Abstract
Despite surgical correction, children with anorectal malformations may experience long-term bowel dysfunction, including fecal incontinence and/or disorders of evacuation. Anorectal manometry is the most widely used test of anorectal function. Although considerable attention has been devoted to its application in the anorectal malformation cohort, there have been few attempts to consolidate the findings obtained. This systematic review aimed to (1) synthesize and evaluate the existing data regarding anorectal manometry results in children following anorectal malformation repair, and (2) evaluate the manometry protocols utilized, including equipment, assessment approach, and interpretation. We reviewed four databases (Embase, MEDLINE, the Cochrane Library, and PubMed) for relevant articles published between 1 January 1985 and 10 March 2022. Studies reporting post-operative anorectal manometry in children (<18 years) following anorectal malformation repair were evaluated for eligibility. Sixty-three studies were eligible for inclusion. Of the combined total cohort of 2155 patients, anorectal manometry results were reported for 1755 children following repair of anorectal malformations. Reduced resting pressure was consistently identified in children with anorectal malformations, particularly in those with more complex malformation types and/or fecal incontinence. Significant variability was identified in relation to manometry equipment, protocols, and interpretation. Few studies provided adequate cohort medical characteristics to facilitate interpretation of anorectal manometry findings within the context of the broader continence mechanism. This review highlights a widespread lack of standardization in the anorectal manometry procedure used to assess anorectal function in children following anorectal malformation repair. Consequently, interpretation and comparison of findings, both within and between institutions, is exceedingly challenging, if not impossible. Standardized manometry protocols, accompanied by a consistent approach to analysis, including definitions of normality and abnormality, are essential to enhance the comparability and clinical relevance of results.
1. Introduction
Anorectal malformations represent a spectrum of anomalies affecting the anus, rectum, urinary, and/or genital tracts [1]. The fundamental aims of surgical correction remain consistent today with those described by Rudolph Matas in 1897: “the ideal result of this kind of operation is the restoration of the passage of stool, creating an anus in a normal position with bowel control” [2]. Outcomes with respect to bowel function have greatly improved alongside the evolution of operative repair techniques, most notably, following the advent of the posterior sagittal anorectoplasty [PSARP]) [3]. However, persistent bowel dysfunction, including constipation and fecal incontinence, continues to impact upon a significant proportion of patients long-term [4,5].
As the anal sphincter plays a critical role in both fecal continence and defecation, its function in children with persistent bowel problems after surgical procedures becomes a focal point for investigation. Anorectal manometry is the most widely used investigation to identify abnormalities of anorectal coordination and/or anal sphincter complex dysfunction [6]. The assessment typically comprises a combination of pressure measurements, including evaluation of involuntary function of the anal canal (at rest); voluntary function (squeeze); rectal balloon distension to determine the existence of the rectoanal inhibitory reflex (RAIR); rectoanal coordination during simulated defecation (push maneuver); and rectal sensation [6,7,8,9].
Despite extensive testing with anorectal manometry, the relationships between manometry results and patient symptoms remain poorly defined. In this review, we sought to summarize the methodology and outcomes of anorectal manometry performed in children following repair of anorectal malformations, to appraise current understanding of anorectal function, and guide future work in this cohort.
2. Methods
This systematic review was conducted in compliance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [10]. A primary search was conducted in Embase, MEDLINE, PubMed, and the Cochrane Library in March 2020, and subsequently repeated in March 2022. The search was restricted to human studies published since 1st January 1985. The methodology was published prospectively on PROSPERO (PROSPERO registration: CRD42020177344). The search strategy is summarized in Appendix A.
2.1. Study Selection
After removal of duplicate articles, title and abstract were assessed for eligibility independently by two authors (H.E.B. and M.Y.T.). Cohort studies, case studies, longitudinal studies, and clinical trials were included for review. Conference abstracts, meta-analyses, systematic reviews, animal studies, and in vitro studies were excluded.
The following inclusion criteria were utilized for abstract screening: anorectal manometry performed in children following surgical repair of an anorectal malformation, published in the English language. Studies reporting manometry outcomes in mixed populations (anorectal malformations and other conditions, mixed pediatric and adult cohorts) were included, provided results from children (aged 18 years or less) with anorectal malformations were reported separately in the final analysis. Studies reporting only the pre-operative use of anorectal manometry were excluded.
2.2. Data Extraction
Data were independently extracted by two authors (H.E.B. and M.Y.T.). Extracted cohort characteristics included patient sex; age at assessment; anorectal malformation type; associated anomalies; and post-operative bowel function, including assessment instruments and outcomes. With respect to manometry characteristics, extracted data points included manometry type, including catheter specifications; assessment protocol, including parameters assessed; and motility outcomes, including bowel function correlates.
2.3. Quality Assessment
Non-randomized studies were appraised using the Newcastle–Ottawa Scale [11]. The scale consists of eight items, which evaluate methodological quality based on criteria related to selection, comparability, and exposure. A maximum total of nine may be awarded to the highest quality studies [11].
3. Results
3.1. Search Results
A total of 283 unique articles were identified after removal of duplicate records. Following full-text review, 63 articles were identified, which reported findings of anorectal manometry in children with repaired anorectal malformations. Search results and study selection are presented in Figure 1.
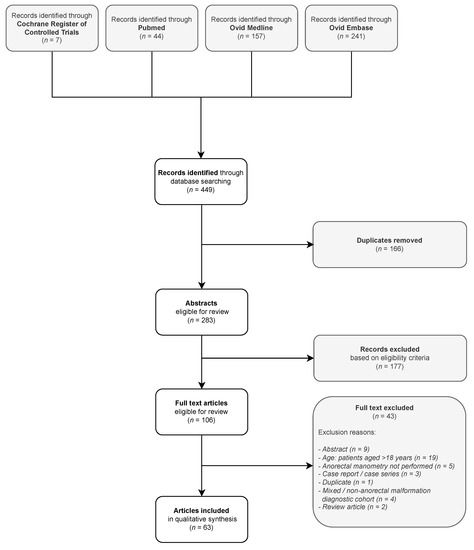
Figure 1.
Study selection flow diagram.
From the combined total cohort of 2155 patients, anorectal manometry results were reported for 1755 children (age range 2 months–18 years) with repaired anorectal malformations. The remainder were either part of a study with a mixed diagnostic cohort (and had a condition other than an anorectal malformation), and/or only a proportion of the cohort underwent anorectal manometry. The median manometry cohort size was 22 children (range 5–115). Insufficient data were provided to calculate the median age or sex ratio. Study characteristics are summarized in Table 1.
Anorectal malformation type was specified for the majority of the cohort (1523/1755 children, 86.8%). The Krickenbeck and Wingspread anorectal malformation classification systems were the most frequently utilized [12,13]. The most frequently reported malformation types were, “high” (267 children); “rectoprostatic fistula” (198 children); and “intermediate” (169 children). The approach to operative repair type was reported for 1250/1755 (71.2%) children in the manometry cohort. Of these, the posterior sagittal anorectoplasty (PSARP) and its variants were the most commonly utilized procedures (868/1250, 69.4%), followed by laparoscopically assisted anorectoplasty (LAARP) (73/1250, 5.8%). Details regarding associated malformations (including sacrospinal anomalies) were provided by less than half of the studies identified for review (28/63, 44.4%). Cohort clinical characteristics are summarized in Table 1.
Studies utilized anorectal manometry to evaluate a range of aspects relating to the management of anorectal malformation patients. Anorectal manometry was performed to compare malformation types [14,15,16,17,18,19]; appraise operative techniques [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]; evaluate post-operative assessment modalities [40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55]; assess and/or prognosticate bowel function [45,56,57,58,59,60]; and investigate the pathophysiology [46,61,62,63,64] and management [65,66,67,68,69,70,71,72] of post-operative bowel dysfunction.
3.2. Quality Assessment
Only 12 included studies adequately addressed the criteria outlined in the Newcastle Ottawa Scale and were classified as “good quality”. The majority were classified as “poor quality”, predominately due to limitations identified in the “comparability” category. Quality evaluations are presented in Table S1.

Table 1.
Clinical characteristics of included studies.
Table 1.
Clinical characteristics of included studies.
| First Author | Year | Cohort (Total (Male)) | Study Population Summary | Age at Time of Manometry | Reported Anorectal Malformation Type 1 | Associated Anomalies | Surgical Repair Type | |
|---|---|---|---|---|---|---|---|---|
| Total 2 | Manometry 3 | |||||||
| Arnoldi [14] | 2014 | 30 (11) | 30 (11) | Toilet-trained children with anorectal malformation with a good, predicted prognosis 4 | Range: 2.5–10 years. Measure of central tendency not provided. Mean follow-up at assessment: 5 years. | Rectoperineal fistula: 19 Rectovestibular fistula: 10 Imperforate anus: 1 | Tethered cord: 6/30 (20%) Excluded: abnormal sacrum. Other anomalies not reported. | Three-stage repair (diverting colostomy, PSARP, colostomy closure): 9 (30%) Primary PSARP: 21/30 (70%) |
| Banasiuk [64] | 2021 | 12 (-) | 12 (-) | Children who had undergone surgery for anorectal disorders, including anal atresia | Median 70 (16–195) months | Perineal fistula (7) Rectourethral fistula (4) Persistent cloaca (1) | Not reported | Not reported |
| Becmeur [23] | 2001 | 14 (9) | 10 (-) | Children following three-flap anoplasty for primary or re-do repair | Not reported. Mean age at study conclusion: 6 years (range 3–14). | High/intermediate: rectobulbar fistula (8); rectovesical fistula (1); cloacal defect (1); long rectal atresia (1). Low: rectovulvar fistula (3). Not specified for manometry cohort | T21 (1); HD (1); psychomotor troubles (2); complex caudal malformation (3); GI duplication (1); ductus arteriosus (1); crossed renal ectopia (1); renal cystic dysplasia (1); hypospadias (1); supernumerary hemivertebra (1). | Three flap anoplasty: 14/14 Primary repair: 9/14 Re-do procedure: 5/14 |
| Bhat [56] | 2008 | 10 (9) | 10 (9) | High or intermediate anorectal malformation, following sigmoid colostomy formation but prior to PSARP | Post-PSARP age: mean 26.3 months (range 15–57). | Rectoprostatic fistula: 6 Rectobulbar fistula: 3 Rectovaginal fistula: 1 | Not reported | PSARP: 10/10 |
| Burjonrappa [61] | 2010 | 86 (53) | 6/14 (4) 5 | Patients with megarectum following surgery for anorectal malformation | Not reported. | High: 23 -developed megarectum: 6 (26%) Low: 63 -developed megarectum: 8 (13%) | Sacral vertebral anomalies: 13/86 | Children with megarectum: Mollard anterior approach: 1 Cutback: 1 Anal transposition: 2 Laparoscopic primary pullthrough: 3 Posterior-sagittal pullthrough: 2 Y-V plasty: 2 Dilatation only: 2 |
| Cahill [24] | 1985 | 6 (6) | 5 (5) | Patients with anorectal malformation following PSARP | Mean: 2.2 years (range 1.25–3.5 years) | Rectoprostatic fistula: 6 | Sacral anomaly: 1 | PSARP: 6/6 |
| Caldaro [43] | 2012 | 17 (13) | 17 (13) | Neurologically healthy children, >4 years, with constipation/FI, following anorectal malformation repair | Mean: 8.3 years (range 5–15 years). | High: rectobladderneck fistula (2); rectourethral fistula (4); cloaca (1). Intermediate: rectourethral fistula (4). Low: rectoperineal fistula (2); rectovestibular fistula (3); anal stenosis (1). | Myelomeningocele: 2 Tethered cord: 1 Renal: 2 VACTERL syndrome: 1 | PSARP: 17/17 |
| Caruso [67] | 2015 | 25 (15) | 25 (15) | Neurologically heathy children >4 years with “true” FI following anorectal malformation repair | Mean: 6.5 years (range 5–9 years). | Vestibular fistula: 3 Rectal atresia: 8 Bulbar fistula: 5 Prostatic fistula: 2 Cloaca: 2 Vaginal fistula: 1 Vesical fistula: 4 | Renal: 12 Genital: 10 Spinal: 5 | PSARP: 25 Laparoscopically assisted proportion not defined. |
| Caruso [72] | 2021 | 14 (-) | 14 (-) | Children with FI or bowel dysfunction not responsive to conventional laxative treatment, receiving transanal irrigation | Mean 10.29 ± 3.25 years | Rectobulbar fistula: 4 Rectovaginal fistula: 2 Rectovesical fistula: 4 Rectoprostatic fistula: 2 Perineal fistula: 2 | Spinal: 6 | Not reported |
| Chen [73] | 1998 | 58 (34) | 44 (-) | All children with anorectal malformation repaired by a single surgeon | Not reported. Manometry was performed within the 1st year of the repair and repeated at 1–2-year intervals. | High/intermediate. Blind pouch (10); fistula: rectobulbar (4); rectoprostatic (7); rectovesical (2); rectovaginal (1); rectovestibular (4); cloacal anomaly (2). Low. Fistula: anocutaneous and anterior perineal anus (16); rectoperineal (4); anovulvar or anovestibular (8). Not specified for manometry cohort | High/intermediate: EA (1); T21 (2); spinal (2); urogenital (5); cardiac (3). Low: EA (1); urogenital anomaly (2); duodenal obstruction (1); cardiac (2). | LSARP: 32 PSARP: 29 R-ASPA: 5 Total surgical cohort (n = 66). Operative details of study (n = 58) and manometry (n = 44) cohorts not provided. |
| Chung [22] | 2018 | 30 (-) | 30 (-) | Toilet-trained children following PSARP or LAARP without neurological comorbidities or cloacal malformation | PSARP: 15.5 years (range 8–32) LAARP: 9 years (range 5–14) | Krickenbeck classification: (PSARP, LAARP) Rectovesical: 2, 3 Rectoprostatic: 7, 8 Rectobulbar: 5, 5 | Not reported | PSARP: 14/30 (46.7%) LAARP: 16/30 (53.3%) |
| Doolin [44] | 1993 | 25 (15) | 25 (15) | Children following repair of anal atresia | Mean: 9.6 years (range 6–16) | Rectourethral fistula: 15 Rectovaginal fistula: 5 Vestibular fistula: 1 Cloaca: 3 Anorectal malformation without fistula: 1 | Not reported | Abdominoperineal pullthrough: 20 Presacral pullthrough: 4 Perineal anoplasty: 1 |
| El-Debeiky [25] | 2009 | 15 (15) | 9 (9) | Males with high anorectal malformation treated with laparoscopic-assisted pull-through | Not reported. Assessed at 3 years of age or older. | Rectobladderneck fistula: 15/15 | Not reported | Laparoscopically assisted pull-through: 15/15 |
| Emblem [40] | 1994 | 16 (8) | 16 (8) | Adolescents with low anorectal malformations following repair | Mean: 14.9 years (12–16) | Anocutaneous fistula: 16 (100%) | Not reported | Anal dilatation: 5 Anal cutback: 11 Secondary procedures: Anal transposition: 3 Posterior anoplasty: 2 |
| Emblem [45] | 1997 | 33 (16) | 33 (16) | Adolescents with anorectal malformations following repair | Intermediate/high: mean 15.8 years (14.6–17.1) Low: mean 14.9 years (13.7–16.2) | High/intermediate: 16 (48%) Low: 17 (52%) | Not reported | Sacroperineal, sacroabdominoperineal, abdominoperineal, perineal procedures according to the malformation type. Cohort distribution not reported. |
| Fukata [41] | 1997 | 15 (14) | 15 (14) | Patients with high or intermediate anorectal malformations | Median: 14 years (8–18) | High: 10 (67%) Intermediate: 5 (33%) | Not reported | Abdominoperineal rectoplasty: 15 (100%) |
| Hedlund [46] | 1992 | 30 (-) | 30 (-) | Patients with anorectal malformations following PSARP, without major sacral malformation | Range: 5–18 years. Measure of central tendency not provided | Bulbar fistula: 9 Prostatic fistula: 8 Vaginal fistula: 1 Vestibular fistula: 6 Rectal atresia: 3 No fistula: 3 | Not reported | PSARP: 30 |
| Heikenen [74] | 1999 | 13 (6) | Colonic manometry: 13 (6) Anorectal manometry: 10 (4) | Children with FI refractory to standard medical therapy following repair of anorectal malformation | Mean 8.6 years (range 5–13) | High: 7/10 Low: 3/10 | Not reported | Not reported |
| Hettiarachchi [47] | 2002 | 15 (5) | 15 (5) | Children with chronic constipation and/or FI following anorectal malformation repair | Median 2.5 years (range 1–15) | High: 6 Intermediate: 5 Low: 4 | Minor sacroneural anomalies: 3 Partial trisomy 22: 2 | “Variety of techniques used for reconstruction” [47]; not further specified. |
| Huang [20] | 2017 | 89 (0) | 43 (0) | Female patients with rectovestibular fistula | Not reported. Age at operation: -Modified semi-PSARP: 1.6 months (9 days–2.5 months) -Transperineal anal transposition: 6.4 (5–8) months Anorectal manometry performed 12 months post-operatively. | Imperforate anus with rectovestibular fistula: 43 | Cardiac: 27 Renal: 10 OA: 2 Polydactyly: 1 Absent coccyx: 1 Sacrococcygeal pilonidal sinus: 1 | One-stage modified semi-PSARP: 39 Transperineal anal transposition: 50 Manometry recipients: 43/89 (48% total cohort) -Modified semi-PSARP: 17 (39%) -Transperineal anal transposition: 26 (61%) |
| Husberg [26] | 1992 | 48 (24) | 43 (-) | Children with high or intermediate anorectal malformation | Range 7 months–16 years | Rectovesical fistula: 1 Rectoprostatic fistula: 15 Rectobulbar fistula: 4 Blind-ending rectum: 5 Cloacal malformation: 11 Rectovaginal fistula: 1 Rectovestibular fistula: 11 Not specified for manometry cohort | Concomitant malformations: 44 | Posterior sagittal approach: 48 |
| Ishihara [48] | 1987 | 49 (-) | 49 (-) | Patients with anorectal malformations following repair | Mean 9.5 years (range 5–20 years 6). | Translevator: 9 Intermediate: 6 Supralevator: 24 Operated at another hospital: 10 | Not reported | Not reported |
| Iwai [15] | 1988 | 28 (-) | 17 (-) | Patients with anorectal malformations following repair | Range: 5–14 years. Measure of central tendency not provided | High: 13 Intermediate: 6 Low: 9 Not specified for manometry cohort | Not reported | Not reported. Department practice -high/intermediate: abdominoperineal rectoplasty -low: perineoplasty |
| Iwai [68] | 1993 | 8 (-) | 8 (-) | Children undergoing biofeedback training for FI following anorectal malformation repair | Range: 6–12 years. Measure of central tendency not provided | High: 6 Intermediate: 2 | Not reported | Abdominoperineal rectoplasty: 7 Abdominosacroperineal rectoplasty: 1 |
| Iwai [65] | 1997 | 14 (-) | 14 (-) | Children undergoing biofeedback training for FI following anorectal malformation repair | Range: 5–14 years. Measure of central tendency not provided | High: 12 Intermediate: 2 | Sacral deformity: 0 | Not reported |
| Iwai [66] | 2007 | 5 (-) | 5 (-) | Children with severe constipation following anorectal malformation repair, treated with herbal medication | Mean: 11.5 years (range 7–17 years) | High: 4 Cloacal anomaly: 1 | Not reported | Not reported |
| Keshtgar [69] | 2007 | 16 (7) | 16 (7) | Children undergoing excision of megarectum for intractable FI | Median: 9 years (range 2–15 years) | High: 6 Intermediate: 4 Low: 6 | EA: 3 Duodenal atresia: 1 Caudal regression with sacral dysgenesis: 1 T21: 1 | Various approaches described for wider population; detail not provided for manometry cohort. |
| Keshtgar [49] | 2008 | 54 (27) | 54 (27) | Children with intractable FI/constipation following anorectal malformation repair | High (n = 34) 7 Median: 10.5 years (range 3.9–21.8) Low (n = 20) Median: 9.4 years (range 4.1–15.3). | Low: anal stenosis and anterior ectopic anus (12); perineal fistula (8). High: rectovestibular fistula (12); rectovesical (2); cloacal malformation (1); rectoprostatic urethral fistula (19). | Megarectum (16); megarectum + neuropathy (11); neuropathy (8); caudal regression (2); sacral dysgenesis (1); esophageal atresia (9); HD (1); T21 (1); T22 (1). | PSARP: 24 Abdominoperineal pullthrough: 8 Stephens: 2 Mollard: 1 Durham Smith: 3 Anal transposition: 7 Anoplasty: 9 |
| Kimura [27] | 2010 | 28 (25) | 28 (25) | Infants managed for high anorectal malformation | Not reported | Rectoprostatic fistula: 21 No fistula: 3 Rectovaginal fistula: 2 Rectovesical fistula: 1 Cloacal malformation: 1 | Not reported | Open ARP: 15 Laparoscopic ARP: 13 |
| Kudou [28] | 2005 | 20 (-) | 20 (-) | Children following LAARP or PSARP for management of high anorectal malformation | LAARP: mean 50.5 months (SD 10 months) PSARP: mean 73 months (SD 12 months). | LAARP: rectourethral fistula (7); rectovesical fistula (2); no fistula (1); rectovaginal fistula (2); cloaca (1). PSARP: rectourethral fistula (2); rectovesical fistula (2); no fistula (1); cloaca (2). | Spinal lipoma: 2 | LAARP: 13 PSARP: 7 |
| Kumar [57] | 2010 | 32 (18) | 32 (18) | Children with anorectal malformations following repair | Infant group: mean 8 months (range 6–12 months) Child group: mean 3.4 years (range 15 months–5.9 years) | Rectoprostatic fistula: 5 Rectobulbar fistula: 3 No fistula: 3 Rectovestibular fistula: 2 Rectovaginal fistula: 1 Anocutaneous fistula: 7 Rectoperineal fistula: 2 Anovestibular fistula: 9 | Renal: 13 Cardiac: 16 Sacral: 4 VACTERL: 1 Chromosomal: 1 | PSARP (high anomalies) or anoplasty (low anomalies). |
| Langemeijer [29] | 1991 | 50 (28) | 39 (-) | Patients with high malformation following PSARP | Not reported. Age at operation: -primary PSARP: 1 month–5 years -redo PSARP: 6–16 years | High: 39 | Not reported | Primary PSARP: 40 Redo PSARP: 10 Not specified for manometry cohort |
| Leung [70] | 2006 | 12 (10) | 9 (-) | Children >5 years old with FI following anorectal malformation repair | Age range: 5–17 years during program completion. | High: 7 Intermediate: 5 Not specified for manometry cohort | Not reported | Pullthrough: 7 PSARP: 5 |
| Lin [30] | 1996 | 27 (-) | 27 (-) | Children with high or intermediate malformation following PSARP or R-APSA | PSARP: <4 years: 10 >4 years: 13 R-APSA: <4 years: 4 | Rectoprostatic fistula: 8 Rectobulbar fistula: 3 Rectovaginal fistula: 3 Blind: 11 Cloacal anomaly: 2 | Spinal: 1 T21: 1 Renal: 2 Genital: 3 Esophageal: 1 | PSARP: 23 R-APSA: 4 |
| Lin [31] | 2003 | 22 (16) | 22 (16) | Patients with high or intermediate malformations following LAR or PSARP | LAR group: mean 16.2 months (range: -) PSARP: mean 17.1 months (range: -) | Rectoprostatic fistula: 12 Rectobulbar fistula: 3 Rectovaginal fistula: 6 Blind pouch: 1 | T21: 2 Genital: 3 Cardiac: 2 Renal: 1 Esophageal: 1 | LAR: 9 PSARP: 13 |
| Liu [32] | 2004 | 113 (90) | 113 (90) | Patients with intermediate or high malformations following PSARP | Not reported. Median age at last follow up: -Group 1: 7.8 years (range 4.9–13 years) -Group 2: 6.7 years (range 5.3–11.6 years) | Rectovesical fistula: 5 Rectoprostatic fistula: 10 Anorectal agenesis w/o fistula: 15 Rectovaginal fistula: 1 Rectobulbar fistula: 49 Anal agenesis w/o fistula: 12 Rectovestibular fistula: 21 | Sacral anomalies: 6 T21: 2 Genital: 4 | Traditional PSARP: 48 One-stage PSARP: 65 |
| Martins [50] | 1996 | 27 (17) | 27 (17) | Patients with intermediate or high malformations following PSARP | Range: 4–11 years. Measure of central tendency not provided. | Rectourethral fistula: 17 Rectovaginal fistula: 5 Rectovestibular fistula: 5 | Sacral malformation: 10 | PSARP: 27 |
| Mert [55] | 2021 | 23 (18) | 23 (18) | Children following anorectal malformation repair, able to cooperate during anorectal manometry without neurological or neurosurgical disorders | Median: 7 (range 5–14) years | Anorectal agenesis without fistula: 5 Rectovesical fistula: 5 Rectobulbar fistula: 4 Rectovestibular fistula: 2 8 Rectoperineal fistula: 7 | Not reported | Not reported |
| Mollard [75] | 1991 | 21 (-) | 13 (-) | Patients with intermediate or high malformations following repair | Not reported | High: 7 Intermediate: 6 | Not reported | Anterior perineal approach |
| Nagashima [62] | 1992 | 159 (108) | 32 (-) | Children following repair of anorectal malformations | Mean: 9 years (range 5–16 years). | High: 17 Intermediate: 6 Low: 9 | Not reported | Abdominoperineal rectoplasty: high/intermediate (23) Perineoplasty: low (9) |
| Niedzielski [33] | 2008 | 94 (44) | 91 (42) | Children following PSARP | Not reported. Assessed 6 months–16 years following PSARP (mean 11.4 years). | Not specified for manometry cohort Perineal fistula (26); vestibular fistula (17); vaginal fistula (5: 2 low, 3 high); anal stenosis (3); cutaneous fistula (1); cloaca (4); no fistula (10); midline raphe fistula (6); bulbar fistula (5); prostatic fistula (9); rectoanal stenosis (5); bladder neck fistula (2); rectal atresia (1). Specified for manometry cohort: high (68); low (23). | Not reported | PSARP: 91 |
| Ninan [71] | 1994 | 13 (9) | 13 (9) | Children undergoing levatorplasty for management of FI following anorectal malformation repair | Not reported. Age at levatorplasty: mean 10.7 years (4–17) | High malformation: 11 Rectovestibular fistula: 1 Cloaca: 1 | Renal: 6 Cardiac: 1 Esophageal: 2 T21: 1 Spinal: 1 | Sacroperineal pullthrough: 5 Sacroabdominoperineal pullthrough: 7 Anoplasty: 1 |
| Okada [21] | 1993 | 10 (4) | 6 (-) | Patients following ASARP for re-operation due to FI following anorectal malformation repair | Not reported. Median age at redo operation: 4.5 years (range 2–7). Median follow-up at assessment: 3.29 years (range 1.1–5.3). | High: 3 Intermediate: 5 Low: 2 Not specified for manometry cohort | Not reported | ASARP (re-operation): 10/10 |
| Penninckx [16] | 1986 | 54 (20) | 19 (-) | Infants with anorectal malformation treated at a single center | Vaginal anal canal: mean 31 ± 15 months Urethral anal canal: mean 7 ± 3 months Vesical anal canal: mean 43 ± 6 months No orifice: mean 14 ± 15 months | Vaginal anal canal: 6 Urethral anal canal: 5 Vesical anal canal: 2 No orifice: 6 | Not reported | Variety of repair strategies reported, without specification of cohort size. |
| Ray [76] | 2004 | 115 (69) | 115 (69) | Children with intermediate or high malformation, following PSARP | Not reported. | High: 12 Intermediate: 103 | Spinal: 2 Renal: 3 | PSARP: - ASARP: - |
| Ren [34] | 2019 | 48 (48) | 22 (22) | Children with intermediate malformations following SILAARP or PSARP | SILAARP: 29.20 months ± 10.21 PSARP: 32.07 months ± 10.54 | Rectobulbar fistula: 48 | Spinal: 18 Renal: 16 Cardiac: 11 | PSARP: 14 SILAARP: 34 |
| Rintala [35] | 1990 | 30 (25) | 30 (25) | Patients with intermediate or high malformations following repair | Group 1: mean 3.1 years (range 1–6 years) Group 2: mean 8.8 years (range 5–13 years) | High: 25 Intermediate: 5 | Not reported | Group 1: 14 PSARP (12) or sacroperineal pull-through (2). Group 2: 16 primary sacro-abdominoperineal pull-through (16); with nine undergoing secondary reconstruction by PSARP (9). |
| Rintala [36] | 1995 | 65 (36) | 53 (-) | Patients with intermediate or high malformations | Not reported | Rectoprostatic fistula: 26 Rectobulbar fistula: 5 Anal agenesis: 4 Rectovesical fistula: 2 Cloaca: 9 Rectovestibular fistula: 16 Rectovaginal fistula: 3 Not specified for manometry cohort | Not reported | PSARP: 53 |
| Rintala [58] | 1993 | 40 (22) | 40 (22) | Patients with intermediate or high anorectal malformations | Not reported | Rectoprostatic fistula: 17 Rectobulbar fistula: 4 Anal agenesis: 2 Cloaca: 8 Rectovestibular fistula: 8 Rectovaginal fistula: 1 | Not reported | PSARP: 40 |
| Rintala [17] | 1990 | 10 (-) | 9 (-) | Patients with intermediate or high malformations | Not reported | High: - Intermediate: - | Not reported | PSARP: 9 |
| Rintala [59] | 1995 | 46 (25) | 46 (25) | Patients following PSARP for intermediate and high malformations | Mean 6.2 years (range 3.8–10). | Rectoprostatic fistula: 19 Rectobulbar fistula: 4 Anal agenesis: 3 Cloaca: 9 Rectovestibular fistula: 9 Rectovaginal fistula: 2 | Significant sacral/spinal defects: 11 T21: 2 | PSARP: 46 |
| Rintala [60] | 1995 | 16 (14) | 16 (14) | Patients undergoing secondary PSARP for intractable FI following primary anorectal malformation repair | Not reported. Manometry performed prior to secondary repair. Age at secondary repair: mean 12.4 years (range 8–16). | Rectourethral fistula: 11 Rectovesical fistula: 2 High anomaly, no fistula: 1 Cloaca: 2 | Significant sacral anomalies: 4 | Secondary repair PSARP: 16 Primary repair Sacroabdominoperineal pullthrough: 10 Abdominoperineal pullthrough: 6 |
| Ruttenstock [18] | 2013 | 12 (0) | 12 (0) | Patients with an externally accessible fistula | Median 585 days (range 197–1287 days) | Perineal fistula: 7 Rectovestibular fistula: 5 | Cardiac: 3 Renal: 4 Sacral: 2 Chromosomal: 1 | ASARP: 6 Mini-PSARP: 6 |
| Sangkhathat [63] | 2004 | 24 (18) | 24 (18) | Infants less than three years of age, post-anoplasty for treatment of anorectal malformation | Mean 9.6 months (range 2–36 months) | Perineal fistula: 6 Vestibular fistula: 3 Rectobulbar urethral fistula: 6 Rectovaginal fistula: 1 Blind rectal pouch: 8 | T21: 4 Opitz syndrome: 1 Caudal regression: 1 | PSARP: - Posterior myectomy and Y-V plasty: - Limited PSARP: - |
| Schuster [19] | 2000 | 10 (1) | 10 (1) | Patients managed for perineal fistula using anal transposition technique | Mean 20.75 months (range 6–72 months) | Perineal fistula: 10 | Not reported | Anal transposition technique: 10 |
| Schuster [42] | 2001 | 17 (10) | 17 (10) | Children with anorectal malformations following PSARP | Mean: 5.4 years (32–120 months) | Fistula location: rectovaginal (3); vestibular (2); rectovesical (2); prostatic (1); bulbar urethral (4) perineal (2). Cloacal malformation: 2 Rectal atresia: 1 | Normal sacrum: 7/17 (42%) | PSARP: 17/17 (100%) Secondary PSARP: 4/17 (24%) |
| Senel [51] | 2007 | 18 (12) | 18 (12) | Children with anorectal malformations following repair | Mean 6.2 years (range 63–104 months) | Rectovesical fistula: 1 Rectoprostatic fistula: 4 Rectal atresia: 1 Rectovestibular fistula: 5 Rectovaginal: 1 9 Rectobulbar: 6 | Not reported | PSARP: 9 Sacroperineal pullthrough: 3 Perineal pullthrough: 6 |
| Sonnino [37] | 1991 | 5 (3) | 5 (3) | Children with FI treated with gracilis muscle transposition | Mean: 13 years (range 10–17 years) | High anorectal malformation: 5 | VACTERL: 3 | Gracilis muscle transposition: 5 Primary repair not reported. |
| Tang [52] | 2017 | 6 (2) | 6 (2) | Children with defecation disorders | Mean 5 years (range 4–9) | Not reported | Not reported | PSARP: 6 |
| Tong [38] | 2011 | 61 (50) | 61 (50) | Infants with high anorectal malformation treated with LAARP vs. PSARP | 3.1–4.4 years Age at operation: LAARP: mean 5.3 months (range 3–10) PSARP: mean 4.9 months (range 3–11) | Rectoprostatic fistula: 39 Rectobulbar fistula: 13 Rectovesical fistula: 2 Rectovaginal fistula: 7 | Not reported | LAARPT: 33 PSARP: 28 |
| Vital Junior [53] | 2007 | 82 (46) | 82 (46) | Children with anorectal malformation following PSARP | Mean: 85.5 months (range 12–204) | High: 45 Intermediate: 37 | Not reported | PSARP: 82 |
| Wang [54] | 2016 | 47 (31) | 47 (31) | Children treated at a single center without congenital megarectum, sacral or spinal deformities | Mean: 4 years (range 1.4–8.9) | Rectourethral fistula: 15 Rectovaginal fistula: 2 Rectovesical fistula: 1 Perineal fistula: 11 Anovestibular fistula: 6 Anal stenosis: 2 Anal hole 10: 1 No fistula: 9 | Not reported | PSARP: 23 Transperineal anorectoplasty: 24 |
| Yang [39] | 2009 | 23 (19) | 23 (19) | Children with high anorectal malformations following PSARP or LAARP | LAARP: mean 17.4 months (SD 4.9) PSARP: mean 19.3 months (SD 6.2) | Rectourethral fistula: 6 Rectoprostatic fistula: 5 Rectovesical fistula: 4 Rectovaginal fistula: 3 Anorectal agenesis: 5 | Not reported | LAARPT: 11 (11 male) PSARP: 12 (8 male) |
1 Anorectal malformation type, as reported in original article. 2 Total cohort with anorectal malformation. 3 Refers to cohort of children undergoing post-operative anorectal manometry following anorectal malformation repair. 4 Good prognosis: specific malformation types (rectoperineal fistula, rectovestibular fistula, imperforate anus without fistula, rectal atresia, cloaca with common channel < 3 cm); associated with a prominent midline groove, suggestive of good perineal muscle, and a normal sacrum. 5 Six of 14 patients with megarectum underwent post-operative anorectal manometry. 6 Subgroup of children operated on at another hospital with normal bowel function excluded due to age >18 years. Other analyses included in the narrative synthesis. 7 Findings of the “high” malformation group excluded from synthesis due to inclusion of participants >18 years of age. 8 Table 1 listed a total of 29 patients, including eight patients following repair of rectovestibular fistula, which is greater than the total study number reported (n = 23). Table 2 (n = 23) reported two patients with rectovestibular fistulae: data taken from Table 2. 9 The number of patients reported to have undergone repair of rectovaginal fistulae differed in the article; data included as presented in Table 1 and Table 2. 10 Not further specified. ARP: abdominoperineal rectoplasty; ASARP: anterior sagittal anorectoplasty; CM: colonic manometry; EA: esophageal atresia; FI: fecal incontinence; GI: gastrointestinal; HD: Hirschsprung disease; LAARP: laparoscopically assisted anorectoplasty; LAARPT: laparoscopically assisted anorectal pullthrough; LAR: laparoscopically assisted pull-through anorectoplasty; LSARP: limited sagittal anorectoplasty; PSARP: posterior sagittal anorectoplasty; R-APSA: Rehbein’s mucosa-stripping endorectal pull-through; R-ASPA: Rehbein’s mucosa-stripping endorectal pull-through in combination with anterior sagittal perineal anorectoplasty; SILAARP: single-incision laparoscopic-assisted anorectoplasty; SD: standard deviation; T21: trisomy 21; T22: trisomy 22; VACTERL: Vertebral, Anorectal Malformation, Cardiac, Tracheo-esophageal, Renal, Limb anomalies.
3.3. Anorectal Manometry Characteristics
3.3.1. Equipment
A range of approaches to anorectal manometry were reported. Fluid-perfused (water, saline or not described) catheters were used by the majority. Other reported methods included balloon or microballoon [16,37,49,50,69], solid-state [25], and microtransducer [40,45,64]. High-resolution manometry was utilized in six studies [22,34,52,54,64,72]. The number of sensors ranged from a single sensor region using the open tip method, to 256 sensors utilized to perform high-resolution anorectal manometry (HRAM) [52,64,72]. Although few studies described sensor spacing, the reported inter-sensor interval ranged from 0.5 mm to 2.5 cm [18,25,30,49,51,52,55,57,63,69,73]. Eight studies did not describe the methods used to perform anorectal manometry [20,23,28,33,39,70,71]. Anorectal manometry characteristics are summarized in Table 2.
3.3.2. Preparation and Sedation
Few studies described the bowel preparation or sedation regimen utilized. With respect to preparation, the majority that described their approach reported the use of enemas, including glycerin and sodium phosphate. The bowel was not routinely prepared prior to anorectal manometry assessment in three studies [37,47,64]. A range of sedation strategies were reported, including chloral hydrate, ketamine, and nitrous oxide [26,28,29,30,31,34,35,38,39,47,48,49,54,57,63,69,73]. Anorectal manometry was performed without sedation in nine studies [14,22,32,43,50,52,55,57,67]. Reported approaches to preparation and sedation are summarized in Table 2.

Table 2.
Summary of reported anorectal manometry specifications.
Table 2.
Summary of reported anorectal manometry specifications.
| First Author | Year | Catheter Type | No. Sensors | Sensor Spacing | Preparation | Sedation/Anesthetic |
|---|---|---|---|---|---|---|
| Arnoldi [14] | 2014 | WP | 4 | - | Enema: performed evening prior | No sedation |
| Banasiuk [64] | 2021 | 3D HRAM | 256 | - | No routine preparation. Saline enema, if required | - |
| Becmeur [23] | 2001 | - | - | - | - | - |
| Bhat [56] | 2008 | FP | Open tip | - | - | - |
| Burjonrappa [61] | 2010 | WP | - | - | - | - |
| Cahill [24] | 1985 | WP | 8 | - | - | - |
| Caldaro [43] | 2012 | WP | 4 | - | Enema: performed day prior | No sedation |
| Caruso [67] | 2015 | WP | 4 | - | - | No sedation |
| Caruso [72] | 2021 | 3D HRAM | 256 | - | - | - |
| Chen [73] | 1998 | WP | 4 | 0.5 cm | - | Rectal secobarbital: 6 mg/kg (<2 years) |
| Chung [22] | 2018 | WP HRAM | 8 | - | - | No sedation |
| Doolin [44] | 1993 | SaP | Open tip | - | - | - |
| El-Debeiky [25] | 2009 | S + WP | - | 2.5 cm | - | - |
| Emblem [40] | 1994 | Micro-transducer | - | - | - | - |
| Emblem [45] | 1997 | Micro-transducer | - | - | - | - |
| Fukata [41] | 1997 | WP Foley catheter | 1 | - | - | - |
| Hedlund [46] | 1992 | WP | 1 | - | - | - |
| Heikenen [74] | 1999 | WP | 8 | - | - | - |
| Hettiarachchi [47] | 2002 | WP | 4 | - | No preparation | Ketamine |
| Huang [20] | 2017 | - | - | - | - | - |
| Husberg [26] | 1992 | WP 11 | 1 | - | - | Ketamine or pentothal-N20 (if required). |
| Ishihara [48] | 1987 | WP | 1 | - | Enema | Monosodium trichlorethyl phosphate (<4 years) |
| Iwai [15] | 1988 | FP Foley catheter | - | - | - | - |
| Iwai [68] | 1993 | FP | - | - | - | - |
| Iwai [65] | 1997 | FP | - | - | - | - |
| Iwai [66] | 2007 | FP | - | - | - | - |
| Keshtgar [69] | 2007 | Microballoon | 4 | 1 cm | - | Ketamine |
| Keshtgar [49] | 2008 | Microballoon | 4 | 1 cm | - | Ketamine |
| Kimura [27] | 2010 | WP Foley catheter | - | - | - | - |
| Kudou [28] | 2005 | - | - | - | - | Triclofos sodium |
| Kumar [57] | 2010 | SaP | 4 | 1 cm | Glycerin enema | No sedation |
| Langemeijer [29] | 1991 | WP | Open tip | - | - | Nitrous oxide (<2 years) |
| Leung [70] | 2006 | - | - | - | - | - |
| Lin [30] | 1996 | WP | 4 | 0.5 cm | - | Secobarbiturates (<2 years) |
| Lin [31] | 2003 | WP | 3 | - | - | Secobarbiturates; general anesthetic (<1 year). |
| Liu [32] | 2004 | WP | Open tip | - | - | No sedation |
| Martins [50] | 1996 | Balloon | 2 | - | - | No sedation |
| Mert [55] | 2021 | FP | 8 | 0.5 mm | Enema: performed 2 h prior (70% sorbitol, glycerin, and tri-Sodium citrate hydrate) | No sedation |
| Mollard [75] | 1991 | FP | 2 | 3 cm | - | - |
| Nagashima [62] | 1992 | WP | Open tip | - | Glycerin enema | - |
| Niedzielski [33] | 2008 | - | - | - | - | - |
| Ninan [71] | 1994 | - | - | - | - | - |
| Okada [21] | 1993 | WP | Open tip | - | - | - |
| Penninckx [16] | 1986 | Microballoon | 1–3 | - | - | - |
| Ray [76] | 2004 | FP | - | - | - | - |
| Ren [34] | 2019 | HRAM 12 | - | - | - | Chloral hydrate |
| Rintala [35] | 1990 | SaP | 1 | - | - | Ketamine (if required) |
| Rintala [36] | 1995 | SaP 13 | 1 | - | - | - |
| Rintala [58] | 1993 | SaP 13 | 1 | - | - | - |
| Rintala [17] | 1990 | SaP 14 | 1 | - | - | - |
| Rintala [59] | 1995 | SaP 13 | 1 | - | - | - |
| Rintala [60] | 1995 | SaP 13 | 1 | - | - | - |
| Ruttenstock [18] | 2013 | SaP | 4 | 5 mm | Bowel washout day prior | - |
| Sangkhathat [63] | 2004 | WP | 2 | 2 cm | - | Chloral hydrate |
| Schuster [19] | 2000 | WP | 8 | - | - | - |
| Schuster [42] | 2001 | WP | 8 | - | - | - |
| Senel [51] | 2007 | WP | 4 | 0.5 cm | - | - |
| Sonnino [37] | 1991 | Double balloon | - | - | No preparation | - |
| Tang [52] | 2017 | WP HRAM | 24 | 1 cm | Sodium phosphate rectal fleet enema | No sedation |
| Tong [38] | 2011 | WP | 8 | - | - | Chloral hydrate 1 mL/kg |
| Vital Junior [53] | 2007 | WP | 4 | - | - | - |
| Wang [54] | 2016 | HRAM | 12 | - | Enema | Chloral hydrate 0.3–0.5 mL/kg (if required) |
| Yang [39] | 2009 | - | - | - | - | Chloral hydrate 1 mL/kg |
11 Manometry performed using either open-perfused catheter or water-filled cuff of a Portex endotracheal tube. 12 Catheter type not further defined (e.g., water-perfused, solid-state). 13 Methods as reported by Rintala; use of sedation unclear in this study population [35]. 14 Methods as reported by Rintala; use of sedation unclear in this study population [77]. FP: fluid-perfused; HRAM: high-resolution anorectal manometry; S: solid-state; SaP: saline-perfused; WP: water-perfused; -: not reported.
3.3.3. Parameters
Assessment of a variety of anorectal manometry parameters was reported. The most commonly reported were resting pressure (anal, rectal or both) (55/63, 87%), rectoanal inhibitory reflex (RAIR) (52/63, 83%), and anal squeeze pressure (29/63, 46%). Reported parameters are summarized in Table 3. Criteria used to define assessed parameters were inconsistent; study definitions are summarized in Table S2.

Table 3.
Reported anorectal manometry parameters. Comparable parameters are grouped.
3.4. Anorectal Manometry Outcomes
Studies demonstrated significant variation with respect to the equipment, assessment protocols, and parameter definitions utilized. As such, absolute values for manometry outcomes were not combined. Key findings and study limitations are summarized in Table 4; absolute values of consistently reported parameters are summarized in Table S2.

Table 4.
Summary of key anorectal manometry findings.
3.4.1. Resting Pressure
The resting pressure was reported by 87% of studies. In most studies, this referred to the anal canal at rest [14,16,17,18,19,24,26,27,28,30,31,32,34,36,38,39,40,41,43,45,46,48,49,51,52,54,55,56,57,58,59,60,62,65,66,67,68,69,72,74], but two studies only reported rectal resting pressures [20,44], while another five reported both anal and rectal resting pressure [21,33,35,63,73]. In addition to assessment of the anorectum, one study also included assessment of the rectosigmoid region (resting pressure recorded 20, 15, 10, and 5 cm proximal to the anal verge) [62]. Six studies did not define the location of assessment [23,25,42,50,53,64,76].
Whilst the majority did not specify their approach to assessment of resting pressure [20,23,25,26,28,30,31,32,33,34,36,39,40,49,50,52,53,54,55,58,59,64,65,66,68,69,76], assorted approaches were described by those that did. Resting pressure was variably reported as the mean [14,24,41,43,46,51,56,63,67,72] or maximal [16,17,21,27,45,48,62] resting pressure, or according to study-specific measurements [18,19,35,38,42,57,60,74]. Manometry parameter definitions are summarized in Table S2.
Reported absolute values of resting pressure varied between studies. Resting pressure ranged from 6.57 mmHg (measure of central tendency not described) in the incontinent group assessed by Martins et al. [50], to 75.75 ± 16.8 mmHg identified, using computerized vector manometry, by Schuster et al. [19]. Outcomes of anorectal manometry, including absolute values, are summarized in Table S2.
Resting pressure was consistently reduced in children with anorectal malformations, compared with either normative values obtained from healthy children [42,46,57,64] or other diagnostic groups [72]. More complex malformations were typically associated with lower resting pressures than less complex malformations [23,33,43,45,48,49,51,62,76], although this was not uniform [63]. Reduced resting pressure was frequently identified in the setting of fecal incontinence [25,37,39,40,45,46,48,49,50,51,53,58,65,73,74,76]. With respect to obstructive symptoms, two studies identified significantly higher resting pressures in constipated than non-constipated patients [43,63], whilst another did not [58].
3.4.2. Rectoanal Inhibitory Reflex
Assessment of the RAIR was reported in 52 studies (52/63, 83%); however, the criteria used to define the RAIR varied [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,41,43,44,45,46,47,49,50,51,53,54,55,57,58,59,60,61,63,64,66,68,69,73,74,75,76]. For example, a positive RAIR was defined according to an absolute pressure decrease (i.e., >5 mmHg, >15 mmHg, >1 kPa) [14,49,57,74]; percentage reduction relative to resting pressure (i.e., >25%, >50%) [64,73]; or qualitative criteria (i.e., “relaxation of the internal sphincter”, “decrease of anal pressure”, “anal response”, “clear pressure decrease”) [24,26,44,46,50]. In addition, there were variable inclusion of criteria related to duration of relaxation (i.e., “sustained for 5 seconds”) [22], rectal balloon volume (i.e., [reflex present at] 60 mL, 100–150 mL) [47,69] and/or reflex reproducibility (i.e., “present on 3 consecutive attempts”) [36,58]. The proportion of the cohort with an RAIR identified varied maximally, ranging from 0% [35,50,60,65,66,68,76] to 100% [16,18,24,25,34,40,55,59].
3.4.3. Squeeze Pressure
Squeeze pressure was assessed by 29/63 (46.0%) studies [15,22,25,29,32,37,38,40,42,43,44,45,46,50,52,53,55,60,63,64,65,66,67,68,70,71,72,74,76]. Variable criteria were used to define and assess squeeze pressure, including average/maximal anal squeeze pressure (expressed as absolute values or increment relative to resting pressure), voluntary contraction pressure, voluntary sphincter contraction, peak squeeze pressure, maximal mean segmental pressure during squeeze, and squeeze pressure of the high-pressure zone. Reported squeeze pressures ranged from 0 mmHg (prior to gracilis transposition for treatment of severe fecal incontinence) [37] to a median of 121.7 mmHg (range 38.2–46.8 mmHg) identified by Banasiuk et al. [64]. Of those that reported comparison of squeeze pressure by complexity of malformation type, there was some evidence that more complex malformation types had reduced squeeze pressure relative to less complex types [55,62]; however, this was not uniform [15].
3.4.4. Normal Findings
In order to define abnormalities of anorectal function, an understanding of “normal” pediatric physiology is needed. However, the definitions of what was considered normal were either not reported or incompletely described by most studies included in this review. For example, there was variability with respect to both anorectal manometry parameters considered to be significant, and the absolute pressure values within parameters that were considered within normal range. Consequently, the understanding of “normal” varied markedly between studies (Table S2).
3.4.5. Post-Operative Outcome Assessment
Established measures were used to assess post-operative bowel function in 36 studies [14,15,18,20,21,22,23,25,27,28,32,33,34,38,39,40,41,42,43,45,47,49,51,55,56,60,61,64,65,66,67,68,69,70,72,76]. Measures included the Kelly, Rintala, Wingfield, and Krickenbeck continence scoring methods, with the Kelly score and its variants being utilized most frequently [15,21,25,28,33,38,39,41,42,51,52,56,65,68]. Study-specific assessments of bowel function were reported by 19 studies. Bowel function was either not assessed or not described by the remainder. Few studies provided symptom definitions. In those that reported the definitions utilized, inconsistent criteria were demonstrated. For example, constipation was variably defined by frequency (e.g., “<1 bowel action per day”, “bowel action every 2–3 days”), management requirements (e.g., “cisapride or laxatives but without enemas”, “enema required daily to achieve bowel action”, “dietary requirements”), and/or subjective impression of severity (e.g., “severe, unmanageable”) [33,35,37,58,62,73]. Post-operative bowel function assessment measures and findings are summarized in Table 5.

Table 5.
Reported post-operative bowel function: assessment measures and outcomes.
4. Discussion
A significant proportion of children with anorectal malformations experience disorders of evacuation and/or fecal incontinence following operative repair. Continence may be affected by a variety of factors, including malformation type, associated sacro-/spinal anomalies, and operative repair type, including intra- and/or post-operative complications. Due to the variable etiology of fecal incontinence and evacuation disorders, symptoms alone are often insufficient to direct treatment in cases refractory to conservative management [6]. Anorectal manometry may be used to investigate the pathophysiology underlying anorectal dysfunction. To our knowledge, this review is the first to systematically evaluate post-operative anorectal manometry performed in children with anorectal malformations.
In assessing 63 studies, our overall finding was a complete lack of consistency between manometry protocols, analysis of data, and interpretation of findings. This echoes the conclusion of a similar review of anorectal manometry performed in adult populations [7]. Despite studies identifying abnormalities in anorectal function, definitions of normal were rarely provided or vaguely described. Collectively, this makes interpretation of the findings difficult, whilst comparison of data between studies is impossible.
4.1. Manometry Outcomes
In 1834, Roux de Brignoles described the importance of preserving the fibers of the sphincter mechanism during anorectal malformation repair, demonstrating the long-standing recognition of their importance [2]. In contemporary practice, anorectal manometry may be used to assess post-operative function of the sphincter complex: activity of the internal anal sphincter (IAS) is understood to provide the majority of resting anal pressure, whilst the external anal sphincter (EAS) is largely responsible for voluntary contraction (squeeze pressure). Hypotonia may, therefore, be associated with presentations of fecal incontinence, whilst increased resting pressure may underlie some rectal evacuation disorders.
The most consistently reported findings identified by studies included in this review were of reduced resting pressure in children with repaired anorectal malformations (usually relative to unspecified normative values or other diagnostic cohorts), with the decrease particularly evident in more complex malformation types and/or in the setting of non-retentive fecal incontinence [23,25,33,37,39,40,42,43,45,46,48,49,50,51,53,57,58,62,64,65,72,73,74,76]. Following re-operation for the management of severe fecal incontinence, improvements in resting pressure were similarly associated with improved continence [21,37].
These findings are not unexpected, considering the underlying developmental abnormalities and the subsequent impacts of operative intervention on an underdeveloped continence apparatus in these children. From a clinical perspective, the thresholds at which fecal incontinence may be attributed to sphincter dysfunction are more difficult to determine. Despite reduced resting pressure, not all children with anorectal malformations experience incontinence. Poor concordance between severity of fecal incontinence and tests of anorectal function have been similarly demonstrated in adult populations [77,78]. Whilst these findings may appear to limit the utility of anorectal manometry, several factors may contribute to this apparent discrepancy. Firstly, given the wide range of resting pressures reported by studies included in this review, and a lack of “normal” values, identifying a precise threshold at which incontinence may be expected is challenging. The need to establish optimal manometric measurements for the diagnosis of anorectal dysfunction has been emphasized for this technique globally [6], and the additional challenges inherent to the pediatric setting are well-recognized [9].
Secondly, continence may be impacted upon by factors extrinsic to the anorectum and thus not evaluated by anorectal manometry. The regulation of defecation and its control (continence) is multifactorial; it is reliant on the interplay between key anatomical structures (principally the colon, anorectum, and pelvic floor musculature) and physiological systems (principally nervous, muscular, hormonal, and cognitive) [79]. As colonic motor activity propels luminal contents distally, progressive rectal distension produces the defecatory urge. If the timing is unsuitable, voluntary contraction of the EAS results in deferral of defecation, and retrograde colonic motor patterns return luminal contents to the sigmoid colon [79]. Alternatively, the expulsive phase sees reversal of the rectoanal pressure gradient through (1) voluntary relaxation of the EAS; (2) reflex relaxation of the IAS and pelvic floor musculature; and (3) reduction of the anorectal angle. Following evacuation, the basal rectoanal pressure gradient is restored and continence is re-established [79].
Given the complexity of interactions required for successful control of defecation, it is perhaps unsurprising that a significant proportion of children with anorectal malformations experience disorders of defecation, despite careful anatomic reconstruction [5,80,81]. Characteristic congenital defects of the anus and rectum may be intuitively associated with impaired continence. In addition, under-developed pelvic musculature, surgical interventions (particularly in the setting of revision procedures), and associated sacro-/spinal anomalies may impact upon the neuromuscular integrity of the continence system [1,82,83].
Prior to defecation, rectal filling elicits the RAIR: reflex relaxation of the IAS facilitates anal mucosal “sampling” and discrimination between solid, liquid, and gaseous luminal content [84,85]. Several studies described a reduced or absent RAIR in children with anorectal malformations [57], including in association with high [versus low] malformations [57] and/or neurospinal dysraphism [14]. Others described better continence outcomes associated with presence of an RAIR, including higher scores on assessments of bowel function [14,31], lower prevalence of fecal incontinence [14,26,29,46,53], and/or higher anal resting pressure [26,46,59].
In this review, the array of approaches used to define and assess the RAIR made it challenging to understand the contribution of the reflex to the continence outcomes. It is likely that, alongside any true differences in prevalence, the variability observed was significantly influenced by the inconsistent criteria used. Despite these limitations, there is some evidence that presence of the RAIR impacts positively upon bowel function in this cohort, and, in concert with other parameters, may aid efforts to prognosticate continence outcomes.
As emphasized by Kumar et al., in the setting of anorectal malformations, RAIR absence is often described in relation to IAS dysfunction (resulting from congenital abnormalities and/or surgical disruption) [57]. However, the higher rectal balloon volumes required to elicit the RAIR in their studied cohort, and reflex absence in children with severe sacral anomalies, led the authors to emphasize the other arm of the reflex arc: the impact of disrupted sensory perception (rather than solely IAS dysfunction) in these patients [57]. Future work should seek to carefully characterize the relationship between presence of an RAIR, key medical characteristics (including malformation type, operative repair approach, and sacrospinal anomalies), bowel function, and response to interventions. This may facilitate understanding of the contribution of the RAIR, and utility in relation to prognostication, within the broader continence apparatus.
Proximal to the anal canal, there is increasing recognition of role of the colon in maintaining fecal continence, particularly through the regulation of rectal filling [86,87,88,89]. Included in this review, Heikenen et al. evaluated both colonic and anorectal motility in children with fecal incontinence following anorectal malformation repair [74]. Whilst a considerable proportion of the children demonstrated reduced resting pressure (60%), propagation of an “excessive” number of colonic motor complexes into the neorectum was demonstrated [74]. Although subject to significant limitations, the findings suggest the refractory fecal incontinence demonstrated by their cohort resulted from multiple factors, including those arising beyond the limits of the anorectum [74]. Our current understanding of colonic motility in this cohort remains poor; however, such studies may be of value in helping to understand the ongoing symptoms in children after repair of anorectal malformations.
While not assessed in this paper, several included studies used other modalities, in addition to anorectal manometry, to help define anorectal abnormalities [41,43,47,49,69]. For example, correlation between findings of manometry and anal endosonography were demonstrated in two studies [49,69]. However, these findings have been questioned, given the limited size and composition of the cohort and the probable technical limitations introduced by the use of a Foley catheter for anorectal manometry [41]. Caldaro et al. similarly utilized manometry and anal endosonography in combination to prognosticate response to treatment [43]. Symptoms in the setting of IAS disruption (identified using anal endosonography) were found to be responsive to biofeedback and laxatives if anal resting pressure (identified using manometry) was greater than 20 mmHg [43]. Utilization of a combination of select investigations is recommended to understand structure and function of the anorectum [6]. The need to establish classification systems encompassing outcomes of multiple tests of anorectal structure and function has been highlighted previously, and would similarly be of benefit to this patient cohort [6].
4.2. Manometry Outcomes and Clinical Correlates
The approach to bowel function assessment was highly variable between studies. Few studies provided symptom definitions, designating groups with constipation or fecal incontinence without specifying the diagnostic criteria. Those that did provide an explanation of their diagnostic terminology demonstrated inconsistencies. For example, constipation was defined as “less than three bowel actions per week”, “less than one bowel action per day”, and “enema required daily to achieve bowel action” [32,62,63]. Similarly, criteria used to report severity often lacked specificity. Studies often assigned grades or terminology (such as minor or infrequent), without specifying the features of each category. This discordant approach to outcome assessment limits meaningful comparison of findings between studies, identification of manometry-symptom correlates, and response to manometry-guided management strategies.
4.3. Practice Variability
Variability has been a common theme throughout this review. We have identified variability in cohort reporting, bowel function assessment, and symptom profiles. Variability in practice has been highlighted, with notable differences in the equipment, protocols, motility criteria, and interpretation used by included studies. Despite the impact of the manometry catheter and assessment protocol on absolute values achieved, notably few studies adequately described the catheter and approach utilized, whilst seven studies provided no description of their approach [20,23,28,33,39,70,71]. This presented a significant challenge when attempting to compare outcomes.
Fundamental to improving the consistency of this work is a coordinated effort to standardize anorectal manometry assessment, its interpretation, and reporting of findings, as has recently been developed for adult anorectal manometry studies [6,7]. Future studies should utilize a recognized manometry protocol and reporting framework; consensus statements have been developed for this purpose [8,9]. Similarly, this must be accompanied by robust reporting of relevant cohort medical characteristics (particularly malformation type, approach to operative repair, and associated anomalies affecting the spine and sacrum); evaluation of bowel function; and assessment of their relationship to manometry findings (Figure 2). Development of minimum standards should be considered, to guide reporting of key cohort characteristics in this population.
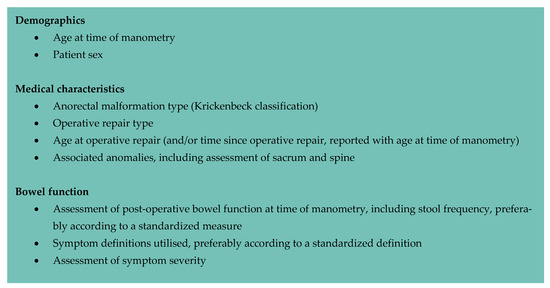
Figure 2.
Suggested key cohort medical characteristics for reporting anorectal manometry studies performed in children with a repaired anorectal malformation.
5. Limitations and Conclusions
This review was limited to children following anorectal malformation repair. Studies including manometry outcomes in this cohort may have been excluded if the findings were not separated by age and/or diagnostic group. Consequently, the included studies may not reflect all anorectal manometry findings in this cohort. Similarly, our review was restricted to studies published in English and may be subject to a language bias.
Whilst altered anorectal function may be intuitively presumed to impact upon continence, regulation of defecation is multifactorial. The prevailing limitation of our current understanding of bowel dysfunction following anorectal malformation repair is the failure to place manometry findings into this wider context. Along with standardization of the approach used to perform anorectal manometry, this should be the focus of future work assessing anorectal function in this cohort. To support this process, the development of reporting guidelines for cohort characteristics and clinical outcomes should be considered, specific to children with anorectal malformations undergoing motility assessment. Whilst high-resolution techniques may provide greater insight into anorectal structure and function, interpreting manometry findings within the context of the broader continence mechanism is essential to enhancing our understanding of the long-term bowel dysfunction experienced by this cohort.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm12072543/s1, Table S1: The Newcastle–Ottawa Scale: study quality assessment [11]; Table S2: Summary of consistently reported anorectal manometry parameters: parameter definitions, resting pressure, squeeze pressure, and rectoanal inhibitory reflex. Units of pressure standardized to mmHg; Table S3: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Checklist [10].
Author Contributions
H.M.E.E.-B. and M.Y.T. performed the literature search, article screening, and data extraction. H.M.E.E.-B. drafted the initial manuscript. M.T., M.S., P.G.D. and J.M.H. critically reviewed and revised the manuscript for intellectual content. S.K.K. conceptualized the study and supervised the execution of the systematic review. All authors have read and agreed to the published version of the manuscript.
Funding
There was no funding for this systematic review. King is generously supported in his role as an Academic Paediatric Surgeon by The Royal Children’s Hospital Foundation. Evans-Barns is supported by an Australian Government Research Training Program (RTP) Scholarship, the Murdoch Children’s Research Institute Professor David Danks Scholarship, and a One in 5000 Foundation Research Award. None of the authors have any financial relationships relevant to this article to disclose.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
AA: anal atresia; aARP: average anal resting pressure; aASP: average anal squeeze pressure; ACL: anal canal length; ACRP: anal canal resting pressure; ARP: abdominoperineal rectoplasty; ArP: anal resting pressure; ARPD: anorectal pressure difference; ARPG: anorectal pressure gradient; ART: anal resting tone; ASARP: anterior sagittal anorectoplasty; ASP: anal squeezing pressure; AUC: area under curve; C: constipated; CM: colonic manometry; EA: esophageal atresia; EAS: external anal sphincter; F: female; FFI: functional fecal incontinence; FI: fecal incontinence; FP: fluid-perfused; GI: gastrointestinal; HD: Hirschsprung disease; HPZ: high pressure zone; HQ: Holschneider’s questionnaire; HRAM: high-resolution anorectal manometry; IAS: internal anal sphincter; KCS: Kelly’s clinical score; KQ: Krickenbeck’s questionnaire; KS: Krickenbeck score; LAARP: laparoscopically assisted anorectoplasty; LAARPT: laparoscopically assisted anorectal pull-through; LAR: laparoscopically assisted pull-through anorectoplasty; LFS: length of internal functional sphincter; LSARP: limited sagittal anorectoplasty; M: male; MARP: mean anal resting pressure; MRI: magnetic resonance imaging; MWS: modified Wingfield score; ND: neurospinal dysraphism; NI: neurological impairment; NRFI: non-retentive fecal incontinence; PQ: Peña’s questionnaire; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses; PROSPERO: International Prospective Register of Systematic Reviews; PSARP: posterior sagittal anorectoplasty; PSP: peak squeeze pressure; QoL: quality of life; RAI: rectoanal inhibition reflex; RAIR: rectoanal inhibitory reflex; RAIRT: rectoanal inhibitory reflex threshold; R-APSA: Rehbein’s mucosa-stripping endorectal pull-through; RAR: rectoanal relaxation reflex; R-ASPA: Rehbein’s mucosa-stripping endorectal pull-through in combination with anterior sagittal perineal anorectoplasty; RFI: retentive fecal incontinence; RP: resting pressure; RQ: Rintala’s questionnaire; RrP: rectal resting pressure; RSR: rectosphincteric reflex; S: solid-state; SILAARP: single-incision laparoscopic-assisted anorectoplasty; SaP: saline-perfused; SD: standard deviation; SP: squeeze pressure; T21: trisomy 21; TAI: transanal irrigation; VACTERL: Vertebral, Anorectal, Cardiac, Tracheo-Esophageal, Renal, Limb anomalies; VCP: voluntary contraction pressure; WP: water-perfused; -: not reported.
Appendix A

Table A1.
Sample search strategy: MEDLINE.
Table A1.
Sample search strategy: MEDLINE.
| 1. anorectal malformations/or anus, imperforate/ |
| 2. ((anorectal or anal or rectal) adj3 (anomal* or atresia* or malformation* or stenos#s)).tw,kf. |
| 3. ((anus adj3 (imperforate* or agenesi* or atresia)) or atresia-ani or atretic-anus).tw,kf. |
| 4. manometry/ |
| 5. manometr*.tw,kf. |
| 6. (1 or 2 or 3) and (4 or 5) |
| 7. exp animals/not human*.sh. |
| 8. 6 not 7 |

Table A2.
Sample search strategy: Embase.
Table A2.
Sample search strategy: Embase.
| 1. anorectal malformation/or anus atresia/ |
| 2. ((anorectal or anal or rectal) adj3 (anomal* or atresia* or malformation* or stenos#s)).tw,kw,dq. |
| 3. ((anus adj3 (imperforate* or agenesi* or atresia)) or atresia-ani or atretic-anus).tw,kw,dq. |
| 4. manometry/ |
| 5. manometr*.tw,kw,dq. |
| 6. (1 or 2 or 3) and (4 or 5) |
| 7. exp animal/not human*.sh. |
| 8. 6 not 7 |
References
- Levitt, M.A.; Peña, A. Anorectal malformations. Orphanet J. Rare Dis. 2007, 2, 33. [Google Scholar] [CrossRef] [PubMed]
- Peña, A.; Bischoff, A. History of the Treatment of Anorectal Malformations; Springer International Publishing: Berlin/Heidelberg, Germany, 2015; pp. 1–16. [Google Scholar] [CrossRef]
- Peña, A.; Devries, P.A. Posterior sagittal anorectoplasty: Important technical considerations and new applications. J. Pediatr. Surg. 1982, 17, 796–811. [Google Scholar] [CrossRef] [PubMed]
- Kyrklund, K.; Pakarinen, M.P.; Rintala, R.J. Long-term bowel function, quality of life and sexual function in patients with anorectal malformations treated during the PSARP era. Semin. Pediatr. Surg. 2017, 26, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Rigueros Springford, L.; Connor, M.J.; Jones, K.; Kapetanakis, V.V.; Giuliani, S. Prevalence of Active Long-term Problems in Patients With Anorectal Malformations: A Systematic Review. Dis. Colon. Rectum. 2016, 59, 570–580. [Google Scholar] [CrossRef] [PubMed]
- Carrington, E.V.; Scott, S.M.; Bharucha, A.; Mion, F.; Remes-Troche, J.M.; Malcolm, A.; Heinrich, H.; Fox, M.; Rao, S.S. Expert consensus document: Advances in the evaluation of anorectal function. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 309–323. [Google Scholar] [CrossRef] [PubMed]
- Carrington, E.V.; Heinrich, H.; Knowles, C.H.; Rao, S.S.; Fox, M.; Scott, S.M. Methods of anorectal manometry vary widely in clinical practice: Results from an international survey. Neurogastroenterol. Motil. 2017, 29, e13016. [Google Scholar] [CrossRef] [PubMed]
- Carrington, E.V.; Heinrich, H.; Knowles, C.H.; Fox, M.; Rao, S.; Altomare, D.F.; Bharucha, A.E.; Burgell, R.; Chey, W.D.; Chiarioni, G.; et al. The international anorectal physiology working group (IAPWG) recommendations: Standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterol. Motil. 2020, 32, e13679. [Google Scholar] [CrossRef]
- Athanasakos, E.; Cleeve, S.; Thapar, N.; Lindley, K.; Perring, S.; Cronin, H.; Borrelli, O.; Mutalib, M. Anorectal manometry in children with defecation disorders BSPGHAN Motility Working Group consensus statement. Neurogastroenterol. Motil. 2020, 32, e13797. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Wells, G.A.; Tugwell, P.; O’Connell, D.; Welch, V.; Peterson, J.; Shea, B.; Losos, M. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm (accessed on 19 November 2020).
- Holschneider, A.; Hutson, J.; Peña, A.; Beket, E.; Chatterjee, S.; Coran, A.; Davies, M.; Georgeson, K.; Grosfeld, J.; Gupta, D.; et al. Preliminary report on the International Conference for the Development of Standards for the Treatment of Anorectal Malformations. J. Pediatr. Surg. 2005, 40, 1521–1526. [Google Scholar] [CrossRef]
- Stephens, F.D.; Smith, D.E.; Paul, N.W. Anorectal malformations in children: Update 1988. March Dimes Birth Defects Found. Birth Defects Orig. Artic. Ser. 1988, 24, 1–604. [Google Scholar]
- Arnoldi, R.; Macchini, F.; Gentilino, V.; Farris, G.; Morandi, A.; Brisighelli, G.; Leva, E. Anorectal malformations with good prognosis: Variables affecting the functional outcome. J. Pediatr. Surg. 2014, 49, 1232–1236. [Google Scholar] [CrossRef] [PubMed]
- Iwai, N.; Yanagihara, J.; Tokiwa, K.; Deguchi, E.; Takahashi, T. Voluntary anal continence after surgery for anorectal malformations. J. Pediatr. Surg. 1988, 23, 393–397. [Google Scholar] [CrossRef]
- Penninckx, F.; Kerremans, R. Internal sphincter-saving in imperforate anus with or without fistula. A manometric study. Int. J. Color. Dis. 1986, 1, 28–32. [Google Scholar] [CrossRef]
- Rintala, R.; Lindahl, H.; Sariola, H.; Rapola, J.; Louhimo, I. The rectourogenital connection in anorectal malformations is an ectopic anal canal. J. Pediatr. Surg. 1990, 25, 665–668. [Google Scholar] [CrossRef] [PubMed]
- Ruttenstock, E.M.; Zani, A.; Huber-Zeyringer, A.; Hollwarth, M.E. Pre- and postoperative rectal manometric assessment of patients with anorectal malformations: Should we preserve the fistula? Dis. Colon. Rectum. 2013, 56, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Schuster, T.; Joppich, I.; Schneider, K.; Jobst, G. A computerised vector manometry study of the so-called ectopic anus. Pediatr. Surg. Int. 2000, 16, 8–14. [Google Scholar] [CrossRef]
- Huang, Y.; Shen, C.; Zheng, S.; Xiao, X. A follow-up study on postoperative function after a modified semi-posterior sagittal one-stage anorectoplasty for female imperforate anus with a rectovesibula fistula. Int. J. Clin. Exp. Med. 2017, 10, 913–920. [Google Scholar]
- Okada, A.; Tamada, H.; Tsuji, H.; Azuma, T.; Yagi, M.; Kubota, A.; Kamata, S. Anterior sagittal anorectoplasty as a redo operation for imperforate anus. J. Pediatr. Surg. 1993, 28, 933–938. [Google Scholar] [CrossRef]
- Chung, P.H.Y.; Wong, C.W.Y.; Wong, K.K.Y.; Tam, P.K.H. Assessing the long term manometric outcomes in patients with previous laparoscopic anorectoplasty (LARP) and posterior sagittal anorectoplasty (PSARP). J. Pediatr. Surg. 2018, 53, 1933–1936. [Google Scholar] [CrossRef]
- Becmeur, F.; Hofmann-Zango, I.; Jouin, H.; Moog, R.; Kauffmann, I.; Sauvage, P. Three-flap anoplasty for imperforate anus: Results for primary procedure or for redoes. Eur. J. Pediatr. Surg. 2001, 11, 311–314. [Google Scholar] [CrossRef] [PubMed]
- Cahill, J.L.; Christie, D.L. Results after posterior sagittal anorectoplasty: A new approach to high imperforate anus. Am. J. Surg. 1985, 149, 629–631. [Google Scholar] [CrossRef] [PubMed]
- El-Debeiky, M.S.; Safan, H.A.; Shafei, I.A.; Kader, H.A.; Hay, S.A. Long-term functional evaluation of fecal continence after laparoscopic-assisted pull-through for high anorectal malformations. J. Laparoendosc. Adv. Surg. Tech. A 2009, 19 (Suppl. 1), S51–S54. [Google Scholar] [CrossRef] [PubMed]
- Husberg, B.; Lindahl, H.; Rintala, R.; Frenckner, B. High and intermediate imperforate anus: Results after surgical correction with special respect to internal sphincter function. J. Pediatr. Surg. 1992, 27, 185–188; discussion 188–189. [Google Scholar] [CrossRef] [PubMed]
- Kimura, O.; Iwai, N.; Sasaki, Y.; Tsuda, T.; Deguchi, E.; Ono, S.; Furukawa, T. Laparoscopic versus open abdominoperineal rectoplasty for infants with high-type anorectal malformation. J. Pediatr. Surg. 2010, 45, 2390–2393. [Google Scholar] [CrossRef] [PubMed]
- Kudou, S.; Iwanaka, T.; Kawashima, H.; Uchida, H.; Nishi, A.; Yotsumoto, K.; Kaneko, M. Midterm follow-up study of high-type imperforate anus after laparoscopically assisted anorectoplasty. J. Pediatr. Surg. 2005, 40, 1923–1926. [Google Scholar] [CrossRef]
- Langemeijer, R.A.T.M.; Molenaar, J.C. Continence after posterior sagittal anorectoplasty. J. Pediatr. Surg. 1991, 26, 587–590. [Google Scholar] [CrossRef]
- Lin, C.-L.; Chen, C.-C. The rectoanal relaxation reflex and continence in repaired anorectal malformations with and without an internal sphincter-saving procedure. J. Pediatr. Surg. 1996, 31, 630–633. [Google Scholar] [CrossRef]
- Lin, C.L.; Wong, K.K.; Lan, L.C.; Chen, C.C.; Tam, P.K. Earlier appearance and higher incidence of the rectoanal relaxation reflex in patients with imperforate anus repaired with laparoscopically assisted anorectoplasty. Surg. Endosc. 2003, 17, 1646–1649. [Google Scholar] [CrossRef]
- Liu, G.; Yuan, J.; Geng, J.; Wang, C.; Li, T. The treatment of high and intermediate anorectal malformations: One stage or three procedures? J. Pediatr. Surg. 2004, 39, 1466–1471. [Google Scholar] [CrossRef]
- Niedzielski, J. Results of surgical correction of anorectal malformations in children—16-years experience. [Polish, English]. Chir. Pol. 2008, 10, 16–29. [Google Scholar]
- Ren, X.; Xu, H.; Jiang, Q.; Diao, M.; Li, X.; Li, L. Single-incision laparoscopic-assisted anorectoplasty for treating children with intermediate-type anorectal malformations and rectobulbar fistula: A comparative study. Pediatr. Surg. Int. 2019, 35, 1255–1263. [Google Scholar] [CrossRef] [PubMed]
- Rintala, R. Postoperative internal sphincter function in anorectal malformations—A manometric study. Pediatr. Surg. Int. 1990, 5, 127–130. [Google Scholar] [CrossRef]
- Rintala, R.; Lindahl, H. Internal sphincter-saving posterior sagittal anorectoplasty for high and intermediate anorectal malformations: Technical considerations. Pediatr. Surg. Int. 1995, 10, 345–349. [Google Scholar] [CrossRef]
- Sonnino, R.E.; Reinberg, O.; Bensoussan, A.L.; Laberge, J.M.; Blanchard, H. Gracilis muscle transposition for anal incontinence in children: Long-term follow-up. J. Pediatr. Surg. 1991, 26, 1219–1223. [Google Scholar] [CrossRef] [PubMed]
- Tong, Q.S.; Tang, S.T.; Pu, J.R.; Mao, Y.Z.; Wang, Y.; Li, S.W.; Cao, Q.Q.; Ruan, Q.L. Laparoscopically assisted anorectal pull-through for high imperforate anus in infants: Intermediate results. J. Pediatr. Surg. 2011, 46, 1578–1586. [Google Scholar] [CrossRef]
- Yang, J.; Zhang, W.; Feng, J.; Guo, X.; Wang, G.; Weng, Y.; Sun, X.; Yu, D. Comparison of clinical outcomes and anorectal manometry in patients with congenital anorectal malformations treated with posterior sagittal anorectoplasty and laparoscopically assisted anorectal pull through. J. Pediatr. Surg. 2009, 44, 2380–2383. [Google Scholar] [CrossRef]
- Emblem, R.; Diseth, T.; Morkrid, L.; Stien, R.; Bjordal, R. Anal endosonography and physiology in adolescents with corrected low anorectal anomalies. J. Pediatr. Surg. 1994, 29, 447–451. [Google Scholar] [CrossRef]
- Fukata, R.; Iwai, N.; Yanagihara, J.; Iwata, G.; Kubota, Y. A comparison of anal endosonography with electromyography and manometry in high and intermediate anorectal anomalies. J. Pediatr. Surg. 1997, 32, 839–842. [Google Scholar] [CrossRef]
- Schuster, T.; Lagler, F.; Pfluger, T.; Dietz, H.G.; Joppich, I. A computerized vector manometry and MRI study in children following posterior sagittal anorectoplasty. Pediatr. Surg. Int. 2001, 17, 48–53. [Google Scholar] [CrossRef]
- Caldaro, T.; Romeo, E.; De Angelis, P.; Gambitta, R.A.; Rea, F.; Torroni, F.; Foschia, F.; Federici Di Abriola, G.; Dall’Oglio, L. Three-dimensional endoanal ultrasound and anorectal manometry in children with anorectal malformations: New discoveries. J. Pediatr. Surg. 2012, 47, 956–963. [Google Scholar] [CrossRef] [PubMed]
- Doolin, E.J.; Black, C.T.; Donaldson, J.S.; Schwartz, D.; Raffensperger, J.G. Rectal manometry, computed tomography, and functional results of anal atresia surgery. J. Pediatr. Surg. 1993, 28, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Emblem, R.; Diseth, T.; Morkrid, L. Anorectal anomalies: Anorectal manometric function and anal endosonography in relation to functional outcome. Pediatr. Surg. Int. 1997, 12, 516–519. [Google Scholar] [CrossRef] [PubMed]
- Hedlund, H.; Pena, A.; Rodriguez, G.; Maza, J. Long-term anorectal function in imperforate anus treated by a posterior sagittal anorectoplasty: Manometric investigation. J. Pediatr. Surg. 1992, 27, 906–909. [Google Scholar] [CrossRef] [PubMed]
- Hettiarachchi, M.; Garcea, G.; de Souza, N.M.; Williams, A.D.; Clayden, G.S.; Ward, H.C. Evaluation of dysfunction following reconstruction of an anorectal anomaly. Pediatr. Surg. Int. 2002, 18, 405–409. [Google Scholar]
- Ishihara, M.; Okabe, I.; Morita, K. Assessment of the percentages of maximum static pressure in the anal canal for postoperative continence in patients with imperforate anus. Jpn. J. Surg. 1987, 17, 230–235. [Google Scholar] [CrossRef]
- Keshtgar, A.S.; Athanasakos, E.; Clayden, G.S.; Ward, H.C. Evaluation of outcome of anorectal anomaly in childhood: The role of anorectal manometry and endosonography. Pediatr. Surg. Int. 2008, 24, 885–892. [Google Scholar] [CrossRef]
- Martins, J.L.; Pinus, J. Clinical and manometric postoperative evaluation of posterior sagital anorectoplasty (PSARP) in patients with upper and intermediate anorectal malformations. Sao Paulo Med. J. 1996, 114, 1303–1308. [Google Scholar] [CrossRef]
- Senel, E.; Demirbag, S.; Tiryaki, T.; Erdogan, D.; Cetinkursun, S.; Cakmak, O. Postoperative anorectal manometric evaluation of patients with anorectal malformation. Pediatr. Int. 2007, 49, 210–214. [Google Scholar] [CrossRef]
- Tang, P.M.Y.; Leung, M.W.Y.; Hung, J.W.S.; Chung, K.L.Y.; Liu, C.S.W.; Chao, N.S.Y.; Liu, K.K.W. Application of three dimensional high resolution anorectal manometry to demonstrate anal sphincter pressure asymmetry in children after anorectal surgery: A pilot study. Hong Kong J. Paediatr. 2017, 22, 204–208. [Google Scholar]
- Vital Junior, P.F.; Martins, J.L.; Peterlini, F.L. Posterior sagittal anorectoplasty in anorectal anomalies: Clinical, manometric and profilometric evaluation. Sao Paulo Med. J. 2007, 125, 163–169. [Google Scholar] [CrossRef]
- Wang, Z.; Hu, L.; Jin, X.; Li, X.; Xu, L. Evaluation of postoperative anal functions using endoanal ultrasonography and anorectal manometry in children with congenital anorectal malformations. J. Pediatr. Surg. 2016, 51, 416–420. [Google Scholar] [CrossRef] [PubMed]
- Mert, M.; Sayan, A.; Köylüoğlu, G. Comparing the fecal continence scores of patients with anorectal malformation with anorectal manometric findings. Pediatr. Surg. Int. 2021, 37, 1013–1019. [Google Scholar] [CrossRef] [PubMed]
- Bhat, N.A.; Grover, V.P.; Bhatnagar, V. Pre-operative manometry of the blind rectal pouch to predict post-operative potential for continence in anorectal malformation. Trop. Gastroenterol. 2008, 29, 51–54. [Google Scholar] [PubMed]
- Kumar, S.; Al Ramadan, S.; Gupta, V.; Helmy, S.; Debnath, P.; Alkholy, A. Use of anorectal manometry for evaluation of postoperative results of patients with anorectal malformation: A study from Kuwait. J. Pediatr. Surg. 2010, 45, 1843–1848. [Google Scholar] [CrossRef] [PubMed]
- Rintala, R.; Lindahl, H.; Marttinen, E.; Sariola, H. Constipation is a major functional complication after internal sphincter-saving posterior sagittal anorectoplasty for high and intermediate anorectal malformations. J. Pediatr. Surg. 1993, 28, 1054–1058. [Google Scholar] [CrossRef]
- Rintala, R.J.; Lindahl, H. Is normal bowel function possible after repair of intermediate and high anorectal malformations? J. Pediatr. Surg. 1995, 30, 491–494. [Google Scholar] [CrossRef]
- Rintala, R.J.; Lindahl, H. Secondary posterior sagittal anorectoplasty for anorectal malformations. Long-term follow-up extending beyond childhood. Pediatr. Surg. Int. 1995, 10, 414–417. [Google Scholar] [CrossRef]
- Burjonrappa, S.; Youssef, S.; Lapierre, S.; Bensoussan, A.; Bouchard, S. Megarectum after surgery for anorectal malformations. J. Pediatr. Surg. 2010, 45, 762–768. [Google Scholar] [CrossRef]
- Nagashima, M.; Iwai, N.; Yanagihara, J.; Shimotake, T. Motility and sensation of the rectosigmoid and the rectum in patients with anorectal malformations. J. Pediatr. Surg. 1992, 27, 1273–1277. [Google Scholar] [CrossRef]
- Sangkhathat, S.; Patrapinyokul, S.; Osatakul, N. Crucial role of rectoanal inhibitory reflex in emptying function after anoplasty in infants with anorectal malformations. Asian J. 2004, 27, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Banasiuk, M.; Dziekiewicz, M.; Dembiński, Ł.; Piotrowski, D.; Kamiński, A.; Banaszkiewicz, A. Three-dimensional high-resolution anorectal manometry in children after surgery for anorectal disorders. In European Review for Medical and Pharmacological Sciences; Verduci: Rome, Italy, 2021; Volume 25, pp. 2981–2993. [Google Scholar]
- Iwai, N.; Iwata, G.; Kimura, O.; Yanagihara, J. Is a new biofeedback therapy effective for fecal incontinence in patients who have anorectal malformations? J. Pediatr. Surg. 1997, 32, 1626–1629. [Google Scholar] [CrossRef] [PubMed]
- Iwai, N.; Kume, Y.; Kimura, O.; Ono, S.; Aoi, S.; Tsuda, T. Effects of herbal medicine Dai-Kenchu-to on anorectal function in children with severe constipation. Eur. J. Pediatr. Surg. 2007, 17, 115–118. [Google Scholar] [CrossRef] [PubMed]
- Caruso, A.M.; Catalano, P.; Li Voti, G.; Salerno, S.; Casuccio, A.; Di Pace, M.R.; Cimador, M. Prognostic evaluation of biofeedback response in patients treated for anorectal malformation. J. Pediatr. Surg. 2015, 50, 1648–1652. [Google Scholar] [CrossRef] [PubMed]
- Iwai, N.; Nagashima, M.; Shimotake, T.; Iwata, G. Biofeedback therapy for fecal incontinence after surgery for anorectal malformations: Preliminary results. J. Pediatr. Surg. 1993, 28, 863–866. [Google Scholar] [CrossRef]
- Keshtgar, A.S.; Ward, H.C.; Richards, C.; Clayden, G.S. Outcome of excision of megarectum in children with anorectal malformation. J. Pediatr. Surg. 2007, 42, 227–233. [Google Scholar] [CrossRef]
- Leung, M.W.; Wong, B.P.; Leung, A.K.; Cho, J.S.; Leung, E.T.; Chao, N.S.; Chung, K.W.; Kwok, W.K.; Liu, K.K. Electrical stimulation and biofeedback exercise of pelvic floor muscle for children with faecal incontinence after surgery for anorectal malformation. Pediatr. Surg. Int. 2006, 22, 975–978. [Google Scholar] [CrossRef]
- Ninan, G.K.; Puri, P. Levatorplasty using a posterior sagittal approach in secondary faecal incontinence. Pediatr. Surg. Int. 1994, 9, 17–20. [Google Scholar] [CrossRef]
- Caruso, A.M.; Milazzo, M.P.M.; Bommarito, D.; Girgenti, V.; Amato, G.; Paviglianiti, G.; Casuccio, A.; Catalano, P.; Cimador, M.; Di Pace, M.R. Advanced Management Protocol of Transanal Irrigation in Order to Improve the Outcome of Pediatric Patients with Fecal Incontinence. Children 2021, 8, 1174. [Google Scholar] [CrossRef]
- Chen, C.C.; Lin, C.L.; Lu, W.T.; Hsu, W.M.; Chen, J.C. Anorectal function and endopelvic dissection in patients with repaired imperforate anus. Pediatr. Surg. Int. 1998, 13, 133–137. [Google Scholar] [CrossRef]
- Heikenen, J.B.; Werlin, S.L.; Di Lorenzo, C.; Hyman, P.E.; Cocjin, J.; Flores, A.F.; Reddy, S.N. Colonic motility in children with repaired imperforate anus. Dig. Dis. Sci. 1999, 44, 1288–1292. [Google Scholar] [CrossRef] [PubMed]
- Mollard, P.; Meunier, P.; Mouriquand, P.; Bonnet, J.P. High and intermediate imperforate anus: Functional results and postoperative manometric assessment. Eur. J. Pediatr. Surg. 1991, 1, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Ray, A.K.; Singhania, A.K.; Mukherjee, S. Post PSARP anorectal manometry—Experience of 115 cases of imperforate anus. J. Indian Med. Assoc. 2004, 102, 253–255. [Google Scholar] [PubMed]
- Heitmann, P.T.; Rabbitt, P.; Schloithe, A.C.; Wattchow, D.A.; Scott, S.M.; Dinning, P.G. The relationships between the results of contemporary tests of anorectal structure and sensorimotor function and the severity of fecal incontinence. Neurogastroenterol. Motil. 2020, 32, e13946. [Google Scholar] [CrossRef] [PubMed]
- Heitmann, P.T.; Rabbitt, P.; Schloithe, A.; Patton, V.; Skuza, P.P.; Wattchow, D.A.; Dinning, P.G. Relationships between the results of anorectal investigations and symptom severity in patients with faecal incontinence. Int. J. Color. Dis. 2019, 34, 1445–1454. [Google Scholar] [CrossRef] [PubMed]
- Heitmann, P.T.; Vollebregt, P.F.; Knowles, C.H.; Lunniss, P.J.; Dinning, P.G.; Scott, S.M. Understanding the physiology of human defaecation and disorders of continence and evacuation. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 751–769. [Google Scholar] [CrossRef] [PubMed]
- Levitt, M.A.; Kant, A.; Peña, A. The morbidity of constipation in patients with anorectal malformations. J. Pediatr. Surg. 2010, 45, 1228–1233. [Google Scholar] [CrossRef]
- Lane, V.A.; Calisto, J.; Deblaauw, I.; Calkins, C.M.; Samuk, I.; Avansino, J.R. Assessing the previously repaired patient with an anorectal malformation who is not doing well. Semin. Pediatr. Surg. 2020, 29, 150995. [Google Scholar] [CrossRef]
- Bischoff, A.; Bealer, J.; Duncan Peña, A. Error traps and culture of safety in anorectal malformations. Semin. Pediatr. Surg. 2019, 28, 131–134. [Google Scholar] [CrossRef]
- King, S.K.; Krois, W.; Lacher, M.; Saadai, P.; Armon, Y.; Midrio, P. Optimal management of the newborn with an anorectal malformation and evaluation of their continence potential. Semin. Pediatr. Surg. 2020, 29, 150996. [Google Scholar] [CrossRef]
- Bajwa, A.; Fellow, R.; Emmanuel, A. The physiology of continence and evacuation. Best Pract. Res. Clin. Gastroenterol. 2009, 23, 477–485. [Google Scholar] [CrossRef]
- Scott, S.M.; Gladman, M.A. Manometric, sensorimotor, and neurophysiologic evaluation of anorectal function. Gastroenterol. Clin. North Am. 2008, 37, 511–538. [Google Scholar] [CrossRef]
- Dinning, P.G.; Wiklendt, L.; Maslen, L.; Gibbins, I.; Patton, V.; Arkwright, J.W.; Lubowski, D.Z.; O’Grady, G.; Bampton, P.A.; Brookes, S.J.; et al. Quantification of in vivo colonic motor patterns in healthy humans before and after a meal revealed by high-resolution fiber-optic manometry. Neurogastroenterol. Motil. 2014, 26, 1443–1457. [Google Scholar] [CrossRef]
- Rao, S.S.; Welcher, K. Periodic rectal motor activity: The intrinsic colonic gatekeeper? Am. J. Gastroenterol. 1996, 91, 890–897. [Google Scholar]
- Patton, V.; Wiklendt, L.; Arkwright, J.W.; Lubowski, D.Z.; Dinning, P.G. The effect of sacral nerve stimulation on distal colonic motility in patients with faecal incontinence. Br. J. Surg. 2013, 100, 959–968. [Google Scholar] [CrossRef] [PubMed]
- Lin, A.Y.; Du, P.; Dinning, P.G.; Arkwright, J.W.; Kamp, J.P.; Cheng, L.K.; Bissett, I.P.; O’Grady, G. High-resolution anatomic correlation of cyclic motor patterns in the human colon: Evidence of a rectosigmoid brake. Am. J. Physiol. Gastrointest. Liver Physiol. 2017, 312, G508–G515. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).