Abstract
Background/Objectives: We assessed the impact of frailty on outcomes of endoscopic retrograde cholangiopancreatography (ERCP) in the United States. Methods: The National Readmission Database (2016–2020) was used to identify index and 30-day ERCP readmissions, which were categorized into low-frailty, intermediate-frailty, and high-frailty groups based on the Hospital Frailty Risk Score (HFRS). Outcomes were then compared. Results: Of 885,416 index admissions, 9.9% were readmitted within 30 days of ERCP. The odds of 30-day readmission were higher in the intermediate-frailty group (12.59% vs. 8.2%, odds ratio [OR] 1.67, 95% confidence interval [CI] 1.64–1.71, p < 0.001) and the high-frailty group (10.57% vs. 8.2%, OR 1.62, 95% CI 1.52–1.73, p < 0.001) compared to the low-frailty group. On readmission, a higher HFRS also increased mean length of stay (intermediate-frailty vs. low-frailty: 8.49 vs. 4.22 days, mean difference (MD) 4.26, 95% CI 4.19–4.34, p < 0.001; high-frailty vs. low-frailty: 10.9 vs. 4.22 days, MD 10.9 days, 95% CI 10.52–11.28, p < 0.001) and mean total hospitalization charges (intermediate-frailty vs. low-frailty: $118,996 vs. $68,034, MD $50,962, 95% CI 48, 854–53,069, p < 0.001; high-frailty vs. low-frailty: $195,584 vs. $68,034, MD $127,550, 95% CI 120,581–134,519, p < 0.001). The odds of inpatient mortality were also higher for the intermediate-frailty and high-frailty compared to the low-frailty subgroup. Conclusions: Frailty was associated with worse clinical outcomes after ERCP.
1. Introduction
Frailty, defined as an aging-related syndrome of physiological decline, is characterized by diminished ability to cope with acute stressors. Numerous physical and psychosocial determinants are factored in when defining frailty. Patient frailty has been identified as an independent risk factor for adverse clinical outcomes for a wide array of medical conditions and procedures [1,2,3,4,5,6]. Furthermore, studies have demonstrated that frailty increases healthcare resource utilization and adds to the economic burden on the healthcare sector [7]. As an example, a UK-based longitudinal study estimated that frailty accounts for an added £5.8 billion/year of healthcare-related expenditure across the country [8]. Despite its ubiquity and significant impact on healthcare outcomes, quantifying frailty has been rather challenging. The lack of such quantification has continued to be a significant barrier to the incorporation of frailty into medical decision-making and physician stewardship of healthcare resources. Furthermore, in addition to being inaccurate, previously used frailty assessment tools were often criticized for being quite cumbersome. These tools required varying degrees of manual assessment, which led to a lack of objectivity.
Developed by Gilbert et al. using the International Classification of Diseases (ICD) codes, the hospital frailty risk score (HFRS) has revolutionized assessment of frailty, particularly in an inpatient setting [9]. Using a set of 109 ICD-10 codes that are highly prevalent in frail patients, Gilbert et al. produced a model to weigh the impact of each diagnosis code on frailty. Essentially, an individual’s HFRS is the arithmetic sum of these numeric values. Using this score, the spectrum of frailty can be categorized, making a comparison of individuals in each category possible [9,10,11,12].
Endoscopic retrograde cholangiopancreatography (ERCP), a vital procedure in the arsenal of therapeutic endoscopists, involves the utilization of a side-viewing endoscope under fluoroscopic guidance to perform a wide variety of interventions for pancreaticobiliary disorders [13]. Due to its widespread availability and minimally invasive nature, the utilization of ERCP is on the rise [14]. Advancements in endoscopic techniques and increasing operator experience have led to ensuring the safe use of ERCP for therapeutic purposes [15]. However, there is a significant paucity of data on the impact of frailty in individuals receiving ERCP, particularly in an inpatient setting. Hence, in this study, we aimed to evaluate the utility of the HFRS in predicting outcomes for inpatient use of ERCP. We used one of the largest publicly available healthcare databases, the nationwide readmissions database (NRD), to study the impact of the HFRS on readmission rates, inpatient mortality, and the healthcare burden in the United States (US).
2. Materials and Methods
2.1. Data Source
The data analyzed for this comparative retrospective study were derived from the NRD. The NRD is the largest, publicly available readmission database in the US maintained by the Agency for Healthcare Research and Quality (AHRQ) Healthcare Cost and Utilization Project (HCUP) State Inpatient Databases [16]. For each calendar year, NRD contains discharge information from geographically dispersed and diverse states. It stores both patient-level and hospital-level information, and the hospitals are stratified according to ownership control, the number of beds, teaching status, and metropolitan/non-metropolitan location, using the International Classification of Disease (ICD) codes. The NRD allows for a weighted analysis to obtain 100% of the US readmissions within a given year.
2.2. Study Population
The NRD was utilized from 2016 to 2020 to identify all adult (≥18 years old) hospitalizations that included therapeutic ERCP during the index hospitalization. Using unique hospitalization identifiers, subsequent hospitalization within 30 days of the index hospitalization were tagged as readmission. Individuals under the age of 18 years, traumatic admissions, and elective hospitalizations were excluded from the analysis (Figure 1).
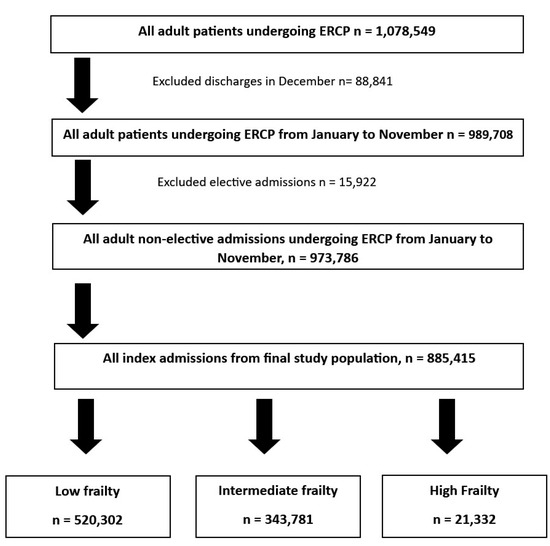
Figure 1.
Inclusion and exclusion criteria used to derive the study sample of adult patients undergoing ERCP on index admission.
2.3. Hospital Frailty Risk Score
ICD-10 codes listed by Gilbert et al. in the original development and validation model were identified in the index admissions receiving ERCP [9]. The same numeric scoring used by Gilbert et al. was used, and the sum of these scores was used to assign HFRS to each admission. They were then classified into low-, intermediate-, and high-frailty groups if their HFRS scores were <5, 5–15, and >15, respectively. These scores were calculated for a single index admission and not cumulatively, ensuring a more accurate frailty status relevant to the admission.
2.4. Statistical Analysis and Outcome Measures
The data were analyzed using Stata® Version 17 software (StataCorp, College Station, TX, USA). All analyses were performed using weighted samples for national estimates in adjunct with HCUP regulations for utilization of the NRD. Hospitalization characteristics were extracted directly from the NRD. The comorbidity burden was quantified using the Charlson Comorbidity Index (CCI) score. The study population was stratified based on gender, age categories, CCI score, insurance type, hospital bed-size, and the odds of 30-day readmission. Mortality within each stratum was calculated using univariate regression analysis with HFRS as the independent variable. Linear regression was used to compare the length of stay (LOS) and total hospitalization charges (THC) at increasing levels of frailty. The THC from 2016 through 2020 was adjusted for inflation in the healthcare sector using the Consumer Price Index (CPI) inflation calculator maintained by the U.S. Bureau of Labor statistics. The Rao–Scott adjusted chi-square test was used in identifying proportions of index and readmission diagnoses.
2.5. Ethical Considerations
The NRD lacks patient- and hospital-specific identifiers. Therefore, this study was exempt from Institutional Review Board (IRB) approval as per the guidelines put forth by our institutional IRB for analysis of the NRD database.
3. Results
3.1. Index Hospitalization Characteristics
Between 2016 and 2020, 885,416 index admissions were identified to have undergone ERCP. Of the index admissions, 520,302 (58.76%) had low frailty, 343,781 (38.83%) had intermediate frailty, and 21,332 (2.41%) had high frailty. As expected, the mean age for low-, intermediate-, and high-frailty index admissions were 55.2, 68.3, and 76.35 years, respectively. The high-frailty group had the highest comorbidity burden with 66.8% of these admissions having a CCI of 3 or more (compared to 16.8% in those with low frailty, and 47.4% in those with intermediate frailty). Furthermore, most of these admissions were largely located in metropolitan areas. Hospitalization characteristics are highlighted in Table 1, Table 2 and Table 3. Indications for ERCP were identified within each cohort. Choledocholithiasis was the most commonly identified indication in all three cohorts (71.8%, 73.49% and 72.64% in the low-, intermediate-, and high-frailty cohorts). This was followed by biliary pancreatitis (28.11%, 25.69%, and 19.59% in the low-, intermediate-, and high-frailty cohorts). A small proportion of the intermediate-frailty (0.13%) and high-frailty (1.21%) admissions underwent ERCP for cholangitis. These distribution of indications for ERCP in the three cohorts is highlighted in Table 4.

Table 1.
Hospitalization characteristics of admissions with HFRS < 5 receiving endoscopic retrograde cholangiopancreatography in the United States.

Table 2.
Hospitalization characteristics of admissions with HFRS 5–15 receiving endoscopic retrograde cholangiopancreatography in the United States.

Table 3.
Hospitalization characteristics of admissions with HFRS > 15 receiving endoscopic retrograde cholangiopancreatography in the United States.

Table 4.
Indication for ERCP on index admission.
3.2. 30-Day Readmissions
The overall 30-day readmission rate for patients who underwent ERCP on index admission was noted to be 9.9%. From index admissions, 8.2%, 12.59%, and 10.57% of patients were readmitted within 30 days in the low-, intermediate-, and high-frailty subgroups, respectively. We noted higher odds of 30-day readmission in the intermediate-frailty (12.59% vs. 8.2%, odds ratio [OR] 1.67, 95% confidence interval [CI] 1.64–1.71, p < 0.001) and the high-frailty groups (10.57% vs. 8.2%, OR 1.62, 95% CI 1.52–1.73, p < 0.001) compared to the low-frailty group (Table 5).

Table 5.
Readmission rates for admissions discharged alive after index admissions that received endoscopic retrograde cholangiopancreatography in the United States.
Upon stratifying by gender, although higher HFRS was associated with higher odds of 30-day readmission for both genders, we noted relatively higher odds of readmission for females in the intermediate-frailty (OR 1.9, 95% CI 1.84–1.96, p < 0.001) and higher-frailty subgroups (OR 1.87, 95% CI 1.72–0.04, p < 0.001) compared to men (OR 1.41, 95% CI 1.37–1.46, p < 0.001 with intermediate frailty and OR 1.34, 95% CI 1.23–1.47, p < 0.001 with severe frailty).
CCI score significantly impacted the predictive capacity of HFRS. Frailty was associated with higher odds of 30-day readmission in patients with a CCI of 1 (OR 1.53, 95% CI 1.45–1.61, p < 0.001 in the intermediate-frailty subgroup and OR 1.49, 95% CI 1.25–1.79, p < 0.0.001 in the high-frailty subgroup). Interestingly, in admissions with a CCI score >1, higher frailty did not increase the odds of readmission. Readmission characteristics are highlighted in Table 1, Table 2 and Table 3.
Through multivariate regression analysis, after adjusting for potential confounders and indication for ERCP, we noted higher odds of 30-day readmission in the intermediate-frailty (adjusted odds ratio [aOR] 1.26, 95% CI 1.23–1.26, p < 0.001) and the high-frailty groups (aOR 1.12, 95% CI 1.04–1.19, p = 0.001) compared to the low-frailty group. These findings are highlighted in Table 6.

Table 6.
Impact of frailty on readmission risks for admissions discharged alive after index admissions that received endoscopic retrograde cholangiopancreatography in the United States—adjusted odds after multivariate regression.
3.3. Inpatient Mortality
The overall inpatient mortality rates were 1.66% and 4.42% for index and 30-day readmissions of ERCP, respectively. With an increase in frailty, we noted higher inpatient mortality for both index and 30-day readmissions. The 30-day readmissions had a higher mortality rate in the low-frailty (1.11% vs. 0.17%, OR 6.86, 95% CI 5.86–8.03, p < 0.001), intermediate-frailty (7.3% vs. 3.49%, OR 2.17, 95% CI 2.04–2.31, p < 0.01), and high-frailty subgroups (10.44% vs. 8.2%, OR 1.29, 95% CI 1.04–1.60, p < 0.001) compared to index admissions. Inpatient mortality is highlighted in Table 7.

Table 7.
Mortality for admissions receiving endoscopic retrograde cholangiopancreatography in the United States.
3.4. Healthcare Burden
The mean THC was higher in the intermediate-frailty ($118,996 vs. $68,034, MD $50,962, 95% CI 48, 854–53,069, p < 0.001) and high-frailty ($195,584 vs. $68,034, MD $127,550, 95% CI 120,581–134,519, p < 0.001) subgroups compared to the low-frailty subgroup. Furthermore, we also noted longer mean LOS for the intermediate-frailty (8.49 vs. 4.22 days, MD 4.26, 95% CI 4.19–4.34, p < 0.001) and high-frailty (10.9 vs. 4.22 days, MD 10.9 days, 95% CI 10.52–11.28, p < 0.001) subgroups compared to the low-frailty subgroup. The healthcare burden is highlighted in Table 8.

Table 8.
Healthcare burden for 30-day readmissions that received endoscopic retrograde cholangiopancreatography in the United States.
3.5. Readmission Diagnoses
We evaluated the most commonly identified principal diagnoses on 30-day readmission within each cohort. Sepsis was the most single most commonly identified readmission diagnosis in each cohort; however, the proportion of readmissions for sepsis was much higher in the intermediate- and high-frailty cohorts (14.8% and 22.22%) compared to the low-frailty cohort (7.9%). Other important principal diagnoses on readmission included pancreatic cancer, acute pancreatitis, choledocholithiasis, cholangiocarcinoma, and cholangitis in the low-frailty cohort. These readmission diagnoses have been highlighted in Table 9.

Table 9.
Commonly identified principal 30-day readmission diagnoses following ERCP, stratified by degree of frailty.
4. Discussion
Our study highlights that increasing frailty is associated with an increase in the rate of 30-day readmission in patients undergoing ERCP, ranging from 8.2% to 12.59% based on the degree of frailty. This increase in odds of readmission was higher for females compared to males. Frailty increased readmission rates in all age groups; However, the presence of frailty in younger patients had a more dramatic increase in the odds of 30-day readmissions. Overall, 30-day readmissions had higher odds of mortality compared to index admissions. Furthermore, the THC and LOS increased significantly with higher frailty scores. In clinical practice, quantifying the impact of frailty on outcomes in patients undergoing ERCP is crucial as it allows therapeutic endoscopists to prognosticate such patients and take preemptive measures to reduce the risk of unfavorable outcomes in these high-risk individuals.
Previous studies have established an association between frailty and readmissions rates for numerous pathologies such as chronic pancreatitis, inflammatory bowel disease, heart failure, and many more [17,18,19]. Despite a clinical understanding of the fact that frail individuals have worse clinical outcomes with ERCP, there is limited data on the impact of frailty on ERCP outcomes [20,21,22,23,24]. Furthermore, the extent of frailty’s impact on these outcomes is also poorly understood, owing to the dearth of real-world data, which has made operationalizing frailty quite challenging. A possible solution for this could be the effective use of HFRS as a frailty indicator. A major finding of our study was increased 30-day readmission rates for frail patients. This finding is in line with a previously published study in 2017 that had a smaller sample size and demonstrated that frail patients undergoing ERCP experienced a higher readmission rate [20]. Another 4-year national study also had similar findings to our study as the authors noted that frailty increased the odds of readmission in admissions for acute biliary pancreatitis [21]. Furthermore, frail patients may have multiple readmissions owing to procedural complications, to which they are more prone compared to the general population [25,26,27,28]. Like any other medical intervention, ERCP is not without risks, and frailty has emerged as a potential predictor for worse clinical outcomes following ERCP. Additional large prospective studies are required to examine the impact of frailty on the incidence of post-ERCP complications, most importantly post-ERCP pancreatitis. An interesting finding in our study was that of a relatively higher readmission risk with increasing frailty in younger patients. There is a substantial amount of literature evaluating frailty in the aged. However, there is scarcity of data on frailty in the young, making this a relatively challenging aspect to contextualize. This finding of our study sheds light on the importance of addressing frailty in the younger patient population. We hypothesize that the fundamental difference in the etiological basis of frailty in younger patients and the psychosocial impact of such frailty play a key role in this finding. Further prospective studies are essential to selectively study the impact of frailty on young patients undergoing ERCP.
Interestingly, another key finding of our study was that in admissions with a CCI score >1, higher frailty did not increase the odds of readmission. This meant that with an increasing comorbid burden, readmission rates become somewhat similar between frail and non-frail patients. This finding further strengthens the reliability of HFRS and reveals the true impact of frailty in individuals with a lower comorbidity burden. CCI scores have previously been used extensively as predictors of readmission in admissions for biliary pathologies [29,30]. However, in patients with lower or no comorbidities, anticipating readmissions becomes more challenging, and limited tools exist to predict readmissions in this subset population. Based on our results, HFRS could prove to be an effective tool for therapeutic endoscopists to screen for and anticipate a higher likelihood of readmission in this subset population.
In our study, we observed that frailty is associated with a significantly higher odds of readmission in females than in males. There are likely multiple reasons for this finding. Firstly, gender-based physiological differences are associated with a higher degree of frailty in women. Low muscle mass and post-menopausal changes attribute a higher degree of frailty to women. Additionally, prior studies have shown that women have a higher risk of post-ERCP complications like post-ERCP pancreatitis [31], which further increases the short-term readmission risk. There are also studies showing that polypharmacy is more prevalent in women [32], which further increases the risk of adverse events. Furthermore, frail women, especially elderly women, may have less robust social support than men, which potentially contributes to poorer care post-discharge, which culminates in higher readmission risk. Women also have a higher prevalence of anxiety and depression [33], which is further worsened by the presence of frailty. This is known to limit optimal post-discharge care, further contributing to a higher readmission burden.
In our study, sepsis was the most commonly identified readmission diagnosis in all three cohorts. This is explained by the association of sepsis with multiple indications for which ERCP is undertaken. These include cholangitis, acute pancreatitis, malignant biliary obstruction, choledocholithiasis with incomplete stone clearance, and so forth. Pancreatic cancer and cholangiocarcinoma were also noted to be significant diagnoses on 30-day readmission. Malignant biliary obstruction can prove to be a therapeutic challenge. ERCP is often undertaken as a measure to provide palliation in this patient population. Owing to the advanced stages at which these malignancies are often diagnosed and the poor therapeutic response encountered in such patients, an inherently high readmission risk is often observed. This is evident in our study as well, where these diagnoses contributed to significant readmission burden across varying degrees of frailty.
Higher frailty is associated with reduced physical activity, multi-morbidity, disability, and adverse outcomes [34]. These can lead to an increased healthcare burden and utilization, in terms of LOS, THC, and inpatient mortality, as observed in our study. In prior published literature, frailty has been also linked to worse in-hospital outcomes with exposure to operative stress [35,36]. A prospective cohort study of 200 patients admitted for acute biliary conditions noted that frail individuals experienced higher rates of mortality and incidence of peri-procedural complications, which translated to longer hospital stays and THC, similar to our study [28]. This further demonstrates that frail patients require more complex, thorough, and multi-disciplinary care to optimize health at discharge and reduce the burden of readmissions. Furthermore, screening for frailty and addressing modifiable factors may be an important factor in optimizing outcomes and reducing the risk of adverse events following ERCP. Further research is needed to develop and validate frailty-screening tools specifically for ERCP and to determine the most effective interventions to mitigate the impact of frailty on procedural outcomes. A multifaceted approach to improve frailty in this high-risk population is crucial. In our study, we only included non-elective admissions. Such admissions need ERCP on a more time-sensitive basis, compared to elective admissions. While this could limit the potential measures to improve frailty pre-procedurally, there is still scope to implement post-procedural measures to reduce frailty-related adverse outcomes. Physical and nutritional rehabilitation, psychosocial support, and vocational rehabilitation could be utilized in optimizing periprocedural patient outcomes and in reducing readmission burden following ERCP, especially in patients with high frailty. Periprocedural optimization of medical comorbidities could directly have a positive impact on reducing readmission burden. Careful selection of patients for periprocedural antimicrobial therapy and early recognition of infectious complications should be emphasized as patients with high frailty are commonly readmitted with sepsis, as evident in our study. Further prospective studies are necessary to evaluate the impact of such measures on reducing frailty-associated adverse outcomes.
Our study has numerous strengths and some limitations. An important strength of our study is the large study population, which has been derived from one of the largest, multi-ethnic and most inclusive inpatient databases in the US. With the weighted nature of the sample, the results of our study are generalizable and applicable to all index hospitalizations and readmissions in the US, offering therapeutic endoscopists real-world data. Despite these strengths, we acknowledge all the limitations associated with our study. The NRD database does not contain information on the etiology, hospital course, pharmacological data, and other treatment aspects of the disease. It also lacks data on patient selection, pre-procedural evaluation, intra-procedural details, specific procedural techniques utilized during the procedure, operator preferences, and pharmacological aspects of management before, during, or after the procedure. Furthermore, due to the retrospective nature of the study design, all biases associated with retrospective studies are applicable to our study. In performing a multivariate regression analysis while evaluating readmission risk, we were unable to adjust for the reason for readmission, due to the nature of the NIS database. Lastly, the NRD is an administrative database maintained through data collection organizations that use the ICD coding system to store inpatient data. Hence, the possibility of human coding errors cannot be excluded. However, despite these limitations, we believe that the large sample size and a comprehensive analysis technique help us better understand the clinical outcomes of 30-day readmissions of ERCP in the US.
In conclusion, ERCP readmissions are a significant healthcare burden that can lead to patient morbidity, mortality, and decreased quality of life. Frailty is a common co-existent factor in patients undergoing ERCP, and it is vital to recognize its key role in readmissions following ERCP. In this study, we noted that frailty not only increases readmissions but also inpatient mortality, LOS, and THC. Furthermore, females are disproportionately affected. HFRS can serve as a vital tool in predicting adverse outcomes, incorporating a multi-disciplinary approach in patient care and careful patient selection to help improve outcomes in patients undergoing ERCP. Additional large prospective studies are essential to assess the utility of incorporating HFRS into complex clinical decision making in an attempt to identify individuals at higher risk of adverse outcomes.
Author Contributions
Conception and design: D.S.D., B.S.M.P., S.C. and N.S. Administrative support: D.S.D., B.S.M.P., S.C., M.K.G. and N.S. Provision, collection, and assembly of data: D.S.D., B.S.M.P., S.C., M.K.G., H.A., S.S. and U.H. Statistical analysis: B.S.M.P. and H.A. Review of literature: all authors. Drafting the manuscript: all authors. Revision of key components of manuscript: all authors. Final approval of manuscript: all authors. Agreement to be accountable for all aspects of the work: all authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The National Readmission Database (NRD) lacks specific patient and hospital identifiers. Hence, the analysis did not require Institutional Review Board (IRB) approval as per the guidelines put forth by our institutional IRB for analysis of database studies.
Informed Consent Statement
The National Readmission Database (NRD) lacks specific patient identifiers. Hence, patient consent was not required.
Data Availability Statement
Restrictions apply to the availability of these data. Data were obtained from Agency for Healthcare Research and Quality and are available from https://hcup-us.ahrq.gov/tech_assist/centdist.jsp (accessed on 1 February 2024) with the permission of the Agency for Healthcare Research and Quality.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Panayi, A.C.; Orkaby, A.R.; Sakthivel, D.; Endo, Y.; Varon, D.; Roh, D.; Orgill, D.; Neppl, R.; Javedan, H.; Bhasin, S.; et al. Impact of frailty on outcomes in surgical patients: A systematic review and meta-analysis. Am. J. Surg. 2019, 218, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Sepehri, A.; Beggs, T.; Hassan, A.; Rigatto, C.; Shaw-Daigle, C.; Tangri, N.; Arora, R.C. The impact of frailty on outcomes after cardiac surgery: A systematic review. J. Thorac. Cardiovasc. Surg. 2014, 148, 3110–3117. [Google Scholar] [CrossRef] [PubMed]
- Graham, M.M.; Galbraith, P.D.; O’Neill, D.; Rolfson, D.B.; Dando, C.; Norris, C.M. Frailty and Outcome in Elderly Patients with Acute Coronary Syndrome. Can. J. Cardiol. 2013, 29, 1610–1615. [Google Scholar] [CrossRef] [PubMed]
- Sy, J.; Johansen, K.L. The impact of frailty on outcomes in dialysis. Curr. Opin. Nephrol. Hypertens. 2017, 26, 537–542. [Google Scholar] [CrossRef] [PubMed]
- Rachel, M.-K.; Javaid, I.; Rebecca, R.; Hatem, E.; Parviz, Y.; Richardson, J.; Sultan, A.; Gunn, J. Impact of frailty on outcomes after percutaneous coronary intervention: A prospective cohort study. Open Heart 2015, 2, e000294. [Google Scholar]
- Green, P.; Arnold, S.V.; Cohen, D.J.; Kirtane, A.J.; Kodali, S.K.; Brown, D.L.; Rihal, C.S.; Xu, K.; Lei, Y.; Hawkey, M.C.; et al. Relation of Frailty to Outcomes After Transcatheter Aortic Valve Replacement (from the PARTNER Trial). Am. J. Cardiol. 2015, 116, 264–269. [Google Scholar] [CrossRef]
- Chi, J.; Chen, F.; Zhang, J.; Niu, X.; Tao, H.; Ruan, H.; Wang, Y.; Hu, J. Impacts of frailty on health care costs among community-dwelling older adults: A meta-analysis of cohort studies. Arch. Gerontol. Geriatr. 2021, 94, 104344. [Google Scholar] [CrossRef]
- Han, L.; Clegg, A.; Doran, T.; Fraser, L. The impact of frailty on healthcare resource use: A longitudinal analysis using the Clinical Practice Research Datalink in England. Age Ageing 2019, 48, 665–671. [Google Scholar] [CrossRef]
- Gilbert, T.; Neuburger, J.; Kraindler, J.; Keeble, E.; Smith, P.; Ariti, C.; Arora, S.; Street, A.; Parker, S.; Roberts, H.C.; et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: An observational study. Lancet 2018, 391, 1775–1782. [Google Scholar] [CrossRef]
- Elsamadicy, A.A.; Koo, A.B.; Reeves, B.C.; Pennington, Z.; Yu, J.; Goodwin, C.R.; Kolb, L.; Laurans, M.; Lo, S.-F.L.; Shin, J.H.; et al. Hospital Frailty Risk Score and healthcare resource utilization after surgery for metastatic spinal column tumors. J. Neurosurg. Spine 2022, 37, 241–251. [Google Scholar] [CrossRef]
- Peterson, R.; Kandregula, S.; Jee, E.; Guthikonda, B. Utility of hospital frailty risk score for predicting postoperative outcomes in craniopharyngioma. J. Neuro-Oncol. 2022, 159, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Elsamadicy, A.A.; Koo, A.B.; Reeves, B.C.; Craft, S.; Sayeed, S.; Sherman, J.J.; Sarkozy, M.; Aurich, L.; Fernandez, T.; Lo, S.-F.L.; et al. Prevalence and Influence of Frailty on Hospital Outcomes After Surgical Resection of Spinal Meningiomas. World Neurosurg. 2023, 173, e121–e131. [Google Scholar] [CrossRef] [PubMed]
- Dahiya, D.S.; Perisetti, A.; Sharma, N.; Inamdar, S.; Goyal, H.; Singh, A.; Rotundo, L.; Garg, R.; Cheng, C.I.; Pisipati, S.; et al. Racial disparities in endoscopic retrograde cholangiopancreatography (ERCP) utilization in the United States: Are we getting better? Surg. Endosc. 2023, 37, 421–433. [Google Scholar] [CrossRef] [PubMed]
- Kröner, P.T.; Bilal, M.; Samuel, R.; Umar, S.; Abougergi, M.S.; Lukens, F.J.; Raimondo, M.; Carr-Locke, D.L. Use of ERCP in the United States over the past decade. Endosc. Int. Open 2020, 8, E761–E769. [Google Scholar] [CrossRef] [PubMed]
- Tarikci Kilic, E.; Kahraman, R.; Ozdil, K. Evaluation of Safety and Outcomes of Endoscopic Retrograde Cholangiopancreatography in 1337 Patients at a Single Center. Medeni. Med. J. 2019, 34, 290–296. [Google Scholar] [PubMed]
- NRD Overview. 2023. Available online: https://www.hcup-us.ahrq.gov/nrdoverview.jsp (accessed on 1 February 2024).
- Kumar, V.; Barkoudah, E.; Jin, D.X.; Banks, P.; McNabb-Baltar, J. Hospital Frailty Risk Score (HFRS) Predicts Adverse Outcomes Among Hospitalized Patients with Chronic Pancreatitis. Dig. Dis. Sci. 2023, 68, 2890–2898. [Google Scholar] [CrossRef]
- Qian, A.S.; Nguyen, N.H.; Elia, J.; Ohno-Machado, L.; Sandborn, W.J.; Singh, S. Frailty Is Independently Associated with Mortality and Readmission in Hospitalized Patients with Inflammatory Bowel Diseases. Clin. Gastroenterol. Hepatol. 2021, 19, 2054–2063.e14. [Google Scholar] [CrossRef]
- Kwok, C.S.; Zieroth, S.; Van Spall, H.G.; Helliwell, T.; Clarson, L.; Mohamed, M.; Mallen, C.; Duckett, S.; Mamas, M.A. The Hospital Frailty Risk Score and its association with in-hospital mortality, cost, length of stay and discharge location in patients with heart failure short running title: Frailty and outcomes in heart failure. Int. J. Cardiol. 2020, 300, 184–190. [Google Scholar] [CrossRef]
- Le, K.; Qian, A.; Nguyen, M.V.; Qiao, E.M.; Nguyen, P.; Krinsky, M.L. S971 The Hospital Frailty Risk Score as a Predictor of Readmission After ERCP. Am. J. Gastroenterol. 2021, 116, S971. [Google Scholar] [CrossRef]
- Ramai, D.; Heaton, J.; Abomhya, A.; Morris, J.; Adler, D.G. Frailty Is Independently Associated with Higher Mortality and Readmissions in Patients with Acute Biliary Pancreatitis: A Nationwide Inpatient Study. Dig. Dis. Sci. 2023, 68, 2196–2203. [Google Scholar] [CrossRef]
- Thomas, M.; Baltatzis, M.; Price, A.; Fox, J.; Pearce, L.; Vilches-Moraga, A. The influence of frailty on outcomes for older adults admitted to hospital with benign biliary disease: A single-centre, observational cohort study. Ann. R. Coll. Surg. Engl. 2023, 105, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Krishna, S.G.; Kruger, A.J.; Patel, N.; Hinton, A.; Yadav, D.; Conwell, D.L. Cholecystectomy During Index Admission for Acute Biliary Pancreatitis Lowers 30-Day Readmission Rates. Pancreas 2018, 47, 996–1002. [Google Scholar] [CrossRef] [PubMed]
- Komici, K.; Cappuccio, M.; Scacchi, A.; Vaschetti, R.; Carpini, G.D.; Picerno, V.; Avella, P.; Brunese, M.C.; Rengo, G.; Guerra, G.; et al. The Prevalence and the Impact of Frailty in Hepato-Biliary Pancreatic Cancers: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 1116. [Google Scholar] [CrossRef] [PubMed]
- Wegner, R.E.; Verma, V.; Hasan, S.; Schiffman, S.; Thakkar, S.; Horne, Z.D.; Kulkarni, A.; Williams, H.K.; Monga, D.; Finley, G.; et al. Incidence and risk factors for post-operative mortality, hospitalization, and readmission rates following pancreatic cancer resection. J. Gastrointest. Oncol. 2019, 10, 1080–1093. [Google Scholar] [CrossRef] [PubMed]
- Sadot, E.; Brennan, M.F.; Lee, S.Y.; Allen, P.J.; Gönen, M.; Groeger, J.S.; Kingham, T.P.; D’angelica, M.I.; DeMatteo, R.P.; Jarnagin, W.R.; et al. Readmission After Pancreatic Resection: Causes and Causality Pattern. Ann. Surg. Oncol. 2014, 21, 4342–4350. [Google Scholar] [CrossRef]
- Smits, F.J.; Verweij, M.E.; Daamen, L.A.; van Werkhoven, C.H.; Goense, L.; Besselink, M.G.; Bonsing, B.A.; Busch, O.R.; van Dam, R.M.; van Eijck, C.H.J.; et al. Impact of Complications After Pancreatoduodenectomy on Mortality, Organ Failure, Hospital Stay, and Readmission: Analysis of a Nationwide Audit. Ann. Surg. 2022, 275, e222–e228. [Google Scholar] [CrossRef]
- Acosta, C.J.; Amin, S.; Goldberg, D. Fr331 utility of frailty assessment in patients with pancreatic cancer undergoing endoscopic retrograde cholangiopancreatography: A nationwide study. Gastroenterology 2021, 160, S295–S296. [Google Scholar] [CrossRef]
- Munigala, S.; Subramaniam, D.; Subramaniam, D.P.; Buchanan, P.; Xian, H.; Burroughs, T.; Trikudanathan, G. Predictors for early readmission in acute pancreatitis (AP) in the United States (US)—A nationwide population based study. Pancreatology 2017, 17, 534–542. [Google Scholar] [CrossRef]
- Wang, Y.; Murphy, D.; Li, S.; Chen, B.; Peluso, H.; Sondhi, V.; Abougergi, M. Thirty-Day Readmission Among Patients with Uncomplicated Choledocholithiasis: A Nationwide Readmission Database Analysis. J. Clin. Gastroenterol. 2023, 57, 624–630. [Google Scholar] [CrossRef]
- Anjella, M.; Vincent, W.; Ahmed, A.; Kaveh, H. S1140 Gender and, E.R.CP Complications: A Nationwide Inpatient Sample Database Analysis. Am. J. Gastroenterol. 2022, 117, e830. [Google Scholar] [CrossRef]
- Cebrino, J.; Portero de la Cruz, S. Polypharmacy and associated factors: A gender perspective in the elderly Spanish population (2011–2020). Front. Pharmacol. 2023, 14, 1189644. [Google Scholar] [CrossRef] [PubMed]
- Altemus, M.; Sarvaiya, N.; Neill Epperson, C. Sex differences in anxiety and depression clinical perspectives. Front. Neuroendocrinol. 2014, 35, 320–330. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wleklik, M.; Uchmanowicz, I.; Jankowska, E.A.; Vitale, C.; Lisiak, M.; Drozd, M.; Pobrotyn, P.; Tkaczyszyn, M.; Lee, C. Multidimensional Approach to Frailty. Front. Psychol. 2020, 11, 564. [Google Scholar] [CrossRef] [PubMed]
- Shinall, M.C., Jr.; Arya, S.; Youk, A.; Varley, P.; Shah, R.; Massarweh, N.N.; Shireman, P.K.; Johanning, J.M.; Brown, A.J.; Christie, N.A.; et al. Association of Preoperative Patient Frailty and Operative Stress with Postoperative Mortality. JAMA Surg. 2020, 155, e194620. [Google Scholar] [CrossRef]
- Basida, S.D.; Dahiya, D.S.; Yousaf, M.N.; Basida, B.; Pinnam, B.S.M.; Gangwani, M.K.; Ali, H.; Singh, S.; Shah, Y.R.; Ahluwalia, D.; et al. Impact of frailty on endoscopic retrograde cholangiopancreatography outcomes in nonagenarians: A United States national experience. World J. Gastrointest. Endosc. 2024, 16, 148–156. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).