Abstract
Traumatic brain injury (TBI) may affect the lives of the individuals concerned and their relatives negatively in many dimensions. Health-related quality of life (HRQoL) is a comprehensive and complex concept that can assess one’s satisfaction with a broad range of areas of life and health. The Quality of Life after Traumatic Brain Injury (QOLIBRI) questionnaire is a TBI-specific measure for HRQoL which is used in research and health services worldwide. When evaluating self-reported HRQoL after TBI, reference values from a general population are helpful to perform clinically relevant evaluations and decisions about the condition of an affected person by comparing the patient scores with reference values. Despite the widespread use of the QOLIBRI, reference values have until now only been available for the Netherlands and the United Kingdom. The aim of this study was to validate the QOLIBRI for the general population in Italy and to provide reference values. An adapted form of the QOLIBRI was administered to 3298 Italians from a healthy general population using an online survey. Their scores were compared with those of 298 individuals post-TBI recruited within the international longitudinal observational cohort CENTER-TBI study in Italian hospitals, who completed the original questionnaire. The psychometric characteristics and the measurement invariance of the QOLIBRI were assessed. A regression analysis was performed to identify predictors relevant for HRQoL in the general population. Reference values were provided using percentiles. Measurement invariance analysis showed that the QOLIBRI captures the same HRQoL constructs in an Italian general population and Italian TBI sample from the observational Center-TBI study. Higher age, higher education and the absence of a chronic health condition were associated with higher QOLIBRI scores, suggesting better HRQoL. Reference values were provided for a general Italian population adjusted for age, sex, education and presence of chronic health conditions. We recommend using these for a better interpretation of the QOLIBRI score in clinical practice and research in Italy.
1. Introduction
Traumatic brain injury (TBI) is an important cause of burden of disease worldwide, as more than 50 million people acquire it every year [1]. In a study published in 2018, Dewan et al. [2] estimated that approximately 69 million people worldwide experience TBI each year. In Italy, the incidence of TBI varies from 212.4 [3] to 848 [4,5] cases per 100,000, depending on the study, placing it among the countries with the highest TBI rates in Europe.
TBI negatively affects the lives of individuals after TBI and their relatives [6,7] by limiting their everyday lives, causing physical [8], cognitive [9] and psychological problems [10], and having negative effects on their emotions [11] and social lives [12,13]. Because of the long-term outcomes, which are similar to those caused by a chronic health condition, TBI has been equated with chronic diseases [14]. In recent decades, the description and treatment of chronic diseases has seen a shift from a biomedical to a biopsychosocial approach to disease and health. Consequently, health is seen as a multidimensional construct that includes physical and psychosocial aspects [15]. In their systematic review, Polinder et al. [16] point out that TBI has a relevant impact on the health-related quality of life (HRQoL) of the individuals concerned.
HRQoL is a comprehensive and complex construct which includes a broad range of areas of life and health. It covers self-reported outcomes on health status and well-being, and can be used to determine the effectiveness of a treatment [16,17]. Sherer and his colleagues [18] postulated that physical function, physical symptoms, cognition, negative and positive emotions, sense of self, and social participation provide a differentiated foundation for understanding the HRQoL of individuals after TBI. HRQoL can be assessed using disease-specific or generic instruments. Generic instruments can be used in the assessment of HRQoL after TBI [19], especially when comparisons are to be made with other diseases [20]. However, these instruments are described as being less sensitive to specific health conditions, which is why the use of disease-specific instruments is recommended [21,22]. Specific instruments are generally more sensitive and more responsive [23] to the problems of a particular disease area and can capture HRQoL more precisely [24]. For example, Harfmann et al. [19] have compared specific and generic instruments in patients after TBI and shown that the TBI-specific measures offer a more detailed assessment of symptoms relevant to TBI than generic ones.
The instrument measuring Quality of Life after Traumatic Brain Injury (QOLIBRI) is the first disease-specific questionnaire that captures HRQoL after TBI [25,26]. It covers all aspects suggested by Sherer et al. [18] within 37 items forming six subscales (cognition, self, autonomy and daily life, social, emotions, physical). The QOLIBRI helps to identify self-perceived deficits that should be further investigated and, if possible, improved. This instrument was developed in 2010 and was validated for the Italian language in 2014 [27], showing good psychometric characteristics.
The QOLIBRI instrument is applied in various settings in the area of TBI, from international research studies to clinical use [28,29,30] and rehabilitation [31]. Until now the QOLIBRI has been translated and validated in more than 26 languages and is widely used internationally for individuals after TBI [31,32,33,34]. However, to better understand the clinical impact of TBI on the HRQoL of patients, reference values for individuals from comparable general populations are required. Reference values are important, e.g., in order to evaluate the HRQoL of an individual after TBI in relation to a comparable general population, so as to capture the HRQoL domains showing deficits. To date, no reference values exist for the Italian version of the QOLIBRI.
Since the QOLIBRI is a TBI-specific measure, it should be adapted for use in the general population. To ensure comparability of the QOLIBRI scores between individuals after TBI and the general population, evidence of measurement invariance (MI) is crucial. MI in this sense means that any observable variation in (adapted) QOLIBRI responses between TBI and the general population can be attributed to real differences in HRQoL. The aim of this study was therefore to validate the QOLIBRI questionnaire for a sample from the Italian general population in order to compile reference values and to compare these with the QOLIBRI scores of individuals after TBI.
2. Methods
2.1. Study Design
This study includes data from two different sources. Data for the general population sample from Italy are derived from a web-based, self-reported, cross-sectional study. The data for individuals after TBI stem from the multicenter, prospective, longitudinal, observational Collaborative European Neuro Trauma Effectiveness Research in Traumatic Brain Injury study (CENTER-TBI; clinicaltrials.gov NCT02210221). For details on enrollment of participants and recruitment, see Steyerberg et al. [35].
2.2. Ethical Approvals
2.2.1. General Population Sample
The study on general population was a part of the CENTER-TBI project. Ethical approval was obtained from the Leids Universitair Centrum—Commissie Medische Ethiek (approval P14.222/NV/nv, 3 December 2014).
2.2.2. TBI Sample
The CENTER-TBI study (EC grant 602150) has been conducted in accordance with all relevant laws of the EU if directly applicable or of direct effect and all relevant laws of the country where the recruiting sites were located, including, but not limited to, the relevant privacy and data protection laws and regulations (the “Privacy Law”), the relevant laws and regulations on the use of human materials, and all relevant guidance relating to clinical studies from time to time in force, including, but not limited to, the ICH Harmonized Tripartite Guideline for Good Clinical Practice (CPMP/ICH/135/95) (“ICH GCP”) and the World Medical Association Declaration of Helsinki entitled “Ethical Principles for Medical Research Involving Human Subjects”. Informed consent was obtained for all patients recruited in the Core Dataset of CENTER-TBI and documented in the e-CRF. Ethical approval was obtained for each recruiting site. The list of sites, Ethical Committees, approval numbers and approval dates can be found on the project’s website https://www.center-tbi.eu/project/ethical-approval (accessed on 15 July 2022).
2.3. Instruments
2.3.1. Quality of Life after Traumatic Brain Injury (QOLIBRI)
The QOLIBRI is the first instrument specifically developed for individuals after TBI to assess their disease-specific HRQoL. It comprises 37 items associated with four scales (Cognition, Self, Daily Life and Autonomy, and Social Relationships) with items measuring satisfaction with various aspects of HRQoL (part A) and two scales (Emotions and Physical Problems) measuring issues that individuals after TBI feel bothered by (part B). Responses to the Part A items are coded on a 5-point Likert scale with 1 corresponding to not at all satisfied and 5 to very satisfied. Responses to the items in Part B are reversely scored to correspond with the items of the Part A. Here, 1 indicates very (bothered) and 5 means not at all bothered. Like other instruments measuring quality of life, when scoring the QOLIBRI scale, means are converted to a 0 to 100 rating scale by subtracting 1 from the mean score and then multiplying it by 25, with a value of 0 indicating the worst possible HRQoL and a value of 100 the best possible HRQoL.
For the general population sample, three items of the original QOLIBRI had to be reworded to remove the reference to a TBI. The fifth item from the scale “Self”, “How satisfied are you with what you have achieved since your brain injury?”, was changed to “How satisfied are you with what you have achieved recently?”. The second item from the scale “Physical”, “How bothered are you by effects of any other injuries you sustained at the same time as your brain injury?”, was changed to “How bothered are you by the effects of any injuries you sustained?”. The last item, also assigned to the scale “Physical”, “Overall, how bothered are you by the effects of your brain injury?”, was changed to “Overall, how bothered are you by the effects of any health problems?”.
2.3.2. Sociodemographic and Health Status Data
The sociodemographic and health status data for both samples contained information on sex, age and the highest level of education achieved. In addition, the presence of chronic health conditions (CHC) was recorded for the general population sample, where multiple answers were possible. The question was: “Do you have any of the following chronic health complaints?” Subjects were asked to tick a box for the response options (multiple answers were possible) listed in Table A1.
Additionally, the Glasgow Coma Scale (GCS) was used in the TBI sample to rate TBI severity [36]. A score of 13 to 15 points indicates mild TBI, 9 to 12 moderate TBI, and 3 to 8 severe TBI. The Glasgow Outcome Scale Extended (GOSE), ranging from 1 (death) to 8 (upper good recovery), was used as a measure of recovery status after TBI [37].
2.4. Participants
2.4.1. General Population Sample
Participants from the general population sample were recruited by a market research agency (Dynata, Shelton, CT, USA) between 29 June and 31 July 2017. To obtain a representative sample, participants were invited until the required quotas for age, sex and level of education had been achieved. Due to the self-reported nature of the data collection, the sex of participants was collected as gender (male, female). Since gender/sex corresponds to the biological categories of males and females, the word “sex” will be used for consistency and to avoid any confusion. Comparison of the quotas with demographic information obtained from the Organization for Economic Cooperation and Development databank (OECD) [38] and Eurostat database [39] revealed a widely comparable distribution of the groups. Within this online survey based on self-report, the data were collected in Italy, the Netherlands, and the UK. The reference values of the QOLIBRI for the Netherlands and the UK have already been published [40].
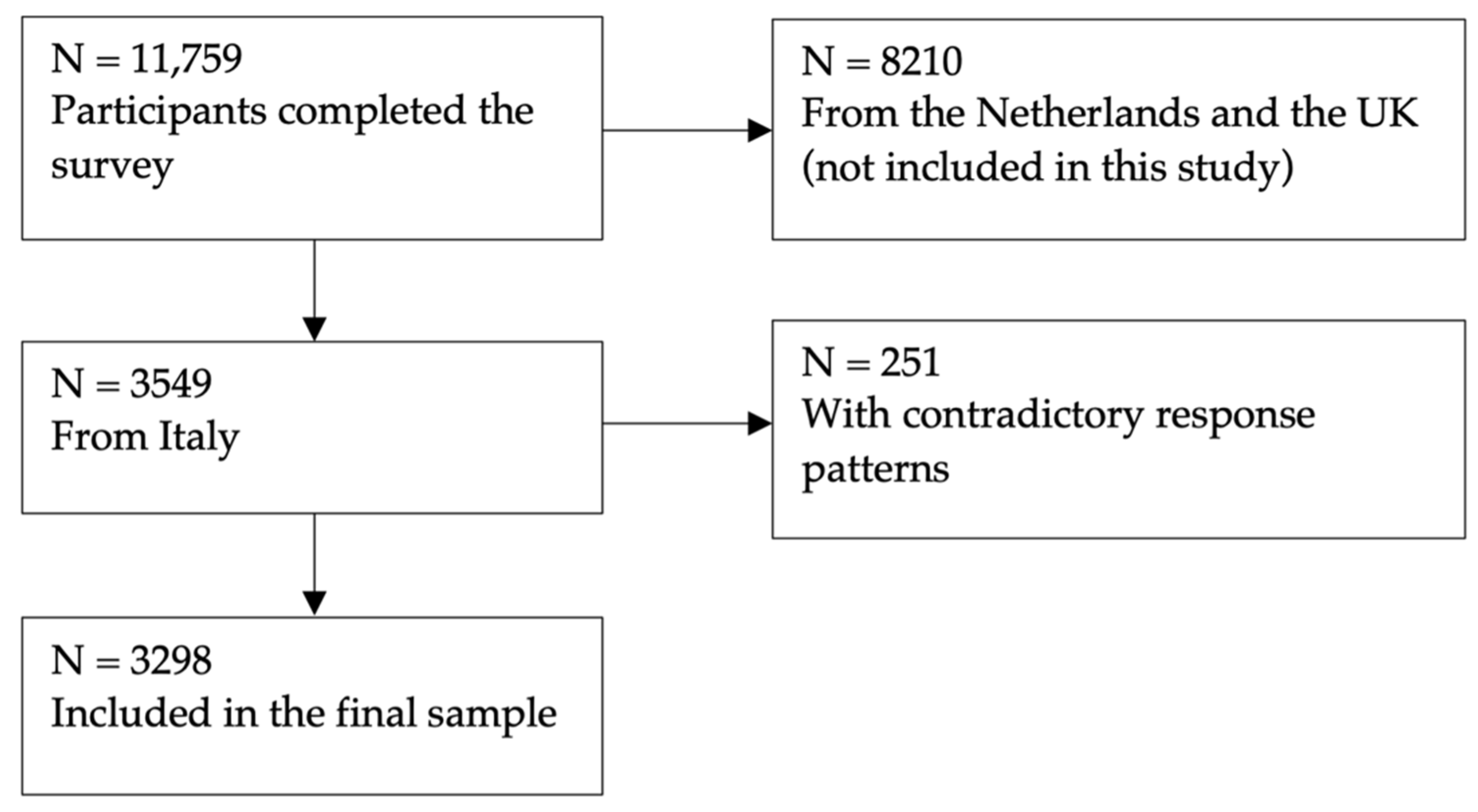
In order to increase the representativeness of the sample, Dynata deployed a variety of methods to engage people with diverse motivations to take part in research and to reach participants with different socioeconomic statuses. To avoid self-selection bias, specific details of the project were not visible at the time of the invitation. The project details were only disclosed later on. Participants who answered the survey in less than five minutes were automatically excluded from the analysis. Additionally, participants with contradictory response patterns were excluded. For the QOLIBRI, the following answers were excluded as they were contradictory: If someone chose responses at either the left or right extremes of the Likert scale, that meant that they were not satisfied at all, but also not bothered at all. All collected data were anonymized. The nonresponse rate of the survey was 14.1%. Figure 1 shows the general Italian population sample attrition.
Figure 1.
General population sample attrition chart.
2.4.2. TBI Sample
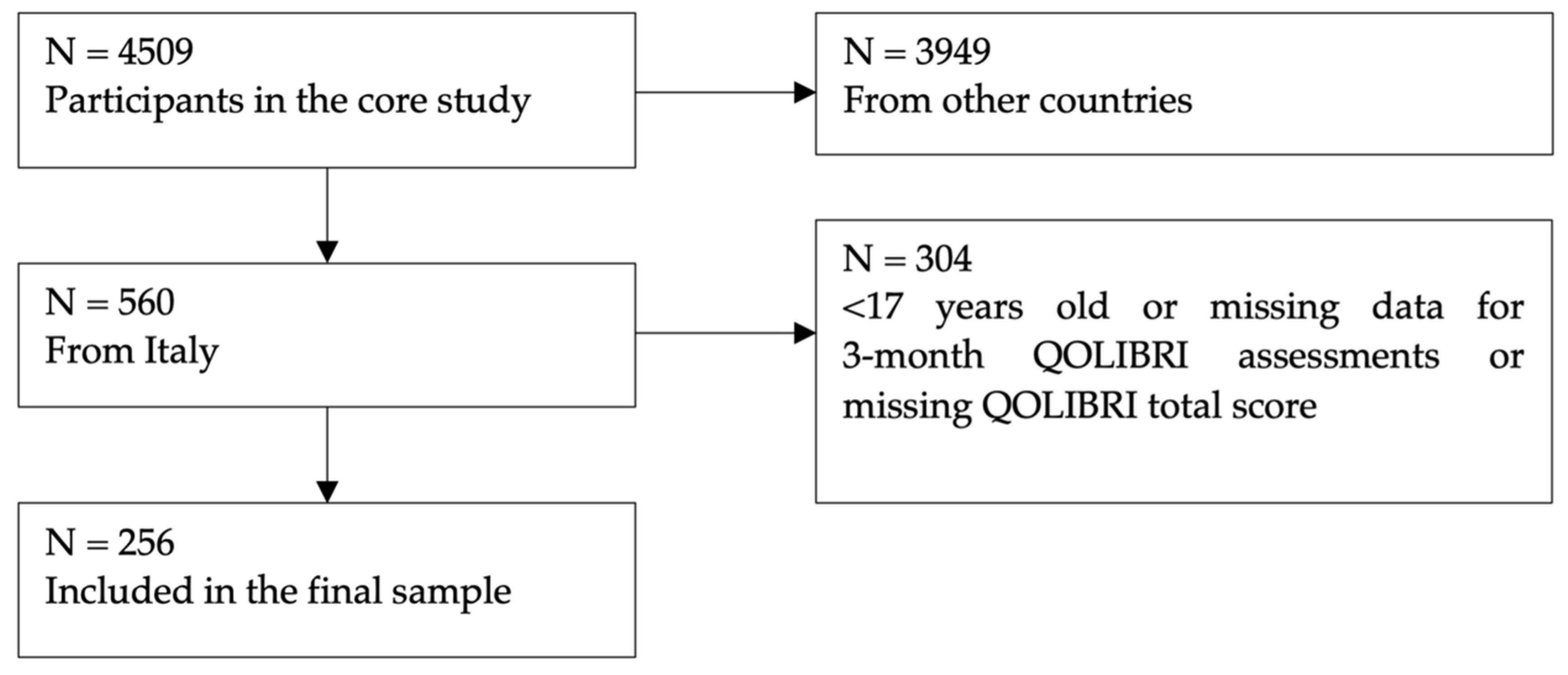
Participants in the TBI sample were a part of the CENTER-TBI study (EC grant 602150), which collected data from 4509 patients in 18 countries [35]. The following inclusion criteria had to be fulfilled: a clinical diagnosis of TBI, presentation in the hospital fewer than 24 h after injury, and an indication for computed tomography (CT). Data were collected between 9 December 2014 and 17 December 2017 via face-to-face visits, in hospital visits, via telephone interviews, or a combination of telephone interview and e-mail. Data on sex, age, time since injury and education was collected at study enrollment based on medical records and self-report. The information on age at study enrollment reflects the age at injury. The QOLIBRI data used was obtained around three months post-injury (i.e., minus two to plus five weeks). Figure 2 shows the TBI sample attrition. No participants with contradictory response patterns were identified. Therefore, all were included in the analyses.
Figure 2.
TBI sample attrition chart.
2.5. Statistical Analyses
The following section describes the statistical analyses in detail. All the analyses were carried out using R version 4.0.3 [41] employing the packages lavaan [42] and semTools [43] for the calculation of Confirmatory Factor Analysis (CFA) and MI, respectively. The significance level was set at 5%.
2.5.1. Item and Scale Characteristics of QOLIBRI in General Population
Firstly, the item characteristics of the reworded QOLIBRI were examined. This included means, standard deviations, skewness, and a check of the floor and ceiling effects. Skewness was characterized as symmetric for values from −0.5 to 0.5, moderately skewed from ±0.5 to ±1, and highly skewed for values above ±1 [44]. On the scale level, the internal consistency of items was calculated using Cronbach’s alpha. Then, the correlation between scales and the range of correlations between items and their home scales were checked. In order to evaluate the ceiling effects, a cut-off value of 40% was chosen for the highest category “very”. This is twice as high as the 20% that could be expected by chance with five categories. For the floor effects, we controlled by combining the response categories “not at all” and “slightly”, with a cut-off of 10%. The recommendations of the World Health Organization Quality of Life (WHOQOL) Group [45] were followed to exclude items with a Corrected Item-Total Correlation (CITC) higher than 0.4. However, no items had to be excluded.
2.5.2. Construct Validity of QOLIBRI in General Population
We used confirmatory factor analysis (CFA) to verify whether the six-factor structure of the original questionnaire could be replicated for the adapted QOLIBRI applied in the general reference population sample. For this purpose, we first estimated three models: a one-factor model, a two-factor model, and the original six-factor model. The one-factor model assumed a general factor HRQoL that is associated equally with all 37 QOLIBRI items. The two-factor model assumed two intercorrelated factors, where one factor included items from the QOLIBRI that represented satisfaction with certain aspects of an individual’s life (Part A) and the second factor reflected feeling bothered with some aspects of one’s life (Part B). The six-factor model which was described above in detail comprised six factors (Cognition, Self, Daily Life and Autonomy, Social Relationships, Emotions and Physical Problems). Finally, the models were compared using chi-square difference tests.
2.5.3. Measurement Invariance between Samples
The examination of the MI included analyses of individual responses from both samples. Due to the limited sample size in the TBI sample, we had to dichotomize the response categories of the QOLIBRI, with the response categories “not at all” and “slightly” forming the lower category and the response categories “moderately”, “quite” and “very” the higher category. We therefore followed the approach of Wu and Estabrook [46] when testing MI for dichotomized response categories. We estimated increasingly constrained models and compared the model fit among these. We first estimated the baseline model, which is mostly equivalent to configural MI and freely estimates all four parameters (thresholds, loadings, intercepts and residuals). Here, the requirement of configural MI is satisfied when the same number of factors and the same pattern of loadings are equal for both groups. We then estimated the second model, where three parameters are restricted and the thresholds are freely estimated, which corresponds to partial MI. Finally, in the last model, all four parameters were restricted, which is equivalent to full MI.
2.5.4. Regression Analysis
Research suggests that age [47], gender [48], education [49] and the presence of chronic health conditions (CHC) [50,51] have an impact on HRQoL. Therefore, to generate reference values that represent HRQoL for meaningful subgroups, we investigated the influence of these factors on HRQoL as measured by the QOLIBRI total score using multiple linear regression. Available information from the general population sample on these variables and their interactions was included in the regression model. Age was binned into six ordered age categories (18 to 24; 25 to 34; 35 to 44; 45 to 54; 55 to 64; older than 65 years). Bearing in mind that the age—in the form of 10-year age bins—had a significant influence on the total score of the short form of the QOLIBRI, its overall scale—QOLIBRI-OS, in the Italian population [52], the same age bins were used here. Sex was categorized as female and male. Education was assessed as the highest level of education and categorized as one of the following three: low (primary school), middle (diploma, secondary school, high school, or post-high school), or high (college or university). Participants were categorized in terms of CHCs either being present (when they reported at least one CHC) or being absent. The dependent variable was the participants’ QOLIBRI total score.
2.5.5. Reference Values from the General Population Sample
Based on the results of a linear regression analysis, tables were presented with population reference values in form of percentiles (2.5%, 5%, 16%, 30%, 40%, 50%, 60%, 70%, 85%, 95% and 97.25%). Values below the 16th percentile and above the 85th percentile (both rounded up to the next integer) represent low and excellent HRQoL, respectively. These can be used to evaluate whether an individual’s QOLIBRI total score is below, equal to, or above the value of the respective reference group.
3. Results
The sociodemographic characteristics of the general population sample are presented in Table 1. Both sexes were represented equally. The mean age of this sample was 45.27 (SD = 14.85) years. Slightly more than a half of the participants (53.97%) reported no CHCs. Detailed information on specific CHCs per age group can be found in Appendix A, Table A1.

Table 1.
Characteristics of the general population sample (N = 3298).
Sociodemographic and clinical characteristics of the TBI sample are presented in Table 2. The mean age was 50.63 (SD = 20.75) years and 68.8% of the TBI sample were males. Most subjects (55.94%) had an intermediate level of education. The majority of the TBI sample sustained a mild TBI. Over half of the participants (53.73%) recovered well after TBI.

Table 2.
Characteristics of the TBI sample (N = 256).
3.1. Item and Scale Characteristics of QOLIBRI in the General Population
Item characteristics including mean value, skewness, and floor and ceiling effects are presented in Table 3. On average, individuals were rather satisfied with their HRQoL (M = 3.62 [3.11–4.02]). The lowest satisfaction scores related to questions on anger or aggression (M = 3.11, SD = 1.26) and the highest satisfaction scores were reported in connection with the ability to find one’s way around (M = 4.02, SD = 0.98), the ability to get out and about (M = 4.02, SD = 1.02), and the ability to carry out domestic activities (M = 4.02, SD = 0.97). With skewness values from 0 to ±0.99, the item distribution can be considered as moderately skewed. None of the satisfaction items from the Part A exceeded the cut-off value for ceiling effects. The reversed scales “Emotions” and “Physical Problems” in Part B, containing bothered items, showed higher values, indicating that individuals from the general population sample were mostly not bothered by problems present in the TBI population. The scales “Cognition” and “Physical Problems” were below the cut-off value of 10%, indicating that the healthy population sample had very few problems in these domains.

Table 3.
Item characteristics of the QOLIBRI in the general population.
Table 4 provides Cronbach’s alpha characterizing the internal consistency of the six QOLILBRI scales. Coefficients ranged from 0.87 to 0.92 indicating good to excellent internal consistency of the QOLIBRI scales [53]. Based on corrected item-total correlations (CITC) and the cut-off of 0.40, all items were considered consistent. The subscales were moderately to highly intercorrelated (r between 0.35 and 0.77). The highest correlation was found between the subscales “Daily Life and Autonomy” and “Self” (r = 0.83), while the lowest correlation was between the scales “Emotions” and “Cognition” (r = 0.35).

Table 4.
Psychometric properties of the QOLIBRI scales in general population.
3.2. Construct Validity of the QOLIBRI in the General Population
In order to evaluate the latent factor structure of the adapted QOLIBRI, CFAs were carried out, comparing the one, two and six factorial models. Table 5 summarizes the goodness of fit indices for these models, showing the best fit for the six factorial model with χ2(614) = 7473, p < 0.001, CFI = 0.994, and RMSEA = 0.058, 90% CI (0.057; 0.059) [54].

Table 5.
Results of confirmatory factor analyses of the QOLIBRI in general population.
3.3. Measurement Invariance
The results of the MI analyses indicated no significant difference between the configural and partial invariance models (Table 6), thus partial invariance can be assumed. However, a comparison of the partial and full invariance models revealed statistically significant differences, indicating that thresholds differed between these models. Further analysis has been undertaken to assess the practical significance of these differences. Examining the thresholds in the partial invariance model showed that these values differed between the general population sample and the TBI sample (Table A2), indicating that the response behavior was not identical in both groups. However, these threshold differences did not exceed 5%. Therefore, the difference between partial and full measurement invariance can be interpreted as being non-significant, resulting in full measurement invariance between the TBI and general population sample. Thus, when comparing QOLIBRI scores between general population and TBI population samples, the differences in scores can be attributed to real differences in HRQoL.

Table 6.
Results of Measurement Invariance testing: Model comparison.
3.4. Linear Regression Analysis
Regression analysis revealed a significant impact of age, CHCs and education (Table 7). Individuals in all other age groups displayed significantly higher QOLIBRI scores than individuals aged 18 to 24 years. The presence of a CHC significantly influenced HRQoL, since healthy individuals had higher QOLIBRI scores than individuals with at least one chronic health condition. Individuals with a high, but not those with a medium level of education had significantly higher QOLIBRI scores than individuals with lower education. The effect of sex or any other interaction did not significantly contribute to explaining the QOLIBRI scores.

Table 7.
Results of the linear regression analysis.
3.5. QOLIBRI Reference Values for the Italian General Population
Based on the results of the regression analysis, reference values were stratified by age, level of education, and the presence of at least one CHC (Table 8). Additionally, we stratified reference values by sex because prior research on HRQoL in individuals after TBI indicates sex effects on HRQoL [55,56,57]. Reference values without categorization by sex can be found in the Appendix A (s. Table A3). Reference tables for the QOLIBRI subscales can be found in Appendix A (s. Table A4, Table A5, Table A6, Table A7, Table A8 and Table A9).

Table 8.
Reference values for the QOLIBRI total score obtained from the general population sample in Italy stratified by sex, health status, age, and education.
The following example will try to illustrate how to use these values. After a TBI, a 50-year-old woman with diabetes presented with a QOLIBRI total score of 65. The appropriate reference values are those of females with at least one CHC in the age group of 45 to 54 years (Table 8). Table 8 shows that about 65% of individuals in her age group reported the same or a lower level of HRQoL. Her value lies in the range of one standard deviation above the median and can thus be considered as being average. Based on the 16%-percentile cut-off value, HRQoL is interpreted as being below average for female individuals of 50 years with one CHC when the QOLIBRI total score is lower than 42.
4. Discussion
The aim of this study was to provide reference values for the QOLIBRI derived from a general Italian population sample. For that purpose, some conditions had to be fulfilled. First, CFA was used to verify that the adjusted QOLIBRI had the assumed six-factorial structure (Cognition, Self, Daily Life and Autonomy, Social Relationships, Emotions, Physical Problems) like the original QOLIBRI version for adults after TBI. This requirement was met and the results were almost consistent with an earlier study [40] that applied the adapted QOLIBRI questionnaire to general population samples from the Netherlands and the UK.
Gorbunova et al. [40] showed that in the Dutch population, the interaction between gender and CHCs was also significant in the regression analysis. This was not the case in the Italian or in the United Kingdom populations. Concerning the QOLIBRI total score without further stratification, a value below 50 obtained from general Italian sample indicates impaired HRQoL. The values obtained from the English and Dutch general population samples were lower (i.e., 44 for the UK) and higher (i.e., 55 for the Netherlands), respectively [40]. Since no differences can be observed in terms of the distribution of the sociodemographic or health-related factors, these findings can be explained by the differences in HRQoL across the countries [58,59,60,61]. For example, Alonso et al. [61] found that participants from the Netherlands (M = 55.2) reported the highest generic mental HRQoL score as measured using the Short Form-36 (SF-36) mental component summary score, compared with other countries (e.g., Italy: M = 50.3). In addition, the European Study of Epidemiology of Mental Disorders within six countries found that the proportion of respondents reporting problems on any of the EuroQol-5 Dimensions (EQ-5D) [62] was significantly higher in France and lower in Spain and Italy [58]. Taken together, all these differences emphasize the importance of country-specific reference values, which is also the case for TBI-specific HRQoL assessments.
The MI analyses indicated that the same construct was measured in the general Italian reference sample and in the TBI population. Although the full MI model differed from the partial MI model in terms of model fit, analyses of threshold fluctuations indicated that thresholds did not differ more than 5% and were thus negligible. The same conclusion could also be drawn for the QOLIBRI in the Dutch and UK samples [40,58,59,60,61].
Our results showed that younger age, presence of CHCs, and lower level of education are associated with worse HRQoL measured using the QOLIBRI. Wu et al. [52] found similar results for the use of the short version of the QOLIBRI, the QOLIBRI-OS, in an Italian general population sample providing reference values. The use of the same age bins in calculating the regression analyses presented, as well as in stratifying the reference values, ensures that the reference values of the two instruments are comparable in the future. Regarding age differences, a study examining HRQoL after heart failure found that older patients’ HRQoL exceeded expectations for their age, whereas younger individuals complained of loss of activities or roles and rated their HRQoL as being correspondingly worse. The authors suggested that better HRQoL in older compared with younger patients was due to the older patients’ ability to reconceptualize their expectations in relation to their health problems. Duke et al. [63] also demonstrated that older people who had adapted their activities to the chronic illness in question had better mental health, suggesting that it is not just the presence of health problems or young age that determines good quality of life.
In addition, it should be noted that sex did not play a role either in the study by Wu et al. [52] nor in the present study. However, the literature on TBI regarding sex or gender differences is inconsistent [57,64,65,66], while there is strong evidence that gender represents an influential factor in TBI [67]. Previous research shows that sex differences were found to possibly affect sustaining a TBI [68], to impact post-concussion symptoms [56,69], depression [70], anxiety [70], as well as recovery after TBI [71,72]. A recent study by Mikolic et al. (2021), examining differences between men and women in treatment and outcome after TBI, finds that after mild TBI women reported lower generic and disease-specific HRQoL than men. Despite controversial research findings, gender/sex seems to be important for outcome assessment after TBI. Therefore, we have also added a stratification of reference values by sex in addition to the stratification by age, presence of CHC and education.
In contrast to our TBI sample showing a negative association between the HRQoL and age (r = −0.18), as well as to prior research that has found a decrease in HRQoL in older subjects with a TBI history [47], the general population sample investigated in the present study displayed higher HRQoL with increasing age. This is in line with findings from a non-TBI Taiwanese sample, which showed a positive effect of age on mental HRQoL and negative influence on physical HRQoL measured using the generic Short Form 12 (SF-12) [73]. In our sample, we used the QOLIBRI total score, which incorporates both mental and physical aspects of HRQoL. Further research should investigate the differential effects of age on individual QOLIBRI dimensions.
It is reasonable to assume that chronic health problems have an influence on HRQoL [74]. Our results showed that individuals with CHCs exhibited lower QOLIBRI total scores than individuals without CHCs. These results are consistent with previous research which indicates an inverse relationship between CHCs and HRQoL [75].
In addition, level of education was also associated with better HRQoL. Individuals with a higher education level reported higher QOLIBRI total scores in comparison to individuals with low education levels. These findings are in line with prior research showing an association between higher education levels and better HRQoL in non-TBI [76] and TBI [77,78] populations. The relationship between education and HRQoL can likely be explained by the opportunities higher education and better socioeconomic status provide, furthering, for example, self-determination through better income and better access to health services [79,80,81].
4.1. Strengths and Limitations
The most important strength of our study is the number of survey participants, which allowed reference values to be calculated stratified by several sub-groups. For example, we were able to provide reference tables for the individuals with and without CHCs and integrating the education levels. The interpretation of HRQoL for Italian individuals after TBI has thereby been improved. Furthermore, reference values based on percentiles are a common approach in clinical practice, facilitating the interpretation and communication of the QOLIBRI scores. The comparison with a (healthy) general population improves the comprehensibility of the test results for the patients.
This study also has several limitations that may require discussion. The first limitation concerns the recruitment of the general population sample. Recruitment was carried out via online platforms and strived for maximum representativeness. However, the online nature of the recruitment only captures certain population groups, such as only those who have Internet access, which may have led to selection biases [82]. In addition, we do not have information about those who declined the survey invitation, which is one of the main issue of online surveys [83]. Possible carelessness in answering online surveys [84] as well as the lack of opportunity to verify the authenticity of the data are notable limitations [82]. Moreover, the severity of the CHCs, as well as their duration, were not recorded because the analyses of these characteristics were beyond the scope of this study. Future studies may investigate the influence of these factors on disease-specific HRQoL.
With respect to the TBI sample, it should be noted that its relatively small size made a dichotomization of the QOLIBRI’s response categories necessary, which always results in a loss of information [85,86]. Furthermore, the vast majority of the TBI sample (71%) consisted of mild TBI, which could have led to response categories not being exhausted (e.g., not at all satisfied or very bothered), requiring the modification of the number of response categories for MI analysis. However, this limitation only concerns the comparison of the QOLIBRI between the general and the TBI sample. To fill this gap, future research should investigate potential differences between Italian TBI and general population samples employing larger TBI samples. With regard to injury severity in the TBI sample, it should be noted that 13.7% of subjects had missing information, which is common in clinical trials. These missing data were not imputed since this information has not been used in the further analyses. The 13.7% of missing values for education were either due to the fact that the level of education was unknown or not reported. Since we did not include any of the above variables in determining the reference values and used them only for the descriptive statistics of the TBI sample, the missing values had no further impact on our results.
The QOLIBRI is an internationally widely used instrument, which has been translated into 26 languages. The reference values for the Italian population presented here may help to consider cultural differences in HRQoL. In addition to the total score, reference values on the subscale level allow the HRQoL domains to be evaluated more precisely. However, to date, there are reference values only for two further countries (i.e., the Netherlands and the UK). Therefore, further studies are required that investigate country-specific reference values for the QOLIBRI in the general population to enable multinational studies on TBI supporting the understanding of the clinical meaning of HRQoL after TBI.
4.2. Conclusions
This study contributes to TBI outcome research by providing reference values for the TBI-specific instrument QOLIBRI for an Italian general population stratified by age, education, gender, and the presence of CHCs. Researchers and clinicians are now able to employ reference values for individuals from Italy which could help them to better interpret HRQoL after TBI in individuals and to adjust their treatment accordingly, which in turn could help to improve the quality of life of the individuals concerned.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm12020491/s1, Membership of CENTER-TBI Participants and Investigators is provided in the Supplementary Materials.
Author Contributions
Data Collection: the CENTER-TBI Participants and Investigators; Research question and design of the study: N.v.S.; Conceptualization: U.K., S.G., M.Z. and N.v.S.; Data curation: U.K., S.G., S.P. and J.H.; Formal analysis: U.K. and S.G.; Investigation: J.H.; Methodology: U.K., S.G., M.Z. and N.v.S.; Software: U.K. and S.G.; Supervision: N.v.S.; Visualization: U.K.; Writing—original draft: U.K.; review and editing: U.K., S.G., M.Z., J.H., S.P. and N.v.S. All authors have read and agreed to the published version of the manuscript.
Funding
CENTER-TBI was supported by the European Union 7th Framework program (EC grant 602150). Additional funding was obtained from the Hannelore Kohl Stiftung (Bonn, Germany), from OneMind (Napa, CA, USA), from Integra LifeSciences Corporation (Princeton, NJ, USA) and from Neurotrauma Sciences (Alpharetta, GA, USA).
Institutional Review Board Statement
The CENTER-TBI study (EC grant 602150) has been conducted in accordance with all relevant laws of the EU if directly applicable or of direct effect and all relevant laws of the country where the recruiting sites were located, including, but not limited to, the relevant privacy and data protection laws and regulations (the “Privacy Law”), the relevant laws and regulations on the use of human materials, and all relevant guidance relating to clinical studies from time to time in force, including, but not limited to, the ICH Harmonized Tripartite Guideline for Good Clinical Practice (CPMP/ICH/135/95) (“ICH GCP”) and the World Medical Association Declaration of Helsinki entitled “Ethical Principles for Medical Research Involving Human Subjects”. Informed consent was obtained for all patients recruited in the Core Dataset of CENTER-TBI and documented in the e-CRF. Ethical approval was obtained for each recruiting site. The list of sites, Ethical Committees, approval numbers and approval dates can be found on the project’s website https://www.center-tbi.eu/project/ethical-approval (accessed on 15 July 2022).
Data Availability Statement
All relevant data are available upon request from CENTER-TBI, and the authors are not legally allowed to share it publicly. The authors confirm that they received no special access privileges to the data. CENTER-TBI is committed to data sharing and in particular to responsible further use of the data. Hereto, we have a data sharing statement in place: https://www.center-tbi.eu/data/sharing (accessed on 1 July 2022). The CENTER-TBI Management Committee, in collaboration with the General Assembly, established the Data Sharing policy, and Publication and Authorship Guidelines to assure correct and appropriate use of the data as the dataset is hugely complex and requires help of experts from the Data Curation Team or Bio- Statistical Team for correct use. This means that we encourage researchers to contact the CENTER-TBI team for any research plans and the Data Curation Team for any help in appropriate use of the data, including sharing of scripts. Requests for data access can be submitted online: https://www.center-tbi.eu/data (accessed on 1 July 2022). The complete Manual for data access is also available online: https://www.center-tbi.eu/files/SOP-Manual-DAPR-2402020.pdf (accessed on 1 July 2022).
Acknowledgments
The authors would like to cordially thank all patients, study participants and CENTER-TBI investigators.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Prevalence of CHC per age group.
Table A1.
Prevalence of CHC per age group.
| CHC (N) | 18–24 (n = 310) | 25–34 (n = 565) | 35–44 (n = 741) | 45–54 (n = 664) | 55–64 (n = 586) | <65 (n = 432) | Total (n = 1518) |
|---|---|---|---|---|---|---|---|
| Asthma | 26 | 48 | 60 | 41 | 41 | 26 | 242 |
| Heart Disease | 2 | 7 | 5 | 10 | 18 | 20 | 62 |
| Stroke | 5 | 6 | 5 | 10 | 5 | 7 | 38 |
| Diabetes | 13 | 25 | 34 | 50 | 52 | 57 | 231 |
| Back Complaints | 12 | 31 | 43 | 50 | 43 | 28 | 207 |
| Arthritis | 6 | 32 | 49 | 64 | 101 | 68 | 320 |
| Rheumatism | 4 | 30 | 43 | 51 | 55 | 37 | 220 |
| Cancer | 5 | 6 | 11 | 11 | 11 | 18 | 62 |
| Memory Problems due to Dementia | 4 | 13 | 13 | 11 | 11 | 2 | 54 |
| Memory Problems due to Ageing | 5 | 7 | 11 | 25 | 47 | 44 | 139 |
| Depression | 57 | 95 | 111 | 105 | 81 | 50 | 499 |
| Other | 19 | 35 | 65 | 89 | 80 | 56 | 344 |

Table A2.
Response probabilities estimated for general population sample from the full invariance model in comparison to TBI sample.
Table A2.
Response probabilities estimated for general population sample from the full invariance model in comparison to TBI sample.
| General Population (TBI as a Ref.) | |
|---|---|
| COGNITION | Thresholds |
| Concentrate | 0.704 (0.000) |
| Expressing yourself | 0.757 (0.000) |
| Memory | 0.670 (0.004) |
| Plan and problem solving | 0.753 (0.000) |
| Decisions | 0.742 (−0.001) |
| Navigate | 0.754 (−0.004) |
| Speed of thinking | 0.766 (0.002) |
| SELF | |
| Energy | 0.597 (0.009) |
| Motivation | 0.628 (0.004) |
| Self-esteem | 0.576 (0.003) |
| Appearance | 0.518 (0.000) |
| Achievements | 0.541 (−0.011) |
| Self-perception | 0.580 (−0.001) |
| Future | 0.435(−0.004) |
| DAILY LIFE AND AUTONOMY | |
| Independence | 0.656 (−0.001) |
| Get out and about | 0.745 (0.002) |
| Domestic activities | 0.750 (0.002) |
| Run personal finances | 0.660 (−0.005) |
| Participation at work | 0.662 (0.001) |
| Social and leisure activities | 0.546 (0.002) |
| In charge of life | 0.628 (−0.002) |
| SOCIAL RELATIONSHIPS | |
| Affection towards others | 0.716 (0.000) |
| Family | 0.709 (−0.001) |
| Friends | 0.649 (−0.002) |
| Partner | 0.649 (0.000) |
| Sex life | 0.547(0.007) |
| Attitudes of others | 0.544 (−0.003) |
| EMOTIONS | |
| Loneliness | 0.482 (−0.004) |
| Boredom | 0.421 (0.000) |
| Anxiety | 0.407 (0.001) |
| Sadness | 0.413 (0.002) |
| Anger/Aggression | 0.378 (0.000) |
| PHYSICAL PROBLEMS | |
| Slow/clumsiness | 0.605 (0.006) |
| Effects other injuries | 0.592 (0.011) |
| Pain | 0.427 (−0.009) |
| Seeing/hearing | 0.534 (−0.005) |
| Effects health problems | 0.447 (−0.004) |
Note: For measurement invariance testing with TBI samples response categories “not at all” and “slightly” were recorded as 1.

Table A3.
Reference values for the QOLIBRI total score obtained from the general population sample in Italy stratified by health status, age, and education.
Table A3.
Reference values for the QOLIBRI total score obtained from the general population sample in Italy stratified by health status, age, and education.
| Health Status × Age | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low HRQoL | −1 SD | Md | +1 SD | High HRQoL | |||||||||
| Health Status | Age | N | 2.5% | 5% | 16% | 30% | 40% | 50% | 60% | 70% | 85% | 95% | 97.25% |
| Healthy | 18–24 | 199 | 39 | 45 | 50 | 56 | 61 | 64 | 67 | 70 | 79 | 91 | 95 |
| 25–34 | 346 | 37 | 42 | 51 | 57 | 62 | 65 | 69 | 73 | 82 | 91 | 98 | |
| 35–44 | 443 | 40 | 44 | 51 | 60 | 65 | 70 | 74 | 79 | 84 | 94 | 98 | |
| 45–54 | 337 | 43 | 48 | 55 | 62 | 67 | 71 | 76 | 80 | 88 | 97 | 100 | |
| 55–64 | 270 | 44 | 48 | 59 | 66 | 72 | 74 | 77 | 82 | 88 | 96 | 100 | |
| ≥65 | 185 | 52 | 55 | 62 | 70 | 74 | 77 | 81 | 85 | 92 | 99 | 100 | |
| At least one CHC | 18–24 | 111 | 24 | 32 | 44 | 48 | 51 | 53 | 58 | 64 | 72 | 85 | 91 |
| 25–34 | 219 | 18 | 27 | 38 | 48 | 50 | 53 | 56 | 61 | 72 | 84 | 89 | |
| 35–44 | 298 | 25 | 35 | 43 | 51 | 55 | 58 | 63 | 67 | 75 | 83 | 87 | |
| 45–54 | 327 | 27 | 31 | 42 | 51 | 55 | 59 | 64 | 69 | 78 | 87 | 90 | |
| 55–64 | 316 | 28 | 32 | 49 | 56 | 60 | 64 | 68 | 73 | 79 | 87 | 92 | |
| ≥65 | 247 | 39 | 42 | 52 | 59 | 63 | 69 | 72 | 77 | 83 | 91 | 94 | |
| Health Status × Education | |||||||||||||
| Low HRQoL | −1 SD | Md | +1 SD | High HRQoL | |||||||||
| Health Status | Education | N | 2.5% | 5% | 16% | 30% | 40% | 50% | 60% | 70% | 85% | 95% | 97.25% |
| Healthy | Low | 591 | 39 | 43 | 50 | 58 | 64 | 68 | 73 | 78 | 85 | 93 | 98 |
| Middle | 1021 | 42 | 47 | 55 | 62 | 67 | 71 | 75 | 79 | 87 | 96 | 100 | |
| High | 168 | 41 | 49 | 55 | 64 | 67 | 71 | 75 | 80 | 86 | 95 | 99 | |
| At least one CHC | Low | 520 | 30 | 35 | 45 | 52 | 56 | 61 | 65 | 70 | 78 | 87 | 89 |
| Middle | 824 | 25 | 30 | 44 | 52 | 56 | 60 | 65 | 70 | 79 | 87 | 92 | |
| High | 174 | 31 | 37 | 46 | 51 | 56 | 60 | 64 | 69 | 79 | 84 | 91 | |
Note: HRQoL: Health-Related Quality of Life; 50% percentiles represent 50% of the distribution corresponding to the median (Md); SD: Standard Deviation; values from −1 standard deviation (16%) to +1 standard deviation (85%) are within the regular range (i.e., not impaired HRQoL). Values below 16% denote low HRQoL and values above 85% indicate outstanding HRQoL.

Table A4.
Reference values for the QOLIBRI Cognition scale obtained from the general population sample in Italy stratified by sex, health status, age, and education.
Table A4.
Reference values for the QOLIBRI Cognition scale obtained from the general population sample in Italy stratified by sex, health status, age, and education.
| Sex × Health Status × Age | Low HRQoL | −1 SD | Md | +1 SD | High HRQoL | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Health Status | Age | N | 2.5% | 5% | 16% | 30% | 40% | 50% | 60% | 70% | 85% | 95% | 97.25% |
| Female | Healthy | 18–24 | 82 | 43 | 47 | 50 | 65 | 72 | 75 | 81 | 85 | 93 | 100 | 100 |
| 25–34 | 159 | 25 | 32 | 54 | 65 | 72 | 75 | 79 | 83 | 93 | 100 | 100 | ||
| 35–44 | 201 | 36 | 43 | 54 | 68 | 72 | 75 | 79 | 86 | 97 | 100 | 100 | ||
| 45–54 | 167 | 44 | 50 | 65 | 72 | 75 | 75 | 79 | 86 | 97 | 100 | 100 | ||
| 55–64 | 136 | 43 | 50 | 61 | 72 | 75 | 75 | 79 | 86 | 93 | 100 | 100 | ||
| ≥65 | 89 | 44 | 50 | 68 | 75 | 76 | 86 | 90 | 93 | 100 | 100 | 100 | ||
| At least one CHC | 18–24 | 63 | 29 | 36 | 50 | 58 | 61 | 65 | 68 | 75 | 83 | 93 | 99 | |
| 25–34 | 125 | 22 | 29 | 43 | 50 | 58 | 68 | 72 | 75 | 86 | 96 | 100 | ||
| 35–44 | 161 | 18 | 25 | 43 | 58 | 65 | 72 | 75 | 79 | 90 | 97 | 100 | ||
| 45–54 | 173 | 34 | 36 | 54 | 65 | 71 | 75 | 75 | 83 | 93 | 100 | 100 | ||
| 55–64 | 169 | 40 | 41 | 61 | 68 | 72 | 75 | 79 | 83 | 93 | 100 | 100 | ||
| ≥65 | 124 | 40 | 50 | 65 | 75 | 75 | 77 | 83 | 86 | 95 | 100 | 100 | ||
| Male | Healthy | 18–24 | 117 | 36 | 50 | 54 | 65 | 72 | 75 | 75 | 83 | 88 | 97 | 100 |
| 25–34 | 187 | 36 | 43 | 50 | 68 | 72 | 75 | 75 | 83 | 90 | 100 | 100 | ||
| 35–44 | 242 | 43 | 50 | 56 | 72 | 75 | 75 | 83 | 86 | 97 | 100 | 100 | ||
| 45–54 | 170 | 43 | 50 | 65 | 75 | 75 | 75 | 79 | 86 | 97 | 100 | 100 | ||
| 55–64 | 134 | 50 | 61 | 72 | 75 | 79 | 84 | 90 | 93 | 100 | 100 | 100 | ||
| ≥65 | 96 | 63 | 65 | 72 | 75 | 79 | 83 | 86 | 90 | 100 | 100 | 100 | ||
| At least one CHC | 18–24 | 48 | 26 | 29 | 50 | 61 | 68 | 75 | 83 | 86 | 90 | 96 | 100 | |
| 25–34 | 94 | 16 | 24 | 40 | 50 | 50 | 58 | 65 | 72 | 83 | 93 | 97 | ||
| 35–44 | 137 | 25 | 32 | 50 | 61 | 68 | 72 | 75 | 75 | 90 | 97 | 100 | ||
| 45–54 | 154 | 24 | 29 | 49 | 58 | 68 | 72 | 75 | 83 | 93 | 100 | 100 | ||
| 55–64 | 147 | 30 | 44 | 59 | 68 | 73 | 75 | 75 | 83 | 90 | 100 | 100 | ||
| ≥65 | 123 | 40 | 50 | 65 | 72 | 75 | 79 | 83 | 86 | 96 | 100 | 100 | ||
| Sex × Health Status × Education | Low HRQoL | −1 SD | MD | +1 SD | High HRQoL | |||||||||
| Sex | Health Status | Education | N | 2.5% | 5% | 16% | 30% | 40% | 50% | 60% | 70% | 85% | 95% | 97.25% |
| Female | Healthy | Low | 321 | 40 | 43 | 50 | 65 | 72 | 75 | 75 | 83 | 93 | 100 | 100 |
| Middle | 445 | 43 | 50 | 61 | 72 | 75 | 75 | 83 | 86 | 97 | 100 | 100 | ||
| High | 68 | 24 | 48 | 71 | 75 | 79 | 83 | 86 | 90 | 97 | 100 | 100 | ||
| At least one CHC | Low | 296 | 29 | 36 | 50 | 61 | 68 | 72 | 75 | 83 | 90 | 100 | 100 | |
| Middle | 439 | 25 | 33 | 50 | 65 | 68 | 72 | 75 | 83 | 90 | 100 | 100 | ||
| High | 80 | 50 | 50 | 61 | 72 | 75 | 75 | 79 | 86 | 93 | 100 | 100 | ||
| Male | Healthy | Low | 270 | 36 | 43 | 54 | 68 | 74 | 75 | 79 | 83 | 93 | 100 | 100 |
| Middle | 576 | 45 | 50 | 65 | 75 | 75 | 79 | 83 | 86 | 97 | 100 | 100 | ||
| High | 100 | 45 | 50 | 61 | 72 | 75 | 75 | 79 | 86 | 97 | 100 | 100 | ||
| At least one CHC | Low | 224 | 28 | 36 | 50 | 65 | 68 | 75 | 75 | 83 | 90 | 100 | 100 | |
| Middle | 385 | 23 | 33 | 50 | 65 | 72 | 75 | 75 | 83 | 90 | 100 | 100 | ||
| High | 94 | 23 | 28 | 47 | 54 | 58 | 68 | 75 | 83 | 90 | 97 | 100 | ||
Note: HRQoL: Health-Related Quality of Life; 50% percentiles represent 50% of the distribution corresponding to the median (Md); SD: Standard Deviation; values from −1 standard deviation (16%) to +1 standard deviation (85%) within the regular range (i.e., not impaired HRQoL). Values below 16% denote low HRQoL and values above 85% indicate outstanding HRQoL.

Table A5.
Reference values for the QOLIBRI Self scale obtained from the general population sample in Italy stratified by sex, health status, age, and education.
Table A5.
Reference values for the QOLIBRI Self scale obtained from the general population sample in Italy stratified by sex, health status, age, and education.
| Sex × Health Status × Age | Low HRQoL | −1 SD | Md | +1 SD | High HRQoL | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Health Status | Age | N | 2.5% | 5% | 16% | 30% | 40% | 50% | 60% | 70% | 85% | 95% | 97.25% |
| Female | Healthy | 18–24 | 82 | 22 | 25 | 40 | 50 | 58 | 65 | 71 | 75 | 79 | 100 | 100 |
| 25–34 | 159 | 8 | 14 | 36 | 50 | 58 | 65 | 72 | 75 | 87 | 100 | 100 | ||
| 35–44 | 201 | 18 | 25 | 40 | 54 | 61 | 68 | 75 | 75 | 86 | 100 | 100 | ||
| 45–54 | 167 | 25 | 29 | 50 | 64 | 68 | 72 | 75 | 79 | 90 | 100 | 100 | ||
| 55–64 | 136 | 18 | 31 | 50 | 58 | 65 | 72 | 75 | 75 | 85 | 97 | 97 | ||
| ≥65 | 89 | 41 | 45 | 58 | 68 | 72 | 75 | 75 | 83 | 93 | 100 | 100 | ||
| At least one CHC | 18–24 | 63 | 8 | 11 | 22 | 36 | 43 | 50 | 55 | 61 | 65 | 75 | 79 | |
| 25–34 | 125 | 8 | 11 | 22 | 40 | 47 | 50 | 58 | 61 | 75 | 82 | 96 | ||
| 35–44 | 161 | 8 | 8 | 29 | 43 | 50 | 54 | 61 | 68 | 75 | 86 | 90 | ||
| 45–54 | 173 | 5 | 11 | 25 | 43 | 50 | 58 | 61 | 68 | 75 | 90 | 96 | ||
| 55–64 | 169 | 11 | 15 | 36 | 50 | 55 | 65 | 68 | 72 | 75 | 90 | 96 | ||
| ≥65 | 124 | 15 | 25 | 40 | 50 | 54 | 61 | 68 | 72 | 79 | 90 | 100 | ||
| Male | Healthy | 18–24 | 117 | 25 | 35 | 50 | 57 | 65 | 68 | 75 | 75 | 86 | 95 | 100 |
| 25–34 | 187 | 25 | 29 | 50 | 54 | 61 | 68 | 72 | 75 | 83 | 99 | 100 | ||
| 35–44 | 242 | 22 | 36 | 50 | 58 | 68 | 72 | 75 | 75 | 86 | 100 | 100 | ||
| 45–54 | 170 | 23 | 36 | 50 | 58 | 65 | 72 | 75 | 75 | 86 | 100 | 100 | ||
| 55–64 | 134 | 36 | 46 | 54 | 65 | 72 | 72 | 75 | 79 | 90 | 100 | 100 | ||
| ≥65 | 96 | 36 | 53 | 62 | 68 | 72 | 75 | 75 | 79 | 89 | 100 | 100 | ||
| At least one CHC | 18–24 | 48 | 11 | 25 | 38 | 50 | 53 | 61 | 68 | 72 | 79 | 94 | 100 | |
| 25–34 | 94 | 6 | 11 | 25 | 39 | 47 | 50 | 53 | 58 | 75 | 86 | 97 | ||
| 35–44 | 137 | 11 | 22 | 36 | 47 | 54 | 58 | 65 | 72 | 78 | 83 | 90 | ||
| 45–54 | 154 | 11 | 18 | 29 | 47 | 50 | 58 | 65 | 69 | 79 | 90 | 93 | ||
| 55–64 | 147 | 15 | 21 | 43 | 54 | 61 | 65 | 72 | 75 | 79 | 90 | 95 | ||
| ≥65 | 123 | 22 | 26 | 50 | 60 | 65 | 68 | 72 | 75 | 83 | 93 | 93 | ||
| Sex × Health Status × Education | Low HRQoL | −1 SD | MD | +1 SD | High HRQoL | |||||||||
| Sex | Health Status | Education | N | 2.5% | 5% | 16% | 30% | 40% | 50% | 60% | 70% | 85% | 95% | 97.25% |
| Female | Healthy | Low | 321 | 11 | 25 | 40 | 54 | 61 | 68 | 75 | 75 | 86 | 100 | 100 |
| Middle | 445 | 22 | 29 | 47 | 58 | 65 | 68 | 75 | 75 | 86 | 100 | 100 | ||
| High | 68 | 28 | 36 | 54 | 65 | 68 | 75 | 75 | 79 | 90 | 100 | 100 | ||
| At least one CHC | Low | 296 | 8 | 15 | 29 | 47 | 50 | 54 | 65 | 68 | 75 | 86 | 96 | |
| Middle | 439 | 8 | 11 | 29 | 43 | 50 | 58 | 61 | 68 | 75 | 90 | 97 | ||
| High | 80 | 15 | 22 | 36 | 50 | 56 | 58 | 65 | 68 | 79 | 83 | 86 | ||
| Male | Healthy | Low | 270 | 25 | 33 | 47 | 54 | 65 | 68 | 75 | 75 | 86 | 100 | 100 |
| Middle | 576 | 27 | 36 | 50 | 61 | 68 | 72 | 75 | 75 | 86 | 100 | 100 | ||
| High | 100 | 25 | 29 | 50 | 64 | 68 | 72 | 75 | 75 | 86 | 100 | 100 | ||
| At least one CHC | Low | 224 | 17 | 25 | 40 | 50 | 58 | 65 | 68 | 72 | 77 | 90 | 98 | |
| Middle | 385 | 11 | 22 | 34 | 47 | 54 | 61 | 65 | 72 | 79 | 89 | 93 | ||
| High | 94 | 6 | 14 | 32 | 43 | 50 | 54 | 65 | 68 | 79 | 93 | 96 | ||
Note: HRQoL: Health-Related Quality of Life; 50% percentiles represent 50% of the distribution corresponding to the median (Md); SD: Standard Deviation; values from −1 standard deviation (16%) to +1 standard deviation (85%) within the regular range (i.e., not impaired HRQoL). Values below 16% denote low HRQoL and values above 85% indicate outstanding HRQoL.

Table A6.
Reference values for the QOLIBRI Daily Life and Autonomy scale obtained from the general population sample in Italy stratified by sex, health status, age, and education.
Table A6.
Reference values for the QOLIBRI Daily Life and Autonomy scale obtained from the general population sample in Italy stratified by sex, health status, age, and education.
| Sex × Health Status × Age | Low HRQoL | −1 SD | MD | +1 SD | High HRQoL | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Health Status | Age | N | 2.5% | 5% | 16% | 30% | 40% | 50% | 60% | 70% | 85% | 95% | 97.25% |
| Female | Healthy | 18–24 | 82 | 33 | 43 | 50 | 54 | 65 | 68 | 72 | 75 | 86 | 100 | 100 |
| 25–34 | 159 | 25 | 33 | 48 | 58 | 68 | 72 | 75 | 83 | 93 | 100 | 100 | ||
| 35–44 | 201 | 36 | 40 | 50 | 61 | 72 | 75 | 79 | 86 | 97 | 100 | 100 | ||
| 45–54 | 167 | 40 | 48 | 58 | 68 | 73 | 75 | 83 | 86 | 100 | 100 | 100 | ||
| 55–64 | 136 | 38 | 40 | 56 | 68 | 75 | 75 | 83 | 86 | 93 | 100 | 100 | ||
| ≥65 | 89 | 48 | 52 | 68 | 75 | 79 | 86 | 90 | 93 | 100 | 100 | 100 | ||
| At least one CHC | 18–24 | 63 | 12 | 18 | 40 | 50 | 50 | 58 | 61 | 68 | 82 | 93 | 95 | |
| 25–34 | 125 | 8 | 16 | 33 | 47 | 54 | 61 | 70 | 75 | 84 | 97 | 100 | ||
| 35–44 | 161 | 15 | 22 | 40 | 50 | 61 | 68 | 75 | 75 | 86 | 97 | 100 | ||
| 45–54 | 173 | 12 | 25 | 43 | 54 | 61 | 68 | 72 | 79 | 86 | 98 | 100 | ||
| 55–64 | 169 | 12 | 27 | 50 | 61 | 68 | 72 | 75 | 79 | 86 | 97 | 100 | ||
| ≥65 | 124 | 36 | 40 | 50 | 61 | 68 | 72 | 79 | 83 | 93 | 100 | 100 | ||
| Male | Healthy | 18–24 | 117 | 33 | 39 | 50 | 58 | 65 | 72 | 75 | 79 | 86 | 97 | 100 |
| 25–34 | 187 | 33 | 41 | 50 | 61 | 68 | 72 | 75 | 79 | 90 | 100 | 100 | ||
| 35–44 | 242 | 25 | 43 | 50 | 68 | 72 | 75 | 75 | 83 | 93 | 100 | 100 | ||
| 45–54 | 170 | 41 | 47 | 61 | 72 | 75 | 75 | 83 | 86 | 93 | 100 | 100 | ||
| 55–64 | 134 | 50 | 53 | 65 | 75 | 75 | 79 | 86 | 90 | 97 | 100 | 100 | ||
| ≥65 | 96 | 58 | 65 | 75 | 75 | 79 | 83 | 86 | 90 | 97 | 100 | 100 | ||
| At least one CHC | 18–24 | 48 | 19 | 24 | 43 | 51 | 54 | 68 | 75 | 75 | 90 | 97 | 100 | |
| 25–34 | 94 | 11 | 22 | 36 | 47 | 50 | 54 | 58 | 65 | 76 | 87 | 96 | ||
| 35–44 | 137 | 25 | 28 | 40 | 50 | 63 | 68 | 72 | 75 | 85 | 97 | 97 | ||
| 45–54 | 154 | 21 | 25 | 43 | 54 | 61 | 68 | 72 | 75 | 86 | 97 | 100 | ||
| 55–64 | 147 | 17 | 34 | 50 | 65 | 68 | 75 | 75 | 79 | 90 | 100 | 100 | ||
| ≥65 | 123 | 25 | 33 | 54 | 68 | 72 | 75 | 79 | 83 | 92 | 100 | 100 | ||
| Sex × Health Status × Education | Low HRQoL | −1 SD | MD | +1 SD | High HRQoL | |||||||||
| Sex | Health Status | Education | N | 2.5% | 5% | 16% | 30% | 40% | 50% | 60% | 70% | 85% | 95% | 97.25% |
| Female | Healthy | Low | 321 | 33 | 40 | 50 | 61 | 68 | 75 | 75 | 83 | 93 | 100 | 100 |
| Middle | 445 | 33 | 40 | 54 | 66 | 74 | 75 | 83 | 90 | 97 | 100 | 100 | ||
| High | 68 | 40 | 45 | 63 | 72 | 75 | 83 | 83 | 90 | 97 | 100 | 100 | ||
| At least one CHC | Low | 296 | 11 | 18 | 40 | 50 | 58 | 68 | 72 | 75 | 86 | 97 | 100 | |
| Middle | 439 | 15 | 22 | 43 | 54 | 61 | 68 | 75 | 79 | 90 | 97 | 100 | ||
| High | 80 | 18 | 36 | 50 | 58 | 68 | 72 | 79 | 83 | 90 | 100 | 100 | ||
| Male | Healthy | Low | 270 | 34 | 41 | 50 | 61 | 71 | 75 | 75 | 83 | 93 | 100 | 100 |
| Middle | 576 | 40 | 50 | 58 | 68 | 75 | 75 | 79 | 83 | 93 | 100 | 100 | ||
| High | 100 | 34 | 47 | 58 | 71 | 75 | 75 | 75 | 86 | 93 | 100 | 100 | ||
| At least one CHC | Low | 224 | 22 | 33 | 47 | 54 | 65 | 68 | 75 | 75 | 86 | 96 | 98 | |
| Middle | 385 | 18 | 25 | 43 | 54 | 65 | 68 | 75 | 75 | 86 | 97 | 100 | ||
| High | 94 | 25 | 31 | 40 | 50 | 58 | 65 | 68 | 75 | 90 | 100 | 100 | ||
Note: HRQoL: Health-Related Quality of Life; 50% percentiles represent 50% of the distribution corresponding to the median (Md); SD: Standard Deviation; values from −1 standard deviation (16%) to +1 standard deviation (85%) within the regular range (i.e., not impaired HRQoL). Values below 16% denote low HRQoL and values above 85% indicate outstanding HRQoL.

Table A7.
Reference values for the QOLIBRI Social Relationships scale obtained from the general population sample in Italy stratified by sex, health status, age, and education.
Table A7.
Reference values for the QOLIBRI Social Relationships scale obtained from the general population sample in Italy stratified by sex, health status, age, and education.
| Sex × Health Status × Age | Low HRQoL | −1 SD | Md | +1 SD | High HRQoL | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Health Status | Age | N | 2.5% | 5% | 16% | 30% | 40% | 50% | 60% | 70% | 85% | 95% | 97.25% |
| Female | Healthy | 18–24 | 82 | 21 | 38 | 50 | 60 | 67 | 71 | 75 | 75 | 88 | 100 | 100 |
| 25–34 | 159 | 21 | 25 | 50 | 60 | 71 | 75 | 75 | 80 | 96 | 100 | 100 | ||
| 35–44 | 201 | 30 | 30 | 50 | 63 | 67 | 75 | 75 | 80 | 96 | 100 | 100 | ||
| 45–54 | 167 | 30 | 42 | 55 | 63 | 71 | 75 | 80 | 84 | 97 | 100 | 100 | ||
| 55–64 | 136 | 30 | 33 | 53 | 67 | 71 | 75 | 75 | 80 | 88 | 100 | 100 | ||
| ≥65 | 89 | 42 | 46 | 55 | 71 | 75 | 75 | 80 | 88 | 92 | 100 | 100 | ||
| At least one CHC | 18–24 | 63 | 15 | 21 | 38 | 46 | 50 | 55 | 63 | 71 | 78 | 95 | 96 | |
| 25–34 | 125 | 9 | 14 | 38 | 50 | 55 | 63 | 67 | 75 | 84 | 95 | 96 | ||
| 35–44 | 161 | 13 | 21 | 42 | 55 | 63 | 67 | 71 | 75 | 88 | 96 | 100 | ||
| 45–54 | 173 | 9 | 17 | 34 | 50 | 59 | 67 | 71 | 75 | 88 | 98 | 100 | ||
| 55–64 | 169 | 18 | 25 | 42 | 55 | 59 | 67 | 75 | 78 | 88 | 96 | 100 | ||
| ≥65 | 124 | 26 | 34 | 46 | 59 | 64 | 71 | 75 | 80 | 88 | 96 | 100 | ||
| Male | Healthy | 18–24 | 117 | 21 | 30 | 50 | 55 | 63 | 67 | 75 | 75 | 84 | 97 | 100 |
| 25–34 | 187 | 20 | 25 | 46 | 59 | 63 | 71 | 75 | 75 | 84 | 96 | 100 | ||
| 35–44 | 242 | 26 | 38 | 50 | 59 | 67 | 75 | 75 | 80 | 92 | 100 | 100 | ||
| 45–54 | 170 | 25 | 30 | 50 | 63 | 71 | 75 | 75 | 81 | 92 | 100 | 100 | ||
| 55–64 | 134 | 27 | 37 | 56 | 67 | 75 | 75 | 80 | 84 | 96 | 100 | 100 | ||
| ≥65 | 96 | 38 | 48 | 63 | 71 | 75 | 75 | 75 | 84 | 92 | 100 | 100 | ||
| At least one CHC | 18–24 | 48 | 14 | 24 | 38 | 46 | 55 | 59 | 65 | 80 | 88 | 96 | 100 | |
| 25–34 | 94 | 13 | 13 | 33 | 42 | 47 | 50 | 58 | 67 | 75 | 92 | 95 | ||
| 35–44 | 137 | 5 | 16 | 37 | 54 | 59 | 67 | 71 | 75 | 80 | 89 | 96 | ||
| 45–54 | 154 | 9 | 13 | 36 | 46 | 55 | 65 | 71 | 75 | 84 | 96 | 100 | ||
| 55–64 | 147 | 25 | 30 | 50 | 59 | 67 | 71 | 75 | 75 | 88 | 96 | 100 | ||
| ≥65 | 123 | 22 | 34 | 50 | 63 | 67 | 71 | 75 | 84 | 91 | 96 | 96 | ||
| Sex × Health Status × Education | Low HRQoL | −1 SD | MD | +1 SD | High HRQoL | |||||||||
| Sex | Health Status | Education | N | 2.5% | 5% | 16% | 30% | 40% | 50% | 60% | 70% | 85% | 95% | 97.25% |
| Female | Healthy | Low | 321 | 21 | 30 | 50 | 63 | 71 | 75 | 75 | 84 | 96 | 100 | 100 |
| Middle | 445 | 26 | 34 | 50 | 63 | 71 | 75 | 75 | 80 | 96 | 100 | 100 | ||
| High | 68 | 34 | 42 | 59 | 67 | 67 | 75 | 80 | 83 | 96 | 100 | 100 | ||
| At least one CHC | Low | 296 | 13 | 17 | 42 | 53 | 59 | 67 | 71 | 75 | 88 | 96 | 100 | |
| Middle | 439 | 9 | 17 | 38 | 50 | 59 | 67 | 71 | 75 | 88 | 96 | 100 | ||
| High | 80 | 25 | 38 | 46 | 55 | 59 | 65 | 71 | 75 | 80 | 92 | 92 | ||
| Male | Healthy | Low | 270 | 25 | 30 | 50 | 59 | 71 | 75 | 75 | 84 | 92 | 100 | 100 |
| Middle | 576 | 25 | 34 | 50 | 63 | 67 | 75 | 75 | 80 | 88 | 100 | 100 | ||
| High | 100 | 17 | 34 | 54 | 63 | 67 | 75 | 75 | 75 | 84 | 100 | 100 | ||
| At least one CHC | Low | 224 | 13 | 25 | 45 | 55 | 63 | 71 | 75 | 76 | 88 | 96 | 100 | |
| Middle | 385 | 11 | 14 | 38 | 50 | 59 | 67 | 71 | 75 | 85 | 96 | 96 | ||
| High | 94 | 14 | 21 | 37 | 50 | 51 | 59 | 66 | 75 | 88 | 98 | 100 | ||
Note: HRQoL: Health-Related Quality of Life; 50% percentiles represent 50% of the distribution corresponding to the median (Md); SD: Standard Deviation; values from −1 standard deviation (16%) to +1 standard deviation (85%) within the regular range (i.e., not impaired HRQoL). Values below 16% denote low HRQoL and values above 85% indicate outstanding HRQoL.

Table A8.
Reference values for the QOLIBRI Emotions scale obtained from the general population sample in Italy stratified by sex, health status, age, and education.
Table A8.
Reference values for the QOLIBRI Emotions scale obtained from the general population sample in Italy stratified by sex, health status, age, and education.
| Sex × Health Status × Age | Low HRQoL | −1 SD | Md | +1 SD | High HRQoL | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Health Status | Age | N | 2.5% | 5% | 16% | 30% | 40% | 50% | 60% | 70% | 85% | 95% | 97.25% |
| Female | Healthy | 18–24 | 82 | 6 | 10 | 25 | 35 | 42 | 50 | 50 | 60 | 75 | 95 | 100 |
| 25–34 | 159 | 5 | 10 | 25 | 35 | 45 | 50 | 55 | 68 | 85 | 100 | 100 | ||
| 35–44 | 201 | 15 | 20 | 30 | 40 | 50 | 50 | 60 | 75 | 85 | 100 | 100 | ||
| 45–54 | 167 | 10 | 15 | 30 | 40 | 50 | 60 | 70 | 80 | 95 | 100 | 100 | ||
| 55–64 | 136 | 25 | 25 | 35 | 50 | 55 | 65 | 75 | 85 | 95 | 100 | 100 | ||
| ≥65 | 89 | 20 | 25 | 40 | 50 | 60 | 75 | 80 | 90 | 100 | 100 | 100 | ||
| At least one CHC | 18–24 | 63 | 0 | 0 | 15 | 23 | 30 | 35 | 36 | 45 | 54 | 80 | 95 | |
| 25–34 | 125 | 0 | 2 | 20 | 25 | 30 | 35 | 45 | 50 | 65 | 85 | 90 | ||
| 35–44 | 161 | 0 | 5 | 20 | 30 | 35 | 45 | 50 | 60 | 75 | 90 | 100 | ||
| 45–54 | 173 | 0 | 5 | 25 | 34 | 40 | 45 | 55 | 65 | 81 | 95 | 100 | ||
| 55–64 | 169 | 10 | 10 | 25 | 35 | 45 | 50 | 60 | 70 | 85 | 95 | 99 | ||
| ≥65 | 124 | 15 | 16 | 30 | 45 | 55 | 65 | 74 | 80 | 90 | 100 | 100 | ||
| Male | Healthy | 18–24 | 117 | 10 | 10 | 25 | 35 | 45 | 45 | 50 | 60 | 78 | 95 | 100 |
| 25–34 | 187 | 10 | 15 | 30 | 40 | 45 | 50 | 60 | 66 | 85 | 100 | 100 | ||
| 35–44 | 242 | 20 | 25 | 30 | 45 | 50 | 60 | 70 | 75 | 90 | 100 | 100 | ||
| 45–54 | 170 | 20 | 25 | 35 | 45 | 50 | 60 | 70 | 80 | 90 | 100 | 100 | ||
| 55–64 | 134 | 17 | 25 | 35 | 50 | 65 | 70 | 79 | 90 | 100 | 100 | 100 | ||
| ≥65 | 96 | 22 | 30 | 42 | 63 | 70 | 78 | 80 | 85 | 95 | 100 | 100 | ||
| At least one CHC | 18–24 | 48 | 10 | 10 | 25 | 30 | 35 | 40 | 50 | 55 | 60 | 84 | 90 | |
| 25–34 | 94 | 0 | 10 | 25 | 35 | 40 | 50 | 50 | 55 | 65 | 84 | 99 | ||
| 35–44 | 137 | 8 | 15 | 25 | 35 | 45 | 50 | 53 | 60 | 75 | 100 | 100 | ||
| 45–54 | 154 | 10 | 15 | 25 | 35 | 45 | 50 | 55 | 65 | 85 | 100 | 100 | ||
| 55–64 | 147 | 17 | 25 | 35 | 45 | 50 | 60 | 65 | 75 | 81 | 95 | 100 | ||
| ≥65 | 123 | 20 | 21 | 40 | 50 | 55 | 65 | 72 | 80 | 90 | 100 | 100 | ||
| Sex × Health Status × Education | Low HRQoL | −1 SD | Md | +1 SD | High HRQoL | |||||||||
| Sex | Health Status | Education | N | 2.5% | 5% | 16% | 30% | 40% | 50% | 60% | 70% | 85% | 95% | 97.25% |
| Female | Healthy | Low | 321 | 15 | 15 | 30 | 40 | 50 | 50 | 65 | 75 | 90 | 100 | 100 |
| Middle | 445 | 10 | 15 | 30 | 40 | 50 | 55 | 65 | 75 | 90 | 100 | 100 | ||
| High | 68 | 12 | 15 | 33 | 45 | 50 | 60 | 71 | 80 | 95 | 100 | 100 | ||
| At least one CHC | Low | 296 | 0 | 0 | 20 | 30 | 40 | 45 | 50 | 65 | 80 | 95 | 100 | |
| Middle | 439 | 5 | 10 | 25 | 30 | 40 | 45 | 55 | 65 | 80 | 95 | 100 | ||
| High | 80 | 10 | 15 | 25 | 35 | 44 | 50 | 55 | 65 | 80 | 85 | 96 | ||
| Male | Healthy | Low | 270 | 14 | 18 | 35 | 50 | 50 | 60 | 70 | 75 | 95 | 100 | 100 |
| Middle | 576 | 15 | 20 | 30 | 45 | 50 | 60 | 70 | 80 | 90 | 100 | 100 | ||
| High | 100 | 10 | 20 | 30 | 40 | 45 | 50 | 67 | 72 | 90 | 100 | 100 | ||
| At least one CHC | Low | 224 | 10 | 16 | 30 | 40 | 50 | 50 | 60 | 70 | 83 | 100 | 100 | |
| Middle | 385 | 10 | 15 | 25 | 40 | 45 | 50 | 55 | 65 | 80 | 95 | 100 | ||
| High | 94 | 5 | 14 | 30 | 40 | 40 | 50 | 55 | 60 | 75 | 90 | 94 | ||
Note: HRQoL: Health-Related Quality of Life; 50% percentiles represent 50% of the distribution corresponding to the median (Md); SD: Standard Deviation; values from −1 standard deviation (16%) to +1 standard deviation (85%) within the regular range (i.e., not impaired HRQoL). Values below 16% denote low HRQoL and values above 85% indicate outstanding HRQoL.

Table A9.
Reference values for the QOLIBRI Physical Problems scale obtained from the general population sample in Italy stratified by sex, health status, age, and education.
Table A9.
Reference values for the QOLIBRI Physical Problems scale obtained from the general population sample in Italy stratified by sex, health status, age, and education.
| Sex × Health Status × Age | Low HRQoL | −1 SD | Md | +1 SD | High HRQoL | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Health Status | Age | N | 2.5% | 5% | 16% | 30% | 40% | 50% | 60% | 70% | 85% | 95% | 97.25% |
| Female | Healthy | 18–24 | 82 | 20 | 26 | 45 | 50 | 52 | 65 | 70 | 75 | 90 | 100 | 100 |
| 25–34 | 159 | 15 | 30 | 45 | 50 | 60 | 65 | 75 | 80 | 100 | 100 | 100 | ||
| 35–44 | 201 | 25 | 25 | 45 | 50 | 60 | 70 | 75 | 85 | 95 | 100 | 100 | ||
| 45–54 | 167 | 25 | 25 | 45 | 55 | 65 | 70 | 80 | 85 | 100 | 100 | 100 | ||
| 55–64 | 136 | 22 | 29 | 40 | 58 | 65 | 75 | 80 | 85 | 90 | 100 | 100 | ||
| ≥65 | 89 | 14 | 27 | 50 | 67 | 75 | 85 | 90 | 95 | 100 | 100 | 100 | ||
| At least one CHC | 18–24 | 63 | 18 | 25 | 30 | 45 | 50 | 55 | 61 | 70 | 80 | 95 | 98 | |
| 25–34 | 125 | 5 | 15 | 25 | 40 | 50 | 50 | 60 | 70 | 80 | 94 | 100 | ||
| 35–44 | 161 | 10 | 20 | 30 | 40 | 45 | 50 | 60 | 65 | 80 | 90 | 95 | ||
| 45–54 | 173 | 5 | 10 | 30 | 40 | 45 | 50 | 62 | 70 | 80 | 98 | 100 | ||
| 55–64 | 169 | 5 | 10 | 25 | 40 | 45 | 50 | 55 | 65 | 80 | 90 | 99 | ||
| ≥65 | 124 | 20 | 25 | 34 | 45 | 52 | 60 | 69 | 80 | 85 | 90 | 95 | ||
| Male | Healthy | 18–24 | 117 | 15 | 25 | 40 | 50 | 55 | 65 | 70 | 75 | 88 | 95 | 100 |
| 25–34 | 187 | 25 | 30 | 40 | 50 | 55 | 65 | 75 | 85 | 100 | 100 | 100 | ||
| 35–44 | 242 | 25 | 30 | 45 | 55 | 60 | 70 | 75 | 85 | 100 | 100 | 100 | ||
| 45–54 | 170 | 25 | 30 | 45 | 59 | 65 | 70 | 80 | 90 | 100 | 100 | 100 | ||
| 55–64 | 134 | 30 | 40 | 52 | 70 | 75 | 80 | 80 | 90 | 100 | 100 | 100 | ||
| ≥65 | 96 | 24 | 30 | 52 | 73 | 75 | 80 | 85 | 90 | 100 | 100 | 100 | ||
| At least one CHC | 18–24 | 48 | 30 | 30 | 40 | 46 | 55 | 65 | 70 | 75 | 80 | 94 | 95 | |
| 25–34 | 94 | 20 | 24 | 40 | 50 | 50 | 60 | 65 | 75 | 80 | 100 | 100 | ||
| 35–44 | 137 | 20 | 25 | 35 | 50 | 50 | 55 | 60 | 70 | 85 | 100 | 100 | ||
| 45–54 | 154 | 10 | 15 | 35 | 45 | 50 | 55 | 65 | 70 | 80 | 92 | 100 | ||
| 55–64 | 147 | 19 | 20 | 35 | 45 | 50 | 60 | 65 | 70 | 80 | 90 | 95 | ||
| ≥65 | 123 | 16 | 20 | 40 | 50 | 55 | 60 | 65 | 75 | 85 | 90 | 95 | ||
| Sex × Health Status × Education | Low HRQoL | −1 SD | Md | +1 SD | High HRQoL | |||||||||
| Sex | Health Status | Education | N | 2.5% | 5% | 16% | 30% | 40% | 50% | 60% | 70% | 85% | 95% | 97.25% |
| Female | Healthy | Low | 321 | 20 | 25 | 40 | 50 | 60 | 65 | 75 | 80 | 90 | 100 | 100 |
| Middle | 445 | 15 | 25 | 45 | 55 | 65 | 75 | 80 | 85 | 100 | 100 | 100 | ||
| High | 68 | 25 | 35 | 45 | 60 | 70 | 73 | 80 | 85 | 100 | 100 | 100 | ||
| At least one CHC | Low | 296 | 5 | 10 | 30 | 40 | 50 | 50 | 60 | 70 | 80 | 95 | 100 | |
| Middle | 439 | 10 | 15 | 30 | 40 | 45 | 50 | 60 | 70 | 80 | 95 | 100 | ||
| High | 80 | 10 | 20 | 35 | 44 | 50 | 60 | 65 | 70 | 80 | 86 | 91 | ||
| Male | Healthy | Low | 270 | 14 | 25 | 45 | 50 | 60 | 70 | 75 | 80 | 95 | 100 | 100 |
| Middle | 576 | 25 | 30 | 45 | 55 | 65 | 75 | 80 | 85 | 100 | 100 | 100 | ||
| High | 100 | 30 | 35 | 50 | 55 | 65 | 75 | 75 | 80 | 96 | 100 | 100 | ||
| At least one CHC | Low | 224 | 10 | 20 | 35 | 50 | 50 | 55 | 65 | 70 | 85 | 95 | 100 | |
| Middle | 385 | 15 | 20 | 35 | 45 | 50 | 60 | 65 | 75 | 80 | 90 | 100 | ||
| High | 94 | 25 | 25 | 40 | 45 | 50 | 55 | 60 | 70 | 85 | 95 | 95 | ||
Note: HRQoL: Health-Related Quality of Life; 50% percentiles represent 50% of the distribution corresponding to the median (Md); SD: Standard Deviation; values from −1 standard deviation (16%) to +1 standard deviation (85%) within the regular range (i.e., not impaired HRQoL). Values below 16% denote low HRQoL and values above 85% indicate outstanding HRQoL.
References
- Maas, A.I.R.; Menon, D.K.; Adelson, P.D.; Andelic, N.; Bell, M.J.; Belli, A.; Bragge, P.; Brazinova, A.; Büki, A.; Chesnut, R.M.; et al. Traumatic Brain Injury: Integrated Approaches to Improve Prevention, Clinical Care, and Research. Lancet Neurol. 2017, 16, 987–1048. [Google Scholar] [CrossRef] [PubMed]
- Dewan, M.C.; Rattani, A.; Gupta, S.; Baticulon, R.E.; Hung, Y.-C.; Punchak, M.; Agrawal, A.; Adeleye, A.O.; Shrime, M.G.; Rubiano, A.M.; et al. Estimating the Global Incidence of Traumatic Brain Injury. J. Neurosurg. 2018, 130, 1080–1097. [Google Scholar] [CrossRef] [PubMed]
- Baldo, V.; Marcolongo, A.; Floreani, A.; Majori, S.; Cristofoletti, M.; Zotto, A.D.; Vazzoler, G.; Trivello, R. Epidemiological Aspect of Traumatic Brain Injury in Northeast Italy. Eur. J. Epidemiol. 2003, 18, 1059–1063. [Google Scholar] [CrossRef] [PubMed]
- Brazinova, A.; Rehorcikova, V.; Taylor, M.S.; Buckova, V.; Majdan, M.; Psota, M.; Peeters, W.; Feigin, V.; Theadom, A.; Holkovic, L.; et al. Epidemiology of Traumatic Brain Injury in Europe: A Living Systematic Review. J. Neurotrauma 2021, 38, 1411–1440. [Google Scholar] [CrossRef] [PubMed]
- Servadei, F.; Ciucci, G.; Piazza, G.; Bianchedi, G.; Rebucci, G.; Gaist, G.; Taggi, F. A Prospective Clinical and Epidemiological Study of Head Injuries in Northern Italy: The Comune of Ravenna. Ital. J. Neurol. Sci. 1988, 9, 449–457. [Google Scholar] [CrossRef]
- Langlois, J.A.; Rutland-Brown, W.; Wald, M.M. The Epidemiology and Impact of Traumatic Brain Injury: A Brief Overview. J. Head Trauma Rehabil. 2006, 21, 375–378. [Google Scholar] [CrossRef]
- Majdan, M.; Plancikova, D.; Brazinova, A.; Rusnak, M.; Nieboer, D.; Feigin, V.; Maas, A. Epidemiology of Traumatic Brain Injuries in Europe: A Cross-Sectional Analysis. Lancet Public Health 2016, 1, e76–e83. [Google Scholar] [CrossRef]
- Lefkovits, A.M.; Hicks, A.J.; Downing, M.; Ponsford, J. Surviving the “Silent Epidemic”: A Qualitative Exploration of the Long-Term Journey after Traumatic Brain Injury. Neuropsychol. Rehabil. 2021, 31, 1582–1606. [Google Scholar] [CrossRef]
- Antonis, T. Cognitive Consequences After Traumatic Brain Injury (TBI). Ann. Clin. Med. Case Rep. 2021, 6, 1–4. [Google Scholar]
- Weis, C.; Webb, E.K.; deRoon-Cassini, T.A.; Larson, C.L. Emotion Dysregulation Following Trauma: Shared Neurocircuitry of Traumatic Brain Injury and Trauma-Related Psychiatric Disorders. Biol. Psychiatry 2021, 91, 470–477. [Google Scholar] [CrossRef]
- Murphy, J.M.; Bennett, J.M.; de la Piedad Garcia, X.; Willis, M.L. Emotion Recognition and Traumatic Brain Injury: A Systematic Review and Meta-Analysis. Neuropsychol. Rev. 2022, 32, 520–536. [Google Scholar] [CrossRef] [PubMed]
- Villa, D.; Causer, H.; Riley, G.A. Experiences That Challenge Self-Identity Following Traumatic Brain Injury: A Meta-Synthesis of Qualitative Research. Disabil. Rehabil. 2021, 43, 3298–3314. [Google Scholar] [CrossRef] [PubMed]
- Milders, M. Relationship between Social Cognition and Social Behaviour Following Traumatic Brain Injury. Brain Inj. 2019, 33, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Masel, B.E.; DeWitt, D.S. Traumatic Brain Injury: A Disease Process, Not an Event. J. Neurotrauma 2010, 27, 1529–1540. [Google Scholar] [CrossRef]
- Thyen, U. Vom Biomedizinischen Zum Biopsychosozialen Verständnis von Krankheit Und Gesundheit. In Sozialpädiatrie; Springer: Berlin/Heidelberg, Germany, 2009. [Google Scholar]
- Polinder, S. Health-Related Quality of Life after TBI: A Systematic Review of Study Design, Instruments, Measurement Propeties, and Outcome. Popul. Health Metrics 2015, 13, 4. [Google Scholar] [CrossRef]
- Gurková, E. Issues in the Definitions of HRQoL. Public Health Rehabil. 2011, 3, 190. [Google Scholar]
- Sherer, M.; Poritz, J.M.P.; Tulsky, D.; Kisala, P.; Leon-Novelo, L.; Ngan, E. Conceptual Structure of Health-Related Quality of Life for Persons With Traumatic Brain Injury: Confirmatory Factor Analysis of the TBI-QOL. Arch. Phys. Med. Rehabil. 2020, 101, 62–71. [Google Scholar] [CrossRef]
- Harfmann, E.J.; deRoon-Cassini, T.A.; McCrea, M.A.; Nader, A.M.; Nelson, L.D. Comparison of Four Quality of Life Inventories for Patients with Traumatic Brain Injuries and Orthopedic Injuries. J. Neurotrauma 2020, 37, 1408–1417. [Google Scholar] [CrossRef]
- Nichol, A.D.; Higgins, A.M.; Gabbe, B.J.; Murray, L.J.; Cooper, D.J.; Cameron, P.A. Measuring Functional and Quality of Life Outcomes Following Major Head Injury: Common Scales and Checklists. Injury 2011, 42, 281–287. [Google Scholar] [CrossRef]
- von Steinbüchel, N.; Meeuwsen, M.; Zeldovich, M.; Vester, J.C.; Maas, A.; Koskinen, S.; Covic, A. Differences in Health-Related Quality of Life after Traumatic Brain Injury between Varying Patient Groups: Sensitivity of a Disease-Specific (QOLIBRI) and a Generic (SF-36) Instrument. J. Neurotrauma 2020, 37, 1242–1254. [Google Scholar] [CrossRef]
- Winter, V.; Powell, J.H.; Greenwood, R. The Problem of Quality of Life after Traumatic Brain Injury: Conceptual and Measurement Issues. Acta Neuropsychiatr. 2005, 3, 36–47. [Google Scholar]
- Wiebe, S.; Guyatt, G.; Weaver, B.; Matijevic, S.; Sidwell, C. Comparative Responsiveness of Generic and Specific Quality-of-Life Instruments. J. Clin. Epidemiol. 2003, 56, 52–60. [Google Scholar] [CrossRef] [PubMed]
- von Steinbuechel, N.; Covic, A.; Polinder, S.; Kohlmann, T.; Cepulyte, U.; Poinstingl, H.; Backhaus, J.; Bakx, W.; Bullinger, M.; Christensen, A.-L.; et al. Assessment of Health-Related Quality of Life after TBI: Comparison of a Disease-Specific (QOLIBRI) with a Generic (SF-36) Instrument. Behav. Neurol. 2016, 2016, 1–14. [Google Scholar] [CrossRef]
- von Steinbuechel, N.; Wilson, L.; Gibbons, H.; Hawthorne, G.; Höfer, S.; Schmidt, S.; Bullinger, M.; Maas, A.; Neugebauer, E.; Powell, J.; et al. Quality of Life after Brain Injury (QOLIBRI): Scale Development and Metric Properties. J. Neurotrauma 2010, 27, 1167–1185. [Google Scholar] [CrossRef] [PubMed]
- von Steinbüchel, N.; Wilson, L.; Gibbons, H.; Hawthorne, G.; Höfer, S.; Schmidt, S.; Bullinger, M.; Maas, A.; Neugebauer, E.; Powell, J.; et al. Quality of Life after Brain Injury (QOLIBRI): Scale Validity and Correlates of Quality of Life. J. Neurotrauma 2010, 27, 1157–1165. [Google Scholar] [CrossRef] [PubMed]
- Giustini, M.; Longo, E.; Azicnuda, E.; Silvestro, D.; D’Ippolito, M.; Rigon, J.; Cedri, C.; Bivona, U.; Barba, C.; Formisano, R. Health-Related Quality of Life after Traumatic Brain Injury: Italian Validation of the QOLIBRI. Funct. Neurol. 2014, 29, 167–176. [Google Scholar]
- von Steinbuechel, N.; Real, R.G.L.; Sasse, N.; Wilson, L.; Otto, C.; Mullins, R.; Behr, R.; Deinsberger, W.; Martinez-Olivera, R.; Puschendorf, W.; et al. German Validation of Quality of Life after Brain Injury (QOLIBRI) Assessment and Associated Factors. PLoS ONE 2017, 12, e0176668. [Google Scholar] [CrossRef] [PubMed]
- Gopaul, R.; Wei, Z.D.; Yan, J.; Gong, F.Y.; Xiao, S.W. Clinical Study of Quality of Life of Traumatic Brain Injury Patients after Decompressive Craniectomy and Related Influencing Factors. Chin. Neurosurg. J. 2016, 2, 33. [Google Scholar] [CrossRef]
- Voormolen, D.C.; Zeldovich, M.; Haagsma, J.A.; Polinder, S.; Friedrich, S.; Maas, A.I.R.; Wilson, L.; Steyerberg, E.W.; Covic, A.; Andelic, N.; et al. Outcomes after Complicated and Uncomplicated Mild Traumatic Brain Injury at Three-and Six-Months Post-Injury: Results from the CENTER-TBI Study. J. Clin. Med. 2020, 9, 1525. [Google Scholar] [CrossRef]
- Siponkoski, S.; Wilson, L.; Steinbüchel, N.; Sarajuuri, J.; Koskinen, S. Quality of Life after Traumatic Brain Injury: Finnish Experience of the QOLIBRI in Residential Rehabilitation. J. Rehabil. Med. 2013, 45, 835–842. [Google Scholar] [CrossRef]
- Hawthorne, G.; Kaye, A.H.; Gruen, R.; Houseman, D.; Bauer, I. Traumatic Brain Injury and Quality of Life: Initial Australian Validation of the QOLIBRI. J. Clin. Neurosci. 2011, 18, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Soberg, H.L.; Roe, C.; Brunborg, C.; von Steinbüchel, N.; Andelic, N. The Norwegian Version of the QOLIBRI – a Study of Metric Properties Based on a 12 Month Follow-up of Persons with Traumatic Brain Injury. Health Qual. Life Outcomes 2017, 15, 14. [Google Scholar] [CrossRef] [PubMed]
- Castaño-León, A.M.; Navarro-Main, B.; Gomez, P.A.; Gil, A.; Soler, M.D.; Lagares, A.; Bernabeu, M.v.; Steinbüchel, N.; Real, R.G.L. Quality of Life After Brain Injury: Psychometric Properties of the Spanish Translation of the QoLIBRI. Eval. Health Prof. 2018, 41, 456–473. [Google Scholar] [CrossRef] [PubMed]
- Steyerberg, E.W.; Wiegers, E.; Sewalt, C.; Buki, A.; Citerio, G.; De Keyser, V.; Ercole, A.; Kunzmann, K.; Lanyon, L.; Lecky, F.; et al. Case-Mix, Care Pathways, and Outcomes in Patients with Traumatic Brain Injury in CENTER-TBI: A European Prospective, Multicentre, Longitudinal, Cohort Study. Lancet Neurol. 2019, 18, 923–934. [Google Scholar] [CrossRef] [PubMed]
- Teasdale, G.; Jennett, B. Assessment of Coma and Impaired Consciousness. A Practical Scale. Lancet 1974, 2, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.T.L.; Pettigrew, L.E.L.; Teasdale, G. Structured Interviews for the Glasgow Outcome Scale and the Extended Glasgow Outcome Scale: Guidelines for Their Use. J. Neurotrauma 1998, 15, 573–585. [Google Scholar] [CrossRef]
- The Organisation for Economic Co-Operation and Development (OECD). Available online: https://stats.oecd.org/ (accessed on 1 March 2022).
- Population by Educational Attainment Level, Sex and Age (%)—Main Indicators. Eurostat. Available online: https://Ec.Europa.Eu/Eurostat/Databrowser/View/EDAT_LFSE_03/Default/Table?Lang=en (accessed on 25 September 2020).
- Gorbunova, A.; Zeldovich, M.; Voormolen, D.C.; Krenz, U.; Polinder, S.; Haagsma, J.A.; Hagmayer, Y.; Covic, A.; Real, R.G.L.; Asendorf, T.; et al. Reference Values of the QOLIBRI from General Population Samples in the United Kingdom and The Netherlands. J. Clin. Med. 2020, 9, 2100. [Google Scholar] [CrossRef]
- RCore, Team. R Version 4.0. 3: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Rosseel, Y. Lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- Jorgensen, T.D.; Pornprasertmanit, S.; Schoemann, A.M.; Rosseel, Y. SemTools: Useful Tools for Structural Equation Modeling. 2021. Available online: https://cran.r-project.org/web/packages/semTools/semTools.pdf (accessed on 1 July 2022).
- Bulmer, M.G. Principles of Statistics; Dover Publications: New York, NY, USA, 1979; ISBN 978-0-486-63760-0. [Google Scholar]
- The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF Quality of Life Assessment. Psychol. Med. 1998, 28, 551–558. [Google Scholar] [CrossRef]
- Wu, H.; Estabrook, R. Identification of Confirmatory Factor Analysis Models of Different Levels of Invariance for Ordered Categorical Outcomes. Psychometrika 2016, 81, 1014–1045. [Google Scholar] [CrossRef]
- Nestvold, K.; Stavem, K. Determinants of Health-Related Quality of Life 22 Years after Hospitalization for Traumatic Brain Injury. Brain Inj. 2009, 23, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Steadman-Pare, D.; Colantonio, A.; Ratcliff, G.; Chase, S.; Vernich, L. Factors Associated with Perceived Quality of Life Many Years after Traumatic Brain Injury. J. Head Trauma Rehabil. 2001, 16, 330–342. [Google Scholar] [CrossRef] [PubMed]
- Helmrich, I.R.A.R.; van Klaveren, D.; Dijkland, S.A.; Lingsma, H.F.; Polinder, S.; Wilson, L.; von Steinbuechel, N.; van der Naalt, J.; Maas, A.I.R.; Steyerberg, E.W.; et al. Development of Prognostic Models for Health-Related Quality of Life Following Traumatic Brain Injury. Qual. Life Res. 2021, 31, 451–471. [Google Scholar] [CrossRef] [PubMed]
- Michelson, H.; Bolund, C.; Brandberg, Y. Multiple Chronic Health Problems Are Negatively Associated with Health Related Quality of Life (HRQoL) Irrespective of Age. Qual. Life Res. 2000, 9, 1093–1104. [Google Scholar] [CrossRef] [PubMed]
- Megari, K. Quality of Life in Chronic Disease Patients. Heath Psychol. Res. 2013, 1, e27. [Google Scholar] [CrossRef]
- Wu, Y.-J.; Rauen, K.; Zeldovich, M.; Voormolen, D.C.; Covic, A.; Cunitz, K.; Plass, A.-M.; Polinder, S.; Haagsma, J.A.; von Steinbuechel, N. Reference Values and Psychometric Properties of the Quality of Life After Traumatic Brain Injury-Overall Scale in Italy, The Netherlands, and the United Kingdom. Value Health 2021, 24, 1319–1327. [Google Scholar] [CrossRef]
- Cronbach, L.J. Coefficient Alpha and the Internal Structure of Tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria versus New Alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Mikolic, A.; Groeniger, J.O.; Zeldovich, M.; Wilson, L.; von Lennep, J.R.; van Klaveren, D. Explaining Outcome Differences between Men and Women Following Mild Traumatic Brain Injury. J. Neurotrauma 2021, 38, 3315–3331. [Google Scholar] [CrossRef]
- Bazarian, J.J.; Blyth, B.; Mookerjee, S.; He, H.; McDermott, M.P. Sex Differences in Outcome after Mild Traumatic Brain Injury. J. Neurotrauma 2010, 27, 527–539. [Google Scholar] [CrossRef]
- Gupte, R.; Brooks, W.; Vukas, R.; Pierce, J.; Harris, J. Sex Differences in Traumatic Brain Injury: What We Know and What We Should Know. J. Neurotrauma 2019, 36, 3063–3091. [Google Scholar] [CrossRef] [PubMed]
- König, H.-H.; Bernert, S.; Angermeyer, M.C.; Matschinger, H.; Martinez, M.; Vilagut, G.; Haro, J.M.; de Girolamo, G.; de Graaf, R.; Kovess, V.; et al. Comparison of Population Health Status in Six European Countries: Results of a Representative Survey Using the EQ-5D Questionnaire. Med. Care 2009, 47, 255–261. [Google Scholar] [CrossRef]
- Gandek, B.; Ware, J.E.; Aaronson, N.K.; Apolone, G.; Bjorner, J.B.; Brazier, J.E.; Bullinger, M.; Kaasa, S.; Leplege, A.; Prieto, L.; et al. Cross-Validation of Item Selection and Scoring for the SF-12 Health Survey in Nine Countries: Results from the IQOLA Project. J. Clin. Epidemiol. 1998, 51, 1171–1178. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, S.; Debensason, D.; Mühlan, H.; Petersen, C.; Power, M.; Simeoni, M.C.; Bullinger, M. The DISABKIDS Generic Quality of Life Instrument Showed Cross-Cultural Validity. J. Clin. Epidemiol. 2006, 59, 587–598. [Google Scholar] [CrossRef] [PubMed]
- Alonso, J.; Ferrer, M.; Gandek, B.; Ware, J.E.; Aaronson, N.K.; Mosconi, P.; Rasmussen, N.K.; Bullinger, M.; Fukuhara, S.; Kaasa, S.; et al. Health-Related Quality of Life Associated with Chronic Conditions in Eight Countries: Results from the International Quality of Life Assessment (IQOLA) Project. Qual. Life Res. 2004, 13, 283–298. [Google Scholar] [CrossRef] [PubMed]
- Balestroni, G.; Bertolotti, G. EuroQol-5D (EQ-5D): An instrument for measuring quality of life. Monaldi Arch. Chest Dis. 2012, 78, 155–159. [Google Scholar] [CrossRef]
- Duke, J.; Leventhal, H.; Brownlee, S.; Leventhal, E.A. Giving Up and Replacing Activities in Response to Illness. J. Gerontol. B Psychol. Sci. Soc. Sci. 2002, 57, P367–P376. [Google Scholar] [CrossRef] [PubMed]
- Farace, E.; Alves, W.M. Do Women Fare Worse: A Metaanalysis of Gender Differences in Traumatic Brain Injury Outcome. J. Neurosurg. 2000, 93, 539–545. [Google Scholar] [CrossRef]
- Mushkudiani, N.A.; Engel, D.C.; Steyerberg, E.W.; Butcher, I.; Lu, J.; Marmarou, A.; Slieker, F.; McHugh, G.S.; Murray, G.D.; Maas, A.I.R. Prognostic Value of Demographic Characteristics in Traumatic Brain Injury: Results from The IMPACT Study. J. Neurotrauma 2007, 24, 259–269. [Google Scholar] [CrossRef]
- Cancelliere, C.; Donovan, J.; Cassidy, J.D. Is Sex an Indicator of Prognosis After Mild Traumatic Brain Injury: A Systematic Analysis of the Findings of the World Health Organization Collaborating Centre Task Force on Mild Traumatic Brain Injury and the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch. Phys. Med. Rehabil. 2016, 97, 5–18. [Google Scholar] [CrossRef]
- Wright, D.W.; Espinoza, T.R.; Merck, L.H.; Ratcliff, J.J.; Backster, A.; Stein, D.G. Gender Differences in Neurological Emergencies Part II: A Consensus Summary and Research Agenda on Traumatic Brain Injury. Acad. Emerg. Med. 2014, 21, 1414–1420. [Google Scholar] [CrossRef] [PubMed]
- Frost, R.B.; Farrer, T.J.; Primosch, M.; Hedges, D.W. Prevalence of Traumatic Brain Injury in the General Adult Population: A Meta-Analysis. Neuroepidemiology 2013, 40, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Levin, H.S.; Temkin, N.R.; Barber, J.; Nelson, L.D.; Robertson, C.; Brennan, J.; Stein, M.B.; Yue, J.K.; Giacino, J.T.; McCrea, M.A.; et al. Association of Sex and Age With Mild Traumatic Brain Injury–Related Symptoms: A TRACK-TBI Study. JAMA Netw. Open 2021, 4, e213046. [Google Scholar] [CrossRef] [PubMed]
- Scholten, A.C.; Haagsma, J.A.; Cnossen, M.C.; Olff, M.; van Beeck, E.F.; Polinder, S. Prevalence of and Risk Factors for Anxiety and Depressive Disorders after Traumatic Brain Injury: A Systematic Review. J. Neurotrauma 2016, 33, 1969–1994. [Google Scholar] [CrossRef] [PubMed]
- Kirkness, C.J.; Burr, R.L.; Mitchell, P.H.; Newell, D.W. Is There a Sex Difference in the Course Following Traumatic Brain Injury? Biol. Res. Nurs. 2004, 5, 299–310. [Google Scholar] [CrossRef]
- Styrke, J.; Sojka, P.; Björnstig, U.; Bylund, P.; Stålnacke, B. Sex-Differences in Symptoms, Disability, and Life Satisfaction Three Years after Mild Traumatic Brain Injury: A Population-Based Cohort Study. J. Rehabil. Med. 2013, 45, 749–757. [Google Scholar] [CrossRef]
- Tseng, H.-Y.; Löckenhoff, C.; Lee, C.-Y.; Yu, S.-H.; Wu, I.-C.; Chang, H.-Y.; Chiu, Y.-F.; Hsiung, C.A. The Paradox of Aging and Health-Related Quality of Life in Asian Chinese: Results from the Healthy Aging Longitudinal Study in Taiwan. BMC Geriatr. 2020, 20, 91. [Google Scholar] [CrossRef]
- Kempen, G.I.J.M.; Jelicic, M.; Ormel, J. Personality, Chronic Medical Morbidity, and Health-Related Quality of Life among Older Persons. Health Psychol. 1997, 16, 539–546. [Google Scholar] [CrossRef]
- Fortin, M.; Lapointe, L.; Hudon, C.; Vanasse, A.; Ntetu, A.L.; Maltais, D. Multimorbidity and Quality of Life in Primary Care: A Systematic Review. Health Qual. Life Outcomes 2004, 2, 51. [Google Scholar] [CrossRef]
- Chapman, B.; Duberstein, P.; Lyness, J.M. Personality Traits, Education, and Health-Related Quality of Life Among Older Adult Primary Care Patients. J. Gerontol. Ser. B 2007, 62, 343–352. [Google Scholar] [CrossRef]
- Verdugo, M.A.; Fernández, M.; Gómez, L.E.; Amor, A.M.; Aza, A. Predictive Factors of Quality of Life in Acquired Brain Injury. Int. J. Clin. Health Psychol. 2019, 19, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Forslund, M.V.; Roe, C.; Sigurdardottir, S.; Andelic, N. Predicting Health-Related Quality of Life 2 Years after Moderate-to-Severe Traumatic Brain Injury. Acta Neurol. Scand. 2013, 128, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Mirowsky, J.; Ross, C.E. Education, Social Status, and Health; Routledge: New York, NY, USA, 2017; ISBN 978-1-351-32808-1. [Google Scholar]
- Didsbury, M.S.; Kim, S.; Medway, M.M.; Tong, A.; McTaggart, S.J.; Walker, A.M.; White, S.; Mackie, F.E.; Kara, T.; Craig, J.C.; et al. Socio-Economic Status and Quality of Life in Children with Chronic Disease: A Systematic Review. J. Paediatr. Child Health 2016, 52, 1062–1069. [Google Scholar] [CrossRef] [PubMed]
- Adler, N.E.; Boyce, T.; Chesney, M.A.; Cohen, S.; Folkman, S.; Kahn, R.L.; Syme, S.L. Socioeconomic Status and Health: The Challenge of the Gradient. Am. Psychol. 1994, 49, 15–24. [Google Scholar] [CrossRef]
- Evans, J.R.; Mathur, A. The Value of Online Surveys: A Look Back and a Look Ahead. Internet Res. 2018, 28, 854–887. [Google Scholar] [CrossRef]
- Hoonakker, P.; Carayon, P. Questionnaire Survey Nonresponse: A Comparison of Postal Mail and Internet Surveys. Int. J. Hum.-Comput. Interact. 2009, 25, 348–373. [Google Scholar] [CrossRef]
- Ward, M.K.; Meade, A.W.; Allred, C.M.; Pappalardo, G.; Stoughton, J.W. Careless Response and Attrition as Sources of Bias in Online Survey Assessments of Personality Traits and Performance. Comput. Hum. Behav. 2017, 76, 417–430. [Google Scholar] [CrossRef]
- Shentu, Y.; Xie, M. A Note on Dichotomization of Continuous Response Variable in the Presence of Contamination and Model Misspecification. Stat. Med. 2010, 29, 2200–2214. [Google Scholar] [CrossRef]
- Royston, P.; Altman, D.G.; Sauerbrei, W. Dichotomizing Continuous Predictors in Multiple Regression: A Bad Idea. Stat. Med. 2006, 25, 127–141. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).