Abstract
Knowledge about critical success factors underpinning beneficial treatment outcomes in psychosomatic inpatient rehabilitation is scarce. The aim of this study was to evaluate the influence of patients’ epistemic stance in relation to the improvement of psychological distress during rehabilitation. In this naturalistic longitudinal observational study, n = 771 patients completed routine assessments for psychological distress (BSI-18), health-related quality of life (HRQOL; WHODAS), and epistemic trust (ETMCQ) before (T1) and after (T2) psychosomatic rehabilitation. Patients were grouped as best, average, and worst responders based on their mean BSI-18 changes during treatment, and their mean change in epistemic trust, mistrust, and credulity was compared using repeated measures analyses of variance (rANOVAs). No associations of performance with sex (p = 0.09), age (p = 0.11), or relationship status (p = 0.58) were found. Best responders reported significantly improved epistemic trust (p = 0.001) and reduced epistemic mistrust (p < 0.001), whereas worst responders reported a significant increase in epistemic mistrust (p < 0.001) and credulity (p < 0.001). Average responders did not change for either epistemic trust (p = 0.11), mistrust (p > 0.99), or credulity (p = 0.96). Our results underscore the role of the epistemic stance in psychosomatic and psychotherapeutic treatments. These results help to better understand what might determine psychosomatic rehabilitation outcomes and indicate the role of epistemic trust as a critical success factor.
1. Introduction
In order to address the increasing challenge of mental disorders as a major incremental reason for overall symptom burden, incapacity for work, and disability pension, psychosomatic rehabilitation clinics are a well-established in-patient treatment offer in Austria and other Western European countries [1]. Following the holistic approach of psychosomatic medicine, psychosomatic rehabilitation integrates a biopsychosocial understanding and multi-factorial etiology of illnesses, whereby biological, psychological, and social factors interact to cause and maintain mental and physical symptoms and impaired functioning. To account for this, psychosomatic rehabilitation provides an interdisciplinary treatment approach with the aim of reducing pathology as well as increasing functioning and quality of life [2,3,4]. In Austria, psychosomatic rehabilitation is normally regulated by the performance profile of the responsible pension scheme (PVA) and generally provides a 6-week (42-day) inpatient rehabilitation treatment consisting of individual and group psychotherapy, pharmacotherapy, medical examinations, physical training, occupational therapy, nutrition counseling, creative therapies, and social counseling [1,5]. The diagnostic spectrum addressed in psychosomatic rehabilitation is wide with high prevalence and co-occurrence of mood, anxiety, adjustment, somatoform, and personality disorders, thereby representing a similar spectrum as encountered in primary health care [4]. Most patients undergoing psychosomatic rehabilitation have been experiencing a chronic course of mental disorders that is associated with significant limitations in social or occupational participation [6]. The overall effectiveness of psychosomatic medicine in the treatment of mental disorders has been shown across numerous studies [7,8,9,10]. In addition, various barriers and facilitators of treatment success have been identified, including the social environment, the preparation for inpatient care, work, and health care, as well as patient characteristics [11]. However, about a quarter of patients (20–30%) do not respond to the offered treatment and about 10% even deteriorate during their stay [12]. Although personal characteristics—mainly in terms of self-reflection, awareness, or acceptance—have also been identified as relevant patient factors of psychosomatic rehabilitation outcome [11], only very little is known about their role as transpersonal and transdiagnostic critical success factors in psychosomatic rehabilitation.
In a recent study, mentalizing has been identified as a potential patient factor affecting psychosomatic rehabilitation regarding the improvement of psychological distress [13]. Fonagy and Bateman first introduced the concept defined mentalizing as a mental process that facilitates the understanding and representation of intentional mental states in oneself and others by taking into account one’s own thoughts, needs, emotions, wishes, and desires as well as those of others [14,15,16]. Our research indicates that the patients’ epistemic stance may be a fundamental prerequisite for the development of their mentalizing abilities during psychosomatic inpatient rehabilitation [13]. ‘Epistemic stance’ refers to the stance an individual takes with respect to the delivery of social knowledge, namely your relation to yourself and others, both as ‘providers of knowledge’ and ‘receivers of knowledge’ [17]. The epistemic stance comprises epistemic trust as well as its disruptions, namely epistemic mistrust and epistemic credulity, and describes the openness to social learning with the ability to appropriately evaluate whether information from other individuals or sources is considered by the patient as trustworthy, relevant to the self, and generalizable to other contexts [18]. Although epistemic mistrust refers to a tendency to consider all information sources as unreliable or ill-intended, resulting in resistance to being influenced by others, epistemic credulity comprises a lack of vigilance and discrimination between trustworthy and untrustworthy information, making individuals more vulnerable to misinformation and exploitation [19]. The significance of this concept is particularly evident in the medical system, where the patient’s epistemic stance significantly shapes the reception of information provided by their healthcare professional, who serves as the knowledge provider, regarding their disease and its treatment. Specifically, patients with heightened levels of epistemic mistrust may encounter considerable difficulty in placing trust in their treating physician or psychologist, increasing the likelihood of discontinuing or altering their treatment.
The development of both epistemic trust and mentalizing is based on experiences in early childhood facilitated by secure attachments and interpersonal relationships alongside adequate experiences of being sensitively responded to [18,20,21]. However, children growing up in an environment characterized by sustained and high parental distress, unreliable or malevolent caregiving experiences, or adverse childhood experiences are assumed to experience compromised learning about the social world that results in underdevelopment or even breakdown of epistemic trust [22,23]. Mistrust may arise as people’s motives are over-interpreted, their intentions assumed to deviate from those declared, and the source of the information perceived as not respected. In addition, epistemic hypervigilance and epistemic mistrust may propel the individual to reject the content of the information, confuse its meaning, or even misinterpret it as being malignant [24]. Epistemic mistrust leads to misattributed intentions and the assumption of malevolent motives behind others’ actions, fostering epistemic hypervigilance or inappropriate trust in informants misjudged as credible [24].
It has been suggested that many types of psychopathology could indeed be characterized by temporary or permanent disruptions of epistemic trust and the social learning process it enables [24], and that, in turn, psychotherapy might offer a chance to break this vicious cycle of epistemic mistrust and credulity by inducing epistemic trust, and therefore, social learning within and beyond the therapeutic relationship [18,25,26,27]. To our knowledge, there is no research assessing the role of the epistemic stance as a potential critical success factor underpinning the patient’s propensity to be open or closed towards new information and relational experiences in inpatient psychosomatic rehabilitation. Therefore, the present study aims to investigate whether the patients’ treatment performance during rehabilitation is associated with changes in epistemic trust, epistemic mistrust, or epistemic credulity.
2. Materials and Methods
2.1. Patients and Procedures
Data were collected as part of the clinical routine procedures at the Psychosomatic Rehabilitation Center Montafon (Schruns, Austria) and the Psychosomatic Rehabilitation Center Oberndorf (Oberndorf, Austria). Adult patients underwent multidisciplinary and multimodal inpatient rehabilitation, with costs being covered by the Austrian Social Security Institution. Data were collected in a systematic standardized survey procedure at the beginning (T1; within the first week) and end (T2; within the last week) of the rehabilitation treatment. At the time of the admission, patients were asked whether they were willing to participate in an observational study. Upon written informed consent, they were included. Data were collected electronically using a multifunctional web-based application called the Life App, which is based on the Computer-Based Health Evaluation Software (CHES v7.4) [28]. Patients were included in this study if (a) they completed the BSI-18 assessment at T1 and T2, (b) key sociodemographic data (age, sex) was available, and (c) if ICD-10 diagnosis at admission was given. This study was approved by the Ethics Commission of the University of Innsbruck (no. 75/2023) and was conducted according to the principles of the Declaration of Helsinki.
2.2. Psychosomatic Inpatient Rehabilitation Treatment
Rehabilitation lasted six weeks with nine hours of therapeutic units per week. Patients received multidisciplinary and multimodal treatment, which typically included two 90 min sessions of symptom-specific group therapy (e.g., for trauma, burn-out, somatization, pain, etc.), one hour of individual psychotherapy, two hours of group sessions for relaxation training, as well as additional occupational therapy and physiotherapy if necessary. Additionally, each patient participated in one group session to develop medium-term goals and therapy focus for the next week, as well as two hourly group sessions for resource activation. The guidelines of the Austrian Social Security Institution, which require certain frequencies for the respective therapies, served as a basis for the treatment planning so that treatment provision reflects state of the art provision as per guidelines [29].
2.3. Measures
2.3.1. Brief Symptom Inventory (BSI-18)
Psychological distress was assessed with the Brief Symptom Inventory (BSI-18) consisting of 18 items. A total score and three subscale scores (depression, anxiety, somatization) can be calculated. Good reliability and validity for the subscales and total scores have been reported [30].
2.3.2. Epistemic Trust, Mistrust, and Credulity Questionnaire (ETMCQ)
The Epistemic Trust, Mistrust, and Credulity Questionnaire (ETMCQ) is used to assess a person’s capability of epistemic trust. It consists of 15 items measuring the three subscales ‘epistemic trust’, ‘mistrust’, and ‘credulity’ resulting in a sum score between 15 and 105. High trust reflects a person’s ability to be open to opportunities for social learning, whereas high mistrust indicates a tendency to treat information sources as unreliable and to avoid being influenced by communication from others. High credulity reflects a person’s lack of clarity about their own position, which can lead to high vulnerability to misinformation and exploitation by others [19]. The ETMCQ has been validated in several languages and cultures [19,31,32].
2.3.3. World Health Organization Disability Assessment Scale (WHODAS)
The World Health Organization Disability Assessment Scale (WHODAS 2.0) is a self-report questionnaire used to assess activity and participation limitations in conjunction with the ICF. It consists of six domains of health-related quality of life (HRQOL), namely mobility, cognition, self-care, social functioning, life activities, and participation in the society), which can be summed up to a total score. The WHODAS 2.0 is scored on a continuum from 0 to 100, where 0 indicates the absence of disability in all domains, whereas 100 indicates maximal disability. The WHODAS 2.0 has been identified as a valid and reliable self-report instrument for the assessment of disability [33].
2.4. Statistical Procedures
Patients with complete datasets for the BSI-18 at T1 and T2 were included in the analyses. To determine the best, average, and worst responders during the rehabilitation, the mean improvement in BSI-18 total scores was divided into three equal groups. To avoid influence of baseline differences, the ‘performance score (T2D)’ was used instead of the delta. The T2D is a simple solution to account for baseline differences, based on the formula T2 + (T2 − T1). The formula reflects the individual performance and considers the functional status at the beginning of rehabilitation (changes from T1 to T2; Δ) without problems of mathematical coupling or regression effects, as seen in ANCOVA [34]. The association’s baseline variables (sex, age, relationship status, and ICD-10 diagnosis) with the performance during rehabilitation were investigated with χ2-tests and analyses of variance (ANOVAs). Additionally, mean group differences in the performance groups regarding the level of HRQOL (WHODAS total score and subscales) at the end of treatment (T2) were analyzed using ANOVAs.
To investigate the association of epistemic trust, mistrust, and credulity with the overall performance during rehabilitation, changes in ETMCQ scores before and at the end of rehabilitation in relation to the BSI-18 performance (best, average, worst performance) were compared using repeated measure ANOVAs with Bonferroni-corrected post hoc analyses. The mean levels of the three ETMCQ subscales served as dependent variables (change from T1 to T2) and the BSI-18 performance groups as grouping variables. Effect size values of d < 0.2 and η2 < 0.01 were considered negligible, d ≥ 0.2 and η2 ≥ 0.01 as small effects, d ≥ 0.5 and η2 ≥ 0.06 as medium effects, and d ≥ 0.8 and η2 ≥ 0.14 as large effects [35,36]. A priori sample size calculations indicated that the given ad hoc sample was sufficiently large to detect mean differences in even small effect size (f = 0.1) in the within–between group interaction (three groups, two time points; α = 0.05; 1 − β = 0.95). Estimation of the sample size was conducted using G*Power (3.1) and all other calculations were conducted using IBM SPSS (v21).
3. Results
Of the initial n = 1065 patients, n = 104 (9.8%) patients were excluded due to missing clinical data and sociodemographic data, and another n = 190 (19.8%) patients due to missing BSI-18 data. The remaining n = 771 patients were included in the analyses. A flow chart is presented in Supplementary Materials. Included and excluded patients did not significantly differ in epistemic trust (p = 0.87), epistemic mistrust (p = 0.63) and epistemic credulity (p = 0.19) at baseline (T1), whereas excluded patients had slightly higher depression (p = 0.051), anxiety (p = 0.021), and somatization scores (p = 0.008). However, effect size calculations indicated that group differences were of negligible effect size (g = 0.14–0.18).
The majority of the included patients were female (60.2%), married (50.8%), and between 50 and 60 years old (45.0%). The most frequent clinician-rated ICD-10 main diagnosis was depressive disorder (62.8%). Based on the patients’ self-reported symptoms (BSI-18), three-quarters of the patients (75.1%) scored above the cut-off for depression, 79.9% for anxiety, and 61.3% for somatization. For details, see Table 1.

Table 1.
Sociodemographic data (N = 771).
3.1. Best, Average, and Worst Responders during Psychosomatic Rehabilitation
Based on the T2D scores of the BSI-18, the sample was divided into best (mean T2D = −10.2 ± 8.1 points; n = 261, 33.9%), average (mean T2D = 5.0 ± 4.2 points; n = 259, 33.6%), and worst responders (mean T2D = 32.0 ± 15.0 points; n = 251, 32.6%). In the context of the BSI-18, higher negative T2D scores usually indicate significant improvement. However, as the T2D accounts for the baseline score, patients may not necessarily have negative T2D scores even if they report a substantial reduction in symptoms. For instance, a decrease from 53 points at T1 to 29 points at T2 results in a T2D score of five. This scenario is analogous to a patient with a score of 5 points at T1 and 5 points at T2, where the T2D score would also be five. Better performance was associated with a significantly better overall QoL and functioning at the end of treatment (T2) (F = 216.605; p < 0.001; η2 = 0.38), as well as a better level of cognitive functioning (F = 129.960; p < 0.001; η2 = 0.32), mobility (F = 177.200; p < 0.001; η2 = 0.26), self-care (F = 90.047; p < 0.001; η2 = 0.19), social functioning (F = 129.491; p < 0.001; η2 = 0.26), domestic responsibilities (F = 100.451; p < 0.001; η2 = 0.21), work responsibilities (F = 113.016; p < 0.001; η2 = 0.24), and social participation (F = 155.063; p < 0.001; η2 = 0.29).
The performance groups did not statistically differ in terms of sex (χ2 = 4.82, p = 0.09), age (F(2, 770) = 2.253, p = 0.11), and relationship status (χ2 = 4.69, p = 0.58). However, ICD-10 diagnosis at baseline was significantly associated with performance: patients with trauma-related disorders were classified as worst responders more often than patients with other disorders, whereas patients with adjustment disorders had the lowest proportion of worst responders (χ2 = 21.61, p = 0.017). For details, see Figure 1.
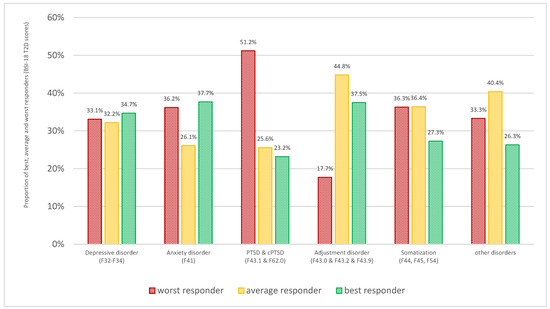
Figure 1.
Proportion of best, average, and worst responders based on the T2D scores of the BSI-18, stratified for ICD-10 diagnostic groups.
3.2. Epistemic Trust as a Critical Success Factor
In the total sample, an overall improvement in epistemic trust was observed (F = 10.902, p = 0.001, η2 = 0.014). However, this was mainly driven by the improved levels of epistemic trust in the best responder group (F = 11.869, p = 0.001, η2 = 0.015), whereas no significant change was observed for average (F = 2.583, p = 0.11, η2 = 0.003) or worst responders (F = 0.479, p = 0.49, η2 = 0.001). At baseline (T1), no significant differences in the epistemic trust subscale levels were observed between the three groups (p = 0.08–0.99). By the end of treatment both best (p < 0.001) and average responders (p = 0.011) reported significantly higher scores than worst responders. For details, see Figure 2 and Table 2.
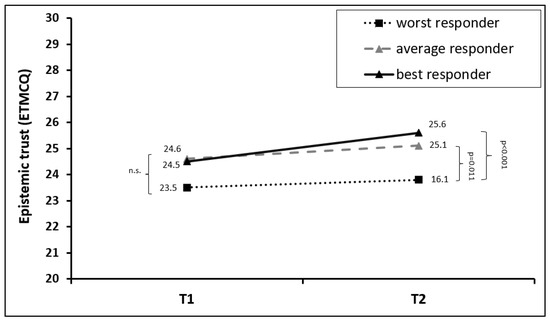
Figure 2.
Mean changes in epistemic trust in the first (T1) and last (T2) week of rehabilitation treatment, stratified for best, average, and worst responders in the T2D BSI-18 total score. The abbreviation “n.s.” stands for “not significant”.

Table 2.
Mean BSI-18 scores in the first (T1) and last (T2) week of rehabilitation, stratified across treatment performance on the BSI-18 (T2D).
In contrast, there was no statistically significant change in epistemic mistrust in the total group (F = 0.459, p = 0.50, η2 = 0.001). However, a significant time × group effect was detected (F = 22.225, p < 0.001, η2 = 0.055), indicating differences in the development of epistemic mistrust across the performance group. Post hoc analyses revealed that the level of epistemic mistrust significantly decreased in the group of best responders (F = 17.354, p < 0.001, η2 = 0.022), whereas it increased in the group of worst responders (F = 27.407, p < 0.001, η2 = 0.035). No significant change was observed in average responders (F = 0.000, p > 0.99, η2 = 0.000). At baseline, a significant difference was only found between average and worst responders (p < 0.001). Interestingly, the best responders scored between average and worst responders but showed the highest decrease in epistemic mistrust during therapy. At the end of the treatment, the worst responders showed significantly more epistemic mistrust than the average and best responders (both p < 0.001). For details, see Figure 3 and Table 2.
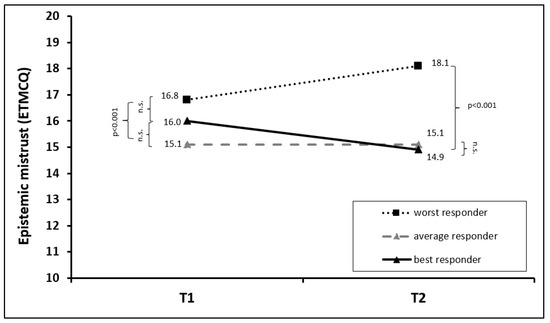
Figure 3.
Mean changes in epistemic mistrust in the first (T1) and last (T2) week of rehabilitation treatment, stratified for best, average, and worst responders in the T2D BSI-18 total score. The abbreviation “n.s.” stands for “not significant”.
For epistemic credulity, a slightly different pattern was observed: overall, there was an increase in epistemic credulity in the total sample (F = 7.374, p = 0.007, η2 = 0.010). In addition, a significant time * group effect was observed (F = 5.110, p = 0.006, η2 = 0.013), indicating differences in the development of epistemic mistrust across the performance group. Post hoc tests revealed that the overall change was mainly caused by a significant increase in epistemic credulity in the worst responders group (F = 17.048, p < 0.001, η2 = 0.022), whereas no significant change was observed for average (F = 0.225, p = 0.64, η2 = 0.000) and good responders (F = 0.002, p = 0.96, η2 = 0.000). Worst responders started therapy with significantly higher credulity scores than average (p < 0.001) and best responders (p = 0.001), whereas those two groups did not differ at baseline (p = 0.56). A similar pattern was observed at the end of treatment: although average and best responders did not change in the extent of their epistemic credulity, in the group of worst responders the credulity levels even increased during therapy. For details, see Figure 4 and Table 2.
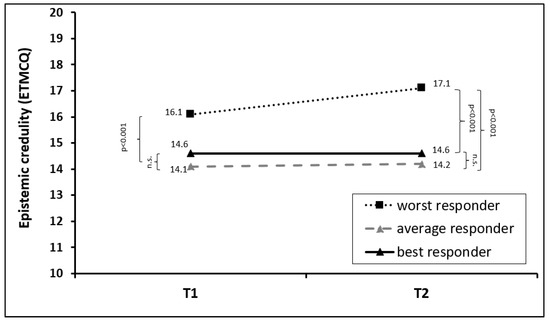
Figure 4.
Mean changes in epistemic credulity in the first (T1) and last (T2) week of rehabilitation treatment, stratified for best, average, and worst responders in the T2D BSI-18 total score. The abbreviation “n.s.” stands for “not significant”.
4. Discussion
Psychosomatic inpatient rehabilitation is a well-established and effective interdisciplinary treatment approach for a variety of mental disorders in various European countries [7,8,9,10]. However, very little is known about the underlying mechanisms that determine treatment success, non-response, or even worsening of patients’ mental health. After grouping patients into three groups of best, average, and well responders based on the change in psychological symptoms during a six-week multimodal inpatient rehabilitation treatment, our results indicate that common patient factors such as sociodemographic characteristics did not determine performance. However, patients with trauma-related disorders were more likely to show worse treatment outcome.
Based on our previous results which identified the patients’ mentalizing capability and epistemic stance as critical success factors underpinning success in psychosomatic rehabilitation outcomes [13], the current study further examined the role of the epistemic stance with regard to the performance during psychosomatic rehabilitation by considering the three specific facets that shape a person’s disposition towards new learning from others and their openness to new relational experiences: trust, mistrust, and credulity. At the beginning of treatment, we found no significant group differences in either trust, mistrust, or credulity between groups, indicating that the initial epistemic stance did not account for subsequent performance during their rehabilitation inpatient stay. These results also suggest that changes in epistemic stance may be engendered through interpersonal experiences during rehabilitation—within the therapeutic alliances with different professionals involved in treatment but also the wider patient collective. In line with this, we observed differentiated changes in the three performance groups. Patients in the best performance group showed significant increases in epistemic trust and simultaneous decreases in epistemic mistrust, whereas no changes were observed regarding epistemic credulity. For average responders, no significant changes could be found in epistemic trust, mistrust, or credulity. In contrast, the worst responders group showed no significant changes in epistemic trust, whereas both epistemic mistrust and credulity increased significantly. In addition, in comparison to the best and average responders, the worst responders demonstrated significantly higher epistemic mistrust and epistemic credulity as well as epistemic credulity at the end of rehabilitation.
It has been described by Nolte, Hutsebaut, Sharp, Campbell, Fonagy, and Bateman [23] that for patients who are prone to avoid mentalizing others (the ‘we-mode’) due to a protective fear of blending with others’ minds, a mentalizing position may be experienced as a threatening experience. It can be unsettling for those prone to feeling overwhelmed or overshadowed by others’ thoughts (epistemic credulity), those who avoid connections (epistemic mistrust), or those swaying between both positions in a disorganized fashion. Hence, it makes sense that patients who showed unfavorable outcomes of psychosomatic rehabilitation might also have experienced a worsening of epistemic mistrust and epistemic gullibility. The mentalization-promoting environment of the psychotherapeutic interventions might have overwhelmed the individual and thus led to a worsening of the epistemic stance.
Our results indicate that changes in the epistemic stance might be directly associated with the performance during psychosomatic rehabilitation. These results can help to better understand the relationship between the epistemic stance and psychopathology. Recent research has shown that mentalizing and epistemic vigilance were associated with an increased risk of acting out behaviors as well as internalizing and externalizing problems in adolescents [37,38] and that epistemic mistrust was associated with an increased risk of developing depressive disorders among young adults during the COVID-19 pandemic [39], whereas robust levels of epistemic trust and mentalizing were identified as protective factors for emotional dysregulation of adolescents during the COVID-19 lockdowns [40]. Research has further suggested that psychopathologies are associated with an impaired epistemic stance and alongside this the disrupted social learning process it enables [24]. Two recent studies demonstrated that epistemic disruption was directly associated with trauma-related disorders [41] and that restoring epistemic trust as well as reductions in epistemic mistrust were linked to improved trauma-related symptoms [42]. Hence, the epistemic stance might prove to be a key component of rehabilitation outcomes. Psychotherapy has been suggested as a means to break the vicious cycle of epistemic mistrust and credulity by inducing epistemic trust [18,25,26,43,44]. Following this line of thinking, psychosomatic rehabilitation might offer an opportunity to use the psychotherapeutic context—including the therapeutic alliance—to its advantage by fostering interpersonal experiences that increase mentalizing and thus build epistemic trust and reduce epistemic mistrust via shared understanding and interpersonal experiences in the so-called ‘we mode’ [23,45]. Fonagy and colleagues highlight that cooperative social learning and the development of epistemic trust need to occur within and beyond the therapeutic relationship [26]. The specific environment of inpatient psychosomatic rehabilitation with its interdisciplinary team and the availability of interactions with other patients offers a direct and safe training ground for a better understanding of self and others. These experiences may be transferred into the broader and thus engendering sustained salutogenetic feedback loops [45]. The importance of trust and the psychotherapeutic relationship becomes even more evident when considering that a dysfunctional—and possibly not trusting—therapeutic alliance has been associated with adverse outcomes during psychosomatic rehabilitation [12,46]. Next to its many advantages, psychosomatic rehabilitation often requires a socio-medical evaluation of patients’ working ability and level of functioning during their stay. This evaluating character might be experienced as challenging when it comes to establishing trust in therapists and physicians. Knowing about the importance of epistemic trust and mistrust might help clinicians better understand possible disruptions during a patient’s treatment by (i) bearing in mind potential causes that might enhance mistrust, (ii) more directly exploring the individual nature of such epistemic dynamics with every patient (e.g., during treatment: ‘What could I do to help us understand better when you feel you cannot trust me?’ or ‘Could you help me spot when I may have said or done something that could undermine your trust in me or the team?’), (iii) communicating to the patient that these difficulties are being recognized, and (iv), as a result, establishing a joint focus for both patient and therapist to come back to this understanding when a rupture occurs. In addition, the facilitation of not only a good but also trustworthy psychotherapeutic relationship alongside encouragement to focus more on positive experiences outside of this relationship might further enhance rehabilitation outcomes. Future research needs to examine this and should consider the epistemic stance as a potential success factor for psychosomatic inpatient rehabilitation while also establishing whether the epistemic stance adds incremental validity in relation to other constructs such as mentalizing, paranoia, or traditional assessments of the therapeutic alliance, all of which are associated with treatment outcome.
Strength and Limitations
This study has several strengths and limitations. To our knowledge, this is the first study to investigate the role of the epistemic stance as a potential factor in explaining therapy outcomes in psychosomatic rehabilitation. The observational design of this study, however, limits the causal interpretation of the study results. Nevertheless, since the data were assessed in clinical routine without a narrow selection of patients, we consider the results of our study to be representative of patients in inpatient rehabilitation treatments. This is further underscored by the similarity of results compared to other studies in the psychosomatic rehabilitation setting [47]. Additionally, a recent study has shown that therapy outcomes in the psychosomatic rehabilitation setting based on real-world data collected from relatively unselected samples during clinical routine may substantially differ from laboratory randomized controlled trials [48] and thus highlight the importance of observational real-world outcome studies.
5. Conclusions
Our results add to the growing body of evidence regarding the role of the epistemic stance in psychopathology as well as psychosomatic and psychotherapeutic treatments. We demonstrate that good performance during psychosomatic rehabilitation is accompanied by improvements in epistemic trust, whereas conversely, worst performance during psychosomatic rehabilitation is associated with increasing epistemic mistrust and credulity. These results help us better understand what might determine psychosomatic rehabilitation outcomes and indicate the role of epistemic trust as a critical success factor.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm13010177/s1, Figure S1: Flow chart for study sample.
Author Contributions
Conceptualization, A.L. and D.R.; methodology, D.R.; formal analysis, D.R.; data curation, A.L., A.K., V.G. and M.J.F.; writing—original draft preparation, D.R. and H.K.; writing—review and editing, A.L., T.N., J.K., V.G., M.J.F., K.L. and C.K.; visualization, D.R.; supervision, A.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the Ethics Commission of the University of Innsbruck (no. 75/2023) and was conducted according to the principles of the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The datasets analyzed in this manuscript are not publicly available due to ethical and legal restrictions. If not already reported within this work, the authors may provide descriptive data on individual medical indicators for admission and discharge or the expected change due to inpatient health care for various groups and diagnoses. Requests for access to anonymized datasets should be directed to the corresponding author (david.riedl@rehabilitation.lbg.ac.at).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sprung, M.; Münch, H.M.; Kaiser, E.; Streibl, L.; Riffer, F. Meta-analysis of evaluation results of psychiatric-psychosomatic rehabilitation in Austria. Neuropsychiatrie 2019, 33, 8–24. [Google Scholar] [CrossRef] [PubMed]
- Burghardt, J.; Riffer, F.; Sprung, M. Gender effects on outcomes of psychosomatic rehabilitation are reduced. PLoS ONE 2021, 16, e0256916. [Google Scholar] [CrossRef] [PubMed]
- Ettlin, T.; Kischka, U. [Psychosomatic Rehabilitation: An Overview]. Ther. Umsch. 2019, 76, 460–464. [Google Scholar] [CrossRef] [PubMed]
- Linden, M. Psychosomatic Inpatient Rehabilitation: The German Model. Psychother. Psychosom. 2014, 83, 205–212. [Google Scholar] [CrossRef]
- Papst, L.; Köllner, V. Using machine learning to investigate earning capacity in patients undergoing psychosomatic rehabilitation-A retrospective health data analysis. Front. Psychiatry 2022, 13, 1039914. [Google Scholar] [CrossRef] [PubMed]
- Glattacker, M.; Rudolph, M.; Bengel, J.; von der Warth, R. Illness Beliefs, Treatment Beliefs, and Fulfilled Treatment Expectations in Psychosomatic Rehabilitation: Associations with Patient Satisfaction. Patient Prefer. Adherence 2022, 16, 3303–3317. [Google Scholar] [CrossRef] [PubMed]
- Baron, S.; Linden, M. Analyzing the effectiveness of inpatient psychosomatic rehabilitation using the mini-ICF-APP. Rehabilitation 2009, 48, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Bermejo, I.; Löschmann, C. 1408—Effectiveness of psychosomatic rehabilitation of depressive disorders. European Psychiatry 2013, 28, 1. [Google Scholar] [CrossRef]
- Löschmann, C.; Steffanowski, A.; Wittmann, W.W.; Nübling, R. Metaanalyse der Effekte stationärer psychosomatischer Rehabilitation—MESTA-Studie. Psychother. Psychosom. Med. Psychol. 2005, 55, S_051. [Google Scholar] [CrossRef][Green Version]
- Piso, B.; Reinsperger, I. Sustainability of psychiatric rehabilitation: Systematic review: Brigitte Piso. Eur. J. Public Health 2014, 24, cku166-107. [Google Scholar] [CrossRef][Green Version]
- Brütt, A.L.; Magaard, J.L.; Andreas, S.; Schulz, H. A qualitative investigation of barriers and facilitators of rehabilitation success from the psychosomatic inpatients’ perspective. Patient Prefer. Adherence 2016, 10, 1881–1888. [Google Scholar] [CrossRef] [PubMed]
- Reuter, L.; Bengel, J.; Scheidt, C.E. Non-response to therapy in acute and rehabilitative psychosomatic inpatient care—A systematic review. Z. Psychosom. Med. Psychother. 2014, 60, 121–145. [Google Scholar] [CrossRef] [PubMed]
- Riedl, D.; Rothmund, M.S.; Grote, V.; Fischer, M.J.; Kampling, H.; Kruse, J.; Nolte, T.; Labek, K.; Lampe, A. Mentalizing and epistemic trust as critical success factors in psychosomatic rehabilitation: Results of a single center longitudinal observational study. Front. Psychiatry 2023, 14, 1150422. [Google Scholar] [CrossRef] [PubMed]
- Bateman, A.; Fonagy, P. Handbook of Mentalizing in Mental Health Practice, 2nd ed.; American Psychiatric Association Publishing: Washington, DC, USA, 2019. [Google Scholar]
- Fonagy, P.; Bateman, A. The development of borderline personality disorder—A mentalizing model. J. Pers. Disord. 2008, 22, 4–21. [Google Scholar] [CrossRef] [PubMed]
- Taubner, S.; Fonagy, P.; Bateman, A. Mentalisierungsbasierte Theraoie; Hogrefe: Göttingen, Germany, 2019; Volume 1. [Google Scholar]
- Fonagy, P.; Allison, E. Beyond Mentalizing: Epistemic Trust and the Transmission of Culture. Psychoanal. Q. 2023, 92, 599–640. [Google Scholar] [CrossRef] [PubMed]
- Fonagy, P.; Allison, E. The role of mentalizing and epistemic trust in the therapeutic relationship. Psychotherapy 2014, 51, 372–380. [Google Scholar] [CrossRef]
- Campbell, C.; Tanzer, M.; Saunders, R.; Booker, T.; Allison, E.; Li, E.; O’Dowda, C.; Luyten, P.; Fonagy, P. Development and validation of a self-report measure of epistemic trust. PLoS ONE 2021, 16, e0250264. [Google Scholar] [CrossRef]
- Beebe, B.; Jaffe, J.; Markese, S.; Buck, K.; Chen, H.; Cohen, P.; Bahrick, L.; Andrews, H.; Feldstein, S. The origins of 12-month attachment: A microanalysis of 4-month mother-infant interaction. Attach. Hum. Dev. 2010, 12, 3–141. [Google Scholar] [CrossRef]
- Innamorati, M.; Imperatori, C.; Harnic, D.; Erbuto, D.; Patitucci, E.; Janiri, L.; Lamis, D.A.; Pompili, M.; Tamburello, S.; Fabbricatore, M. Emotion Regulation and Mentalization in People at Risk for Food Addiction. Behav. Med. 2017, 43, 21–30. [Google Scholar] [CrossRef]
- McGuire, A.; Jackson, Y. A Multilevel Meta-analysis on Academic Achievement Among Maltreated Youth. Clin. Child. Fam. Psychol. Rev. 2018, 21, 450–465. [Google Scholar] [CrossRef]
- Nolte, T.; Hutsebaut, J.; Sharp, C.; Campbell, C.; Fonagy, P.; Bateman, A. The Role of Epistemic Trust in Mentalization-Based Treatment of Borderline Psychopathology. J. Personal. Disord. 2023, 37, 633–659. [Google Scholar] [CrossRef]
- Fonagy, P.; Luyten, P.; Allison, E.; Campbell, C. What we have changed our minds about: Part 2. Borderline personality disorder, epistemic trust and the developmental significance of social communication. Borderline Personal. Disord. Emot. Dysregul. 2017, 4, 9. [Google Scholar] [CrossRef] [PubMed]
- Fonagy, P.; Luyten, P.; Allison, E.; Campbell, C. Mentalizing, Epistemic Trust and the Phenomenology of Psychotherapy. Psychopathology 2019, 52, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Li, E.T.; Midgley, N.; Luyten, P.; Sprecher, E.A.; Campbell, C. Mapping the journey from epistemic mistrust in depressed adolescents receiving psychotherapy. J. Couns. Psychol. 2022, 69, 678–690. [Google Scholar] [CrossRef] [PubMed]
- Fisher, S.; Fonagy, P.; Wiseman, H.; Zilcha-Mano, S. I see you as recognizing me; therefore, I trust you: Operationalizing epistemic trust in psychotherapy. Psychotherapy 2023, 60, 560–572. [Google Scholar] [CrossRef] [PubMed]
- Holzner, B.; Giesinger, J.M.; Pinggera, J.; Zugal, S.; Schopf, F.; Oberguggenberger, A.S.; Gamper, E.M.; Zabernigg, A.; Weber, B.; Rumpold, G. The Computer-based Health Evaluation Software (CHES): A software for electronic patient-reported outcome monitoring. BMC Med. Inform. Decis. Mak. 2012, 12, 126. [Google Scholar] [CrossRef] [PubMed]
- Reiter, D.; Fülöp, G.; Pochobradsky, E.; Röthlin, F.; Stoppacher, A. Austrian Rehabilitation Plan 2020; Gesundheit Österreich: Vienna, Austria, 2020. [Google Scholar]
- Franke, G.H.; Jaeger, S.; Glaesmer, H.; Barkmann, C.; Petrowski, K.; Braehler, E. Psychometric analysis of the brief symptom inventory 18 (BSI-18) in a representative German sample. BMC Med. Res. Methodol. 2017, 17, 14. [Google Scholar] [CrossRef] [PubMed]
- Liotti, M.; Milesi, A.; Spitoni, G.F.; Tanzilli, A.; Speranza, A.M.; Parolin, L.; Campbell, C.; Fonagy, P.; Lingiardi, V.; Giovanardi, G. Unpacking trust: The Italian validation of the Epistemic Trust, Mistrust, and Credulity Questionnaire (ETMCQ). PLoS ONE 2023, 18, e0280328. [Google Scholar] [CrossRef]
- Asgarizadeh, A.; Hunjani, M.; Ghanbari, S. Do we really need “trust”? the incremental validity of epistemic trust over epistemic mistrust and credulity in predicting mentalizing-related constructs. Asian J. Psychiatr. 2023, 87, 103688. [Google Scholar] [CrossRef]
- Federici, S.; Bracalenti, M.; Meloni, F.; Luciano, J.V. World Health Organization disability assessment schedule 2.0: An international systematic review. Disabil. Rehabil. 2017, 39, 2347–2380. [Google Scholar] [CrossRef]
- Zdravkovic, A.; Grote, V.; Pirchl, M.; Stockinger, M.; Crevenna, R.; Fischer, M.J. Comparison of patient- and clinician-reported outcome measures in lower back rehabilitation: Introducing a new integrated performance measure (t2D). Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2022, 31, 303–315. [Google Scholar] [CrossRef] [PubMed]
- Ellis, P.D. The Essential Guide to Effect Sizes: Statistical Power, Meta-Analysis, and the Interpretation of Research Results; Cambridge University Press: Cambridge, MA, USA; New York, NY, USA, 2010. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: New York, NY, USA, 1988. [Google Scholar]
- Malcorps, S.; Vliegen, N.; Luyten, P. Childhood adversity and adolescent acting-out behaviors: The mediating role of mentalizing difficulties and epistemic vigilance. Eur. Child Adolesc. Psychiatry 2023. [Google Scholar] [CrossRef] [PubMed]
- Locati, F.; Benzi, I.M.A.; Milesi, A.; Campbell, C.; Midgley, N.; Fonagy, P.; Parolin, L. Associations of mentalization and epistemic trust with internalizing and externalizing problems in adolescence: A gender-sensitive structural equation modeling approach. J. Adolesc. 2023, 95, 1564–1577. [Google Scholar] [CrossRef] [PubMed]
- De Coninck, D.; Matthijs, K.; Van Bavel, J.; Luyten, P. To be a freshman during the COVID-19 pandemic: A cross-lagged model of depression, mentalizing, and epistemic trust. Personal. Ment. Health, 2023; early view. [Google Scholar] [CrossRef]
- Locati, F.; Milesi, A.; Conte, F.; Campbell, C.; Fonagy, P.; Ensink, K.; Parolin, L. Adolescence in lockdown: The protective role of mentalizing and epistemic trust. J. Clin. Psychol. 2023, 79, 969–984. [Google Scholar] [CrossRef] [PubMed]
- Kampling, H.; Kruse, J.; Lampe, A.; Nolte, T.; Hettich, N.; Brähler, E.; Sachser, C.; Fegert, J.M.; Gingelmaier, S.; Fonagy, P.; et al. Epistemic trust and personality functioning mediate the association between adverse childhood experiences and posttraumatic stress disorder and complex posttraumatic stress disorder in adulthood. Front. Psychiatry 2022, 13, 919191. [Google Scholar] [CrossRef] [PubMed]
- Lampe, A.; Riedl, D.; Kampling, H.; Nolte, T.; Kirchhoff, C.; Grote, V.; Fischer, M.J.; Kruse, J. Improvements of complex posttraumatic stress disorder (cPTSD) symptoms during a psychosomatic inpatient treatment—Results of an observational single center pilot study. Eur. J. Psychotraumatol. 2023; under review. [Google Scholar]
- Tzartzas, K.; de Roten, Y.; Ambresin, G. Intensive and Brief Psychodynamic Psychotherapy in Severely Depressed Inpatients: A Case Study and Thematic Analysis. Psychodyn. Psychiatry 2023, 51, 224–240. [Google Scholar] [CrossRef]
- Knapen, S.; van Diemen, R.; Hutsebaut, J.; Fonagy, P.; Beekman, A. Defining the Concept and Clinical Features of Epistemic Trust: A Delphi study. J. Nerv. Ment. Dis. 2022, 210, 312–314. [Google Scholar] [CrossRef]
- Fonagy, P.; Campbell, C.; Constantinou, M.; Higgitt, A.; Allison, E.; Luyten, P. Culture and psychopathology: An attempt at reconsidering the role of social learning. Dev. Psychopathol. 2022, 34, 1205–1220. [Google Scholar] [CrossRef]
- Henn, J.; Kessemeier, F.; Kobelt-Pönicke, A.; Bassler, M.; Schmidt, J.; Nübling, R. [Rehabilitation Outcome and Therapeutic Alliance of Inpatients of Psychosomatic Rehabilitation with Pension Request]. Psychother. Psychosom. Med. Psychol. 2021, 71, 311–319. [Google Scholar] [CrossRef]
- Peters, M.; Budde, A.; Jeising, A.; Lindner, J.; Schulz, H. [Mentalization ability and treatment success in psychosomatic rehabilitation]. Z. Psychosom. Med. Psychother. 2022, 68, 397–413. [Google Scholar] [CrossRef]
- Oppenauer, C.; Sprung, M.; Gradl, S.; Burghardt, J. Dialectical behaviour therapy for posttraumatic stress disorder (DBT-PTSD): Transportability to everyday clinical care in a residential mental health centre. Eur. J. Psychotraumatol. 2023, 14, 2157159. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).