Abstract
The four principles of Western medical bioethics, i.e., autonomy, nonmaleficence, beneficence and justice, published by Beauchamps and Childress in their seminal ‘Principles of Biomedical Ethics’, are understood as universal. However, Non-Western governments argue that they refer to Western cultural contexts, neglecting specifics of Non-Western, for instance Islamic, civilizations. This paper addresses the claim of bioethical universality of both the West’s and Iran’s Shīʿī Islamic bioethics. We describe the historical development and the normative sources of Western and Shīʿī bioethics, i.e., common morality, the ontogeny of human morality and Shī’ī Islamic religious foundation. Both concepts support nonmaleficence and justice yet diverge with respect to beneficence, autonomy and normative justification. The Iranian screening program for ß-thalassemia major exemplifies the differences in both concepts. We conclude that nonmaleficence and justice are universal moral rules based on the ontogeny of morality. Beneficence can be characterized as a universal moral ideal. In contrast, autonomy, appreciated in the West, is neither justified by common morality nor the ontogeny of morality and has no equivalent in more communitarian-oriented societies. It thus fails to quality as a universal norm.
1. Introduction
The constitution of the World Health Organization (WHO) states “(The) highest attainable standard of health is one of the fundamental rights of every human being” (WHO 1948). Striving for this goal, most of us will come into contact with and rely on the biomedical ethics of healthcare professionals. If at these times of need we find ourselves somewhere far away from our own cultural settings, we probably will have to acknowledge that the interpretation of bioethics may significantly diverge from what we thought guaranteed. The principles of Western1 medical bioethics,2 that is, nonmaleficence, beneficence, autonomy, and justice, published by Tom Beauchamps and James Childress in their seminal ‘Principles of Biomedical Ethics’ (Beauchamps and Childress 2019), were taken up by the United Nations Educational, Scientific and Cultural Organization (UNESCO) in the ‘Universal Declaration on Bioethics and Human Rights’ aiming to provide “a universal framework of principles and procedures to guide states in the formulation of their legislation, policies or other instruments in the field of bioethics” (UNESCO 2005, Article 2, Aims). However, Non-Western governments interpreted the ‘Universal Declaration on Bioethics and Human Rights’ as referring to issues of Western cultural context without taking into account cultural specifics of Non-Western, for instance Islamic, civilizations. In this context, the declaration was interpreted as just an additional manifestation of Western imperialism and colonial thinking.3 This criticism reactivated the discourse on universal as opposed to plural bioethical concepts.
Bioethics deals with a policy-orientated approach to clinical decision making, that is, morality as the informal systems people use for making moral decisions, and a moral theory providing the justification of morality. A moral theory is supposed to deliver moral standards, consistency and a systematic perspective in moral decision making (Flynn 2021). PBE grounds moral decisions in reflective equilibrium with justification based on the normativity of common morality (CM). In contrast, in Shīʿī Islam the principles of bioethics are understood as based on the Qur’an, the traditions of the Prophet, as interpreted by Islamic legal rulings, and the consensus of scholars (Larijani et al. 2005).4
The West defines universal human nature as species-related traits common to all humans despite individual-specific genetic variations. The dilemma—a universal human trait yet myriads of individual gene variations—can be reconciled arguing with evolutionary biology. There, every trait or psychological phenomenon is either an adaptation, a by-product thereof, a product of ‘mutational noise’ or a combination of these. Adaptively evolved personality traits are the result of specific environmental challenges due to ecological or persistent social change. Thus, ‘genes’ and ‘environment’, that is, ‘nature’ and ‘nurture’, interact in a highly structured relationship, with genes and environment as interactive partners in ontogeny (Tooby and Cosmides 1990). Accordingly, human moral ontogeny gives rise to universal, genetically determined, species-specific personality traits, which then serve as building blocks for further variations (Tomasello 2016). In this context a universal principle of morality has to be grounded in universal human characteristics.
With the framework thus outlined, we will describe the historical development of both, Western and Shī’ī Islam bioethics, describe the normative sources for PBE, i.e., common morality as exemplified by Bernard Gert (Gert 2006), and base its claim of universality on the evolution of phylogeny and ontogeny of morality as described by Michael Tomasello (Tomasello 2016, 2019). Thereafter Shī’ī bioethics, its relation to ‘Western’ bioethics, its Islamic bioethical principles based on the normative sources of the revelatory texts, as suggested by Sachedina (Sachedina 2009) will be described in detail. After the theoretical fundaments have thus been laid the Iranian program on the prevention of β-thalassemia will exemplify the bioethical challenges and any divergence from the four-principles approach. Both concepts support nonmaleficence and justice yet diverge with respect to beneficence, autonomy, and normative justification. We conclude that nonmaleficence and justice are universal moral rules based on the ontogeny of morality. Beneficence can be characterized as a universal moral ideal. In contrast, autonomy, appreciated in the West, is neither justified by common morality nor the ontogeny of morality and has no equivalent in more communitarian-oriented societies. It thus fails to quality as a universal norm.
2. Results
2.1. Historical Development of Bioethics
- Western Bioethics
For centuries, medical ethics was based on the Hippocratic Oath, that is, patient confidentiality and nonmaleficence (nil nocere), and a fundamentally paternalistic approach. In the West, this concept changed after World War II. The Nuremberg Code (1947)—in response to human experiments during German National Socialism—reinforced by the Declaration of Geneva (1948), initiated the notion of patient’s informed consent. The Tuskegee Study (1933–1972) and the Human Radiation Experiments (1944–1972) in the United States of America (USA) led the way for the ‘Georgetown Principles’ based on the ‘Belmont Report’ (1979). The Declaration of Helsinki (1964, last revised 2013) and the Guidelines for Good Clinical Practice (GCP) define ethical and scientific guidelines for scientific investigations and clinical studies in humans. There are multiple approaches to bioethics in Western philosophy, with the principle-centered paradigm published by Beauchamps and Childress (1979) seen as mainstream. While moral theories may be seen as too academic for practical value in clinical bioethics, the more practice-oriented theories such as casuistry, narrative ethics or feminist theory did not attain the same widespread use as principlism. Thus, this paper will focus on Western bioethics as outlined by PBE and grounded on the normativity of CM (Beauchamps and Childress 2019; Gert et al. 2006; Gert 2006). PBE is based on the methodology of ‘reflected equilibrium’, delivering a coherentistic medical ethics combining ethical principles with awareness of the specific situation on the basis of nonmaleficence, beneficence, autonomy, justice, health maximization, efficiency and proportionality. The ‘Universal Declaration on Bioethics and Human Rights’ (UNESCO 2005) internationalized these bioethical fundamentals.
- Shī’ī bioethics
The Hippocratic Oath was mandatory for physicians in the Islamic world since the 10th century. ‘The Perfect Art of Medicine’ by Ali ibn Abbas Ahvazi (930–994) and ‘Ethics of a Physician’ by Ishag ibn Ali al-Ruhawi (1200) broadly discuss medical ethics. The first Farsi book on modern bioethics was published in 1963 in Iran (Larijani and Zahedi 2008). During 1970–1990, a period of mostly collaborative research with France and the USA, Iranian bioethics relied on paternalism and the virtuous physician (Aramesh 2015). Further progress was delayed by the Iranian Revolution (1978) and the Iraq-Iran war (1980–1988). The ethical approvals by research bodies, required by international medical journals since around 1990, made reliance in the individual virtuous physician insufficient as the sole basis for bioethical decisions. (Aramesh 2015). Compliance with international regulations became mandatory (Aramesh 2015). The Ministry of Health and Medical Education (MOHME) established the Medical Ethics Research Center (1993) which installed national Medical Research Ethics Committees (1997). The National Committee for Medical Research (1998) was asked (i) to apply Islamic, legal and moral principles to biomedical research, to guard human rights and legally protect the participants, researchers and institutes involved in research; and (ii) to recommend mandatory inclusion of advisors on ethical issues in all research projects (Larijani et al. 2005). Thereafter the compilation of the ‘Specific National Code of Ethics in Biomedical Research’ was concluded in collaboration with religious scholars, physicians, philosophers, legal experts, sociologists and other intellectuals initiating the ‘Specific National Ethical Guidelines for Biomedical Research’. Work-steps included the study of international/national guidelines, and a primary draft later revised by the Medical Ethics and Medical History Research Center experts and a focus group of religious, legal, ethics and medical authorities. A review by religious scholars, law experts, and by the authorities of MOHME finalized the process (Larijani and Zahedi 2008).
2.2. Normative Basis of Western Bioethics
Here, we present the basic ideas of (i) PBE; (ii) Common Morality (CM) as the normative basis to PBE; and (iii) the evolution of human morality that supports PBE’s claim to universality.
PBE is based on ‘principlism’. There a principle is defined as: “an abstract moral norm that is part of a framework of prominent starting-points in the ‘landscape’ of the moral life” (Beauchamps 2016, chp. 1.2, p. 93). “More specifically, rules for healthcare ethics can be formulated by reference to these general principles, but neither rules nor practical judgments can be straightforwardly deduced from the principles” (Beauchamps 2016, chp. 1.2, p. 93). The four basic principles are: nonmaleficence, beneficence, autonomy and justice.
Nonmaleficence states the obligation to abstain from any harm to others, where harming is not necessarily wrongdoing, but thwarting an individual’s interest. Beneficence requires acting to benefit others. Autonomy is defined as respecting the decision-making capacity of autonomous persons, free from interferences and limitations within the individual that prevent choices. It is based on liberty (seen as the absence of controlling influences) and agency (that is, self-initiated intentional action). Justice refers to the fair, due or owed treatment of a person. Healthcare justice describes the moral necessity of a just healthcare system based on mixed principles of egalitarian, libertarian, utilitarian, and other theories (Beauchamps 2016, chp. 1.3, pp. 94–103).
The four principles are connected to moral decision making by the process of specification, that is, adding action-guiding content to general principles. Specification delineates norms and narrows the scope of these norms by “spelling out where, when, why, how, by what means, to whom, or by whom the action is to be done or avoided” (Beauchamps 2016, chp. 4, p. 110).5 Specifications are justified via consistency with the norms of CM. They correspond to the theory-construction in ethics known as reflective equilibrium (Beauchamps 2016, chp. 4, pp. 112–13), a process “by which our considered responses to actual cases influence our moral principles, and those improved-upon principles then provide enhanced guidance for our response to further cases” (Flynn 2021, chp. 4.1, p. 8). The wide reflective equilibrium uphold by PBE surpasses the interplay between individual responses/intuitions about cases and the moral principles used to structure these intuitions by including additional moral and social theories. Therefore, the four principles are “not biomedical principles until they are specifically embedded in a biomedical context” by specification (Beauchamps 2016, chp. 5.1, p. 117).
Beginning in the 1990s some philosophers referred to CM as the ethical standards which are known and approved of by every moral agent. We intuitively know what is right or wrong (Beauchamps 2016, “where what we think about morality encompasses a considerable Mount that we do not think but know”; Ross D.W. cited by Bhaskarjit (Neog 2007, p. 10)).
Bernard Gert (2006) defined CM as the moral system that thoughtful people, that is, all moral agents, implicitly use when making moral decisions/judgments. CM guides the interaction between people. CM presupposes that moral agents understand what kind of behavior it prohibits or allows as without this knowledge actions cannot be morally judged. CM is based on rationality, is related to human nature and independent from religious beliefs.
CM is based on ten moral rules. The first five rules—do not kill, cause pain, disable, deprive of freedom and do not deprive of pleasure—prohibit harmful actions. The second five rules—do not deceive, keep your promises, do not cheat, obey the law, do your duty—prohibit actions that indirectly cause the five basic harms. Moral rules are obligatory. In contrast, moral ideals encourage people to prevent or relieve the harms that the moral rules prohibit them from causing. Thus, the rules prohibit harming, while the ideals encourage helping; as such it is more important to obey the moral rules than to follow the moral ideals. Gert cites John Stuart Mill: “The moral rules which forbid mankind to hurt one another … are more vital to human well-being than any maxims, however important, which only point out the best mode of managing some department of human affairs. … a person may possibly not need the benefits of others, but he always needs that they not do him hurt” (Gert 2006, chp. 1, p. 24). Accordingly, “widespread failure to follow moral ideals prevents a society from flourishing, widespread violations of the moral rules make it impossible to maintain a viable society” (Gert 2006, chp. 1, p. 27).
Gert’s moral theory describes CM as our implicit reasoning about what we morally ought to do (Gert et al. 2006). Rationality is the fundamental normative concept of CM. There acting rational is defined as not acting irrational6 and to fulfil specific qualifications: (i) use only those beliefs that all moral agents have; (ii) restrict these beliefs to rationally required beliefs (Gert et al. 2006, chp. 2, p. 36ff); and (iii) have a basic intelligence and ability to reason, (Gert 2006, chp. 2, p. 88). Gert argues that any rational agent holds these beliefs regardless of the time and place in which they live.7 By limiting themselves to these beliefs impartiality is guaranteed (Gert 2006, chp. 2, p. 91).
How is CM related to professional medical ethics? Moral rules lead to duties: natural duties to each other just in virtue of being human, acquired duties in consequence of what we have done (promises, etc.) and positive or negative duties to act or forbear from acting, respectively. Acting according to one’s duty can accrue by accepting a professional role. In this context “a profession is … an occupational grouping, whose members have a common defining end, such as preserving and restoring health in the case of members of the medical profession” (Alexandra and Miller 2009, p. 74). “Professional ethics is thus teleological in nature. Professional actions and attitudes are seen as morally good or bad, virtuous or vicious according to whether they help or hinder the realization of this defining end” (Alexandra and Miller 2009, p. 75).
In concordance with Gert, PBE defines “the CM” as a set of universal moral norms, that is, principles/rules, virtues, ideals and rights, shared by persons committed to live a moral way of life at all places and all times. There, morality includes rules of obligation comparable to Gert’s moral rules and standards of moral characters, close to Gert’s moral ideals. These norms “counteract the tendency for the quality of people’s life to worsen or for social relationship to disintegrate” (Arras 2009, p. 13; citing Beauchamps 2003, p. 261). PBE describes these moral norms as universally valid moral claims yet not legal rights. The claim on universal morality does not exclude moral pluralism. While universal morality or CM is abstract, moral norms are concrete, non-universal, and particular to cultural context, groups and individuals.
One criticism of Gert’s CM is its lack of empirical grounding, of anthropological data (Palmer 2005). Ten years after Gert passed away data on the evolution of human morality have been painstakingly collected. Using a phylo- and ontogenetic approach Michael Tomasello in ‘A Natural History of Human Morality’ (Tomasello 2016) starts his theory of the evolution of human morality with observations of great apes, representing pre-social behavior. He proceeds with the evolutionary ecological changes hundreds of thousand years ago that enforced human cooperation and further collaboration and cultural context. Tomasello supports his arguments with the ontogeny of children up to three (to five) years of age, the timespan for the development of cooperative behavior and morality. This latter process is independent of cultural influence and can be observed in Western as well as in small tribal societies world-wide, arguing for a universal human developmental process. The following will give a short outline of his theory of the evolution of morality.
The starting point for the evolution of human morality is the pre-social, competitive behavior of great apes at about six million years ago, with chimpanzees and bonobos as contemporary models. Their social life is characterized by competition for food, mates, and intragroup dominance status, cooperation only occurs for group-defense. Reciprocity of favors—based on the prosocial emotion of interdependence-based sympathy, not on any agreement, fairness or equity—emerges only in long-term relationships. These acts of emotion-based reciprocity originating from the interactions in parental care, an oxytocin-based social emotion of sympathy, are the first indication of a morality of sympathy, yet still without a normative sense of fairness and justice (Tomasello 2016, chp. 2, p. 34 ff).
Competition is a basic evolutionary concept. Can cooperation serve as an evolutionary advantage in promoting one’s gene pool in natural selection? Helping one’s kin before helping others may foster these evolutionary aims. Thus, the first evolutionary processes of cooperation were dependency-based mutualism and reciprocity. Tomasello bases the development of human morality on the gene-culture co-evolution of human cooperation, with interdependence as the fundamental concept. Human morality evolved in two steps. Step one, the emergence of obligatory collaborative foraging with partner-choice, where individuals with newly acquired psychological skills of joint intentionality, second-personal agency and self-regulatory processes made joint commitments. These were based on cooperative rationality in dyadic interactions, initially on the morality of sympathy followed by a second-personal morality of fairness, that is, a normative sense of obligation to one’s partner to live up to one’s shared role-ideals. The social interaction became structured from a ‘bird eye view’, an impartial perspective. The second step involved group-minded interactions in cultural contexts of specific socio-ecologic circumstances. There, individuals with skills of collective intentionality and cultural agency made collective commitments to the norms and institutions of their social group. Thus, a group-minded moral psychology evolved based on a kind of cultural rationality. This process of cultural identification shapes an individual’s identity, their rationality and thinking, more and above dyadic interactions, constituting a cooperatively rational way for individuals to treat one another in this new social context (Tomasello 2016, chp. 4, p. 85ff). The objectification of the instrumental values underlying cultural practices and social norms into moral judgements of right and wrong was ‘moral-structural’. Thus, both the second-personal and the group-minded social engagement shape the natural history of human morality, evolving from similar evolutionary sequences: i) changes in ecology; ii) increases in interdependence and cooperation; and iii) the requirement of new cognitive skills to coordinate new forms of co-operation: shared intentionality (from joint to collective intentionality), social-interactive skills of cooperative competence (from second-personal to cultural competence) and new social self-regulation processes (from joint commitment to moral self-governance) (Tomasello 2016, chp. 5.1, p. 135 ff). Human cooperations’ specific characteristics are connected to genuine moral decisions via psychological processes.
To summarize very briefly, interdependence (a socioecological conditions) leads to shared intentionality (that is, cognitive adaptations) which leads to second-personal agency (a social interactive status based on equal respect and deservingness) and joint commitment (a social self-regulation based on cooperative rationality and obligation) with reciprocal interaction of shared intentionality, second-personal agency and joint commitment. As a consequence of evolutionary pressure these dyadic interactions get upscaled to collective intentionality and cultural agency where cultural identification and the objectivation of instrumental values structure human interactions with a genuine human morality. These evolutionary data can be seen as the historical developmental timeline for an implicit moral system. This “common morality” guides the interaction between people.
2.3. Normative Basis of Shīʿī Bioethics
In contrast to Western bioethics, Shīʿī bioethics is based on religious norms. We give a short introduction to Shīʿī Islam and describe the legal methodology in interpreting the divine law. After the ground thus prepared, we discuss the modern developments of a Shīʿī bioethics, followed by the bioethical concepts of Abdulaziz Sachedina (2009) justifying ‘universal’ bioethical principles via the revelatory texts.
Shīʿī Islam holds that Muhammad designated Alī Ibn Abī Ṭalīb as his successor—serving as Imām—providing him, that is, the Imāmate charismatic loyalty (walāya), linking its spiritual authority directly to God (Haider 2014, chp. 1.2). There an Imām is the spiritual leader of the ummah with divine knowledge and authority, offering guidance according to the infallible interpretation (iṣma) of the Qur’ān (Haider 2014, chp. 1.2). During the Abbasid Caliphate, with the 12th Imām hidden from the authorities (‘minor occultation’), four deputies served as mediators between the Imām-in-occultation and his followers. The death of the fourth deputy started the still ongoing ‘major occultation’. The reappearance of the 12th Imām, the Rightly Guided One (Mahdī), will bring about the Day of Judgment. He will appear alongside Jesus Christ and establish the divine kingdom of God (Newman 2019).
In Islam, the sacred texts are seen as providing guidance for a life lived in a right, morally correct way with the goal of subserving God’s purpose. Supporting this goal, the divine law, the Sharī’a has to be interpreted into legally binding prescriptions for everyday life. With a living, accessible Imām there was no need for rational speculation in theology or jurisprudence. This changed with the ‘major occultation’ (Haider 2014, chp. 1.2). Religious scholars, that is, Imāms provided indisputable religious knowledge based on the words and actions of the Prophet and the Imāms, emphasizing rational discourse in the derivation of the law and the rulings of jurists, as the best approximations of God’s will (Haider 2014, chp. 3.7). In the 15th century, the largest group of Shī’ī Islam, the Twelver Shī’ī, was defined by three characteristics, it (i) was built on a theological foundation, partly derived from Mu’tazilism, that is, rationalist theology; (ii) used a rationalist legal methodology (uṣūlī); and (iii) was quietist and politically disengaged, awaiting the Mahdī as the sole legitimate source of religious and political authority (Haider 2014, chp. 3.7). The mujtahid, highly trained scholars representing the Hidden Imām examine the revealed texts, searching for consensus (ijmāʿ) among earlier scholars and offer rulings (fatāwi, singular fatwā), a process referred to as ijtihād (Newman 2019). The Safavid period (1501–1722) saw the transformation of Iran into a Twelver Shī’ī nation. During Qajar rule (1785–1925), uṣūlī scholars developed the concept of the marja’ al-taqlīd (source of emulation) as the primary representative of the Imām leading the community, managing finances and public life without claiming to rule on behalf of the Hidden Imām (Haider 2014, chp. 3.7). The 20th century further politicized Twelver Shī’ī with Khomeini’s vision of a state in which the jurist exercised absolute juridical and political power in the name of the Hidden Imām.
The juridical methodology, that is, ijtihād is the background for the actual bioethical discourse in Shīʿī Islam (Mavani 2014, p. 269). ‘Traditional ijtihād’ relies on the Qur’ān, the Sunna, the twelve infallible guides, consensus and reason. The challenges of modern medicine asked for new methodological devices such as (i) a change in legal rulings due to alteration “in the subject’s essence ... that is, a change in time, place, customs, locality or traditions … in the relationship between the subject matter and the bases upon which the ruling was issued”; or in “secondary injunction (that is a normally prohibited act can become lawful due to the presence of certain characteristics such as public welfare, etc.)”; and (ii) a decree by the ruler of an Islamic state” (Mavani 2014, pp. 271–72) For instance, the traditional hierarchy of human dignity, preferring Muslim patients over Non-Muslim patients, men over women or the permission of slavery, is current and applicable under the paradigm of ‘traditional ijtihād’ because these injunctions are viewed as fixed and eternal (Mavani 2014, p. 273). However, acceptance of secondary principles and precepts allows legal adjustments. For instance the concept of public welfare (maṣlaḥa), adopted by Ayatollah Khomeini, can override scriptural authority and justify almost everything (Mavani 2014, p. 275). In contrast, ‘foundational ijtihād’ is not constrained by existing legal theory. There “the moral values are the crucial pivot of the entire overall system, and from them flows the law.” (Mavani 2014, p. 273) ‘Foundational ijtihād’ states that all discriminatory rulings based on man-made characteristics (race, gender, national origin, religion, etc.) violate the Qur’ānic ethos of justice, equity, fairness, and universal human dignity.8 Thus, ‘foundational ijtihād’ relies on certain Qur’ānic normative ethical values and general principles for the development of a hierarchy of values (justice, equity, human dignity, etc.). ‘Foundational ijtihad’ provides a coherent framework, reconstructing theology and ethics giving the intellect (‘aql) and modern sciences a larger role in ethical decision making. Problems pertain to the subjective criteria for distinguishing between the permanent and the immutable domains. ‘Foundational ijtihad’, despite of its bases on non-religious universal norms, grounds its ethical decisions to the religious ethos of Islam and thus limits its application to Muslims (Mavani 2014, p. 281).
To summarize, in an ongoing discourse ‘traditional ijtihad’ allows for secondary principles, especially maṣlaḥa, to adjust the attributes of injunctions which in principle are seen as the immutable and eternal law of the Qur’ān or the Sunna. In contrast ‘foundational ijtihad’ refers to certain Qur’ānic normative ethical values and general principles to create a hierarchy of ethical values aiming for egalitarian justice and allowing adaptation to time and space.
‘Traditional’ and ‘foundational ijtihād’ provide the arguments for Shīʿī Islamic discourse about the bioethical challenges. Evolving approaches are (i) taking up mainstream (Western) biomedical ethics (MBME); (ii) using MBME and adjust it to Islamic belief; (iii) basing bioethical decisions on a system of fatāwi; or (iv) searching for a Islamic justification of bioethics, an Islamic biomedical ethics (IBME) (Moosapour et al. 2018).
Can Shīʿī Islam bioethics be identical to MBME understood as the ‘four-principles approach’? Many bioethical concepts (medical professionalism, resource allocation in healthcare) overlap, but are justified in different ways. In addition, MBME lack Islamic considerations for or approach to specific topics (Moosapour et al. 2018, p. 3).9 Thus, a simple transfer of MBME into Islamic cultural context is not considered possible.
Can MBME be adjusted to Muslim belief? Both use similar philosophical approaches such as (i) virtue ethics, describing the virtuous unbiased physician; (ii) deontological ethics, with IBME based on moral obligations defined in the Sharī’a; (iii) references to the principle of common good (maṣlaḥa), interpreted as a consequentialist view; and (iv) the four-principles approach, which can be found in Islamic resources, yet may show different applications, especially with autonomy. These similarities allow for effective communication. However, defining Islamic considerations (for instance autonomy), finding consensus on the offered solutions and their adequacy remains challenging (Moosapour et al. 2018, p. 4).
Could fatāwi serve as basis of an Islamic bioethics? Fatāwi define the religious duty for an individual and legitimize specific concerns at the social level without being legally obligatory. However, difficulties arise due to (i) the diversity of fatāwi; (ii) their unexplained relation between juridical and ethical solidity; and (iii) the question whether a fatwā has to cover the full range of bioethical concerns. In conclusion, for medical issues not fully covered by the Sharī’a, fatāwi may provide ethical guidance. However, their diversity and their difficult legal aspects argue against fatāwi as the basis of bioethical reasoning (Moosapour et al. 2018, p. 5).
Sachedina suggests an IBME approach to ethical reasoning based on principles similar to MBME. Islamic principles (that is, ‘public interest’ or ‘the common good’ (maṣlaḥa); ‘no harm, no harassment’ (la darar wa la derar); ‘necessity’ (darura); and ‘no hardship’ (la haraj)) developed by Islamic jurisprudence (fiqh) can be of use in bioethics. IBME could provide “a distinctly Islamic, and yet cross-culturally communicable, principle/rule-based deontological-teleological ethics” Yet, consent about principles/rules as well as definition of the agents who should apply them is a necessary prerogative (Moosapour et al. 2018, p. 7).
To summarize, the challenges of modern medicine initiated an Islamic bioethical discourse. Despite the initial acceptance of the four-principles approach, it became clear that hereby (i) some Islamic considerations are neglected (ii) the interpretation of some issues differs substantially or is not applicable at all. A pragmatic approach to adapt the four-principles according to Islamic considerations would need a consensus on the definition of specific Islamic considerations and the solutions offered. Fatāwi due to their diversity, their undefined balance of legal and ethical soundness, and their mostly small range of issues solved are seen as unsuitable for IBME. A specific Islamic approach, that is, an IBME, principle-based and justified by the revelatory texts, as offered by Sachedina is an option still under discussion.
The following chapters describe the most comprehensive suggestion and justification of Islamic bioethics as of today, that is, ‘Islamic Biomedical Ethics, Principles and Application’ (Sachedina 2009), based on universal moral principles yet justified by the divine texts.
In Islamic thought, ethical reasoning is directly related to religious epistemology. The analysis of the rational (‘illa) and the purpose behind the paradigmatic rulings (al-aṣl, plural uṣūl) provides principles for future decisions. These principles are conceptually based on (i) justice (‘aḍala, “putting something in its appropriate place”) as the theoretical background for human obedience to divine commands and human capacity towards moral-religious obligations (takālif shar’iya); and (ii) obligation (wujūb, “promulgation of divine command and prohibition”) defining the nature of the divine command and providing deontological grounds for complying with it (Sachedina 2009, chp. 2, p. 34). The derived principles are regarded as an interpretation of the Qur’ān to discover God’s will, as God’s knowledge of ethical challenges is all-encompassing and infallible (Sachedina 2009, chp. 2, p. 33). Therefore, “the revealed law of Islam is concerned with apprehending divine wisdom through the study of rules derived from revelatory sources for the acts of people under legal-moral obligation” (Sachedina 2009, chp. 2, p. 36).
Shī’ī ethical objectivism or deontological theory is grounded in the idea that humans can know much of what is right and wrong because of the intrinsic goodness or badness of actions. The Sharī’a ranks human acts from obligatory to forbidden with ‘independent’10 reason categorizing legal characteristics of an act as either necessary, good or evil. Moral responsibility arises as humans are (i) causative for an act and morally obliged to deter harm; and (ii) have an autonomous and intuitive knowledge, supported by reason, of an act’s characteristics. (Sachedina 2009, chp. 2, p. 43).
The derivation of bioethical principles and rules is regulated by legal methodology such as istiḥsān (prioritization of two or more equally valid judgments through juristic practice) and istiṣlāḥ (promoting and securing benefits, preventing and removing harm in the public sphere), allowing adaptability to time and place. The principle of public good, maṣlaḥa, based on the Sharī’a’s aim of justice, investigates the consequences of an act for everyone affected by such a ruling, while istiṣlāḥ here means “to seek to maximize benefit and minimize harm” (Sachedina 2009, chp. 2, p. 51ff). In short, “the principle of public good is the basis for legal-ethical decisions in cases in which the welfare of all the people is under consideration” (Sachedina 2009, chp. 2, p. 61), while the individual good functions as the context for derivative rulings. Thus, bioethical decisions represent general moral considerations related to the principle of public good.
The principle of nonmaleficence, that is, rejection of harm, is central to the Islamic conceptions of healthcare (Sachedina 2009, chp. 2, p. 68). The theological justification is the credo that all God’s acts are purposeful. Since God’s purpose cannot be evil, responsibility for the act with a purpose other than beneficence falls upon the human agent. The principle of ‘no harm, no harassment’ indicates that any command by the sacred lawgiver must be free of harm in its execution. It denies any legitimacy to harm in Islam. The subsidiary rule ‘hardship necessitates relief’ demands the avoidance of harm to society by legislation. (Sachedina 2009, chp. 2, p. 70).
To summarize, Shī’ī Islamic principles of bioethical reasoning are based on religious epistemology and reason-based legal methodology, related to social interactions and thus on the interest of public good. Humans are seen as capable to intuitively judge an act as right or wrong. The principle of ‘considerations of public good (istiṣlāḥ) is referred to where the Sharī’a lacks relevant statement. The act-based ethical thinking refers to maṣlaḥa as the Sharī’a’s aim of justice and the peoples’ best interest. Bioethical decisions overwhelmingly refer to the principle of ‘no harm, no harassment’, with common interest and individual welfare being balanced according to circumstances. The principle ‘no harm, no harassment’ is seen as equivalent to the Western principles of nonmalevolence and beneficence, with a preponderance of ‘no harm’.
2.4. The Bioethical Challenges Exemplified via the Iranian Program of the Prevention of ß-Thalassemia Major (ßTMa)
To further the understanding of how the Iranian theocratic republic deals with the bioethical challenges of modern medicine, ßTMa may serve as an example. ßTMa is an inherited, recessive disease with a prevalence of ß-thalassemia alleles of 4–8%, that is, 3 750,000 carriers and 20,000 homozygotes (Rahimi 2013). The direct and indirect costs accrue to about 150,000,000 USD/year, with the government covering 66%, health insurance 19% and the patient 15%, respectively. The latter is unaffordable for many patients increasing their burden by the disease with the additional burden of poverty (Esameilzadeh et al. 2016). A cost effectiveness analysis (CEA) from 2021 demonstrated ßTMa therapy as cost-effective with 11.8 quality of life years (QALY) at 11.571 USD/QUALY at an effectiveness threshold of three times the per capita gross-domestic product (13.325 USD). However, screening for ßTMa is more cost effective, generating a net profit of 103.908 USD per prevention of one birth with ßTMa (Esmaeilzadeh et al. 2021). Untreated ßTMa reduces life expectancy into early adult age. In Iran the mean survival of patients with therapy is 50 years (Ansari-Moghaddam et al. 2018). Therapy may not result in full physical ability or the achievement of a ‘normal life’ due to a significant decrease in the quality of life (Adib-Hajbaghery et al. 2015).
To summarize, ßTMa is a severe, costly hereditary disease with a high prevalence in Iran, posing a substantial burden on the healthcare system and the afflicted individual.
Prevention of inherited diseases relies on genetic counselling, defined “as the process of helping people understand and adopt to the medical, psychological and familial implications of genetic contributions to disease” (Bittles 2012, chp. 18, p. 204).11 Genetic counselling is required as part of genetic screening (Figure 1 (29)), that is, pre-marital screening (PMS) or pre-natal diagnosis (PND).
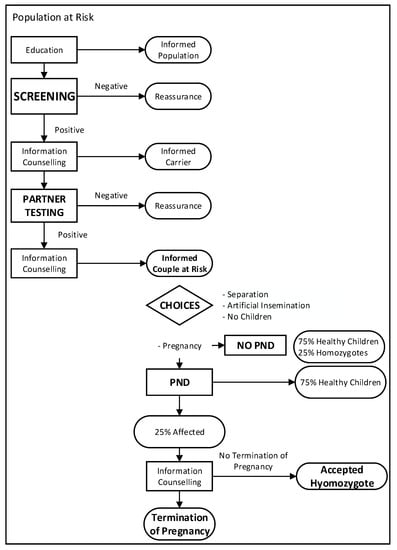
Figure 1.
Flowchart Pre-marital screening for hereditary recessive diseases (WHO 1993, adapted).
Basic requirements in PMS are (i) efficacy-evaluation of knowledge-increase due to pre-marital counselling; (ii) options for couples-at-risk, that is, not marrying, marrying but not having children, marrying and undergo PND and eventually abortion of a homozygote embryo; and (iii) awareness of cultural traditions (close relatives or being a member of a close community may influence the decision towards marriage despite the diagnosis; fulfilling a contracted marriage arrangement thereby preventing a disruption of family relationships may outweigh the problems due to a diseased child (Bittles 2012, chp. 18, p. 197). PND requires pre-test counselling. Here, prerequisites are access to genetic specialist expertise, information on the possibility of false positive/false negative results, and the chance to terminate the pregnancy. In 1997 the Grand Ayatollah Khamenei issued a fatwā (approved by the Islamic Guardian Council in 2005) permitting therapeutic abortion (Hedayat et al. 2006; Najmabadi et al. 2006).
To reduce the public and individual burden of ßTMa, a mandatory PMS program based on a primary care genetic-counseling network was initiated in Shiraz (1991) and extended to all provinces in 1995/1997 (Rahimi 2013; Samavat and Modell 2004). The head of the Genetic Office at the MOHME, Ashraf Samavat explicitly states that the Iranian program follows the WHO’s ethical principles. These were nonmaleficence, beneficence, autonomy and justice, in addition to avoidance of stigmatization, voluntariness of testing, openness for the decisions of those tested, as well as confidentiality (Samavat and Modell 2004; WHO 1998, 2006).
Before PND became available, 90% of couples-at-risk refrained from their planned marriage. This percentage has declined substantially with PND available (Ghanei et al. 1997; Rahimi 2013). By 2009 the incidence of ßTMa was reduced by 83%. However, in provinces with a high prevalence of the thalassemic gene and a Sunni tradition of unregistered marriages the reduction was significantly lower (Hashemieh et al. 2015).
The next paragraphs focus on the program’s claim of adherence to the Western four-principles approach. Nonmaleficence states the obligation to abstain from any harm to others, where harming is not necessarily wrong doing, but thwarting an individual’s interest (Beauchamps 2016, chp. 1, p. 100). Thus, the prevention of stigmatization and ethnic discrimination by carrier screening is mandatory and prerequisites a broad information/education campaign at the community level (WHO 2006). As a mandatory nationwide program PMS avoids ethnic discrimination. Inadvertently, certain religious groups (the Sunni of southern Iran) circumvented the mandatory counseling of a Shīʿī clergy due to marriage procedures within their religious community, leading to a persistently high incidence of ßTMa. These results were interpreted as a lack of awareness of a traditional way of life and specific education was suggested to avoid further stigmatization (Hadipour Dehshal et al. 2019; Hashemieh et al. 2015). Thus, the Iranian program acknowledged the possibility of social harm and suggested solutions (Nouri et al. 2017). Still, individual harm by mandatory screening and its consequences is not accounted for.12
To summarize, the principle of nonmaleficence for possible social harm is in accordance with the Western understanding. However, mandatory screening denies the acknowledgement of possible individual harm. There common interest prevails over individual welfare in accordance with Shīʿī Islam bioethics but in contrast to Western interpretation where most screening programs for ßTMa are voluntary with PND being available from the very beginning (Cao and Kan 2013).
Beneficence requires the prevention of harm. It calls for action for the benefit of others (Beauchamps 2016, chp. 1, p. 99). As a prerequisite for PMS the WHO suggests the inclusion of patient support organizations (WHO 2006) to help patients with medical decisions, act as lobbyists, raise awareness, financial, and psychosocial support (Cao and Kan 2013). No paper reports the inclusion of patient support groups (PSG) despite the existence of an Iranian thalassemia PSG. However, this ‘invisibility’ of PSG may express the little importance given to beneficence in Shīʿī Islam bioethics, where “preventing harm has a priority over promoting good” (Sachedina 2009, chp. 2, p. 75). In contrast, PBE defines patient care as acting for the patient’s best interest, not only avoiding harm, but aiming for maximum benefit.
To summarize, the interpretation of beneficence differs significantly between Western and Shīʿī bioethical thinking.
Autonomy is defined as respecting the decision-making capacity of autonomous persons, free from interferences and limitations that prevent choices. It is “based on liberty (the absence of controlling influences) and agency (self-initiated intentional action)” (Beauchamps 2016, chp. 1, p. 94). Autonomy has been translated into operational concepts as informed consent, non-directive counselling, the right ‘not to know’ and the right on voluntary decisions, free from coercion (Borry et al. 2013, chp. 5, p. 76). Accordingly, counselling should provide sufficient knowledge for informed consent (WHO 2006). Unfortunately, the Iranian counselling program has a low efficacy with only eight percent of the couples demonstrating good knowledge after the intervention (Moodi et al. 2013). The educational program’s low efficiency violates the principle of autonomy. Furthermore the WHO states “Decisions to participate in all genetic screening programs should be voluntary and informed” (WHO 2006, chp. 1, p. 2). Yet, mandatory screening deprives the individual of the freedom to decide on ‘Not-Knowing’. Here, Shīʿī bioethics gives precedent to public good over individual decisions, in accordance with the more communitarian bioethics in Iran and in contrast to the Western understanding of autonomy. Furthermore participation and prospective choices in genetic testing/screening programs should be “substantially free from control by others” (WHO 2006, chp. 4, p. 59). However, marital decisions may have been unduly influenced by the presence of the couple’s parents “who act as custodians and ensure the health of their prospective son/daughter-in-law” (Ghanei et al. 1997, p. 155), with the parents likely having their own agenda for the marriage; couples-at-risk who decided to marry were exposed to public pressure, as the local clergy refused to register the marriage; stigmatization of female carrier may reduce their chance to find another prospective husband; arranged marriage may by itself reduce the choices for the couple-at-risk (Bittles 2012, chp. 18). Clearly, the Iranian procedure violates the right for individual autonomous decisions by exposing the couples-at-risk to social/familial pressure (WHO 2006, chp. 4, p. 31). Last, but not least, privacy, derived from the principle of autonomy, refers to the protection of unauthorized access to personal data (WHO 2006), asking for informed consent to data storage and each new investigation. The Iranian PMS includes a network of organizations storing and connecting data. Reports on the program’s efficacy refer to these data-sources, yet information on consent forms for data storage and evaluation is lacking (see for instance (Miri et al. 2013)). While absence of proof is not proof by itself, it prepares the ground for the idea that there is no such sophisticated organization of data security as is asked for in dealing with genetic data, as suggested by the WHO, resulting in a breach of privacy, violating the principle of autonomy and nonmaleficence.
To summarize, community welfare, the public good, prevails over individual autonomy in Shīʿī bioethics at practically every aspect of individual autonomy, be it informed consent, decision making or privacy.
Justice, according to PBE, describes the moral imperative for social justice of a public health system. Thus, mandatory screening should exclude a high financial burden on those screened and include the availability of the choices offered for all couples-at-risk (PND, in vitro fertilization). Furthermore, transparency is a prerequisite for egalitarian justice in healthcare allocation, that is, the parameters used for the calculation of CEA are publicly available and the relevant stakeholders should ideally be involved in the decision-making process. The Iranian screening program includes every couple intent on marriage and thus corresponds to an egalitarian intent. However, with a more communitarian view, those in need should attain more attention. Thus, populations with a high prevalence of ßTMa or those that have been demonstrated to insufficiently profit from the screening project should be awarded more attention to achieve comparable advantages (Hashemieh et al. 2015). This has been partially acknowledged (see p. 12, para. 4). Despite the Iranian strife for an all-comprehensive healthcare, out-of-pocket costs (co-payment for PND/in vitro fertilization, reimbursement of travel cost to access one of the nine PND centers) are prohibitive for most citizens (Strauss 2009). Unfortunately, transparency and stakeholder participation could not be evaluated as no English papers are available.
To summarize, the Iranian theocratic republic strives for an affordable and just healthcare system with already considerable success.13 Yet, there are still substantial problems to deliver on this promise (Doshmangir et al. 2019) as is evident with the deficiencies of the screening program. In principle the aim to deliver an egalitarian justice in healthcare is comparable in both Western and Shīʿī bioethical thinking, yet far from reality in almost every country worldwide.
3. Discussion
What conclusions can be drawn from these bioethical observations? The program started in 1991 in Shiraz. Its planning coincided with the first period of the bioethical discourse (1970–1990) in Iran (Aramesh 2015), possibly reflecting the post-colonial relations between Iran and the West. The intellectual elite active in this discourse was mostly educated in Western countries, identified itself with Western values and saw the West as a role-model for the modernization of their native country. Accepting the four-principles approach to bioethics as suggested by the WHO for the Iranian program (Samavat and Modell 2004) can be seen in line with this thinking. The instalment of the theocratic republic of Iran changed this view. Religion, that is, Shīʿī Islam serves as the defining feature of a differentiation from the West, where Western civilization is the fundamental and negative Other (Aderyani and Kiani 2015). The religious law determines all social interactions, with a still ongoing discourse on Islamic bioethics.
After the Shah regime—seen as subservient to the USA—nation-building, as observed in many post-colonial states, was not a priority. The Iran saw itself already as a great nation with a long imperial and highly developed cultural history. It aspired to resume this role. Besides military prowess, scientific success was one of the goals on the way to becoming a leading nation again.14 At this time, international journals began to require bioethical statements for published research, referring to Western standards in their instructions to the authors. Thus, accepting without restrictions the four-principles approach for the screening program—especially so as the program was supported by the WHO, with Bernadette Modell as a WHO consultant (Samavat and Modell 2004)—seemed to be a necessary first step. Yet, already from the very beginning, with the publications citing the four-principles as the bioethical background, interpretation of the four principles, especially ‘autonomy’, differed substantially from Western concepts, without stating these differences in the publications. Acknowledgement of these problems initiated the still ongoing discourse for a specific Shīʿī bioethics (Moosapour et al. 2018).
A recent publication declares that Western bioethics is to some extent inconsistent with the cultural context, customs and religion of Shīʿī Islam (Aderyani and Kiani 2015).15 Western bioethics is described as based on ‘rationalism’, ‘scientism’, ‘humanism’, and ‘secularism’, that is, CM, and thus cannot be implemented in an Islamic community, where ‘Godcentrism’, ‘pure human servitude to God’, the ‘belief in returning of humans to God’, ‘resurrection day’ and ‘human’s accountability to God’ are seen as fundamental beliefs for ethical considerations. The ‘theory of evolution’ and ‘natural selection’ means “… implementing the ‘rational utility’ project in Nazi Germany based on Hegel’s thought exemplifying the plausible outcome of this way of thinking” (citing Alexander 1949, p. 241; Aderyani and Kiani 2015, p. 31). The paper can probably be seen as representing a rather conservative spectrum of the discourse on Islamic bioethics. At the other end of the spectrum an outline of an Islamic bioethics has been drafted by Sachedina (Sachedina 2015).16 His work aims at “the universal principles based on human conditions to derive solutions to the problems in bioethics” (Sachedina 2015, p. 547), justifying these universal principles via the revelatory texts.
Analyzing both, the medical papers describing practical issues of bioethics and the more philosophical papers dealing with the justification of bioethics, a rather pragmatic picture arises. The need to state the bioethics of human research in international science journals is taken care of by referring to the Western four-principles approach. However, no reference is made to the diverging interpretation of these moral rules within the framework of Shīʿī bioethical considerations, which are used in the practical dealings with patients. Thus, presently the four-principles approach pragmatically adjusted to Shīʿī bioethical thinking prevails in practice.
Nonmaleficence or the respective principle of ‘no harm, no harassment’ of Shīʿī bioethics overlap closely. The West understands harm as primarily directed towards the individual, emphasizing the prevention of individual harm (stigmatization, choices, etc.). In contrast, in Shīʿī bioethics, the prevention of social harm, that is, harm for the healthcare community, overrides individual harm. Beneficence in Shīʿī bioethics is subservient to nonmaleficence. In this line Gert citing John Stuart Mill “a person may possibly not need the benefit of others, but he always needs that they do him no hurt” (Gert 2006, chp. 1, p. 24) sees beneficence as a moral ideal. However, professional morality extends moral rules to include beneficence as a basic morality in dealing with patients. The patients in their needs ask the physician not only to avoid putting them in harm’s way but to do them good. According to this line of thinking Beauchamps refuses to subsume beneficence under nonmaleficence (Beauchamps 2016). The concept of autonomy as defined by Beauchamps sees liberty and agency as its basic conditions (Beauchamps 2016, p. 94). Yet, the respect for autonomy is clearly not absolute. Choices undermining public health, harm others, require scarce resources could justifiably override the respect for autonomy (Beauchamps 2016, p. 96). Despite these relativizations the principle of autonomy has been challenged as expressing Western ethical imperialism in bioethics, especially so in cultural context where family- or community-informed consent prevails (Gordon 2011). Even Western countries support community-related concepts of ‘relational autonomy’ taking into account the influence of social relationship on decision making in predictive genetic testing (Zimmermann et al. 2021). Common sense, knowing that no man is an island, is aware of ‘relational autonomy’ in decision making. PBE acknowledges adaptation to social conditions as a specification of autonomy: “respect for autonomy is not exclusively individualistic to the neglect of the social nature of individuals, … emotions, … and social practices” (Beauchamps and Childress 2019, chp. 4, p. 99). Can Shīʿī bioethics by embedding the individual within the community be interpreted as ‘relational autonomy’? Sachedina holds that in contrast to the emphasis on autonomy as acting in one’s own interest, the communitarian ethics of Islam balances an individual’s well-being against the scale of general goods (Sachedina 2009, chp. 8, p. 216). Here, communitarian ethics asks to submit voluntarily to considerations of communal instead of individual interests. Childress sees this still in accordance with individual autonomy. A person may choose to yield decision making to the family or to a religious institution, exercising second-order autonomy, that is, heteronomy (Childress 1990). However, Shīʿī bioethics goes far beyond relational or heteronomous autonomy. Shīʿī bioethics is based on “the principle of public good … in cases in which the welfare of all the people is under consideration” (Sachedina 2009, chp. 2, p. 61). Thus, it is the community welfare, the public good, that prevails over individual decisions (Sachedina 2009). This is illustrated by the primacy of reducing the incidence of ßTMa over an individual’s autonomous decision, thereby legitimizing mandatory screening. Similarly, family influence in decision making, a cultural custom that represents the ‘public good’, outweighs the individual interests of couples-at-risk. Sachedina and others clearly state that there is no concept of individual autonomy in the communitarian ethics of Islam (Moosapour et al. 2018; Sachedina 2009).
PBE’s approach to a just healthcare is rather pragmatic, with a preponderance on egalitarian thinking and balancing the healthcare costs and public health resources (Beauchamps and Childress 2019, chp. 7, p. 281). However, it is difficult to achieve coherence of all issues of quality healthcare (equal access, free choice, social efficiency, etc.) in all social administration systems and one theory of justice. In the USA, more so than in most parts of Europe, the ethical considerations concerning just distribution of healthcare resources are wishful thinking. The EU, while tackling with resource allocation, for instance with its rare disease policy, does not refer to any underlying ethical strategy. In Shīʿī Islam justice is defined as “granting the right to their owners” with justice being the implementation of this right (Akrami et al. 2018, p. 56) The social dimension of justice is built on equality and the avoidance of discrimination. Distributive justice in healthcare is therefore based on egalitarian thinking. Yet, the dilemma of disability healthcare costs and the rational of allocating financial resources is not publicly discussed. It is only if peoples with disabilities such as ßTMa are treated equal with everyone else in a rating scheme then no human right is denied (Bickenbach 2021). The goal of reducing healthcare costs of ßTMa denies humans with a by-chance combination of genes the right to live, especially since treating ßTMa has been shown to be cost-effective. In summary, setting up an egalitarian healthcare system is a challenge for each and every healthcare system. Healthcare resources are always limited. Allocation or rationing occurs in most countries along a strategy of CEA. If using QALY or a simple egalitarian theory do not solve the dilemma of a just healthcare allocation, resource-allocation policy should at least be formalized and transparent. Yet worldwide, the gap between bioethical goals and reality is evident. If, however, one takes into account the historical development of the healthcare system in Iran after the revolution bioethical considerations are noticeable and necessary steps have been undertaken and we would like to conclude this paragraph with a citation of Sachedina: “There is nothing for humans to do but strive to do their best” (Sachedina 2009, chp. 2, p. 76).
To summarize, we demonstrated that the principles of nonmaleficence and justice are similar for both the Western four-principles approach and Shīʿī bioethics, while autonomy and beneficence demonstrate diverging interpretations.
Historically the initial acceptance of the four-principles approach can be interpreted as the ‘transfer of knowledge’ by the colonizing West to the colonized. Its adaptation to Iranian cultural context underscores that encounters with the colonial powers are guided by the cultural logic of the local people involved, and refutes the notion that global expansion of Western capitalism has made the “colonized” people passive objects of their own history and not its authors (Asad 1993). This corresponds well with the appropriation of the four-principles approach by Shīʿī Islamic thinking. It can be described as a transformational process, where knowledge is taken up by a society’s ‘knowledge economy’, that is, the “ensemble of its social institutions and processes producing and reproducing the knowledge at its disposal, and in particular, the knowledge on which its reproduction as a society relies” (Renn 2020, chp. 1, p. 7).
We will now proceed to investigate the claim of universality for both, the Western and the Shīʿī bioethical approach: Is there a universal morality CM or Shīʿī Islam are based upon? And if so, how do particular moralities (PM) relate to this universal morality? Further, what significance do diverging justifications have for a universal morality?
The question of universalism of morality was first brought up by Herodotus, a Greek historian (−5th century) describing customs of different societies, each claiming theirs being the right way things ought to be done. Would an ethical relativism, seen as tolerance for other cultures, deprive us of a common human basis for the judgment of right or wrong? Anthropological data are of little use here, since they only describe differences and similarities. In contrast, human ontogeny, the evolutionary process of becoming human, may offer insights in the development of a morality that is to be observed in all humans, being characteristic of their humanity. Tomasello sees human ontogeny with its evolutionary need for human cooperation—first dyadically, later culturally—as resulting in a morality of sympathy and fairness. The moral rules of CM reflect this morality of sympathy and fairness, supporting their claim on universality beyond their grounding in rationality. In bioethics, this morality of sympathy and fairness is equated to the principles of nonmaleficence, justice and beneficence, reflected in the rules of obligations and virtues, that is, moral rules and moral ideals of CM (Beauchamps 2016, chp. 2, p. 105). Here, CM is seen as “a set of norms shared by all persons committed to morality, the CM. This morality is not merely a morality, in contrast to other moralities. It is applicable to all persons, in all places, and we appropriately judge all human conduct by its standards” (Beauchamps and Childress 2019, chp. 1, p. 3). From there particular moralities (PM) are defined as containing nonuniversal, concrete and content-rich norms, based on different cultural, religious and institutional sources adapted to time and place. A PM must always be consistent with CM in order to be a morality and not merely a cultural convention. “The better a PM applies to all persons in all places the closer it is to CM” (Beauchamps and Childress 2009, p. 382; cited by Gordon 2011, p. 257). This indicates that the universal content of CM can be achieved by different means, that is, through different particular moralities (Gordon 2011).
To summarize, applying the theory of the ontogeny of human morality to CM supports the argument of a universal morality on which Beauchamps’ principlism is based upon. Here, PMs can be interpreted as pluralistic expressions of a common universal morality.
Are all four principles of “Western” bioethics or Shīʿī bioethics based on a universal morality? Both, Beauchamps and Sachedina see nonmaleficence as a universal norm, based on CM grounded in rationality or an intuitive human knowledge of right or wrong acts grounded in Shīʿī Islam, respectively. The phylogenetic and ontogenetic data provided by Tomasello support both, human rationality (Gert/Beauchamps) and intuitive knowledge (Sachedina) as the basis of bioethical thinking. Tomasello anchors human morality in a universal evolutionary development of human psychology, a cognitive and emotional development that is universally observable in each and every cultural context and characterizes us as human beings capable of cooperation due to the development of a morality of sympathy and fairness. There nonmaleficence represents the basic universal norm to enable cooperation. Healthcare justice, described as the fair-opportunity rule or according to Beauchamps, those not responsible for their disadvantages should receive help to overcome the unfortunate effects of life’s lottery of health (Beauchamps and Childress 2019, chp. 7, p. 282) refers to distributive fairness. Shīʿī Islam argues for a just healthcare based on the endowment of dignity by God. Supporting the concept of a universal fairness is the evolvement of human cooperation with its view of one’s partner or the members of the same cultural group as deserving equal treatment and the extension of a morality of sympathy beyond kin and friends to the cultural group and interpreted as an engrained human trait in part hormonally regulated. Thus, healthcare justice is part of the universal morality of sympathy and fairness. Would the above argument hold for beneficence as well? Beneficence is the foundational value of healthcare ethics for Beauchamps (Beauchamps 2016, chp. 2, p. 98), yet subsumed to nonmaleficence which is given precedent for all medical acts by Sachedina. According to Tomasello helping others may be one of the earliest signs of human morality, a morality of sympathy connected to kins and friends. With expanding cooperation helping one’s partner may become a strategic goal, ultimately supporting a common goal (Tomasello 2016). While cultural social norms do not create morality, moral judgments may be induced if nonconformity with social norms results in harm or disrespect. Thereby, social norms are connected to humans’ natural second-personal morality, that is, humans’ natural attitude of sympathy and fairness that has existed since before there were group-minded, norm-based cultural groups. This would hold for all individuals in all moral communities across all cultural contexts. There, diverging interpretations of sympathy/harm, fairness/unfairness in particular situations will refer to the natural morality shared by all humans allowing a range of definitions for cultural specifications, grounding the moral discourse in the natural morality shared by all humans. In this context the argument of beneficence as a universal morality is convincing and not impaired by the diverging interpretation of Western and Shīʿī bioethics.
Can the principle of autonomy claim universality as suggested by Beauchamps and Childress? Autonomy, as interpreted by Western thinking primarily refers to the autonomous individual, free from interferences and limitations that prevent choices, based on liberty and agency. Gert criticizes the principle of autonomy specified as autonomous actions. This, he claims, is an ambiguous concept due to the difficulties of knowing what is an autonomous act, the choice to give up drinking alcohol or choosing to continue? Due to these difficulties Gert prefers the concept of rational/irrational choices over autonomous choices (Gert et al. 2006). Additionally, autonomy defined as something that should be respected or promoted fails to distinguish between obligatory moral rules and non-obligatory moral ideals (Gert et al. 2006), disqualifying autonomy as a basic universal principle.
Beauchamps accepts limitations to individual autonomy (Beauchamps 2016, p. 96). However, it is the individual that comes first, and social restrictions are second. This is in contrast to Shīʿī bioethics were the common good is the primary goal and restrictions due to individual harm come second. There individual autonomy is an irrelevant concept. Globalization with an increase in Western lifestyles may increase the acceptance of individual autonomy. However, many ‘Westernized’ countries in Asia such as Japan or South Korea still display a more communitarian view on individual decisions, despite a superficial Western lifestyle. The individual’s responsibility for the community, the integration of the individual in the group and the restraint on individual preferences via the communal good seems the more basic cultural attitude. Individual autonomy can thus be better seen as a social construct, evolving from a secular, liberal Western viewpoint, conflicting with a more communitarian ethics, prioritizing the common vs. the individual good. While there may be some overlapping of both attitudes, differences prevail and there is no common denominator allowing to describe both attitudes as particular moralities based on an identical normative meaning. The evolutionary argument sees the development of human morality as an evolving capacity for creating effectively surviving human (tribal, later cultural) communities. Individual decisions are embedded in a communitarian approach, a ‘we > me’ concern that is part of our moral identity for dyadic interactions and group-minded ‘we’. Accepting this as part of our universal human morality the principle of autonomy will have to be denied this categorization.
To summarize, the principles of nonmaleficence and beneficence as expressed in Western bioethics or the principle of ‘no harm, no harassment’ of an emerging Shī’ī bioethics can be seen as universal principles, as expressions of a universal human morality. Furthermore, the principles of justice, an egalitarian distributive justice in healthcare, corresponds to a morality of fairness, described as a universal principle by Tomasello. In contrast, the Western principle of autonomy may be interpreted as a social norm, confined to Western secular and liberal thinking, a cultural norm not grounded in universal morality.
4. Conclusions
This paper compares Western bioethics, pertaining to the four-principles approach, to the bioethical discourse of Shīʿī Islam in Iran and the concept of Sachedina’s Islamic bioethics. We described the bioethical challenges of the Iranian program to reduce the prevalence of ßTMa. While the program has reportedly been in accordance with the four-principles approach, a detailed analysis demonstrated its interpretation of the principles according to Shīʿī bioethics with the subsequent divergences from the recommendation of the WHO and UNSECO. While nonmaleficence and justice were interpreted similarly, beneficence is not seen as an independent principle but subsumed to nonmaleficence in Shīʿī bioethics. Finally, individual autonomy has no correspondence in the more communitarian bioethics of Shīʿī Islam.
We present arguments supporting the claim of universality for nonmaleficence, justice and beneficence as part of the ontogeny of human morality. The different justifications of the principles by CM or Shīʿī Islam presented by Sachedina do not affect their claim on universality. Shīʿī bioethics represents a particular morality, in accordance with CM, respecting the sensitivity of Islamic belief, adjusted to time and customs of Shīʿī Islam.
In contrast, autonomy claimed as a universal principle by Western bioethics has evolved as a principle of secular liberalism, failing to account for the more communitarian aspect of human morality that evolved with cooperation. The ontogeny of human morality thus does not support autonomy as a universal principle.
Author Contributions
Conceptualization, U.P. and U.A.; investigation, U.P.; writing—original draft preparation, U.P.; writing—review and editing, U.P. and U.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no Funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Glossary
| Allele | An allele is a variant form of a gene, at the gene’s specific place on a chromosome. With the pairing of chromosomes during fertilization two genes are paired. If the two paired genes contain the same allele, the gene is homozygote, with different alleles heterozygote with respect this gene. |
| Belmont Report | The Belmont Report was commissioned by the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research (USA). The Commission, created as a result of the National Research Act of 1974, was charged with identifying the basic ethical principles that should underlie the conduct of biomedical and behavioral research involving human subjects and developing guidelines to assure that such research is conducted in accordance with those principles. For details see https://www.hhs.gov/ohrp/regulations-and-policy/belmont-report/index.html, accessed on 28 August 2021. (Department of Health and Human Services (HHS) 2021) |
| Beta-thalassemia major (ßTMa) | ßTMa is characterized by mutations on chromosome 11, encoding the ß-chain of hemoglobin A, i.e., the oxygen carrier-protein in red blood cells consisting of 2 a- and 2 ß-chains. Without functional ß-chains (ß0), i.e., a genotype of ß0/ß0, ßTMa, the most severe form of thalassemia, will occur. Intermediate forms, genotype ß0/ß+, or ß+/ß+, (ß+, partial function of the ß chain) are defined as ß-thalassemia intermedia, while those least affected are heterozygous with a genotype ß/ß+ or ß/ß0, resulting in mild anemia, i.e., ß-thalassemia minor (ßTMi). So far, 52 different mutations, with different mutations in 21% of consanguineous couples, indicate the heterogenous picture of ßTMa in Iran. These genetic variants result in different phenotypes. Predicting these phenotypes, i.e., classifying the disease into categories of severe or intermediate, requires costly genetic screening (Rahimi 2013). ßTMi requires no medical treatment, while those with ßTMa require regular blood transfusions. Regular blood transfusions lead to iron-overload necessitating chelation therapy, i.e., iron is bound to a chelating agent which then is excreted. Despite and in part related to transfusion therapy, patients with ßTMa suffer major complications of the disease, such as a reduced growth rate in children, diabetes mellitus (5.4%), heart failure (6.4%), cardiac arrhythmias (5.0%), hypothyroidism (11.6%), hypoparathyroidism, adrenal insufficiency and hypogonadism (reduced sexual function and/or infertility, 55%), thrombosis (1.1%) and HIV infection (1.8%). Antibody formation, i.e., alloimmunization prohibits further transfusion therapy. Today, therapy offers patients a life expectancy well into adulthood with integration into employment and marriage. However, ultimately the patients die of the disease mostly due to heart failure. In the United Kingdom up to the year 2000 50% of patients died before age 35 years, today 80% of the patients live longer than 40 years (Borgna-Pignatti et al. 2006; Needs et al. 2022). |
| Bonobo | Pan paniscus, i.e., a pygmy chimpanzee, one of the two species making up the genus Pan. Scientifical classification: Kingdom: Animalia, Phylum: Chordata, Class: Mammalia, Order: Primates, Suborder: Haplorhini, Infraorder: Simiiformes, Family: Hominoidae, Subfamily: Hominidae, Tribe: Homini, Genus: Pan, Species: P. paniscuis (Schwartz 1929). |
| Carrier status | A “genetic” carrier is a carrier of either an autosomal recessive disease or of a X-linked disorder or a balanced chromosomal rearrangement. Being a carrier does usually not affect the carrier’s health but could have consequences for the offspring (Borry et al. 2013). |
| Clinical | Clinical refers to the direct observation of the patient. In clinical medicine medical the physician assesses patients in order to diagnose, treat or prevent disease. |
| Communitarianism | Communitarian justice holds a just distribution to each person according to principles of fair distribution derived from concepts of the good developed in moral communities (Beauchamps and Childress 2019). |
| Cost effectiveness analysis (CEA) | A strategy on which heath care resource rationing is based. If healthcare is defined as a “health need”, health resource efficiency, i.e., the ultimate goal of CEA using health resources to minimize ill health without wasting resources, is asked for. To achieve distributive fairness parameters of healthcare metrics (for instance quality-of-life years (QUALY) as a metric for the benefit achieved) and efficiency as the costs of achieving a benefit, are balanced for a prioritization strategy. However, the inherent problems with CEA and QUALY, i.e., the aggregation problem, the priority problem, the problems of “democracy” and indirect benefit will have to be considered17 and lastly the fair vs. the best outcome problem, a tension between a utilitarian approach vs. an egalitarian concern for fairness. Added to these are the problematic interpretations of QUALY or disability-adjusted life years (DALY) as the indicators for benefit in the CEA calculations.18 CEA is used most often on an institutional level, many of its decision hidden in hospital reimbursement policies or clinical guidelines. Due to the difficult process of gaining reliable data, most healthcare budgets are due to an interplay of politics and bureaucratic pressure or the ability to pay, all highly ineffective as demonstrated by Doshmangir et al. for the Iranian system (Doshmangir et al. 2019; Doshmangir et al. 2016). |
| Declaration of Geneva | Details and new versions of the “Declaration of Geneva” are to be found https://www.wma.net/what-we-do/medical-ethics/declaration-of-geneva, accessed on 24 August 2021, (World Medical Association 1948) |
| Declaration of Helsinki | The “Declaration of Helsinki” states the ethical principles for medical research involving human subjects. For details see https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/, accessed on 8 August 2021, (World Medical Association 2013) |
| Deontology | In moral philosophy, deontological ethics is the normative ethical theory that the morality of an action should be based on whether that action itself is right or wrong under a series of rules, i.e., based on an inherent rightness of the established rules, rather than based on the consequences of this action. It is sometimes described as duty-, obligation- or rule-based ethics (Alexander and Moore 2020). Deontological ethics argues with formal criteria such as equality or impartiality (Britannica 2021). |
| Egalitarian theories | Egalitarian theories of justice hold to each person an equal measure of liberty and equal access to goods in life that every rational person values; |
| European Rare Diseases (E-RARE) and European Reference Networks (ERNs) | E-RARE, the EU’s strategic objective for rare diseases is to improve patient access to diagnosis, information and care. It assists in pooling scarce resources spread across the EU, enabling patients and professionals to share expertise and information. https://ec.europa.eu/health/non_communicable_diseases/rare_diseases_de, accessed on 27 June 2021. ERNs, Health systems in the European Union aim to provide high-quality, cost-effective care. This is particularly difficult, however, in cases of rare or low-prevalence complex diseases which affect the daily lives of around 30 million EU citizens. European Reference Networks (ERNs) are virtual networks involving healthcare providers across Europe. They aim to facilitate discussion on complex or rare diseases and conditions that require highly specialized treatment, and concentrated knowledge and resources. https://ec.europa.eu/health/ern_de, accessed on 27 June 2021. |
| fatwa | The authoritative ruling of a religious scholar on questions (masāʾel) of Islamic jurisprudence that are either dubious or obscure in nature (šobohāt) or which have newly arisen without known precedent (mostaḥdaṯāt). The query eliciting a fatwā may, however, relate to an existing ordinance (ḥokm) of Islamic law, unknown to the questioner, or to its application to a specific case or occurrence; the fatwā then functions simply as a clarification of the relevant ordinance (tabyīn-e ḥokm). Although the fatwā is typically concerned with legal matters, doctrinal considerations are necessarily involved whenever a fatwā results in takfīr, the condemnation of individuals or groups as unbelievers. The ruling provided in a fatwā is not intrinsically obligatory, for it is essentially an expression of learned opinion. In Shī’ī Islam, however, the authority to deliver a fatwā is generally restricted to the mojtahed, the jurist equipped to deduce the specific ordinances of the law (forūʿ) from its sources (oṣūl), and obedience to the mojtahed of their choice—designated as marjaʿ-e taqlīd—is incumbent on all who lack the same learned qualifications; to follow the ruling given in the fatwā of a mojtahed is therefore obligatory for those who solicit it. |
| Foundationalism | “Foundationalism is a view about the structure of justification or knowledge. The foundationalist’s thesis in short is that all knowledge or justified belief rest ultimately on a foundation of non-inferential knowledge or justified belief” (Hasan and Fumerton 2018). |
| Gene co-culture of human behavior | Tomasello refers to genetic adaptation based on the interaction of changes in both, the natural environment and cultural settings. According to Toby and Cosmides evolutionary psychology (EP) primarily explores the design of the universal, evolved psychological and neural architecture that we all share by virtue of being human. EP is usually less interested in human characteristics that vary due to genetic differences because, as these differences are unlikely to be evolved adaptations central to human nature. Of the three kinds of characteristics that are found in the design of organisms—adaptations, by-products, and noise—traits caused by genetic variants are predominantly evolutionary noise, with little adaptive significance, while complex adaptations are likely to be universal in the species” (Tooby and Cosmides 2005, p. 39; Downes 2021). “Evolution acts through genes, but it acts on the relationship between the genes and the environment. The environment is as much part of the process of evolutionary inheritance as are the “genes” and equally as “biological” and “evolved” (Tooby and Cosmides 1990, p. 20). |
| Genetic counselling | The process of genetic counselling is complex and includes (i) the interpretation of family and medical histories to assess the risk of disease occurrence/recurrence; (ii) education about inheritance, testing, management, prevention, resources and research and (iii) counselling to promote informed choices and adaptation to the risk or condition (Bittles 2012, chp. 13, p. 204). |
| Good Clinical Practice | The guidelines for Good Clinical Practice (GCP) were initiated in the USA in 1977, homogenized with Japan and the European Union (EU) in 1996 and legalized into the Medicines Act (Arzneimittelgesetz) in Germany in 2004. There all practical details for clinical studies are regimented. For details see https://ichgcp.net/de#, accessed on 15 April 2021. (Bundesministerium für Justiz und Verbraucherschutz 2021; ICH 2021; Irrgang 2015; World Medical Association 2013) |
| Healthcare resources | Seen as for instance treatment, interventions, medication, rehabilitation, health care services and service providers, etc. They are scare due to the allocation of funds of the government budget are or intrinsically scare as for instance transplantable organs. |
| Homozygous/heterozygous | Zygosity is the degree to which both copies of a chromosome or gene have the same genetic sequence, i.e., the same form of gene. With both alleles of the gene the same, the organism is homozygous at this locus. If they are different the organism is heterozygous (Cambridge Dictionary). https://dictionary.cambridge.org/dictionary/english/homozygous, accessed on 2. April 2021. |
| Human Radiation Experiments | Experiments performed in the USA exposing humans to radioactive material without informed consent. The information on these experiments was published after President Bill Clinton formed the Advisory Committee on Human Radiation Experiments (ACHRE, 1994) https://ehss.energy.gov/ohre/roadmap/achre/summary.html, accessed on 2 April 2021. |
| Ijtihād | independent legal thinking and hermeneutics |
| Intuitionalism | The classic intuitionists maintained that basic moral propositions are self-evident—that is, evident in and of themselves—and so can be known without the need of any argument. Intuition is immediate apprehension by the understanding. It is the way that we apprehend self-evident truths, general and abstract ideas, “and anything else we may discover, without making any use of any process of reasoning (Stratton-Lake 2020). |
| Istiṣlāh | istiṣlāh means seeking the common good, considerations of public good; a source of legislation that requires balancing all aspects of benefit and harm that are included in the three goals of the Sharī’a. |
| Joint intentionality | The “skill and motivation to construct with others an interdependent, plural-agent ‘we’” (Tomasello 2016, chp. 1, p. 4). This interdependence goes beyond a sense of sympathy towards kins and friends, an oxytocin-based social emotion of sympathy. Thus, joint, i.e., shared intentionality gives rise to the change from strategic cooperation to genuine morality. “This new form of interdependence meant that early human now extended their sense of sympathy beyond kin and friend to collaborative partners” (Tomasello 2016, chp. 1, p. 4). Joint intentionality presupposes cognitive, psychological skills of “common-ground understanding of the ideal way that each role has to be played for joint success. These common ground ideals may be thought of as the original socially shared normative standards” (Tomasello 2016, chp. 1, p. 4). |
| Libertarian theories | Libertarian theories of justice pertain to each person a maximum of liberty and property resulting from the exercise of liberty rights and participation in fair free market exchange (Beauchamps and Childress 2019). |
| Morality of Sympathy | Morality of sympathy describes a kin- and friendship-based prosociality found in human’s last common ancestors, based on oxytocin induced social emotion of sympathy (Tomasello 2016, p. 31). The psychological characteristics of a morality of sympathy can be described as based on cognition (individual intentionality for flexible and informed decisions, as well as understanding and predicting the intentional states of others for purposes of competition), social motivation (i) the capacity to form social relations of dominance and friendship; (ii) the capacity to have and express basic emotions and recognize these emotions in others; (iii) the capacity to communicate intentionally and (iv) the sympathy based motivation to help others instrumentally, especially kin and friends) and self-regulation (the ability to control impulses for immediate self-gratification and the ability to collaborate with others to produce new resources) (Tomasello 2016, p. 35). Most importantly this morality of sympathy still lacks any socially normative sense of fairness or justice concerning how they “ought” to treat others or how others “ought” to treat them (Tomasello 2016, p. 36). |
| Mu’tazilah theology | Originally the term meant political or religious neutralists. Later (10th century) Mu’tazilah refers to a school of speculative theology using the methods of Hellenistic philosophy to develop three distinct dogmatic points: First, the absolute uniqueness of God, concluding that the Qur’ān could not be the word of God, as God had no separable parts. The Qur’ān was therefore created and not coeternal with God. Second, due to God’s justice God desires for only the best for man, but through free will man choses between good and evil and becomes responsible for his actions. Third, due to God’s justice God must reward the good and punish the evil. These premises are accepted by Shī’ī Muslim (Britannica 2020) Mu’tazilis’ rationalist theology; Muʿtazilah a major theological school of Islam was renowned for holding reason (ʿaql) above scripture and other sources of religious knowledge and for its development of the method of dialectical theology (ʿilm al-kalām) (El Omari 2016). Mu’tazilites are the followers of the rationalist-naturalist theology that privileged human reason the ability to know moral truth (Sachedina 2009, chp. 2, p. 32). |
| Nuremberg Code | The ten articles of the Nuremberg Code, as defined by “Trials of War Criminals before the Nuremberg Military Tribunals under Control Council Law No. 10”, Vol. 2, pp. 181-182. Washington, D.C.: U.S. Government Printing Office, 1949 are indicated via the NIH website https://history.nih.gov/display/history/Nuremberg+Code, accessed on 24 August 2021 (National Institute of Health 2021). |
| Ontogeny | Ontogeny describes the development of an organism during the lifetime of an individual organism, in contrast to the evolvement of species (phylogeny). There, a causal explanation of a phenomenon relates to the interplay of genes and mechanical forces, i.e., genetics and physics (Love 2022). |
| Oxytocin | A peptide-hormone secreted from the pituitary gland, it effects, via g-protein coupled receptors, milk ejection during lactation, uterine contractions during labor and may play a role in sexual arousal. Psychologically oxytocin positively affects in-group bonding, enhancing prosocial behavior by facilitating trust and attachment between in -group members, increasing empathy during perspective taking, and conditioned reward learning. For details see reference (Jurek and Neumann 2018). |
| Primary care genetic counselling network | A primary care genetic counselling network was set up as suggested by the WHO (Samavat and Modell 2004; WHO 1993, 1998) The counselling team comprises a physician and a professional (BSc.) in health studies, trained by specialists of the National Genetics Committee. Information of the public as well as target groups is organized via a national multidisciplinary educational committee, linked to corresponding provincial committees, and further down the line to primary care centers. In addition, high school students and young men in the military are educated about thalassemia. The judiciary is linked to the program through annual meetings for marriage registrars (many of whom are clergy). Laboratory services are provided by an accredited national professional laboratory network, supervised by a national reference laboratory and directorate for laboratory affairs. Laboratory staff follows national screening protocols based on international guidelines, participate in quality control, and attend regular educational courses. Data (number of couples counselled, their choice, referrals to DNA laboratories, follow-up on carrier couples and children born with thalassemia) from genetic counselling and primary care health houses are reported to the genetic offices, which report back and serve as a surveillance system. The screening process using the respective markers for thalassemia follows the flow chart provided by the WHO (see Figure 1). |
| QUALY | Quality adjusted life years are calculated as the QoL ranging from 0 (death) to 1 (perfect) multiplied with the respective life expectancy. For instance, (i) if the QoL is 0.3 and the life expectancy 5 years then the QUALY is 1.5; (ii) the British National Institute for Health and Care Excellence sees any medications with costs more than 300,000 pounds per QUALY as not cost-effective (Meissner 2010). |
| Rare Disease Policy of the EU | The EU created an operational framework in the field of rare diseases, opting for cross-border healthcare and coordination of classifications, codifications, European Reference Networks, orphan medicinal products and expert group on rare diseases, putting rare diseases in a privileged position in the health care agenda (Moliner and Waligora 2017). https://health.ec.europa.eu/non-communicable-diseases/steering-group/rare-diseases_de accessed on 27 June 2021. European Reference Networks: https://health.ec.europa.eu/european-reference-networks/overview_en, accessed on 27 June 2021. |
| Reflective equilibrium | Reflective equilibrium is the end-point of a deliberative process in which we reflect on and revise our beliefs about an area of inquiry, moral or non-moral. The inquiry might be as specific as the moral question, “What is the right thing to do in this case?” or the logical question, “Is this the correct inference to make?” Alternatively, the inquiry might be much more general, asking which theory or account of justice or right action we should accept, or which principles of inductive reasoning we should use. We can also refer to the process or method itself as the “method of reflective equilibrium” (Daniels 2020). Reflective equilibrium describes a position of reciprocal relationship between moral principles and casuistry, i.e., case-based reasoning, a process by which our considered responses to actual cases influence our moral principles, and those improved-upon principles then provide enhanced guidance for our responses to further cases. Reflective the source of the source of coherentism, with the appeal to the common morality meant to provide a foundation. Beauchamp and Childress accord foundational status to the common morality, and it is the common morality that underwrites their four principles (autonomy, non-maleficence, beneficence and justice) (Flynn 2021). |
| Relational autonomy | Relational autonomy is seen as a procedural conception of autonomous and self-reflective decisions of competent individuals, emphasizing the influence of the social environment on self-reflectiveness. Thus, instead of individual autonomy Zimmermann et al. take into account the social influence of i) relatives, as especially predictive genetic testing impinges on the interest of relatives, their right “to know” or “not to now” as this may lead to competing interests; and ii) healthcare professionals despite nondirective counselling (Zimmermann et al. 2021). |
| Second-personal agency | Second-personal agency refers to the interdependent collaborative activities structured by joint intentionality that fostered in participants a new kind of cooperative rationality … particular collaborative activities had role ideals—socially normative standards—that applied to either of them indifferently, which implied a kind of self-other equivalence. Based on the recognition of self-other equivalence, there arose a mutual respect between partners, and a sense of mutual deservingness of partners, thus creating second-personal agents (Tomasello 2016). |
| Second-personal morality | Second-personal morality can be described as the sense of mutual deservingness emerging from joint activity. Thus, second-person morality is a “dyadic morality of face to face interactions between agents collaborating, and feeling responsible to one another, as a jointly committed ‘we’” (Insern-Mas and Gomila 2022, p. 202). |
| Teleological ethics | Teleological ethics refer to normative ethical theory based on the goodness of the consequences of an action. It is based on the good, valuable and desirable. Teleological ethics argues with material or substantive criteria such as happiness or pleasure (Britannica 2021). |
| Tuskegee Study | The United States Public Health Service (USPHS) initiated a study “The Tuskegee Study of Untreated Syphilis in Negro Males” (USPHS Syphilis Study at Tuskegee) in 1933. There participants had been neither given informed consent to the study and despite the availability of penicillin since 1943, were not offered treatment. When the study details became public in 1972 the study was closed and free medical care for survivors of the study was initiated in 1973, which was later extended to the widows and children of the participants. In 1997 President Clinton issued a formal Presidential Apology (The United States Public Health Service 2021). https://www.cdc.gov/tuskegee/timeline.htm, accessed on 11 July 2021. |
| Twelfer Shi’ah | The Twelvers believe that, at the death of the Prophet Muhammad in 632 CE, the spiritual-political leadership (the imamate) of the Muslim community was ordained to pass down to ʿAlī, the Prophet’s cousin and son-in-law, and then to ʿAlī’s son Ḥusayn and thence to other Imams down to the 12th, Muḥammad ibn al-Ḥasan, who is understood to have been born circa 870 but to have gone into occultation (Arabic ghaybah; Persian ghaybat)—a state of concealment by God—soon after his father’s death circa 874. The “Hidden Imam,” as he is sometimes called, is considered to be still alive and will return when God determines it to be appropriate and safe (Newman 2019). |
| Ummah | Ummah literally means community. It is a synonym for ummat al-Islām, the Islamic community, i.e., the collective community of Islamic people. In the Qur’an the ummah typically refers to a single group that shares common religious beliefs, specifically those that are the objects of a divine plan of salvation. |
| Universal Declaration on Bioethics and Human Rights | For details see https://www.unesco.org/en/legal-affairs/universal-declaration-bioethics-and-human-rights (accessed on 3 May 2021). (UNESCO 2005) |
| Uṣūl al-fiqh | Islamic legal theory |
| Utilitarianism | A utilitarian approach to justice, i.e., to each person according to rules and actions that maximize social utility (Beauchamps and Childress 2019) |
Notes
| 1 | Within the framework of this paper the ‘West’ comprises the cultural sphere of influence of Europe and populations originating from Europe as the Americas and Australasia. Specifically, ‘Western’ thinking is defined by a postcolonial view where the ‘West’ (the ‘Occident’) and the ‘East’ (the ‘Orient’) are seen as opposing and mutually dependent (Said 2003). Thus, any comparison between ‘Western’ bioethical thinking and the bioethics of Shī’ī Islam will have to take into account this interdependence and the interpretation of the claim of universality of ‘Western’ bioethics as possibly Eurocentric. |
| 2 | Medical bioethics covers clinical bioethics, scientific investigations into humans and healthcare ethics. Due to our specific focus on medical bioethics, we abstain from using the additional term ‘medical’ throughout. |
| 3 | For in-depth discussion on the universality of human rights and the related religious discourse see (Auga 2020). |
| 4 | A glossary is provided as a supplementary file, covering special medical and Islamic expressions. |
| 5 | Here, different groups may diverge, creating multiple, particular moralities (PM), for instance a religious morality. For example, if prayers before all public meetings are required, this rule cannot include those in society who do not share this belief/practice. This limitation is a disadvantage inherent in PM operating in pluralistic societies. On the other hand, the advantages of a PM, retaining universal morality, is the possible richness and specificity that are lacking in universal morality. |
| 6 | Gert holds that the concept of irrationality makes it easier to grasp rationality (Gert 2006). |
| 7 | Examples for rational beliefs may be: all people are mortal, people can kill other people, cause pain, disable another; people generally do not want to have pain inflicted on them or to be disabled; and persons can deprive others of their freedom, but people generally do not want to be so deprived (Gert 2006, ibid., chp. 2, p. 88ff). |
| 8 | There bioethical rulings by Shīʿī Ayatollah Ali Sistani (Iraq) such as mandatory cardiovascular resuscitation for Muslim, but not for Non-Muslim, would not be possible due to the prohibition of religion-based discrimination (Mavani 2014). |
| 9 | For instance, religious guidance on bioethical issues may specify divine rewards or punishments to guarantee obedience (Moosapour et al. 2018). |
| 10 | ‘Independent’ reason is understood as a reasoning that is based on the prior notion that the revelation is true and as such is the major source of knowledge of the duties prescribed by the Sharī’a. |
| 11 | The concept of autosomal recessive disease is difficult to understand, for instance a 25%-risk misunderstood as the birth of one child with illness followed by three healthy children. Many Islamic societies belief that more genetic information is passed on by the father than the mother, thus the disease would only to be expected through cousin-marriage on the paternal side of the family. Being carrier of a disease and being healthy is often difficult to accept, especially from the fathers’ side of the family, preferentially redirecting the responsibility of an inherited disease exclusively on the mother. These difficulties are exacerbated by insufficient genetic knowledge of healthcare providers (Bittles 2012). |
| 12 | For instance misinterpretations of the carrier status as the presence of disease leading to discrimination in insurance/employment or relating responsibility for the disease only to the female carrier (Bittles 2012, ibid. 13, pp. 193–94). |
| 13 | Indicators of healthcare quality (life expectancy, maternal mortality rate, access to healthcare, population/physician ratio, etc.) increased substantially. By 2019 92% of the population were covered by at least one health insurance system and individual out-of-pocket payments decreased from 54% to 41%, yet still far from the goal of 30%. (Doshmangir et al. 2019). |
| 14 | Auditing peer-revied publications demonstrated for 1990: 37 medical papers, 60% with an impact factor (IF) < 1; for 2007: 3176, 70% with an IF > 1 (Azizi 2009). |
| 15 | The paper is part of medical ethics PhD thesis, with the last author Head of the Department of Medical Ethics at the Shahid Beheshti University of Medical Sciences in Teheran. |
| 16 | Abdulaziz Sachedina is a Muslim American citizen born in Tanzania, working as Professor of Islamic Studies at George Mason University, Fairfax, Virginia, and as such does not represent the Iranian religious elite. |
| 17 | An aggregation problem occurs when a low-cost and low-benefit procedure widely used will rank higher than a high-cost and high-benefit but rarely used procedure; the priority problem that impacts the equality and impartiality of healthcare, i.e., should the one with higher needs of these resources have priority? And if this is the case, how do we determine those “worst off”, the deaf or the blind? the democracy problem asks whose values will be decisive, the community who pays for the resources or some bureaucratic elites; the problem of indirect benefits, i.e., health is not an individual problem, a healthy person benefits the society by working, paying higher taxes, etc. Problems arise with the quantification of these benefits and how are these societal benefits merged with healthcare organization. |
| 18 | For instance, (i) the idea that QoL indicates an objective degree of well-being independent of the underlying disease. Yet, adaptation and adjusting processes of the disabled person may result in the “disability paradox” with a significantly less reduced QoL than estimated by a healthy person. It is a well-known phenomenon that life is the more valuable the less is left. The example indicates that QoL metric denies the fact that there is no persistent value of any resource across a population and time (Bickenbach 2021); (ii) the overall burden of a disease (effects on employment, social functioning, stigmatization, etc.) afflicts QoL-metric. As the burden of living with a disability is caused as much by the social environment as by the disease, we would have to include the problems of a failed policy to combat stigma and lack of accommodation, as healthcare by itself would not increase the overall QoL situation ibid. |
References
- Aderyani, Mohsen Rezaei, and Mehrzad Kiani. 2015. A Comparative Study of the Foundations of Medical Ethics in Secular and Islamic Thought. Journal for the Study of Religions and Ideologies 14: 27–46. [Google Scholar]
- Adib-Hajbaghery, M., M. Ahmadi, and S. Poormansouri. 2015. Health Related Quality of Life, Depression, Anxiety and Stress in Patients with Beta-Thalassemia Major. Iranian Journal of Pediatric Hematology and Oncology 5: 193. [Google Scholar] [PubMed]
- Akrami, Forouzan, Abbas Karimi, Mahmoud Abbasi, and Akbar Shahrivari. 2018. Adapting the prinicples of biomedical ethics to Islamic principles and values in the context of public health policy. Journal for the Study of Religions and Ideologies 17: 46–59. [Google Scholar]
- Alexander, L. 1949. Medical Science under Dictatorship. New England Journal of Medicine 241: 39–47. [Google Scholar] [CrossRef]
- Alexander, L., and M. Moore. 2020. Deontological Ethics. Available online: https://plato.stanford.edu/archives/win2020/entries/ethics-deontological/ (accessed on 7 June 2021).
- Alexandra, Andrew, and Seumas Miller. 2009. Ethical theory, “common morality”, and professional obligations. Theoretical Medicine and Bioethics 30: 69–80. [Google Scholar] [CrossRef]
- Ansari-Moghaddam, Alireza, Hossein Ali Adineh, Iraj Zareban, Mehdi Mohammadi, and Mahtab Maghsoodlu. 2018. The survival rate of patients with beta-thalassemia major and intermedia and its trends in recent years in Iran. Epidemiology and Health 40: 9. [Google Scholar] [CrossRef]
- Aramesh, Kiarash. 2015. A Brief History of Biomedical Research Ethics in Iran: Conflict of Paradigms. Developing World Bioethics 15: 107–12. [Google Scholar] [CrossRef]
- Arras, John D. 2009. The hedgehog and the Borg: Common morality in bioethics. Theoretical Medicine and Bioethics 30: 11–30. [Google Scholar] [CrossRef]
- Asad, Talal. 1993. Genealogies of Religion. Discipline and Reasons of Power in Christianity and Islam. Baltimore and London: The John Hopkins University Press. [Google Scholar]
- Auga, Ulrike E. 2020. Human Rights, Gender and Religion: Controversies in Political, Social, Cultural and Sexuality Discourse. In An Epistemology of Religion and Gender: Biopolitics–Performativity–Agency. London and New York: Routledge. [Google Scholar]
- Azizi, Farhad. 2009. Medical Education in the Islamic Republic of Iran: Three Decades of Success. Iranian Journal of Public Health 38: 19–26. [Google Scholar]
- Beauchamps, Tom L. 2003. Ä defense of the common morality. Kennedy Institute of Ethics Journal 13: 259–74. [Google Scholar] [CrossRef]
- Beauchamps, Tom L. 2016. Principles of Biomedical Ethics. In The Principles of Biomedical Ethics as Universal Principles; Islamic Perspectives on the Principles of Biomedical Ethics. Edited by Mohammed Ghaly. London: World Scientific Publisher, pp. 89–120. [Google Scholar]
- Beauchamp, Tom L., and James F. Childress. 2009. Principles of Biomedical Ethics, 6th ed. New York: Oxford University Press. [Google Scholar]
- Beauchamps, Tom L., and James F. Childress. 2019. Principles of Biomedical Ethics, 8th ed. New York: Oxford University Press. [Google Scholar]
- Bickenbach, Jerome. 2021. Disability and Health Care Rationing. Available online: https://plato.stanford.edu/archives/spr2021/entries/disability-care-rationing (accessed on 8 August 2021).
- Bittles, Alan H. 2012. Consanguinity in Context. Cambridge: Cambridge University Press. [Google Scholar]
- Borgna-Picatti, Caterina, Simone Rugolotto, Piero De Stefano, Antonio Piga, Felicia Di Gregorio, Maria Rita Gamberini, Vincenzo Sabato, Caterina Melevendi, Maria Domenica Cappellini, and Giuseppe Verlato. 2006. Survival and Disease Complications in Thalassaemia Major. Annals New York Academy of Sciences 850: 227–31. [Google Scholar] [CrossRef] [PubMed]
- Borry, Pascal, Marieke Teeuw, and Martina C. Cornel. 2013. Genetic Testing and Counseling in the Case of Consanguinity: Facts, Ethical and Legal Consequences. In Currents of Encounter. Studies on the Contact between Christianity and other Religions, Beliefs, and Cultures. Looking Beneath the Surface. Medical Ethics from Islamic and Western Perspectives. Edited by Hendrik M. Vroom, Petra Verdonk, Marzouk Aulad Abdellah and Martina C. Cornel. Amsterdam: Rodopi, vol. 8. [Google Scholar]
- Britannica. 2020. Muʿtazilah. Available online: https://www.britannica.com/topic/Mutazilah (accessed on 17 July 2021).
- Britannica. 2021. Normative Ethics. Available online: https://www.britannica.com/topic/normative-ethics (accessed on 29 April 2021).
- Bundesministerium für Justiz und Verbraucherschutz. 2021. Gesetz über den Verkehr mit Arzneimitteln. Available online: https://www.gesetze-im-internet.de/amg_1976/ (accessed on 19 April 2021).
- Cao, Antonio, and Yuet Wai Kan. 2013. The Prevention of Thalassemia. Cold Spring Harbor Perspectives in Medicine 3: 1–15. [Google Scholar] [CrossRef] [PubMed]
- Childress, James F. 1990. The Place of Autonomy in Bioethics. The Hastings Center Report 20: 12–17. [Google Scholar] [CrossRef] [PubMed]
- Daniels, Norman. 2020. Reflective Equilibrium. Available online: https://plato.stanford.edu/archives/sum2020/entries/reflective-equilibrium/ (accessed on 30 April 2021).
- Doshmangir, Leila, Arash Rashidian, Mehdi Jafari, Hamid Ravaghi, and Amirhossein Takian. 2016. Fail to prepare and you can prepare to fail: The experience of financing path changes in teaching hospitals in Iran. BMC Health Services Research 16: 138. [Google Scholar] [CrossRef]
- Doshmangir, Leila, Mohammad Bazyar, Reza Majdzadeh, and Amirhossein Takian. 2019. So Near, So Far: Four Decades of Health Policy Reforms in Iran, Achievements and Challenges. Archives of Iranian Medicine 22: 592–605. Available online: http://www.aimjournal.ir/Article/aim-7991 (accessed on 24 August 2021). [PubMed]
- Downes, Stephen M. 2021. Evolutionary Psychology. In The Stanford Emcyclopedia of Philosophy. Edited by Edward Nouri Zalta. Available online: https://plato.stanford.edu/archives/spr2021/entries/evolutionary-psychology/ (accessed on 24 August 2021).
- El Omari, R. 2016. The Mu’tazilite Movement(I): The origin of the Mu’tazila. Oxford: Oxford University Press. [Google Scholar]
- Esmaeilzadeh, Firooz, Azita Azarkeivan, Sara Emamgholipour, Ali Akbari Sari, Mehdi Yaseri, Batoul Ahmadi, and Mohtasham Ghaffari. 2016. Economic Burden of Thalassemia Major in Iran. Journal of Research in Health Science 16: 111–15. [Google Scholar]
- Esmaeilzadeh, Firooz, Batoul Ahmadi, Sajad Vahedi, Saeed Barzegari, and Abdolhalim Rajabi. 2021. Major Thalassemia, Screening or Treatment: An Economic Evaluation Study in Iran. International Journal of Health Policy and Management 11: 1112–19. [Google Scholar] [CrossRef]
- Flynn, Jennifer. 2021. Theory and Bioethics. Available online: https://plato.stanford.edu/archives/spr2021/entries/theory-bioethics (accessed on 19 April 2021).
- Gert, Bernard. 2006. Common Morality: Deciding What to Do. Available online: https://academic.oup.com/book/8298 (accessed on 1 June 2021).
- Gert, Bernard, Charles M. Culver, and K. Danner Clouser. 2006. Bioethics: A Systematic Approach. New York: Oxford University Press. [Google Scholar]
- Ghanei, M., P. Adibi, M. Movahedi, M. A. Kham, R. L. Ghasemi, T. Azarm, B. Zolfaghari, H. R. Jamshidi, and R. Sadri. 1997. Pre-marriage prevention of thalassaemia: Report of a 100,000 case experience in Isfahan. Public Health Genomics 111: 153–56. [Google Scholar] [CrossRef]
- Gordon, John-Stewart. 2011. Global Ethics and Principlism. Kennedy Institute of Ethics Journal 21: 251–76. [Google Scholar] [CrossRef] [PubMed]
- Hadipour Dehshal, Mahmoud, Mehdi Tabrizi Namini, Razieh Hantoushzadeh, and Sakineh Yousefi Darestani. 2019. β-Thalassemia in Iran: Things Everyone Needs to Know About This Disease. Hemoglobin 43: 166–73. [Google Scholar] [CrossRef]
- Haider, Najam. 2014. Shi’i Islam: An Introduction. Cambridge: Cambridge University Press. [Google Scholar]
- Hasan, Ali, and Richard Fumerton. 2018. Foundationalist Theories of Epistemic Justification. In The Stanford Encyclopedia of Philosophy. Edited by Edward Nouri Zalta. Stanford: Stanford University, Metaphysics Research Lab. Available online: https://plato.stanford.edu/entries/justep-foundational/ (accessed on 21 June 2021).
- Hashemieh, M., H. Timori Naghadeh, M. Tabrizi Namini, H. Neamatzadeh, and M. Hadipour Dehshal. 2015. The Iran Thalassemia Prevention Program: Success or Failure? Iranian Journal of Pediatric Hematology Oncology 5: 161–66. [Google Scholar] [PubMed]
- Hedayat, Kamyar M., Peiman Shooshtarizadeh, and Mohsin Raza. 2006. Therapeutic abortion in Islam: Contemporary views of Muslim Shiite scholars and effect of recent Iranian legislation. Journal of Medical Ethics 32: 652–57. [Google Scholar] [CrossRef] [PubMed]
- ICH (International Conference on Harmonisation of technical requirements for registration of pharmaceuticals for human use). 2021. ICH harmonised guideline integrated addendum to ICH E6(R1): Guideline for Good Clinical Practice ICH E6(R2) ICH Consensus Guideline. Available online: https://ichgcp.net/ (accessed on 19 April 2021).
- Isern-Mas, Carme, and Antoni Gomila. 2022. A second-personal approach to the Evolution of Morality. Biological Theory, 199–209. [Google Scholar] [CrossRef]
- Irrgang, Bernhard. 2015. Medizinethik für Mediziner. Stuttgart: Steiner Verlag. [Google Scholar]
- Jurek, Benjamin, and Inga D. Neumann. 2018. The Oxytocin Receptor: From Intracellular Signaling to Behavior. Physiological Reviews 98: 1805–908. [Google Scholar] [CrossRef]
- Larijani, Bagher, and Farzaneh Zahedi. 2008. Contemporary Medical Ethics: An Overview from Iran. Developing World Bioethics 8: 192–96. [Google Scholar] [CrossRef]
- Larijani, Bagher, Farzaneh Zahedi, and Hossein Malek Afzali. 2005. Medical ethics in the Islamic Republic of Iran. Eastern Mediterranean Health Journal 11: 1061–72. [Google Scholar]
- Love, Alan. 2022. Developmental Biology. In The Stanford Encyclopedia of Philosophy. Edited by Edward Nouri Zalta. Available online: https://plato.stanford.edu/archives/sum2022/entries/biology-developmental/ (accessed on 11 November 2022).
- Mavani, Hamid. 2014. Two shi’i jurisprudential methodologies to address medical and bioethical challenges: Traditional ijtihad and foundational ijtihad. Journal of Religious Ethics 42: 263–84. [Google Scholar] [CrossRef]
- Meissner, Marc. 2010. Was ist ein QUALY? Deutsches Ärzteblatt 107: A-546. Available online: https://www.aerzteblatt.de/archiv/70329/Was-ist-ein-Qaly (accessed on 17 August 2021).
- Miri, Maedehsadat, Mehdi Tabrizi Namini, Mahmoud Hadipour Dehshal, Forouzan Sadeghian Varnosfaderani, Alireza Ahmadvand, Sakineh Yousefi Darestani, and Mohsen Manshadi. 2013. Thalassemia in Iran in Last Twenty Years: The Carrier Rates and the Births Trend. Iranian Journal of Blood and Cancer 6: 11–18. [Google Scholar]
- Moliner, Antoni Montserrat, and Jaroslaw Waligora. 2017. The European Policy in the Field of Rare Disease. Advances in Experimental Medicine and Biology 1031: 561–87. [Google Scholar] [CrossRef]
- Moodi, Mitra, Mohammad-Reza Miri, and Gholam-Reza Sharifirad. 2013. The effect of instruction on knowledge and attitude of couples attending pre-marriage counseling classes. Journal of Education and Health Promotion 2: 1–5. [Google Scholar] [CrossRef] [PubMed]
- Moosapour, Hamideh, Jannat Mashayekhi, Farzaneh Zahedi, Akbar Soltani, and Bagher Larijani. 2018. General approaches to ethical reasoning in Islamic biomedical ethics discourse. Journal of Medical Ethics and History of Medicine 11: 11–21. [Google Scholar] [PubMed]
- Najmabadi, Hossein, Alireza Ghamari, Farhad Sahebjam, Roxana Kariminejad, Valeh Hadavi, Talayeh Khatibi, Ashraf Samavat, Elaheh Mehdipour, Bernadette Modell, and Mohammand Hassan Kariminejad. 2006. Fourteen-Year Experience of Prenatal Diagnosis of Thalassemia in Iran. Community Genet 9: 93–97. [Google Scholar] [CrossRef]
- National Institute of Health. 2021. The Nuremberg Code. Available online: https://history.nih.gov/display/history/Nuremberg+Code (accessed on 24 August 2021).
- Needs, T., L.-F. Gonzales-Mosquera, and D. T. Lynch. 2022. Beta Thalassemia; Treasure Island: StatPearls Publishing. Available online: https://www.ncbi.nlm.nih.gov/books/NBK531481/ (accessed on 16 May 2022).
- Neog, B. 2007. An Understanding of Common Morality. Utrecht: Utrecht University. [Google Scholar]
- Newman, Andrew J. 2019. Twelver Shi’ah. Available online: https://www.britannica.com/topic/Twelver-Shia (accessed on 9 April 2021).
- Nouri, Narges, Nayereh Nouri, Samane Tirgar, Elham Soleimani, Vida Yazdani, Farzaneh Zahedi, and Bagher Larijani. 2017. Consanguineous marriages in the genetic counseling centers of Isfahan and the ethical issues of clinical consultations. Journal of Medical Ethics and History of Medicine 10: 10. [Google Scholar]
- Palmer, Bernard. 2005. Common Morality: Deciding What to Do. The Review of Metaphysics 59: 178–80. [Google Scholar]
- Rahimi, Zohreh. 2013. Genetic Epidemiology, Hematological and Clinical Features of Hemoglobinopathies in Iran. BioMed Research International 2013: 803487. [Google Scholar] [CrossRef] [PubMed]
- Renn, Jürgen. 2020. The Evolution of Knowledge Rethinking Science for the Anthropocene. Princeton and Oxford: Princeton University Press. [Google Scholar]
- Sachedina, Abdulaziz. 2009. Islamic Biomedical Ethics Principles and Application. Available online: https://doi.org/10.1093/acprof:oso/9780195378504.001.0001 (accessed on 6 May 2021).
- Sachedina, Abdulaziz. 2015. Continuing the conversation about comparative ethics. Journal of Religious Ethics 43: 543–56. [Google Scholar] [CrossRef]
- Said, Edward W. 2003. Orientalism. Modern Classics London: Penguin Books. [Google Scholar]
- Samavat, Ashraf, and Bernadette Modell. 2004. Iranian national thalassaemia screening programme. BMJ 329: 1134–37. [Google Scholar] [CrossRef]
- Schwartz. 1929. Wilson&Reeder’s Mammals Species of the World (Online). Available online: http://www.departments.bucknell.edu/biology/resources/msw3/browse.asp?id=12100797 (accessed on 28 June 2021).
- Stratton-Lake, Peter. 2020. Intuitionism in Ethics. Available online: https://plato.stanford.edu/archives/sum2020/entries/intuitionism-ethics/ (accessed on 19 July 2021).
- Strauss, Bernard S. 2009. Genetic Counseling for Thalassemia in the Islamic Republic of Iran. Perspectives in Biology and Medicine 52: 364–76. [Google Scholar] [CrossRef]
- The United States Public Health Service. 2021. The U.S. Public Health Service Syphilis Study at Tuskegee. Available online: https://www.cdc.gov/tuskegee/timeline.htm (accessed on 11 July 2021).
- Tomasello, Michael. 2016. A Natural History of Human Morality. Cambridge: Harvard University Press. [Google Scholar]
- Tomasello, Michael. 2019. Becoming Human a Theory of Ontogeny. Cambridge: Harvard University Press. [Google Scholar]
- Tooby, John, and Leda Cosmides. 1990. On the Universality of Human Nature and the Uniqueness of the Individual: The Role of Genetics and Adaptation. Journal of Personality 58: 17–67. [Google Scholar] [CrossRef]
- Tooby, John, and Leda Cosmides. 2005. Conceptual Foundations of Evolutionary Psychology. In The Handbook of Evolutionary Psychology. Edited by D. Buss. Hoboken: John Wiley and Sons. [Google Scholar]
- UNESCO. 2005. Universal Declaration of Bioethics and Human Rights. Available online: https://www.unesco.org/en/legal-affairs/universal-declaration-bioethics-and-human-rights (accessed on 3 May 2021).
- WHO. 1948. Constitution of the World Health Organisation. Available online: https://www.who.int/about/governance/constitution (accessed on 3 May 2021).
- WHO. 1993. Control of Hereditary Diseases: Report of a WHO Scientific Group. WHO Technical Report Series 865. Geneva: World Health Organization. Available online: https://apps.who.int/iris/handle/10665/41846 (accessed on 24 August 2021).
- WHO. 1998. Proposed International Guidelines on Ethical Issues in Medical Genetics and Genetic Services. Report of a WHO Meeting on Ethical Issues in Medical Genetics 1997. Geneva: World Health Organization. Available online: https://apps.who.int/iris/handle/10665/63910 (accessed on 3 May 2021).
- WHO. 2006. Medical genetic services in developing countries: The ethical, legal and social implications of genetic testing and screening. In Human Genetics, Chronic Diseases and Health Promotion. Geneva: World Health Organization. Available online: https://apps.who.int/iris/handle/10665/43288 (accessed on 3 May 2021).
- World Medical Association. 1948. Declaration of Geneva. Available online: https://www.wma.net/what-we-do/medical-ethics/declaration-of-geneva/ (accessed on 24 August 2021).
- World Medical Association. 2013. World Medical Association Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 8 August 2021).
- Zimmermann, Bettina M., Insa Koné, David Shaw, and Bernice Elger. 2021. Autonomy and social influence in predictive genetic testing decision-making: A qualitative interview study. Bioethics 35: 199–206. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).