Abstract
Background/Objectives: The goal of reconstructive hand surgery is to achieve both functional and aesthetic restoration. The primary aim of this study is to perform a detailed, practice-oriented evaluation of perforator-based and local flaps for soft-tissue reconstruction of the hand and digits, focusing specifically on their functional reliability, anatomical consistency, complication profile, and aesthetic integration in a real-world, high-complexity referral population. Methods: This retrospective single-center study included 37 patients with soft tissue defects of the hand that required flap coverage between September 2021 and September 2024. The study assessed patient demographics, defect characteristics, flap selection, surgical techniques, and outcomes including satisfactory soft tissue coverage, functional results and occurrence of complications. Various perforator flaps were analyzed, including the dorsal metacarpal artery flap, reverse radial forearm flap, reverse posterior interosseous artery flap, reverse homodigital and heterodigital island flaps, and the thenar flap. Results: Satisfactory soft tissue coverage was achieved in 35 out of 37 patients. One case involved partial distal flap necrosis, and another presented with Foucher flap failure. The remaining flaps demonstrated stable integration, preserved perfusion, and durable soft-tissue coverage with satisfactory contour and pliability. Functional outcomes were favorable, with restoration of joint mobility and absence of secondary deformities. Conclusions: This study supports the continued use of perforator and local flaps in upper extremity reconstruction, emphasizing the need for individualized planning to optimize the outcomes.
1. Introduction
The primary objective of reconstructive hand surgery is the restoration of function while maintaining an aesthetically acceptable appearance. The hand is a highly visible and functionally complex organ, making both aspects equally important [1]. Despite significant advancements in microsurgical techniques, an optimal strategy for soft tissue coverage remains a subject of discussion. The literature has extensively documented various flap techniques; however, there is still an ongoing debate regarding the ideal balance between function, aesthetic outcomes, and donor-site morbidity [2,3,4].
A systematic approach to hand defect coverage begins with thorough wound debridement, performed under tourniquet control to ensure the removal of all nonviable tissues while preserving vital structures. Once debridement is complete, the reconstructive ladder concept helps guide the decision-making process, categorizing defects into those that are simple, suitable for direct closure, skin grafting, the use of a dermal substitute, or secondary wound healing; and complex, requiring flap-based reconstruction [5]. For cases necessitating soft tissue coverage beyond a skin graft, perforator-based flaps and local pedicled flaps have gained prominence as a reliable solution due to their ability to provide pliable, well-vascularized coverage with minimal donor-site morbidity [6]. Alternatives to these options include free flaps and distant pedicled flaps.
In this study, we present our experience using perforator flaps for reconstruction of palm and dorsum of the hand, as well as thumb and digit defects, emphasizing their efficacy in achieving functional recovery and aesthetic integration. We analyze the indications, technical aspects, complications, and outcomes associated with the following flaps:
- Dorsal Metacarpal Artery Flaps;
- Reverse Radial Forearm Flap;
- Reverse Posterior Interosseous Artery (PIA) Flap;
- Reverse Homodigital and Heterodigital Island Flaps;
- Thenar Flap.
2. Materials and Methods
2.1. The Patient Selection and Study Design
This retrospective study included 37 patients who underwent soft tissue reconstruction for hand defects at Department of Plastic and Hand Surgery, St. Hedwig of Silesia Hospital, Trzebnica, Poland, between September 2021 and September 2024. All patients required soft tissue coverage beyond direct closure or skin grafting. Inclusion criteria consisted of:
- Patients with soft tissue defects of the hand requiring flap coverage;
- Availability of adequate recipient area and donor site possibility;
- No contraindications to regional flap surgery;
- At least 6-month follow-up.
A total of 37 patients (32 males, 5 females) with a mean age of 47 years (range: 26–76 years) were included. The majority (94.6%) of defects resulted from traumatic injuries (31 sharp/crush injuries, 3 burns, 1 dog bite), while 2 cases were non-traumatic (Dupuytren’s contracture and diabetic thumb infection).
The majority of our patients were referred from external centers after unsuccessful primary management (n = 25; 67.6%), often presenting with infected or devitalized wounds, necrosis following replantation, chronic scarring or contractures, and traumatic wound beds resulting from previous interventions, as well as burns (thermal, electrical, or chemical).
2.2. Wound Debridement
Surgical debridement of the defect site was performed as soon as possible—ideally within 24 h since the emergence of a defect—necrotic tissues, contaminated substances adhering to the wound site, and foreign bodies were removed from the surgical wound. If there were concerns about spread of infection or the appearance of additional areas of tissue necrosis, coverage of the defect was postponed for 1–2 days to ensure the good condition of the local tissues, while the defect was left open and covered with an occlusive dressing In cases of chronic defects, our goal has been to achieve one-stage surgery defect management that included both debridement of the defect and definitive closure using a flap procedure. If there were any concerns regarding the feasibility of definitive management of the defect, the coverage is postponed for 1–2 days, similar to the approach used for acute post-traumatic defects. In cases where clinical indications suggested infection, microbiological and laboratory examinations were conducted to identify the pathogen and guide targeted antibiotic therapy in addition to surgical treatment [7,8].
2.3. Preoperative Planning and Flap Selection
Preoperative assessment included hand vascular mapping with Doppler ultrasonography to evaluate the presence and course of critical perforators. Flap selection was based on defect size, location, and tissue requirements. Flaps were harvested according to standard anatomical landmarks and microvascular techniques. The reconstructive approach followed the reconstructive elevator principle, prioritizing local flaps before considering regional or distant options [9]. Our target was to perform definite flap coverage within 72 h from debridement [10,11].
2.4. Surgical Techniques
Each flap type was performed according to well-established techniques:
2.4.1. Reverse Posterior Interosseous Artery (PIA) Flap
The reverse posterior interosseous artery (PIA) flap is supplied by perforators arising from the PIA, which are situated in the intermuscular septum between the fifth and sixth extensor tendon compartments—specifically between the extensor carpi ulnaris and extensor digiti minimi—in the middle third of the forearm. The pivot point is situated roughly 3 cm proximal to the distal radioulnar joint, at the site where the PIA forms an anastomosis with the anterior interosseous artery. This flap can cover defects on the dorsum of the hand such as the MCP joints defects or the first webspace [12,13,14]. In our study this flap was used to cover 2 medium-size dorsal hand defects and in one case of contracting scar tissue of first webspace (Figure 1).


Figure 1.
(a) A 26-year-old male with contracting scarring of the first webspace due to thermal burn. (b) PIA flap design; (c) Early post-operative effect; (d) Result 3 months after surgery.
2.4.2. Dorsal Metacarpal Artery (DMA) Flap
The Kite, or Foucher, flap is a commonly employed technique for reconstructing and preserving thumb integrity after injury. It is derived from the first dorsal metacarpal artery flap. The name “Foucher flap” honors the French surgeon Guy Foucher, who first performed and reported this method in 1979 [15]. The first dorsal metacarpal artery flap arises from the radial artery and courses alongside the second metacarpal of the index finger, lying superficial to the fascia of the first dorsal interosseous muscle.
Modifications of this flap may include the dorsal sensory branch of the radial nerve, the second metacarpal, the extensor indicis proprius muscle, and the first dorsal interosseous muscle for management of more complex defects. Most frequently this technique is used for management of both dorsal and palmar thumb defects as well as defects of the first webspace [16].
Variations in this flap, including the reverse or extended metacarpal artery flaps, permit successful coverage distal to the interphalangeal joint via the palmar-dorsal anastomosis located at the level of the proximal phalanx rather than the metacarpal neck [17,18].
This flap was used in 9 patients with thumb soft tissue defects (Figure 2).


Figure 2.
(a) A 56-year-old man presented with thumb infection with soft tissue necrosis in course of untreated diabetes; (b) Foucher flap design; (c) Flap raising; (d) Insetting of the flap (e,f) Results 6 weeks post-surgery.
Use of the second dorsal metacarpal artery, a branch of the dorsal carpal arch, enables coverage of ulnar defects on the dorsal aspect of the hand and fingers. Those flaps can be found in the literature under the name Maruyama or Quaba flap. Microsurgical expertise is necessary to raise these flaps, and from a technical standpoint the operation is of moderate difficulty [16,19,20,21]. This flap was used in 4 patients with PIP region soft tissue defects of the digits (Figure 3).


Figure 3.
(a) A 44-year-old male presented with PIP 2 and PIP 4 defects due to industrial injury resulting in third digit amputation; (b) DMCA flap design; (c) Flap raising; (d) Early post-operative outcome (e) Post-operative outcome 12 weeks after surgery.
2.4.3. Reverse Radial Forearm (RRF) Flap
Flaps based on the radial artery are highly versatile and can be used to reconstruct a wide variety of hand defects. The reversed radial fasciocutaneous or adipofascial flap is most commonly employed for coverage of defects on the dorsal or palmar aspects of the hand. In addition, several modifications have been reported in the literature, including its use as an osteofasciocutaneous flap, a cutaneous perforator-based flap, and as a free flap [18,22]. The palmaris longus tendon can be included in the flap design along with the lateral antebrachial cutaneous nerve to provide both motor function and sensory innervation. The traditional RRF flap is dependent on reverse flow from the ulnar artery traveling through the deep palmar arch and ultimately supplying the radial artery. Consequently, an abnormal Allen test prior to surgery serves as an absolute contraindication to utilizing this technique. For post-traumatic reconstruction of composite thumb defects, it may be used as radial forearm flap covering the skeletonized thumb fragment or other osseous transplant in the place of a thumb [23].
The flap is oriented along the course of the radial artery, with the skin paddle preferably positioned over the middle third of the forearm. A common pitfall is positioning the skin paddle too proximally, as most perforators are located in the distal third of the forearm. The flap can effectively cover defects measuring up to 10–20 cm, extending to the proximal interphalangeal joint. Although the dissection of the RRF flap is relatively straightforward and anatomical variation is minimal, some surgeons express reluctance to use this flap due to the requirement for sacrificing the radial artery. If used as a proximally based free flap, careful closure and imbrication of muscle over the distal flexor carpi radialis tendon is imperative to reduce donor morbidity and improve skin graft take to the donor site [24,25]. In the material, this flap was used to cover 5 medium-to large dorsal hand defects as well as 2 palmar hand defects and 2 thumb defects (Figure 4).
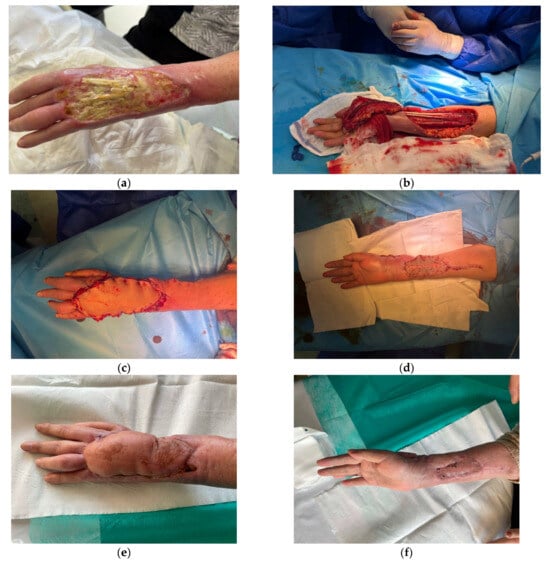
Figure 4.
(a) A 76-year-old female suffered chemical burn which resulted in dorsal hand defect exposing extension tendons; (b) Reverse radial artery flap raising; (c) Immediate post-operative result; (d) Donor site covered with split-thickness skin graft; (e) Post-operative outcome 8 weeks after surgery; (f) Donor site 8 weeks after surgery.
2.4.4. Reverse Homodigital and Heterodigital Island Flap
This is a versatile option for coverage of both dorsal and palmar defects of the fingers, with the maximum size of 2.5 cm to 3 cm. The main advantage of homodigital island flap technique is that all defects are confined to one finger, preserving other fingers uninjured. An axial pattern flap derives its blood supply from reverse flow of the radial or ulnar digital artery. Three anastomotic sites link the radial and ulnar digital arteries: at the proximal cruciate ligament, at the distal cruciate ligament, and at the fingertip just distal to the profundus tendon insertion. Any one of these connections can provide sufficient perfusion for the flap. This flap is technically demanding, requiring meticulous dissection of the nerve from the artery. Due to the necessity of retracting the nerve, most patients may experience a transient neurapraxia postoperatively [26]. The flap can also be planned as a heterodigital flap to reconstruct defects of adjacent fingers. Similarly to the reverse-flow homodigital flap, the heterodigital flap offers considerable freedom in its arc of rotation, making it suitable for coverage of both volar and dorsal finger defects [27] (Figure 5).
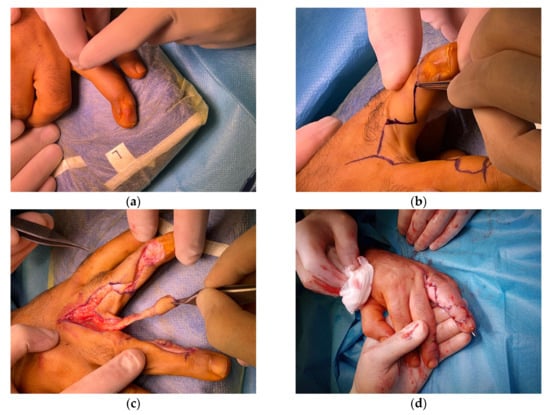
Figure 5.
(a) A 37-year-old male with dorsal IV finger DIP joint defect with a fistula due to open fracture; (b) Flap design; (c) Island finger reverse artery flap raising; (d) Early post-operative outcome.
2.4.5. Thenar Flap
Gatewood originally introduced the thenar flap technique in 1926, and since that time it has appeared in the literature with various modifications for the reconstruction of fingertip injuries and amputations [28] (Figure 6).


Figure 6.
(a) A 53-year-old male sustained fingertip amputation of the fourth digit due to mechanical injury; (b) Early post-operative outcome of covering the defect with thenar flap; (c) Outcome 6 weeks after surgery; (d) Outcome 3 months after surgery.
Table 1 shows the individual flaps that were used in our department to cover soft tissue defects of the hand region between September 2021 and September 2024.

Table 1.
Type of flaps used to cover soft tissue defects in the hand area at the Department of Plastic and Hand Surgery, St. Hedwig of Silesia Hospital, Trzebnica, Poland, (2021–2024).
2.5. Postoperative Management
Post-operative treatment consisted of regular flap monitoring (at least once every 6 h) for 5 days, subcutaneous enoxaparin administration twice daily in therapeutic dosage and non-adhesive dressing changes. In cases of simpler reconstruction techniques, e.g., thenar flap, patients were discharged from the hospital on the first day after surgery, and follow-up appointments were conducted on the third and seventh days post-surgery. Flap division was performed on 14th day POD Sutures were removed on the 14th post-operative day and early physical therapy was started as soon as viability of the flap was secured [29,30]. Table 2 summarizes the postoperative management of the operated patients.

Table 2.
Postoperative Management of the operated patients.
3. Results
A total of 37 patients underwent soft-tissue reconstruction of the hand and digits using a variety of regional and local flaps. The cohort represented a spectrum of post-traumatic and post-necrotic tissue losses involving both the dorsal and volar aspects of the hand, thumb, and fingers.
The etiologies of the defects were predominantly mechanical trauma (n = 25; 67,5%), followed by secondary necrosis following crushing injury or failed replantation (n = 7; 18,9%), burns of thermal, electrical, or chemical origin (n = 3; 8,1%), infection associated with diabetes mellitus (n = 1; 2,7%), and recurrent Dupuytren’s contracture (n = 1; 2,7%).
The anatomic distribution of defects included dorsal and palmar defects of the hand (n = 9), thumb (n = 11), fingertips (n = 9), and phalangeal or web space defects (n = 8). Flap selection was individualized according to defect location, size, and depth, as well as donor-site characteristics and vascular anatomy.
The major complication rate (requiring secondary surgical procedure) was 5.4%. One patient developed partial distal flap necrosis following a dog bite, managed successfully with surgical debridement and split-thickness skin graft. Another case, a diabetic patient with an infected volar thumb defect reconstructed using a Foucher flap, experienced total flap failure necessitating secondary coverage. The minor complications consisted of transient neuropraxia in patients treated with island digital flaps that resolved within 3 months without any intervention. All of the complications mentioned were classified as early complications, occurring within four weeks following the procedure.
In all remaining patients, the flaps demonstrated stable integration, preserved perfusion, and durable soft-tissue coverage with satisfactory contour and pliability. Functional outcomes were favorable, with restoration of joint mobility and absence of secondary deformities. Functionally, most patients were able to resume hand mobility by postoperative day 14, following our standardized early-mobilization protocol. Aesthetic integration was satisfactory across flap types. These results suggest that perforator-based reconstruction remains robust even in suboptimal wound environments, supporting its use in tertiary referral settings where reconstructive demands exceed what is typically described in the literature.
3.1. Flap Selection and Outcomes
Flap selection and outcomes are presented in Table 3.

Table 3.
Flap selection and outcomes.
3.2. Complications
Postoperative complications are listed below:
- 1 case of partial flap necrosis (managed with debridement and split-thickness skin graft—STSG);
- 1 case of total flap failure (necessitating secondary reconstruction);
- Transient neuropraxia in reverse digital artery flaps (resolved within 3 months).
4. Discussion
The reconstructive elevator concept suggests that the simplest option for coverage might not always be the best in terms of form and function, emphasizing the need for individualized reconstructive planning [31].
The selection of appropriate flap techniques for soft tissue defects of the hand requires a nuanced understanding of various factors, including defect characteristics, patient condition, and specific functional and aesthetic requirements. Early reconstruction of soft tissue defects in the hand has been associated with favorable outcomes, facilitating the patient’s return to high functional levels. Our findings reinforce the effectiveness of perforator flaps in achieving stable soft tissue coverage while preserving hand function. Early reconstruction was associated with lower infection rates and improved functional recovery, aligning with literature emphasizing early intervention (within 72 h) for optimal outcomes [10,11]. It is crucial for the hand surgeon to recognize that multiple reconstructive options often exist for a given defect. A thorough assessment of tissue type, as well as functional and aesthetic goals, is essential to achieve optimal outcomes. The “like with like” principle, which advocates for replacing lost tissue with similar tissue in appearance and function, is fundamental in hand reconstruction [2,3,4,5]. Additionally, flap thinning is often necessary to ensure that the reconstructed tissue closely matches the native hand tissue in thickness and pliability, thereby enhancing both functional and cosmetic results [3,5,13]. The best functional and aesthetic results in these patients are achieved with free flaps coverage; however, when early free flap transfer is not feasible due to patient instability or other contraindications, alternative options such as local and regional flaps should be considered. Local flaps, which consist of skin and subcutaneous tissue harvested from a site adjacent to the defect while maintaining their intrinsic blood supply, can be reliable sources for soft tissue replacement in the hand [4,6]. We emphasize achieving favorable reconstructive outcomes in compromised tissue beds, scenarios where perforator-based reconstructions are frequently avoided in the literature. Highlighting the reliability of these flaps in such adverse conditions provides clinically significant, practice-modifying information. A critical comparison of our results with existing literature provides insights into the relative advantages and limitations of each technique.
4.1. Reverse Posterior Interosseous Artery (PIA) Flap
The reverse PIA flap is particularly advantageous for dorsal hand defects due to its anatomical proximity and reliable blood supply. Our positive outcomes with this flap are consistent with those reported in the literature. Nonetheless, the PIA flap’s utility may be limited by anatomical variations and a steep learning curve, necessitating meticulous preoperative planning and surgical expertise [12,13,14].
4.2. Dorsal Metacarpal Artery Flaps
The dorsal metacarpal artery (DMA) flap is a versatile option for resurfacing soft-tissue defects of the fingers. Our findings align with those of Sebastin et al., who demonstrated that the DMA perforator flap is effective for defects proximal to the fingertip, offering reliable coverage with satisfactory aesthetic and functional outcomes. However, donor site morbidity, such as the need for skin grafting (if harvested flap is more than 3.5 cm in width), has been reported. Innovative techniques, like the use of digital dorsal advancement flaps to repair donor sites, have been proposed to address these challenges [16,17,19,20,21].
4.3. Reverse Radial Forearm Flap
The reverse radial forearm flap has been a cornerstone in reconstructive surgery due to its robust vascularity and pliability. Our results corroborate existing literature, indicating that this flap provides durable coverage for extensive soft tissue defects. However, donor site morbidity remains a concern. Alternative approaches, such as the radial artery perforator flap, have been explored to mitigate these issues by preserving the radial artery, thereby reducing complications; however, it has greater limitations resulting from the length of the pedicle [24,25].
4.4. Reverse Homodigital and Heterodigital Island Flaps
Reverse digital artery island flaps are widely employed for fingertip reconstructions, offering good aesthetic and functional results. Our experience aligns with studies demonstrating that these flaps provide reliable coverage with satisfactory sensory recovery [26]. However, donor site morbidity, such as the need for skin grafting if donor side defect is too big to be covered primarily, has been reported. Innovative techniques, like the use of digital dorsal advancement flaps to repair donor sites, have been proposed to address these challenges [27].
4.5. Thenar Flap
The thenar flap is a traditional method for reconstructing fingertip and pulp defects, particularly in young patients. Our results with the thenar flap are comparable to those in existing literature, showing favorable outcomes in terms of flap survival and functional recovery. However, limitations such as joint stiffness and the need for a two-stage procedure should be considered when selecting this technique [28].
5. Limitations
This study has several limitations. Its retrospective design may constrain the ability to draw definitive conclusions regarding causality and treatment efficacy. With only 37 patients included, the sample size may be insufficient for generalizing findings to broader populations. Additionally, as a single-center study, the applicability of the results may be limited to specific settings. Variability in patient demographics, defect types, and surgical techniques complicates objective comparisons between functional and aesthetic outcomes. Future studies would benefit from the use of objective measures or standardized scoring systems to enhance evaluation.
6. Conclusions
Perforator flaps remain a cornerstone in reconstructive hand surgery, offering functional and aesthetic advantages. While no single flap is universally superior, an individualized approach based on defect characteristics, patient factors, and surgeon expertise optimizes outcomes. Future research should focus on long-term functional recovery and comparative studies between perforator flaps and alternative reconstructive options.
Author Contributions
Conceptualization, P.W. and A.E.; methodology, A.E. and S.M.; resources, J.K., P.O. and P.S.; data curation, M.C., M.S. and S.M.; writing—original draft preparation, P.W.; writing—review and editing, M.J., P.O., M.C., P.S., J.K., P.W., P.P. and D.K.; supervision, A.E. and D.K.; project administration, M.S., M.J. and P.P.; funding acquisition, P.P. and D.K. All authors have read and agreed to the published version of the manuscript.
Funding
The APC was funded by Wroclaw University of Science and Technology; the research received no further external funding.
Institutional Review Board Statement
This retrospective study was conducted using standard and previously published surgical methods. No new experimental procedures were performed. The study was conducted in accordance with institutional requirements, and they were performed in accordance with the World Medical Association Declaration of Helsinki.
Informed Consent Statement
Informed consent was waived because the study was retrospective.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| PIA | posterior interosseous artery |
| PIAF | posterior interosseous artery flap |
| DMA | dorsal metacarpal artery |
| DMCAF | dorsal metacarpal artery flap |
| RRF | reverse radial flap |
| POD | post-operative day |
| RAF | radial artery flap |
| MCP | metacarpophalangeal (joint) |
| PIP | proximal interphalangeal (joint) |
| DIP | distal interphalangeal (joint) |
| STSG | split-thickness skin graft |
References
- McCash, C.R. Cosmetic Aspects of Hand Surgery. Hand 1969, 1, 67–71. [Google Scholar] [CrossRef]
- Jakubietz, R.G.; Jakubietz, M.G.; Kloss, D.; Gruenert, J.G. Defining the Basic Aesthetics of the Hand. Aesthetic Plast. Surg. 2005, 29, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Manske, P.R. Aesthetic Hand Surgery. J. Hand Surg. 2002, 27, 383–384. [Google Scholar] [CrossRef] [PubMed]
- Rehim, S.A.; Kowalski, E.; Chung, K.C. Enhancing Aesthetic Outcomes of Soft-Tissue Coverage of the Hand. Plast. Reconstr. Surg. 2015, 135, 413e–428e. [Google Scholar] [CrossRef] [PubMed]
- Miller, E.A.; Friedrich, J. Soft Tissue Coverage of the Hand and Upper Extremity: The Reconstructive Elevator. J. Hand Surg. 2016, 41, 782–792. [Google Scholar] [CrossRef]
- Saint-Cyr, M.; Gupta, A. Indications and Selection of Free Flaps for Soft Tissue Coverage of the Upper Extremity. Hand Clin. 2007, 23, 37–48. [Google Scholar] [CrossRef]
- Jagosz, M.; Węgrzyn, P.; Chęciński, M.; Smorąg, M.; Króliński, J.; Manasterski, S.; Ostrowski, P.; Elsaftawy, A. Reconstructive Strategies in Post-Traumatic Osteomyelitis of the Lower Limb: A Case Series and Surgical Algorithm Analysis. J. Clin. Med. 2025, 14, 6746. [Google Scholar] [CrossRef]
- Elsaftawy, A.; Jabłecki, J. Acute Compartment Syndrome after Open Forearm Fracture-Scale of the Problem and Case Report. Pol. Prz. Chir. Pol. J. Surg. 2014, 86, 44–47. [Google Scholar] [CrossRef]
- Jagosz, M.; Węgrzyn, P.; Smorąg, M.; Ostrowski, P.; Bonczar, M.; Chęciński, M.; Manasterski, S.; Elsaftawy, A. In the Era of Advanced Microsurgery, Is There Still a Place for Pedicled Abdominal Flaps? A Retrospective Analysis. J. Clin. Med. 2025, 14, 1696. [Google Scholar] [CrossRef]
- Colen, D.L.; Colen, L.B.; Levin, L.S.; Kovach, S.J. Godina’s Principles in the Twenty-First Century and the Evolution of Lower Extremity Trauma Reconstruction. J. Reconstr. Microsurg. 2018, 34, 563–571. [Google Scholar] [CrossRef]
- Park, K.H.; Woo, S.J.; Kang, D.-H. The Role of Surgical Timing in Upper Extremity Free Flap Reconstruction Following Trauma: A 10-Year Single-Center, Single-Surgeon Experience. Arch. Hand Microsurg. 2024, 29, 53–59. [Google Scholar] [CrossRef]
- Biswas, D.; Wysocki, R.W.; Fernandez, J.J.; Cohen, M.S. Local and Regional Flaps for Hand Coverage. J. Hand Surg. 2014, 39, 992–1004. [Google Scholar] [CrossRef] [PubMed]
- Cavadas, P.C.; Thione, A.; Rubí, C. The Simplified Posterior Interosseous Flap. J. Hand Surg. 2016, 41, e303–e307. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.L.; Colonna, M.R.; Vindigni, V.; Bassetto, F.; Tiengo, C. Reverse Posterior Interosseous Flap: Different Approaches over the Years—A Systematic Review. J. Plast. Reconstr. Aesthet. Surg. 2022, 75, 4023–4041. [Google Scholar] [CrossRef]
- Foucher, G.; Braun, J.B. A New Island Flap Transfer from the Dorsum of the Index to the Thumb. Plast. Reconstr. Surg. 1979, 63, 344–349. [Google Scholar] [CrossRef]
- Muyldermans, T.; Hierner, R. First Dorsal Metacarpal Artery Flap for Thumb Reconstruction: A Retrospective Clinical Study. Strateg. Trauma Limb Reconstr. 2009, 4, 27–33. [Google Scholar] [CrossRef]
- Sebastin, S.J.; Mendoza, R.T.; Chong, A.K.S.; Peng, Y.P.; Ono, S.; Chung, K.C.; Lim, A.Y.T. Application of the Dorsal Metacarpal Artery Perforator Flap for Resurfacing Soft-Tissue Defects Proximal to the Fingertip. Plast. Reconstr. Surg. 2011, 128, 166e–178e. [Google Scholar] [CrossRef]
- Yannascoli, S.M.; Thibaudeau, S.; Levin, L.S. Management of Soft Tissue Defects of the Hand. J. Hand Surg. Am. 2015, 40, 1237–1244. [Google Scholar] [CrossRef]
- Makkar, R.M. The Innervated First Dorsal Metacarpal Artery Island Flap for Reconstruction of Post-Traumatic Thumb Defect. Eur. J. Plast. Surg. 2012, 35, 881–886. [Google Scholar] [CrossRef]
- Ravada, S.; Mahipathy, S.R.V.; Durairaj, A.R.; Sundaramurthy, N.; Jayachandiran, A.P. Functional and Aesthetic Outcomes of First Dorsal Metacarpal Artery Flap for Thumb Reconstruction: A Prospective Study. Int. Surg. J. 2020, 7, 2268–2274. [Google Scholar] [CrossRef]
- Rehim, S.A.; Chung, K.C. Local Flaps of the Hand. Hand Clin. 2014, 30, 137–151. [Google Scholar] [CrossRef] [PubMed]
- Kammien, A.J.; Colen, D.L. Composite Osteo-Tendino-Cutaneous Reverse Radial Forearm Flap for Complex Thumb Reconstruction: A Case Report. Orthoplastic Surg. 2024, 17, 15–22. [Google Scholar] [CrossRef]
- Elsaftawy, A.; Jablecki, J. Post-Traumatic Thumb Reconstruction with Radial Forearm Flap. Pol. Prz. Chir. Pol. J. Surg. 2013, 85, 351–353. [Google Scholar] [CrossRef]
- Akdag, O.; Karamese, M.; NebilSelimoglu, M.; Akatekin, A.; Abacı, M.; Sutcu, M.; Tosun, Z. Reverse Adipofascial Radial Forearm Flap Surgery for Soft-Tissue Reconstruction of Hand Defects. Eplasty 2016, 16, e35. [Google Scholar] [PubMed]
- Maan, Z.N.; Legrand, A.; Long, C.; Chang, J.C. Reverse Radial Forearm Flap. Plast. Reconstr. Surg. Glob. Open 2017, 5, e1287. [Google Scholar] [CrossRef] [PubMed]
- Khan, W.U.; Appukuttan, A.; Loh, C.Y.Y. Homodigital Pedicled Digital Artery Perforator Flaps for Fingertip Reconstruction—A Review of Flap Options. JPRAS Open 2022, 34, 199. [Google Scholar] [CrossRef]
- Gurbuz, K.; Dogar, F.; Yontar, Y. Comparison of Clinical Outcomes of Heterodigital Neurovascular Island Flap, Reverse Homodigital Neurovascular Island Flap, and Cross-Finger Flap Used for Fingertip Reconstruction. Indian J. Orthop. 2022, 56, 847–855. [Google Scholar] [CrossRef]
- Kang, H.J.; Sung, S.Y.; Whang, J.; Hong, J.J.; Park, H.S.; Kim, J.S. Extended Thenar Flap for Two Adjacent Fingertip Amputations. J. Plast. Reconstr. Aesthet. Surg. 2020, 73, 65–71. [Google Scholar] [CrossRef]
- Kallenberger, A.K.; Xiong, L.; Gazyakan, E.; Ziegler, B.; Will, P.; Kneser, U.; Hirche, C. Intraoperative Heparin Bolus and Postoperative Anticoagulation with Low Molecular Weight Heparin Increase Reliability of Microsurgical Free Flaps for Upper Extremity Reconstruction. J. Reconstr. Microsurg. 2023, 39, 334–342. [Google Scholar] [CrossRef]
- Elsaftawy, A.; Jabłecki, J. Unsuccesful Replantation of Metacarpal Hand after Venous Thrombosis—Case Report. Pol. Prz. Chir. Pol. J. Surg. 2013, 85, 721–726. [Google Scholar] [CrossRef]
- Bennett, N.; Choudhary, S. Why Climb a Ladder When You Can Take the Elevator? Plast. Reconstr. Surg. 2000, 105, 2266–2267. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.