The Safety and Efficacy of an Unflanged 4F Pancreatic Stent in Transpancreatic Precut Sphincterotomy for Patients with Difficult Biliary Cannulation: A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
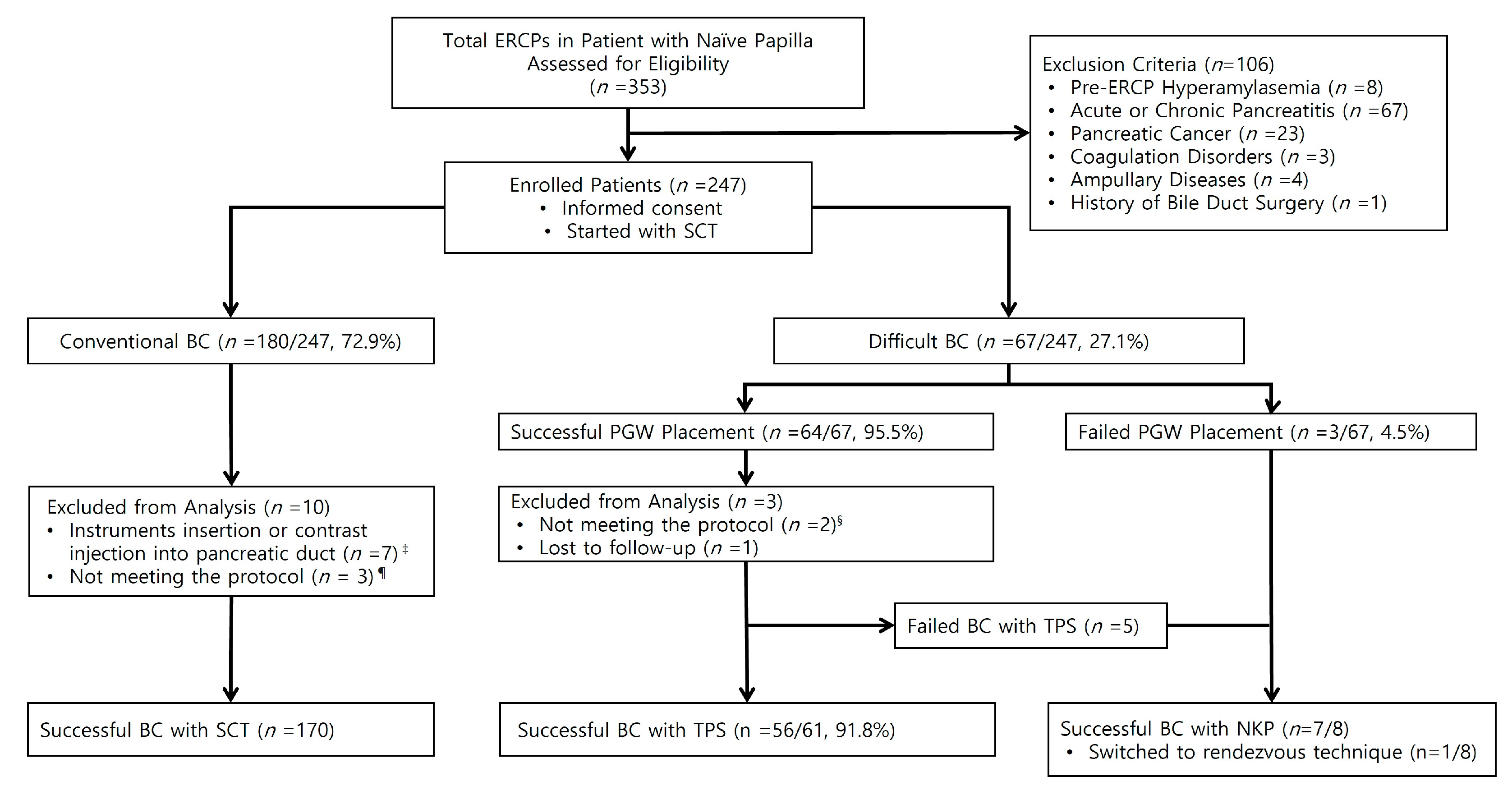
2.1. Patients and Study Design
2.2. Definition and Outcome Measurement
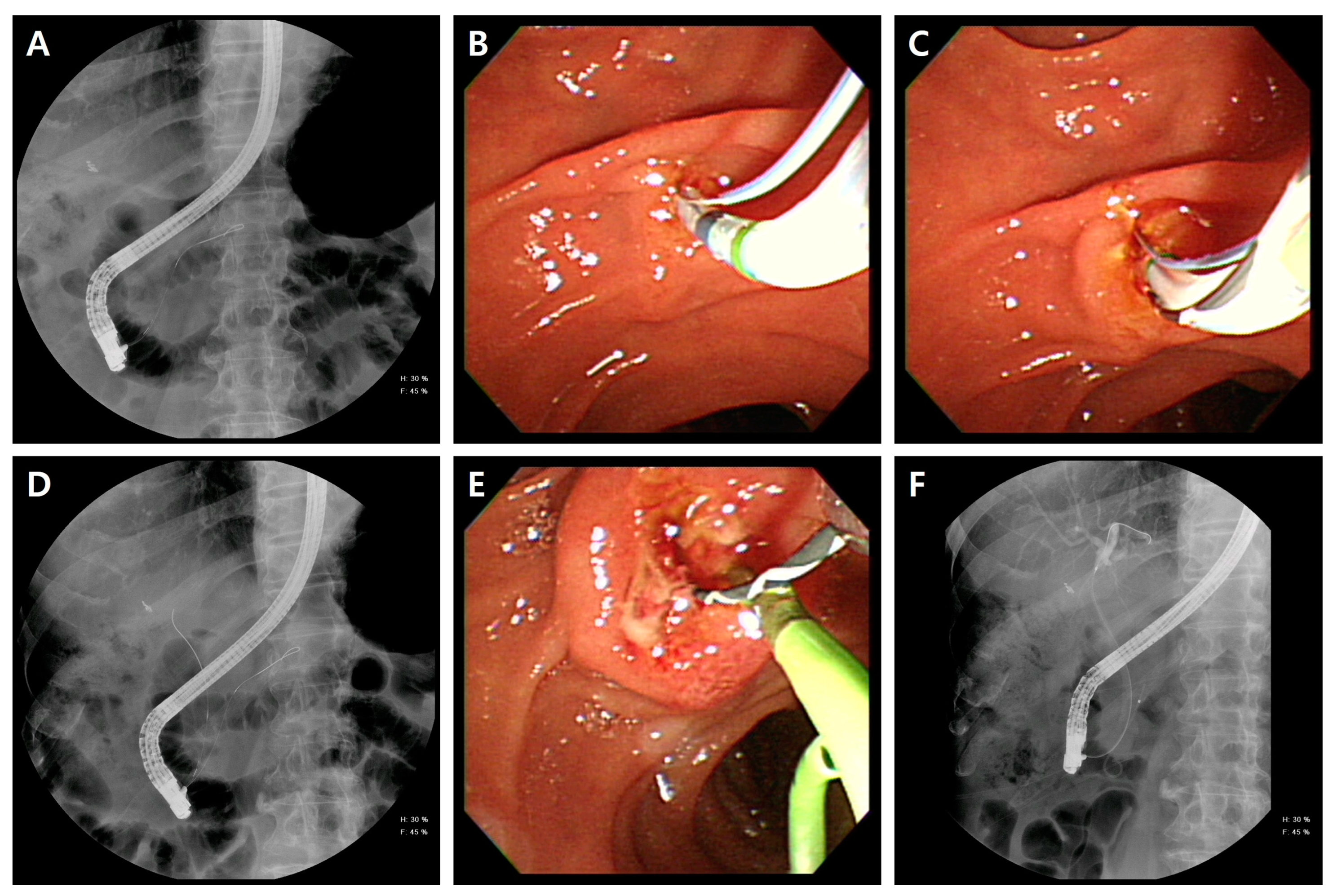
2.3. Endoscopic Procedures
2.4. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
3.2. Post-ERCP Complications
3.3. Technical Outcomes
3.4. Dislodgement Rate
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Freeman, M.L.; Guda, N.M. Prevention of post-ERCP pancreatitis: A comprehensive review. Gastrointest. Endosc. 2004, 59, 845–864. [Google Scholar] [CrossRef]
- Freeman, M.L. Adverse outcomes of ERCP. Gastrointest. Endosc. 2002, 56, S273–S282. [Google Scholar] [CrossRef]
- Vandervoort, J.; Soetikno, R.M.; Tham, T.C.K.; Wong, R.C.K.; Ferrari, A.P.; Montes, H.; Roston, A.D.; Slivka, A.; Lichtenstein, D.R.; Ruymann, F.W.; et al. Risk factors for complications after performance of ERCP. Gastrointest. Endosc. 2002, 56, 652–656. [Google Scholar] [CrossRef]
- Halttunen, J.; Meisner, S.; Aabakken, L.; Arnelo, U.; Grönroos, J.; Hauge, T.; Kleveland, P.M.; Nordblad Schmidt, P.; Saarela, A.; Swahn, F.; et al. Difficult cannulation as defined by a prospective study of the Scandinavian Association for Digestive Endoscopy (SADE) in 907 ERCPs. Scand. J. Gastroenterol. 2014, 49, 752–758. [Google Scholar] [CrossRef]
- Zou, X.P.; Leung, J.W.; Li, Y.H.; Yao, Y.L.; Pei, Q.S.; Wu, Y.L.; He, Q.B.; Cao, J.; Ding, X.W. Comparison of sequential pancreatic duct guidewire placement technique and needle knife precut sphincterotomy for difficult biliary cannulation. J. Dig. Dis. 2015, 16, 741–746. [Google Scholar] [CrossRef]
- Angsuwatcharakon, P.; Rerknimitr, R.; Ridtitid, W.; Ponauthai, Y.; Kullavanijaya, P. Success rate and cannulation time between precut sphincterotomy and double-guidewire technique in truly difficult biliary cannulation. J. Gastroenterol. Hepatol. 2012, 27, 356–361. [Google Scholar] [CrossRef]
- de Tejada, A.H.; Calleja, J.L.; Díaz, G.; Pertejo, V.; Espinel, J.; Cacho, G.; Jiménez, J.; Millán, I.; García, F.; Abreu, L.; et al. Double-guidewire technique for difficult bile duct cannulation: A multicenter randomized, controlled trial. Gastrointest. Endosc. 2009, 70, 700–709. [Google Scholar] [CrossRef]
- Katsinelos, P.; Paroutoglou, G.; Kountouras, J.; Chatzimavroudis, G.; Zavos, C.; Pilpilidis, I.; Tzelas, G.; Tzovaras, G. A comparative study of standard ERCP catheter and hydrophilic guide wire in the selective cannulation of the common bile duct. Endoscopy 2008, 40, 302–307. [Google Scholar] [CrossRef]
- Schwacha, H.; Allgaier, H.-P.; Deibert, P.; Olschewski, M.; Allgaier, U.; Blum, H.E. A sphincterotome-based technique for selective transpapillary common bile duct cannulation. Gastrointest. Endosc. 2000, 52, 387–391. [Google Scholar] [CrossRef]
- Tang, S.-J.; Haber, G.B.; Kortan, P.; Zanati, S.; Cirocco, M.; Ennis, M.; Elfant, A.; Scheider, D.; Ter, H.; Dorais, J. Precut papillotomy versus persistence in difficult biliary cannulation: A prospective randomized trial. Endoscopy 2005, 37, 58–65. [Google Scholar] [CrossRef]
- Lee, T.H.; Park, D.H. Endoscopic prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis. World J. Gastroenterol. 2014, 20, 16582–16595. [Google Scholar] [CrossRef] [PubMed]
- Tang, Z.; Yang, Y.; Yang, Z.; Meng, W.; Li, X. Early precut sphincterotomy does not increase the risk of adverse events for patients with difficult biliary access: A systematic review of randomized clinical trials with meta-analysis and trial sequential analysis. Medicine 2018, 97, e12213. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Wan, J.H.; Wu, D.Y.; Shu, W.Q.; Xia, L.; Lu, N.H. Assessing quality of precut sphincterotomy in patients with difficult biliary access: An updated meta-analysis of randomized controlled trials. J. Clin. Gastroenterol. 2018, 52, 573–578. [Google Scholar] [CrossRef] [PubMed]
- Mavrogiannis, C.; Liatsos, C.; Romanos, A.; Petoumenos, C.; Nakos, A.; Karvountzis, G. Needle-knife fistulotomy versus needle-knife precut papillotomy for the treatment of common bile duct stones. Gastrointest. Endosc. 1999, 50, 334–339. [Google Scholar] [CrossRef] [PubMed]
- Dumonceau, J.M.; Devière, J.; Cremer, M. A new method of achieving deep cannulation of the common bile duct during endoscopic retrograde cholangiopancreatography. Endoscopy 1998, 30, S80. [Google Scholar] [CrossRef]
- Maeda, S.; Hayashi, H.; Hosokawa, O.; Dohden, K.; Hattori, M.; Morita, M.; Kidani, E.; Ibe, N.; Tatsumi, S. Prospective randomized pilot trial of selective biliary cannulation using pancreatic guide-wire placement. Endoscopy 2003, 35, 721–724. [Google Scholar] [CrossRef]
- Facciorusso, A.; Ramai, D.; Gkolfakis, P.; Khan, S.R.; Papanikolaou, I.S.; Triantafyllou, K.; Tringali, A.; Chandan, S.; Mohan, B.P.; Adler, D.G. Comparative efficacy of different methods for difficult biliary cannulation in ERCP: Systematic review and network meta-analysis. Gastrointest. Endosc. 2022, 95, 60–71. [Google Scholar] [CrossRef]
- Goff, J.S. Common bile duct pre-cut sphincterotomy: Transpancreatic sphincter approach. Gastrointest. Endosc. 1995, 41, 502–505. [Google Scholar] [CrossRef]
- Chen, J.W.C.; Saccone, G.T.P.; Toouli, J. Sphincter of Oddi dysfunction and acute pancreatitis. Gut 1998, 43, 305–308. [Google Scholar] [CrossRef]
- Joo, Y.W.; Yoon, J.H.; Cho, S.C.; Lee, K.N.; Ha, N.R.; Lee, H.L.; Lee, O.Y.; Yoon, B.C.; Choi, H.S.; Hahm, J.S.; et al. Endoscopic pancreatic sphincterotomy: Indications and complications. Korean J. Intern. Med. 2009, 24, 190–195. [Google Scholar] [CrossRef]
- Lehman, G.A.; Sherman, S.; Nisi, R.; Hawes, R.H. Pancreas divisum: Results of minor papilla sphincterotomy. Gastrointest. Endosc. 1993, 39, 1–8. [Google Scholar] [CrossRef]
- Pécsi, D.; Farkas, N.; Hegyi, P.; Balaskó, M.; Czimmer, J.; Garami, A.; Illés, A.; Mosztbacher, D.; Pár, G.; Párniczky, A.; et al. Transpancreatic sphincterotomy has a higher cannulation success rate than needle-knife precut papillotomy—A meta-analysis. Endoscopy 2017, 49, 874–887. [Google Scholar] [CrossRef] [PubMed]
- Freeman, M.L.; Nelson, D.B.; Sherman, S.; Haber, G.B.; Herman, M.E.; Dorsher, P.J.; Moore, J.P.; Fennerty, M.B.; Ryan, M.E.; Shaw, M.J.; et al. Complications of endoscopic biliary sphincterotomy. N. Engl. J. Med. 1996, 335, 909–919. [Google Scholar] [CrossRef] [PubMed]
- Masci, E.; Mariani, A.; Curioni, S.; Testoni, P.A. Risk factors for pancreatitis following endoscopic retrograde cholangiopancreatography: A meta-analysis. Endoscopy 2003, 35, 830–834. [Google Scholar] [CrossRef] [PubMed]
- Masci, E.; Toti, G.; Mariani, A.; Curioni, S.; Lomazzi, A.; Dinelli, M.; Minoli, G.; Crosta, C.; Comin, U.; Fertitta, A.; et al. Complications of diagnostic and therapeutic ERCP: A prospective multicenter study. Am. J. Gastroenterol. 2001, 96, 417–423. [Google Scholar] [CrossRef]
- Cennamo, V.; Fuccio, L.; Repici, A.; Fabbri, C.; Grilli, D.; Conio, M.; D’Imperio, N.; Bazzoli, F. Timing of precut procedure does not influence success rate and complications of ERCP procedure: A prospective randomized comparative study. Gastrointest. Endosc. 2009, 69, 473–479. [Google Scholar] [CrossRef]
- Wang, P.; Li, Z.-S.; Liu, F.; Ren, X.; Lu, N.-H.; Fan, Z.-N.; Huang, Q.; Zhang, X.; He, L.-P.; Sun, W.-S.; et al. Risk factors for ERCP-related complications: A prospective multicenter study. Am. J. Gastroenterol. 2009, 104, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Mazaki, T.; Mado, K.; Masuda, H.; Shiono, M. Prophylactic pancreatic stent placement and post-ERCP pancreatitis: An updated meta-analysis. J. Gastroenterol. 2014, 49, 343–355. [Google Scholar] [CrossRef]
- Dumonceau, J.-M.; Kapral, C.; Aabakken, L.; Papanikolaou, I.S.; Tringali, A.; Vanbiervliet, G.; Beyna, T.; Dinis-Ribeiro, M.; Hritz, I.; Mariani, A.; et al. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 2020, 52, 127–149. [Google Scholar] [CrossRef]
- Choudhary, A.; Bechtold, M.L.; Arif, M.; Szary, N.M.; Puli, S.R.; Othman, M.O.; Pais, W.P.; Antillon, M.R.; Roy, P.K. Pancreatic stents for prophylaxis against post-ERCP pancreatitis: A meta-analysis and systematic review. Gastrointest. Endosc. 2011, 73, 275–282. [Google Scholar] [CrossRef]
- Kubota, K.; Sato, T.; Kato, S.; Watanabe, S.; Hosono, K.; Kobayashi, N.; Hisatomi, K.; Matsuhashi, N.; Nakajima, A. Needle-knife precut papillotomy with a small incision over a pancreatic stent improves the success rate and reduces the complication rate in difficult biliary cannulations. J. Hepato-Biliary-Pancreat. Sci. 2013, 20, 382–388. [Google Scholar] [CrossRef] [PubMed]
- Mazaki, T.; Masuda, H.; Takayama, T. Prophylactic pancreatic stent placement and post-ERCP pancreatitis: A systematic review and meta-analysis. Endoscopy 2010, 42, 842–853. [Google Scholar] [CrossRef] [PubMed]
- Testoni, P.A.; Testoni, S.; Giussani, A. Difficult biliary cannulation during ERCP: How to facilitate biliary access and minimize the risk of post-ERCP pancreatitis. Dig. Liver Dis. 2011, 43, 596–603. [Google Scholar] [CrossRef]
- Freeman, M.L.; Guda, N.M. ERCP cannulation: A review of reported techniques. Gastrointest. Endosc. 2005, 61, 112–125. [Google Scholar] [CrossRef]
- Dumonceau, J.-M.; Andriulli, A.; Devière, J.; Mariani, A.; Rigaux, J.; Baron, T.H.; Testoni, P.A. European Society of Gastrointestinal Endoscopy (ESGE) Guideline: Prophylaxis of post-ERCP pancreatitis. Endoscopy 2010, 42, 503–515. [Google Scholar] [CrossRef]
- Testoni, P.A.; Mariani, A.; Aabakken, L.; Arvanitakis, M.; Bories, E.; Costamagna, G.; Devière, J.; Dinis-Ribeiro, M.; Dumonceau, J.-M.; Giovannini, M.; et al. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2016, 48, 657–683. [Google Scholar] [CrossRef]
- Yoo, Y.W.; Cha, S.-W.; Lee, W.C.; Kim, S.H.; Kim, A.; Cho, Y.D. Double guidewire technique vs transpancreatic precut sphincterotomy in difficult biliary cannulation. World J. Gastroenterol. 2013, 19, 108–114. [Google Scholar] [CrossRef]
- Cotton, P.B.; Lehman, G.; Vennes, J.; Geenen, J.E.; Russell, R.C.; Meyers, W.C.; Liguory, C.; Nickl, N. Endoscopic sphincterotomy complications and their management: An attempt at consensus. Gastrointest. Endosc. 1991, 37, 383–393. [Google Scholar] [CrossRef]
- ASGE Standards of Practice Committee; Chandrasekhara, V.; Khashab, M.A.; Muthusamy, V.R.; Acosta, R.D.; Agrawal, D.; Bruining, D.H.; Eloubeidi, M.A.; Fanelli, R.D.; Faulx, A.L.; et al. Adverse events associated with ERCP. Gastrointest. Endosc. 2017, 85, 32–47. [Google Scholar] [CrossRef]
- Ferreira, L.E.; Baron, T.H. Post-sphincterotomy bleeding: Who, what, when, and how. Am. J. Gastroenterol. 2007, 102, 2850–2858. [Google Scholar] [CrossRef]
- Coté, G.A.; Keswani, R.N.; Jackson, T.; Fogel, E.; Lehman, G.A.; McHenry, L.; Watkins, J.; Sherman, S. Individual and practice differences among physicians who perform ERCP at varying frequency: A national survey. Gastrointest. Endosc. 2011, 74, 65–73.e12. [Google Scholar] [CrossRef] [PubMed]
- Saritas, U.; Üstündağ, Y.; Harmandar, F. Precut sphincterotomy: A reliable salvage for difficult biliary cannulation. World J. Gastroenterol. 2013, 19, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Tse, F.; Yuan, Y.; Bukhari, M.; Leontiadis, G.I.; Moayyedi, P.; Barkun, A. Pancreatic duct guidewire placement for biliary cannulation for the prevention of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis. Cochrane Database Syst. Rev. 2016, 5, CD010571. [Google Scholar] [CrossRef] [PubMed]
- Rabenstein, T.; Ruppert, T.; Schneider, H.T.; Hahn, E.G.; Ell, C. Benefits and risks of needle-knife papillotomy. Gastrointest. Endosc. 1997, 46, 207–211. [Google Scholar] [CrossRef]
- Dowsett, J.F.; Polydorou, A.A.; Vaira, D.; D’Anna, L.M.; Ashraf, M.; Croker, J.; Salmon, P.R.; Russell, R.C.; Hatfield, A.R. Needle knife papillotomy: How safe and how effective? Gut 1990, 31, 905–908. [Google Scholar] [CrossRef]
- Gholson, C.F.; Favrot, D. Needle knife papillotomy in a university referral practice: Safety and efficacy of a modified technique. J. Clin. Gastroenterol. 1996, 23, 177–180. [Google Scholar] [CrossRef]
- Freeman, M.L. Complications of endoscopic biliary sphincterotomy: A review. Endoscopy 1997, 29, 288–297. [Google Scholar] [CrossRef]
- Kim, C.W.; Chang, J.H.; Kim, T.H.; Han, S.W. Sequential double-guidewire technique and transpancreatic precut sphincterotomy for difficult biliary cannulation. Saudi J. Gastroenterol. 2015, 21, 18–24. [Google Scholar] [CrossRef]
- Kapetanos, D.; Kokozidis, G.; Christodoulou, D.; Mistakidis, K.; Dimakopoulos, K.; Katodritou, E.; Kitis, G.; Tsianos, E.V. Case series of transpancreatic septotomy as precutting technique for difficult bile duct cannulation. Endoscopy 2007, 39, 802–806. [Google Scholar] [CrossRef]
- Berry, R.; Han, J.Y.; Tabibian, J.H. Difficult biliary cannulation: Historical perspective, practical updates, and guide for the endoscopist. World J. Gastrointest. Endosc. 2019, 11, 5–21. [Google Scholar] [CrossRef]
- Kylänpää, L.; Koskensalo, V.; Saarela, A.; Ejstrud, P.; Udd, M.; Lindström, O.; Rainio, M.; Tenca, A.; Halttunen, J.; Qvigstad, G.; et al. Transpancreatic biliary sphincterotomy versus double guidewire in difficult biliary cannulation: A randomized controlled trial. Endoscopy 2021, 53, 1011–1019. [Google Scholar] [CrossRef] [PubMed]
- Freeman, M.L.; DiSario, J.A.; Nelson, D.B.; Fennerty, M.B.; Lee, J.G.; Bjorkman, D.J.; Overby, C.S.; Aas, J.; Ryan, M.E.; Bochna, G.S.; et al. Risk factors for post-ERCP pancreatitis: A prospective, multicenter study. Gastrointest. Endosc. 2001, 54, 425–434. [Google Scholar] [CrossRef] [PubMed]
- Andriulli, A.; Loperfido, S.; Napolitano, G.; Niro, G.; Valvano, M.R.; Spirito, F.; Pilotto, A.; Forlano, R. Incidence rates of post-ERCP complications: A systematic survey of prospective studies. Am. J. Gastroenterol. 2007, 102, 1781–1788. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.J.; Hwang, J.C.; Yoo, B.M.; Kim, J.H.; Ryu, H.-K.; Kim, S.S.; Kang, J.K.; Kim, M.K. Wire-guided cannulation over a pancreatic stent versus double guidewire technique in patients with difficult biliary cannulation. BMC Gastroenterol. 2015, 15, 150. [Google Scholar] [CrossRef] [PubMed]
- Akashi, R.; Kiyozumi, T.; Jinnouchi, K.; Yoshida, M.; Adachi, Y.; Sagara, K. Pancreatic sphincter precutting to gain selective access to the common bile duct: A series of 172 patients. Endoscopy 2004, 36, 405–410. [Google Scholar] [CrossRef]
- Miyatani, H.; Yoshida, Y. Endoscopic needle knife precut papillotomy for inaccessible bile duct following failed pancreatic duct access. Ther. Adv. Gastroenterol. Endosc. 2009, 2, S1120. [Google Scholar] [CrossRef]
- Catalano, M.F.; Linder, J.D.; Geenen, J.E. Endoscopic transpancreatic papillary septotomy for inaccessible obstructed bile ducts: Comparison with standard pre-cut papillotomy. Gastrointest. Endosc. 2004, 60, 557–561. [Google Scholar] [CrossRef]
- Lin, L.-F. Transpancreatic precut sphincterotomy for biliary access: The relation of sphincterotomy size to immediate success rate of biliary cannulation. Diagn. Ther. Endosc. 2014, 2014, 864082. [Google Scholar] [CrossRef]
- Sakai, Y.; Tsuyuguchi, T.; Sugiyama, H.; Kurosawa, J.; Saito, M.; Tawada, K.; Mikata, R.; Tada, M.; Ishihara, T.; Yokosuka, O. Transpancreatic precut papillotomy in patients with difficulty in selective biliary cannulation. Hepatogastroenterology 2011, 58, 1853–1858. [Google Scholar] [CrossRef]
- Cha, S.-W.; Leung, W.D.; Lehman, G.A.; Watkins, J.L.; McHenry, L.; Fogel, E.L.; Sherman, S. Does leaving a main pancreatic duct stent in place reduce the incidence of precut biliary sphincterotomy—Associated pancreatitis? A randomized, prospective study. Gastrointest. Endosc. 2013, 77, 209–216. [Google Scholar] [CrossRef]
- Vadalà di Prampero, S.F.; Faleschini, G.; Panic, N.; Bulajic, M. Endoscopic and pharmacological treatment for prophylaxis against postendoscopic retrograde cholangiopancreatography pancreatitis: A meta-analysis and systematic review. Eur. J. Gastroenterol. Hepatol. 2016, 28, 1415–1424. [Google Scholar] [CrossRef] [PubMed]
- Da Cruz Portela, J.C.; Bernardo, W.M.; de Moura, D.T.H.; Franzini, T.A.P.; de Azeredo Coutinho, L.M.; Brunaldi, V.O.; Guedes, H.G.; de Moura, E.T.H.; dos Santos, M.E.L.; Luz, G.O.; et al. Pancreatic stent placement for prevention of post-ERCP pancreatitis in high-risk patients: A systematic review and meta-analysis. J. Pancreas. 2019, 20, 16–23. [Google Scholar]
- Fan, J.-H.; Qian, J.-B.; Wang, Y.-M.; Shi, R.-H.; Zhao, C.-J. Updated meta-analysis of pancreatic stent placement in preventing post-endoscopic retrograde cholangiopancreatography pancreatitis. World J. Gastroenterol. 2015, 21, 7577–7583. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.-Q.; Ning, X.-Y.; Zhan, L.-L.; Tang, G.-D.; Lv, X.-P. Placement of prophylactic pancreatic stents to prevent post-endoscopic retrograde cholangiopancreatography pancreatitis in high-risk patients: A meta-analysis. World J. Gastroenterol. 2014, 20, 7040–7048. [Google Scholar] [CrossRef] [PubMed]
- Dumonceau, J.-M.; Andriulli, A.; Elmunzer, B.J.; Mariani, A.; Meister, T.; Deviere, J.; Marek, T.; Baron, T.H.; Hassan, C.; Testoni, P.A.; et al. Prophylaxis of post-ERCP pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Guideline—Updated June 2014. Endoscopy 2014, 46, 799–815. [Google Scholar] [CrossRef]
- Afghani, E.; Akshintala, V.S.; Khashab, M.A.; Law, J.K.; Hutfless, S.M.; Kim, K.J.; Lennon, A.M.; Kalloo, A.N.; Singh, V.K. 5-Fr vs. 3-Fr pancreatic stents for the prevention of post-ERCP pancreatitis in high-risk patients: A systematic review and network meta-analysis. Endoscopy 2014, 46, 573–580. [Google Scholar] [CrossRef]
- Chahal, P.; Tarnasky, P.R.; Petersen, B.T.; Topazian, M.D.; Levy, M.J.; Gostout, C.J.; Baron, T.H. Short 5Fr vs long 3Fr pancreatic stents in patients at risk for post-endoscopic retrograde cholangiopancreatography pancreatitis. Clin. Gastroenterol. Hepatol. 2009, 7, 834–839. [Google Scholar] [CrossRef]
- Zolotarevsky, E.; Fehmi, S.M.; Anderson, M.A.; Schoenfeld, P.S.; Elmunzer, B.J.; Kwon, R.S.; Piraka, C.R.; Wamsteker, E.-J.; Scheiman, J.M.; Korsnes, S.J.; et al. Prophylactic 5-Fr pancreatic duct stents are superior to 3-Fr stents: A randomized controlled trial. Endoscopy 2011, 43, 325–330. [Google Scholar] [CrossRef]
- Fujisawa, T.; Kagawa, K.; Ochiai, K.; Hisatomi, K.; Kubota, K.; Sato, H.; Nakajima, A.; Matsuhashi, N. Prophylactic Efficacy of 3- or 5-cm Pancreatic Stents for Preventing post-ERCP Pancreatitis. J. Clin. Gastroenterol. 2016, 50, e30–e34. [Google Scholar] [CrossRef]
- Sugimoto, M.; Takagi, T.; Suzuki, R.; Konno, N.; Asama, H.; Sato, Y.; Irie, H.; Watanabe, K.; Nakamura, J.; Kikuchi, H.; et al. Pancreatic stents for the prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis should be inserted up to the pancreatic body or tail. World J. Gastroenterol. 2018, 24, 2392–2399. [Google Scholar] [CrossRef]
- He, Q.; Wang, L.; Peng, C.; Zou, X.; Zhan, Q.; Xu, Y.; Liu, Q.; Qian, J.; Gong, L.; Shen, Y.; et al. Modified prophylactic 5-Fr pancreatic duct stent enhances the rate of spontaneous dislodgement: A multicenter randomized controlled trial. United Eur. Gastroenterol. J. 2018, 6, 1519–1526. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, K.; Katanuma, A.; Maguchi, H. Endoscopic removal technique of migrated pancreatic plastic stents. J. Hepato-Biliary-Pancreat. Sci. 2014, 21, E34–E40. [Google Scholar] [CrossRef] [PubMed]
- Conigliaro, R.; Manta, R.; Bertani, H.; Manno, M.; Barbera, C.; Caruso, A.; Olivetti, G.; Melotti, G.; Frazzoni, M. Pancreatic duct stenting for the duration of ERCP only does not prevent pancreatitis after accidental pancreatic duct cannulation: A prospective randomized trial. Surg. Endosc. 2013, 27, 569–574. [Google Scholar] [CrossRef] [PubMed]
- Dultz, G.; Gerber, L.; Zeuzem, S.; Bojunga, J.; Friedrich-Rust, M. Prolonged retention of prophylactic pancreatic stents is not associated with increased complications. Pancreatology 2019, 19, 39–43. [Google Scholar] [CrossRef] [PubMed]
| Data | SCT, n (%) | TPS, n (%) | p-Value |
|---|---|---|---|
| Gender | 0.939 | ||
| Male Female | 91 (53.5) 79 (46.5) | 33 (54.1) 28 (45.9) | |
| Age, years (mean ± SD) | 69.21 ± 15.81 | 68.98 ± 15.88 | 0.989 |
| BMI, kg/m2 (mean ± SD) | 24.21 ± 3.92 | 24.45 ± 4.49 | 0.556 |
| Indications | 0.337 | ||
| Cholelithiasis BD Cancer/stricture | 138 (81.2) 32 (18.8) | 46 (75.4) 15 (24.6) | |
| Comorbidities | |||
| Diabetes Mellitus Hypertension Chronic Liver Disease Chronic Kidney Disease History of Cholecystectomy History of Pancreatitis Antiplatelet Medication | 48 (28.2) 86 (50.6) 11 (6.5) 8 (4.7) 15 (8.8) 1 (0.6) 51 (30.0) | 15 (24.6) 29 (47.5) 3 (4.9) 1 (1.6) 2 (3.3) 1 (1.6) 13 (21.3) | 0.583 0.683 1.00 0.451 0.251 0.459 0.193 |
| Laboratory Findings | |||
| Hemoglobin, g/dL (mean ± SD) hsCRP, mg/dL (mean ± SD) Total bilirubin, mg/dL (mean ± SD) ALT, IU/L (mean ± SD) Creatinine, mg/dL (mean ± SD) Amylase, U/L (mean ± SD) Lipase, U/L (mean ± SD) | 12.66 ± 1.77 4.49 ± 5.95 4.17 ± 5.19 197.14 ± 212.70 1.06 ± 1.35 61.34 ± 25.62 42.42 ± 28.99 | 12.98 ± 1.49 3.26± 5.37 3.99± 4.64 168.82 ± 180.91 0.87 ± 0.24 65.59 ± 27.83 43.00 ± 27.83 | 0.201 0.158 0.809 0.355 0.266 0.181 0.893 |
| Periampullary Diverticulum | 64 (37.6) | 19 (31.1) | 0.364 |
| Image findings | |||
| Diameter of PD, mm (mean ± SD) Diameter of BD, mm (mean ± SD) | 2.16 ± 1.65 13.49 ± 5.31 | 2.01 ± 1.08 14.31 ± 5.17 | 0.524 0.304 |
| Complications | SCT, n (%) | TPS, n (%) | p-Value |
|---|---|---|---|
| Post-ERCP Hyperamylasemia | 49/170 (28.8%) | 32/61 (52.5) | 0.001 * |
| Overall PEP † | 6/170 (3.5) | 1/61 (1.6) | 0.679 |
| Mild | 5/170 (2.9) | 1/50 (1.6) | |
| Moderate | 1/170 (0.6) | 0/50 (0.0) | |
| Severe | 0/170 (0.0) | 0/50 (0.0) | |
| Overall PSB | 13/170 (7.6) | 4/61 (6.6) | 1.00 |
| Clinically Insignificant | 10/170 (5.9) | 4/61 (6.6) | 0.765 |
| Hemostatic Procedure | 3/170 (1.8) | 0/61 (0.0) | 0.568 |
| Clinically Significant ‡ | 3/170 (1.8) | 0/61 (0.0) | 0.568 |
| Mild Moderate Severe | 2/170 (1.2) 1/170 (0.6) 0/170 (0.0) | 0/61 (0.0) 0/61 (0.0) 0/61 (0.0) | |
| Perforation | 0/168 (0.0) | 0/61 (0.0) | NA |
| SCT | Difficult Cannulation | ||
|---|---|---|---|
| TPS | NKP | ||
| Success Rate for Deep SBC, n (%) | 180/247 (72.9) | 59/64 (92.2) | 7/8 (87.5) |
| Total ERCP Procedure Time, min (mean ± SD) | 19.5 ± 11.4 | 26.3 ± 12.9 | 41.8 ± 11.8 |
| Total Cannulation Time, min (mean ± SD) | 3.2 ± 2.0 | 9.4 ± 11.5 | 31.9 ± 12.0 |
| Time to Selective BC †, min (mean ± SD) | 3.2 ± 2.0 | 6.0 ±10.6 | 10.9 ± 9.6 |
| n | (%) | |
|---|---|---|
| Successful Spontaneous Dislodgement | 60/61 | 98.4 |
| Within 12 h | 0/61 | 0.0 |
| Within 48 h | 5/61 | 8.2 |
| Within 2 weeks | 40/61 | 65.6 |
| Within 8 weeks | 15/61 | 24.6 |
| Failed Spontaneous Dislodgement | 1/61 | 4.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ryu, J.; Paik, K.-H.; Kwon, C.-I.; Koh, D.H.; Song, T.J.; Jeong, S.; Park, W.S. The Safety and Efficacy of an Unflanged 4F Pancreatic Stent in Transpancreatic Precut Sphincterotomy for Patients with Difficult Biliary Cannulation: A Prospective Cohort Study. J. Clin. Med. 2022, 11, 5692. https://doi.org/10.3390/jcm11195692
Ryu J, Paik K-H, Kwon C-I, Koh DH, Song TJ, Jeong S, Park WS. The Safety and Efficacy of an Unflanged 4F Pancreatic Stent in Transpancreatic Precut Sphincterotomy for Patients with Difficult Biliary Cannulation: A Prospective Cohort Study. Journal of Clinical Medicine. 2022; 11(19):5692. https://doi.org/10.3390/jcm11195692
Chicago/Turabian StyleRyu, Jieun, Kyu-Hyun Paik, Chang-Il Kwon, Dong Hee Koh, Tae Jun Song, Seok Jeong, and Won Suk Park. 2022. "The Safety and Efficacy of an Unflanged 4F Pancreatic Stent in Transpancreatic Precut Sphincterotomy for Patients with Difficult Biliary Cannulation: A Prospective Cohort Study" Journal of Clinical Medicine 11, no. 19: 5692. https://doi.org/10.3390/jcm11195692
APA StyleRyu, J., Paik, K.-H., Kwon, C.-I., Koh, D. H., Song, T. J., Jeong, S., & Park, W. S. (2022). The Safety and Efficacy of an Unflanged 4F Pancreatic Stent in Transpancreatic Precut Sphincterotomy for Patients with Difficult Biliary Cannulation: A Prospective Cohort Study. Journal of Clinical Medicine, 11(19), 5692. https://doi.org/10.3390/jcm11195692






