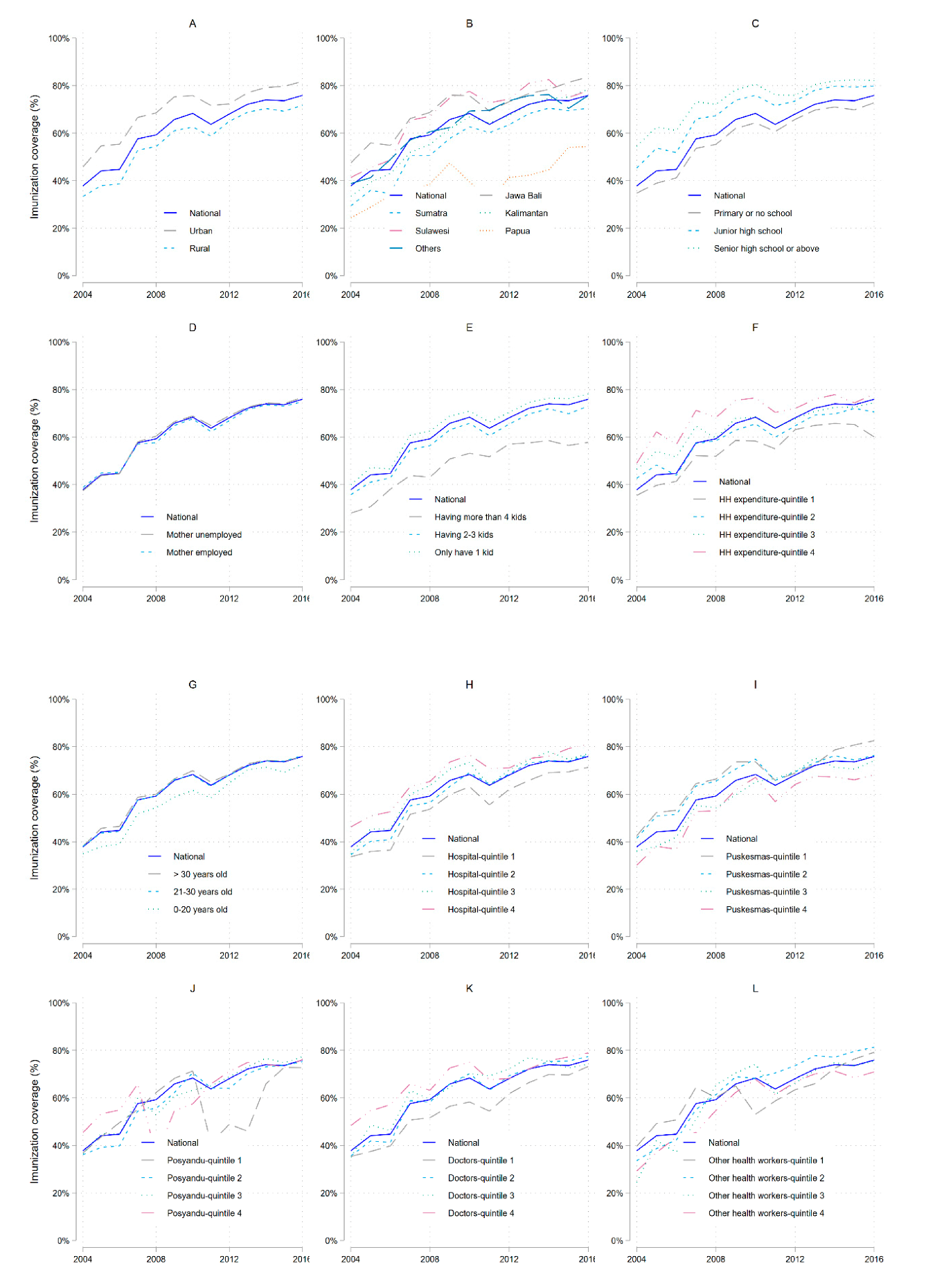
Trends, Spatial Disparities, and Social Determinants of DTP3 Immunization Status in Indonesia 2004–2016
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design and Data
2.2. Sociodemographic and District Factors
2.3. Statistical Analysis
3. Results
4. Discussion
Study Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Informed Consent
References
- Zakikhany, K.; Efstratiou, A. Diphtheria in Europe: Current problems and new challenges. Future Microbiol. 2012, 7, 595–607. [Google Scholar] [CrossRef] [PubMed]
- Clarke, K.E.N.; MacNeil, A.; Hadler, S.; Scott, C.; Tiwari, T.S.P.; Cherian, T. Global epidemiology of diphtheria, 2000–2017. Emerg. Infect. Dis. 2019, 25, 1834–1842. [Google Scholar] [CrossRef] [PubMed]
- Hughes, G.J.; Mikhail, A.F.W.; Husada, D.; Irawan, E.; Kafatos, G.; Bracebridge, S.; Pebody, R.; Efstratiou, A. Seroprevalence and determinants of immunity to diphtheria for children living in two districts of contrasting incidence during an outbreak in East Java, Indonesia. Pediatr. Infect. Dis. J. 2015, 34, 1152–1156. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Diphteria Reported Cases; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Tosepu, R.; Gunawan, J.; Effendy, D.S.; Ahmad, L.O.A.I.; Farzan, A. The outbreak of diphtheria in Indonesia. Pan Afr. Med. J. 2018, 31, 1–5. [Google Scholar] [CrossRef]
- Holipah; Maharani, A.; Kuroda, Y. Determinants of immunization status among 12- to 23-month-old children in Indonesia (2008-2013): A multilevel analysis. BMC Public Health 2018, 18, 1–11. [Google Scholar] [CrossRef]
- Herliana, P.; Douiri, A. Determinants of immunisation coverage of children aged 12–59 months in Indonesia: A cross-sectional study. BMJ Open 2017, 7, e015790. [Google Scholar] [CrossRef]
- Streatfield, K.; Singarimbun, M. Social factors affecting use of immunization in Indonesia. Soc. Sci. Med. 1988, 27, 1237–1245. [Google Scholar]
- Directorat General for Disease Control and Environmental Health. Comprehensive Multi Year Plan National Immunization Program Indonesia. 2010. Available online: https://www.gavi.org/sites/default/files/document/comprehensive-multi-year-plan-for--2010-2014pdf.pdf (accessed on 25 September 2019).
- World Health Organization (WHO). WHO Vaccine-Preventable Diseases: Monitoring System. 2019 Global Summary. Available online: https://apps.who.int/immunization_monitoring/globalsummary/countries?countrycriteria%5Bcountry%5D%5B%5D=IDN (accessed on 25 September 2019).
- Surbakti, P. The Development of Susenas in Indonesia’s National Socio-Economic Survey: A Continual Data Source for Analysis on Welfare Development; Central Bureau of Statistics: Jakarta, Indonesia, 1995; pp. 14–15. [Google Scholar]
- Van de Walle, D. On the Use of the Susenas for Modelling Consumer Behaviour. Bull. Indones. Econ. Stud. 1988, 24, 107–121. [Google Scholar] [CrossRef]
- Statistics Indonesia. In Indonesia-Village Potential 2014; Jakarta, 2016; Available online: https://microdata.bps.go.id/mikrodata/index.php/catalog/648 (accessed on 12 December 2019).
- Deaton, A.; Zaidi, S. Guidelines for Constructing Consumption Aggregates for Wefare Annalysis; The World Bank: Washington, DC, USA, 2002; ISBN 0821349902. [Google Scholar]
- Sullivan, M.C.; Tegegn, A.; Tessema, F.; Galea, S.; Hadley, C. Minding the immunization gap: Family characteristics associated with completion rates in rural Ethiopia. J. Community Health 2010, 35, 53–59. [Google Scholar] [CrossRef]
- Abadura, S.A.; Lerebo, W.T.; Kulkarni, U.; Mekonnen, Z.A. Individual and community level determinants of childhood full immunization in Ethiopia: A multilevel analysis. BMC Public Health 2015, 15, 972. [Google Scholar] [CrossRef]
- Babirye, J.N.; Engebretsen, I.M.S.; Makumbi, F.; Fadnes, L.T.; Wamani, H.; Tylleskar, T.; Nuwaha, F. Timeliness of childhood vaccinations in kampala uganda: A community-based cross-sectional study. PLoS ONE 2012, 7, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, R.; Rammohan, A.; Awofeso, N. Correlates of first dose of measles vaccination delivery and uptake in Indonesia. Asian Pac. J. Trop. Med. 2011, 4, 140–145. [Google Scholar] [CrossRef]
- Larsen, K.; Merlo, J. Appropriate assessment of neighborhood effects on individual health: Integrating random and fixed effects in multilevel logistic regression. Am. J. Epidemiol. 2005, 161, 81–88. [Google Scholar] [CrossRef] [PubMed]
- De, P.; Bhattacharya, B.N. Determinants of child immunization in four less-developed states of North India. J. Child Heal. Care 2002, 6, 34–50. [Google Scholar] [CrossRef]
- Cui, F.Q.; Gofin, R. Immunization coverage and its determinants in children aged 12–23 months in Gansu, China. Vaccine 2007, 25, 664–671. [Google Scholar] [CrossRef]
- Glatman-Freedman, A.; Nichols, K. The effect of social determinants on immunization programs. Hum. Vaccin. Immunother. 2012, 8, 293–301. [Google Scholar] [CrossRef]
- Reynolds, H.W.; Wong, E.L.; Tucker, H. Adolescents’ use of maternal and child health services in developing countries. Int. Fam. Plan. Perspect. 2006, 32, 6–16. [Google Scholar] [CrossRef]
- Adedokun, S.T.; Uthman, O.A.; Adekanmbi, V.T.; Wiysonge, C.S. Incomplete childhood immunization in Nigeria: A multilevel analysis of individual and contextual factors. BMC Public Health 2017, 17, 236. [Google Scholar] [CrossRef]
- Onsomu, E.O.; Abuya, B.A.; Okech, I.N.; Moore, D.K.; Collins-McNeil, J. Maternal Education and Immunization Status Among Children in Kenya. Matern. Child Health J. 2015, 19, 1724–1733. [Google Scholar] [CrossRef]
- Usman, H.R.; Kristensen, S.; Rahbar, M.H.; Vermund, S.H.; Habib, F.; Chamot, E. Determinants of third dose of diphtheria-tetanus-pertussis (DTP) completion among children who received DTP1 at rural immunization centres in Pakistan: A cohort study. Trop. Med. Int. Heal. 2010, 15, 140–147. [Google Scholar] [CrossRef]
- Fernandez, R.C.; Awofeso, N.; Rammohan, A. Determinants of apparent rural-urban differentials in measles vaccination uptake in Indonesia. Rural Remote Health 2011, 11, 1–14. [Google Scholar]
- Torun, S.D.; Bakirci, N. Vaccination coverage and reasons for non-vaccination in a district of Istanbul. BMC Public Health 2006, 6, 125. [Google Scholar] [CrossRef]
- Grossman, M. Chapter 10 Education and Nonmarket Outcomes. Handb. Econ. Educ. 2006, 1, 577–633. [Google Scholar]
- Lindeboorn, M.; Llena-Nozal, A.; van der Klaauw, B. Parental education and child health: Evidence from a schooling reform. J. Heal. Econ. 2009, 28, 109. [Google Scholar] [CrossRef] [PubMed]
- Cawley, J.; Liu, F. Maternal employment and childhood obesity: A search for mechanisms in time use data. Econ. Hum. Biol. 2012, 10, 352–364. [Google Scholar] [CrossRef]
- Sia, D.; Fournier, P.; Kobiané, J.-F.; Sondo, B.K. Rates of coverage and determinants of complete vaccination of children in rural areas of Burkina Faso (1998–2003). BMC Public Health 2009, 9, 416. [Google Scholar] [CrossRef] [PubMed]
- Maharani, A.; Tampubolon, G. Has decentralisation affected child immunisation status in Indonesia? Glob. Health Action 2014, 7, 24913. [Google Scholar] [CrossRef] [PubMed]
- Kawakatsu, Y.; Tanaka, J.; Ogawa, K.; Ogendo, K.; Honda, S. Effects of three interventions and determinants of full vaccination among children aged 12-59 months in Nyanza province, Kenya. Public Health 2015, 129, 1530–1538. [Google Scholar] [CrossRef] [PubMed]
- Mbengue, M.A.S.; Sarr, M.; Faye, A.; Badiane, O.; Camara, F.B.N.; Mboup, S.; Dieye, T.N. Determinants of complete immunization among senegalese children aged 12–23 months: Evidence from the demographic and health survey. BMC Public Health 2017, 17, 630. [Google Scholar] [CrossRef]
- Tandiara, N. Improving immunization coverage: A review of EPI in West Sulawesi Province, Indonesia. In Proceedings of the 45th International Course in Health Development, 11–22 September 2008 Amsterdam, The Netherlands; KIT (Royal Trpical Institute/Vrije Universiteit Amsterdam: Amsterdam, The Netherlands, 2009; Available online: http://www.bibalex.org/search4dev/files/352398/185348.pdf (accessed on 14 December 2019).
- Lundine, J.; Hadikusumah, R.Y.; Sudrajat, T. Indonesia’s progress on the 2015 Millenium Development Goals. Strateg. Rev. 2013, 3, 54–66. [Google Scholar]
- Nazri, C.; Yamazaki, C.; Kameo, S.; Herawati, D.M.D.; Sekarwana, N.; Raksanagara, A.; Koyama, H. Factors influencing mother’s participation in Posyandu for improving nutritional status of children under-five in Aceh Utara district, Aceh province, Indonesia. BMC Public Health 2016, 16, 69. [Google Scholar] [CrossRef] [PubMed]
- Paramita, S.A.; Yamazaki, C.; Setiawati, E.P.; Koyama, H. Distribution trends of Indonesia’s health care resources in the decentralization era. Int. J. Health Plan. Manag. 2018, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Republic of Indonesia. Indonesia Health Profile 2014; 2015; Volume 1, ISBN 9788578110796. Available online: https://www.kemkes.go.id/resources/download/pusdatin/profil-kesehatan-indonesia/profil-kesehatan-indonesia-2014.pdf (accessed on 14 December 2019).
- Maternal, R.; Lives, S. Reducing Maternal and Neonatal Mortality in Indonesia; 2013; ISBN 978-0-309-29076-0. Available online: https://www.ncbi.nlm.nih.gov/books/NBK201706/pdf/Bookshelf_NBK201706.pdf (accessed on 4 January 2020).
- Anderson, I.; Andreasta, M.; Puti, M.; Eko, P. The Production, Distribution, and Performance of Physicians, Nurses, and Midwives in Indonesia an Update. 2014. Available online: http://documents1.worldbank.org/curated/en/912471468254690409/pdf/913240WP0UHC0C00Box385331B00PUBLIC0.pdf (accessed on 4 January 2020).
- Mahendradhata, Y.; Trisnantoro, L.; Listyadewi, S.; Soewondo, P.; Marthias, T.; Harimurti, P. The Republic of Indonesia Health System Review; World Health Organization: Geneve, Switzerland, 2017; Volume 7, ISBN 978-92-9022-516-4. [Google Scholar]


| 2004 | 2010 | 2016 | All Years | |
|---|---|---|---|---|
| Island of residence Papua | Reference | Reference | Reference | Reference |
| Java-Bali | 1.2 (0.61–2.36) | 4.38 (2.25–8.51) ** | 1.53 (0.94–2.48) | 4.46 (3.34–5.97) ** |
| Sumatra | 0.79 (0.43–1.44) | 2.03 (1.1–3.73) * | 0.81 (0.52–1.25) | 2.14 (1.62–2.83) ** |
| Kalimantan | 1.00 (0.54–1.87) | 2.52 (1.32–4.79) * | 1.47 (0.93–2.33) | 2.59 (1.89–3.55) ** |
| Sulawesi | 1.85 (0.99–3.44) | 5.65 (2.99–10.7) ** | 1.53 (0.97–2.41) | 4.37 (3.24–5.9) ** |
| Other islands (Nusa Tenggara, Maluku) | 1.17 (0.6–2.28) | 4.23 (2.2–8.13) ** | 1.25 (0.78–1.99) | 3.1 (2.26–4.27) ** |
| Living area Rural | Reference | Reference | Reference | Reference |
| Urban | 1.14 (1.05–1.23) * | 1.19 (1.1–1.28) ** | 1.24 (1.11–1.37) ** | 1.16 (1.13–1.18) ** |
| Birth attended by health professional No | Reference | Reference | Reference | Reference |
| Yes | 1.57 (1.46–1.7) ** | 1.61 (1.48–1.75) ** | 1.97 (1.71–2.26) ** | 1.53 (1.5–1.56) ** |
| Mother’s age 20 years | Reference | Reference | Reference | Reference |
| 21–30 years | 1.15 (1.02–1.29) * | 1.19 (1.05–1.35) * | 1.3 (1.09–1.54) * | 1.15 (1.11–1.19) ** |
| >30 years | 1.13 (0.99–1.29) | 1.32 (1.15–1.53) ** | 1.44 (1.2–1.73) ** | 1.27 (1.22–1.32) ** |
| Mother’s educational level Primary | Reference | Reference | Reference | Reference |
| Secondary | 1.21 (1.13–1.31) ** | 1.34 (1.24–1.46) ** | 1.3 (1.18–1.44) ** | 1.3 (1.27–1.33) ** |
| Higher | 1.37 (1.19–1.58) ** | 1.43 (1.26–1.63) ** | 1.42 (1.24–1.63) ** | 1.39 (1.34–1.44) ** |
| Mother’s working status No | Reference | Reference | Reference | Reference |
| Yes | 1.07 (1.00–1.15) * | 1.12 (1.04–1.2) * | 0.99 (0.9–1.08) | 1.04 (1.02–1.06) ** |
| Number of children Few | Reference | Reference | Reference | Reference |
| Intermediate | 0.92 (0.85–0.99) * | 0.89 (0.82–0.97) * | 0.85 (0.77–0.95) * | 0.87 (0.86–0.89) ** |
| Many | 0.72 (0.61–0.84) ** | 0.62 (0.52–0.73) ** | 0.56 (0.44–0.72) ** | 0.66 (0.64–0.7) ** |
| Household income | 1.38 (1.29–1.48) ** | 1.36 (1.26–1.46) ** | 1.11 (1.03–1.21) * | 1.27 (1.24–1.29) ** |
| Medical resources/1000 population | ||||
| Hospitals | 1.19 (1.05–1.34) * | 1.2 (1.04–1.39) * | 1.19 (1.06–1.33) * | 0.95 (0.47–1.91) |
| Health centers | 0.41 (0.16–1.09) | 0.88 (0.36–2.15) | 0.63 (0.34–1.16) | 0.94 (0.79–1.11) |
| Village health posts | 2.36 (1.76–3.16) ** | 0.91 (0.59–1.41) | 1.37 (1.12–1.69) * | 1.19 (1.15–1.23) * |
| Doctors | 1.58 (0.8–3.13) | 0.84 (0.44–1.62) | 0.66 (0.35–1.26) | 1.2 (1.07–1.35) * |
| Other health workers | 0.65 (0.45–0.93) * | 1.03 (0.9–1.18) | 0.91 (0.84–0.99) * | 0.97 (0.95–0.98) * |
| Between-district variance | 0.17 | 0.24 | 0.53 | 0.16 |
| ICC | 0.67 | 1.06 | 0.13 | 0.61 |
| Median odds ratio | 2.19 | 2.67 | 2. | 2.11 |
| Island | Hospitals/1000 pop | Health Centers/1000 pop | Integrated Health Posts/1000 pop | Doctors/1000 pop | Other Health Worker/1000 pop |
|---|---|---|---|---|---|
| Papua | 2.52 (0.21–29.73) | 1.82 (1.26–1.52) * | 1.61 (1.37–1.9) ** | 0.64 (0.46–0.89) * | 0.86 (0.81–0.91) ** |
| Java | 4.13 (0.91–18.82) | 3.02 (1.09–8.41) * | 1.06 (0.97–1.16) | 0.93 (0.71–1.2) | 1.19 (1.08–1.31) ** |
| Sumatera | 1.65 (0.59–4.63) | 0.9 (0.64–1.25) | 1.39 (1.3–1.49) ** | 1.24 (1.03–1.51) * | 0.99 (0.96–1.03) |
| Kalimantan | 0.07 (0.00–0.84) * | 0.52 (0.34–0.81) * | 1.01 (0.91–1.13) | 1.26 (0.82–1.94) | 1.09 (1.04–1.16) * |
| Sulawesi | 5.75 (0.37–89.55) | 0.52 (0.36–0.76) * | 1.07 (0.97–1.18) | 1.22 (0.84–1.78) | 0.95 (0.91–0.99) * |
| 2004 n (%) | 2016 n (%) | |
|---|---|---|
| DTP | ||
| Complete | 10,231 (37.83) | 14,329 (75.93) |
| Non complete | 16,814 (62.17) | 4542 (24.07) |
| Polio | ||
| Complete | 10,338 (38.23) | 14,924 (79.24) |
| Non complete | 16,703 (61.77) | 3911 (20.76) |
| Hepatitis B | ||
| Complete | 6948 (25.70) | 13,649 (75.37) |
| Non complete | 20,085 (74.30) | 4461 (24.63) |
| BCG | ||
| Complete | 23,444 (86.70) | 17,472 (92.89) |
| Non complete | 3596 (13.30) | 1337 (7.11) |
| Measles | ||
| Complete | 21,371 (79.05) | 16,003 (85.56) |
| Non complete | 5664 (20.95) | 2701 (14.44) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holipah, H.; Maharani, A.; Sujarwoto, S.; Hinoura, T.; Kuroda, Y. Trends, Spatial Disparities, and Social Determinants of DTP3 Immunization Status in Indonesia 2004–2016. Vaccines 2020, 8, 518. https://doi.org/10.3390/vaccines8030518
Holipah H, Maharani A, Sujarwoto S, Hinoura T, Kuroda Y. Trends, Spatial Disparities, and Social Determinants of DTP3 Immunization Status in Indonesia 2004–2016. Vaccines. 2020; 8(3):518. https://doi.org/10.3390/vaccines8030518
Chicago/Turabian StyleHolipah, Holipah, Asri Maharani, Sujarwoto Sujarwoto, Takuji Hinoura, and Yoshiki Kuroda. 2020. "Trends, Spatial Disparities, and Social Determinants of DTP3 Immunization Status in Indonesia 2004–2016" Vaccines 8, no. 3: 518. https://doi.org/10.3390/vaccines8030518
APA StyleHolipah, H., Maharani, A., Sujarwoto, S., Hinoura, T., & Kuroda, Y. (2020). Trends, Spatial Disparities, and Social Determinants of DTP3 Immunization Status in Indonesia 2004–2016. Vaccines, 8(3), 518. https://doi.org/10.3390/vaccines8030518






