Abstract
Stand-alone (SA) zero-profile implants are an alternative to cervical plating (CP) in anterior cervical discectomy and fusion (ACDF). In this study, we investigate differences in surgical outcomes between SA and CP in ACDF. We conducted a retrospective analysis of 166 patients with myelopathy and/or radiculopathy who had ACDF with SA or CP from Jan 2013–Dec 2016. We measured surgical outcomes including Bazaz dysphagia score at 3 months, Nurick grade at last follow-up, and length of hospital stay. 166 patients (92F/74M) were reviewed. 92 presented with radiculopathy (55%), 37 with myelopathy (22%), and 37 with myeloradiculopathy (22%). The average operative time with CP was longer than SA (194 ± 69 vs. 126 ± 46 min) (p < 0.001), as was the average length of hospital stay (2.1 ± 2 vs. 1.5 ± 1 days) (p = 0.006). At 3 months, 82 patients (49.4%) had a follow-up for dysphagia, with 3 patients reporting mild dysphagia and none reporting moderate or severe dysphagia. Nurick grade at last follow-up for the myelopathy and myeloradiculopathy cohorts improved in 63 patients (85%). Prolonged length of stay was associated with reduced odds of having an optimal outcome by 0.50 (CI = 0.35–0.85, p = 0.003). Overall, we demonstrate that there is no significant difference in neurological outcome or rates of dysphagia between SA and CP, and that both lead to overall improvement of symptoms based on Nurick grading. However, we also show that the SA group has shorter length of hospital stay and operative time compared to CP.
1. Introduction
Degenerative disease of the cervical spine manifests in a wide spectrum of pathologies that encompass disc degeneration, disc herniation, vertebral restructuring, osteophyte formation, and ligamentous hypertrophy [1]. Compression of the neural elements can lead to cervical radiculopathy, myelopathy, or myeloradiculopathy. In the treatment of these pathologies, an anterior, posterior, or combined anterior/posterior surgical approach can be undertaken. However, anterior approaches are often favored for patients with single level disc disease, kyphotic deformity and large focal anterior pathology [2].
Anterior cervical discectomy and fusion (ACDF) is considered the gold standard in the management of cervical disc disease [3,4]. This procedure has been improved on over time since first described by Smith and Robinson in the 1950s, mainly via technological advances. Over the past few decades, ACDF has been coupled with anterior cervical plating (CP), which is thought to reduce the risk of graft extrusion, increase the likelihood of fusion, maintain appropriate lordosis, and reduce the risk of subsidence [5]. In recent years, zero-profile, stand-alone (SA) interbody spacers have been developed as an alternative aimed at decreasing operative time, improving dysphagia complication rates, and preventing adjacent level disease [6], Figure 1. Indications for ACDF with plating or stand-alone cages are variable and are operator dependent, however, the following indications are often used, cases of instability (degenerative or post-traumatic), presence of significant degeneration, concern for fusion failure including in cases of poor bone quality (osteoporosis, rheumatoid arthritis) and tobacco use. In addition, further indication exists with significant alignment correction and increasing number of operated segments [7,8].
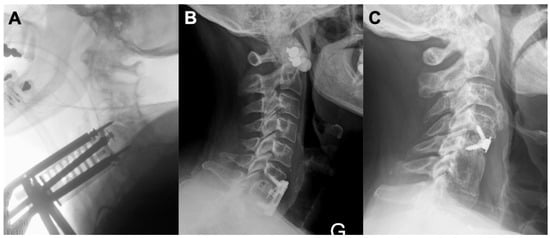
Figure 1.
Anterior cervical cage placement and fixation. (A) Intraoperative lateral X-ray to assess ACDF cage placement. Casper pins can be seen in the vertebral bodies above and below. (B) Post-operative lateral X-ray showing a single level ACDF (HRCC, Eurospine) at C6-C7 secured by a plate (Venture, Medtronic). (C) Post-operative lateral X-ray showing a single level ACDF at C4-5 (Zero-P cage, DePuy Synthes) for the treatment of myelopathy due to adjacent segment disease after a fusion with autologous iliac crest bone at C5-6. ACDF = Anterior Cervical Discectomy and Fusion.
There is a dearth of studies in the literature comparing outcomes between SA and CP in single and multilevel ACDF for degenerative cervical disc disease. When compared, the clinical outcomes and dysphagia rates have been either equivocal or not statistically significant [5,9,10,11,12,13]. It remains unclear if this has been due to the limited number patients in these studies and/or the amount of follow-up time.
We sought to study a large North American patient population undergoing ACDF with SA or CP for single and multilevel degenerative disc disease. Herein, we report our experience on a retrospectively collected series of patients with follow-up of up to 24 months after surgery, and describe clinical outcomes and dysphagia rates related to these two techniques. To our knowledge, this cohort represents one of the largest that has been studied in North America.
2. Materials and Methods
Between January 2013 to December 2016, a total of 182 patients underwent single to three-level ACDF in the Department of Neurosurgery at Yale New Haven Hospital, New Haven, CT, USA. Of the 182 patients, we retrospectively reviewed 166 consecutive patients that had received ACDF (Figure 2). Yale University’s IRB approved the protocol for this study (protocol number 200020713), and the study was exempt from informed consent. Inclusion criteria included: signs and symptoms of cervical radiculopathy, myelopathy, or myeloradiculopathy, unresponsiveness to conservative measures, ages between 18–85, and disc herniation identified by MRI with evidence of nerve root and/or cord compression. Exclusion criteria included: patients presenting with ossification of the posterior longitudinal ligament, a history of malignancy, evidence of systemic or local infection, history of cervical spine trauma, prior cervical spine surgery, and patients requiring simultaneous anterior and posterior surgery. Demographic information, medical comorbidities, selected medications and selected personal history were also collected.
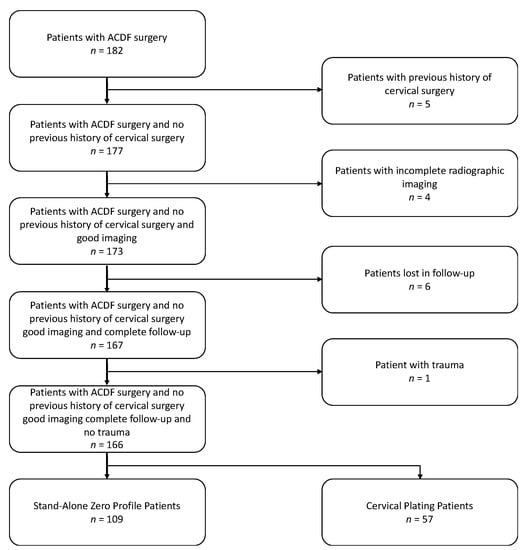
Figure 2.
Flow Chart of Patient Cohort. ACDF = Anterior Cervical Discectomy and Fusion.
2.1. Surgical Procedure
All surgical procedures were performed by two senior spine surgeons using the standard Smith-Robinson approach on the patient’s right side. After sterile prep and draping, a right-sided transverse incision was made with a #10 blade. The platysma was transected using bovie electrocautery. Fascial planes under the platysma were exposed cranially and caudally using Metzenbaum scissors. A corridor was then made in between the sternocleidomastoid muscle and strap muscles, preserving their respective fascial planes. Using Cloward hand-held retractors, the esophagus was protected medially and the carotid laterally. The prevertebral fascia was dissected off the ventral spine, exposing our index disc level(s) and longus colli bilaterally. Once our index disc level(s) were confirmed with a needle and fluoroscopy, bilateral colli were dissected of the lateral ventral spine using bovie electrocautery. Appropriately sized retraction blades with teeth were placed under the dissected longus colli to retract over the longus colli away from our working field. Caspar pins were then applied to the vertebral bodies above and below to help distract our disc space. Disc was removed with great care taken in removing the cartilaginous endplate to avoid disruption and damage of the bony integrity of the endplates. Posterior osteophytes were drilled using a high-speed cutting burr in combination with Kerrison rongeurs. After decompression of the spinal cord and nerve roots, the appropriate size cage was selected using trial spacers under fluoroscopic guidance to ensure good height and width as well as to not over-distract the facet joints. We used demineralized bone matrix to pack all interbody spacers. For patients undergoing SA device insertion (Globus Coalition AGX, Audubon, PA, USA), the implant was placed into the intervertebral disc space and a pilot hole was drilled at the rostral and caudal endplates under fluoroscopic guidance and this was followed by screw insertion. For patients undergoing CP devices, the spacer was inserted under fluoroscopic guidance followed by positioning of a 4-hole plate across the midline of rostral and caudal ventral vertebral bodies. Pilot holes were drilled into rostral and caudal vertebral bodies followed by screw insertion, again using fluoroscopy to ensure proper placement.
2.2. Clinical Measures
The operative procedure details such as the post-operative symptoms, the post-operative Nurick grade, the number of index levels, operating time, blood loss, presence of a CSF leak, and hospital length of stay were all collected. Nurick grade scores were collected on pre-op, 2 weeks, 3-, 6-, 12-months, and up to 24-months or last follow-up. Neurological outcome was dichotomized in the Nurick grade. Outcome measures included Bazaz dysphagia score at 3 months [14]. We defined optimal outcome as an improvement in the Nurick grade. We defined suboptimal outcome as no change or a decline in Nurick grade.
2.3. Statistical Analysis
Statistical analysis was performed with R-studio Desktop v1.1.383 (R-studio, Boston, MA, USA) programming software. Continuous variables are presented as mean (standard deviation (SD)) or median (interquartile range (IQR)), while discrete variables are presented as count (percentage (%)).
Assessments of potentially significant differences between patients with optimal and suboptimal outcomes groups were performed using the Fisher exact test for categorical variables and the Mann-Whitney U test for continuous variables.
We constructed a multivariable logistic regression model by including variables that reached a predetermined significance level of p < 0.2 in univariate analysis. Additionally, universal confounders and other variables selected based on expert opinion were forced into the model, including Nurick grade and number of levels of surgery. Covariates with p > 0.1 were removed and collinearity was assessed based on variance inflation factor. A 2-sided p value of <0.05 was used to determine which variables were independently associated with an optimal outcome.
3. Results
3.1. Demographics
Our baseline patient population characteristics are reported in Table 1. A total of 166 patients (92 females and 74 males) underwent ACDF and met our inclusion criteria, with age ranging from 23 to 85 (mean 53 years). Of the 166 patients, 92 (55%) presented with radiculopathy, 37 (22%) with myelopathy, and 37 (22%) with myeloradiculopathy. In comparing SA and CP patients, 61% and 46% suffered from radiculopathy, 14% and 39% from myelopathy, and 26% and 16% from myeloradiculopathy, respectively.

Table 1.
Population Characteristics.
Twenty-four (14%) of our patients had diabetes, 45 (27%) were current tobacco users, 47 (28%) had a history of tobacco use longer than 1-year and 3 patients (2%) were formally diagnosed with osteoporosis. For preoperative pain management, 61 (37%) patients were currently using opioid medications, 40 (24%) were on Gabapentin or Pregabalin, 58 (35%) were using NSAIDs for over 3 months, 54 (33%) were on antidepressants, and 13 (8%) were taking steroids chronically for medical conditions. In addition, 98 (59%) patients were actively involved in physical therapy and 22 (13%) had at least one epidural steroid injection.
Among the 166 patients, 109 underwent ACDF with SA devices (66%) and 57 underwent ACDF with CP (34%). Eighty-five patients (51%) underwent 1 level ACDF; 65 patients (39%) underwent 2 levels and 16 patients (10%) had 3 levels. There was no difference in the number of levels of surgery between the SA and CP groups (Table 2). The average duration of surgery for all ACDF procedures was 150 (±64) min, with 194 (±69) and 126 (±46) min for CP and for SA respectively (p < 0.001). The blood loss was minimal; only 4 patients (2%) had more than 100 mL of blood loss. Only one patient had a CSF leak. The average length of hospital stay for the total population was 1.7 ± 1 days, with the SA group having a shorter length of stay compared to the CP group (1.5 ± 1 vs. 2.1 ± 2 days) (p = 0.006).

Table 2.
Surgical Details.
3.2. Clinical Outcomes
The mean follow-up for the SA and plate groups was 7.5 months and 10.6 months, respectively, with an overall mean follow-up of 8.6 months. Of the 166 patients, 82 (49%) had a post-surgical follow-up appointment at 3 months to assess for dysphagia. Three patients had mild dysphagia and none of them had moderate or severe dysphagia. However, all of these patients recovered with no further consequences at the last follow-up. As shown in Table 3, the mean Nurick score for the myelopathy and myeloradiculopathy groups improved regardless of the surgical technique or number of index levels. The baseline Nurick score was a score of 1 for 21 patients (28%), a score of 2 for 41 patients (55%), a score of 3 for 8 patients (11%), a score of 4 for 3 patients (4%) and a score of 6 for 1 patient (1%). The Nurick score at last follow up was 0 for 55 patients (74%), 1 for 12 patients (16%), 2 for 5 patients (7%), 3 for 1 patient (1%), and 6 for 1 patient (1%). Overall, 63 patients improved their Nurick score (defined as an optimal outcome) while 11 patients showed no change or decline in their Nurick score (defined as a suboptimal outcome).

Table 3.
Surgery Outcomes for Myelopathy and Myeloradiculopathy Cohorts.
Multivariable analysis (Table 4) revealed that length of stay is a statistically significant independent predictor of suboptimal outcome. Prolonged length of stay was associated with reduced odds of having an optimal outcome by 0.50 (95% CI = 0.35–0.85, p = 0.003). Moreover, the SA technique was not found to be an independent predictor of better outcomes.

Table 4.
Multivariable Analysis.
4. Discussion
ACDF is a well-established surgical treatment for anterior degenerative cervical pathology. ACDF is often done with the use of an anterior vertebral body plate, with the goal of maintaining stability, promoting fusion, preventing graft extrusion, preventing graft subsidence, and maintaining desired cervical lordosis. Potential instability in both degenerative and traumatic cases is a common reason for the addition of additional structural support via plate fixation. However, a known morbidity of ACDF with cervical plating is post-operative dysphagia, ranging from 2 to 67% in the post-operative period [15]. With the goal of reducing dysphagia and other perioperative morbidities, stand-alone (SA) ACDF systems were developed. Additional potential benefits of SA devices include that they can provide lordotic correction and are anchored with screw fixation. The latter aspect may be relevant in patients with segmental degenerative instability.
Despite the introduction of stand-alone cages as an alternative to cervical plating, clinical outcomes appear to be similar between the two groups. A systematic review by Cheung et al. of 19 studies comparing ACDF with a cage-only technique and conventional cage-plate technique found that stand-alone cage was associated with less dysphagia, intraoperative blood loss, and adjacent segment disease. However, the stand-alone cage was also shown to have increased rates of subsidence and less restoration of cervical lordosis [5]. Similarly, a recent meta-analysis by Gabr et al. demonstrated that stand-alone anchored spacers were associated with less dysphagia compared to the plate-screw construct [16]. Lastly, a systematic review by Boer et al. showed that there was no difference in clinical (visual analog scale, neck disability index) or radiological (cervical lordosis and fusion) outcomes between the two groups, but stand-alone devices were associated with shorter operative time [17].
The pathogenesis of dysphagia in ACDF has not been clearly elucidated. Previous studies have implicated that injury to the esophagus, soft tissue edema, localized bleeding, and adhesions surrounding the CP may contribute to post-operative dysphagia [15]. Indeed, removal of the anterior plate and lysis of associated adhesions has been shown to clinically improve patients’ experience of dysphagia both immediately after surgery and at later timepoints [18]. A study by Lee et al. also noted a correlation between the thickness of the cervical plate and post-operative dysphagia, suggesting that physical obstruction may also play a role [19].
In addition to demonstrating no statistically significant difference in morbidity of SA and CP with respect to post-operative dysphagia, our study also found no significant difference in intraoperative blood loss. This data differs slightly from the results described in Cheung et al., which suggest that a cage-only technique is associated with less intraoperative bleeding. However, it is important to note that the average blood loss of ACDF is quite low, so the difference that was noted between SA and CP is not likely to be clinically significant [5]. We also found a significant reduction in operative time with cage-only implants, as well as a decrease in hospital length of stay. Consistent with other studies comparing SA to CP, our data support that either intervention confers optimal outcomes in patients with degenerative cervical myelopathy or radiculopathy. Based on Nurick scores postoperatively, 85% of patients treated in our study had improvement in neurological symptoms, social independence, walking ability, and ability to work full time, with no significant difference in outcomes between SA and CP.
Given our findings with respect to morbidity, there is no clear advantage of stand-alone cage over cervical plating. The stand-alone cage was not found to be a predictor of superior outcomes. Based on these results, it will be important in future studies to investigate the cost-effectiveness of CP vs. SA in anterior cervical discectomy and fusion; in the setting of similar surgical outcomes, as was reported in our study, the more affordable option should be pursued.
An important point to note is that while anterior approaches are indicated in patients with kyphosis, it is unclear how the choice of these 2 techniques affects surgical decision-making. Some may prefer stand-alone cages in such instances given that they can provide different degrees of lordosis. On the other hand, if the implicated disc is present adjacent to a kyphotic segment, increasing lordosis at that level may increase segmental kyphosis at the adjacent level. Further research is warranted with regards to whether these 2 techniques carry different risks and benefits with regards to patients with cervical kyphosis or malalignment.
5. Limitations
There are important limitations with our study. First, patients were not randomized to treatment modality. The two surgeons in this study had different preferences in using SA vs. CP, such that one surgeon used only SA while the other used only CP in their practice. Thus, outcomes and operative time may be biased by surgeon experience, number of years in practice, and technique. However, this also eliminates selection bias, as patients were not selected to receive SA versus CP based on any preoperative parameters or surgeon preference, as each surgeon exclusively performs ACDF with SA or CP. Second, this study does not include a power analysis to determine if the sample size in adequate. Nonetheless, it is important to note that this cohort represents one of the largest studies that examines surgical outcomes between SA and CP, and is one of few in North America. Third, our study warrants a cost analysis between the two approaches to further identify which is more favorable if no change in morbidity is observed. Moreover, if dysphagia avoidance is not an indication for SA grafts, other variables such as the relationship of operative time and blood loss, or graft extrusion, pseudoarthrosis, subsidence, and sagittal alignment should be further assessed between SA and CP techniques to further understand the advantages of the SA technique. Fourth, the Bazaz criteria were used in this study rather than other metrics, such as the EAT assessment, which have been validated as an outcome tool for dysphagia. Lastly, because this study is a retrospective analysis, we were unable to assess the presence of dysphagia in every patient included in this study, due to inconsistent reporting in the absence of symptoms.
6. Conclusions
Patients undergoing ACDF with SA had significantly decreased hospital length of stay and operative time compared to patients with CP. The type of procedure did not affect neurological outcome based on Nurick grade. Hospital length of stay was found to be a predictor of a poor outcome regardless of technique. In general, both ACDF with CP and SA are effective treatment options and provide comparable outcomes.
Author Contributions
Conceptualization, S.S., J.C.-Q. and A.N.; methodology, S.S., J.C.-Q. and A.N..; software, S.S., J.C.-Q. and A.N..; validation, S.S., J.C.-Q. and A.N.; formal analysis, S.S., J.C.-Q. and A.N.; investigation, S.S., J.C.-Q. and A.N.; resources, S.S., J.C.-Q. and A.N.; data curation, S.S., J.C.-Q. and A.N.; writing—original draft preparation, S.S., J.C.-Q., A.N., and K.P.; writing—review and editing, all authors; visualization, S.S., J.C.-Q. and A.N.; supervision, J.C.; project administration, J.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Yale University (protocol code 200020713).
Informed Consent Statement
The study was exempt from informed consent.
Data Availability Statement
Data available on request (not publicly available for privacy protection).
Acknowledgments
We would like to acknowledge Murat Gunel and Patrick Tomak for their critical review of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Nouri, A.; Tetreault, L.; Singh, A.; Karadimas, S.K.; Fehlings, M. Degenerative Cervical Myelopathy. Spine 2015, 40, E675–E693. [Google Scholar] [CrossRef] [PubMed]
- Nouri, A.; Martin, A.R.; Nater, A.; Witiw, C.D.; Kato, S.; Tetreault, L.; Reihani-Kermani, H.; Santaguida, C.; Fehlings, M.G. Influence of Magnetic Resonance Imaging Features on Surgical Decision-Making in Degenerative Cervical Myelopathy: Results from a Global Survey of AOSpine International Members. World Neurosurg. 2017, 105, 864–874. [Google Scholar] [CrossRef] [PubMed]
- Angevine, P.D.; Arons, R.R.; McCormick, P.C. National and Regional Rates and Variation of Cervical Discectomy with and Without Anterior Fusion, 1990–1999. Spine 2003, 28, 931–939. [Google Scholar] [CrossRef] [PubMed]
- Korinth, M.C. Treatment of Cervical Degenerative Disc Disease–Current Status and Trends. Cent. Eur. Neurosurg. Zent. Neurochir. 2008, 69, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Cheung, Z.B.; Gidumal, S.; White, S.; Shin, J.; Phan, K.; Osman, N.; Bronheim, R.; Vargas, L.; Kim, J.; Cho, S.K. Comparison of Anterior Cervical Discectomy and Fusion with a Stand-Alone Interbody Cage Versus a Conventional Cage-Plate Technique: A Systematic Review and Meta-Analysis. Glob. Spine J. 2018, 9, 446–455. [Google Scholar] [CrossRef] [PubMed]
- Barbagallo, G.M.V.; Romano, D.; Certo, F.; Milone, P.; Albanese, V. Zero-P: A new zero-profile cage-plate device for single and multilevel ACDF. A single Institution series with four years maximum follow-up and review of the literature on zero-profile devices. Eur. Spine J. 2013, 22, 868–878. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matz, P.G.; Pritchard, P.R.; Hadley, M.N. Anterior cervical approach for the treatment of cervical myelopathy. Neurosurgery 2007, 60, S1–S64. [Google Scholar] [CrossRef] [PubMed]
- Bible, J.E.; Kang, J.D. Anterior cervical discectomy and fusion: Surgical indications and outcomes. Semin. Spine Surg. 2016, 28, 80–83. [Google Scholar] [CrossRef]
- Chen, Y.; Chen, H.; Wu, X.; Wang, X.; Lin, W.; Yuan, W. Comparative analysis of clinical outcomes between zero-profile implant and cages with plate fixation in treating multilevel cervical spondilotic myelopathy: A three-year follow-up. Clin. Neurol. Neurosurg. 2016, 144, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Song, K.-J.; Taghavi, C.E.; Lee, K.-B.; Song, J.-H.; Eun, J.-P. The Efficacy of Plate Construct Augmentation Versus Cage Alone in Anterior Cervical Fusion. Spine 2009, 34, 2886–2892. [Google Scholar] [CrossRef] [PubMed]
- Yun, D.-J.; Lee, S.-J.; Park, S.-J.; Oh, H.S.; Lee, Y.J.; Oh, H.M. Use of a Zero-Profile Device for Contiguous 2-Level Anterior Cervical Diskectomy and Fusion: Comparison with Cage with Plate Construct. World Neurosurg. 2017, 97, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Liu, Z.-D.; Li, X.-F.; Qian, L.; Zhong, G.-B.; Chen, F.-J. Comparison of plate-cage construct and stand-alone anchored spacer in the surgical treatment of three-level cervical spondylotic myelopathy: A preliminary clinical study. Spine J. 2015, 15, 1973–1980. [Google Scholar] [CrossRef] [PubMed]
- Vaněk, P.; Bradáč, O.; DeLacy, P.; Lacman, J.; Beneš, V. Anterior Interbody Fusion of the Cervical Spine with Zero-P Spacer. Spine 2013, 38, E792–E797. [Google Scholar] [CrossRef] [PubMed]
- Bazaz, R.; Lee, M.J.; Yoo, J.U. Incidence of Dysphagia after Anterior Cervical Spine Surgery. Spine 2002, 27, 2453–2458. [Google Scholar] [CrossRef] [PubMed]
- Fountas, K.N.; Kapsalaki, E.Z.; Nikolakakos, L.G.; Smisson, H.F.; Johnston, K.W.; Grigorian, A.A.; Lee, G.P.; Robinson, J.S. Anterior Cervical Discectomy and Fusion Associated Complications. Spine 2007, 32, 2310–2317. [Google Scholar] [CrossRef] [PubMed]
- Gabr, M.A.; Touko, E.; Yadav, A.P.; Karikari, I.; Goodwin, C.R.; Groff, M.W.; Ramirez, L.; Abd-El-Barr, M.M. Improved Dysphagia Outcomes in Anchored Spacers Versus Plate-Screw Systems in Anterior Cervical Discectomy and Fusion: A Systematic Review. Glob. Spine J. 2020, 10, 1057–1065. [Google Scholar] [CrossRef] [PubMed]
- Boer, L.F.R.; Zorzetto, E.; Yeh, F.; Wajchenberg, M.; Martins, D.E. Degenerative Cervical Disorder—Stand-alone Cage Versus Cage and Cervical Plate: A Systematic Review. Glob. Spine J. 2021, 11, 249–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fogel, G.R.; McDonnell, M.F. Surgical treatment of dysphagia after anterior cervical interbody fusion. Spine J. 2005, 5, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-H.; Hyun, S.-J.; Kim, M.J.; Yeom, J.S.; Kim, W.H.; Kim, K.-J.; Jahng, T.-A.; Kim, H.-J.; Yoon, S.H. Comparative Analysis of 3 Different Construct Systems for Single-level Anterior Cervical Discectomy and Fusion. J. Spinal Disord. Tech. 2013, 26, 112–118. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).