Aggregation Susceptibility of Low-Density Lipoproteins—A Novel Modifiable Biomarker of Cardiovascular Risk
Abstract
1. Introduction
2. LDL Particles—The Major Cholesterol Carriers in the Circulation
3. Potential Mechanisms of Aggregation of LDL Particles in the Arterial Intima
4. Uptake of Aggregated LDL Particles with Ensuing Foam Cell Formation and Inflammasome Activation
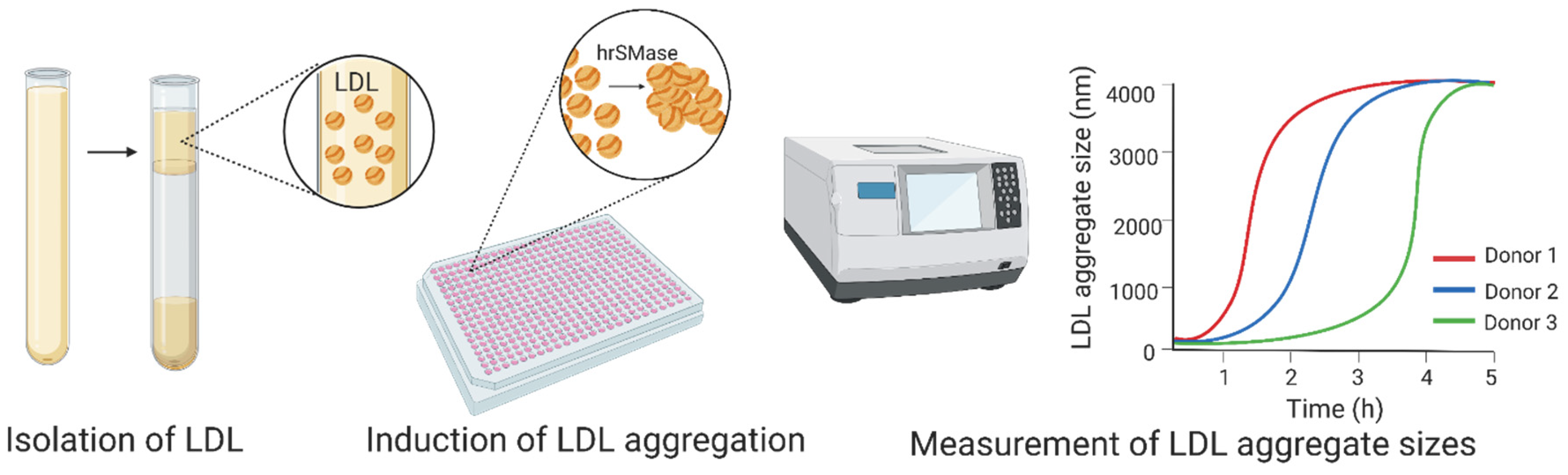
5. Measurement of Aggregation Susceptibility of LDL Particles
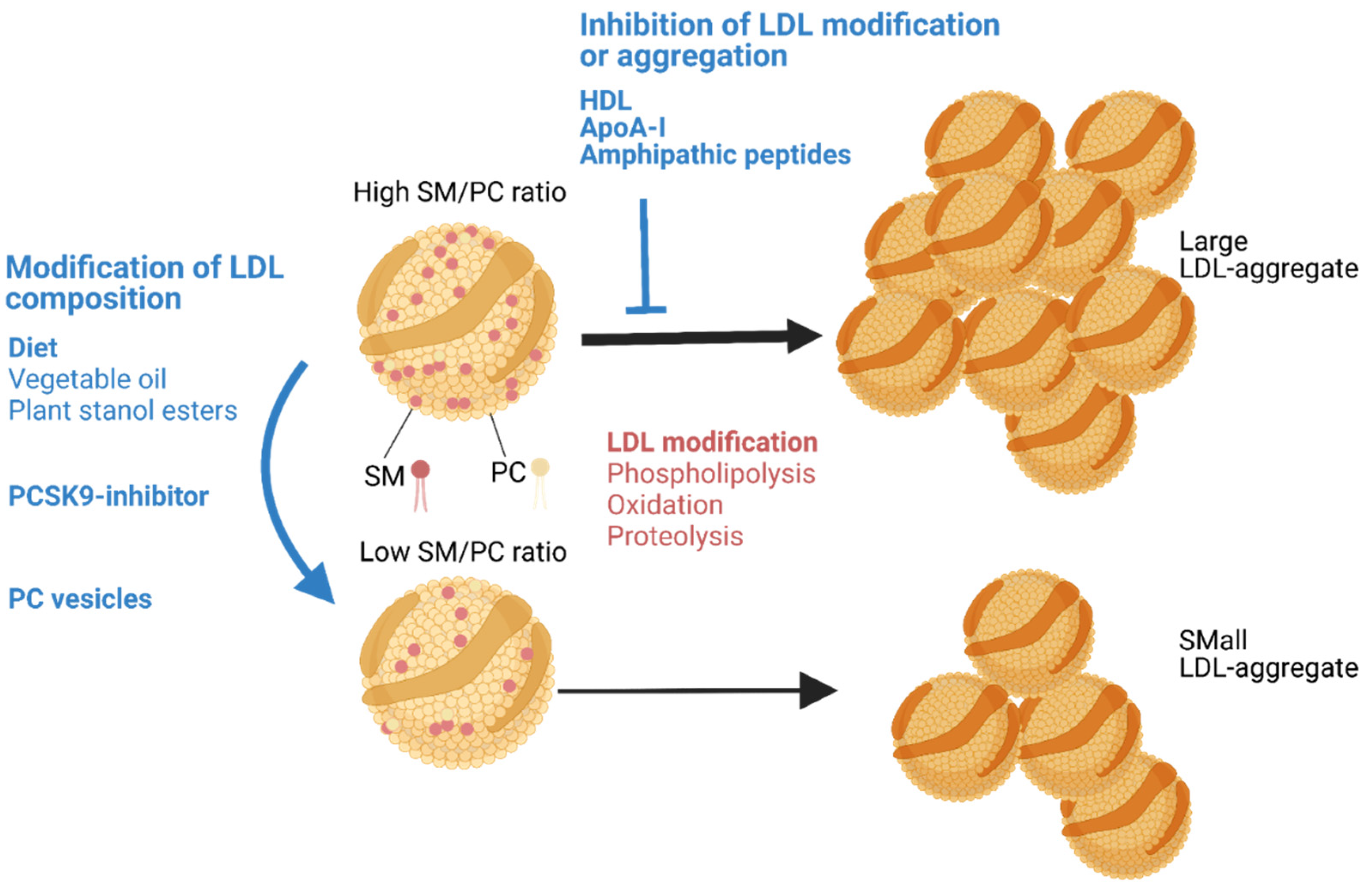
6. Increased Aggregation Susceptibility of LDL Particles in Human Atherosclerotic Cardiovascular Disease—Particle Lipid Composition as an Explanatory Factor
7. Attempts to Reduce the Aggregation Susceptibility of LDL Particles—From Molecular Understanding to Studies in Animal Models and Human Subjects
8. Conclusions and Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Borén, J.; Chapman, M.J.; Krauss, R.M.; Packard, C.J.; Bentzon, J.F.; Binder, C.J.; Daemen, M.J.; Demer, L.L.; Hegele, R.A.; Nicholls, S.J.; et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: Pathophysiological, genetic, and therapeutic insights: A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2020, 41, 2313–2330. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.B. Molecular interactions in human atherosclerotic plaques. Am. J. Pathol. 1977, 86, 665–674. [Google Scholar] [PubMed]
- Eliska, O.; Eliskova, M.; Miller, A.J. The absence of lymphatics in normal and atherosclerotic coronary arteries in man: A morphologic study. Lymphology 2006, 39, 76–83. [Google Scholar]
- Syväranta, S.; Helske, S.; Lappalainen, J.; Kupari, M.; Kovanen, P.T. Lymphangiogenesis in aortic valve stenosis—Novel regulatory roles for valvular myofibroblasts and mast cells. Atherosclerosis 2012, 221, 366–374. [Google Scholar] [CrossRef] [PubMed]
- Varricchi, G.; Marone, G.; Kovanen, P.T. Cardiac Mast Cells: Underappreciated Immune Cells in Cardiovascular Homeostasis and Disease. Trends Immunol. 2020, 41, 734–746. [Google Scholar] [CrossRef] [PubMed]
- Borén, J.; Williams, K.J. The central role of arterial retention of cholesterol-rich apolipoprotein-B-containing lipoproteins in the pathogenesis of atherosclerosis: A triumph of simplicity. Curr. Opin. Lipidol. 2016, 27, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.J.; Tabas, I. The Response-to-Retention Hypothesis of Early Atherogenesis. Arter. Thromb. Vasc. Biol. 1995, 15, 551–561. [Google Scholar] [CrossRef] [PubMed]
- Öörni, K.; Pentikäinen, M.O.; Ala-Korpela, M.; Kovanen, P.T. Aggregation, fusion, and vesicle formation of modified low density lipoprotein particles: Molecular mechanisms and effects on matrix interactions. J. Lipid Res. 2000, 41, 1703–1714. [Google Scholar] [CrossRef]
- Pentikäinen, M.O.; Öörni, K.; Kovanen, P.T. Lipoprotein Lipase (LPL) Strongly Links Native and Oxidized Low Density Lipoprotein Particles to Decorin-coated Collagen: Roles for both dimeric and monomeric forms of LPL. J. Biol. Chem. 2000, 275, 5694–5701. [Google Scholar] [CrossRef]
- Pasquinelli, G.; Preda, P.; Vici, M.; Gargiulo, M.; Stella, A.; D’Addato, M.; Laschi, R. Electron microscopy of lipid deposits in human atherosclerosis. Scanning Microsc. 1989, 3, 1151–1159. [Google Scholar]
- Guyton, J.R.; Klemp, K.F. Development of the atherosclerotic core region. Chemical and ultrastructural analysis of microdissected atherosclerotic lesions from human aorta. Arter. Thromb. J. Vasc. Biol. 1994, 14, 1305–1314. [Google Scholar] [CrossRef] [PubMed]
- Lehti, S.; Nguyen, S.D.; Belevich, I.; Vihinen, H.; Heikkilä, H.M.; Soliymani, R.; Käkelä, R.; Saksi, J.; Jauhiainen, M.; Grabowski, G.A.; et al. Extracellular Lipids Accumulate in Human Carotid Arteries as Distinct Three-Dimensional Structures and Have Proinflammatory Properties. Am. J. Pathol. 2018, 188, 525–538. [Google Scholar] [CrossRef]
- Packard, C.J.; Boren, J.; Taskinen, M.-R. Causes and Consequences of Hypertriglyceridemia. Front. Endocrinol. 2020, 11, 252. [Google Scholar] [CrossRef]
- Barter, P.J.; Brewer, H.B., Jr.; Chapman, M.J.; Hennekens, C.H.; Rader, D.J.; Tall, A.R. Cholesteryl Ester Transfer Protein. Arter. Thromb. Vasc. Biol. 2003, 23, 160–167. [Google Scholar] [CrossRef]
- Chapman, M.J.; Le Goff, W.; Guerin, M.; Kontush, A. Cholesteryl ester transfer protein: At the heart of the action of lipid-modulating therapy with statins, fibrates, niacin, and cholesteryl ester transfer protein inhibitors. Eur. Heart J. 2010, 31, 149–164. [Google Scholar] [CrossRef] [PubMed]
- Teng, B.; Thompson, G.R.; Sniderman, A.D.; Forte, T.M.; Krauss, R.M.; Kwiterovich, P.O. Composition and distribution of low density lipoprotein fractions in hyperapobetalipoproteinemia, normolipidemia, and familial hypercholesterolemia. Proc. Natl. Acad. Sci. USA 1983, 80, 6662–6666. [Google Scholar] [CrossRef] [PubMed]
- Kumpula, L.S.; Kumpula, J.M.; Taskinen, M.-R.; Jauhiainen, M.; Kaski, K.; Ala-Korpela, M. Reconsideration of hydrophobic lipid distributions in lipoprotein particles. Chem. Phys. Lipids 2008, 155, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Hevonoja, T.; Pentikäinen, M.O.; Hyvönen, M.T.; Kovanen, P.T.; Ala-Korpela, M. Structure of low density lipoprotein (LDL) particles: Basis for understanding molecular changes in modified LDL. Biochim. Biophys. 2000, 1488, 189–210. [Google Scholar] [CrossRef]
- Esterbauer, H.; Gebicki, J.; Puhl, H.; Jürgens, G. The role of lipid peroxidation and antioxidants in oxidative modification of LDL. Free Radic. Biol. Med. 1992, 13, 341–390. [Google Scholar] [CrossRef]
- Sommer, A.; Prenner, E.; Gorges, R.; Stütz, H.; Grillhofer, H.; Kostner, G.; Paltauf, F.; Hermetter, A. Organization of phosphatidylcholine and sphingomyelin in the surface monolayer of low density lipoprotein and lipoprotein(a) as determined by time-resolved fluorometry. J. Biol. Chem. 1992, 267, 24217–24222. [Google Scholar] [CrossRef]
- Schissel, S.L.; Tweedie-Hardman, J.; Rapp, J.H.; Graham, G.; Williams, K.J.; Tabas, I. Rabbit aorta and human atherosclerotic lesions hydrolyze the sphingomyelin of retained low-density lipoprotein. Proposed role for arterial-wall sphingomyelinase in subendothelial retention and aggregation of atherogenic lipoproteins. J. Clin. Investig. 1996, 98, 1455–1464. [Google Scholar] [CrossRef] [PubMed]
- Lund-Katz, S.; Phillips, M.C. Packing of cholesterol molecules in human low-density lipoprotein. Biochemistry 1986, 25, 1562–1568. [Google Scholar] [CrossRef] [PubMed]
- Khoo, J.C.; Miller, E.; McLoughlin, P.; Steinberg, D. Prevention of low density lipoprotein aggregation by high density lipoprotein or apolipoprotein A–I. J. Lipid Res. 1990, 31, 645–652. [Google Scholar] [CrossRef]
- Nievelstein, P.F.; Fogelman, A.M.; Mottino, G.; Frank, J.S. Lipid accumulation in rabbit aortic intima 2 hours after bolus infusion of low density lipoprotein. A deep-etch and immunolocalization study of ultrarapidly frozen tissue. Arter. Thromb. J. Vasc. Biol. 1991, 11, 1795–1805. [Google Scholar] [CrossRef]
- Steinbrecher, U.P.; Lougheed, M. Scavenger receptor-independent stimulation of cholesterol esterification in macrophages by low density lipoprotein extracted from human aortic intima. Arter. Thromb. J. Vasc. Biol. 1992, 12, 608–625. [Google Scholar] [CrossRef][Green Version]
- Hoff, H.F.; Morton, R.E. Lipoproteins Containing Apo B Extracted from Human Aortas Structure and Functiona. Ann. N. Y. Acad. Sci. 1985, 454, 183–194. [Google Scholar] [CrossRef]
- Tîrziu, D.; Dobrian, A.; Tasca, C.; Simionescu, M.; Simionescu, N. Intimal thickenings of human aorta contain modified reassembled lipoproteins. Atherosclerosis 1995, 112, 101–114. [Google Scholar] [CrossRef]
- Rapp, J.H.; Lespine, A.; Hamilton, R.L.; Colyvas, N.; Chaumeton, A.H.; Tweedie-Hardman, J.; Kotite, L.; Kunitake, S.T.; Havel, R.J.; Kane, J.P. Triglyceride-rich lipoproteins isolated by selected-affinity anti-apolipoprotein B immunosorption from human atherosclerotic plaque. Arter. Thromb. J. Vasc. Biol. 1994, 14, 1767–1774. [Google Scholar] [CrossRef]
- Chung, B.H.; Tallis, G.; Yalamoori, V.; Anantharamaiah, G.M.; Segrest, J.P. Liposome-like particles isolated from human atherosclerotic plaques are structurally and compositionally similar to surface remnants of triglyceride-rich lipoproteins. Arter. Thromb. J. Vasc. Biol. 1994, 14, 622–635. [Google Scholar] [CrossRef]
- Seifert, P.S.; Hugo, F.; Tranum-Jensen, J.; Zâhringer, U.; Muhly, M.; Bhakdi, S. Isolation and characterization of a complement-activating lipid extracted from human atherosclerotic lesions. J. Exp. Med. 1990, 172, 547–557. [Google Scholar] [CrossRef]
- Chao, F.F.; Amende, L.M.; Blanchette-Mackie, E.J.; Skarlatos, S.I.; Gamble, W.; Resau, J.H.; Mergner, W.T.; Kruth, H.S. Unesterified cholesterol-rich lipid particles in atherosclerotic lesions of human and rabbit aortas. Am. J. Pathol. 1988, 131, 73–83. [Google Scholar] [PubMed]
- Ylä-Herttuala, S.; Palinski, W.; Rosenfeld, M.E.; Parthasarathy, S.; Carew, T.E.; Butler, S.; Witztum, J.L.; Steinberg, D. Evidence for the presence of oxidatively modified low density lipoprotein in atherosclerotic lesions of rabbit and man. J. Clin. Investig. 1989, 84, 1086–1095. [Google Scholar] [CrossRef]
- Tailleux, A.; Torpier, G.; Caron, B.; Fruchart, J.; Fievet, C. Immunological properties of apoB-containing lipoprotein particles in human atherosclerotic arteries. J. Lipid Res. 1993, 34, 719–728. [Google Scholar] [CrossRef]
- Miller, Y.I.; Choi, S.-H.; Wiesner, P.; Fang, L.; Harkewicz, R.; Hartvigsen, K.; Boullier, A.; Gonen, A.; Diehl, C.J.; Que, X.; et al. Oxidation-Specific Epitopes Are Danger-Associated Molecular Patterns Recognized by Pattern Recognition Receptors of Innate Immunity. Circ. Res. 2011, 108, 235–248. [Google Scholar] [CrossRef]
- Jayaraman, S.; Gantz, D.L.; Gursky, O. Effects of phospholipase A2 and its products on structural stability of human LDL: Relevance to formation of LDL-derived lipid droplets. J. Lipid Res. 2011, 52, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Sneck, M.; Nguyen, S.D.; Pihlajamaa, T.; Yohannes, G.; Riekkola, M.-L.; Milne, R.; Kovanen, P.T.; Öörni, K. Conformational changes of apoB-100 in SMase-modified LDL mediate formation of large aggregates at acidic pH. J. Lipid Res. 2012, 53, 1832–1839. [Google Scholar] [CrossRef] [PubMed]
- Ruuth, M.; Nguyen, S.D.; Vihervaara, T.; Hilvo, M.; Laajala, T.D.; Kondadi, P.K.; Gisterå, A.; Lähteenmäki, H.; Kittilä, T.; Huusko, J.; et al. Susceptibility of low-density lipoprotein particles to aggregate depends on particle lipidome, is modifiable, and associates with future cardiovascular deaths. Eur. Heart J. 2018, 39, 2562–2573. [Google Scholar] [CrossRef]
- Bancells, C.; Beniítez, S.; Villegas, S.; Jorba, O.; Ordóñez-Llanos, J.; Sánchez-Quesada, J.L. Novel Phospholipolytic Activities Associated with Electronegative Low-Density Lipoprotein Are Involved in Increased Self-Aggregation. Biochemistry 2008, 47, 8186–8194. [Google Scholar] [CrossRef] [PubMed]
- Bancells, C.; Villegas, S.; Blanco, F.J.; Benítez, S.; Gállego, I.; Beloki, L.; Pérez-Cuellar, M.; Ordóñez-Llanos, J.; Sánchez-Quesada, J.L. Aggregated Electronegative Low Density Lipoprotein in Human Plasma Shows a High Tendency toward Phospholipolysis and Particle Fusion. J. Biol. Chem. 2010, 285, 32425–32435. [Google Scholar] [CrossRef] [PubMed]
- Bancells, C.; Benítez, S.; Jauhiainen, M.; Ordóñez-Llanos, J.; Kovanen, P.T.; Villegas, S.; Sánchez-Quesada, J.L.; Katariina, O. High binding affinity of electronegative LDL to human aortic proteoglycans depends on its aggregation level. J. Lipid Res. 2009, 50, 446–455. [Google Scholar] [CrossRef] [PubMed]
- Galis, Z.S.; Sukhova, G.K.; Lark, M.W.; Libby, P. Increased expression of matrix metalloproteinases and matrix degrading activity in vulnerable regions of human atherosclerotic plaques. J. Clin. Investig. 1994, 94, 2493–2503. [Google Scholar] [CrossRef]
- Maaninka, K.; Nguyen, S.D.; Mäyränpää, M.I.; Plihtari, R.; Rajamäki, K.; Lindsberg, P.J.; Kovanen, P.T.; Öörni, K. Human mast cell neutral proteases generate modified LDL particles with increased proteoglycan binding. Atherosclerosis 2018, 275, 390–399. [Google Scholar] [CrossRef] [PubMed]
- Öörni, K.; Sneck, M.; Brömme, D.; Pentikäinen, M.O.; Lindstedt, K.A.; Mayranpaa, M.; Aitio, H.; Kovanen, P.T. Cysteine Protease Cathepsin F Is Expressed in Human Atherosclerotic Lesions, Is Secreted by Cultured Macrophages, and Modifies Low Density Lipoprotein Particles in Vitro. J. Biol. Chem. 2004, 279, 34776–34784. [Google Scholar] [CrossRef] [PubMed]
- Sukhova, G.K.; Zhang, Y.; Pan, J.-H.; Wada, Y.; Yamamoto, T.; Naito, M.; Kodama, T.; Tsimikas, S.; Witztum, J.L.; Lu, M.L.; et al. Deficiency of cathepsin S reduces atherosclerosis in LDL receptor–deficient mice. J. Clin. Investig. 2003, 111, 897–906. [Google Scholar] [CrossRef] [PubMed]
- Hakala, J.K.; Oksjoki, R.; Laine, P.; Du, H.; Grabowski, G.A.; Kovanen, P.T.; Pentikäinen, M.O. Lysosomal Enzymes Are Released From Cultured Human Macrophages, Hydrolyze LDL In Vitro, and Are Present Extracellularly in Human Atherosclerotic Lesions. Arter. Thromb. Vasc. Biol. 2003, 23, 1430–1436. [Google Scholar] [CrossRef]
- Piha, M.; Lindstedt, L.; Kovanen, P.T. Fusion of Proteolyzed Low-Density Lipoproteins in the Fluid Phase: A Novel Mechanism Generating Atherogenic Lipoprotein Particles. Biochemistry 1995, 34, 10120–10129. [Google Scholar] [CrossRef] [PubMed]
- Torzewski, M.; Suriyaphol, P.; Paprotka, K.; Spath, L.; Ochsenhirt, V.; Schmitt, A.; Han, S.-R.; Husmann, M.; Gerl, V.B.; Bhakdi, S.; et al. Enzymatic Modification of Low-Density Lipoprotein in the Arterial Wall. Arter. Thromb. Vasc. Biol. 2004, 24, 2130–2136. [Google Scholar] [CrossRef]
- Plihtari, R.; Hurt-Camejo, E.; Öörni, K.; Kovanen, P.T. Proteolysis sensitizes LDL particles to phospholipolysis by secretory phospholipase A2 group V and secretory sphingomyelinase. J. Lipid Res. 2010, 51, 1801–1809. [Google Scholar] [CrossRef]
- Torzewski, M.; Klouche, M.; Hock, J.; Meßner, M.; Dorweiler, B.; Torzewski, J.; Gabbert, H.E.; Bhakdi, S. Immunohistochemical Demonstration of Enzymatically Modified Human LDL and Its Colocalization With the Terminal Complement Complex in the Early Atherosclerotic Lesion. Arter. Thromb. Vasc. Biol. 1998, 18, 369–378. [Google Scholar] [CrossRef]
- Bhakdi, S.; Dorweiler, B.; Kirchmann, R.; Torzewski, J.; Weise, E.; Tranum-Jensen, J.; Walev, I.; Wieland, E. On the pathogenesis of atherosclerosis: Enzymatic transformation of human low density lipoprotein to an atherogenic moiety. J. Exp. Med. 1995, 182, 1959–1971. [Google Scholar] [CrossRef]
- Taskinen, S.; Hyvönen, M.; Kovanen, P.T.; Meri, S.; Pentikäinen, M.O. C-reactive protein binds to the 3β-OH group of cholesterol in LDL particles. Biochem. Biophys. Res. Commun. 2005, 329, 1208–1216. [Google Scholar] [CrossRef]
- Bhakdi, S.; Torzewski, M.; Paprotka, K.; Schmitt, S.; Barsoom, H.; Suriyaphol, P.; Han, S.-R.; Lackner, K.J.; Husmann, M. Possible Protective Role for C-Reactive Protein in Atherogenesis. Circulation 2004, 109, 1870–1876. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bhakdi, S.; Torzewski, M.; Klouche, M.; Hemmes, M. Complement and Atherogenesis. Arter. Thromb. Vasc. Biol. 1999, 19, 2348–2354. [Google Scholar] [CrossRef]
- Jayaraman, S.; Chavez, O.R.; Pérez, A.; Miñambres, I.; Sánchez-Quesada, J.L.; Gursky, O. Binding to heparin triggers deleterious structural and biochemical changes in human low-density lipoprotein, which are amplified in hyperglycemia. Biochim. Biophys. Acta 2020, 1865, 158712. [Google Scholar] [CrossRef]
- Hakala, J.K.; Öörni, K.; Ala-Korpela, M.; Kovanen, P.T. Lipolytic Modification of LDL by Phospholipase A 2 Induces Particle Aggregation in the Absence and Fusion in the Presence of Heparin. Arter. Thromb. Vasc. Biol. 1999, 19, 1276–1283. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hurt-Camejo, E.; Camejo, G.; Rosengren, B.; López, F.; Ahlström, C.; Fager, G.; Bondjers, G. Effect of arterial proteoglycans and glycosaminoglycans on low density lipoprotein oxidation and its uptake by human macrophages and arterial smooth muscle cells. Arter. Thromb. J. Vasc. Biol. 1992, 12, 569–583. [Google Scholar] [CrossRef] [PubMed]
- Naghavi, M.; John, R.; Naguib, S.; Siadaty, M.S.; Grasu, R.; Kurian, K.; Van Winkle, W.; Soller, B.; Litovsky, S.; Madjid, M.; et al. pH Heterogeneity of human and rabbit atherosclerotic plaques; a new insight into detection of vulnerable plaque. Atherosclerosis 2002, 164, 27–35. [Google Scholar] [CrossRef]
- Öörni, K.; Kovanen, P.T. Enhanced extracellular lipid accumulation in acidic environments. Curr. Opin. Lipidol. 2006, 17, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Öörni, K.; Rajamäki, K.; Nguyen, S.D.; Lähdesmäki, K.; Plihtari, R.; Lee-Rueckert, M.; Kovanen, P.T. Acidification of the intimal fluid: The perfect storm for atherogenesis. J. Lipid Res. 2015, 56, 203–214. [Google Scholar] [CrossRef] [PubMed]
- Leake, D.S. Does an acidic pH explain why low density lipoprotein is oxidised in atherosclerotic lesions? Atherosclerosis 1997, 129, 149–157. [Google Scholar] [CrossRef]
- Schissel, S.L.; Jiang, X.-C.; Tweedie-Hardman, J.; Jeong, T.-S.; Camejo, E.H.; Najib, J.; Rapp, J.H.; Williams, K.J.; Tabas, I. Secretory Sphingomyelinase, a Product of the Acid Sphingomyelinase Gene, Can Hydrolyze Atherogenic Lipoproteins at Neutral pH: Implications for atherosclerotic lesion development. J. Biol. Chem. 1998, 273, 2738–2746. [Google Scholar] [CrossRef] [PubMed]
- Lopes-Virella, M.F.; Virella, G.; Orchard, T.J.; Koskinen, S.; Evans, R.W.; Becker, D.J.; Forrest, K.Y.-Z. Antibodies to Oxidized LDL and LDL-Containing Immune Complexes as Risk Factors for Coronary Artery Disease in Diabetes Mellitus. Clin. Immunol. 1999, 90, 165–172. [Google Scholar] [CrossRef]
- Lopes-Virella, M.F.; Hunt, K.J.; Baker, N.L.; Virella, G.; Moritz, T. The levels of MDA-LDL in circulating immune complexes predict myocardial infarction in the VADT study. Atherosclerosis 2012, 224, 526–531. [Google Scholar] [CrossRef] [PubMed]
- Lopes-Virella, M.F.; Hunt, K.J.; Baker, N.L.; Lachin, J.; Nathan, D.M.; Virella, G.; The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Levels of Oxidized LDL and Advanced Glycation End Products-Modified LDL in Circulating Immune Complexes Are Strongly Associated With Increased Levels of Carotid Intima-Media Thickness and Its Progression in Type 1 Diabetes. Diabetes 2010, 60, 582–589. [Google Scholar] [CrossRef] [PubMed]
- Lopes-Virella, M.F.; McHenry, M.B.; Lipsitz, S.; Yim, E.; Wilson, P.F.; Lackland, D.T.; Lyons, T.; Jenkins, A.J.; Virella, G. Immune complexes containing modified lipoproteins are related to the progression of internal carotid intima-media thickness in patients with type 1 diabetes. Atherosclerosis 2007, 190, 359–369. [Google Scholar] [CrossRef]
- Ylä-Herttuala, S.; Palinski, W.; Butler, S.W.; Picard, S.; Steinberg, D.; Witztum, J.L. Rabbit and human atherosclerotic lesions contain IgG that recognizes epitopes of oxidized LDL. Arter. Thromb. J. Vasc. Biol. 1994, 14, 32–40. [Google Scholar] [CrossRef]
- Witztum, J.L. You are right too! J. Clin. Investig. 2005, 115, 2072–2075. [Google Scholar] [CrossRef]
- Schulz, B.; Liebisch, G.; Grandl, M.; Werner, T.; Barlage, S.; Schmitz, G. β-Amyloid (Aβ40, Aβ42) binding to modified LDL accelerates macrophage foam cell formation. Biochim. Biophys. Acta 2007, 1771, 1335–1344. [Google Scholar] [CrossRef]
- Grosheva, I.; Haka, A.S.; Qin, C.; Pierini, L.M.; Maxfield, F.R. Aggregated LDL in Contact With Macrophages Induces Local Increases in Free Cholesterol Levels That Regulate Local Actin Polymerization. Arter. Thromb. Vasc. Biol. 2009, 29, 1615–1621. [Google Scholar] [CrossRef]
- Haka, A.S.; Grosheva, I.; Chiang, E.; Buxbaum, A.R.; Baird, B.A.; Pierini, L.M.; Maxfield, F.R. Macrophages Create an Acidic Extracellular Hydrolytic Compartment to Digest Aggregated Lipoproteins. Mol. Biol. Cell 2009, 20, 4932–4940. [Google Scholar] [CrossRef]
- Singh, R.K.; Haka, A.S.; Bhardwaj, P.; Zha, X.; Maxfield, F.R. Dynamic Actin Reorganization and Vav/Cdc42-Dependent Actin Polymerization Promote Macrophage Aggregated LDL (Low-Density Lipoprotein) Uptake and Catabolism. Arter. Thromb. Vasc. Biol. 2019, 39, 137–149. [Google Scholar] [CrossRef]
- Singh, R.K.; Haka, A.S.; Asmal, A.; Barbosa-Lorenzi, V.C.; Grosheva, I.; Chin, H.F.; Xiong, Y.; Hla, T.; Maxfield, F.R. TLR4 (Toll-Like Receptor 4)-Dependent Signaling Drives Extracellular Catabolism of LDL (Low-Density Lipoprotein) Aggregates. Arter. Thromb. Vasc. Biol. 2020, 40, 86–102. [Google Scholar] [CrossRef]
- Brown, M.S.; Goldstein, J.L. Lipoprotein Metabolism in the Macrophage: Implications for Cholesterol Deposition in Atherosclerosis. Annu. Rev. Biochem. 1983, 52, 223–261. [Google Scholar] [CrossRef]
- Sheedy, F.J.; Grebe, A.; Rayner, K.J.; Kalantari, P.; Ramkhelawon, B.; Carpenter, S.B.; Becker, C.E.; Ediriweera, H.N.; Mullick, A.E.; Golenbock, D.T.; et al. CD36 coordinates NLRP3 inflammasome activation by facilitating intracellular nucleation of soluble ligands into particulate ligands in sterile inflammation. Nat. Immunol. 2013, 14, 812–820. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, F.; Leake, D.S. Lysosomal oxidation of LDL alters lysosomal pH, induces senescence, and increases secretion of pro-inflammatory cytokines in human macrophages. J. Lipid Res. 2019, 60, 98–110. [Google Scholar] [CrossRef] [PubMed]
- Wen, Y.; Ahmad, F.; Mohri, Z.; Weinberg, P.D.; Leake, D.S. Cysteamine inhibits lysosomal oxidation of low density lipoprotein in human macrophages and reduces atherosclerosis in mice. Atherosclerosis 2019, 291, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Bäck, M.; Yurdagul, A., Jr.; Tabas, I.; Öörni, K.; Kovanen, P.T. Inflammation and its resolution in atherosclerosis: Mediators and therapeutic opportunities. Nat. Rev. Cardiol. 2019, 16, 389–406. [Google Scholar] [CrossRef]
- He, Y.; Hara, H.; Núñez, G. Mechanism and Regulation of NLRP3 Inflammasome Activation. Trends Biochem. Sci. 2016, 41, 1012–1021. [Google Scholar] [CrossRef]
- Patel, M.N.; Carroll, R.G.; Galván-Peña, S.; Mills, E.L.; Olden, R.; Triantafilou, M.; Wolf, A.I.; Bryant, C.E.; Triantafilou, K.; Masters, S.L. Inflammasome Priming in Sterile Inflammatory Disease. Trends Mol. Med. 2017, 23, 165–180. [Google Scholar] [CrossRef]
- Rajamäki, K.; Mäyränpää, M.I.; Risco, A.; Tuimala, J.; Nurmi, K.; Cuenda, A.; Eklund, K.K.; Öörni, K.; Kovanen, P.T. p38δ MAPK. Arter. Thromb. Vasc. Biol. 2016, 36, 1937–1946. [Google Scholar] [CrossRef]
- Pryma, C.S.; Ortega, C.; Dubland, J.A.; Francis, G.A. Pathways of smooth muscle foam cell formation in atherosclerosis. Curr. Opin. Lipidol. 2019, 30, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Llorente-Cortés, V.; Martínez-González, J.; Badimon, L. LDL Receptor–Related Protein Mediates Uptake of Aggregated LDL in Human Vascular Smooth Muscle Cells. Arter. Thromb. Vasc. Biol. 2000, 20, 1572–1579. [Google Scholar] [CrossRef] [PubMed]
- Llorente-Cortés, V.; Otero-Viñas, M.; Sánchez, S.; Rodríguez, C.; Badimon, L. Low-Density Lipoprotein Upregulates Low-Density Lipoprotein Receptor-Related Protein Expression in Vascular Smooth Muscle Cells. Circulation 2002, 106, 3104–3110. [Google Scholar] [CrossRef] [PubMed]
- De Gonzalo-Calvo, D.; Cenarro, A.; Martínez-Bujidos, M.; Badimon, L.; Bayes-Genis, A.; Ordonez-Llanos, J.; Civeira, F.; Llorente-Cortés, V. Circulating soluble low-density lipoprotein receptor-related protein 1 (sLRP1) concentration is associated with hypercholesterolemia: A new potential biomarker for atherosclerosis. Int. J. Cardiol. 2015, 201, 20–29. [Google Scholar] [CrossRef]
- De Gonzalo-Calvo, D.; Elosua, R.; Vea, A.; Subirana, I.; Sayols-Baixeras, S.; Marrugat, J.; Llorente-Cortés, V. Soluble low-density lipoprotein receptor-related protein 1 as a biomarker of coronary risk: Predictive capacity and association with clinical events. Atherosclerosis 2019, 287, 93–99. [Google Scholar] [CrossRef]
- Ruuth, M.; Janssen, L.G.M.; Äikäs, L.; Tigistu-Sahle, F.; Nahon, K.J.; Ritvos, O.; Ruhanen, H.; Käkelä, R.; Boon, M.R.; Öörni, K.; et al. LDL aggregation susceptibility is higher in healthy South Asian compared with white Caucasian men. J. Clin. Lipidol. 2019, 13, 910–919.e2. [Google Scholar] [CrossRef]
- Heffron, S.P.; Ruuth, M.K.; Xia, Y.; Hernandez, G.; Äikäs, L.; Rodriguez, C.; Öörni, K.; Berger, J.S. Low-density lipoprotein aggregation predicts adverse cardiovascular events in peripheral artery disease. Atherosclerosis 2021, 316, 53–57. [Google Scholar] [CrossRef]
- Christensen, J.J.; Narverud, I.; Ruuth, M.; Heier, M.; Jauhiainen, M.; Ulven, S.M.; Bogsrud, M.P.; Kovanen, P.T.; Halvorsen, B.; Oda, M.N.; et al. Children with familial hypercholesterolemia display changes in LDL and HDL function: A cross-sectional study. medRxiv 2020. [Google Scholar] [CrossRef]
- Uchida, Y.; Uchida, Y.; Kobayashi, T.; Shirai, S.; Hiruta, N.; Shimoyama, E.; Tabata, T. Detection of Ceramide, a Risk Factor for Coronary Artery Disease, in Human Coronary Plaques by Fluorescent Angioscopy. Circ. J. 2017, 81, 1886–1893. [Google Scholar] [CrossRef]
- Abbas, A.; Aukrust, P.; Russell, D.; Krohg-Sørensen, K.; Almås, T.; Bundgaard, D.; Bjerkeli, V.; Sagen, E.L.; Michelsen, A.E.; Dahl, T.B.; et al. Matrix Metalloproteinase 7 Is Associated with Symptomatic Lesions and Adverse Events in Patients with Carotid Atherosclerosis. PLoS ONE 2014, 9, e84935. [Google Scholar] [CrossRef]
- Laaksonen, R.; Ekroos, K.; Sysi-Aho, M.; Hilvo, M.; Vihervaara, T.; Kauhanen, D.; Suoniemi, M.; Hurme, R.; März, W.; Scharnagl, H.; et al. Plasma ceramides predict cardiovascular death in patients with stable coronary artery disease and acute coronary syndromes beyond LDL-cholesterol. Eur. Heart J. 2016, 37, 1967–1976. [Google Scholar] [CrossRef]
- Peterson, L.R.; Xanthakis, V.; Duncan, M.S.; Gross, S.; Friedrich, N.; Völzke, H.; Felix, S.B.; Jiang, H.; Sidhu, R.; Nauck, M.; et al. Ceramide Remodeling and Risk of Cardiovascular Events and Mortality. J. Am. Heart Assoc. 2018, 7, e007931. [Google Scholar] [CrossRef]
- Havulinna, A.S.; Sysi-Aho, M.; Hilvo, M.; Kauhanen, D.; Hurme, R.; Ekroos, K.; Salomaa, V.; Laaksonen, R. Circulating Ceramides Predict Cardiovascular Outcomes in the Population-Based FINRISK 2002 Cohort. Arter. Thromb. Vasc. Biol. 2016, 36, 2424–2430. [Google Scholar] [CrossRef]
- De Carvalho, L.P.; Tan, S.H.; Ow, G.-S.; Tang, Z.; Ching, J.; Kovalik, J.-P.; Poh, S.C.; Chin, C.-T.; Richards, A.M.; Martinez, E.C.; et al. Plasma Ceramides as Prognostic Biomarkers and Their Arterial and Myocardial Tissue Correlates in Acute Myocardial Infarction. JACC Basic Transl. Sci. 2018, 3, 163–175. [Google Scholar] [CrossRef]
- Li, Q.; Wang, X.; Pang, J.; Zhang, Y.; Zhang, H.; Xu, Z.; Chen, Q.; Ling, W. Associations between plasma ceramides and mortality in patients with coronary artery disease. Atherosclerosis 2020, 314, 77–83. [Google Scholar] [CrossRef]
- Öörni, K.; Jauhiainen, M.; Kovanen, P.T. Why and how increased plasma ceramides predict future cardiovascular events? Atherosclerosis 2020, 314, 71–73. [Google Scholar] [CrossRef] [PubMed]
- Hilvo, M.; Wallentin, L.; Lakic, T.G.; Held, C.; Kauhanen, D.; Jylhä, A.; Lindbäck, J.; Siegbahn, A.; Granger, C.B.; Koenig, W.; et al. Prediction of Residual Risk by Ceramide-Phospholipid Score in Patients With Stable Coronary Heart Disease on Optimal Medical Therapy. J. Am. Heart Assoc. 2020, 9, e015258. [Google Scholar] [CrossRef] [PubMed]
- Gencer, B.; Morrow, D.A.; Braunwald, E.; Goodrich, E.L.; Hilvo, M.; Kauhanen, D.; Sabatine, M.S.; Laaksonen, R.; O’Donoghue, M.L. Plasma ceramide and phospholipid-based risk score and the risk of cardiovascular death in patients after acute coronary syndrome. Eur. J. Prev. Cardiol. 2020. [Google Scholar] [CrossRef]
- Vuorio, A.; Watts, G.F.; Kovanen, P.T. Initiation of PCSK9 inhibition in patients with heterozygous familial hypercholesterolaemia entering adulthood: A new design for living with a high-risk condition? Eur. Heart J. 2016, 37, 1353–1356. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brown, M.S.; Goldstein, J.L. Biomedicine. Lowering LDL—Not only how low, but how long? Science 2006, 311, 1721–1723. [Google Scholar] [CrossRef] [PubMed]
- Vuorio, A.; Docherty, K.F.; Humphries, S.E.; Kuoppala, J.; Kovanen, P.T. Statin treatment of children with familial hypercholesterolemia—Trying to balance incomplete evidence of long-term safety and clinical accountability: Are we approaching a consensus? Atherosclerosis 2013, 226, 315–320. [Google Scholar] [CrossRef]
- Ruuth, M.; Äikäs, L.; Tigistu-Sahle, F.; Käkelä, R.; Lindholm, H.; Simonen, P.; Kovanen, P.T.; Gylling, H.; Öörni, K. Plant Stanol Esters Reduce LDL (Low-Density Lipoprotein) Aggregation by Altering LDL Surface Lipids: The BLOOD FLOW Randomized Intervention Study. Arter. Thromb. Vasc. Biol. 2020, 40, 2310–2321. [Google Scholar] [CrossRef]
- Hilvo, M.; Simolin, H.; Metso, J.; Ruuth, M.; Öörni, K.; Jauhiainen, M.; Laaksonen, R.; Baruch, A. PCSK9 inhibition alters the lipidome of plasma and lipoprotein fractions. Atherosclerosis 2018, 269, 159–165. [Google Scholar] [CrossRef]
- Liu, H.; Scraba, D.G.; Ryan, R.O. Prevention of phospholipase-C induced aggregation of low density lipoprotein by amphipathic apolipoproteins. FEBS Lett. 1993, 316, 27–33. [Google Scholar] [CrossRef]
- Nguyen, S.D.; Javanainen, M.; Rissanen, S.; Zhao, H.; Huusko, J.; Kivelä, A.M.; Ylä-Herttuala, S.; Navab, M.; Fogelman, A.M.; Vattulainen, I.; et al. Apolipoprotein A-I mimetic peptide 4F blocks sphingomyelinase-induced LDL aggregation. J. Lipid Res. 2015, 56, 1206–1221. [Google Scholar] [CrossRef]
- Navab, M.; Anantharamaiah, G.M.; Reddy, S.T.; Hama, S.; Hough, G.; Grijalva, V.R.; Yu, N.; Ansell, B.J.; Datta, G.; Garber, D.W.; et al. Apolipoprotein A–I Mimetic Peptides. Arter. Thromb. Vasc. Biol. 2005, 25, 1325–1331. [Google Scholar] [CrossRef] [PubMed]
- Navab, M.; Anantharamaiah, G.M.; Reddy, S.T.; Fogelman, A.M. Apolipoprotein A–I mimetic peptides and their role in atherosclerosis prevention. Nat. Clin. Pr. Neurol. 2006, 3, 540–547. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Chyu, K.-Y.; Neto, J.R.F.; Yano, J.; Nathwani, N.; Ferreira, C.; Dimayuga, P.C.; Cercek, B.; Kaul, S.; Shah, P.K. Differential Effects of Apolipoprotein A-I–Mimetic Peptide on Evolving and Established Atherosclerosis in Apolipoprotein E-Null Mice. Circulation 2004, 110, 1701–1705. [Google Scholar] [CrossRef] [PubMed]
- Rivas-Urbina, A.; Rull, A.; Montoliu-Gaya, L.; Pérez-Cuellar, M.; Ordóñez-Llanos, J.; Villegas, S.; Sánchez-Quesada, J.L. Low-density lipoprotein aggregation is inhibited by apolipoprotein J-derived mimetic peptide D-[113–122]apoJ. Biochim. Biophys. Acta 2020, 1865, 158541. [Google Scholar] [CrossRef] [PubMed]
- Rivas-Urbina, A.; Rull, A.; Aldana-Ramos, J.; Santos, D.; Puig, N.; Farre-Cabrerizo, N.; Benitez, S.; Perez, A.; De Gonzalo-Calvo, D.; Escola-Gil, J.C.; et al. Subcutaneous Administration of Apolipoprotein J-Derived Mimetic Peptide d-[113–122]apoJ Improves LDL and HDL Function and Prevents Atherosclerosis in LDLR-KO Mice. Biomolecules 2020, 10, 829. [Google Scholar] [CrossRef]
- Sherman, C.B.; Peterson, S.J.; Frishman, W.H. Apolipoprotein A-I Mimetic Peptides. Cardiol. Rev. 2010, 18, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Dunbar, R.L.; Movva, R.; Bloedon, L.T.; Duffy, D.; Norris, R.B.; Navab, M.; Fogelman, A.M.; Rader, D.J. Oral Apolipoprotein A-I Mimetic D-4F Lowers HDL-Inflammatory Index in High-Risk Patients: A First-in-Human Multiple-Dose, Randomized Controlled Trial. Clin. Transl. Sci. 2017, 10, 455–469. [Google Scholar] [CrossRef] [PubMed]
- Kingwell, B.A.; Chapman, M.J.; Kontush, A.; Miller, N.E. HDL-targeted therapies: Progress, failures and future. Nat. Rev. Drug Discov. 2014, 13, 445–464. [Google Scholar] [CrossRef] [PubMed]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef] [PubMed]
- Kjellmo, C.A.; Hovland, A.; Lappegård, K.T. CVD Risk Stratification in the PCSK9 Era: Is There a Role for LDL Subfractions? Diseases 2018, 6, 45. [Google Scholar] [CrossRef] [PubMed]
- Kjellmo, C.A.; Pop, G.; Lappegård, K.T.; Hovland, A. Intensive lipid lowering therapy reduces large, but not small, dense low-density lipoprotein particles measured by gel electrophoresis, in elderly patients with atrial fibrillation. Eur. J. Prev. Cardiol. 2019, 26, 2017–2018. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.-J.; Tseng, W.-K.; Yin, W.-H.; Yeh, H.-I.; Chen, J.-W.; Wu, C.-C. Residual Risk Factors to Predict Major Adverse Cardiovascular Events in Atherosclerotic Cardiovascular Disease Patients with and without Diabetes Mellitus. Sci. Rep. 2017, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
| Lipoprotein | Size | Characteristics | Reference |
|---|---|---|---|
| Extracellular lipoproteins | 20 to >200 nm | LDL-like particles and lipid droplets | [26,28,29,30] |
| Uni- and multilamellar vesicles | 70 to 300 nm | Enriched in unesterified cholesterol | [30,31] |
| Aggregates | 100 to 2000 nm | Connected to cholesterol crystals | [12,21] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Öörni, K.; Kovanen, P.T. Aggregation Susceptibility of Low-Density Lipoproteins—A Novel Modifiable Biomarker of Cardiovascular Risk. J. Clin. Med. 2021, 10, 1769. https://doi.org/10.3390/jcm10081769
Öörni K, Kovanen PT. Aggregation Susceptibility of Low-Density Lipoproteins—A Novel Modifiable Biomarker of Cardiovascular Risk. Journal of Clinical Medicine. 2021; 10(8):1769. https://doi.org/10.3390/jcm10081769
Chicago/Turabian StyleÖörni, Katariina, and Petri T. Kovanen. 2021. "Aggregation Susceptibility of Low-Density Lipoproteins—A Novel Modifiable Biomarker of Cardiovascular Risk" Journal of Clinical Medicine 10, no. 8: 1769. https://doi.org/10.3390/jcm10081769
APA StyleÖörni, K., & Kovanen, P. T. (2021). Aggregation Susceptibility of Low-Density Lipoproteins—A Novel Modifiable Biomarker of Cardiovascular Risk. Journal of Clinical Medicine, 10(8), 1769. https://doi.org/10.3390/jcm10081769






