Abstract
Background: Cytomegalovirus (CMV) infection represents a major issue worldwide, since it constitutes the most common viral congenital infection, with a prevalence of 0.58% and 1–5% in developed and developing countries, respectively. According to recent studies, prenatal treatment significantly decreases the risk of vertical CMV transmission, and early intervention may even prevent the termination of pregnancy. This study aimed to investigate the level of awareness of CMV among pregnant patients through a semi-systematic review. Methods: We included all of the original articles investigating knowledge and awareness about CMV infection among pregnant women. Our research included the PubMed database. Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement, the Covidence system automatically guided us to screen the titles and/or abstracts, and then full-texts, followed by data extraction from the eligible studies. Results: We screened 764 studies altogether, with 13 studies included in this analysis. Knowledge about the existence of CMV infection risk varied between the articles, ranging from 11.4% in a study performed in Ireland to 60% reported in a study on the French population. Studies analyzing the impact of educational interventions on patients’ knowledge about preventive measures reported significant improvement compared to their level of awareness before the intervention. Conclusions: Patients’ awareness and knowledge about CMV seemed to be generally low or very low during the last decade before the development of effective secondary prevention methods. Educational interventions seem to be effective, and therefore their wide use could be of potential benefit. In the era of available secondary prevention of vertical transmission, it is crucial to concentrate the efforts of different stakeholders to increase the awareness of cCMV among pregnant women.
1. Introduction
Cytomegalovirus (CMV) is a DNA virus belonging to the Herpesviridae family [1]. Prenatal CMV infection represents a major issue worldwide since it constitutes the most common viral congenital infection, with a prevalence of 0.58% and 1–5% in developed and developing countries, respectively [2,3,4,5]. The concern is primarily associated with the risk of long-term complications for the affected individuals. Notably, congenital neurological defects, particularly non-genetic sensorineural hearing loss (SNHL), are predominantly caused by CMV, both in cases of primary and non-primary maternal infection [6]. SNHL is observed in approximately 10.7–32.4% of all children diagnosed with congenital CMV (cCMV) [7]. Other complications include several ophthalmologic manifestations, developmental delays, and neuroimaging abnormalities [8,9,10]. Furthermore, these possible sequelae necessitate prolonged medical observation and various therapeutic interventions. This has prompted further research and the revision of screening and treatment protocols.
Regarding the possibilities of secondary prevention and prenatal treatment, many limitations were concerned with the potential teratogenic and mutagenic effects of valganciclovir [11]. According to recent studies, valacyclovir treatment significantly decreases the risk of vertical CMV transmission, and early intervention may even prevent the termination of pregnancy [12,13,14]. Valacyclovir is characterized by pregnancy category B, according to the Food and Drug Administration (FDA) [15]. With concentrations ten and seven times higher than in human plasma levels, no teratogenic effect in rodents was observed [15]. Therefore, valacyclovir treatment is recognized for the secondary prevention of cCMV. However, it is important to emphasize that the basis for preventing cCMV infection remains primary prevention among pregnant women. This includes compliance with principles of hygiene such as washing hands after changing diapers or touching toys, avoiding contact with contaminated bodily fluids, including saliva, urine, breast milk, genital secretions, and plasma, and refraining from sharing food or drinks with young children or kissing them. Consequently, raising awareness about the risk of cCMV infection among patients might mitigate the issue by preventing primary infection and, if needed, initiating antiviral therapy during gestation. Nonetheless, this would only be possible with proper patient awareness.
This study aimed to investigate the level of the awareness of cCMV among the population of pregnant patients through a semi-systematic review. We investigated three different areas of knowledge about cCMV: the infection itself, preventive measures, and complications following infection.
2. Materials and Methods
2.1. Selection of Studies
We included all of the original articles investigating knowledge and awareness about cCMV infection among pregnant women. Additionally, our inclusion criteria comprised a requirement for the availability of the full text in the English language. We excluded studies enrolling non-pregnant individuals or postpartum women. We used Covidence software (Veritas Health Innovation Ltd., Melbourne, Australia) for study selection and data extraction [16]. Two co-authors (J.K.B. and A.U.) screened the studies for their eligibility. In cases of discrepancy, a third co-author (E.B. or P.B.) was consulted. Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement, the Covidence system automatically guided us to screen first the titles and/or abstracts, and then perform full-text reviews, followed by data extraction from the eligible studies [16,17].
2.2. Search Strategy
Our research included the PubMed database. We defined the population as pregnant women, both primiparous and multiparous, as awareness during pregnancy is crucial for the primary and secondary prevention of cCMV. To address our research question, we used Medical Subject Headings (MeSH) of the relevant terms for cCMV and neonate, as well as various synonyms of ‘awareness’. Our PubMed advanced search query was the following: ((((((CMV) OR (Human cytomegalovirus)) OR (Cytomegalovirus)) OR (cytomegalovirus infection)) OR (HCMV)) AND ((((((awareness) OR (knowledge)) OR (attitude)) OR (Perception)) OR (Familiarity)) OR (Education))) AND ((((((congenital) OR (Inborn)) OR (neonatal)) OR (perinatal)) OR (neonate)) OR (fetal)). The search was performed on 30 January 2024. Our study did not employ any additional search strategies beyond the initial approach.
2.3. Data Extraction
Following the completion of the study selection process, we compiled the following information from the full text: authors’ names, publication year, country, sample size, data collection method, and the results of questions inquiring about general information about cCMV infection, primary preventive measures (PPM), and possible complications.
3. Results
We screened 764 studies altogether, including 13 studies in the final analysis (Figure 1). The detailed results of a review of the selected studies are presented in Summary Table 1. Knowledge about the existence of cCMV infection risk varied between the studies, ranging from 11.4% in a study by Basit et al. performed in Ireland to 60% reported in a study on the French population by Cordier et al. [18,19]. The baseline level of knowledge about the possible primary prevention of cCMV infection was rather unsatisfactory. Studies analyzing the impact of educational interventions on patients’ knowledge about preventive measures reported significant improvement compared to the levels of awareness before the intervention [20,21,22]. The most commonly identified complication of cCMV infection was hearing loss; however, in the majority of cases, the studied population initially had little to no knowledge of complications associated with CMV infection in pregnancy.
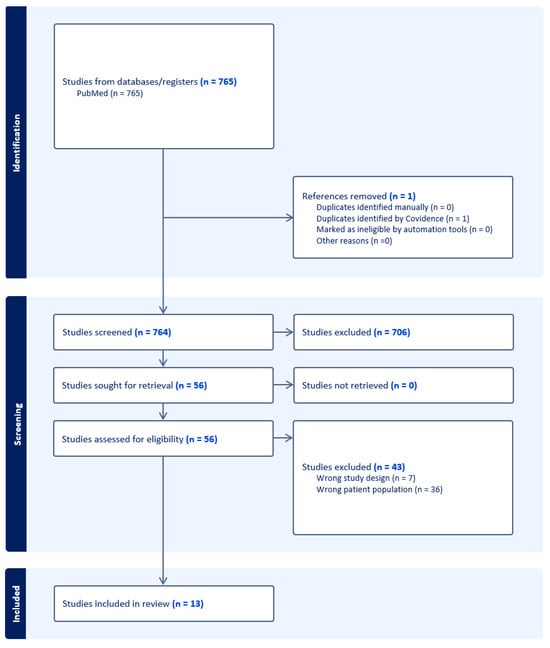
Figure 1.
PRISMA flow diagram of the screening process.

Table 1.
Data extraction results.
4. Discussion
In the results of our review, the complex issue of cCMV awareness among pregnant women emerges as a multifaceted concern warranting a comprehensive examination. Numerous insightful observations can be extracted from our analysis.
Based on the studies included in our review, it is noteworthy that all analyzed studies, even if published after 2020, described the awareness of populations evaluated predating this year (Table 1). It is significant in the light of the publication of the first randomized controlled trial (RCT) proving the effectiveness of high doses of oral valacyclovir in the secondary prevention of cCMV [12]. The very study mentioned has changed the general approach toward cCMV, especially following a recent meta-analysis from 2024, which included two additional observational studies confirming the effectiveness of valacyclovir [31]. Therefore, the lack of proven and effective secondary prophylaxis at the time of all of the analyzed awareness studies should be taken into account.
The general awareness about cCMV in all of the analyzed studies was considered to be low or very low—the lowest percentage of patients who declared an awareness of cCMV was 11.4% in the Irish population (Table 1) [18]. It is important to notice that all of the analyzed study groups were recruited from developed countries (Table 1). In 11 out of 13 analyzed articles, the declared awareness ratio did not exceed 40% of the studied groups [20,21,22,23,24,25,27,28,29,30]. The two exceptions were the Italian study by Vena et al., which reported a ratio of 59.1%, and the French study by Cordier et al., which showed a general ratio of knowledge of 60% [18,24]. Even those relatively satisfactory awareness ratios should be approached with caution. When patients in the study by Vena et al. were further asked about primary preventive measures against cCMV infection, only 8.4% of respondents correctly identified all three proposed behaviors [26]. Based on these findings, it can be suspected that respondents could overestimate their knowledge and understanding of what cCMV is. Furthermore, in the study by Cordier et al., the analyzed group consisted of patients from a university hospital, in which 74% of respondents declared CMV awareness, and from a general hospital, where only 34% of respondents stated the same [19]. The ratio collected in the latter hospital is similar to other studies and can be considered to be more representative of the general population.
As the general knowledge of cCMV was low, one-third of the analyzed studies tried to identify demographical factors associated with higher levels of cCMV awareness [18,19,27]. Higher cCMV awareness was associated with specific demographic factors traditionally typical for higher socioeconomic status: higher education [18,19], non-migrant status [18], and employment status, especially in the healthcare sector [27]. Unfortunately, no study examined the association between demographic factors and not only CMV awareness, but also the knowledge of primary preventive methods or actual preventive behaviors.
Only one of the analyzed studies, performed by Suga et al., tried to estimate the changes in cCMV awareness over time [30]. The study period was 6 years and was divided into four periods; no significant changes were observed. No specific educational intervention was performed over the examined period. Similarly, upon comparing the overlooked findings of all of the studies, no consistent trend toward changes in CMV awareness can be seen; the study with the lowest knowledge ratio was from 2019, while the one with the highest was from 2012 [18,19]. The studies were of heterogeneous design and explored different patient groups.
The knowledge about effective PPM in the analyzed studies is, in most cases, considered even poorer than the general awareness of cCMV. Among the included studies, nine analyzed patients’ knowledge about PPM, one investigated the use of PPM, and one reported patients’ attitudes towards PPM. Across all studies (six in total), in which comparison was feasible, the percentage of correct answers regarding various PPM was lower than the declared knowledge or awareness about cCMV [18,19,25,26,28,30]. The study that analyzed attitudes towards the proposed PPM found a generally positive outlook, with a strong belief in their overall ease of application [27]. The study that analyzed the use of PPM focused on the effect of educational intervention and did not provide specific ratios of initial PPM use [20].
The knowledge about the complications of cCMV was analyzed only in six out of thirteen of the included studies [19,20,21,22,25,29]. One of the studies, unfortunately, did not present its results on this topic at all [21]. The general knowledge about the complications of cCMV did not differ from the previously analyzed two topics, and could be considered to be low or very low. Knowledge about severe complications of cCMV did not exceed 20% of the included patients, except in the aforementioned French study by Cordier et al., in which the neurological complications following cCMV were correctly identified by up to 53% [19]. In this case, however, the population in the study was highly specific and consisted of a large proportion of women from a university hospital.
An interesting topic studied by three of the analyzed studies was the effectiveness of educational interventions [20,21,23]. The authors of the studies agreed that, in the context of low knowledge about cCMV in the general population, there is an urgent need to change that situation. All of the studies proved the significant positive impact of educational interventions, which ranged from educational videos to educational leaflets. The positive impact was seen in all of the analyzed aspects—knowledge about cCMV, PPM, and the complications. The English study by Colbert et al. was designed as a pilot study for a wider intervention in the general UK population, and this context proved the possible effectiveness of educational interventions for the general population [20]. All of the mentioned studies, unfortunately, lacked an analysis of the effectiveness on actual cCMV infection rates and cost-effectiveness calculations.
Considering the recent findings on effective secondary prevention and prenatal treatment opportunities, it is even more clinically relevant to provide pregnant patients with access to reliable educational resources and increase their awareness about cCMV [12,13,31]. One of the strengths of this semi-systematic review is understanding the general perspective and current knowledge status, as well as the identification of areas for improvement due to the inspection of studies including pregnant patients. We decided to include all pregnant patients as they are the target group for secondary prevention during pregnancy. Without their knowledge about the existence and consequences of cCMV, it is not possible to effectively introduce prenatal treatment and avoid/decrease the severity of vertical infections. Our study also indicated a lack of accessible data on the awareness of pregnant women from the low- and middle-income countries and identified a need for adequate research in those settings.
In the opinion of the authors of the review, future studies analyzing CMV awareness and various educational interventions should include knowledge about effective secondary prevention in the form of high doses of valacyclovir. The presented results support a high demand for updating societies’ guidelines to include the possibility of secondary prevention and prenatal treatment for cCMV as well as proposals for increasing pregnant patients’ awareness of cCMV [12,31,32].
5. Conclusions
Patients’ awareness and knowledge about cCMV in developed countries seemed to be generally low or very low during the last decade before the development of effective secondary prevention methods. Educational interventions seem to be effective, and therefore their wide use could be of potential benefit. In the era of available secondary prevention of vertical transmission, it is crucial to concentrate the efforts of different stakeholders to increase the awareness of cCMV among pregnant women.
Author Contributions
Conceptualization, P.B., A.B., M.C., J.K.-B. and E.B.; methodology, P.B., A.B., M.C., J.K.-B., E.B. and J.S.; software, E.B.; validation, J.K.-B., A.U. and E.B; formal analysis, P.B. and A.B.; investigation, P.B., A.B., J.K.-B., A.U. and E.B.; data curation, P.B. and E.B.; writing—original draft preparation, P.B., A.B. and J.K.-B.; writing—review and editing, A.S., E.B., M.C., J.S. and E.R.-W.; supervision, M.C., E.R.-W. and J.S.; project administration, P.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All obtained datasets are included in this publication.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Francki, R.I.B.; Fauquet, C.M.; Knudson, D.L.; Brown, F. (Eds.) Classification and Nomenclature of Viruses: Fifth Report of the International Committee on Taxonomy of Viruses. Virology Division of the International Union of Microbiological Societies; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2012. [Google Scholar]
- Goderis, J.; De Leenheer, E.; Smets, K.; Van Hoecke, H.; Keymeulen, A.; Dhooge, I. Hearing loss and congenital CMV infection: A systematic review. Pediatrics 2014, 134, 972–982. [Google Scholar] [CrossRef] [PubMed]
- Manicklal, S.; Emery, V.C.; Lazzarotto, T.; Boppana, S.B.; Gupta, R.K. The “silent” global burden of congenital cytomegalovirus. Clin. Microbiol. Rev. 2013, 26, 86–102. [Google Scholar] [CrossRef] [PubMed]
- Ssentongo, P.; Hehnly, C.; Birungi, P.; Roach, M.A.; Spady, J.; Fronterre, C.; Wang, M.; Murray-Kolb, L.E.; Al-Shaar, L.; Chinchilli, V.M.; et al. Congenital Cytomegalovirus Infection Burden and Epidemiologic Risk Factors in Countries with Universal Screening: A Systematic Review and Meta-analysis. JAMA Netw. Open 2021, 4, e2120736. [Google Scholar] [CrossRef] [PubMed]
- Rybak-Krzyszkowska, M.; Górecka, J.; Huras, H.; Massalska-Wolska, M.; Staśkiewicz, M.; Gach, A.; Kondracka, A.; Staniczek, J.; Górczewski, W.; Borowski, D.; et al. Cytomegalovirus Infection in Pregnancy Prevention and Treatment Options: A Systematic Review and Meta-Analysis. Viruses 2023, 15, 2142. [Google Scholar] [CrossRef] [PubMed]
- Maltezou, P.G.; Kourlaba, G.; Kourkouni, Ε.; Luck, S.; Blazquez-Gamero, D.; Ville, Y.; Lilleri, D.; Dimopoulou, D.; Karalexi, M.; Papaevangelou, V. Maternal type of CMV infection and sequelae in infants with congenital CMV: Systematic review and meta-analysis. J. Clin. Virol. 2020, 129, 104518. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, K.T.; Horrell, E.M.W.; Ayugi, J.; Irungu, C.; Muthoka, M.; Creel, L.M.; Lester, C.; Bush, M.L. The Natural History and Rehabilitative Outcomes of Hearing Loss in Congenital Cytomegalovirus: A Systematic Review. Otol. Neurotol. 2018, 39, 854–864. [Google Scholar] [CrossRef] [PubMed]
- Pesch, M.H.; Schleiss, M.R. Emerging Concepts in Congenital Cytomegalovirus. Pediatrics 2022, 150, e2021055896. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.P.; Mei, M.J.; Wang, X.Z.; Huang, S.N.; Chen, L.; Zhang, M.; Li, X.Y.; Qin, H.B.; Dong, X.; Cheng, S.; et al. A congenital CMV infection model for follow-up studies of neurodevelopmental disorders, neuroimaging abnormalities, and treatment. JCI Insight 2022, 7, e152551. [Google Scholar] [CrossRef] [PubMed]
- Rybak-Krzyszkowska, M.; Górecka, J.; Huras, H.; Staśkiewicz, M.; Kondracka, A.; Staniczek, J.; Górczewski, W.; Borowski, D.; Grzesiak, M.; Krzeszowski, W.; et al. Ultrasonographic Signs of Cytomegalovirus Infection in the Fetus-A Systematic Review of the Literature. Diagnostics 2023, 13, 2397. [Google Scholar] [CrossRef] [PubMed]
- Pikis, A. Clinical Review: Valcyte® (Valganciclovir Hydrochloride). New Drug Application NDA 22-257/SN00 and sNDA 21-304/SN07. Available online: https://www.fda.gov/files/drugs/published/22257-Valganciclovir-Clinical-PREA.pdf (accessed on 21 March 2024).
- Shahar-Nissan, K.; Pardo, J.; Peled, O.; Krause, I.; Bilavsky, E.; Wiznitzer, A.; Hadar, E.; Amir, J. Valaciclovir to prevent vertical transmission of cytomegalovirus after maternal primary infection during pregnancy: A randomised, double-blind, placebo-controlled trial. Lancet 2020, 396, 779–785. [Google Scholar] [CrossRef]
- D’Antonio, F.; Marinceu, D.; Prasad, S.; Khalil, A. Effectiveness and safety of prenatal valacyclovir for congenital cytomegalovirus infection: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2023, 61, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Zammarchi, L.; Tomasoni, L.R.; Liuzzi, G.; Simonazzi, G.; Dionisi, C.; Mazzarelli, L.L.; Seidenari, A.; Maruotti, G.M.; Ornaghi, S.; Castelli, F.; et al. Treatment with valacyclovir during pregnancy for prevention of congenital cytomegalovirus infection: A real-life multicenter Italian observational study. Am. J. Obstet. Gynecol. MFM 2023, 5, 101101. [Google Scholar] [CrossRef] [PubMed]
- VALTREX® (Valacyclovir Hydrochloride) Caplets Prescribing Information. New Drug Application NDA 20-487/S-007. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021304s008,022257s003lbl.pdf (accessed on 21 March 2024).
- Covidence Systematic Review Software, Veritas Health Innovation, Melbourne, Australia. Available online: www.covidence.org (accessed on 21 March 2024).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Bmj 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Basit, I.; Crowley, D.; Geary, M.; Kirkham, C.; Mc Dermott, R.; Cafferkey, M.; Sayers, G. Awareness and Preventative Behaviours Regarding Toxoplasma, Listeria and Cytomegalovirus Among Pregnant Women. Ir. Med. J. 2019, 112, 947. [Google Scholar] [PubMed]
- Cordier, A.G.; Guitton, S.; Vauloup-Fellous, C.; Grangeot-Keros, L.; Ayoubi, J.M.; Benachi, A.; Picone, O. Awareness of cytomegalovirus infection among pregnant women in France. J. Clin. Virol. 2012, 53, 332–337. [Google Scholar] [CrossRef] [PubMed]
- Calvert, A.; Vandrevala, T.; Parsons, R.; Barber, V.; Book, A.; Book, G.; Carrington, D.; Greening, V.; Griffiths, P.; Hake, D.; et al. Changing knowledge, attitudes and behaviours towards cytomegalovirus in pregnancy through film-based antenatal education: A feasibility randomised controlled trial of a digital educational intervention. BMC Pregnancy Childbirth 2021, 21, 565. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, M.R.; Holttum, J.; Olson, M.; Westenberg, D.; Rubin, N.; Schleiss, M.R.; Nyholm, J. Development and Assessment of a Prenatal Cytomegalovirus (CMV) Educational Survey: Implementation and Impact in a Metropolitan University-Based Clinic. Int. J. Womens Health 2020, 12, 1205–1214. [Google Scholar] [CrossRef] [PubMed]
- Lazzaro, A.; Vo, M.L.; Zeltzer, J.; Rawlinson, W.; Nassar, N.; Daly, K.; Lainchbury, A.; Shand, A. Knowledge of congenital cytomegalovirus (CMV) in pregnant women in Australia is low, and improved with education. Aust. N. Z. J. Obstet. Gynaecol. 2019, 59, 843–849. [Google Scholar] [CrossRef] [PubMed]
- Beaudoin, M.L.; Renaud, C.; Boucher, M.; Kakkar, F.; Gantt, S.; Boucoiran, I. Perspectives of women on screening and prevention of CMV in pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 258, 409–413. [Google Scholar] [CrossRef]
- Greye, H.; Henning, S.; Freese, K.; Köhn, A.; Lux, A.; Radusch, A.; Redlich, A.; Schleef, D.; Seeger, S.; Thäle, V.; et al. Cross-sectional study to assess awareness of cytomegalovirus infection among pregnant women in Germany. BMC Pregnancy Childbirth 2022, 22, 964. [Google Scholar] [CrossRef]
- Monteiro, S.; Gonçalves, A.; Torrão, M.M.; Costa, V.; Almeida, A. Knowledge of cytomegalovirus and available prevention strategies in pregnancy: A cross-sectional study in Portugal. J. Matern. Fetal Neonatal Med. 2023, 36, 2183754. [Google Scholar] [CrossRef] [PubMed]
- Vena, F.; D’Ambrosio, V.; Pajno, C.; Boccherini, C.; Corno, S.; Di Mascio, D.; Piccioni, M.G.; Salerno, M.G.; Bisogni, F.; Brunelli, R.; et al. Pregnant women’s knowledge and behaviour to prevent cytomegalovirus infection: An observational study. J. Perinat. Med. 2021, 49, 327–332. [Google Scholar] [CrossRef]
- Lim, S.L.; Tan, W.C.; Tan, L.K. Awareness of and attitudes toward congenital cytomegalovirus infection among pregnant women in Singapore. Int. J. Gynaecol. Obstet. 2012, 117, 268–272. [Google Scholar] [CrossRef] [PubMed]
- Morioka, I.; Sonoyama, A.; Tairaku, S.; Ebina, Y.; Nagamata, S.; Morizane, M.; Tanimura, K.; Iijima, K.; Yamada, H. Awareness of and knowledge about mother-to-child infections in Japanese pregnant women. Congenit. Anom. 2014, 54, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, M.; Okahashi, A.; Okuyama, K.; Hiraishi, N.; Morioka, I. Awareness and knowledge of congenital cytomegalovirus infection among pregnant women and the general public: A web-based survey in Japan. Environ. Health Prev. Med. 2021, 26, 117. [Google Scholar] [CrossRef] [PubMed]
- Suga, S.; Fujioka, K.; Nakasone, R.; Abe, S.; Fukushima, S.; Ashina, M.; Nishida, K.; Nozu, K.; Iijima, K.; Tanimura, K.; et al. Changes in awareness and knowledge concerning mother-to-child infections among Japanese pregnant women between 2012 and 2018. PLoS ONE 2021, 16, e0244945. [Google Scholar] [CrossRef] [PubMed]
- Chatzakis, C.; Shahar-Nissan, K.; Faure-Bardon, V.; Picone, O.; Hadar, E.; Amir, J.; Egloff, C.; Vivanti, A.; Sotiriadis, A.; Leruez-Ville, M.; et al. The effect of valacyclovir on secondary prevention of congenital cytomegalovirus infection, following primary maternal infection acquired periconceptionally or in the first trimester of pregnancy. An individual patient data meta-analysis. Am. J. Obstet. Gynecol. 2024, 230, 109–117.e2. [Google Scholar] [CrossRef] [PubMed]
- Coll, O.; Benoist, G.; Ville, Y.; Weisman, L.E.; Botet, F.; Maurizio, M.; Anceschi, T.W.P.I.W.G.; Greenough, A.; Gibbs, R.S.; Carbonell-Estrany, X. Guidelines on CMV congenital infection. J. Perinat. Med. 2009, 37, 433–445. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).