Abstract
(1) Background: Thrombophilia testing utility has remained controversial since its clinical introduction, because data on its influence on treatment decisions are limited. (2) Methods: We conducted a single-center retrospective cohort study of 3550 unselected patients referred for thrombophilia consultation at the Bern University Hospital in Switzerland from January 2010 to October 2020. We studied the influence of thrombophilia testing results on treatment decisions and evaluated the association between thrombophilia and thromboembolic and pregnancy-related morbidity events after testing up to 03/2021. (3) Results: In 1192/3550 patients (34%), at least one case of thrombophilia was found and 366 (10%) had high-risk thrombophilia. A total of 211/3550 (6%) work-ups (111/826 (13%) with low-risk thrombophilia and 100/366 (27%) with high-risk thrombophilia) led to an appropriate decision to extend or initiate anticoagulation, and 189 (5%) negative results led to the withholding of anticoagulation therapy inappropriately. A total of 2492 patients (69%) were followed up for >30 days, with a median follow-up of 49 months (range, 1–183 months). Patients with high-risk thrombophilia had a higher risk of subsequent venous thromboembolic events and pregnancy-related morbidity compared to those without thrombophilia. (4) Conclusions: Our study demonstrated the limited usefulness of thrombophilia work-up in clinical decision-making. High-risk thrombophilia was associated with subsequent venous thromboembolism and pregnancy-related morbidity.
1. Introduction
The clinical utility of thrombophilia testing has remained a subject of controversy since its introduction in clinical practice [1]. As guidelines of thrombophilia testing include only conditional recommendations, patterns of thrombophilia testing vary strongly across centers [2,3,4,5]. Considering the high cost of the work-up, testing is dependent on patients’ and physicians’ individual preference, financial status and the local healthcare system [6]. Moreover, the influence of test results on treatment decisions is still a matter of ongoing debate [1,4].
Data showing the clinical usefulness and benefits of positive thrombophilia testing results for further clinical decisions on treatment after venous thromboembolism (VTE) are limited. Garcia-Horton et al. showed the limited relevance of thrombophilia work-up in clinical decision-making after unprovoked VTE at a tertiary thrombosis center in Canada [7]. Given the growing body of evidence of the rather limited impact of thrombophilia upon the recurrence of VTE and overall mortality [8,9,10,11,12], current scientific data emphasize strict but variable selection criteria for thrombophilia testing [5,13,14,15,16,17].
Since most studies on thrombophilia testing focus on accuracy and guideline interpretation [18,19,20], the quantification of its guidance on treatment decisions and impact on VTE outcome remains unclear. The potential negative effect of withholding anticoagulation or overtreating patients because of the work-up is being debated, whereas its significance is uncertain [1]. Thrombophilia work-up and its clinical consequences in patients with arterial thrombosis, pregnancy-related morbidities or asymptomatic thrombophilia carriers is even less defined [21,22,23,24] and clinical trials in this context are absent [25].
To investigate the impact of thrombophilia testing on the management and clinical course of thromboembolic disease and pregnancy-related morbidity, we conducted a large 10-year single-center retrospective cohort study. We analyzed the work-up patterns of thrombophilia and their impact on treatment decisions, and the subsequent occurrence of venous and arterial thrombosis and pregnancy-related morbidities.
2. Materials and Methods
2.1. Study Design and Patients
A single-center retrospective cohort study was conducted at the Department of Hematology of the Bern University Hospital in Switzerland between January 2010 and October 2020. We systematically screened consecutive patients referred for testing of hereditary and/or acquired thrombophilia by general practitioners or non-hematologist medical specialists with the support of the hospital data management service using internal specified codes for thrombophilia work-up. Patients with general consent were included if thrombophilia testing was performed and they had a documented history of objectively confirmed VTE and/or arterial thrombosis in any location, a history of pregnancy-related morbidity or were referred for thrombophilia testing due to a positive family history for VTE or hereditary thrombophilia.
The objective diagnosis of deep vein thrombosis (DVT), superficial vein thrombosis and muscle vein thrombosis was defined by a positive compression ultrasonography or venography [26], and pulmonary embolism (PE) was defined by a new high-probability ventilation/perfusion lung scan or a new contrast filling defect on spiral computed tomography (CT) or pulmonary angiography [26]. Arterial thrombosis was defined by the presence of stroke on brain magnetic resonance (MR) imaging or CT or by a diagnostic coronary angiography in patients with myocardial infarction [27,28]. A critical limb ischemia of a peripheral artery disease was established by arterial Doppler ultrasound, CT angiography, MR angiography or catheter-based arteriography [29]. Renal artery or vein thrombosis, splanchnic vein thrombosis, cerebral vein thrombosis and thrombosis of aorta and vena cava were defined as filling defects in the corresponding vessel on CT or MR angiography or venography [30,31,32]. Other types of thromboembolism, such as retinal vein or artery thrombosis, penis vein thrombosis, osteonecrosis or chronic inflammatory disease, along with pregnancy-related morbidity, were defined by relevant specialists using a referral report. Pregnancy-related morbidities were defined as pregnancy loss at all gestational ages, placenta failure, preeclampsia [33] and HELLP syndrome (hemolysis, elevated liver enzyme levels, low platelet count) according to obstetrical diagnostic criteria [34].
Clinical data were collected from structured electronic forms using a standardized case report form and entered into a computerized database (REDCap software) by two persons. Data comprised demographic characteristics of patients and their family history of VTE in first- and second-degree relatives, details of all previous thrombotic events or pregnancy-related morbidity (date and location), risk factors for most recent VTE and arterial thrombosis event (namely heavy smoking (>20 pack years), immobilization > 4 h, infections requiring bedrest > 3 days, estrogen-based medications, pregnancy and peripartum, intravenous catheters, active cancer, obesity (body mass index [BMI] > 30 kg m−2), trauma, surgery, cancer medication, presence of extended varicose veins, patent foramen ovale or other septal defect) and co-morbidities (diabetes mellitus, arterial hypertension, liver cirrhosis, kidney failure, rheumatic disease, depression, chronic inflammatory disease, dyslipidemia, cardiovascular diseases, pulmonary diseases, neurological diseases).
2.2. Thrombophilia Testing
Thrombophilia testing was performed between 3 and 6 months following the index event, after the evaluation of the patient by a hematologist, taking into consideration age, risk factors, family history of VTE, co-morbidities and type of thrombosis or pregnancy-related morbidity. A thrombophilia work-up was considered as “performed” if one or more of the following thrombophilia parameters were tested: factor V Leiden (FVL) mutation status, prothrombin gene 20210G>A mutation status, protein C (PC) and antithrombin (AT) activity as well as free protein S (PS) antigen, lupus anticoagulant (LA), anticardiolipin antibodies and anti-β2-glycoprotein I antibodies. Only results of accurate thrombophilia testing were considered, excluding PC and PS testing whilst on vitamin K antagonists (VKA) or PS level during pregnancy.
Testing for PC (Protein C Berichrom®, Siemens, Marburg, Germany; Protein C COAG, Siemens, Marburg, Germany), PS (Free protein S, Asserachrom®, Diagnostica Stago, Asnières, France from 2010 to 2015,; Free Protein S Antigen, Innovance®, Siemens, Marburg, Germany from 2015 to 2020) and AT activity (LR Antithrombin, Coamatic®, Diapharma, Bedford, USA from 2010 to 2013; LRT Antithrombin, Biophen®, Endotell, Allschwil, Switzerland from 2013 to 2014, and Antithrombin Innovance®, Siemens, Marburg, Germany from 2014 to 2020) was performed in the routine hemostasis laboratory (Bern University Hospital). Antiphospholipid antibodies were tested using Varelisa diagnostic kits (Phadia®, ThermoFisher, Freiburg, Germany) from 2010 to 2014, fluorescence enzyme immunoassay (Phadia® 250, ThermoFisher, Freiburg, Germany) from 2014 to 2015 and automated chemiluminescence assay (Bio-flash®, Inova Diagnostics, San Diego, USA) from 2015 to 2020 and dilute Russell’s viper venom time (Cryocheck®, Endotell, Allschwil, Switzerland). The diagnosis of an antiphospholipid antibody syndrome was established by persistent laboratory evidence of antiphospholipid antibodies at least 12 weeks later and the presence of VTE, arterial thrombosis or criteria pregnancy-related morbidity [35]. Genetic mutations were detected by the polymerase chain reaction method (FVL and Prothrombin, RealFast Assay®, Vienna Lab Diagnostics, Vienna, Austria).
2.3. Classification of Thrombophilia and Risk Factors
Categorization as minor and major provoking risk factors was based on the guidance provided by the International Society on Thrombosis and Haemostasis (ISTH) [36]. In addition to the ISTH-based criteria, the presence of an intravenous catheter [37] and May-Thurner syndrome (>70% iliofemoral compression) [38] were categorized as major risk factors, whereas immobilization > 4 h [39] and heavy smoking (>20 pack years) [40] as minor risk factors. VTE in the presence of merely an environmental risk factor (male sex and older age) was categorized as unprovoked thromboembolism.
Minor thrombophilia was defined as isolated heterozygous FVL or prothrombin 20210G>A mutation according to institutional guidelines. AT activity < 70%, PC activity < 69% and PS free antigen < 59%, antiphospholipid antibody syndrome, homozygous FVL or prothrombin 20210G>A or any compound thrombophilias were considered as high-risk thrombophilia.
2.4. Follow-Up and Outcomes
The primary study outcome was the influence of thrombophilia testing on anticoagulation management decisions. Secondary outcomes included the occurrence of first or recurrent VTE, arterial thrombosis or pregnancy-related morbidity after thrombophilia testing.
The influence of thrombophilia testing on management decisions was assessed from a structured medical report of each patient by two persons and classified as follows: (1) no influence on management; (2) appropriate management decision and (3) results not considered/overlooked, meaning a positive or potential positive influence; (4) decision to overtreat and (5) decision to undertreat, showing a negative influence (Table 1). Because of the implementation of a structured reporting form at our center before 2010, considering clinical and laboratory factors leading to the choice of management, we were able to document clinical decisions on treatment that were merely based on thrombophilia. Therefore, management decisions based on clinical characteristics of thrombotic event (e.g., unprovoked or recurrent VTE), patient family history for VTE, preferences or high-bleeding risk were categorized as non-influential, irrespective of the thrombophilia result. We exclusively assessed the thrombophilia-based management decisions on prophylactic and therapeutic anticoagulation treatment, and did not consider other decisions or patient education, such as avoidance of estrogen-based treatment, change in type of anticoagulant or lifestyle modification. Guidance for the appropriateness of management decisions regarding thrombotic events, pregnancy-related morbidity or asymptomatic carriership of thrombophilia was based on international guidelines [16,17,41,42].

Table 1.
Classification of thrombophilia result influence on treatment decisions.
Data from all complete hospital records, including other disciplines, for the identification of subsequent VTE, arterial thrombosis or pregnancy-related morbidity after the thrombophilia consultation were investigated until March 2021. Only objectively confirmed events, according to the previously mentioned inclusion criteria, were considered. As 36 patients had a partial thrombophilia work-up before January 2010 in our clinic and were referred for a second time, the start of the follow-up time was defined by the first performed work-up from December 2004 to March 2021. For time-to-event analyses, we considered only patients with a follow-up >30 days and censored patients at the time of last hospital record or time of event.
2.5. Statistical Analysis
Continuous variables are presented as mean ± standard deviation (SD) and were compared using one-way ANOVA. Categorical variables are shown as percentages and compared with x2 test. Univariable logistic regression models were used to assess the influence of thrombophilia on treatment decisions. As the negative result did not lead to any influence on treatment, heterozygous FVL mutation was used as a reference due to its lowest impact on treatment decision. Associations between low- and high-risk thrombophilia and the time to new thrombotic event or pregnancy-related morbidity were assessed using Cox proportional hazard models, yielding hazard ratios (HR) with their corresponding 95% confidence intervals (CI) and p-values for the failure event of primary interest. We adjusted the models for previously published predictors of venous and arterial thrombosis, including age > 50 years, male sex and risk factors and co-morbidities, such as smoking, diabetes mellitus, obesity, arterial hypertension, kidney failure, dyslipidemia, depression, chronic inflammatory disease and active cancer [43,44,45]. The Kaplan–Meier method was used to plot time from work-up for thrombophilia to recurrence of new thrombotic event or pregnancy-related morbidity. Only complete case analysis was performed, without an attempt to replace missing values with imputation methods. A value of p < 0.05 was considered statistically significant. All analyses were performed with R 4.1.1 and figures were edited with GraphPad Prism v9.1.2.
3. Results
3.1. Study Cohort
Of 5064 patients screened for eligibility, we excluded 1356 patients (27%) without general consent, 136 patients (3%) because no thrombophilia work-up was performed and 22 patients (0.4%) because of the absence of the objective documentation of thromboembolism or pregnancy-related morbidity, leaving a study sample of 3550 patients (Figure 1). Of them, 2429 patients (68%) had a follow-up of more than 30 days and were considered for time-to-event analysis. Their median follow-up duration was 49 months (range, 1–183 months).
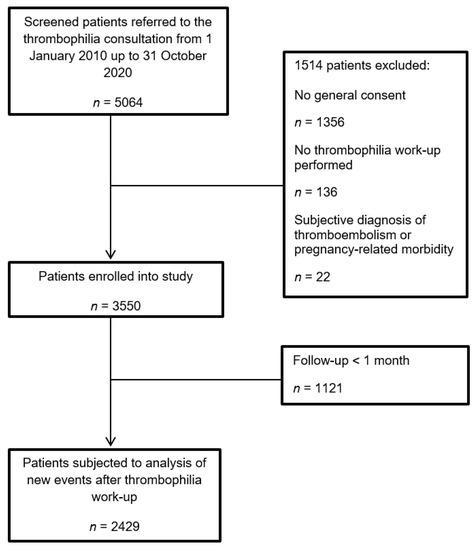
Figure 1.
Flow diagram of patients.
At the time of thrombophilia work-up, the mean age was 42 years (±15) and 2118 patients (60%) were women (Table 2). Most patients (2343, 66%) were referred because of VTE, mainly DVT and/or PE (1791/2343, 76%), whereas 583 (16%) patients had a positive history of unexplained arterial thrombosis, mainly stroke (444/583, 76%) (Supplemental Table S1). A total of 504 (14%) patients had no prior thromboembolic event, but a positive family history for VTE in first-degree (306/504, 61%) or second-degree (143/504, 28%) relatives. A minority of referrals were due to pregnancy-related morbidity (120, 3%). Most patients (1999, 56%) had no documented co-morbidities and one third (1259, 35%) had no documented risk factors for VTE or arterial thrombosis (Table 2). Co-morbidities and risk factors of the cohort patients are presented in Supplemental Table S1, comprising mostly arterial hypertension (578, 16%) and dyslipidemia (405, 11%) as risk factors for arterial thrombosis, and immobilization > 4 h (743, 21%) and estrogen-based medication (706, 20%) representing minor risk factors for VTE. The major risk factors for VTE were found in 415 (12%) cohort patients (Table 2).

Table 2.
Clinical characteristics of the patients included in the study in accordance with thrombophilia work-up result.
3.2. Prevalence of Thrombophilia in the Cohort Study
A total of 1260 thrombophilias were found in 1192 (34%) patients. The most common type of thrombophilia was heterozygous FVL mutation (714 patients, 20%), followed by heterozygous prothrombin 20210G>A mutation (193 patients, 5%) and antiphospholipid antibody syndrome (119 patients, 3%) (Figure 2). One hundred and seven patients (3%) had more than one thrombophilia. Patients with thrombophilia were younger and were less likely to have co-morbidities or risk factors. More patients with thrombophilia were referred because of a recurrent VTE. Patients with arterial thrombosis had significantly less positive thrombophilia results compared to other patient groups, whereas women with pregnancy-related morbidities and asymptomatic patients with a positive family history were more likely to test positive (Table 2).
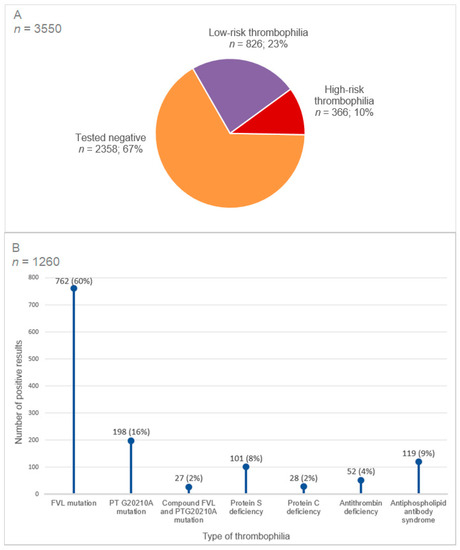
Figure 2.
Prevalence of thrombophilia in the cohort. (A) Prevalence of high-risk and low-risk thrombophilia in the cohort. (B) Type of thrombophilia in the cohort. Abbreviations: FVL, factor V Leiden; PT, prothrombin. Testing was not performed or missing for presence of FVL mutation (6%), PT G20210A mutation (13%), antithrombin deficiency (20%), protein C deficiency (30%), protein S deficiency (29%) and antiphospholipid antibody syndrome (11%). Low-risk thrombophilia comprises heterozygous factor V Leiden or heterozygous prothrombin 20210G>A mutation. High-risk thrombophilia comprises homozygous factor V Leiden mutation, homozygous prothrombin 20210G>A mutation, antithrombin < 70%, protein C < 69% and protein S < 59%, antiphospholipid antibody syndrome and compound thrombophilias.
3.3. Impact of Thrombophilia Testing on Treatment Decisions
In 3050 patients (86%), a thrombophilia work-up did not have any influence on the treatment decision, mostly when patients tested negative (2171 patients, 71%) or confirming low-risk thrombophilia (671 patients, 22%) (Table 3). A total of 211 positive work-ups (6%) led to an appropriate decision to extend or initiate anticoagulation; 82 positive work-ups (2.2%) were inappropriately overlooked—21 (26%) with antiphospholipid antibody syndrome, 20 (24%) with heterozygous factor V Leiden mutation and 14 (17%) with heterozygous prothrombin 20210G>A mutation. Of 195 patients (5.4%) with an inappropriate treatment decision, 181 patients (93%) had a negative thrombophilia work-up. Only 11 patients (0.3%) had a positive work-up that led to overtreatment.

Table 3.
Influence of thrombophilia work-up on treatment decision.
The presence of antiphospholipid antibody syndrome had the highest positive influence on treatment decision (71/119, 60%), followed by high-risk hereditary thrombophilia (86/247, 35%) (Table 3). However, only 17% positive results (136/826) for low-risk thrombophilia led to a change in treatment, and merely 116 out of 714 (16%) carrierships of a heterozygous FVL mutation provided further guidance (Supplemental Table S2). Compared with the presence of a heterozygous FVL mutation, antiphospholipid antibody syndrome (odds ratio (OR), 8.26; 95% CI, 5.40–12.62), AT deficiency (OR, 5.15; 95% CI, 2.84–9.34) and homozygous FVL mutation (OR, 3.93; 95% CI, 2.10–7.34) influenced further treatment the most (Table 4).

Table 4.
Influence of the type of thrombophilia on therapy.
3.4. Association between Thrombophilia and Thromboembolic Events or Pregnancy-Related Morbidity during Follow-Up
In 2429 patients with follow-up >30 days, 255 events (10.5%) occurred, comprising 142 VTE (5.8%), 91 arterial thrombosis (3.7%) and 22 pregnancy-related morbidities (1.4% of women with follow-up) during the follow-up period, which corresponds to an incidence rate per 100 person years of 1.4 (95% CI, 1.2–1.7), 0.89 (95% CI, 0.72–1.1) and 0.21 (95% CI, 0.13–0.32), respectively. Distributions of clinical characteristics and prevalence of thrombophilia of patients with and without follow-up for>30 days are represented in Supplemental Table S3.
Compared with patients without thrombophilia, patients with high-risk thrombophilia had a higher risk of VTE (adjusted HR, 2.55; 95% CI, 1.49–4.35) during follow-up, and patients with antiphospholipid antibody syndrome a higher risk of VTE (adjusted HR, adjusted HR, 2.50; 95% CI, 1.20–5.19) and pregnancy-related morbidity (HR, 3.86; 95% CI, 1.07–13.97) during follow-up (Figure 3, Table 5). Low-risk thrombophilia was not associated with venous or arterial thrombosis or pregnancy-associated morbidity during follow-up. None of the thrombophilias was associated with arterial thrombosis during follow-up (Figure 3, Table 5). Notably, hereditary high-risk thrombophilia and antiphospholipid antibody syndrome were not only associated with a subsequent VTE during follow-up in the entire study cohort, but also with recurrent VTE, after the exclusion of patients with arterial thrombosis and pregnancy-related morbidity and asymptomatic patients (HR, 2.00; 95% CI, 1.12- 3.57; and HR, 2.82; 95% CI, 1.28–6.29, respectively).
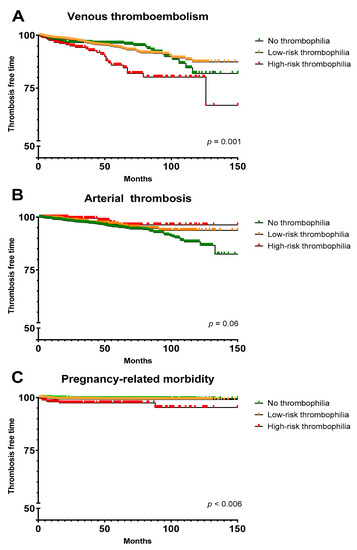
Figure 3.
Kaplan–Meier survival curves in patients with no thrombophilia, low-risk thrombophilia and high-risk thrombophilia. (A) Patients with subsequent venous thromboembolism. (B) Patients with subsequent arterial thrombosis. (C) Women with subsequent pregnancy-related morbidity. Due to small sample size, a modification of y-axis scale was applied for presentation purposes. Low-risk thrombophilia comprises heterozygous factor V Leiden or heterozygous prothrombin 20210G>A mutation. High-risk thrombophilia comprises homozygous factor V Leiden mutation, homozygous prothrombin 20210G>A mutation, antithrombin < 70%, protein C < 69% and protein S < 59%, antiphospholipid antibody syndrome and compound thrombophilias.

Table 5.
Cause-specific hazard ratios for subsequent events after thrombophilia testing during follow-up according to thrombophilia status.
4. Discussion
In this large retrospective cohort study of 3550 patients performed at a single tertiary hematology department, we evaluated the impact of thrombophilia work-up and its result on treatment decisions, as well as the association between thrombophilia and thromboembolic events and pregnancy-related morbidity, in a real-world setting. In 86% of patients in this cohort, the result of the thrombophilia work-up did not lead to a change in treatment decision, while, in 5% of the cohort, patients’ anticoagulation was withheld inappropriately because of a negative thrombophilia work-up. Positive work-ups for hereditary high-risk thrombophilia and antiphospholipid antibody syndrome had significantly more influence on treatment decisions compared to low-risk thrombophilia, and patients with these thrombophilias were more likely to develop subsequent VTE and pregnancy-related morbidity during follow-up.
Considering that the aim of our study was to demonstrate the utility of thrombophilia work-up in a real-world setting in a tertiary care center, the cohort reflected the expected clinical characteristics of patients pre-selected by general practitioners or other specialists. Therefore, the cohort comprised young patients with few co-morbidities or major risk factors for thromboembolism. The prevalence of thrombophilia was in line with previously reported cohorts of thrombophilia work-up in Europe [21,46,47,48]. Data from our center show the limited clinical utility of thrombophilia work-up in reference to the length of anticoagulation in already pre-selected younger patients, which is in line with the findings of a few other studies in smaller, combined inpatient and outpatient VTE or arterial thrombosis cohorts from a tertiary non-hematologic care center [49,50] and tertiary hematology center [6]. Furthermore, an adverse outcome of the work-up could be demonstrated in terms of the withholding of indicated anticoagulant treatment in 5% of the cohort patients due to a negative thrombophilia work-up. Although a high-risk thrombophilia was only found in 10% of the cohort patients, it contributed to the treatment decision in 4.3% of cohort patients, providing a greater impact compared to low-risk hereditary thrombophilia. Besides continuous training to interpret the results of thrombophilia work-up, better-defined predictive factors for hereditary and acquired high-risk thrombophilia are needed to increase the utility of the work-up.
The presence of high-risk hereditary thrombophilia and antiphospholipid antibody syndrome was independently associated with subsequent and recurrent VTE and antiphospholipid antibody syndrome with pregnancy-related morbidity after the work-up. Although the thrombophilia risk for first VTE is well established [51], data on the recurrence of VTE are less clear. Multiple reports indicate no association of a positive thrombophilia result with the recurrence of VTE, mostly in low-risk hereditary thrombophilia [9,10,12], and heterogeneous results on recurrent pregnancy morbidity [52,53,54] with the exception of antiphospholipid antibody syndrome [55]. However, data on hereditary high-risk thrombophilia are limited and studies including the whole panel of thrombophilia are sparse. To our knowledge, this is the first study reporting on new and recurrent thrombotic events and pregnancy-related morbidity after the work-up, including all types of main thrombophilia and indications of testing from real-world practice. Therefore, it seems that despite the treatment change due to high-risk thrombophilia, it still has an impact on the clinical course of VTE and pregnancy-related morbidities and its clinical management should be further investigated.
Our study has several limitations. Firstly, the retrospective study design may have introduced selection and information bias due to the possible misclassification of primary outcomes. Nevertheless, because of the introduction of a structured reporting system and testing pattern in our center before 2010, and cross-evaluation of the data by two individuals, missing values and random errors were limited. Secondly, we could not consistently retrieve information on death, major bleeding and anticoagulation status at the time of subsequent thrombotic events and pregnancy-related morbidity due to insufficient documentation of these events and regulatory restrictions to search civil registries for death. Therefore, our findings do not allow the balancing of the risks and benefits of anticoagulant interventions and treatment decisions, and, moreover, analyses could not be adjusted for death as a competing event, which may lead to biased outcome rates. Thirdly, the definition of high-risk thrombophilia is not well established and may be debatable, especially in the context of pregnancy-related morbidity. Nevertheless, the study gives a new, comprehensive insight into the impact and outcome of thrombophilia work-up and its result. Fourthly, a very small proportion of patients with PS type II deficiency might have been missed, because no systemic measurement of PS activity was performed. Lastly, we evaluated the impact of thrombophilia on prophylactic and therapeutic anticoagulation treatment and did not consider other positive aspects of the work-up, such as a change in anticoagulant in reference to antiphospholipid antibody syndrome or any other high-risk thrombophilia, stronger motivation for lifestyle modification, avoidance of estrogen-based treatments or positive psychological effects of testing negative. Therefore, no conclusions can be made about the overall benefit–risk balance of the testing.
In conclusion, we found that the benefit of thrombophilia testing is limited in already pre-selected outpatients and has some adverse effects on the clinician’s management of anticoagulation in all types of index thrombotic events and pregnancy-related morbidity. Better selection criteria to identify patients who may benefit from testing for hereditary and acquired high-risk thrombophilia are needed to improve the diagnostic and therapeutic yield of thrombophilia work-up and reduce the risk of inappropriate management decisions based on negative tests, the high costs of the investigations and the unfavorable impact on the psychological status of patients due to the results of unnecessary tests. Therefore, the clinical utility of the current selection criteria and the strongest factors associated with treatment should be investigated in order to establish better clinically oriented testing guidelines for thrombophilia work-up.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11144188/s1, Table S1: Clinical characteristics of cohort patients in accordance with thrombophilia work-up result; Table S2: Influence of different thrombophilias on treatment decisions; Table S3: Clinical characteristics and prevalence of thrombophilia in cohort patients according to follow-up status.
Author Contributions
Conceptualization, K.V.-B., T.T. and A.A.-S.; methodology, K.V.-B. and A.A.-S.; software, A.H.; validation, A.H., K.V.-B., A.A.-S. and H.B.; formal analysis, A.H.; investigation, K.V.-B., A.A.-S. and H.B.; data curation, K.V.-B., H.B. and J.B.; writing—original draft preparation, K.V.-B. and T.T.; writing—review and editing, K.V.-B., T.T., K.A.J., D.A., A.R., J.A.K.H. and N.A.P.; visualization, K.V.-B.; supervision, A.A.-S.; project administration, K.V.-B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by Swiss Ethics Committee, Project ID: 2019-02102.
Informed Consent Statement
Patient consent was waived according to the Swiss Ethics Committee, as the further use of health-related datasets and samples is permissible without the consent of the participants if all criteria of Articles 34 and 37–40 of the Swiss Human Research Act are fulfilled, as was the case for this study.
Data Availability Statement
There were no publicly archived datasets analyzed or generated during the study.
Conflicts of Interest
T.T. is an investigator of the CanVECTOR Network; the Network receives grant funding from the Canadian Institutes of Health Research (CDT-142654). The remaining authors declare no competing financial interests. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Middeldorp, S. Inherited thrombophilia: A double-edged sword. Hematol. Am. Soc. Hematol. Educ. Program. 2016, 2016, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Connors, J.M. Thrombophilia Testing and Venous Thrombosis. N. Engl. J. Med. 2017, 377, 1177–1187. [Google Scholar] [CrossRef] [PubMed]
- Ulas, T.; Dal, M.S. Should we screen hereditary thrombophilia testing in patients with provoked/unprovoked venous thromboembolism? Int. J. Cardiol. 2018, 271, 323. [Google Scholar] [CrossRef]
- Khan, F.; Le Gal, G.; Rodger, M.A. The authors respond to “Thrombophilia testing in venous thromboembolism”. CMAJ 2018, 190, E172. [Google Scholar] [CrossRef] [PubMed]
- De Stefano, V.; Rossi, E. Testing for inherited thrombophilia and consequences for antithrombotic prophylaxis in patients with venous thromboembolism and their relatives. A review of the Guidelines from Scientific Societies and Working Groups. Thromb. Haemost. 2013, 110, 697–705. [Google Scholar] [PubMed]
- Gaddh, M.; Cheng, E.; Elsebaie, M.A.; Bodó, I. Clinical Utilization and Cost of Thrombophilia Testing in Patients with Venous Thromboembolism. TH Open 2020, 4, e153–e162. [Google Scholar] [CrossRef]
- Garcia-Horton, A.; Kovacs, M.J.; Abdulrehman, J.; Taylor, J.E.; Sharma, S.; Lazo-Langner, A. Impact of thrombophilia screening on venous thromboembolism management practices. Thromb. Res. 2017, 149, 76–80. [Google Scholar] [CrossRef]
- Reitter-Pfoertner, S.; Waldhoer, T.; Mayerhofer, M.; Eigenbauer, E.; Ay, C.; Mannhalter, C.; Kyrle, P.A.; Pabinger, I. The influence of thrombophilia on the long-term survival of patients with a history of venous thromboembolism. Thromb. Haemost. 2013, 109, 79–84. [Google Scholar] [CrossRef]
- Coppens, M.; Reijnders, J.H.; Middeldorp, S.; Doggen, C.J.M.; Rosendaal, F.R. Testing for inherited thrombophilia does not reduce the recurrence of venous thrombosis. J. Thromb. Haemost. 2008, 6, 1474–1477. [Google Scholar] [CrossRef]
- Lian, T.-Y.; Lu, D.; Yan, X.-X.; Tan, J.-S.; Peng, F.-H.; Zhu, Y.-J.; Wei, Y.-P.; Wu, T.; Sun, K.; Jiang, X.; et al. Association between congenital thrombophilia and outcomes in pulmonary embolism patients. Blood Adv. 2020, 4, 5958–5965. [Google Scholar] [CrossRef]
- Baglin, T.; Luddington, R.; Brown, K.; Baglin, C. Incidence of recurrent venous thromboembolism in relation to clinical and thrombophilic risk factors: Prospective cohort study. Lancet 2003, 362, 523–526. [Google Scholar] [CrossRef]
- Christiansen, S.C.; Cannegieter, S.C.; Koster, T.; Vandenbroucke, J.P.; Rosendaal, F.R. Thrombophilia, Clinical Factors, and Recurrent Venous Thrombotic Events. JAMA 2005, 293, 2352–2361. [Google Scholar] [CrossRef] [PubMed]
- Colucci, G.; Tsakiris, D.A. Thrombophilia screening revisited: An issue of personalized medicine. J. Thromb. Thrombolysis 2020, 49, 618–629. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, N.; Visweshwar, N.; Jaglal, M.; Sokol, L.; Laber, D. Evolving paradigm in thrombophilia screening. Blood Coagul. Fibrinolysis 2019, 30, 249–252. [Google Scholar] [CrossRef] [PubMed]
- McCormack, T.; Harrisingh, M.C.; Horner, D.; Bewley, S. Venous thromboembolism in adults: Summary of updated NICE guidance on diagnosis, management, and thrombophilia testing. BMJ 2020, 369, m1565. [Google Scholar] [CrossRef] [PubMed]
- Stevens, S.M.; Woller, S.C.; Bauer, K.A.; Kasthuri, R.; Cushman, M.; Streiff, M.; Lim, W.; Douketis, J.D. Guidance for the evaluation and treatment of hereditary and acquired thrombophilia. J. Thromb. Thrombolysis 2016, 41, 154–164. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Cushman, M.; Burnett, A.E.; Kahn, S.R.; Beyer-Westendorf, J.; Spencer, F.A.; Rezende, S.M.; Zakai, N.A.; Bauer, K.A.; Dentali, F.; et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: Prophylaxis for hospitalized and nonhospitalized medical patients. Blood Adv. 2018, 2, 3198–3225. [Google Scholar] [CrossRef]
- Kwon, A.J.; Roshal, M.; DeSancho, M.T. Clinical adherence to thrombophilia screening guidelines at a major tertiary care hospital. J. Thromb. Haemost. 2016, 14, 982–986. [Google Scholar] [CrossRef]
- Meyer, M.R.; Witt, D.M.; Delate, T.; Johnson, S.G.; Fang, M.; Go, A.; Clark, N.P. Thrombophilia testing patterns amongst patients with acute venous thromboembolism. Thromb. Res. 2015, 136, 1160–1164. [Google Scholar] [CrossRef][Green Version]
- Virparia, R.; Brunetti, L.; Vigdor, S.; Adams, C.D. Appropriateness of thrombophilia testing in patients in the acute care setting and an evaluation of the associated costs. J. Thromb. Thrombolysis 2019, 49, 108–112. [Google Scholar] [CrossRef]
- Alakbarzade, V.; Taylor, A.; Scully, M.; Simister, R.; Chandratheva, A. Utility of current thrombophilia screening in young patients with stroke and TIA. Stroke Vasc. Neurol. 2018, 3, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Lopes, L.; Jacob, G.P. Thrombophilia testing in pregnancy: Should we agree to disagree? J. Perinat Med. 2015, 43, 269–272. [Google Scholar] [CrossRef] [PubMed]
- Hiedemann, B.; Vernon, E.; Bowie, B.H. Re-Examining Genetic Screening and Oral Contraceptives: A Patient-Centered Review. J. Pers. Med. 2019, 9, 4. [Google Scholar] [CrossRef] [PubMed]
- Turrini, M.; Bourgain, C. Appraising screening, making risk in/visible. The medical debate over Non-Rare Thrombophilia (NRT) testing before prescribing the pill. Sociol. Health Illn. 2021, 43, 1627–1642. [Google Scholar] [CrossRef]
- Cohn, D.M.; Middeldorp, S. Early termination of the multicentre randomised clinical trial to evaluate the benefit of testing for thrombophilia following a first venous thromboembolism: The NOSTRADAMUS study. Ned. Tijdschr. Geneeskd. 2008, 152, 2093–2094. [Google Scholar]
- Wilbur, J.; Shian, B. Diagnosis of deep venous thrombosis and pulmonary embolism. Am. Fam. Physician 2012, 86, 913–919. [Google Scholar]
- Hasan, T.F.; Rabinstein, A.A.; Middlebrooks, E.H.; Haranhalli, N.; Silliman, S.L.; Meschia, J.F.; Tawk, R.G. Diagnosis and Management of Acute Ischemic Stroke. Mayo Clin. Proc. 2018, 93, 523–538. [Google Scholar] [CrossRef]
- Anderson, J.L.; Morrow, D.A. Acute Myocardial Infarction. N. Engl. J. Med. 2017, 376, 2053–2064. [Google Scholar] [CrossRef]
- Firnhaber, J.M.; Powell, C.S. Lower Extremity Peripheral Artery Disease: Diagnosis and Treatment. Am. Fam. Physician 2019, 99, 362–369. [Google Scholar]
- Rajesh, S.; Mukund, A.; Arora, A. Imaging Diagnosis of Splanchnic Venous Thrombosis. Gastroenterol. Res. Pr. 2015, 2015, 1–29. [Google Scholar] [CrossRef]
- Karaosmanoglu, A.D.; Uysal, A.; Akata, D.; Ozmen, M.N.; Karcaaltincaba, M. Role of imaging in visceral vascular emergencies. Insights Imaging 2020, 11, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Ghoneim, A.; Straiton, J.; Pollard, C.; Macdonald, K.; Jampana, R. Imaging of cerebral venous thrombosis. Clin. Radiol. 2020, 75, 254–264. [Google Scholar] [CrossRef] [PubMed]
- Davenport, W.B.; Kutteh, W.H. Inherited thrombophilias and adverse pregnancy outcomes: A review of screening patterns and recommendations. Obstet. Gynecol. Clin. N. Am. 2014, 41, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.; Feinberg, B.; Burwick, R. Thrombotic microangiopathies of pregnancy: Differential diagnosis. Pregnancy Hypertens. 2018, 12, 29–34. [Google Scholar] [CrossRef]
- Miyakis, S.; Lockshin, M.D.; Atsumi, T.; Branch, D.W.; Brey, R.L.; Cervera, R.; Derksen, R.H.W.M.; De Groot, P.G.; Koike, T.; Meroni, P.L.; et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J. Thromb. Haemost. 2006, 4, 295–306. [Google Scholar] [CrossRef]
- Kearon, C.; Ageno, W.; Cannegieter, S.C.; Cosmi, B.; Geersing, G.-J.; Kyrle, P.A. Categorization of patients as having provoked or unprovoked venous thromboembolism: Guidance from the SSC of ISTH. J. Thromb. Haemost. 2016, 14, 1480–1483. [Google Scholar] [CrossRef]
- Lu, H.; Yang, Q.; Yang, L.; Qu, K.; Tian, B.; Xiao, Q.; Xin, X.; Lv, Y.; Zheng, X. The risk of venous thromboembolism associated with midline catheters compared with peripherally inserted central catheters: A systematic review and meta-analysis. Nurs. Open 2021, 9, 1873–1882. [Google Scholar] [CrossRef]
- Harbin, M.M.; Lutsey, P.L. May-Thurner syndrome: History of understanding and need for defining population prevalence. J. Thromb. Haemost. 2019, 18, 534–542. [Google Scholar] [CrossRef]
- Chandra, D.; Parisini, E.; Mozaffarian, D. Meta-analysis: Travel and risk for venous thromboembolism. Ann. Intern. Med. 2009, 151, 180–190. [Google Scholar] [CrossRef]
- Enga, K.F.; Braekkan, S.K.; Hansen-Krone, I.J.; le Cessie, S.; Rosendaal, F.R.; Hansen, J.-B. Cigarette smoking and the risk of venous thromboembolism: The Tromsø Study. J. Thromb. Haemost. 2012, 10, 2068–2074. [Google Scholar] [CrossRef]
- ACOG Practice Bulletin No. 197: Inherited Thrombophilias in Pregnancy: Correction. Obstet. Gynecol. 2018, 132, 1069.
- Kahn, S.R.; Lim, W.; Dunn, A.S.; Cushman, M.; Dentali, F.; Akl, E.A.; Cook, J.K.; Balekian, A.A.; Klein, C.R.; Le, H.; et al. Prevention of VTE in Nonsurgical Patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012, 141, e195S–e226S. [Google Scholar] [CrossRef]
- George, M.G. Risk Factors for Ischemic Stroke in Younger Adults: A Focused Update. Stroke 2020, 51, 729–735. [Google Scholar] [CrossRef] [PubMed]
- Crous-Bou, M.; Harrington, L.B.; Kabrhel, C. Environmental and Genetic Risk Factors Associated with Venous Thromboembolism. Semin. Thromb. Hemost. 2016, 42, 808–820. [Google Scholar] [CrossRef] [PubMed]
- Mehta, P.K.; Minissian, M.; Merz, C.N.B. Adverse pregnancy outcomes and cardiovascular risk factor management. Semin. Perinatol. 2015, 39, 268–275. [Google Scholar] [CrossRef]
- Gaddh, M.; Rosovsky, R.P. Venous Thromboembolism: Genetics and Thrombophilias. Semin Resp Crit Care Med. 2021, 42, 271–283. [Google Scholar] [CrossRef]
- Shen, Y.-M.; Tsai, J.; Taiwo, E.; Gavva, C.; Yates, S.G.; Patel, V.; Frenkel, E.; Sarode, R. Analysis of Thrombophilia Test Ordering Practices at an Academic Center: A Proposal for Appropriate Testing to Reduce Harm and Cost. PLoS ONE 2016, 11, e0155326. [Google Scholar] [CrossRef]
- Khan, S.; Dickerman, J.D. Hereditary thrombophilia. Thromb. J. 2006, 4, 15. [Google Scholar] [CrossRef][Green Version]
- Omran, S.S.; Lerario, M.P.; Gialdini, G.; Merkler, A.E.; Moya, A.; Chen, M.L.; Kamel, H.; DeSancho, M.; Navi, B.B. Clinical Impact of Thrombophilia Screening in Young Adults with Ischemic Stroke. J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2019, 28, 882–889. [Google Scholar] [CrossRef]
- May, J.E.; Martin, K.D.; Taylor, L.J.; Gangaraju, R.; Lin, C. Current Practice and Clinical Utility of Thrombophilia Testing in Hospitalized Patients with Acute Ischemic Stroke. J. Stroke Cerebrovasc. Dis. 2020, 29, 105209. [Google Scholar] [CrossRef]
- Vossen, C.Y.; Conard, J.; Fontcuberta, J.; Makris, M.; van der Meer, F.J.M.; Pabinger, I.; Palareti, G.; Preston, F.E.; Scharrer, I.; Souto, J.C.; et al. Risk of a first venous thrombotic event in carriers of a familial thrombophilic defect. The European Prospective Cohort on Thrombophilia (EPCOT). J. Thromb. Haemost. 2005, 3, 459–464. [Google Scholar] [CrossRef] [PubMed]
- Pabinger, I. Thrombophilia and its impact on pregnancy11Adapted from Pabinger I, Thrombophilia and its impact on pregnancy. Thromb. Res. 2009, 123, S16–S21. [Google Scholar] [CrossRef]
- Stefanski, A.-L.; Specker, C.; Fischer-Betz, R.; Henrich, W.; Schleussner, E.; Dörner, T. Maternal Thrombophilia and Recurrent Miscarriage—Is There Evidence That Heparin is Indicated as Prophylaxis against Recurrence? Geburtshilfe Frauenheilkd. 2018, 78, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Chen, Y.; Ye, C.; Xing, D.; Wu, R.; Li, F.; Chen, L.; Wang, T. Hereditary thrombophilia and recurrent pregnancy loss: A systematic review and meta-analysis. Hum. Reprod. 2021, 36, 1213–1229. [Google Scholar] [CrossRef] [PubMed]
- Ortel, T.L.; Meleth, S.; Catellier, D.; Crowther, M.; Erkan, D.; Fortin, P.R.; Garcia, D.; Haywood, N.; Kosinski, A.S.; Levine, S.R.; et al. Recurrent thrombosis in patients with antiphospholipid antibodies and an initial venous or arterial thromboembolic event: A systematic review and meta-analysis. J. Thromb. Haemost. 2020, 18, 2274–2286. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).