Abstract
A minority of patients with severe acute respiratory syndrome coronavirus 2 (COVID-19) develop cardiovascular complications, such as acute cardiac lesions with elevated troponins, de novo systolic heart failure, pericardial effusion and, rarely, acute myocarditis. The prevalence of COVID-19-related myocarditis ranges from 10 to 105 cases per 100,000 COVID-19-infected individuals, with a male predominance (58%) and a median age of 50 years. The etiopathogenetic mechanism is currently unclear, but may involve direct virus-mediated damage or an exaggerated immune response to the virus. Mortality is high, as fulminant myocarditis (FM) develops very often in the form of cardiogenic shock and ventricular arrhythmias. Hence, medical therapy with ACE inhibitors and beta-blockers may not always be sufficient, in which case inotropic and immunosuppressive drugs, most commonly corticosteroids, may be necessary. In this review we analyze the current data on COVID-19 myocarditis, management strategies and therapy, with a brief description of COVID-19 vaccine-associated myocarditis to help clinicians dealing with this peculiar form of myocarditis.
1. Introduction
CoronaVIrus Disease 19 (COVID-19) has emerged as a major cause of morbidity and mortality worldwide [1,2]. The range of its clinical presentations consists of cough, fever, fatigue, dyspnea, anosmia, ageusia, myalgia and pharyngodynia, but it may also dramatically evolve into acute respiratory distress and multiorgan failure [3,4]. Although COVID-19 has been primarily considered a respiratory disease [5], it is now recognized as a complex pathological condition that may involve several systems, including the cardiovascular system, which represents its second major target [6]. Among cardiac manifestations of COVID-19, acute myocarditis (AM) appears to be one of the most clinically significant, as it triggers a sudden deterioration of patients’ clinical status and may lead to death [7]. Indeed, in a large multinational registry of COVID-19 patients, an association was observed between myocarditis diagnosis and increased mortality [7]. Despite the clinical relevance of myocarditis, its incidence is still debated due to a high number of mildly symptomatic cases that might go undetected. Moreover, the pathogenesis is not completely understood.
Comprehensive management of COVID-19 associated myocarditis, from diagnostic tools to specific treatments, is crucial to avoid repercussions on patients’ health.
Therefore, the following narrative review aims to summarize the current literature on the relationship between COVID-19 and AM with regards to its epidemiology, pathogenetic mechanisms, diagnostic and prognostic features, and possible therapeutic approaches. The review also discusses SARS-CoV-2 vaccination-related AM. For our literature search, we used the following terms: “COVID-19 related myocarditis” or “Cardiovascular Sequelae of COVID-19” or “Post-Acute Sequelae of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)” or “COVID-19 and myocarditis” or “COVID-19–Associated Acute Myocarditis” and “COVID-19/myocarditis and SARS-CoV-2”. We included articles published from 2020 to 1 March 2023, in English, on both PubMed and MEDLINE. We reviewed original articles and meta-analyses and selected the most recent papers and those with the largest sample size. Reviews, consensus papers, and guidelines were included when deemed relevant and related to the topic.
2. Myocardial Injury during COVID-19 and COVID-19-Related Myocarditis: Epidemiological Aspects
According to the Fourth Universal Definition of Myocardial Infarction, acute myocardial injury (MI) is defined by a rise and/or fall of cardiac troponin (cTn) values with at least one value above the 99th percentile upper reference limit [8]. Conversely, AM is a disease characterized by a specific clinical presentation, with cardiac symptoms such as acute/new-onset chest pain or signs of left and/or right heart failure and/or unexplained arrhythmias or aborted sudden death, in addition to elevated cTn values and abnormal electrocardiographic/echocardiographic/cardiac magnetic resonance (CMR)/histopathologic findings, in the absence of coronary artery, valvular, or congenital heart disease [9]. MI is more common in COVID-19 patients than in patients with other severe diseases caused by different respiratory viruses [10]. It occurs in about 20% of hospitalized COVID-19 patients and in about 40–50% of critically ill COVID-19 patients [11,12]. A recent meta-analysis by Santoso et al., shows that MI is a frequent occurrence in COVID-19 and a poor prognostic factor, as it is associated with a higher risk of malignant arrhythmias, need for intensive care, shock, and death [13]. It is, therefore, crucial to recognize and diagnose it during COVID-19 in order to identify “high-risk” patients and limit its consequences on patients’ health [14]. According to the most recent data, the prevalence of myocarditis has been estimated to be about 2/100,000 patients [15]. Similar data found by Golpour et al. showed that the worldwide prevalence of AM ranges from 10 to 105 cases per 100,000 subjects depending on geographic differences and locally available diagnostics procedures [16]. The incidence and prevalence of COVID-19-related myocarditis is rarely investigated because of different—and often unclear—definitions and due to the lack of systematic data collection during the recent pandemic. According to a population-based analysis conducted by Singer et al. [17] involving young adults from 48 United States healthcare organizations, the incidence of myocarditis during SARS-CoV-2 infection amounted roughly to 45 per 100,000 patients. In a recent multinational, retrospective study by Ammirati et al. involving 23 cardiology centers, the estimated prevalence of COVID-19-related myocarditis was about two cases per 1000. Regardless of the context, SARS-CoV-2-related AM is more common in men [14,16,18,19].
3. Diagnostic Evaluation in COVID-19-Related Myocarditis
In most patients affected by COVID-19, AM occurs during the acute infection. Clinical presentation, electrocardiography, echocardiography, and laboratory tests, as well as cardiac magnetic resonance (CMR), are the cornerstone tools for diagnosis [20]. In patients affected by SARS-CoV-2 infection with a low clinical suspicion for cardiac involvement, no further cardiac testing is needed. Chest pain or discomfort, dyspnea, palpitations, and syncope are suggestive of cardiac involvement during COVID-19 [21]. In patients with symptoms indicative of cardiac involvement, a 12-lead electrocardiogram (ECG), an echocardiogram, and blood samples for cardiac troponin are indicated [21]. Electrocardiographic abnormalities in myocarditis are not pathognomonic, but sinus tachycardia, ectopic ventricular beats, ST segment elevation without reciprocal ST segment depression, diffuse T-wave inversion, QT interval prolongation, QRS prolongation, low voltages, atrioventricular block, bundle branch block and ventricular tachycardia may be present [22,23]. The most common electrocardiographic abnormalities are ST segment alterations and sinus tachycardia, which are both reported in 38% patients with COVID-19 related myocarditis. T wave abnormalities are described in about one fifth of patients with COVID-19 related myocarditis, whilst low QRS voltage or low QRS progression are reported only in 17% of patients. Ectopic rhythm origin and ventricular tachycardia are increasingly rare and reported respectively in 12% and 7% of patients affected by COVID-19 related myocarditis. In about 5% of patients, no pathological electrocardiographic features may be found [20].
Echocardiography is the first line imaging test in COVID-19 related myocarditis, with common echocardiographic alterations being regional hypokinesia (reported in 36% of patients), systolic dysfunction (reported in 83% of patients), left ventricular diastolic dysfunction, and impaired left ventricular myocardial deformation (abnormal ventricular strain) [24,25]. Pericardial effusion has been described in 29% of COVID-19-related myocarditis patients, while mitral or tricuspid regurgitation is reported in only 6% of patients [20]. Inflammatory markers, such as C-reactive protein (CRP), that is found to be increased in about 95% of patients with AM, as well as procalcitonin, ferritin, and interleukin-6, are usually elevated, together with the white blood cell count. Cardiac biomarkers, such as D-dimer, N-terminal brain natriuretic peptide (NT-pro-BNP) or brain natriuretic peptide (BNP), and cardiac troponins (cTn), are elevated in almost 95% of patients. Their rise is indicative of a hyperinflammatory state and is a surrogate of myocardial injury, suggesting a possible diagnosis of AM [20,26]. In such cases, additional tests can be used to rule out AM and/or to diagnose other pathological conditions, such as invasive coronary angiography (ICA) or computed tomography coronary angiography (CTCA) to exclude ischemic heart disease and computed tomography pulmonary angiography (CTPA) to exclude pulmonary embolism. If clinically stable COVID-19-related myocarditis is suspected, cardiac magnetic resonance (CMR) imaging should be considered in order to confirm the diagnosis of myocarditis or other myocardial (and pericardial) diseases [27]. The Lake Louise criteria for myocarditis have been fulfilled in about two-thirds of patients affected by COVID-19-related myocarditis [20]. Non-ischemic myocardial injury characterized by sub-epicardial or transmural late gadolinium enhancement (LGE) and myocardial edema are the most common CMR features observed in COVID-19-related myocarditis [28,29]. Endomyocardial biopsy (EMB) is considered the gold-standard for myocarditis diagnosis, but it is rarely used in clinical practice as it is an invasive procedure [30]. Moreover, it is associated with a high false-negative rate and a rate of complications of about 6% [31,32]. Hence, in cases of suspected COVID-19-related myocarditis, EBM should be considered only in hemodynamically unstable patients or those with rapid clinical deterioration after exclusion of coronary artery disease [21] (Table 1).

Table 1.
Comparison of patients’ features/ECG/echo findings at admission in patients affected by myocarditis according to a large recent registry and data available in patients affected by COVID-19-related myocarditis. ECG,—Electrocardiogram; LVEF—left ventricular ejection fraction.
4. Pathophysiology of COVID-19 Related Myocarditis
The pathogenesis of COVID-19-related myocarditis is currently unknown. Direct cardiac injury by SARS-CoV-2 has been hypothesized as studies have shown that the virus can bind its spike protein to angiotensin-converting enzyme 2 (ACE2) receptors on ciliated columnar epithelial cells of the respiratory tract, type II pneumocytes, and cardiomyocytes. Therefore, SARS-CoV-2 may directly infect the heart, especially in the setting of pre-existing heart failure, where ACE2 receptors are upregulated, despite the presence of viral receptors not being accurate predictors of tropism [33]. The binding between the spike protein and ACE2 leads to apoptosis and to the release of viral and cardiac antigens. These antigens, in turn, cause the release of interleukins (IL-1, IL-6, IL-12, TNF-alpha) that might activate T lymphocytes and increase myocardial damage through cell-mediated cytotoxicity, leading to a vicious cycle of immune activation and myocardial injury [34]. However, currently available data suggest other hypotheses since myocardial biopsies in patients with COVID-19-related myocarditis have rarely documented viral presence in cardiac cells [14,35]. In most cases, an infiltration with interstitial macrophages and more rarely lymphocytes have been found [36,37]. Therefore, it seems reasonable that COVID-19 could trigger AM through a non-specific innate and/or adaptive immune response in genetically susceptible patients [38]. A recent analysis showed an increased risk of arrhythmias and myocarditis up to 12 months after infection [39,40]. Therefore, a third hypothesis of a molecular mimicry between viral proteins and cardiomyocytes has been developed. This latter might require a longer time between exposure to the virus and the development of cardiac damage. In conclusion, given the paucity of published data and the heterogeneous results, the mechanisms through which SARS-CoV-2 can induce myocardial damage and inflammation are yet to be outlined (Figure 1)
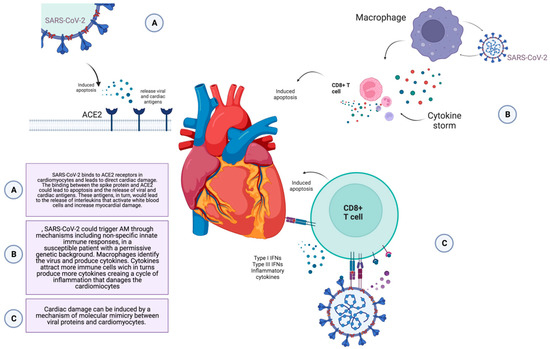
Figure 1.
Potential pathogenetic mechanisms involved in COVID-19 related myocarditis. ACE 2—the angiotensin-converting enzyme 2 receptors. Created with Biorender.com, accessed on 23 April 2023.
5. Prognosis of COVID-19 Related Myocarditis
Previous reports, such as the Lombardy registry on non-COVID-19-related myocarditis, found that fulminant myocarditis (FM) accounted for 8.3% of cases [14,41], whereas in a multicentre study conducted by Ammirati et al., a high percentage (38.9%) of patients with COVID-19-associated myocarditis had FM (cardiogenic shock and arrhythmias) [14]. A recent registry report confirmed gigantocellular myocarditis as having the highest mortality or need for HTx (81% at 3-year follow-up), followed by eosinophilic myocarditis in the context of systemic inflammatory diseases or drug allergies such as DRESS (drug rash with eosinophilia and systemic symptoms). Lymphocytic FM also proved to be a high-risk condition, with a death or HTx rate of 19.5% at 60 days and 40% at 3 years [42]. Its cause is often viral, as shown by a systematic review that showed that AM from influenza viruses was associated with an overall mortality rate of 14.7% [43]. Patients with COVID-19-associated myocarditis had a higher mortality rate; in fact, 18.5% of patients with FM and cardiogenic shock required temporary mechanical circulatory support (t-MCS). According to the available evidence, left ventricular EF is frequently low on the first echocardiogram, and the evolution to a fulminant form is not related to the presence of pneumonia [14]. This is of particular interest, since the severity of myocarditis triggered by SARS-CoV-2 seems also to be independent from the occurrence of viral pneumonia, despite patients with associated pneumonia usually having a worse prognosis [14]. In a review of 38 published cases of suspected myocarditis with COVID-19, the mortality rate was very high (13.8%), although there may be a publication bias that led to an overestimation of mortality [26]. However, the high mortality rate may also be explained by milder forms of AM being underestimated, unrecognized, and/or not attributed to COVID-19. In this regard, in two studies that evaluated cardiac involvement in athletes with COVID-19, myocarditis was often asymptomatic or paucisymptomatic and in a mild form (the lowest EF found at CMR was 41%). After several months of follow-up, none of the patients had any adverse cardiac events [18,44]. Further studies providing more information on both in-hospital and long-term mortality and cardiovascular complications are required.
6. Treatment of COVID-19 Related Myocarditis
No randomized controlled trials have tested specific therapies for AM associated with COVID-19, with the available data being based on observational studies. In general, the management is the same as that of heart failure, including pharmacological therapy, fluid management, and advanced therapies in cases of unresponsive or cardiogenic shock [45]. The use of angiotensin-converting enzyme inhibitors (ACE-I) or angiotensin receptor blockers (ARB) together with mineralocorticoid receptor antagonists (MRA) is considered to be a part of the management of patients affected by COVID-19-related myocarditis [46]. The same applies to beta-blockers (BBs), which are indicated for their anti-arrhythmic effect, especially in the presence of reduced EF. From the data of the Lombardy registry, BBs were among the most prescribed drugs in patients with AM regardless of etiology [41], and in the study conducted by Ammirati et al., BBs were also used in 55.5% of patients [14].
This analysis also showed a high number of FM requiring inotropes and/or vasopressors (38.9%). Immunosuppressive therapies were used in 59.2% of cases, with a high prevalence of intravenous corticosteroid use, independently from the presence or absence of pneumonia (43.4% and 48.3%, respectively (p = 0.79)). In some cases, a combination of corticosteroids and intravenous immunoglobulins (IVIG) or tocilizumab was used, while IVIG alone was administered in only two patients [14]. The clinical benefit of corticosteroids in hospitalized patients with COVID-19 has now been shown in some trials, but in the specific context of AM data are lacking [47,48,49]. Small case series have shown a favorable prognosis associated with the use of intravenous corticosteroids in adults with COVID-19 multisystem inflammatory syndrome (MIS) and myocarditis [39,48]. Several immunosuppressive therapies, such as interleukin-1 (anakinra and canakinumab) and interleukin-6 (tocilizumab and sarilumab) antagonists, have demonstrated promising results in selected patients hospitalized for COVID-19 [50,51,52,53]. However, none of these drugs have been investigated specifically for COVID-19-related myocarditis. In summary, corticosteroids may be a choice in hospitalized patients with myocarditis and COVID-19, regardless of pneumonia and hypoxemia, but should be avoided in less severe forms [45].
7. Update of Myocarditis after SARS-CoV-2 Vaccination
In the past, vaccination-associated myocarditis was a very rare adverse event that occurred following the administration of the smallpox attenuated virus vaccine and, less commonly, after other vaccines, such as those for diphtheria, tetanus, polio, influenza and hepatitis B [54]. With the implementation of the COVID-19 vaccination campaign, several countries introduced reporting systems for vaccine-adverse events, such as VAERS that monitored outcomes in approximately 200 million individuals in the United States. Using data from this large database, a small but stable rate of patients presented with post-vaccination myocarditis and/or pericarditis. By June 2021, a total of 1226 cases of suspected vaccine-associated pericarditis and myocarditis had been recorded in VAERS, with 40% of the events having occurred in individuals aged ≤30 years [55]. Of these, 323 reports were confirmed by CDC (Centers for Disease Control and Prevention) [56]. The estimated rate of myocarditis/pericarditis in subjects aged <30 years after receiving the second dose of the mRNA vaccine was approximately 40 cases per million among men and 4.2 cases per million among women. When considering the age group ≥ 30 years, these rates were significantly reduced to 2.4 and 1.0 per million in men and women, respectively [57]. The most recent US data showed that incidence peaks in young males aged 15–17 years, with 105.9 cases per million doses administered, and identified the second dose as being associated with the highest risk [54]. The true incidence of vaccination-related myocarditis is unknown, as available reports only refer to symptomatic patients. To estimate the true incidence, a systematic evaluation by means of instrumental and laboratory examinations should be performed in a larger population of individuals who have received the vaccine [57]. Reports about myocarditis after SARS-CoV-2 vaccination are heterogeneous due to different inclusion criteria in studies, different characteristics (age, sex, etc.) of the subjects, different criteria to diagnose post-vaccination myocarditis, different types and doses of vaccines, and different follow-up periods after vaccination. Simone et al. found post-vaccination myocarditis to be a very rare event (0.58 per 100,000 individuals vaccinated with a second dose) in a multiethnic population (31.2% “White”, 6.7% “Black”, 37.8% “Hispanic”, 14.3% “Asian”) after a follow-up of 10 days from the second dose [58]. From a review of 90 cases published in the literature [59], the median age was 25 years (interquartile range 17–27)—comparable to that observed in VAERS [60]—and with a marked male prevalence (93%). In most subjects, myocarditis occurred after the second dose, with a mean time of 3 days between the last dose and the onset of symptoms. These results suggested an immune-mediated reaction to vaccine administration [54]. Indeed, the proposed mechanisms by which SARS-CoV-2 vaccines could induce myocarditis might involve the activation of both innate and adaptive immune responses against the SARS-CoV-2 spike glycoprotein, but also the recognition of the mRNA itself as an antigen by the immune system [55]. Since, like other viral myocarditis, post-vaccine myocarditis occurs predominantly in young men, sex hormones may play a role in genetically susceptible individuals. With regards to the clinical presentation, the most frequent symptom was chest pain (in 96% of cases) generally preceded by fever (in 85%). The ECG was altered (mild, diffuse ST-segment changes, PQ-segment depressions or non-specific ST-segment changes) in 77% of patients, while the echocardiogram showed only a slight reduction in left ventricular EF (mean EF of 53%), with pericardial effusion in less than one third of patients [60]. CMR was often altered, with a pattern suggestive of myocarditis (according to the updated Lake Louise Criteria). EBM was rarely performed, most often with negative or non-specific histological findings [61,62,63,64,65]. Concerning therapy, non-steroidal anti-inflammatory drugs (NSAIDs) were most commonly used, followed by corticosteroids and, in a smaller percentage, by IVIG. Colchicine and anakinra were rarely used. In most cases, immunosuppressive agents were used in combination [61]. The prognosis is generally favorable. In a case series of 139 adolescents (all <21 years of age) with suspected myocarditis within 30 days of COVID-19 vaccination, none died or required t-MCS. No patients had cardiac events at 6 months of follow-up [66]. An analysis of the Israeli “Clalit Health Services” registry compared a cohort of over 800,000 BNT162b2 (Pfizer) mRNA-vaccinated individuals aged 16 years and older with an unvaccinated cohort of patients with SARS-CoV-2 infection documented by polymerase viral chain reaction (PCR). The cohorts were followed up for 42 days, starting on the day of administration of the first dose of COVID-19 vaccine. The cohort of unvaccinated SARS-CoV-2 infected patients experienced a significantly higher risk of myocarditis than the cohort of BNT162b2 mRNA-vaccinated subjects in the order of 11 cases vs. 2.7 cases per 100,000 individuals, respectively. In addition, the vaccinated cohort developed a mild and rapidly resolving myocarditis, whereas the unvaccinated cohort had an increased risk of other serious cardiac complications, such as arrhythmias and myocardial infarction. Despite its limitations, the results showed a risk-benefit profile strongly in favor of vaccination against COVID-19 [67] (Figure 2).
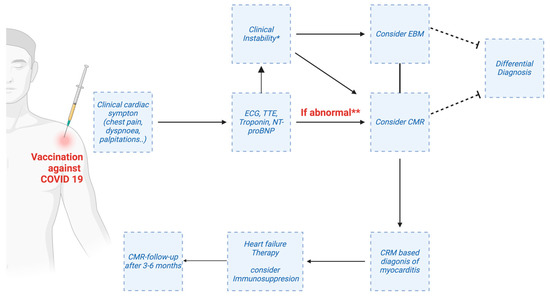
Figure 2.
Potential workflow for the use of advanced cardiac magnetic resonance (CMR) in patients post-vaccination and suspected myo-/pericarditis. ECG—electrocardiogram; EBM—endomyocardial biopsy; NT-proBNP—N-terminal pro-B-type natriuretic peptide; TTE—transthoracic echocardiography. * e.g., Severe arrhythmias, worsening heart failure. ** always rule out other causes of troponin elevation (e.g., myocardial infarction, pulmonary embolism.). Created with Biorender.com.
8. Conclusions
Although AM is not a frequent complication of COVID-19 infection, it is associated with a significant increase in morbidity and mortality. Its incidence is likely to be underestimated as there is no uniformity in diagnostic criteria. A central role in diagnosis is played by CMR and, where necessary, also by EMB. Currently, the management of SARS-CoV-2 myocarditis follows standard guidelines for heart failure, and immunosuppressive drugs have often been used with encouraging results. The use of corticosteroids, at least in severe forms, is still debated. Further studies are needed to fully understand the pathophysiological mechanisms and thus choose the most appropriate therapy. Although we have no long-term data, COVID-19 vaccine-associated myocarditis, on the other hand, is a rare, self-limiting event with a favorable prognosis. This confirms the benefits of COVID-19 vaccination over the risks associated with infection.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Chang, D.; Chang, X.; He, Y.; Tan, K.J.K. The Determinants of COVID-19 Morbidity and Mortality across Countries. Sci. Rep. 2022, 12, 5888. [Google Scholar] [CrossRef] [PubMed]
- Flaxman, S.; Whittaker, C.; Semenova, E.; Rashid, T.; Parks, R.M.; Blenkinsop, A.; Unwin, H.J.T.; Mishra, S.; Bhatt, S.; Gurdasani, D.; et al. Assessment of COVID-19 as the Underlying Cause of Death Among Children and Young People Aged 0 to 19 Years in the US. JAMA Netw. Open 2023, 6, e2253590. [Google Scholar] [CrossRef] [PubMed]
- Vihta, K.D.; Pouwels, K.B.; Peto, T.E.A.; Pritchard, E.; Eyre, D.W.; House, T.; Gethings, O.; Studley, R.; Rourke, E.; Cook, D.; et al. Symptoms and Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Positivity in the General Population in the United Kingdom. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2022, 75, e329–e337. [Google Scholar] [CrossRef]
- Baj, J.; Karakuła-Juchnowicz, H.; Teresiński, G.; Buszewicz, G.; Ciesielka, M.; Sitarz, R.; Forma, A.; Karakuła, K.; Flieger, W.; Portincasa, P.; et al. COVID-19: Specific and Non-Specific Clinical Manifestations and Symptoms: The Current State of Knowledge. J. Clin. Med. 2020, 9, 1753. [Google Scholar] [CrossRef]
- Brosnahan, S.B.; Jonkman, A.H.; Kugler, M.C.; Munger, J.S.; Kaufman, D.A. COVID-19 and Respiratory System Disorders. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 2586–2597. [Google Scholar] [CrossRef] [PubMed]
- Sagris, M.; Theofilis, P.; Antonopoulos, A.S.; Tsioufis, C.; Oikonomou, E.; Antoniades, C.; Crea, F.; Kaski, J.C.; Tousoulis, D. Inflammatory Mechanisms in COVID-19 and Atherosclerosis: Current Pharmaceutical Perspectives. Int. J. Mol. Sci. 2021, 22, 6607. [Google Scholar] [CrossRef]
- Annie, F.H.; Alkhaimy, H.; Nanjundappa, A.; Elashery, A. Association Between Myocarditis and Mortality in COVID-19 Patients in a Large Registry. Mayo Clin. Proc. Innov. Qual. Outcomes 2022, 6, 114–119. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. ESC Scientific Document Group Fourth Universal Definition of Myocardial Infarction (2018). Eur. Heart J. 2019, 40, 237–269. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Cheng, M.P.; Cau, A.; Lee, T.C.; Brodie, D.; Slutsky, A.; Marshall, J.; Murthy, S.; Lee, T.; Singer, J.; Demir, K.K.; et al. Acute Cardiac Injury in Coronavirus Disease 2019 and Other Viral Infections-A Systematic Review and Meta-Analysis. Crit. Care Med. 2021, 49, 1558–1566. [Google Scholar] [CrossRef]
- Abate, S.M.; Mantefardo, B.; Nega, S.; Chekole, Y.A.; Basu, B.; Ali, S.A.; Taddesse, M. Global Burden of Acute Myocardial Injury Associated with COVID-19: A Systematic Review, Meta-Analysis, and Meta-Regression. Ann. Med. Surg. 2021, 68, 102594. [Google Scholar] [CrossRef] [PubMed]
- Italia, L.; Tomasoni, D.; Bisegna, S.; Pancaldi, E.; Stretti, L.; Adamo, M.; Metra, M. COVID-19 and Heart Failure: From Epidemiology During the Pandemic to Myocardial Injury, Myocarditis, and Heart Failure Sequelae. Front. Cardiovasc. Med. 2021, 8, 713560. [Google Scholar] [CrossRef] [PubMed]
- Santoso, A.; Pranata, R.; Wibowo, A.; Al-Farabi, M.J.; Huang, I.; Antariksa, B. Cardiac Injury Is Associated with Mortality and Critically Ill Pneumonia in COVID-19: A Meta-Analysis. Am. J. Emerg. Med. 2021, 44, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Ammirati, E.; Lupi, L.; Palazzini, M.; Hendren, N.S.; Grodin, J.L.; Cannistraci, C.V.; Schmidt, M.; Hekimian, G.; Peretto, G.; Bochaton, T.; et al. Prevalence, Characteristics, and Outcomes of COVID-19-Associated Acute Myocarditis. Circulation 2022, 145, 1123–1139. [Google Scholar] [CrossRef]
- Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 301 Acute and Chronic Diseases and Injuries in 188 Countries, 1990–2013: A Systematic Analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 743–800. [CrossRef]
- Golpour, A.; Patriki, D.; Hanson, P.J.; McManus, B.; Heidecker, B. Epidemiological Impact of Myocarditis. J. Clin. Med. 2021, 10, 603. [Google Scholar] [CrossRef]
- Singer, M.E.; Taub, I.B.; Kaelber, D.C. Risk of Myocarditis from COVID-19 Infection in People Under Age 20: A Population-Based Analysis. medRxiv 2022. [Google Scholar] [CrossRef]
- Moulson, N.; Petek, B.J.; Drezner, J.A.; Harmon, K.G.; Kliethermes, S.A.; Patel, M.R.; Baggish, A.L.; Outcomes Registry for Cardiac Conditions in Athletes Investigators. SARS-CoV-2 Cardiac Involvement in Young Competitive Athletes. Circulation 2021, 144, 256–266. [Google Scholar] [CrossRef]
- Theocharis, P.; Wong, J.; Pushparajah, K.; Mathur, S.K.; Simpson, J.M.; Pascall, E.; Cleary, A.; Stewart, K.; Adhvaryu, K.; Savis, A.; et al. Multimodality Cardiac Evaluation in Children and Young Adults with Multisystem Inflammation Associated with COVID-19. Eur. Heart J. Cardiovasc. Imaging 2021, 22, 896–903. [Google Scholar] [CrossRef]
- Urban, S.; Fułek, M.; Błaziak, M.; Iwanek, G.; Jura, M.; Fułek, K.; Guzik, M.; Garus, M.; Gajewski, P.; Lewandowski, Ł.; et al. COVID-19 Related Myocarditis in Adults: A Systematic Review of Case Reports. J. Clin. Med. 2022, 11, 5519. [Google Scholar] [CrossRef]
- Gluckman, T.J.; Bhave, N.M.; Allen, L.A.; Chung, E.H.; Spatz, E.S.; Ammirati, E.; Baggish, A.L.; Bozkurt, B.; Cornwell, W.K.; Harmon, K.G.; et al. 2022 ACC Expert Consensus Decision Pathway on Cardiovascular Sequelae of COVID-19 in Adults: Myocarditis and Other Myocardial Involvement, Post-Acute Sequelae of SARS-CoV-2 Infection, and Return to Play: A Report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 2022, 79, 1717–1756. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Chen, S.; Li, Z.; Zhou, P.; Huang, W.; Wang, H.; Shi, J.; Ni, Y.; Lin, L.; Lei, Y. Role of Electrocardiograms in Assessment of Severity and Analysis of the Characteristics of ST Elevation in Acute Myocarditis: A Two-Centre Study. Exp. Ther. Med. 2020, 20, 20. [Google Scholar] [CrossRef] [PubMed]
- Buttà, C.; Zappia, L.; Laterra, G.; Roberto, M. Diagnostic and Prognostic Role of Electrocardiogram in Acute Myocarditis: A Comprehensive Review. Ann. Noninvasive Electrocardiol. 2020, 25, e12726. [Google Scholar] [CrossRef]
- Carrizales-Sepúlveda, E.F.; Vera-Pineda, R.; Flores-Ramírez, R.; Hernández-Guajardo, D.A.; Pérez-Contreras, E.; Lozano-Ibarra, M.M.; Ordaz-Farías, A. Echocardiographic Manifestations in COVID-19: A Review. Heart Lung Circ. 2021, 30, 1117–1129. [Google Scholar] [CrossRef]
- Fayol, A.; Livrozet, M.; Boutouyrie, P.; Khettab, H.; Betton, M.; Tea, V.; Blanchard, A.; Bruno, R.-M.; Hulot, J.-S.; French COVID Cohort Study Group. Cardiac Performance in Patients Hospitalized with COVID-19: A 6 Month Follow-up Study. ESC Heart Fail. 2021, 8, 2232–2239. [Google Scholar] [CrossRef] [PubMed]
- Castiello, T.; Georgiopoulos, G.; Finocchiaro, G.; Claudia, M.; Gianatti, A.; Delialis, D.; Aimo, A.; Prasad, S. COVID-19 and Myocarditis: A Systematic Review and Overview of Current Challenges. Heart Fail. Rev. 2022, 27, 251–261. [Google Scholar] [CrossRef]
- Petersen, S.E.; Friedrich, M.G.; Leiner, T.; Elias, M.D.; Ferreira, V.M.; Fenski, M.; Flamm, S.D.; Fogel, M.; Garg, R.; Halushka, M.K.; et al. Cardiovascular Magnetic Resonance for Patients With COVID-19. JACC Cardiovasc. Imaging 2022, 15, 685–699. [Google Scholar] [CrossRef]
- Peretto, G.; Sala, S.; Caforio, A.L.P. Acute Myocardial Injury, MINOCA, or Myocarditis? Improving Characterization of Coronavirus-Associated Myocardial Involvement. Eur. Heart J. 2020, 41, 2124–2125. [Google Scholar] [CrossRef]
- Cooper, L.T.; Keren, A.; Sliwa, K.; Matsumori, A.; Mensah, G.A. The Global Burden of Myocarditis: Part 1: A Systematic Literature Review for the Global Burden of Diseases, Injuries, and Risk Factors 2010 Study. Glob. Heart 2014, 9, 121–129. [Google Scholar] [CrossRef]
- Caforio, A.L.P.; Pankuweit, S.; Arbustini, E.; Basso, C.; Gimeno-Blanes, J.; Felix, S.B.; Fu, M.; Heliö, T.; Heymans, S.; Jahns, R.; et al. Current State of Knowledge on Aetiology, Diagnosis, Management, and Therapy of Myocarditis: A Position Statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 2013, 34, 2636–2648. [Google Scholar] [CrossRef]
- From, A.M.; Maleszewski, J.J.; Rihal, C.S. Current Status of Endomyocardial Biopsy. Mayo Clin. Proc. 2011, 86, 1095–1102. [Google Scholar] [CrossRef] [PubMed]
- Cooper, L.T.; Baughman, K.L.; Feldman, A.M.; Frustaci, A.; Jessup, M.; Kuhl, U.; Levine, G.N.; Narula, J.; Starling, R.C.; Towbin, J.; et al. The Role of Endomyocardial Biopsy in the Management of Cardiovascular Disease: A Scientific Statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Endorsed by the Heart Failure Society of America and the Heart Failure Association of the European Society of Cardiology. J. Am. Coll. Cardiol. 2007, 50, 1914–1931. [Google Scholar] [CrossRef] [PubMed]
- Siripanthong, B.; Nazarian, S.; Muser, D.; Deo, R.; Santangeli, P.; Khanji, M.Y.; Cooper, L.T.; Chahal, C.A.A. Recognizing COVID-19-Related Myocarditis: The Possible Pathophysiology and Proposed Guideline for Diagnosis and Management. Heart Rhythm 2020, 17, 1463–1471. [Google Scholar] [CrossRef] [PubMed]
- Jaiswal, V.; Sarfraz, Z.; Sarfraz, A.; Mukherjee, D.; Batra, N.; Hitawala, G.; Yaqoob, S.; Patel, A.; Agarwala, P.; Ruchika; et al. COVID-19 Infection and Myocarditis: A State-of-the-Art Systematic Review. J. Prim. Care Community Health 2021, 12, 21501327211056800. [Google Scholar] [CrossRef]
- Escher, F.; Pietsch, H.; Aleshcheva, G.; Bock, T.; Baumeier, C.; Elsaesser, A.; Wenzel, P.; Hamm, C.; Westenfeld, R.; Schultheiss, M.; et al. Detection of Viral SARS-CoV-2 Genomes and Histopathological Changes in Endomyocardial Biopsies. ESC Heart Fail. 2020, 7, 2440–2447. [Google Scholar] [CrossRef] [PubMed]
- Basso, C.; Leone, O.; Rizzo, S.; De Gaspari, M.; van der Wal, A.C.; Aubry, M.-C.; Bois, M.C.; Lin, P.T.; Maleszewski, J.J.; Stone, J.R. Pathological Features of COVID-19-Associated Myocardial Injury: A Multicentre Cardiovascular Pathology Study. Eur. Heart J. 2020, 41, 3827–3835. [Google Scholar] [CrossRef]
- Greulich, S.; Klingel, K. COVID-19 and Myocarditis: Findings from Cardiac Magnetic Resonance Imaging and Endomyocardial Biopsies. Hamostaseologie 2021, 41, 366–370. [Google Scholar] [CrossRef]
- Yu, Y.; Xu, D.; Fu, S.; Zhang, J.; Yang, X.; Xu, L.; Xu, J.; Wu, Y.; Huang, C.; Ouyang, Y.; et al. Patients with COVID-19 in 19 ICUs in Wuhan, China: A Cross-Sectional Study. Crit. Care 2020, 24, 219. [Google Scholar] [CrossRef]
- Bajaj, R.; Sinclair, H.C.; Patel, K.; Low, B.; Pericao, A.; Manisty, C.; Guttmann, O.; Zemrak, F.; Miller, O.; Longhi, P.; et al. Delayed-Onset Myocarditis Following COVID-19. Lancet Respir. Med. 2021, 9, e32–e34. [Google Scholar] [CrossRef]
- Xie, Y.; Xu, E.; Bowe, B.; Al-Aly, Z. Long-Term Cardiovascular Outcomes of COVID-19. Nat. Med. 2022, 28, 583–590. [Google Scholar] [CrossRef]
- Ammirati, E.; Cipriani, M.; Moro, C.; Raineri, C.; Pini, D.; Sormani, P.; Mantovani, R.; Varrenti, M.; Pedrotti, P.; Conca, C.; et al. Clinical Presentation and Outcome in a Contemporary Cohort of Patients With Acute Myocarditis: Multicenter Lombardy Registry. Circulation 2018, 138, 1088–1099. [Google Scholar] [CrossRef]
- Ammirati, E.; Veronese, G.; Bottiroli, M.; Wang, D.W.; Cipriani, M.; Garascia, A.; Pedrotti, P.; Adler, E.D.; Frigerio, M. Update on acute myocarditis. Trends Cardiovasc. Med. 2020, 31, 370–379. [Google Scholar] [CrossRef]
- Radovanovic, M.; Petrovic, M.; Barsoum, M.K.; Nordstrom, C.W.; Calvin, A.D.; Dumic, I.; Jevtic, D.; Hanna, R.D. Influenza Myopericarditis and Pericarditis: A Literature Review. J. Clin. Med. 2022, 11, 4123. [Google Scholar] [CrossRef] [PubMed]
- Martinez, M.W.; Tucker, A.M.; Bloom, O.J.; Green, G.; DiFiori, J.P.; Solomon, G.; Phelan, D.; Kim, J.H.; Meeuwisse, W.; Sills, A.K.; et al. Prevalence of Inflammatory Heart Disease Among Professional Athletes With Prior COVID-19 Infection Who Received Systematic Return-to-Play Cardiac Screening. JAMA Cardiol. 2021, 6, 745–752. [Google Scholar] [CrossRef]
- Abou Hassan, O.K.; Sheng, C.C.; Wang, T.K.M.; Cremer, P.C. SARS-CoV-2 Myocarditis: Insights Into Incidence, Prognosis, and Therapeutic Implications. Curr. Cardiol. Rep. 2021, 23, 129. [Google Scholar] [CrossRef]
- The Writing Committee for the REMAP-CAP Investigators. Effect of Hydrocortisone on Mortality and Organ Support in Patients With Severe COVID-19: The REMAP-CAP COVID-19 Corticosteroid Domain Randomized Clinical Trial. JAMA 2020, 324, 1317–1329. [Google Scholar] [CrossRef]
- Chau, V.Q.; Giustino, G.; Mahmood, K.; Oliveros, E.; Neibart, E.; Oloomi, M.; Moss, N.; Mitter, S.S.; Contreras, J.P.; Croft, L.; et al. Cardiogenic Shock and Hyperinflammatory Syndrome in Young Males With COVID-19. Circ. Heart Fail. 2020, 13, e007485. [Google Scholar] [CrossRef] [PubMed]
- Dequin, P.-F.; Heming, N.; Meziani, F.; Plantefève, G.; Voiriot, G.; Badié, J.; François, B.; Aubron, C.; Ricard, J.-D.; Ehrmann, S.; et al. Effect of Hydrocortisone on 21-Day Mortality or Respiratory Support Among Critically Ill Patients With COVID-19: A Randomized Clinical Trial. JAMA 2020, 324, 1298–1306. [Google Scholar] [CrossRef]
- Dexamethasone in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [CrossRef] [PubMed]
- Cavalli, G.; De Luca, G.; Campochiaro, C.; Della-Torre, E.; Ripa, M.; Canetti, D.; Oltolini, C.; Castiglioni, B.; Tassan Din, C.; Boffini, N.; et al. Interleukin-1 Blockade with High-Dose Anakinra in Patients with COVID-19, Acute Respiratory Distress Syndrome, and Hyperinflammation: A Retrospective Cohort Study. Lancet Rheumatol. 2020, 2, e325–e331. [Google Scholar] [CrossRef]
- Gordon, A.C.; Mouncey, P.R.; Al-Beidh, F.; Rowan, K.M.; Nichol, A.D.; Arabi, Y.M.; Annane, D.; Beane, A.; Van Bentum-Puijk, W.; Berry, L.R.; et al. Interleukin-6 Receptor Antagonists in Critically Ill Patients with COVID-19. N. Engl. J. Med. 2021, 384, 1491–1502. [Google Scholar] [CrossRef] [PubMed]
- Ucciferri, C.; Auricchio, A.; Di Nicola, M.; Potere, N.; Abbate, A.; Cipollone, F.; Vecchiet, J.; Falasca, K. Canakinumab in a Subgroup of Patients with COVID-19. Lancet Rheumatol. 2020, 2, e457–e458. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Wang, W.; Hayek, S.S.; Chan, L.; Mathews, K.S.; Melamed, M.L.; Brenner, S.K.; Leonberg-Yoo, A.; Schenck, E.J.; Radbel, J.; et al. Association Between Early Treatment With Tocilizumab and Mortality Among Critically Ill Patients With COVID-19. JAMA Intern. Med. 2021, 181, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Heidecker, B.; Dagan, N.; Balicer, R.; Eriksson, U.; Rosano, G.; Coats, A.; Tschöpe, C.; Kelle, S.; Poland, G.A.; Frustaci, A.; et al. Myocarditis Following COVID-19 Vaccine: Incidence, Presentation, Diagnosis, Pathophysiology, Therapy, and Outcomes Put into Perspective. A Clinical Consensus Document Supported by the Heart Failure Association of the European Society of Cardiology (ESC) and the ESC Working Group on Myocardial and Pericardial Diseases. Eur. J. Heart Fail. 2022, 24, 2000–2018. [Google Scholar] [CrossRef]
- VAERS—Guide to Interpreting VAERS Data. Available online: https://vaers.hhs.gov/data/dataguide.html (accessed on 21 May 2023).
- Gargano, J.W. Use of MRNA COVID-19 Vaccine After Reports of Myocarditis Among Vaccine Recipients: Update from the Advisory Committee on Immunization Practices—United States, June 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 977–982. [Google Scholar] [CrossRef]
- Sinagra, G.; Porcari, A.; Merlo, M.; Barillà, F.; Basso, C.; Ciccone, M.M.; Curcio, A.; Mancone, M.; Mercuro, G.; Muscoli, S.; et al. Myocarditis and pericarditis following mRNA COVID-19 vaccination. Expert opinion of the Italian Society of Cardiology. G. Ital. Cardiol. (2006) 2021, 22, 894–899. [Google Scholar] [CrossRef]
- Sinagra, G.; Porcari, A.; Merlo, M.; Fabris, E.; Imazio, M.; Barillà, F.; Basso, C.; Ciccone, M.M.; Curcio, A.; Mancone, M.; et al. 2022 Update on myocarditis and pericarditis following COVID-19 vaccination. Expert Opinion of the Italian Society of Cardiology. G. Ital. Cardiol. (2006) 2022, 23, 408–413. [Google Scholar] [CrossRef]
- Simone, A.; Herald, J.; Chen, A.; Gulati, N.; Shen, A.Y.-J.; Lewin, B.; Lee, M.-S. Acute Myocarditis Following COVID-19 MRNA Vaccination in Adults Aged 18 Years or Older. JAMA Intern. Med. 2021, 181, 1668–1670. [Google Scholar] [CrossRef]
- Ammirati, E.; Bizzi, E.; Veronese, G.; Groh, M.; Van de Heyning, C.M.; Lehtonen, J.; Pineton de Chambrun, M.; Cereda, A.; Picchi, C.; Trotta, L.; et al. Immunomodulating Therapies in Acute Myocarditis and Recurrent/Acute Pericarditis. Front. Med. 2022, 9, 838564. [Google Scholar] [CrossRef]
- Bozkurt, B.; Kamat, I.; Hotez, P.J. Myocarditis With COVID-19 MRNA Vaccines. Circulation 2021, 144, 471–484. [Google Scholar] [CrossRef]
- Abbate, A.; Gavin, J.; Madanchi, N.; Kim, C.; Shah, P.R.; Klein, K.; Boatman, J.; Roberts, C.; Patel, S.; Danielides, S. Fulminant Myocarditis and Systemic Hyperinflammation Temporally Associated with BNT162b2 MRNA COVID-19 Vaccination in Two Patients. Int. J. Cardiol. 2021, 340, 119–121. [Google Scholar] [CrossRef]
- Larson, K.F.; Ammirati, E.; Adler, E.D.; Cooper, L.T.; Hong, K.N.; Saponara, G.; Couri, D.; Cereda, A.; Procopio, A.; Cavalotti, C.; et al. Myocarditis After BNT162b2 and MRNA-1273 Vaccination. Circulation 2021, 144, 506–508. [Google Scholar] [CrossRef] [PubMed]
- Rosner, C.M.; Genovese, L.; Tehrani, B.N.; Atkins, M.; Bakhshi, H.; Chaudhri, S.; Damluji, A.A.; de Lemos, J.A.; Desai, S.S.; Emaminia, A.; et al. Myocarditis Temporally Associated With COVID-19 Vaccination. Circulation 2021, 144, 502–505. [Google Scholar] [CrossRef]
- Corradetti, S.; Sclafani, M.; Mistrulli, R.; Gallo, G.; Pagannone, E.; Di Girolamo, M.; Autore, C.; Battistoni, A.; Volpe, M. Features and Follow-up of Patients Affected by Noninflammatory Myocarditis after Coronavirus Disease 2019 Vaccination. J. Cardiovasc. Med. 2023, 24, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Truong, D.T.; Dionne, A.; Muniz, J.C.; McHugh, K.E.; Portman, M.A.; Lambert, L.M.; Thacker, D.; Elias, M.D.; Li, J.S.; Toro-Salazar, O.H.; et al. Clinically Suspected Myocarditis Temporally Related to COVID-19 Vaccination in Adolescents and Young Adults: Suspected Myocarditis After COVID-19 Vaccination. Circulation 2022, 145, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Barda, N.; Dagan, N.; Ben-Shlomo, Y.; Kepten, E.; Waxman, J.; Ohana, R.; Hernán, M.A.; Lipsitch, M.; Kohane, I.; Netzer, D.; et al. Safety of the BNT162b2 MRNA COVID-19 Vaccine in a Nationwide Setting. N. Engl. J. Med. 2021, 385, 1078–1090. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).