. Meta-Analysis
2.2.1. Clinical Cure
One study reported clinical cure data of 32 patients treated with azithromycin and six patients treated with moxifloxacin [9]; the clinical cure rates in these two groups were 75% (24/32) and 100% (6/6), respectively. Moxifloxacin treatment did not improve the clinical cure rate compared with azithromycin treatment (OR 4.51, 95% CI 0.23–88.3).
2.2.2. Microbiologic Cure
Microbiologic cure data from 516 patients treated with azithromycin and 99 patients treated with moxifloxacin were reported in four studies [9,19,20,21]. The microbiologic cure rates in the two groups were 77.5% (400/516) and 94.9% (94/99), respectively. Moxifloxacin treatment significantly improved the microbiologic cure rate when compared to the azithromycin treatment (OR 2.79, 95% CI 1.06–7.35, I2 = 0%; Figure 2).

Figure 2.
Forest plot presenting odds ratios for microbiologic cure comparing azithromycin and moxifloxacin in patients with M. genitalium infection.
2.2.3. Safety
One study reported adverse events in 63 and 84 patients treated with azithromycin and moxifloxacin, respectively [20]. The incidence of adverse events was 12.7% (8/63) in patients treated with azithromycin and 8.3% (7/84) in those treated with moxifloxacin. The incidence of adverse events was not significantly different between the two antibiotic treatments (OR 0.63, 95% CI 0.21–1.83).
3. Discussion
A previous systematic review regarding the antibiotic susceptibility of M. genitalium and treatment efficacy of existing antibiotics has mentioned that moxifloxacin remains the most effective treatment despite the emergence of treatment failures and quinolone resistance [22]. However, most studies included in the review reported the efficacy of moxifloxacin treatment in patients who experienced azithromycin treatment failure. Therefore, we performed a meta-analysis to investigate the efficacy of azithromycin versus moxifloxacin as a first-line treatment for M. genitalium infection. Our meta-analysis showed superior microbiological cure rate in patients treated with moxifloxacin compared with patients treated with azithromycin. Moreover, all patients treated with moxifloxacin improved clinical cure, whereas 15% of patients treated with azithromycin did not improve clinical cure. Consequently, our findings indicated that moxifloxacin was a more effective first-line treatment for eradicating M. genitalium than azithromycin.
The eradication rate of M. genitalium from a single dose of 1 g azithromycin seems to decrease over time [23]. To date, there have been discussions about the most suitable dosing regimen of azithromycin for microbiologic cure in patients with M. genitalium infection. Previous studies reported that the eradication rate of M. genitalium in patients administered various dosing regimens of azithromycin showed no statistically significant difference between azithromycin 1 g in a single dose and other dosing regimens [19,20,21]. Hence, various azithromycin dosing regimens have been prescribed for the treatment of M. genitalium infections. Recently, a meta-analysis that reported the prevalence of mutations associated with resistance to macrolides in M. genitalium reported that the prevalence was significantly greater in the Americas than in the European region [24]. A conceivable cause is that the recommended dosing regimen based on treatment guidelines for M. genitalium is not standardized or optimized [3,25]. Therefore, global measures to optimize the efficacy of antibiotic treatments are urgently needed to prevent the further spread of macrolide-resistant strains.
A recent meta-analysis revealed that the prevalence of azithromycin-resistant M. genitalium increased from 10% before 2010 to 51% in 2016–2017, while that of moxifloxacin-resistant M. genitalium with parC (quinolone resistance-associated mutation, QRM) was 8% and did not change over time [24]. Among patients diagnosed with M. genitalium infection in 2017–2018, 64.4% had 23S ribosomal ribonucleic acid (rRNA) loci (MRMs), 11.5% had parC, and 0% had gyrA (QRM) [26]. The minimum inhibitory concentration (MIC) of azithromycin against all M. genitalium isolates with MRMs was over 8 mg/L [27,28]. According to these data, MRMs could contribute to increasing the MIC of azithromycin. Therefore, careful consideration of its use as a first-line treatment for M. genitalium infections is warranted. On the other hand, MICs of moxifloxacin against M. genitalium isolates with either parC, gyrA, or a mixture of both were 0.03–0.5 mg/L but adding MRMs to M. genitalium isolates with both QRMs led to moxifloxacin-resistant strains with MICs of over 2 mg/L [28]. Therefore, a single mutation in QRMs might not influence an increase in the MIC of moxifloxacin in M. genitalium. However, the correlation between parC and/or gyrA and moxifloxacin resistance is unclear because of limited data from cultured M. genitalium.
To date, two meta-analyses reported microbiological cure rates for infections due to M. genitalium [17,29]. According to the meta-analyses, the pooled microbiological cure rate of azithromycin was 67%, whereas that of moxifloxacin was 96%. In subgroup analyses of moxifloxacin, the pooled microbial cure rates for the initial use of moxifloxacin and the use of moxifloxacin after antibiotic treatment failure were 99% and 94%, respectively [29]. In the light of our findings, moxifloxacin can be effective as a first-line treatment as well as a second-line treatment for M. genitalium infections.
To our knowledge, this is the first meta-analysis to compare the efficacy and safety of azithromycin and moxifloxacin in patients with M. genitalium infections. However, our meta-analysis had several limitations. First, the number of studies included in our meta-analysis was relatively low and lacked information regarding patient backgrounds; therefore, subgroup analyses on various types of confounding factors, such as type of infection, susceptibility (mutation), and dosing regimen were not performed. Moreover, our meta-analysis only included single-center retrospective studies which might have increased the likelihood of reporting and selection bias. However, there was no heterogeneity (I2 = 0%) in the present study. Second, whether azithromycin and moxifloxacin were appropriate for the patients in the included studies was unclear because the results of susceptibility testing with the detected isolates were not reported. Indeed, culturing M. genitalium is difficult and is only performed in a few facilities worldwide. Finally, moxifloxacin cannot be prescribed for patients with M. genitalium infection in Japan because this antibiotic is only allowed to treat respiratory infections and skin and soft tissue infections. Instead, sitafloxacin, which is of the same generation as quinolone as moxifloxacin, is one of the standard treatments for M. genitalium infection in Japan. However, few studies have compared patients treated with azithromycin with those treated with sitafloxacin as a first-line treatment for M. genitalium.
4. Materials and Methods
4.1. Data Sources and Search Strategy
This study was performed in accordance with the PRISMA guidelines (Supplementary Material Table S1), except for the protocol registration on reporting systematic reviews and meta-analyses [30,31]. The following PICO criteria were used to select relevant studies: population (P), patients with M. genitalium infection; intervention (I), patients treated with azithromycin; comparison (C), patients treated with moxifloxacin; and outcome (O), efficacy and safety. All studies were identified through a systematic review of the EMBASE, PubMed, Scopus, Ichushi, and CINAHL databases until 1 December 2021, using the following terms: “Mycoplasma genitalium, macrolide, quinolone, urethritis,” and cervicitis.” Language restrictions were applied, except for English and Japanese.
4.2. Study Selection
Two authors independently reviewed articles based on titles and abstracts and then assessed the full-text articles. The full texts of eligible articles were reviewed to apply the inclusion criteria and identify articles for the final qualitative synthesis and meta-analysis. Any disagreement was resolved through discussion or based on the judgement of the third author (HM).
4.3. Eligibility Criteria
Studies that met the following criteria were extracted: (i) randomized controlled trials (RCTs), retrospective observational or cohort studies; (ii) patients diagnosed with urethritis or cervicitis infected with M. genitalium; and (iii) patients receiving azithromycin or moxifloxacin treatment. Studies reporting the efficacy of moxifloxacin for azithromycin treatment failure were excluded. No restrictions were placed on the antibiotic regimen or duration of antibiotic treatment. We evaluated the clinical cure, microbiologic cure, and safety of patients treated with azithromycin or moxifloxacin. A clinical cure was defined as the absence of signs and/or symptoms related to M. genitalium infection. A microbiologic cure was defined as a case when there was an absence of M. genitalium DNA or RNA after polymerase chain reaction (PCR) or transcription-mediated amplification of a urine sample, urethral or cervical swab, or biopsy specimen. The safety outcome was defined as the presence or absence of persistent diarrhea.
4.4. Data Extraction and Risk-of-Bias Assessment
The following data were extracted: study design, setting, period, country of study, drug regimen, number of participants, age, type of infection, antibiotic susceptibility, and clinical outcome. The risk-of-bias was assessed using the Newcastle–Ottawa Quality Assessment tool for retrospective studies [32]. This scale consists of nine items assessing different study characteristics such as selection, comparability, and exposure. Two authors independently assessed the risk-of-bias.
4.5. Statistical Analysis
Our meta-analysis using Review Manager (RevMan, version 5.4; Nordic Cochrane StataCorp LLC, College Station, TX, USA) was performed according to a previous study [33]. Statistical heterogeneity between studies was evaluated using the chi-squared test. A p-value < 0.1 indicated significant heterogeneity. I2 represents the degree of heterogeneity (0–25%, low heterogeneity; 25–50%, moderate heterogeneity; 50–75%, substantial heterogeneity; and 75–100%, considerable heterogeneity). Heterogeneity was regarded as significant when p < 0.1, or I2 > 50%. A random-effects model was applied if the data were heterogeneous. In the other cases, a fixed-effects model was applied. The risk of clinical outcomes was calculated using odds ratios (ORs) and 95% confidence intervals (Cis) were calculated. The pooled Ors and 95% Cis were calculated using the fixed-effects and random-effects models, respectively, and the Ors from the results were compared.
5. Conclusions
In conclusion, our meta-analysis showed that moxifloxacin improved the microbiologic cure rate. The findings of this meta-analysis have provided evidence that azithromycin may be less effective than moxifloxacin in treating M. genitalium infection, whereas current guidelines recommend its use as a first-line treatment. However, national and international surveillance of antibiotic resistance in M. genitalium is needed to prevent the spread of moxifloxacin-resistant M. genitalium by inappropriate use of moxifloxacin. In the future, new treatment strategies, such as the development of novel antibiotics and antibiotic combination therapies, should be considered.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/antibiotics11030353/s1, Table S1: PRISMA 2020 Checklist.
Author Contributions
Conceptualization, H.K. and H.M.; methodology, H.K. and M.H.; software, H.K.; validation, N.A. and J.H.; formal analysis, H.K. and M.H.; investigation, H.K. and M.H.; resources, H.K. and N.A.; data curation, H.K. and N.A.; writing—original draft preparation, H.K.; writing—review and editing, M.H., N.A., J.H., Y.Y., T.I., and H.M.; visualization, H.K. and M.H.; supervision, H.M.; project administration, H.K.; funding acquisition, H.M. All authors have read and agreed to the published version of the manuscript.
Funding
None of the authors have financial relationships with any commercial entity with an interest in the subject of this manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data are applicable in the paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Horner, P.J.; Gilroy, C.B.; Thomas, B.J.; Naidoo, R.O.; Taylor-Robinson, D. Association of Mycoplasma genitalium with acute non-gonococcal urethritis. Lancet 1993, 342, 582–585. [Google Scholar] [CrossRef]
- Jensen, J.S.; Orsum, R.; Dohn, B.; Uldum, S.; Worm, A.M.; Lind, K. Mycoplasma genitalium: A cause of male urethritis? Genitourin. Med. 1993, 69, 265–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manhart, L.E.; Critchlow, C.W.; Holmes, K.K.; Dutro, S.M.; Eschenbach, D.A.; Stevens, C.E.; Totten, P.A. Mucopurulent cervicitis and Mycoplasma genitalium and acute endometritis. Lancet 2003, 187, 650–657. [Google Scholar]
- Manhart, L.E.; Holmes, K.K.; Hughes, J.P.; Houston, L.S.; Totten, P.A. Mycoplasma genitalium among young adults in the United States: An emerging sexually transmitted infection. Am. J. Public Health 2007, 97, 1118–1125. [Google Scholar] [CrossRef]
- Sena, A.C.; Lee, J.Y.; Schwebke, J.; Philip, S.S.; Wiesenfeld, H.C.; Rompalo, A.M.; Cook, R.L.; Hobbs, M.M. A silent epidemic: The prevalence, incidence and persistence of Mycoplasma genitalium among young, asymptomatic high-risk women in the United States. Clin. Infect. Dis. 2018, 67, 73–79. [Google Scholar] [CrossRef]
- Baumann, L.; Cina, M.; Egli-Gany, D.; Goutaki, M.; Halbeisen, F.S.; Lohrer, G.-R.; Ali, H.; Scott, P.; Low, N. Prevalence of Mycoplasma genitalium in different population groups: Systematic review and meta-analysis. Sex. Transm. Infect. 2018, 94, 255–262. [Google Scholar] [CrossRef] [Green Version]
- Totten, P.A.; Schwartz, M.A.; Sjosstrom, K.E.; Kenny, G.E.; Handsfield, H.H.; Weiss, J.B.; Whittington, W.L. Association of Mycoplasma genitalium with nongonococcal urethritis in heterosexual men. J. Infect. Dis. 2001, 183, 269–276. [Google Scholar] [CrossRef] [Green Version]
- Mena, L.A.; Mroczkowski, T.F.; Nsuami, M.; Martin, D.H. A randomized comparison of azithromycin and doxycycline for the treatment of Mycoplasma genitalium-positive urethritis in men. Clin. Infect. Dis. 2009, 48, 1649–1654. [Google Scholar] [CrossRef] [Green Version]
- Bradshaw, C.S.; Jensen, J.S.; Tabrizi, S.N.; Read, T.R.H.; Garland, S.M.; Hopkins, C.A.; Moss, L.M.; Fairley, C.K. Azithromycin failure in Mycoplasma genitalium urethritis. Emerg. Infect. Dis. 2006, 12, 1149–1152. [Google Scholar] [CrossRef]
- Wright, A.; Grulich, A.; Roy, K.; Boyd, M.; Cornelisse, V.; Russell, D.; O’Donnell, D.; Whittaker, B.; Crooks, L.; Zablotska, I. Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine HIV pre-exposure prophylaxis: Clinical guidelines. J. Virus Erad. 2017, 3, 168–184. [Google Scholar] [CrossRef]
- Jensen, J.S.; Cusini, M.; Gomberg, M.; Moi, H. 2016 European guideline on Mycoplasma genitalium infections. J. Eur. Acad. Dermatol. Venereol. 2016, 30, 1650–1656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jensen, J.S.; Bradshaw, C.S.; Tabrizi, S.N.; Fairley, C.K.; Hamasuna, R. Azithromycin treatment failure in Mycoplasma genitalium-positive patients with nongonococcal urethritis is associated with induced macrolide resistance. Clin. Infect. Dis. 2008, 47, 1546–1553. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gratrix, J.; Plitt, S.; Turnbull, L.; Smyczek, P.; Brandley, J.; Scarrott, R.; Naidu, P.; Parker, P.; Blore, B.; Bull, A.; et al. Prevalence and antibiotic resistance of Mycoplasma genitalium among STI clinic attendees in Western Canada: A cross-sectional analysis. BMJ Open 2017, 7, e016300. [Google Scholar] [CrossRef]
- Read, T.R.H.; Fairley, C.K.; Tabrizi, S.N.; Bissessor, M.; Lenka, V.; Chow, E.P.F.; Grant, M.; Danielewski, J.; Garland, S.M.; Hocking, J.S.; et al. Azithromycin 1.5 g over 5 days compared to 1 g single dose in urethral Mycoplasma genitalium: Impact on treatment outcome and resistance. Clin. Infect. Dis. 2017, 64, 250–256. [Google Scholar] [CrossRef] [Green Version]
- Jensen, J.S.; Bradshaw, C. Management of Mycoplasma genitalium infections-can we hit a moving target? BMC Infect. Dis. 2015, 15, 343. [Google Scholar] [CrossRef] [Green Version]
- Horner, P.; Ingle, S.M.; Garrett, F.; Blee, K.; Kong, F.; Muir, P.; Moi, H. Which azithromycin regimen should be used for treating Mycoplasma genitalium? A meta-analysis. Sex. Trasm. Infect. 2018, 94, 14–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.; Le, W.J.; Li, S.; Cao, Y.P.; Su, X.H. Meta-analysis of the efficacy of moxifloxacin in treating Mycoplasma genitalium infection. Int. J. STD AIDS 2017, 28, 1106–1114. [Google Scholar] [CrossRef]
- US Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States; US Department of Health and Human Services: Atlanta, GA, USA, 2019. [Google Scholar]
- Jernberg, E.; Monghaddam, A.; Moi, H. Azithromycin and moxifloxacin for microbiological cure of Mycoplasma genitalium infection: An open study. Int. J. STD AIDS 2008, 19, 676–679. [Google Scholar] [CrossRef]
- Terada, M.; Izumi, K.; Ohki, E.; Yamagishi, Y.; Mikamo, H. Antimicrobial efficacies of several antibiotics against uterine cervicitis caused by Mycoplasma genitalium. J. Infect. Chemother. 2012, 18, 313–317. [Google Scholar] [CrossRef]
- Gundevia, Z.; Foster, R.; Jamil, M.S.; McNulty, A. Positivity at test of cure following first-line treatment for genital Mycoplasma genitalium: Follow-up of a clinical cohort. Sex. Transm. Infect. 2015, 91, 11–13. [Google Scholar] [CrossRef] [Green Version]
- Manhart, L.E.; Jensen, J.S.; Bradshaw, C.S.; Golden, M.R.; Martin, D.H. Efficacy of antimicrobial therapy for Mycoplasma genitalium infections. Clin. Infect. Dis. 2015, 61, S802–S817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manhart, L.E.; Gillespie, C.W.; Lowens, M.S.; Khosropour, C.M.; Colombara, D.V.; Golden, M.R.; Hakhu, N.R.; Thomas, K.K.; Hughes, J.P.; Jensen, N.L.; et al. Standard treatment regimens for nongonococcal urethritis have similar but declining cure rates: A randomized controlled trial. Clin. Infect. Dis. 2013, 56, 934–942. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Machalek, D.; Tao, Y.; Shilling, H.; Jensen, J.S.; Unemo, M.; Murray, G.; Chow, E.P.F.; Low, N.; Garland, S.M.; Vodstrcil, L.; et al. Prevalence of mutations associated with resistance to macrolides and fluoroquinolones in Mycoplasma genitalium: A systematic review and meta-analysis. Lancet Infect. Dis. 2020, 20, 1302–1314. [Google Scholar] [CrossRef]
- Workowski, K.A.; Bolan, G.A.; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm. Rep. 2016, 64, 1–137. [Google Scholar]
- Bachmann, L.H.; Kirkcaldy, R.D.; Geisler, W.M.; Wiesenfeld, H.C.; Manhart, L.E.; Taylor, S.N.; Sena, A.C.; McNeil, C.J.; Newman, L.; Myler, N.; et al. Prevalence of Mycoplasma genitalium infection, antimicrobial resistance mutations, and symptom resolution following treatment of urethritis. Clin. Infect. Dis. 2020, 71, e624–e632. [Google Scholar] [CrossRef] [Green Version]
- Wood, G.E.; Jensen, N.L.; Astete, S.; Jensen, J.S.; Kenny, G.E.; Khosropour, C.M.; Gillespie, C.W.; Manhart, L.; Totten, P.A. Azithromycin and doxycycline resistance profiles of U.S. Mycoplasma genitalium strains and their association with treatment outcomes. J. Clin. Microbiol. 2021, 59, e0081921. [Google Scholar] [CrossRef]
- Hamasuna, R.; Le, P.T.; Kutsuna, S.; Furubayashi, K.; Matsumoto, M.; Ohmagari, N.; Fujimoto, N.; Matsumoto, T.; Jensen, J.S. Mutations in ParC and GyrA of moxifloxacin-resistant and susceptible Mycoplasma genitalium strains. PLoS ONE 2018, 13, e0198355. [Google Scholar]
- Lau, A.; Bradshaw, C.S.; Lewis, D.; Fairley, C.K.; Chen, M.Y.; Kong, F.Y.S.; Hocking, J.S. The efficacy of azithromycin for the treatment of genital Mycoplasma genitalium: A systematic review and meta-analysis. Clin. Infect. Dis. 2015, 61, 1389–1399. [Google Scholar] [CrossRef] [Green Version]
- The Guidelines of Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) Statement. Available online: http://prisma-statement.org (accessed on 1 December 2021).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Wells, G.A.; Shea, B.; Paterson, J. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. 2000. Available online: http://www.ohri.ca/Programs/clinical_epidemiology/default.asp (accessed on 20 January 2022).
- Kato, H.; Hagihara, M.; Asai, N.; Shibata, Y.; Yamagishi, Y.; Iwamoto, T.; Mikamo, H. A systematic review and meta-analysis of decontamination methods to prevent hospital environmental contamination and transmission of Clostridioides difficile. Anaerobe 2021, 73, 102478. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).