Abstract
Modern healthcare research has only in recent years investigated the impact of health care workers’ religious and other moral values on medical practice, interaction with patients, and ethically complex decision-making. Thus far, no international data exist on the way such values vary across different countries. We therefore established the NERSH International Collaboration on Values in Medicine with datasets on physician religious characteristics and values based on the same survey instrument. The present article provides (a) an overview of the development of the original and optimized survey instruments, (b) an overview of the content of the NERSH data pool at this stage and (c) a brief review of insights gained from articles published with the questionnaire. The questionnaire was developed in 2002, after extensive pretesting in the United States and subsequently translated from English into other languages using forward-backward translations with Face Validations. In 2013, representatives of several national research groups came together and worked at optimizing the survey instrument for future use on the basis of the existing datasets. Research groups were identified through personal contacts with researchers requesting to use the instrument, as well as through two literature searches. Data were assembled in Stata and synchronized for their comparability using a matched intersection design based on the items in the original questionnaire. With a few optimizations and added modules appropriate for cultures more secular than that of the United States, the survey instrument holds promise as a tool for future comparative analyses. The pool at this stage consists of data from eleven studies conducted by research teams in nine different countries over six continents with responses from more than 6000 health professionals. Inspection of data between groups suggests large differences in religious and other moral values across nations and cultures, and that these values account for differences in health professional’s clinical practices.
1. Introduction
This article describes the development, contents, and first cross national comparisons based on an international research tool, first developed in 2002 and executed in 2003 with subsequent publications [1,2,3,4,5,6,7,8,9,10], translated into seven languages [11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28] and optimized in 2013. The data document the impact of Health Professionals’ (HPs’) religious and secular beliefs and values on the clinical encounter.
Research publications on the relationship between religion, spirituality and health have increased significantly over recent years. This is evident by simple searches on Medline using the search words Religion (understood as the communal convictions and practices believers engage in as they search for the sacred) and especially Spirituality (mostly referring to the interior life individuals experience in their search for the sacred, not ruling out fellowship with other believers), and a number of journals have been dedicated to the study of the relationship between Spirituality and Health. Various articles have been dedicated to the conceptualization of religion, spirituality and faith (abbreviated R/S in this article) [29,30,31].
Historically, most religions include substantial reflection on the nexus of spirituality, health and suffering. This holds for Christianity as well. Thus, Amanda Porterfield describes how Christianity historically focused on disease through spiritual resources and practices, but also through altruistically motivated care for sufferers, which contributed significantly to the growth of Christianity in Roman times and throughout Western history. Indeed, modern health care has historical roots in the Christian vision of active charity that in Western Monasteries saw significant scientific and organizational anchoring [32].
Still today, many countries know nurses as sisters (a title for nuns) and numerous hospitals are still attached to and draw inspiration from monastic orders. A recent Lancet Series on Faith-Based Health Care focused on how faith institutions continue to have tremendous importance in third world countries [33]. In modern times, a stronger emphasis on scientific approaches to medicine has led to relatively little appreciation of religion within institutionalized health care. In part this has reflected broader critiques of religion in the works of positivists such as Auguste Comte and among clinicians such as Sigmund Freud, who saw religion as “universal compulsory neurosis”, “infantile helplessness” and “regression to primary narcissism” [34,35]. Within health care, R/S orientations and resources of patients often have been relegated to the private sphere, although substantial research indicates that when sick, people are most likely to care about existential, spiritual and religious questions [36].
Not surprisingly, then, modern healthcare research has only seen limited interest in the impact of HPs’ personal values and their impact on the medical practice, the interaction with patients, and ethically complex decision-making. To date no scientific reviews have been published on the impact of spirituality on medical practice.
Things have started to change with Farr Curlin and colleagues developing the survey Religion and Spirituality in Medicine: Physicians’ Perspectives (RSMPP 2002) in 2002. After administering this questionnaire to a representative sample of more than 1100 US physicians, the researchers published a series of papers describing their findings [1,2,3,4,5,6,7,8,9,10]. After translation into other languages, the RSMPP has so far led to the publication of ten other research articles [11,12,13,14,15,16,17,18,19,20] and eight theses [21,22,23,24,25,26,27,28]. Curlin and colleagues went on to develop other questionnaires focusing on specific aspects of health care, leading to more than 32 further publications [37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66]. However, other researchers introduced various changes to the original questionnaire which complicated comparisons across different studies. Therefore, we established the NERSH International Collaboration on Values in Medicine to discuss these different versions and finally to consent the “core” elements of the questionnaire battery, and to add further items or to specify some phrasings.
The NERSH collaboration on Values in Medicine is hosted by the Board of the Network for Research in Spirituality and Health (NERSH—www.nersh.org). In 2011, the Board members met at the founding seminar of Internationale Gesellschaft für Gesundheit und Spiritualität (www.iggs-online.org) in Munich and later as members of the editorial board of Spiritual Care—Zeitschrift für Spiritualität in den Gesundheitsberufen (Journal of Spirituality in Health Care—http://www.degruyter.com/view/j/spircare) and who had collaborated variously in the Scandinavian Network for Faith and Health (www.faith-health.org), and the European Network of Research on Religion, Spirituality and Health (http://www.fisg.ch). Baumann, Büssing and Hvidt were subsequently granted fellowships as an Interdisciplinary Research Group (IRG) at the German Freiburg Institute for Advanced Studies (FRIAS) from October 2012 to March 2014 with the aim of improving research based attention to spiritual needs and challenges of patients (esp. with chronic diseases), relatives and HPs who care for them [67,68,69]. Like Eckhard Frick, they had started independently to conduct research involving the RSMPP in translated form [22,23,24,25,26] or other similar instruments for the measurement of HP values [70]. The shared interests came together at FRIAS.
Farr Curlin’s study was the first of its kind [1], and soon the NERSH founders discovered a lacuna in the international research community: Until now, no large-scale international comparisons exist to describe how HP values vary across different nations and cultures and how that potentially affects their professional life. Therefore, the NERSH International Collaboration on Values in Medicine was established with datasets on physician values from the research teams that used the RSMPP, covering eleven studies conducted by research teams in nine different countries over six continents. The present article is the first publication from this collaboration. It provides (1) an overview of the development of the original and optimized survey instruments; (2) an overview of the content of the NERSH data pool at this stage; (3) a brief overview of insights gained from individual articles published with the questionnaire until now.
2. Methods and Materials
2.1. Development of the RSMPP
The NERSH questionnaire mainly builds on the RSMPP questionnaire developed by Curlin et al. in 2002. It includes a number of sections:
- Physician perspectives on religion/spirituality (R/S) and health containing 50 items. The items were written by Curlin and colleagues after thorough review of relevant literature and data gathered from qualitative pilot interviews. Items were subsequently revised for clarity and cogency through multiple expert panel reviews [2].
- Religious Characteristics consisting of 21 questions based on existing religiosity measures: 3A Religious affiliation, 3B Intrinsic religiosity, 3C Frequency of religious service attendance, 3D Beliefs, 3E Spirituality vs. Religiosity, 3F Religious Coping [1], and
- Demographics containing 18 items.
Development of the RSMPP has been described in detail in prior publication [1].
2.2. International Translations and Validations of the RSMPP
International research teams translated the RSMPP using mainly forward-backward translations with Face Validations in the following years [11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28].
At Freiburg, Germany in December 2008–January 2009, Eunmi Lee and Klaus Baumann translated the primary parts of the RSMPP and added a few items they deemed appropriate for their setting. In Denmark Christian Balslev van Randwijk and Niels Christian Hvidt translated it into Danish in 2010 [28] with a few necessary adaptations to the Danish context. At Munich, Germany in 2010, Inga Wermuth and Andreas Schulze translated the RSMPP in its entirety, likewise; a few alterations were inspired by the Danish adaptations. Both slightly different German translations are now harmonized in one German version available at the NERSH.org—Tool-box. Nada A. AlYousefi translated it into Arabic in 2009, Giancarlo Lucchetti into Portuguese in 2010, Tryphon Mukwayakala into French in 2012, and Can Kuseyri into Turkish in 2015. In 2014, Eunmi Lee translated the Freiburg version into Korean.
2.3. Development of the NERSH Instrument
The establishment of the NERSH International Collaboration on Values in Medicine collaboration and the optimized NERSH instrument involved (1) two expert round table meetings six months apart at FRIAS with use of Nominal Group Technique (NGT) voting consensus procedure on items; and (2) internal reliability analyses (Cronbach’s Alpha) with some parts of the questionnaire.
2.3.1. Expert Round Table Meetings with NGT
The first meeting took place from 20–22 February 2013 and the second from 30 September to 1 October 2013.
US team representatives had sent beforehand a list of items that they had previously employed in questionnaires and worked particularly well, and that they deemed appropriate to include in the NERSH questionnaire. These were presented to participants beforehand and were part of a proposed updated (new) NERSH instrument.
Second, an adapted form of Nominal Group Technique (NGT) [71,72], a qualitative research method which enables researchers to gather information and opinions from experts was used. Initially, all items were reviewed in a round table discussion so that the purpose and functionality of all items were clearly present to all experts, recalling the use they had made of the items in their individual experience with the RSMPP. Then, all attending experts (n = 14) scored all items on a scale of zero (low appreciation) to three (high appreciation). Results were noted down on a flipchart and later transferred to a word document containing all items. Items that received an overall score lower than ten were excluded from the updated questionnaire.
It became clear that the original RSMPP included items from Koenig et al.’s DUREL (Duke Religiosity Index) five-item measure but had left out one item that was now reinserted. Furthermore, items the Freiburg group had benefited from using were added. Three scales by Büssing, appropriate for analyses in more secular culture (ASP [73,74] and SpREUK-15 [75,76]) were proposed as additional modules for future research. More items that were identified during the NGT-process as thematically related were grouped in leading to fewer overall questionnaire batteries (see Section 2.4 below).
Finally, it was decided to create a new acronym for the instrument, the future joint data pool and the collaboration itself as the RSMPP acronym was found difficult to remember and a new acronym was needed to indicate that the instrument was truly improved and the joint pool and collaboration constituted new initiatives.
2.3.2. Internal Reliability
On the basis of datasets obtained by then (Balslev, Curlin, Lee, Mukwaiakala, Wermuth), Büssing performed internal reliability analyses (Cronbach’s Alpha) with the aim of looking for topics in the questionnaire that had some quality with respect to internal congruence, also in view of identifying items that could be eliminated. However, as the basic questionnaire was primarily intended to collect opinions (survey), and not to measure and quantify specific attitudes, convictions and behaviors, only some topics were identified as being suitable as scales (see Appendix A).
The respective topics will be revalidated in future studies using the updated NERSH questionnaire.
2.3.3. Face Validation
Both the English and translated German versions of the NERSH questionnaire were tested for comprehension and clarity through Face Validation, interviewing HPs that had filled in the questionnaire. Adjustments were made both to the original English and the German version.
2.4. Characteristics of NERSH Questionnaire
The revised NERSH questionnaire now consists of the same sections as the original RSMPP but in different sequence and with some more items: (1) Demographics (10 items vs. originally 14 items); (2) Evaluation of Patient Values (19 items vs. 22 items); (3) Evaluation of HP’s Values (16 items vs. 12 items) with proposed added modules appropriate for research in secular cultures: ASP, SpREUK (see NERSH questionnaire in English and German, including version with highlighted differences between the RSMPP and the NERSH questionnaire in Supplementary Materials S1–S3). The reason why the updated and complemented NERSH questionnaire counts fewer items is that more items have now been grouped in thematically congruent batteries following the NGT rounds as mentioned above under Section 2.3.1.
Until now the NERSH questionnaire has been translated into German and Portuguese in 2015 with data available in the NERSH pool only in German until now.
2.5. Identification of Eligible Datasets for Inclusion in NERSH International Data Pool on Values in Medicine
Research groups that had used the RSMPP and updated NERSH questionnaire were identified in three ways:
2.5.1. Personal Contacts
Farr Curlin kept record of researchers who had requested permission to use the RSMPP and shared that information with the NERSH board.
2.5.2. Citation Search
In March 2016 Hvidt and Kørup conducted a citation search in Web of Science of articles that quoted any of the original articles published on the RSMPP (Appendix B). It led to a total of 316 hits. References were screened in the Review program Covidence by the second author. A total of 292 were identified as irrelevant, 24 scanned for possible relevance, and two studies emerged of which Curlin had no knowledge, one from Brazil, the other from Saudi Arabia. They had both used parts of Curlin’s questionnaire, mainly the sections on physician evaluation of spirituality among patients [12,13]. Hvidt contacted the authors who agreed to participate.
2.5.3. Systematic Search
In order to make sure that no studies had been overlooked, Hvidt and Kørup conducted a literature search in Medline, Embase, PsychInfo, Web of Science and Google Scholar. In Medline, for instance, the search string was the following: ((questionn * or survey * or cross-section * or national sample *) and (religious or religio * or spiritual * or religiosity)) adj3 (professional * or physician * or psychiatris * or doctor * or staff * or ((nurs * or medic *) adj3 professor *))).mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]. See the detailed search strings for the other databases in Appendix C.
The search yielded 1572 hits. Hvidt and Kørup each reviewed half of these references for eligibility. The search did not identify any further studies that had used the RSMPP for data collection.
2.6. Description of Pool of Data Harvested with Versions of the RSMPP and the NERSH Instruments
Data are collected in STATA and synchronized for their comparability using a matched intersection design based on the items in the original RSMPP questionnaire. Data are stored on a secure Stata Server at the Research Unit of General Practice at the University of Southern Denmark and can be made available to all upon request.
The international pool from the NERSH collaboration at the present (April 2016) consists of data from eleven studies conducted by research teams in nine different countries over six continents (see map—Figure 1 and overview of the International NERSH Data Pool in Appendix D). All datasets are based on the original RSMPP questionnaire developed by Farr Curlin in 2002, including 48 items on “Religion and Spirituality in Medicine”, and although minor alterations have been made by some of the researchers in order to optimize the tool for local settings, the primary items are included in all datasets.
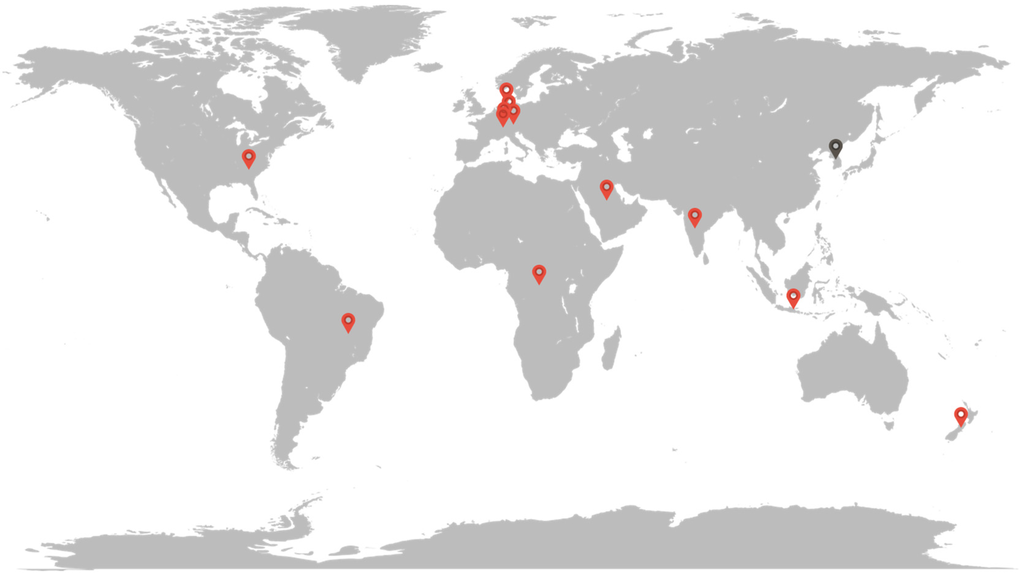
Figure 1.
Map showing the countries where the NERSH data has been collected. Red pins are samples included in the NERSH pool to date, grey pins are samples soon to be included in the pool.
In Curlin’s first data collection the RSMPP questionnaires was sent to a random sample of 2000 practicing U.S. Physicians with a response rate of 63%.
The first data collection using a translated version of the RSMPP was done by AlYousefi in 2009–2010. The Indonesian sample by Karimah was collected in 2010, and the Indian version was collected from 2010 to 2012 by Ramakrishnan. The Danish version was translated in 2009 but data was first collected in the years 2011–2012. Meanwhile in Freiburg, Germany, Baumann et al. collected their data using the German translation in 2008 (Pilot) and nationwide in 2011. The New Zealand, Congo and Brazil datasets were all collected entirely during 2012. Later, the nation-wide German sample by Wermuth et al. was collected over two years from 2013 to 2014. During 2014 a German sample related to transplantation medicine was performed as well as the Austrian sample of hospital workers in Salzburg. Last to be collected into the pool in 2016 were the Turkish sample of physicians working in Germany and the Swiss Sample of practitioners working outside the hospital. Data from a recent data collection from South Korea will be added in the near future.
Currently, some datasets are still in process of completion and will be added in the near future; this preliminary description thus focuses on the raw data collected from the individual research units. Additional statistics and combined statistics of the NERSH pool including reliability measures of previous suggested subscales in the original questionnaire by Lucchetti (2015) will be published in a future article once the pool has been completely established.
The NERSH data was thus collected between 2002 and 2016, and includes a total of 6137 individuals (3318 females and 2611 males plus one transgender and 207 unknown). Mean age in the studies varies from 28.4 (27.0–29.8) among the Brazilian nurse students and 29.2 (CI95% 28.4–29.9) in the Indonesian sample to 49.0 (CI95% 48.5–49.5) found in the sample of 1144 American physicians. The Danish study of 911 physicians has a mean age of 48.9 (48.0–49.8) with a bimodal distribution. The study from New Zealand only measured age in deciles, but 64.7% of the individuals lie in the range of 40 to 59 years of age, which is similar to the Danish and American study.
The pool contains 4019 physicians, 1028 nurses, 77 psychologists/psychotherapists and 1013 of other or unknown occupation. Response rates range from as low as 18% (116 responses out of 642 questionnaires sent in New Zealand) to 95% (Brazil) and 99% (Indonesia)—the latter two secured due to tight follow-up including personal meetings and encouragements to complete the forms.
The current description of the data is based on the individual contributions from NERSH collaborators. At the time of writing the data pool is still undergoing synchronization. The process of synchronization and a detailed quantitative description of the data pool will soon be published in another article by Kørup et al.
3. Results
3.1. Chronological Overview of Existing Studies Using the Original RSMPP
The first publication based on the RSMPP questionnaire was published in 2005 and centred on “Religious characteristics of U.S. physicians” [1]. The objective was to provide a description of U.S. physicians’ religious characteristics compared to those of the U.S. population. Curlin found that compared to the general population, physicians in the US were less likely to say they try to carry their religious beliefs over into all their dealings with life (58% vs. 73%) and twice as likely to say they cope with life crises without relying on God (61% vs. 29%). At the same time, 55% of physicians reported that religious beliefs influence their medical practice. Curlin proposed that these findings suggested the need for attention to the way religious commitments shape clinical engagements.
The second publication from 2006 reported “The association of physicians’ religious characteristics with their attitudes and self-reported behaviors regarding religion and spirituality in the clinical encounter” [2]. The vast majority of physicians agree that it is acceptable to address R/S issues if the patients bring it up, but are more reluctant to inquire about patient’s R/S (45% agree), talk about their own beliefs (14% say never, 43% say only when the patient brings it up) and pray with the patient (17% say never, 43% only when patients bring it up). Religious physicians are more likely to address R/S issues in the clinical encounter across all of these measures.
The third article raised the question: “Do religious physicians disproportionately care for the underserved?” [3] Those physicians who were highly spiritual, who agreed that their religious beliefs influenced their practice of medicine, or who were raised in a family emphasizing needs of the poor were significantly more likely to report practice among the undeserved; those who were more religious were more likely to view their medical practice as a calling, but they were not more likely to practice among the undeserved.
The fourth article had an ethical focus. It was titled “Religion, conscience, and controversial clinical practices” and was published with the New England Journal of Medicine [4]. The article centers on the ethical rights and obligations of physicians regarding the provision of treatment to which they morally object; 63% of physicians believe it to be acceptable to disclose moral objections to patients, 86% believe that physicians are obligated to present all options to patients, and 71% agree they are obligated to refer to physicians who do not object.
The fifth article centered on differences in how psychiatrist and other physicians evaluate the R/S of their patients: “The relationship between psychiatry and religion among U.S. physicians” [5]. Psychiatrists recognize the positive influence of R/S on health but are more likely than other physicians to consider R/S being sometimes a source of patient suffering through negative emotions (82% vs. 44%), and are more likely to encounter R/S issues in their clinical setting (92% vs. 74%). Likewise, psychiatrists are more comfortable than their non-psychiatrist colleagues in addressing R/S issues with their patients.
The sixth article likewise had a particular focus on psychiatry: “The relationship between psychiatry and religion among U.S. physicians.” The article documents that psychiatrists are less religious on a number of measures, although compared to other physicians they were more likely to be Jewish (29% vs. 13%) [6]. Non-psychiatrist physicians who were religious were more likely to refer patients to clergy members and religious counselors and less willing to refer them to psychologists and psychiatrists, leading to the conclusion that “historic tensions between religion and psychiatry continue to shape the care patients receive for mental health concerns”.
The seventh article centered on “Physicians’ observations and interpretations of the influence of religion and spirituality on health” and how such interpretations depend on physician’s own R/S [7]. Sixty-three percent believed R/S influenced health of patients, 76% believed it could help patients cope with disease, give them a peaceful state of mind (75%) and provide emotional and practical help via the religious community (55%). More religious physicians were more likely to report observing positive religious health influences.
The eighth article focused on ethical dilemmas of terminal care and in particular to what degree physicians have “religious and other objections to physician-assisted suicide, terminal sedation, and withdrawal of life support.” [8]. Sixty-nine percent object to the first, 18% to the second and 5% to the third practice, and objections were more pronounced among highly religious and Asian physicians, as well as among those who have more experience caring for the dying. These findings suggest that care for patients at the end of life may depend on value differences among physicians.
The ninth article (by Stern et al.) using Curlin’s 2003 data focused on “Jewish physicians’ beliefs and practices regarding religion/spirituality in the clinical encounter.” [9]. On each of four dimensions of physician beliefs and practices regarding R/S in clinical practice, Jewish physicians ascribed less importance to the effect of R/S on health and lesser role for physicians in addressing R/S in the clinical encounter. Stern et al. found that these differences were mediated by lower R/S among Jewish physicians as well as R/S practice level and demographics, once again pointing to how R/S—here focusing on affiliation—impacts clinically-relevant beliefs.
Finally, in the tenth publication, “Physicians in the USA: Attendance, beliefs and patient interactions Franzen used the same 2003 dataset to investigate the association of Physicians’ R/S attendance and beliefs with patient interactions, in particular religious support in the clinical encounter, asking what characteristics are related to inclusion or avoidance [10]. Franzen finds that R/S orientation, more than religious attendance, predicts the inclusion of R/S topics. Furthermore, Franzen found that some physician specialties have more R/S physicians than others, suggesting again that clinical interaction on R/S issues is not distributed evenly in the health care system.
In conclusion, the US studies from the RSMPP suggest that values, spirituality and religiosity impact multiple areas of health care in multiple ways.
3.2. Chronological Overview of Articles Using Translations of the RSMPP
The first article based on translations of the RSMPP was published in 2011 by Lee at al. on the basis of pilot study data collection in Freiburg, Germany and centered on “The meaning of religion/spirituality in psychiatry from staff’s perspective” [11]. The survey was answered by 197 (response rate 44%) at the department of psychiatry and psychotherapy of the Freiburg University Hospital in 2009. Although 95% of the respondent considered R/S as an important patient coping strategy, they did not integrate R/S practices in their therapies, mainly due to lack of time and training as well as the fear of offending patients.
The second article written by Tomasso et al. focused on the “Knowledge and attitudes of nursing professors and students from Brazil concerning the interface between spirituality, religiosity and health” [12]. It was answered by 30 nursing professors and 118 students. 95% of participants were religiously affiliated. Similarly to the aforementioned German sample, 96% believed R/S influences patients’ health. Seventy-seven percent wished to address R/S issues, but only 36% felt prepared to do so, mainly due to lack of time, fear of imposing personal beliefs and offending patients
The third article was published in 2012 by Al-Yousefi and reported “Observations of Muslim physicians regarding the influence of religion on health and their clinical approach” [13]. It was written based on data from 225 Muslim physicians working in a tertiary care hospital in Saudi Arabia. As in the aforementioned studies, 91% agreed that R/S had a positive influence on health. However, 62% believed R/S could lead patients to refuse recommended medical therapy, much higher than the 2% of physicians in Curlin’s 2005 study that found R/S led patients to refuse, delay or stop medically indicated therapy. Over 50% of physicians never queried about R/S issues. Family physicians were the most likely to initiate R/S discussion, and—not surprisingly—physicians with high R/S were more likely to share own religious views. The main barriers to addressing R/S were the same as in the aforementioned studies.
The fourth article was published 2013 by Lee and Baumann on the now nationwide psychiatric staff sample and reports “German psychiatrists’ observation and interpretation of religiosity/spirituality” in regard to their therapies” [14]. The data shows that German psychiatrists consider R/S influences on patients’ mental health to be positive and important. It also indicates that the R/S orientation of the psychiatrists themselves significantly influences this appreciation and their attitude toward R/S in the clinical setting.
The fifth article was published in 2013 by Ramakrishnan et al. on “Perspectives of Indian traditional and allopathic professionals on religion/spirituality and its role in medicine: Basis for developing an integrative medicine program” [15]. Data was collected in five TCAM and two allopathic tertiary care medical institutes in India. Both groups (75%/85%) of practitioners believed that spiritual focus increases with illness, 58% of both groups reported that patients receive support from their religious communities and 87% of TCAM (traditional complementary and alternative medicine prescriber) and 73% of conventional medical doctors (termed “allopaths”) considered spiritual healing a beneficial complement to allopathic medicine. Only 11% of allopaths and 40% of TCAMs had received training in R/S, however 82% of TCAM and 63% of allopaths considered integration of spirituality an important element of the health care system.
The sixth article from 2014 was based on the same dataset and focused on “Indian health care professionals’ attitude towards spiritual healing and its role in alleviating stigma of psychiatric services” [16]. It gauged TCAM and allopathic practitioners’ perspectives on patients’ R/S needs in mental health services. Just below half of both groups believed that their patients approach R/S or TCAM practitioners for mental illness treatment; 91% of TCAM and 70% of allopaths were satisfied with R/S healers. 91% of TCAM and 73% of allopaths believe mental health stigma could be minimized by integration with spiritual care services.
The seventh article, also from 2014, involved a combination of the aforementioned dataset with data collected in Indonesia by Karimah et al. in a cross-cultural comparison on “Religious/spiritual characteristics of Indian and Indonesian physicians and their acceptance of spirituality in health care” [17]. The researchers investigated differences in Indian and Indonesian physicians’ R/S characteristics and found Indonesian physicians to score higher on a range of R/S measures than their Indian colleagues. They also gauged different attitudes toward integration of TCAM with the modern health care system. As expected, they found Indonesian physicians (that are known for their integration of traditional medicine with modern medicine) to be more in favor of such integration than Indian physicians; the more spiritually inclined physicians, TCAM physicians in particular, were most comfortable attending to patients’ spiritual needs.
The eighth article, by Lee et al. from 2014, building on the aforementioned nationwide German dataset, first published 2013 is titled: “Religiosity/spirituality and mental health: Psychiatric staff’s attitudes and behaviors. It shows the tension and ambivalences of mental health staff between their readiness to integrate R/S aspects into treatment—basically considered as appropriate to be dealt with in therapies—and their attitudes and claims of professional neutrality [18].
In the ninth article, again from the Freiburg, Germany group, Lee et al. (2015) asked “How do psychiatric staffs approach religiosity/spirituality in clinical practice? Differing perceptions among psychiatric staff members and clinical chaplains” [19] and continued the research focus of their main study but also included responses from clinical chaplains and their mutual perceptions. In general, psychiatric staff members (psychiatrist, psychologists and nurses) saw themselves as “prepared and open to dealing with religiosity/spirituality in therapeutic settings”. However, the perception of Chaplains differs significantly from the staff’s own self-rating, leading the authors to suggest additional dialogue between the two groups of professionals with daily presence in the mental health care system. In 2014–2015, Lee and Baumann initiated a study in South Korean hospitals with psychiatric wards. Data have been collected and are going to be analyzed.
The tenth article was by Lucchetti et al., titled “Spirituality, religiosity, and health: a comparison of physicians’ attitudes in Brazil, India, and Indonesia” [20]. It compared the aforementioned datasets from Brazil, India and Indonesia and found Indonesian doctors to be the most religious, Brazilian doctors to be most convinced that R/S influences health; Indonesian and Brazilian doctors were both more convinced than Indian physicians that it was appropriate to discuss R/S with patients. The authors conclude from these and other differences that “Ethnicity and culture can have an important influence on how spirituality is approached in medical practice. S/R curricula that train physicians how to address spirituality in clinical practice must take these differences into account.”
As mentioned, eight doctoral theses were or are being published on the basis of translations of the RSMPP [21,22,23,24,25,26,27,28]. Their topics cover many of the topics addressed above, but their populations are often unique as in Kuseyri’s sample of Turkish physicians living in Germany [23], Mukwayakala’s study of physicians in Congo [24], Schouten’s nationwide study of HPs in perinatal medicine [25], and Randwijk’s study of highly secular Danish physicians [26].
The same conclusion emerges from the overview of the international publications from the RSMPP: Values, spirituality and religiosity impact health care in multiple ways, regardless of national and cultural settings.
3.3. Glimpse of Trends in the NERSH Data Pool of Physician Values
Preliminary analyses indicate large cross-national differences illustrated with a sample of items (see Table 1). Ninety-six percent of the 122 Indonesian physicians answered that they believe in a life after death, whereas only 20% of the Danish physicians share this belief. More than half of the American and Austrian physicians believe in life after death.

Table 1.
Differences in percent of important sample items of the NERSHS Data Pool.
When physicians were asked if they agreed or strongly agreed with the statement that their whole approach to life is based on their religion, 93% of the Indonesian sample agree with this, whereas only 11% of the Danish physicians agree. In cases where religious or spiritual topics arise in the clinical setting 91% of Danish physicians would never pray with the patient, while in Brazil only 7% answered that they would never pray with the patient. Likewise, 55% of Danish physicians would never share their own religious ideas and experiences, while only 6% of the Brazilian doctors and none of the physicians from Congo selected that answer.
More than 9 out of 10 of the physicians from Indonesia, Brazil, Austria and USA find it appropriate for physicians to discuss religious or spiritual issues when a patient brings them up in the clinical setting (Item marked either Always appropriate or Usually appropriate). For Denmark, this proportion is 83% and for Congo this is surprisingly low at 67%. The German samples cover specific groups of physicians with specific results for these groups.
As mentioned we are currently working on another article for a more in-depth quantitative description of the data pool including an overview of the distribution of participant occupation and religious affiliation across the included countries.
4. Summary
The NERSH survey instrument has been found to work well across cultures, and with a few optimizations and additions targeting secular cultures, it holds promise as a tool for future comparative analyses. Data are comparable and individual publications until now as well as initial analyses of the joint data pool suggest that large differences do exist across nations and cultures.
The articles published from versions of the RSMPP and data collected with the RSMPP and updated NERSH instruments already suggest three important initial insights:
- In the eyes of HPs, R/S is an important element of the life of patients. R/S may help patients cope with their disease and may positively influence their health. However, HPs also report various barriers for engaging their patients on R/S themes. These are mainly centred on lack of training, lack of time and fear of offending patients or imposing own beliefs on them.
- The idea that health care is a value neutral sphere, mainly driven by a scientifically neutral and “objective” approach, is challenged by research. HP values (both R/S and atheistic) are subjective, personal, and deep. They have a profound influence on communication with patients, in particular when it comes to existential and R/S issues, controversial issues in Health Care, and understanding of one’s own professional identity.
- Just as HPs’ personal values impact health care (communication, ethics and professional identity), so are the same values highly impacted by culture. This is clear in the enormous differences in R/S when comparing for instance Denmark with Brazil and the impact these differences have on HPs evaluation of patient R/S. This insight might help HPs to adopt a humble attitude while reflecting on the context of their own values, which may lead to improved attention to the particular values and needs of patients, be they atheist or R/S. Such reflecting may improve critical ethical reflection, increase respect for both religious and agnostic worldviews and improve communication with patients in their search for resources for dealing with their illness.
5. Invitation for Researchers to Join and Availability of Questionnaire
The development of the NERSH International Collaboration on Values in Medicine is considered an ongoing process. Researchers who wish to publish research papers on the existing NERSH data are invited to contact the NERSH board and propose what article they would like to publish on the data, with a proposed title and abstract. Researchers who contributed with original data have first priority, but apart from that article ideas are allocated to potential first authors in the order that the ideas are presented to the board.
Likewise, we invite researchers to use the updated NERSH Questionnaire to complement the existing NERSH Pool with data from their respective data. In particular, data is needed from the Slavic cultures. A written NERSH Agreement has been drafted for those who wish to participate in the NERSH International Collaboration on Values in Medicine. It stipulates the rights of all participants to be invited as co-authors on articles that employ data they contributed, and allows the NERSH collaborators the rights to propose articles and to use the data accordingly, as long as the NERSH board is in agreement. Another identical Agreement exists that further stipulates the rights to use the NERSH Questionnaire and contribute data as mentioned above. All who contribute to the pool co-authoring this article have signed this Agreement. Users of the NERSH questionnaire are requested to code their data according to the NERSH Physician Values Coding Manual, available on the Toolbox of www.nersh.org.
6. Limitations
The NERSH collaboration depends on the rigor of each research team involved and shares the limitations reported by each individual research article to which we refer [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28]. Not all sample sizes and response rates are equally good which may impact generalizability of findings.
Comparability of data for future joint NERSH articles will be challenged by the fact that some themes are inquired upon with different numbers of items, response categories, and formulations, that may even have different meanings in different cultural contexts. How we address these challenges and potential limitations in the existing dataset will be one of the issues of the next upcoming article of the NERSH collaboration. As mentioned in the present article, one of the primary incentives of the development of the optimized NERSH questionnaire was precisely to address some of these limitations in future data collections.
Finally, the NERSH database could benefit from future data collections from cultures under-represented or not represented at all, such as the Slavic countries in order to reflect a higher degree of global representability.
Supplementary Materials
The optimized NERSH instrument is available in the supplementary material under www.mdpi.com/2077-1444/7/8/107/s1 in English for physicians (Figure S1) and all HPs (Figure S2) as well as German for physicians (Figure S3) and all HPs (Figure S4); we provide a version in which differences between the original RSMPP and the updated NERSH have been noted in the margin (Figure S5). The final versions S1, S2, S3, and S4 are available as well on the Toolbox menu of www.nersh.org. Researchers wishing to use the NERSH questionnaire are invited to contact the first author and NERSH coordinator Niels Christian Hvidt.
Acknowledgments
We wish to thank the Freiburg Institute for Advanced Studies (FRIAS) for financial, institutional and practical support for the NERSH initiation. The original RSMPP was supported by The Robert Wood Johnson Foundation and The Greenwall Foundation The Danish study received funding from I.M. Dæhnfeldt Foundation, from The Danish College of General Practitioners as well as from the Faculty of Health Sciences, University of Southern Denmark. The Freiburg study received a starting grant by the innovative research fund of Albert-Ludwig-University Freiburg, Germany; we are grateful to Mathias Berger MD, Ulrich Voderholzer MD and Anne Zahn MD (who coauthored some of the Freiburg articles) for their support and cooperation. The Indonesian study received funding from the AdiBhat foundation; we are greatful to Kuntaman Kuntaman, MD, PhD, for coordinating the study between India and Indonesia and participating on paper writing. The Brazilian group expresses gratitude to Claudia Tomasso RN, Gabriela Romano MD and Alessandra Lucchetti MD (who coauthored some of the Brazilian articles) for their support and cooperation. The Indian study was made possible by the generosity in time, personal and financial support of HELP and AdiBhat Foundations in USA and India, respectively. The HELP Foundation is a nonprofit organization in Omaha, NE, USA, serving the underprivileged population with its community-based urgent care clinics. AdiBhat is a nonprofit organization founded in New Delhi to develop spirituality as a medical subject. The Indonesia study received funding as well from the AdiBhat Foundation. Kuntaman Kuntaman, MD, PhD, is acknowledged for coordinating the study between India and Indonesia and participating on paper writing.
Author Contributions
Niels Christian Hvidt, wrote the article, conceived, designed, performed the experiments for the local data collections, he was involved with, co-founder and coordinator of the NERSH-Network;
Alex Kappel Kørup, managed the joint NERSH-database, analyzed the data, contributed to the writing of the article;
Farr A. Curlin, conceived, designed, performed the experiments for the original data collection RSMPP questionnaire and data collection, contributed to the writing of the article;
Klaus Baumann, conceived, designed, performed the experiments for the local data collection, he was involved with, co-founder of the NERSH-Network;
Eckhard Frick, conceived, designed, performed the experiments for the local data collection, he was involved with, co-founder of the NERSH-Network;
Jens Søndergaard, hosting of NERSH-database, research oversight;
Jesper Bo Nielsen, hosting of NERSH-database, research oversight;
René dePont Christensen, statistical oversight on final NERSH-database;
Ryan Lawrence, conceived, designed, performed the experiments for the local data collection, he was involved with;
Giancarlo Lucchetti, conceived, designed, performed the experiments for the local data collection, he was involved with;
Parameshwaran Ramakrishnan, conceived, designed, performed the experiments for the local data collection, he was involved with;
Azimatul Karimah, conceived, designed, performed the experiments for the local data collection, she was involved with;
Andreas Schulze, conceived, designed, performed the experiments for the local data collection, he was involved with;
Inga Wermuth, conceived, designed, performed the experiments for the local data collection, she was involved with;
Esther Schouten, conceived, designed, performed the experiments for the local data collection, she was involved with;
René Hefti, conceived, designed, performed the experiments for the local data collection, he was involved with;
Eunmi Lee, conceived, designed, performed the experiments for the local data collection, she was involved with;
Nada A. AlYousefi, conceived, designed, performed the experiments for the local data collection, she was involved with;
Christian Balslev van Randwijk, conceived, designed, performed the experiments for the local data collection, he was involved with;
Can Kuseyri, conceived, designed, performed the experiments for the local data collection, he was involved with;
Tryphon Mukwayakala, conceived, designed, performed the experiments for the local data collection, he was involved with;
Miriam Wey, conceived, designed, performed the experiments for the local data collection, she was involved with;
Micha Eglin, conceived, designed, performed the experiments for the local data collection, she was involved with;
Tobias Opsahl, contributed to materials;
Arndt Büssing, analysed the data, contributed to the writing of the paper, co-founder of the NERSH-Network.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ASP | Aspects of Spirituality |
| DUREL | Duke Religiosity Index |
| FRIAS | Freiburg Institute for Advanced Studies |
| HPs | Health Professionals |
| IRG | Interdisciplinary Research Group |
| NERSH | Network for Research in Spirituality and Health |
| NGT | Nominal Group Technique |
| R/S | R/s understood as a unit of both, although they conceptually and phenomenologically have different traits |
| RSMPP | Questionnaire Religion and Spirituality in Medicine: Physicians’ Perspectives |
| SpREUK | Spiritual and Religious Attitudes in Dealing with Illness |
| TCAM | Traditional Complementary and Alternative Medicine |
Appendix A
Item Complexes
- Item complex #20: Positive experience of r/s in the clinical practice (i.e., helps patients to cope with and endure illness and suffering; causes guilt, anxiety, or other negative emotions that lead to increased patient suffering; gives patients a positive, hopeful state of mind; leads patients to refuse, delay, or stop medically indicated therapy; helps to prevent severe consequences of disease, etc.). Cronbach´s alphas ranged from 0.60 to 0.79 between the four samples. This indicates that the putative scale is of questionable to acceptable internal validity. Therefore, we added additional items as used in the Freiburg sample that had the best internal reliability with a 6-item version of the scale (i.e., adding: patients receive emotional or practical support from their religious community; religiosity/spirituality in general influences the health of patients/relatives positively; is strengthened or deepened through the experience of illness).
- Item complex # 21: Inquiry about religious/spiritual issues in specific situations (i.e., When a patient presents with a minor illness or injury; faces a frightening diagnosis or crisis; faces the end of life; suffers from anxiety or depression; comes for a history and physical; faces an ethical quandary). This topic was addressed in four datasets; Cronbach´s alpha ranged from 0.83 to 0.90 which indicates a good to very good internal reliability of this putative scale.
- Item complex #22: Frequency of specific responses when religious/spiritual issues come up in discussions with patients (i.e., listen carefully and empathetically; try to change the subject in a tactful way; encourage patients in their own religious/spiritual beliefs and practices; respectfully share my own religious ideas and experiences; pray with the patient). This topic was addressed in five datasets, but was found to be of questionable to acceptable internal validity (Cronbach´s alpha ranged from 0.61 to 0.74).
- Item complex #28: Controversial Issues in Medicine (i.e., Physician assisted suicide; Sedation to unconsciousness in dying patients; Withdrawal of artificial life support; Abortion for congenital abnormalities; Abortion for failed contraception; Prescription of birth control to teenagers between the age of 14 and 16 if their parents do not approve). This topic was addressed in four datasets, and was found to be of questionable to acceptable internal validity (Cronbach´s alpha ranged from 0.62 to 0.78).
Appendix B—Citation Search in Web of Science
Table B1.
Overview of Citation Search in Web of Science.

| ID | Term(s) | Results |
|---|---|---|
| 1 | Religious characteristics of US physicians–A national survey [1] | 1 |
| 2 | Citing articles | 85 |

| ID | Term(s) | Results |
|---|---|---|
| 1 | The association of physicians’ religious characteristics with their attitudes and self-reported behaviors regarding religion and spirituality in the clinical encounter [2] | 1 |
| 2 | Citing articles | 59 |

| ID | Term(s) | Results |
|---|---|---|
| 1 | Do religious physicians disproportionately care for the underserved? [3] | 1 |
| 2 | Citing articles | 15 |

| ID | Term(s) | Results |
|---|---|---|
| 1 | Religion, conscience, and controversial clinical practices AND Curlin [4] | 1 |
| 2 | Citing articles | 131 |

| ID | Term(s) | Results |
|---|---|---|
| 1 | Religion, spirituality, and medicine: Psychiatrists’ and other physicians’ differing observations, interpretations, and clinical approaches [5] | 1 |
| 2 | Citing articles | 46 |

| ID | Term(s) | Results |
|---|---|---|
| 1 | The relationship between psychiatry and religion among US physicians [6] | 1 |
| 2 | Citing articles | 32 |

| ID | Term(s) | Results |
|---|---|---|
| 1 | Physicians’ observations and interpretations of the influence of religion and spirituality on health [7] | 1 |
| 2 | Citing articles | 43 |

| ID | Term(s) | Results |
|---|---|---|
| 1 | To die, to sleep: US physicians’ religious and other objections to physician-assisted suicide, terminal sedation, and withdrawal of life support [8] | 1 |
| 2 | Citing articles | 34 |
Appendix C—Literature Search

Table C1.
Overview.
| Database | Interface | Date of Search |
|---|---|---|
| Google Scholar | Internet | 12-04-16 |
| Web of Science | Internet | 13-04-16 |
| Embase | Ovid | 12-04-16 |
| Medline | Ovid | 13-04-16 |
| PsychInfo | Ovid | 13-04-16 |

Table C2.
Google Scholar.
| ID | Term(s) | Results |
|---|---|---|
| 1 | “Religion and Spirituality in Medicine: Physicians’ Perspectives” | 8 |

Table C3.
Web of Science.
| ID | Term(s) | Results |
|---|---|---|
| 1 | TOPIC:(((questionn * OR survey * OR cross-section * OR national sample *) AND (religious OR religio * OR spiritual * OR religiosity) near/3 (professional * OR physician * OR psychiatris * OR doctor * OR staff * OR ((nurs * or medic *) near/3 (professor *))))) | 308 |
| 2 | Refined by: LANGUAGES: ( ENGLISH OR DANISH OR SPANISH OR FRENCH OR GERMAN ) Timespan: All years. Search language = Auto | 305 |

Table C4.
Embase (Embase + Embase Classic).
| ID | Term(s) | Results |
|---|---|---|
| 1 | (((questionn * or survey * or cross-section * or national sample *) and (religious or religio * or spiritual * or religiosity)) adj3 (professional * or physician * or psychiatris * or doctor * or staff * or ((nurs * or medic *) adj3 professor *))).mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword] | 1431 |
| 2 | limit 1 to (danish or english or french or german or italian or norwegian or spanish or swedish) | 1400 |

Table C5.
Medline.
| ID | Term(s) | Results |
|---|---|---|
| 1 | ((questionn * or survey * or cross-section * or national sample *) and (religious or religio * or spiritual * or religiosity)) adj3 (professional * or physician * or psychiatris * or doctor * or staff * or ((nurs * or medic *) adj3 professor *))).mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] | 1021 |
| 2 | limit 1 to (danish or english or french or german or italian or norwegian or spanish or swedish) | 998 |

Table C6.
PsychInfo.
| ID | Term(s) | Results |
|---|---|---|
| 1 | (((questionn * or survey * or cross-section * or national sample *) and (religious or religio * or spiritual * or religiosity)) adj3 (professional * or physician * or psychiatris * or doctor * or staff * or ((nurs * or medic *) adj3 professor *))).mp. [mp = title, abstract, heading word, table of contents, key concepts, original title, tests & measures] | 829 |
| 2 | limit 1 to (danish or english or french or german or italian or norwegian or spanish or swedish) | 804 |
Appendix D

Table D.
Overview of the International NERSH Data Pool.
| Country | Location | Sampling Year(s) | Occupation | n | Specialties | n | % | Religious Affiliation (%) | n | % | ntotal | RR* | Gender | n | % | Mean Age (CI95%) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| USA | Nationwide | 2002 | All physicians | Anesthesiology | 39 | 3.4 | None | 80 | 7.0 | 1144 | 63% | Male | 842 | 73.6 | 49.0 (48.5-49.5) | |||
| General Pract | 17 | 1.5 | Atheist | 19 | 1.7 | Female | 300 | 26.2 | ||||||||||
| Neuro | 18 | 1.6 | Agnostic | 18 | 1.6 | n/a | 2 | 0.2 | ||||||||||
| OB/GYN | 80 | 7.0 | Buddhist | 13 | 1.1 | |||||||||||||
| Optho | 18 | 1.6 | Hindu | 54 | 4.7 | |||||||||||||
| Pathology | 20 | 1.7 | Jewish | 181 | 15.8 | |||||||||||||
| Peds - General | 87 | 7.6 | Mormon | 17 | 1.5 | |||||||||||||
| Physiatry | 16 | 1.4 | Muslim | 33 | 2.9 | |||||||||||||
| Psych | 100 | 8.7 | Protestants | 428 | 37.4 | |||||||||||||
| Ped Subspec. | 60 | 5.2 | Catholic | 244 | 21.3 | |||||||||||||
| Gen Med | 129 | 11.3 | Orthodox | 22 | 1.9 | |||||||||||||
| FP | 158 | 13.8 | Other | 18 | 1.6 | |||||||||||||
| EM | 15 | 1.3 | Unanswered | 17 | 1.5 | |||||||||||||
| Dermathology | 11 | 1.0 | ||||||||||||||||
| Med Subspec. | 231 | 20.2 | ||||||||||||||||
| Radiology | 25 | 2.2 | ||||||||||||||||
| Unanswered | 2 | 0.2 | ||||||||||||||||
| General Surgery | 23 | 2.0 | ||||||||||||||||
| Surg Subsp. | 77 | 6.7 | ||||||||||||||||
| Other | 18 | 1.6 | ||||||||||||||||
| Germany | Freiburg. University clinic | 2008–2009 | Mixed psychiatric staff | Physicians | 18 | 21.1 | Protestants | 30 | 34.9 | 87 | 44% | Male | 38 | 43.2 | 41.5 | |||
| Psychologists and psychotherapists | 11 | 12.9 | Catholics | 28 | 32.5 | Female | 49 | 56.8 | ||||||||||
| Nursing staff | 39 | 44.7 | No affiliation | 23 | 26.5 | |||||||||||||
| Other psychiatric staff | 18 | 21.2 | ||||||||||||||||
| Saudi Arabia | Riyadh, King Abdul-Aziz Medical City | 2009–2010 | All physicians | Family medicine | 73 | 32.4 | Muslim | 225 | 100 | 225 | 64% | Male | 128 | 56.9 | 36.6 (35.4–37.6) | |||
| Internal med. and subspec. | 38 | 16.9 | Female | 97 | 43.1 | |||||||||||||
| OB/GYN | 31 | 13.8 | ||||||||||||||||
| Pediatrics | 21 | 9.3 | ||||||||||||||||
| Surgical subspec. | 30 | 13.3 | ||||||||||||||||
| Emergency med. | 9 | 4 | ||||||||||||||||
| Oncology and palliative care | 19 | 8.4 | ||||||||||||||||
| ICU and anaesthesia | 4 | 1.8 | ||||||||||||||||
| Indonesia | Dr. Soetomo General Hospital, Surabaya, East Java | 2010 | All physicians | Anatomy | 1 | None | 2 | 1,6 | 122 | 99% | Male | 55 | 45.1 | 29.2 (28.4–29.9) | ||||
| Microbiology | 1 | 0.8 | Other | 7 | 5.7 | Female | 65 | 53.3 | ||||||||||
| Pathology | 3 | 2.5 | Hindu | 2 | 1.6 | n/a | 2 | 1.6 | ||||||||||
| Forensic | 1 | 0.88 | Christian | 7 | 5.7 | |||||||||||||
| Ophtalmology | 10 | 8.2 | Muslim | 104 | 85.2 | |||||||||||||
| ENT | 1 | 0.8 | ||||||||||||||||
| Pediatric | 2 | 1.6 | ||||||||||||||||
| General medicine | 23 | 18.9 | ||||||||||||||||
| Surgery | 14 | 11.5 | ||||||||||||||||
| OBG | 7 | 5.7 | ||||||||||||||||
| Psychiatry/neurology | 17 | 13.9 | ||||||||||||||||
| Radiology | 8 | 6.6 | ||||||||||||||||
| Anesthesiology | 8 | 6.6 | ||||||||||||||||
| Psychotherapist | 1 | 0.8 | ||||||||||||||||
| Unanswered | 14 | 11.5 | ||||||||||||||||
| Brazil | São Paulo | 2010 | Teachers | 30 | Nursing | Teachers | 148 | 99% | Male | 15 | 10.1 | Teachers 41.4 (38.6–44.2) Students 28.4 (27.0–29.8) | ||||||
| Students | 118 | Catholics | 25 | 16.7 | Female | 133 | 89.9 | |||||||||||
| Spiritists | 20 | 13.3 | ||||||||||||||||
| Evangelical | 20 | 13.3 | ||||||||||||||||
| Students | ||||||||||||||||||
| Catholics, 30.8% | 46 | 30.8 | ||||||||||||||||
| Evangelicals, 11.1% | 16 | 11.1 | ||||||||||||||||
| None or others | 22 | 14.8 | ||||||||||||||||
| Germany, Freiburg | Nationwide. Departments of psychiatry and psychotherapy in university clinics + faith based clinics. | 2010–2011 | Psychiatrist | 121 | All psychiatry | No affiliation | 88 | 21.8 | 404 | 24% | Male | 145 | 35.9 | 39.9 (38.8–41) | ||||
| Psychotherapist | 16 | Catholic | 115 | 28.5 | Female | 252 | 62.4 | |||||||||||
| Other therapeut | 25 | Protestant | 128 | 31.7 | n/a | 7 | 1.7 | |||||||||||
| Psychologist | 32 | Free Church | 10 | 2.5 | ||||||||||||||
| Nurse or assistant | 160 | Orthodox | 1 | 0.2 | ||||||||||||||
| Other | 32 | Muslim | 5 | 1,2 | ||||||||||||||
| Buddhist | 7 | 1,7 | ||||||||||||||||
| Agnostic/Atheist | 34 | 8,4 | ||||||||||||||||
| Other | 9 | 2,2 | ||||||||||||||||
| India | Selected hospitals | 2010–2012 | TCAM | 192 | Anatomy | 8 | 2 | None or others | 11 | 3.7 | 394 | 50% | Male | 148 | 37.6 | 31.6 (30.5–32.8) | ||
| -Physicians | 79 | Physiology | 15 | 3.8 | Hindu | 257 | 65.2 | Female | 230 | 58.4 | ||||||||
| -Nurses | 0 | Biochemisty | 5 | 1.3 | Christian | 54 | 13.7 | n/a | 16 | 4 | ||||||||
| -Residents | 48 | Pharmacology | 23 | 5.8 | Muslim | 58 | 14.7 | |||||||||||
| -Interns | 0 | Microbiology | 4 | 1 | ||||||||||||||
| -Students | 36 | Pathology | 7 | 1.8 | ||||||||||||||
| -All-Therapists | 0 | Forensic | 6 | 1.5 | ||||||||||||||
| -Non-clinical physicians | 13 | Opthalmoloy | 1 | 0.3 | ||||||||||||||
| -Unknown | 16 | ENT | 11 | 2.8 | ||||||||||||||
| PSM | 12 | 3.0 | ||||||||||||||||
| Allopaths | 201 | Gen medicine | 49 | 12.4 | ||||||||||||||
| -Physicians | 54 | Surgery | 4 | 1.0 | ||||||||||||||
| -Nurses | 29 | OBG | 16 | 4.0 | ||||||||||||||
| -Residents | 44 | Psychiatry+neuro | 57 | 14.5 | ||||||||||||||
| -Interns | 0 | Pediatrics | 26 | 6.6 | ||||||||||||||
| -Students | 33 | Radiology | 0 | 0 | ||||||||||||||
| -All-Therapists | 0 | Anesthesiology | 18 | 4.6 | ||||||||||||||
| -Non-clinical physicians | 35 | Psychotherapist | 16 | 4.1 | ||||||||||||||
| -Unknown | 6 | Physical medicine and rehab +spec. | 18 | 4.6 | ||||||||||||||
| Denmark | Nationwide, selection criteria? | 2011–2012 | All physicians | General practitioner | 261 | 28.6 | Missing 8 (0.9) | 8 | 0.9 | 911 | 61% | Male | 524 | 57.5 | 48.9 (48.0–49.8) | |||
| Mixed hospital physicians | 650 | 71.4 | Do not wish to answer | 4 | 0.4 | Female | 387 | 42.5 | ||||||||||
| No affiliation | 183 | 20.1 | ||||||||||||||||
| Other | 20 | 2.2 | ||||||||||||||||
| Buddhist | 2 | 0.2 | ||||||||||||||||
| Hindu | 1 | 0.1 | ||||||||||||||||
| Muslim | 6 | 0.7 | ||||||||||||||||
| The Orthodox Church | 11 | 1.2 | ||||||||||||||||
| Roman Catholic Church | 29 | 3.2 | ||||||||||||||||
| Danish National Church | 647 | 71.0 | ||||||||||||||||
| Other | 4 | 0.4 | ||||||||||||||||
| New Zealand | Psychiatry | 2012 | Psychiatrists | 91 | All psychiatry | No affiliation | 53 | 45.7 | 116 | 18% | Male | 73 | 62.9 | Agegroups (n) | ||||
| Non specialists | 25 | Christian | 42 | 36.2 | Female | 39 | 33.6 | 20-29 | 4 | |||||||||
| Buddhist | 3 | 2.6 | Trans-gender | 1 | 0.9 | 40-49 | 32 | |||||||||||
| Hindu | 4 | 3.4 | n/a | 3 | 2.6 | 30-39 | 19 | |||||||||||
| Other | 4 | 3.4 | 50-59 | 43 | ||||||||||||||
| Object to answer | 3 | 2.6 | 60-69 | 14 | ||||||||||||||
| Unanswered | 7 | 6.0 | 70+ | 3 | ||||||||||||||
| Brazil | Marilia - Marília University Hospital | 2012 | Physicians | 81 | Internal Med. | 146 | 75.3 | None | 9 | 7.4 | 194 | 95% | Male | 145 | 74.7 | 37.7 (36.1–39.3) | ||
| Residents | 113 | Pediatricians | 12 | 6.2 | Other | 0 | 0 | Female | 49 | 25.3 | ||||||||
| Surgeons/surgical physicians | 26 | 13.4 | Hindu | 0 | 0 | |||||||||||||
| OB/GYN | 10 | 5.2 | Christian | 166 | 94.9 | |||||||||||||
| Muslim | 0 | 0 | ||||||||||||||||
| Congo R.D. | University Hospital of Kinshasa | 2012 | Mixed hospital physicians | No data | No affiliation | 12 | 11 | 112 | 82% | Male | 84 | 75 | 35 (33.5–36.8) | |||||
| Roman Catholics | 43 | 38 | Female | 28 | 25 | |||||||||||||
| Orthodox Christians | 1 | 1 | ||||||||||||||||
| Protestant Christians | 22 | 10 | ||||||||||||||||
| Others | 34 | 30 | ||||||||||||||||
| Germany, Munich | Nationwide Perinatal | 2013–2014 | Physicians | 482 | Perinatal hospital professionals | Does not apply | 115 | 7 | 1,637 | 82% | Male | 192 | 11.7 | 39.1 (38.6–39.6) | ||||
| Midwife | 257 | No response | 15 | 0.9 | Female | 1312 | 80.1 | |||||||||||
| Nurses | 529 | None | 409 | 25.0 | n/a | 133 | 8.1 | |||||||||||
| Psychologist | 18 | Roman | 639 | 39.0 | ||||||||||||||
| Others | 351 | Orthodox | 8 | 0.5 | ||||||||||||||
| Protestant (without Free-Church) | 409 | 25.0 | ||||||||||||||||
| Other Christian denominations | 21 | 1.3 | ||||||||||||||||
| Islam | 13 | 0.8 | ||||||||||||||||
| Jewish | 1 | 0.1 | ||||||||||||||||
| Buddhist | 6 | 0.4 | ||||||||||||||||
| Other non-Christian denominations | 1 | 0.1 | ||||||||||||||||
| Germany, Munich | Transplantation medicine | 2014 | Physician | 48 | Internal med. | 3 | 1.6 | 187 | 64% | Male | 53 | 28.3 | 34.6 (32.9–36.3) | |||||
| Nurse | 127 | Intensive care | 88 | 47.1 | Female | 134 | 71.7 | |||||||||||
| Other | 12 | Surgery | 38 | 20.3 | ||||||||||||||
| Neurology | 7 | 3.7 | ||||||||||||||||
| Anesthesiology | 19 | 10.2 | ||||||||||||||||
| Other | 32 | 17.1 | ||||||||||||||||
| Austria, Salzburg | Brothers of Mercy hospital | 2014 | Physician | 28 | Internal medicine | 54 | 23 | Not religious | 29 | 13 | 231 | 52% | Male | 54 | 23 | 39.3 (37.7–41.0) | ||
| Nursing care | 114 | Surgery | 37 | 16 | Catholic | 143 | 62 | Female | 133 | 58 | ||||||||
| Other | 29 | Anesthetics | 12 | 5 | Protestant | 8 | 3 | n/a | 44 | 19 | ||||||||
| Unanswered | 60 | Others | 62 | 27 | Others | 6 | 8 | |||||||||||
| Unanswered | 66 | 29 | Unanswered, | 45 | 19 | |||||||||||||
| Switzerland | Region of Bale and Aarau | 2015–2016 | All physicians, practicing outside the hospital | General practitioner | 104 | 100 | Christian | 80 | 76.2 | 104 | 75% | Male | 73 | 70.5 | 53.8 (51.9–55.7) | |||
| Jewish | 2 | 1.9 | Female | 31 | 29.5 | |||||||||||||
| Islam | 2 | 1.9 | ||||||||||||||||
| No affiliation | 19 | 18.1 | ||||||||||||||||
| Unanswered | 2 | 1.9 | ||||||||||||||||
| Germany, Munich | Turkish physicians | 2016 | All physicians | Psychiatry + psychotherapists | 9 | 7.4 | Muslim | 79 | 65.3 | 121 | 22% | Male | 42 | 34.8 | 33.2 (31.7–34.7) | |||
| Anesthetics | 1 | 0.8 | No affiliation | 21 | 17.4 | Female | 79 | 65.3 | ||||||||||
| Orthopedics | 4 | 3.3 | Exited a religious community | 1 | 0.8 | |||||||||||||
| Intensive care | 3 | 2.5 | Roman catholic | 1 | 0.8 | |||||||||||||
| OB/GYN | 5 | 4.1 | Other | 1 | 0.8 | |||||||||||||
| Internal medicine | 16 | 13.2 | Unanswered | 18 | 14.9 | |||||||||||||
| Surgery | 17 | 14 | ||||||||||||||||
| Neurology | 10 | 8.3 | ||||||||||||||||
| Pediatric | 9 | 7.4 | ||||||||||||||||
| Other 28 | 28 | 23.1 | ||||||||||||||||
| Unanswered | 19 | 15.7 | ||||||||||||||||
Note: * = Response Rat.
References
- Farr A. Curlin, John D. Lantos, Chad J. Roach, Sarah A. Sellergren, and Marshall H. Chin. “Religious Characteristics of U.S. Physicians: A National Survey.” Journal of General Internal Medicine 20 (2005): 629–34. [Google Scholar] [CrossRef] [PubMed]
- Farr A. Curlin, Marshall H. Chin, Sarah A. Sellergren, Chad J. Roach, and John D. Lantos. “The Association of Physicians’ Religious Characteristics with Their Attitudes and Self-Reported Behaviors Regarding Religion and Spirituality in the Clinical Encounter.” Medical Care 44 (2006): 446–53. [Google Scholar] [CrossRef] [PubMed]
- Farr A. Curlin, Lydia S. Dugdale, John D. Lantos, and Marshall H. Chin. “Do religious physicians disproportionately care for the underserved? ” The Annals of Family Medicine 5 (2007): 353–60. [Google Scholar] [CrossRef] [PubMed]
- Farr A. Curlin, Ryan E. Lawrence, Marshall H. Chin, and John D. Lantos. “Religion, Conscience, and Controversial Clinical Practices.” New England Journal of Medicine 356 (2007): 593–600. [Google Scholar] [CrossRef] [PubMed]
- Farr A. Curlin, Ryan E. Lawrence, Shaun Odell, Marshall H. Chin, John D. Lantos, Harold G. Koenig, and Keith G. Meador. “Religion, Spirituality, and Medicine: Psychiatrists’ and Other Physicians’ Differing Observations, Interpretations, and Clinical Approaches.” American Journal of Psychiatry 164 (2007): 1825–31. [Google Scholar] [CrossRef] [PubMed]
- Farr A. Curlin, Shaun V. Odell, Ryan E. Lawrence, Marshall H. Chin, John D. Lantos, Keith G. Meador, and Harold G. Koenig. “The Relationship between Psychiatry and Religion among U.S. Physicians.” Psychiatric Services 58 (2007): 1193–208. [Google Scholar] [CrossRef] [PubMed]
- Farr A. Curlin, Sarah A. Sellergren, John D. Lantos, and Marshall H. Chin. “Physicians’ Observations and Interpretations of the Influence of Religion and Spirituality on Health.” Archives of Internal Medicine 167 (2007): 649–54. [Google Scholar] [CrossRef] [PubMed]
- Farr A. Curlin, Chinyere Nwodim, Jennifer L. Vance, Marshall H. Chin, and John D. Lantos. “To Die, to Sleep: Us Physicians’ Religious and Other Objections to Physician-Assisted Suicide, Terminal Sedation, and Withdrawal of Life Support.” American Journal of Hospice and Palliative Medicine 25 (2008): 112–20. [Google Scholar] [CrossRef] [PubMed]
- Robert M. Stern, Kenneth A. Rasinski, and Farr A. Curlin. “Jewish Physicians’ Beliefs and Practices Regarding Religion/Spirituality in the Clinical Encounter.” Journal of Religion and Health 50 (2011): 806–17. [Google Scholar] [CrossRef] [PubMed]
- Aaron B. Franzen. “Physicians in the USA: Attendance, Beliefs and Patient Interactions.” Journal of Religion and Health 54 (2015): 1886–900. [Google Scholar] [CrossRef] [PubMed]
- Klaus Baumann, Eunmi Lee, and Anne Zahn. “‘Religion in Psychiatry and Psychotherapy?’ A Pilot Study: The Meaning of Religiosity/Spirituality from Staff’s Perspective in Psychiatry and Psychotherapy.” Religions 2 (2011): 525–35. [Google Scholar]
- Claudia de Souza Tomasso, Ideraldo Luiz Beltrame, and Giancarlo Lucchetti. “Knowledge and Attitudes of Nursing Professors and Students Concerning the Interface between Spirituality, Religiosity and Health.” Revista Latino-Americana De Enfermagem 19 (2011): 1205–13. [Google Scholar] [CrossRef]
- Nada A. Al-Yousefi. “Observations of Muslim Physicians Regarding the Influence of Religion on Health and Their Clinical Approach.” Journal of Religion and Health 51 (2012): 269–80. [Google Scholar] [CrossRef] [PubMed]
- Eunmi Lee, and Klaus Baumann. “German Psychiatrists’ Observation and Interpretation of Religiosity/Spirituality.” Evidence-Based Complementary and Alternative Medicine 2013 (2013): article 280168. [Google Scholar] [CrossRef] [PubMed]
- P. Ramakrishnan, A. Dias, A. Rane, A. Shukla, S. Lakshmi, B. K. Ansari, R. S. Ramaswamy, A. R. Reddy, A. Tribulato, A. K. Agarwal, and et al. “Perspectives of Indian Traditional and Allopathic Professionals on Religion/Spirituality and Its Role in Medicine: Basis for Developing an Integrative Medicine Program.” Journal of Religion and Health 53 (2013): 1161–75. [Google Scholar] [CrossRef] [PubMed]
- P. Ramakrishnan, A. Rane, A. Dias, J. Bhat, A. Shukla, S. Lakshmi, B. K. Ansari, R. S. Ramaswamy, R. A. Reddy, A. Tribulato, and et al. “Indian Health Care Professionals’ Attitude Towards Spiritual Healing and Its Role in Alleviating Stigma of Psychiatric Services.” Journal of Religion and Health 53 (2014): 1800–14. [Google Scholar] [CrossRef] [PubMed]
- P. Ramakrishnan, A. Karimah, K. Kuntaman, A. Shukla, B. K. Ansari, P. H. Rao, M. Ahmed, A. Tribulato, A. K. Agarwal, H. G. Koenig, and et al. “Religious/Spiritual Characteristics of Indian and Indonesian Physicians and Their Acceptance of Spirituality in Health Care: A Cross-Cultural Comparison.” Journal of Religion and Health 54 (2014): 649–63. [Google Scholar] [CrossRef] [PubMed]
- Eunmi Lee, Anne Zahn, and Klaus Baumann. “Religiosity/Spirituality and Mental Health: Psychiatric Staff’s Attitudes and Behaviors.” Open Journal of Social Sciences 2 (2014): 7. [Google Scholar] [CrossRef]
- Eunmi Lee, Anne Zahn, and Klaus Baumann. “How Do Psychiatric Staffs Approach Religiosity/Spirituality in Clinical Practice? Differing Perceptions among Psychiatric Staff Members and Clinical Chaplains.” Religions 6 (2015): 930–47. [Google Scholar] [CrossRef]
- Giancarlo Lucchetti, Parameshwaran Ramakrishnan, Azimatul Karimah, Gabriela R. Oliveira, Amit Dias, Anil Rane, A. Shukla, S. Lakshmi, B. K. Ansari, R. S. Ramaswamy, and et al. “Spirituality, Religiosity, and Health: A Comparison of Physicians’ Attitudes in Brazil, India, and Indonesia.” International Journal of Behavioral Medicine 23 (2016): 63–70. [Google Scholar] [CrossRef] [PubMed]
- Wyatt Butcher. “Spirituality, Religion and Psychiatric Practice in New Zealand: A Survey of Psychiatrists in New Zealand.” 2013. Available online: https://ourarchive.otago.ac.nz/handle/10523/242/browse?value=Butcher%2C+Wyatt+Hillary&type=author (accessed on 5 April 2016).
- Eunmi Lee. Religiosität Bzw. Spiritualität in Psychiatrie Und Psychotherapie. Ihre Bedeutung Für Psychiatrisches Wirken Aus Der Sicht Des Psychiatrischen Personals Anhand Einer Bundesweiten Personalbefragung. Studien Zur Theologie Und Praxis Der Caritas Und Sozialen Pastoral, 28. Würzburg: Echter, 2014. [Google Scholar]
- Can Kuseyri. “Spiritualität Türkischstämmiger Ärzte in Deutschland.” MD Thesis (German Dr.med.), Ludwig Maximilian University, 2016. Available online: http://www.nersh.org (accessed on 6 August 2016). [Google Scholar]
- Tryphon Mukwayakala-Kisamba. “Spiritualität Bei Ärzten Im Kongo.” MD Thesis (German Dr.med.), Ludwig Maximilian University, 2016. Available online: http://www.nersh.org (accessed on 6 August 2016). [Google Scholar]
- Esther Schouten. “Spiritualität in Der Perinatologie.” MD Thesis (German Dr.med.), Ludwig Maximilian University, 2016. Available online: http://www.nersh.org (accessed on 6 August 2016). [Google Scholar]
- Christian Balslev Van Randwijk. “Faith and Values of Danish Physicians.” Ph.D. Dissertation, University of Southern Denmark, 2016. Available online: http://www.nersh.org (accessed on 6 August 2016). [Google Scholar]
- Micha Eglin. “Religious Beliefs and Patient Observation in Swiss General Practitioners.” MD Thesis (Swiss Dr.Med.), University of Basel, 2016. Available online: http://www.nersh.org (accessed on 6 August 2016). [Google Scholar]
- Miriam Wey. “Religious Beliefs and Medical Practice in Swiss General Practitioners.” MD Thesis (Swiss Dr.Med.), University of Basel, 2016. Available online: http://www.nersh.org (accessed on 6 August 2016). [Google Scholar]
- Daniel E. Hall, Harold G. Koenig, and Keith G. Meador. “Conceptualizing ‘Religion’.” Perspectives in Biology and Medicine 47 (2004): 386–401. [Google Scholar] [CrossRef] [PubMed]
- Peter C. Hill, Kenneth Pargament II, Ralph W. Hood Jr., Michael E. McCullough, James P. Swyers, David B. Larson, and Brian J. Zinnbauer. “Conceptualizing Religion and Spirituality: Points of Commonality, Points of Departure.” Journal for the Theory of Social Behaviour 30 (2000): 51–77. [Google Scholar] [CrossRef]
- Peter La Cour, and Niels Christian Hvidt. “Research on Meaning-Making and Health in Secular Society: Secular, Spiritual and Religious Existential Orientations.” Social Science & Medicine 71 (2010): 1292–99. [Google Scholar] [CrossRef] [PubMed]
- Amanda Porterfield. Healing in the History of Christianity. New York: Oxford University Press, 2005. [Google Scholar]
- “Lancet Series on Faith-Based Health Care.” Available online: http://www.thelancet.com/series/faith-based-health-care (accessed on 6 April 2016).
- Sigmund Freud. Civilizations and Its Discontents. New York: W. W. Norton, 1959. [Google Scholar]
- Klaus Baumann. “The Birth of Human Sciences, Especially Psychology.” In L’uomo Moderno E La Chiesa—Atti Del Congresso (Analecta Gregoriana, 317). Edited by Paul Gilbert. Rome: Gregorian & Biblical Press, 2012, pp. 391–408. [Google Scholar]
- Harold G. Koenig, Dana E. King, and Verna Benner Carson. Handbook of Religion and Health, 2nd ed. Oxford and New York: Oxford University Press, 2012. [Google Scholar]
- Ryan E. Lawrence, and Farr A. Curlin. “Physicians’ Beliefs About Conscience in Medicine: A National Survey.” Academic Medicine 84 (2009): 1276–82. [Google Scholar] [CrossRef] [PubMed]
- Ryan E. Lawrence, and Farr A. Curlin. “Autonomy, Religion and Clinical Decisions: Findings from a National Physician Survey.” Journal of Medical Ethics 35 (2009): 214–18. [Google Scholar] [CrossRef] [PubMed]
- Ryan E. Lawrence, Kenneth A. Rasinski, John D. Yoon, and Farr A. Curlin. “Obstetrician-Gynecologist Physicians’ Beliefs About Emergency Contraception: A National Survey.” Contraception 82 (2010): 324–30. [Google Scholar] [CrossRef] [PubMed]
- Ryan E. Lawrence, Kenneth A. Rasinski, John D. Yoon, and Farr A. Curlin. “Obstetrician-Gynecologists’ Beliefs About Assisted Reproductive Technologies.” Obstetrics & Gynecology 116 (2010): 127–35. [Google Scholar] [CrossRef] [PubMed]
- Debra B. Stulberg, Ryan E. Lawrence, Jason Shattuck, and Farr A. Curlin. “Religious Hospitals and Primary Care Physicians: Conflicts over Policies for Patient Care.” Journal of General Internal Medicine 25 (2010): 725–30. [Google Scholar] [CrossRef] [PubMed]
- John D. Yoon, Kenneth A. Rasinski, and Farr A. Curlin. “Conflict and Emotional Exhaustion in Obstetrician-Gynaecologists: A National Survey.” Journal of Medical Ethics 36 (2010): 731–35. [Google Scholar] [CrossRef] [PubMed]
- John D. Yoon, Kenneth A. Rasinski, and Farr A. Curlin. “Moral Controversy, Directive Counsel, and the Doctor’s Role: Findings from a National Survey of Obstetrician-Gynecologists.” Academic Medicine 85 (2010): 1475–81. [Google Scholar] [CrossRef] [PubMed]
- Ryan E. Lawrence, Kenneth A. Rasinski, John D. Yoon, and Farr A. Curlin. “Adolescents, Contraception and Confidentiality: A National Survey of Obstetrician-Gynecologists.” Contraception 84 (2011): 259–65. [Google Scholar] [CrossRef] [PubMed]
- Ryan E. Lawrence, Kenneth A. Rasinski, John D. Yoon, and Farr A. Curlin. “Obstetrician-Gynecologists’ Beliefs About Safe-Sex and Abstinence Counseling.” International Journal of Gynecology & Obstetrics 114 (2011): 281–85. [Google Scholar] [CrossRef] [PubMed]
- Ryan E. Lawrence, Kenneth A. Rasinski, John D. Yoon, and Farr A. Curlin. “Obstetrician-Gynecologists’ Views on Contraception and Natural Family Planning: A National Survey.” American Journal of Obstetrics and Gynecology 204 (2011): 124.e1–e7. [Google Scholar] [CrossRef] [PubMed]
- R. E. Lawrence, K. A. Rasinski, J. D. Yoon, and F. A. Curlin. “Factors Influencing Physicians’ Advice About Female Sterilization in USA: A National Survey.” Human Reproduction 26 (2011): 106–11. [Google Scholar] [CrossRef] [PubMed]
- Kenneth A. Rasinski, Youssef G. Kalad, John D. Yoon, and Farr A. Curlin. “An Assessment of Us Physicians’ Training in Religion, Spirituality, and Medicine.” Medical Teacher 33 (2011): 944–45. [Google Scholar] [CrossRef] [PubMed]
- Kenneth A. Rasinski, John D. Yoon, Youssef G. Kalad, and Farr A. Curlin. “Obstetrician-Gynaecologists’ Opinions About Conscientious Refusal of a Request for Abortion: Results from a National Vignette Experiment.” Journal of Medical Ethics 37 (2011): 711–14. [Google Scholar] [CrossRef] [PubMed]
- Debra B. Stulberg, Annie M. Dude, Irma Dahlquist, and Farr A. Curlin. “Abortion Provision among Practicing Obstetrician-Gynecologists.” Obstetrics & Gynecology 118 (2011): 609–14. [Google Scholar] [CrossRef] [PubMed]
- Ryan E. Lawrence, Kenneth A. Rasinski, John D. Yoon, Harold G. Koenig, Keith G. Meador, and Farr A. Curlin. “Physicians’ Beliefs About Faith-Based Treatments for Alcoholism.” Psychiatric Services 63 (2012): 597–604. [Google Scholar] [CrossRef] [PubMed]
- R. E. Lawrence, K. A. Rasinski, J. D. Yoon, K. G. Meador, H. G. Koenig, and F. A. Curlin. “Primary Care Physicians’ and Psychiatrists’ Approaches to Treating Mild Depression.” Acta Psychiatrica Scandinavica 126 (2012): 385–92. [Google Scholar] [CrossRef] [PubMed]
- Kenneth A. Rasinski, Ryan E. Lawrence, John D. Yoon, and Farr A. Curlin. “A Sense of Calling and Primary Care Physicians’ Satisfaction in Treating Smoking, Alcoholism, and Obesity.” Archives of Internal Medicine 172 (2012): 1423–24. [Google Scholar] [CrossRef] [PubMed]
- Debra B. Stulberg, Annie M. Dude, Irma Dahlquist, and Farr A. Curlin. “Obstetrician-Gynecologists, Religious Institutions, and Conflicts Regarding Patient-Care Policies.” American Journal of Obstetrics & Gynecology 207 (2012): 73e1–e5. [Google Scholar] [CrossRef] [PubMed]
- Ryan E. Lawrence, Kenneth A. Rasinski, John D. Yoon, and Farr A. Curlin. “Religion and Anxiety Treatments in Primary Care Patients.” Anxiety Stress Coping 26 (2013): 526–38. [Google Scholar] [CrossRef] [PubMed]
- Ryan E. Lawrence, Kenneth A. Rasinski, John D. Yoon, and Farr A. Curlin. “Religion and Beliefs About Treating Medically Unexplained Symptoms: A Survey of Primary Care Physicians and Psychiatrists.” The International Journal of Psychiatry in Medicine 45 (2013): 31–44. [Google Scholar] [CrossRef] [PubMed]
- Ryan E. Lawrence, Kenneth A. Rasinski, John D. Yoon, and Farr A. Curlin. “Physicians’ Beliefs About the Nature of Addiction: A Survey of Primary Care Physicians and Psychiatrists.” The American Journal on Addictions 22 (2013): 255–60. [Google Scholar] [CrossRef] [PubMed]
- M. S. Putman, and F. A. Curlin. “Authors’ Reply to Dirksen et al.” Journal of Pain and Symptom Management 45 (2013): e2–e3. [Google Scholar] [CrossRef] [PubMed]
- Michael S. Putman, John D. Yoon, Kenneth A. Rasinski, and Farr A. Curlin. “Intentional Sedation to Unconsciousness at the End of Life: Findings from a National Physician Survey.” Journal of Pain and Symptom Management 46 (2013): 326–34. [Google Scholar] [CrossRef] [PubMed]
- Kelly M. Wolenberg, John D. Yoon, Kenneth A. Rasinski, and Farr A. Curlin. “Religion and United States Physicians’ Opinions and Self-Predicted Practices Concerning Artificial Nutrition and Hydration.” Journal of Religion and Health 52 (2013): 1051–65. [Google Scholar] [CrossRef] [PubMed]
- Ryan E. Lawrence, Kenneth A. Rasinski, John D. Yoon, and Farr A. Curlin. “Physician Race and Treatment Preferences for Depression, Anxiety, and Medically Unexplained Symptoms.” Ethnicity & Health 20 (2015): 354–64. [Google Scholar] [CrossRef] [PubMed]
- Ryan E. Lawrence, Kenneth A. Rasinski, John D. Yoon, and Farr A. Curlin. “Primary Care Physicians’ and Psychiatrists’ Willingness to Refer to Religious Mental Health Providers.” International Journal of Social Psychiatry 60 (2014): 627–36. [Google Scholar] [CrossRef] [PubMed]
- Michael S. Putman, John D. Yoon, Kenneth A. Rasinski, and Farr A. Curlin. “Directive Counsel and Morally Controversial Medical Decision-Making: Findings from Two National Surveys of Primary Care Physicians.” Journal of General Internal Medicine 29 (2014): 335–40. [Google Scholar] [CrossRef] [PubMed]
- Ryan E. Lawrence, Kenneth A. Rasinski, John D. Yoon, and Farr A. Curlin. “Psychiatrists’ and Primary Care Physicians’ Beliefs About Overtreatment of Depression and Anxiety.” The Journal of Nervous and Mental Disease 203 (2015): 120–25. [Google Scholar] [CrossRef] [PubMed]
- Krishna C. Ravella, Farr A. Curlin, and John D. Yoon. “Medical School Ranking and Medical Student Vocational Identity.” Teaching and Learning in Medicine 27 (2015): 123–29. [Google Scholar] [CrossRef] [PubMed]
- John D. Yoon, Jiwon H. Shin, Andy L. Nian, and Farr A. Curlin. “Religion, Sense of Calling, and the Practice of Medicine: Findings from a National Survey of Primary Care Physicians and Psychiatrists.” Southern Medical Journal 108 (2015): 189–95. [Google Scholar] [CrossRef] [PubMed]
- Klaus Baumann, Arndt Büssing, and Niels Chrsitian Hvidt. “Geisteswissenschaftliches Kolloquium Klaus Baumann (Freiburg)/Arndt Büssing (Witten/Herdecke)/Niels Hvidt (Odense): Empirische Forschung Über Religiöse Und Spirituelle Aspekte Bei Patientinnen Und Ärztinnen.” Freiburg Institute for Advanced Studies. Available online: https://www.frias.uni-freiburg.de/en/events/humanities-and-social-sciences-colloquium/geisteswissenschaftliches-kolloquium-klaus-baumann-freiburg-arndt-bussing-witten-herdecke-niels-hvidt-odense-empirische-forschung-uber-religiose-und-spirituelle-aspekte-bei-patientinnen-und-arztinnen (accessed on 6 April 2016).
- Arndt Büssing, Klaus Baumann, Niels Christian Hvidt, Harold G. Koenig, Christina M. Puchalski, and John Swinton. “Spirituality and Health. Editorial.” Evidence-Based Complementary and Alternative Medicine 2014 (2014): article 682817. [Google Scholar] [CrossRef] [PubMed]
- A. Büssing, A. T. Hirdes, K. Baumann, Niels Christian Hvidt, and P. Heusser. “Aspects of Spirituality in Medical Doctors and Their Relation to Specific Views of Illness and Dealing with Their Patients’ Individual Situation.” Evidence-Based Complementary and Alternative Medicine 2013 (2013): article 734392. [Google Scholar] [CrossRef] [PubMed]
- Edgar Voltmer, Arndt Büssing, HaroldG Koenig, and Faten Al Zaben. “Religiosity/Spirituality of German Doctors in Private Practice and Likelihood of Addressing R/S Issues with Patients.” Journal of Religion and Health 53 (2013): 1741–52. [Google Scholar] [CrossRef] [PubMed]
- Andre L. Delbecq, Andrew H. Van de Ven, and David H. Gustafson. Group Techniques for Program Planning: A Guide to Nominal Group and Delphi Processes. Glenview: Scott Foresman, 1975. [Google Scholar]
- Jeremy Jones, and Duncan Hunter. “Consensus Methods for Medical and Health Services Research.” British Medical Journal 311 (1995): 376–80. [Google Scholar] [CrossRef] [PubMed]
- Arndt Büssing, Thomas Ostermann, and Peter F. Matthiessen. “Distinct Expressions of Vital Spirituality ‘the Asp Questionnaire as an Explorative Research Tool‘.” Journal of Religion and Health 46 (2007): 267–86. [Google Scholar] [CrossRef]
- A Büssing, D. R. Recchia, J. Surzykiewicz, and K. Baumann. “Ausdrucksformen Der Spiritualität Bei Schülern Und Jungen Erwachsenen.” Spiritual Care. forthcoming.
- Arndt Bussing, Thomas Ostermann, and Peter Matthiessen. “Role of Religion and Spirituality in Medical Patients: Confirmatory Results with the Spreuk Questionnaire.” Health and Quality of Life Outcomes 3 (2005): 10. [Google Scholar] [CrossRef] [PubMed]
- Arndt Büssing. “Spirituality as a Resource to Rely on in Chronic Illness: The Spreuk Questionnaire.” Religions 1 (2010): 9–17. [Google Scholar] [CrossRef]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).