Abstract
Background: Non-ST elevation acute coronary syndrome (NSTE-ACS) is one of the most frequent manifestations of coronary artery disease. The occurrence of serious heart rhythm disorders (SHRDs) in NSTE-ACS is not well documented. However, continuous heart rhythm monitoring is recommended during the initial management of NSTE-ACS. The targeted monitoring of patients at greater risk for SHRDs could facilitate patients’ care in emergency departments (EDs) where the flow of patients is continuously increasing. Methods: This retrospective single-center study included 480 patients from emergency and cardiology departments within the Strasbourg University Hospital between 1 January 2019 and 31 December 2020. The objective was to estimate the frequency of the occurrence of SHRDs among patients with NSTE-ACS. The secondary objective was to highlight the factors associated with a higher risk of SHRDs. Results: The proportion of SHRDs during the first 48 h of hospital care was 2.3% (CI95%: 1.2–4.1%, n = 11). Two time periods were considered: before coronary angiography (1.0%), and during, or after coronary angiography (1.3%). In the first group, two patients required immediate treatment (0.4% of the patients) and no death occurred. In the univariate analysis, the variables significantly associated with SHRDs were age, anticoagulant medication, a decrease in glomerular filtration rate, plasmatic hemoglobin, and left ventricle ejection fraction (LVEF), and an increase in plasmatic troponin, BNP, and CRP levels. In the multivariable analysis, plasmatic hemoglobin > 12 g/dL seemed to be a protective factor for SHRDs. Conclusions: In this study, SHRDs were rare and, most often, spontaneously resolved. These data challenge the relevance of systematic rhythm monitoring during the initial management of patients with NSTE-ACS.
1. Introduction
Cardiovascular disease is the leading cause of death worldwide. According to the World Health Organization (WHO), the most frequent cause of death of a cardiovascular origin is coronary artery disease, causing more than seven million deaths per year in the world and representing more than 13% of global mortality [1]. The acute expression of coronary artery disease encountered in emergency medicine is acute coronary syndrome (ACS), of which the clinical symptom is chest pain, making this frequent symptom a major diagnostic and therapeutic issue in emergency departments [2].
After performing an electrocardiogram (ECG), two groups of patients are distinguished, and the groups undergo a different management and prognosis: patients with persistent ST-segment elevation for more than 20 min (ST-segment elevation myocardial infarction, STEMI) and patients without persistent ST-segment elevation (non-ST elevation acute coronary syndrome, NSTE-ACS), including unstable angina and non-ST segment elevation myocardial infarction (NSTEMI). In NSTE-ACS, electrocardiographic changes may include transient ST segment elevation, ST segment depression (persistent or transient), and T-wave inversion or flattening, but the result of the ECG may also be normal [3]. NSTE-ACS represents more than 60% of ACS, and observations over the past decade suggest that the incidence of STEMI has decreased, while that of NSTE-ACS has increased [4,5]. Once diagnosed based on the results of the ECG, the management of STEMI involves immediate myocardial reperfusion [6]. In contrast, the management of NSTE-ACS is based on a risk assessment using scores (e.g., TIMI, ESC, GRACE, etc.), and it also depends on the measurement of cardiac biomarkers.
Complications of myocardial infarction can occur during NSTE-ACS, but these are less common compared to those associated with STEMI, including rhythm and conduction disorders potentially associated with death. Currently, few studies have investigated the frequency of the occurrence of serious rhythm and conduction disorders in NSTE-ACS. These studies are mostly related to inter-hospital transport, suggesting that the frequency of serious events detected on a cardioscope is low [7,8]. However, it is recommended to provide continuous rhythm monitoring for NSTE-ACS patients [9], which mobilizes material and human resources, both during out-of-hospital and in-hospital patient management. In the case of NSTE-ACS, this monitoring for several hours while waiting for the first biological results may cause difficulties in managing the flow of patients within the emergency department. In the context of overcrowding in these units, the study of the predictive factors associated with the occurrence of serious rhythm disorders appears to be of paramount importance to select continuous rhythm monitoring in high-risk patients.
In the present study, the authors aimed to estimate the frequency of the occurrence of serious heart rhythm disorders (SHRDs) during the first 48 h of hospital care in a population of NSTE-ACS patients admitted to emergency and cardiology departments.
2. Materials and Methods
2.1. Study Design and Population
The authors conducted a retrospective study in the emergency and cardiology departments of a university hospital in France. Data were collected between October 2021 and March 2022. The medical records used for the data collection were those of patients admitted to the emergency and cardiology departments for NSTE-ACS between January 2019 and December 2020. This explains the retrospective nature of the study, and such a design was considered appropriate to address the research question. Since patients with NSTE-ACS were identified before the study, this allowed for the study of rare events (in this case, SHRDs due du NSTE-ACS) in a shorter period of time than a prospective cohort study. A total of 500 consecutive patients aged over 18 years were admitted for NSTE-ACS, based on the International Classification of Diseases—Tenth Revision (ICD-10), codings I21.4-(NSTEMI), and I20.0 (unstable angina) to the emergency and cardiology departments of the University Hospital of Strasbourg were included.
2.2. End-Point Definitions
The primary objective was to estimate the frequency of SHRDs in patients with NSTE-ACS during the first 48 h of in-hospital management. The SHRDs include potentially lethal arrhythmias warranting continuous heart rhythm monitoring. Therefore, the authors used a composite primary end point corresponding to the following events: ventricular rhythm disorders (torsade de pointes, ventricular tachycardia [VT], ventricular fibrillation [VF]), high-grade conductive disorders (second-degree atrioventricular blocks [AVB] type Mobitz 2, complete AVB, and trifascicular blocks), electromechanical dissociation (EMD), and/or asystole. The occurrence of at least one of the above events was sought for each patient during the first 48 h of their hospitalization, the period accepted as when patients are at the highest risk of suffering rhythmic complications [10,11].
The secondary objective was to study the individual factors associated with the occurrence of SHRDs.
2.3. Data Collection
Hospitalization and monitoring data were obtained from the patients’ electronic medical records (EMRs). Using each patient’s EMRs, the following data were collected and entered into a computerized case report form: demographic and anthropometric characteristics, cardiovascular risk factors (CVRFs), comorbidities, long-term treatment, vital signs at the time of admission, characteristics of the first ECG, laboratory tests results at admission, patient’s description of a “typical” chest pain according to the European Society of Cardiology (ESC) criteria [9], initial management including whether or not a coronary angiography was performed, the SYNTAX score (SXS), and clinical SYNTAX score (CSS) values calculated from the lesions visualized during coronary angiography. These scores are predictive of the occurrence of major cardiovascular events after myocardial revascularization [12,13].
2.4. Statistical Analysis
All data were analyzed using the 4.0.2 version of R statistical software. The analysis consists of a descriptive and an analytical part. The descriptive analysis is univariate and bivariate, according to the presence or absence of SHRDs. For comparative analyses, a p value < 0.05 is considered statistically significant. For categorical variables, the analysis summarizes the variables by the number and frequency of each modality. Comparisons were made using Fischer’s exact test. The quantitative variables were described using the median with an interquartile range. Comparisons were made using Student’s t-test for continuous variables, or a Kruskal–Wallis test according to the normality of the variable.
The estimation of the frequency of the occurrence of SHRDs in patients with NSTE-ACS was performed by calculating the proportion of patients who presented an SHRD and the associated 95% confidence interval. The calculation of the confidence interval was performed using the Agresti–Coull method.
The identification of the factors associated with the occurrence of an SHRD was performed using the multivariable logistic regression model. First, univariate analyses between the dependent variable (occurrence of an SHRD) and all the potential associated factors were performed. For the second step, the multivariable model was constructed by integrating the variables presenting a p-value lower than 0.01 in univariate analysis and/or the variables of clinical interest. The results are presented as odds ratios with their 95% confidence intervals.
The number of subjects was calculated by determining the precision (width of the 95% confidence interval) of the expected estimate on the primary end point. Data from the literature suggest that complications such as conduction disorders and asystole would be in the range of 0.9 to 2.2% [14,15,16], whereas ventricular rhythm disorders would occur in 7.6 to 12.9% of NSTE-ACS [11,17]. Thus, the frequency of SHRDs during NSTE-ACS could be between 8.5% and 15.1%. However, this frequency is probably overestimated. Indeed, none of the estimates described above consider that the same patient may present several rhythmic complications. The inclusion of 400 patients allows us to estimate this frequency with a precision of 5 to 9%, depending on the value of the point estimate. This precision was considered clinically satisfactory. In order to take into account possible missing data, the number of subjects required was set at 500.
2.5. Ethics
This study was conducted in accordance with the principles set forth by the Good Clinical Practice guidelines and the Declaration of Helsinki. The study was approved by the Ethics Committee (CE No.-2021-117). In accordance with French legislation, formal written informed consent was not required for this type of study because the data studied were entirely retrospectively [18]. An information and non-opposition form was sent to each patient, allowing them to express a possible refusal of inclusion in the study.
3. Results
Between 1 January 2019, and 31 December 2020, 728 patients admitted to the emergency and cardiology departments were selected, and 500 met the inclusion criteria. In total, 7 patients refused the anonymized use of their medical record data, and 13 could not be informed because they did not have a valid address. The records of 480 patients were retained for the analysis (Figure 1).
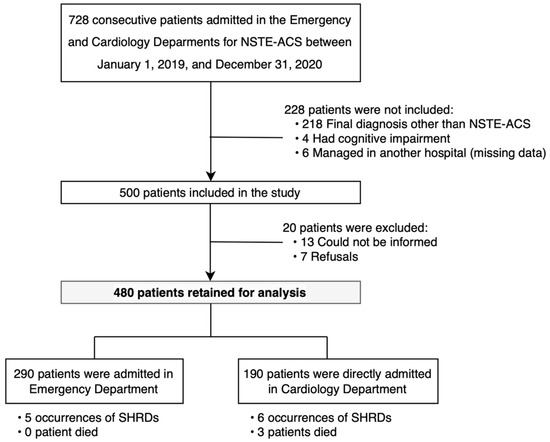
Figure 1.
Flow chart of the study population. Abbreviations: NSTE-ACS: non-ST elevation acute coronary syndrome.
3.1. Baseline Characteristics of the Study Population
The characteristics of the 480 patients analyzed are presented in Table 1. In this study, 330 men and 150 women were included, and the median age was 69 years (interquartile range [IQR] [59.0; 78.0]). The predominant cardiovascular risk factors (CVRFs) were hypertension (68.5%, n = 329) and dyslipidemia (52.1%, n = 250). Almost half of the patients admitted for NSTE-ACS had a history of ischemic heart disease (48.1%, n = 231).
Among the individual patient characteristics, only older age appeared to be associated with the occurrence of SHRDs. In contrast, the percentage of anticoagulation was statistically significantly higher in patients with an SHRD. The type of antiplatelet therapy and other cardiovascular treatments were not associated with the occurrence of SHRDs.

Table 1.
Baseline characteristics of the study population according to occurrence or not of serious heart rhythm disorder (SHRD).
Table 1.
Baseline characteristics of the study population according to occurrence or not of serious heart rhythm disorder (SHRD).
| Variable | Study Population | No SHRD | SHRD | p-Value | |
|---|---|---|---|---|---|
| n = 480 | n = 469 | n = 11 | |||
| Individual characteristics, median [IQR] | |||||
| Age, in years | 69.0 [59.0; 78.0] | 69.0 [59.0; 78.0] | 85.0 [71.5; 88.5] | 0.004 * | |
| BMI, kg/m2 | 26.46 [23.89; 30.45] | 26.5 [24.1; 30.5] | 23.9 [22.8; 30.2] | 0.361 | |
| Female, n (%) | 150 (31.2) | 144 (30.7) | 6 (54.5) | 0.175 | |
| Cardiovascular risk factors (CVRFs), n (%) | |||||
| Heredity | 102 (21.2) | 101 (21.5) | 1 (9.1) | 0.532 | |
| Smoking | 125 (26.0) | 124 (26.4) | 1 (9.1) | 0.343 | |
| High blood pressure | 329 (68.5) | 321 (68.4) | 8 (72.7) | 1.000 | |
| Diabetes mellitus | 175 (36.5) | 169 (36.0) | 6 (54.5) | 0.345 | |
| Dyslipidemia | 250 (52.1) | 244 (52.0) | 6 (54.5) | 1.000 | |
| Obesity | 122 (25.4) | 118 (25.2) | 4 (36.4) | 0.622 | |
| Number of CVRFs, median [IQR] | 2.0 [1.0; 3.0] | 2.0 [1.0; 3.0] | 2.0 [1.0; 3.5] | 0.872 | |
| Comorbidities, n (%) | |||||
| Ischemic heart disease | 231 (48.1) | 225 (48.0) | 6 (54.5) | 0.900 | |
| Ischemic stroke | 41 (8.5) | 40 (8.5) | 1 (9.1) | 1.000 | |
| Peripheral arterial disease | 67 (14.0) | 65 (13.9) | 2 (18.2) | 1.000 | |
| Renal failure | 81 (16.9) | 77 (16.4) | 4 (36.4) | 0.181 | |
| Heart failure | 23 (4.8) | 23 (4.9) | 0 (0.0) | 0.969 | |
| Supraventricular rhythm disorder | 65 (13.5) | 63 (13.4) | 2 (18.2) | 0.993 | |
| Long-term treatment, n (%) | |||||
| Anticoagulant | 67 (14.0) | 65 (13.9) | 2 (18.2) | 0.010 * | |
| Antiplatelet agent | 243 (50.6) | 237 (50.5) | 6 (54.5) | 1.000 | |
| ACE inhibitor | 134 (27.9) | 132 (28.1) | 2 (18.2) | 0.698 | |
| ARB | 116 (24.2) | 115 (24.5) | 1 (9.1) | 0.409 | |
| Beta-blocker | 237 (49.5) | 233 (49.8) | 4 (36.4) | 0.565 | |
| Statin | 215 (44.8) | 210 (44.8) | 5 (45.5) | 1.000 | |
* p < 0.05. Abbreviations: SHRD: serious heart rhythm disorder, IQR: interquartile range, BMI: body mass index, CVRFs: cardiovascular risk factors, ACE: angiotensin-converting enzyme, ARB: angiotensin receptor blocker.
3.2. In-Hospital Management
The characteristics at admission and complications during initial management are summarized in Table 2. Patients were usually admitted to the emergency department (60.4%, n = 290), less often to the cardiology department (39.6%, n = 190). Being managed in the cardiology department rather than the emergency department at admission did not have a significant impact on the occurrence of SHRDs.

Table 2.
Characteristics and complications during in-hospital management according to the occurrence of serious heart rhythm disorder (SHRD).
Typical chest pain, as described by the ESC, was reported by 55.6% (n = 266) of patients. The ECG at admission was abnormal in 58.1% (n = 279) of cases, with a majority of T-wave changes (69.5%, n = 194). ST segment depression was present in 25.4% (n = 71) of the abnormal admission ECGs, and the median sum of the depression in all leads was 5.0 mm (IQR [3.0; 6.0]). These repolarization disorders mainly involved the inferior (20.3%, n = 54) and extended anterior territory (15.8%, n = 42). Only 1.7% (n = 8) of patients in this study had a new onset supraventricular rhythm disorder at admission, and it was atrial fibrillation in all cases. Extrasystoles were present in 9% (n = 43) of patients. None of the electrocardiographic abnormalities appeared to be associated with the occurrence of SHRDs. No association was found between the coronary territory involved and the occurrence of SHRDs. As expected, the prevalence of cardiogenic shock and death was significantly higher in SHRD patients.
Regarding the initial biological characteristics, the SHRD patients’ group were more often anemic with a lower median GFR and higher plasma troponin, BNP, and CRP. LVEF was also lower in SHRD patients.
Coronary angiography was performed in 75.4% (n = 362) of patients within 48 h after their admission, and 79.6% (n = 288) of them underwent percutaneous coronary angioplasty during this procedure. Before angioplasty, an analgesic drug (excluding nitrates) was administered to 20.2% (n = 97) of patients. In more than two thirds of cases, the highest level of pain medication used was paracetamol (68.0%, n = 66) and, more rarely, a level 2 analgesic (14.4%, n = 14) or morphine (17.5%, n = 17).
3.3. Primary End-Point
Among the 480 patients of the study, SHRDs occurred for 11 patients (2.3%) within the first 48 h of management, with a 95% confidence interval of [1.2%; 4.1%]. The distribution of SHRDs is presented in Figure 2, and the characteristics of these events are presented in Table 3.
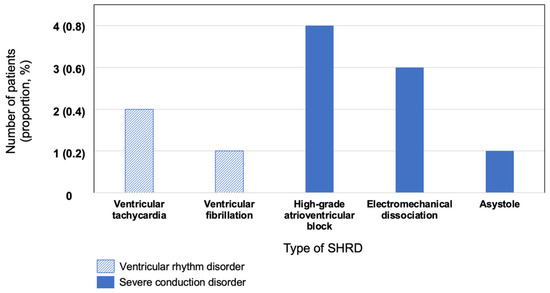
Figure 2.
Distribution of serious heart rhythm disorders (SHRDs). Abbreviations: SHRD: serious heart rhythm disorder, CI95%: 95% confidence interval.

Table 3.
Specific characteristics related to the occurrence of serious heart rhythm disorder (SHRD).
Six SHRDs occurred during or after coronary angiography with angioplasty (patients N°6, 7, 8, 9, 10, and 11). This represents 1.3% of the population (95% CI [0.5%; 2.8%]) and three of these patients died after the revascularization procedure (N°6, 8, and 9). Patients N°6 and N°9 died of refractory cardiogenic shock following return of spontaneous circulation. Patient N°8 died of refractory cardiac arrest. No deaths occurred before coronary angiography. A more detailed description of the patients and events is available in Supplementary Material S1.
3.4. Multivariable Analysis
Variables with the lowest p-values (age, troponin, BNP, CRP, hemoglobin, and GFR), or those whose association with SHRDs is well documented in the literature (LVEF) were retained for the multivariable analysis (Table 4). The analysis was performed considering that the risk increases proportionally with changes in the variable of interest. The variables troponin, CRP, GFR, and hemoglobin were each analyzed using a threshold to distinguish a normal value from a pathological value. The thresholds chosen were based on the standards used in the Strasbourg University Hospital laboratories. In this study, plasmatic hemoglobin > 12 g/dL is associated with a lower risk of SHRD (OR = 0.12, 95% CI [0.02; 0.48]) and, therefore, could be considered a protective factor for SHRD in patients with NSTE-ACS.

Table 4.
Multivariable analysis of factors associated with serious heart rhythm disorder occurrence.
4. Discussion
In this retrospective study including patients hospitalized in the emergency and cardiology departments for NSTE-ACS, 11 patients out of 480 presented an SHRD during the first 48 h of in-hospital management, which represents 2.3% of the study population (95% CI [1.2%; 4.1%]). Most of these were severe conduction disorders. The occurrence of SHRDs does not appear to differ according to the realization or not of a coronary angiography; six of these events occurred during or in the hours following coronary angiography for 1.3% of the study population (95% CI [0.5%; 2.8%]) and three of them died after inaugural electro-mechanical dissociation. An SHRD before coronary angiography concerned five patients (1.0% of the study population) (95% CI [0.4%; 2.5%]), therapeutic intervention was required for only two of them (0.4% of the study population, 95% CI [0.01%; 1.6%]), and none died during the first 48 h of in-hospital management. Among the factors studied, older age, anticoagulant medication, a decrease in LVEF, GFR, and plasma hemoglobin, and an increase in plasma troponin, BNP, and CRP were statistically associated with the occurrence of SHRD. Significantly higher troponin and BNP values are suggestive of greater myocardial involvement in the SHRD population, while the decreased LVEF observed in this population might increase the risk of myocardial infarction. After multivariable analysis, having plasmatic hemoglobin above 12 g/dL appears to be independently associated with a lower risk of SHRD occurrence.
To the best of the authors’ knowledge, this study is the first to comprehensively estimate the frequency of SHRD, including both ventricular rhythm disorders and severe conduction disorders in NSTE-ACS.
With regard to ventricular rhythm disorders, the prevalence within 48 h of inclusion was estimated at 0.6% by Piccini et al. [19] for patients presenting a high-risk NSTE-ACS. This prevalence is lower than the estimated prevalence of rhythm disorders in NSTE-ACS in other studies, which is supposed to be between 5 and 10% [19]. In the study by Gupta et al. [11], the prevalence of ventricular rhythm disorders was 7.6%, and 60% occurred in the first 48 h. For Tran et al. [17], this estimate was higher, with 11.3% of VT and 1.6% of VF, but the difference may be partly explained by the period of interest in this study, whereas it appears that a significant proportion of rhythm disorders in association with NSTE-ACS occur beyond 48 h [11,17,19]. Regarding conduction disorders and asystole, the study by Alnsasra et al. [20] included 49 patients with high-grade AVB out of 5612 with NSTE-ACS, i.e., 0.9% of the population. This estimate was 0.6% in the study by Misumida et al. [14] and 0.4% in the study by Pokorney et al. [15]. The prevalence of asystole and EMD was estimated to be 0.5% and 0.1%, respectively, in the study by Pokorney et al. [15].
The percentage of complications related to coronary angiography for all indications combined was estimated at 1.7% by Gach et al. [21], taking into account major complications of the procedure such as death, rhythm disorders, stroke, vascular complications, or hemodynamic and allergic complications.
In previous studies, advanced age, elevated plasma troponin, impaired renal function, and decreased LVEF were identified as the factors significantly associated with the occurrence of SHRDs in patients with NSTE-ACS [11,14,15,19,20]. To our knowledge, there is no data in the literature regarding the association between the occurrence of SHRDs and BNP, CRP, and hemoglobin values in patients with NSTE-ACS. The study of Sauer et al. [22] showed an increased risk of ventricular rhythm disorders with morphine administration in patients with STEMI. Furthermore, the studies of Tran et al. [23] and Liu et al. [24] suggested an increased risk of rhythm disorders with hyperglycemia in patients with NSTE-ACS.
4.1. Strengths and Limitations
The retrospective nature of the study and the small number of events of interest are limitations that have to be taken into account when interpreting the results. There are indeed few SHRDs, and such a small number of cases certainly led to insufficient statistical power and a biased estimate of logistic regression coefficients. The results of the univariate analysis and the multivariable model should, therefore, be cautiously interpreted.
Despite these limitations, the main strength of the study is that it was conducted with a large cohort of patients. Many potential risk factors, including clinical, biological, or electrocardiographic, were taken into account. Some of them, such as hemoglobin, have never been studied in the literature. The a priori calculation of the number of required subjects ensured a certain degree of precision in the estimate.
4.2. Implications
The present study provides interesting initial data for a simple estimation of the overall risk of SHRDs. These results could be confirmed and completed by a larger study to identify a population at risk. Similar work on pre-hospital and inter-hospital transport would be interesting, given their potential impact on the means to be used for transporting these patients. A precise individual assessment of the risk of SHRDs (e.g., using a prediction score) would allow for less strict but more appropriate monitoring. This could lead to new recommendations outlining the criteria for monitoring NSTE-ACS patients, instead of the current guidelines that recommend the routine monitoring of all these patients. This approach aims to make patient management more fluid, without reducing the quality and safety of care.
5. Conclusions
In this study, serious heart rhythm disorders (SHRDs) occurring during the first 48 h of hospital management were rare and, most often, spontaneously resolved. Currently, continuous heart rhythm monitoring for at least 24 h is recommended during the management of patients with NSTE-ACS. These recommendations are not evidence based, and, to date, no studies have addressed the prevalence of all SHRDs in NSTE-ACS. The low proportion of SHRDs challenges the value of systematic cardiac rhythm monitoring during initial management, once the diagnosis of STEMI has been eliminated.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm12103456/s1, Supplementary Material S1: Supplementary Material to Table 3 in the “Results” section—Specific characteristics related to the occurrence of serious heart rhythm disorder (SHRD).
Author Contributions
Conceptualization, V.W., S.H. and O.M.; methodology, V.W., F.S., and S.H.; software, V.W., S.H. and F.S.; validation, V.W., S.H., O.M., S.K., F.S., A.C., P.B. and P.L.B.; formal analysis, V.W., S.H. and F.S.; investigation, V.W., S.H., O.M. and S.K.; data curation, V.W., A.C., O.M., S.H., S.K., P.B. and P.L.B.; writing—original draft preparation, V.W. and S.K.; writing—review and editing, V.W., F.S., S.K., O.M., A.C., S.H., P.L.B. and P.B.; visualization, V.W., A.C., P.L.B. and P.B.; supervision, V.W., S.H., S.K. and O.M.; project administration, V.W., S.H. and O.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of the University of Strasbourg (CE No.-2021-117, 21 September 2021). Formal written consent was not necessary in accordance with French legislation in this retrospective study.
Informed Consent Statement
In accordance with French legislation, the need for written informed consent was waived by the Ethics Committee of the Faculties of Medicine, Odontology, Pharmacy, Schools of Nursing, Physiotherapy, Maieutics, and Hospitals of the University of Strasbourg (CE No.-2021-117) due to retrospective nature of the study. However, each patient was sent an information and non-opposition form.
Data Availability Statement
All data generated or analyzed during the study are included in this published article.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
ACS: acute coronary syndrome, STEMI: ST elevation myocardial infarction, NSTE-ACS: non-ST elevation acute coronary syndrome, NSTEMI: non-ST elevation myocardial infarction, SHRD(s): serious heart rhythm disorder(s), ED: emergency department, WHO: World Health Organization, NHC: Nouvel Hôpital Civil, AVB: atrioventricular block, EMD: electromechanical dissociation, VT: ventricular tachycardia, VF: ventricular fibrillation, EMR: electronic medical record, CVRFs: cardiovascular risk factors, ESC: European Society of Cardiology, SXS: SYNTAX score, CSS: clinical SYNTAX score, GFR: glomerular filtration rate, LVEF: left ventricle ejection fraction, AIA: anterior interventricular artery.
References
- World Health Organization. Cardiovascular Diseases. Available online: https://www.who.int/fr/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 19 November 2022).
- Pines, J.M.; Pollack, C.V.; Diercks, D.B.; Chang, A.M.; Shofer, F.S.; Hollander, J.E. The Association between Emergency Department Crowding and Adverse Cardiovascular Outcomes in Patients with Chest Pain. Acad. Emerg. Med. 2009, 16, 617–625. [Google Scholar] [CrossRef] [PubMed]
- Roffi, M.; Patrono, C.; Collet, J.P.; Mueller, C.; Valgimigli, M.; Andreotti, F.; Bax, J.J.; Borger, M.A.; Brotons, C.; Chew, D.P.; et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2016, 37, 267–315. [Google Scholar] [CrossRef] [PubMed]
- McManus, D.D.; Gore, J.; Yarzebski, J.; Spencer, F.; Lessard, D.; Goldberg, R.J. Recent Trends in the Incidence, Treatment, and Outcomes of Patients with STEMI and NSTEMI. Am. J. Med. 2011, 124, 40–47. [Google Scholar] [CrossRef]
- Amsterdam, E.A.; Wenger, N.K.; Brindis, R.G.; Casey, D.E., Jr.; Ganiats, T.G.; Holmes, D.R., Jr.; Jaffe, A.S.; Jneid, H.; Kelly, R.F.; Kontos, M.C.; et al. 2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes. J. Am. Coll. Cardiol. 2014, 64, e139–e228. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef]
- Lenglet, A.; Balen, F.; Charpentier, S.; Sourbes, A.; Arcuset, D.; Delonglée, V.; Fort, P.; Bounes, V.; Dadone, B.C. Adverse events during inter-hospital transports of patients with Non ST-elevation acute coronary syndrome. Ann. Fr. Med. Urgence 2019, 9, 369–374. [Google Scholar] [CrossRef]
- Trebouet, E.; Boiffard, E.; Debierre, V.; Fradin, P. Study of complications occuring during inter-hospital transports of patients Non ST-elevation acute coronary syndrome. Ann. Cardiol. Angéiologie 2019, 68, 13–16. [Google Scholar] [CrossRef]
- Collet, J.-P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- Ghuran, A.V.; Camm, A.J. Ischaemic heart disease presenting as arrhythmias. Br. Med. Bull. 2001, 59, 193–210. [Google Scholar] [CrossRef]
- Gupta, S.; Pressman, G.S.; Figueredo, V.M. Incidence of, predictors for, and mortality associated with malignant ventricular arrhythmias in non-ST elevation myocardial infarction patients. Coron. Artery Dis. 2010, 21, 460–465. [Google Scholar] [CrossRef]
- Serruys, P.; Onuma, Y.; Garg, S.; Sarno, G.; Brand, M.V.D.; Kappetein, A.-P.; Van Dyck, N.; Mack, M.; Holmes, D.; Feldman, T.; et al. Assessment of the SYNTAX score in the Syntax study. EuroIntervention 2009, 5, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.; Sarno, G.; Garcia-Garcia, H.M.; Girasis, C.; Wykrzykowska, J.; Dawkins, K.D.; Serruys, P.W.; on behalf of the ARTS-II Investigators. A New Tool for the Risk Stratification of Patients With Complex Coronary Artery Disease: The Clinical SYNTAX Score. Circ. Cardiovasc. Interv. 2010, 3, 317–326. [Google Scholar] [CrossRef]
- Misumida, N.; Ogunbayo, G.O.; Kim, S.M.; Abdel-Latif, A.; Ziada, K.M.; Elayi, C.S. Frequency and Significance of High-Degree Atrioventricular Block and Sinoatrial Node Dysfunction in Patients with Non-ST-Elevation Myocardial Infarction. Am. J. Cardiol. 2018, 122, 1598–1603. [Google Scholar] [CrossRef]
- Pokorney, S.D.; Radder, C.; Schulte, P.J.; Al-Khatib, S.M.; Tricocci, P.; Van de Werf, F.; James, S.K.; Cannon, C.P.; Armstrong, P.W.; White, H.D.; et al. High-degree atrioventricular block, asystole, and electro-mechanical dissociation complicating non–ST-segment elevation myocardial infarction. Am. Heart J. 2016, 171, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Huang, Y.C. Comparison of STEMI and NSTEMI patients in the emergency department. J. Acute Med. 2011, 1, 1–4. [Google Scholar] [CrossRef]
- Tran, H.V.; Ash, A.S.; Gore, J.M.; Darling, C.E.; Kiefe, C.I.; Goldberg, R.J. Twenty-five year trends (1986–2011) in hospital incidence and case-fatality rates of ventricular tachycardia and ventricular fibrillation complicating acute myocardial infarction. Am. Heart J. 2019, 208, 1–10. [Google Scholar] [CrossRef]
- Toulouse, E.; Masseguin, C.; Lafont, B.; McGurk, G.; Harbonn, A.; Roberts, J.A.; Granier, S.; Dupeyron, A.; Bazin, J.E. French legal approach to clinical research. Anaesth. Crit. Care Pain Med. 2018, 37, 607–614. [Google Scholar] [CrossRef] [PubMed]
- Piccini, J.P.; White, J.A.; Mehta, R.H.; Lokhnygina, Y.; Al-Khatib, S.M.; Tricoci, P.; Pollack, J.C.V.; Montalescot, G.; Van de Werf, F.; Gibson, C.M.; et al. Sustained Ventricular Tachycardia and Ventricular Fibrillation Complicating Non–ST-Segment–Elevation Acute Coronary Syndromes. Circulation 2012, 126, 41–49. [Google Scholar] [CrossRef]
- Alnsasra, H.; Ben-Avraham, B.; Gottlieb, S.; Ben-Avraham, M.; Kronowski, R.; Iakobishvili, Z.; Goldenberg, I.; Strasberg, B.; Haim, M. High-grade atrioventricular block in patients with acute myocardial infarction. Insights from a contemporary multi-center survey. J. Electrocardiol. 2018, 51, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Gach, O.; Davin, L.; Lempereur, M.; Marechal, P.; Martinez, C.; Lancellotti, P. Diagnostic coronarography. Rev. Med. Liege 2019, 74, S17–S21. Available online: https://orbi.uliege.be/bitstream/2268/239766/1/2019S1_04.pdf (accessed on 22 November 2022).
- Sauer, F.; Jesel, L.; Marchandot, B.; Derimay, F.; Bochaton, T.; Amaz, C.; Roubille, F.; Cayla, G.; Rioufol, G.; Garcia-Dorado, D.; et al. Life-threatening arrhythmias in anterior ST-segment elevation myocardial infarction patients treated by percutaneous coronary intervention: Adverse impact of morphine. Eur. Heart J. Acute Cardiovas. Care 2021, 10, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Tran, H.V.; Gore, J.M.; Darling, C.E.; Ash, A.S.; Kiefe, C.I.; Goldberg, R.J. Hyperglycemia and risk of ventricular tachycardia among patients hospitalized with acute myocardial infarction. Cardiovasc. Diabetol. 2018, 17, 136. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Li, Z.; Xing, S.; Xu, Y. Effect of Admission Hyperglycemia on Short-Term Prognosis of Patients with Non-ST Elevation Acute Coronary Syndrome without Diabetes Mellitus. J. Diabetes Res. 2021, 2021, 1321289. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).