Anal Human Papillomavirus Infection among MSM Attending University in China: Implications for Vaccination
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Sample Collection and Testing
2.4. Variables and Definitions
2.5. Statistical Analyses
3. Results
3.1. Participant Characteristics
3.2. Sexual and High-Risk Behaviors
3.3. Anal HPV Detection and Types
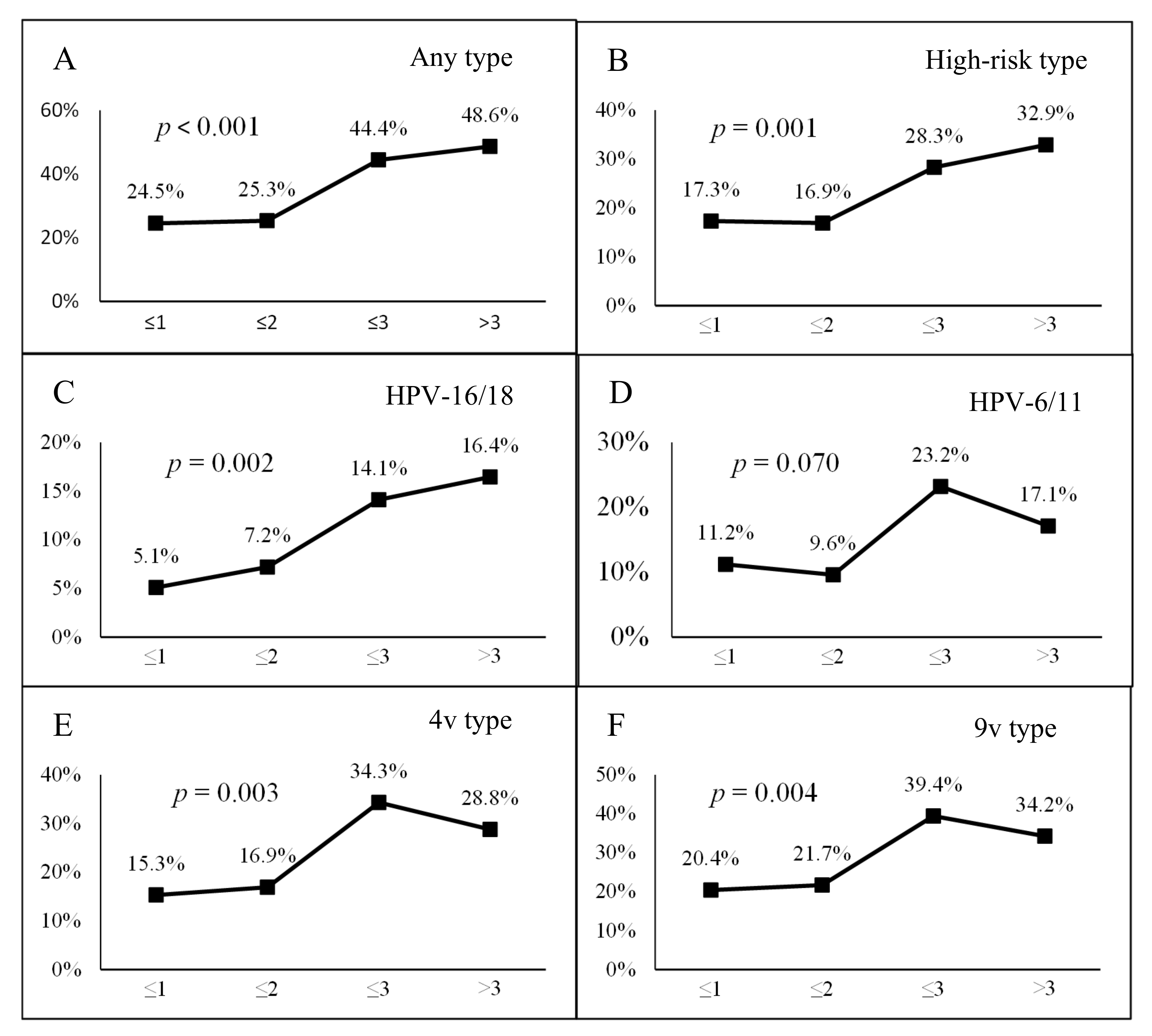
3.4. Risk Factors of Anal HPV Infection
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Brianti, P.; De Flammineis, E.; Mercuri, S.R. Review of HPV-related diseases and cancers. New Microbiol. 2017, 40, 80–85. [Google Scholar]
- Winer, R.L.; Kiviat, N.B.; Hughes, J.P.; Adam, D.E.; Lee, S.K.; Kuypers, J.M.; Koutsky, L.A. Development and duration of human papillomavirus lesions, after initial infection. J. Infect. Dis. 2005, 191, 731–738. [Google Scholar] [CrossRef]
- Shanmugasundaram, S.; You, J. Targeting Persistent Human Papillomavirus Infection. Viruses 2017, 9, 229. [Google Scholar] [CrossRef]
- Anic, G.M.; Lee, J.H.; Stockwell, H.; Rollison, D.E.; Wu, Y.; Papenfuss, M.R.; Villa, L.L.; Lazcano-Ponce, E.; Gage, C.; Silva, R.J.; et al. Incidence and human papillomavirus (HPV) type distribution of genital warts in a multinational cohort of men: The HPV in men study. J. Infect. Dis. 2011, 204, 1886–1892. [Google Scholar] [CrossRef]
- De Martel, C.; Plummer, M.; Vignat, J.; Franceschi, S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int. J. Cancer 2017, 141, 664–670. [Google Scholar] [CrossRef]
- Houlihan, C.F.; Larke, N.L.; Watson-Jones, D.; Smith-McCune, K.K.; Shiboski, S.; Gravitt, P.E.; Smith, J.S.; Kuhn, L.; Wang, C.; Hayes, R. Human papillomavirus infection and increased risk of HIV acquisition. A systematic review and meta-analysis. AIDS (Lond. Engl.) 2012, 26, 2211–2222. [Google Scholar] [CrossRef]
- Geskus, R.B.; Gonzalez, C.; Torres, M.; Del Romero, J.; Viciana, P.; Masia, M.; Blanco, J.R.; Iribarren, M.; De Sanjose, S.; Hernandez-Novoa, B.; et al. Incidence and clearance of anal high-risk human papillomavirus in HIV-positive men who have sex with men: Estimates and risk factors. AIDS (Lond. Engl.) 2016, 30, 37–44. [Google Scholar] [CrossRef]
- Zou, H.; Fairley, C.K.; Hocking, J.S.; Garland, S.M.; Grulich, A.E.; Chen, M.Y. The prevalence of anal human papillomavirus among young HIV negative men who have sex with men. BMC Infect. Dis. 2012, 12, 341. [Google Scholar] [CrossRef]
- Wang, L.; Ding, Z.-W.; Yan, R.-X.; Li, D.-M.; Guo, W.; Ding, G.-W.; Wang, L.-Y.; Qin, Q.-Q.; Hei, F.-X.; Li, P.-L. HIV/AIDS epidemic situation and data analysis among young students from 2006-2009 in China. Chin. J. Epidemiol. 2010, 31, 1017–1021. [Google Scholar] [CrossRef]
- Fan, S.; Yang, Z.; Hou, F.; Yu, M.; Luo, Z.; Liao, M.; Gong, Y.; Meng, X.; Cai, Y.; Zou, H. HIV and syphilis and sexual risk behaviours among men who have sex with men attending university in China: A systematic review and meta-analysis. Sex. Health 2019. [Google Scholar] [CrossRef]
- Zou, H.; Tucker, J.D.; Fan, S.; Xu, J.; Yu, M.; Luo, Z.; Cai, W.; Grulich, A.E. Learning about HIV the hard way: HIV among Chinese MSM attending university. Lancet Infect. Dis. 2018, 18, 16–18. [Google Scholar] [CrossRef]
- World Health Organization. Human papillomavirus vaccines: WHO position paper, May 2017. Wkly. Epidemiol. Rec. 2017, 92, 241–268. [Google Scholar]
- Harper, D.M.; DeMars, L.R. HPV vaccines—A review of the first decade. Gynecol. Oncol. 2017, 146, 196–204. [Google Scholar] [CrossRef]
- Zou, H.; Zhang, L.; Puifung, C.E.; Zhang, L. Teenage men who have sex with men should be vaccinated against human papillomavirus infection. Zhonghua Liu Xing Bing Xue Za Zhi 2014, 35, 1072–1073. [Google Scholar] [CrossRef]
- Fan, S.; Liu, Z.; Luo, Z.; Yu, M.; Ouyang, L.; Gong, H.; Ding, Y.; Li, P.; Yuan, T.; Zhou, Y.; et al. Effect of availability of HIV self-testing on HIV testing frequency among men who have sex with men attending university in China (UniTest): Protocol of a stepped-wedge randomized controlled trial. BMC Infect. Dis. 2020, 20, 194. [Google Scholar] [CrossRef]
- Pimenoff, V.N.; Felez-Sanchez, M.; Tous, S.; Clavero, O.; Godinez, J.M.; Klaustermeier, J.; Saunier, M.; Molijn, A.; Alemany, L.; Quint, W.; et al. Disagreement in high-grade/low-grade intraepithelial neoplasia and high-risk/low-risk HPV infection: Clinical implications for anal cancer precursor lesions in HIV-positive and HIV-negative MSM. Clin. Microbiol. Infect. 2015, 21, 605–609. [Google Scholar] [CrossRef]
- IARC. Human Papillomaviruses. IARC Monogr. Eval. Carcinog. Risks Hum. 2007, 90, 1–636. [Google Scholar]
- Chow, E.P.; Tucker, J.D.; Wong, F.Y.; Nehl, E.J.; Wang, Y.; Zhuang, X.; Zhang, L. Disparities and risks of sexually transmissible infections among men who have sex with men in China: A meta-analysis and data synthesis. PLoS ONE 2014, 9, e89959. [Google Scholar] [CrossRef]
- Ma, X.; Wang, Q.; Ong, J.J.; Fairley, C.K.; Su, S.; Peng, P.; Jing, J.; Wang, L.; Soe, N.N.; Cheng, F.; et al. Prevalence of human papillomavirus by geographical regions, sexual orientation and HIV status in China: A systematic review and meta-analysis. Sex. Transm. Infect. 2018, 94, 434–442. [Google Scholar] [CrossRef]
- Zhou, Y.; Lin, Y.-F.; Meng, X.; Duan, Q.; Wang, Z.; Yang, B.; Zheng, H.; Li, P.; Li, M.; Lu, Y.; et al. Anal human papillomavirus among men who have sex with men in three metropolitan cities in southern China: Implications for HPV vaccination. Vaccine 2020. [Google Scholar] [CrossRef]
- Daling, J.R.; Madeleine, M.M.; Johnson, L.G.; Schwartz, S.M.; Shera, K.A.; Wurscher, M.A.; Carter, J.J.; Porter, P.L.; Galloway, D.A.; McDougall, J.K. Human papillomavirus, smoking, and sexual practices in the etiology of anal cancer. Cancer 2004, 101, 270–280. [Google Scholar] [CrossRef] [PubMed]
- Mann, L.M.; Llata, E.; Flagg, E.W.; Hong, J.; Asbel, L.; Carlos-Henderson, J.; Kerani, R.P.; Kohn, R.; Pathela, P.; Schumacher, C.; et al. Trends in the Prevalence of Anogenital Warts Among Patients at Sexually Transmitted Disease Clinics-Sexually Transmitted Disease Surveillance Network, United States, 2010-2016. J. Infect. Dis. 2019, 219, 1389–1397. [Google Scholar] [CrossRef] [PubMed]
- Lin, A.; Ong, K.J.; Hobbelen, P.; King, E.; Mesher, D.; Edmunds, W.J.; Sonnenberg, P.; Gilson, R.; Bains, I.; Choi, Y.H.; et al. Impact and Cost-effectiveness of Selective Human Papillomavirus Vaccination of Men Who Have Sex With Men. Clin. Infect. Dis. 2017, 64, 580–588. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Regan, D.G.; Ong, J.J.; Gambhir, M.; Chow, E.P.F.; Zou, H.; Law, M.; Hocking, J.; Fairley, C.K. Targeted human papillomavirus vaccination for young men who have sex with men in Australia yields significant population benefits and is cost-effective. Vaccine 2017, 35, 4923–4929. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Li, M.; Yang, Y.; Zhong, X.; Feng, B.; Xin, H.; Li, Z.; Jin, Q.; Gao, L. Anal HPV/HIV co-infection among Men Who Have Sex with Men: A cross-sectional survey from three cities in China. Sci. Rep. 2016, 6, 21368. [Google Scholar] [CrossRef]
- Ren, X.; Ke, W.; Zheng, H.; Yang, L.; Huang, S.; Qin, X.; Yang, B.; Zou, H. Human Papillomavirus Positivity in the Anal Canal in HIV-Infected and HIV-Uninfected Men Who Have Anal Sex with Men in Guangzhou, China: Implication for Anal Exams and Early Vaccination. Biomed. Res. Int. 2017, 2017, 2641259. [Google Scholar] [CrossRef]
- Zou, H.; Fan, S. Characteristics of men who have sex with men who use smartphone geosocial networking applications and implications for HIV interventions: A systematic review and meta-analysis. Arch. Sex. Behav. 2017, 46, 885–894. [Google Scholar] [CrossRef]
- Davey, G.; De Lian, C.; Higgins, L. The university entrance examination system in China. J. Furth. High. Educ. 2007, 31, 385–396. [Google Scholar] [CrossRef]
- Zhang, X.; Yu, J.; Li, M.; Sun, X.; Han, Q.; Li, M.; Zhou, F.; Li, X.; Yang, Y.; Xiao, D.; et al. Prevalence and related risk behaviors of HIV, syphilis, and anal HPV infection among men who have sex with men from Beijing, China. AIDS Behav. 2013, 17, 1129–1136. [Google Scholar] [CrossRef]
- Gao, L.; Zhou, F.; Li, X.; Yang, Y.; Ruan, Y.; Jin, Q. Anal HPV infection in HIV-positive men who have sex with men from China. PLoS ONE 2010, 5, e15256. [Google Scholar] [CrossRef]
- Zhang, D.Y.; Yin, Y.P.; Feng, T.J.; Hong, F.C.; Jiang, N.; Wang, B.X.; Chen, X.S. HPV infections among MSM in Shenzhen, China. PLoS ONE 2014, 9, e96364. [Google Scholar] [CrossRef]
- Yu, M.H.; Gong, H.; Guo, Y.; Dong, X.Y. Meta-analysis on the positive rate of HIV among MSM with bathhouse as the major venue of sexual practice. Zhonghua Liu Xing Bing Xue Za Zhi 2016, 37, 1152–1158. [Google Scholar] [CrossRef]
- Kennedy, C.E.; Bernard, L.J.; Muessig, K.E.; Konda, K.A.; Akl, E.A.; Lo, Y.R.; Gerbase, A.; O’Reilly, K.R. Serosorting and HIV/STI Infection among HIV-Negative MSM and Transgender People: A Systematic Review and Meta-Analysis to Inform WHO Guidelines. J. Sex. Transm. Dis. 2013, 2013, 583627. [Google Scholar] [CrossRef]
- Golden, M.R.; Stekler, J.; Hughes, J.P.; Wood, R.W. HIV serosorting in men who have sex with men: Is it safe? J. Acquir. Immune Defic. Syndr. 2008, 49, 212–218. [Google Scholar] [CrossRef]
- Sichero, L.; Giuliano, A.R.; Villa, L.L. Human Papillomavirus and Genital Disease in Men: What We Have Learned from the HIM Study. Acta Cytol. 2019, 63, 109–117. [Google Scholar] [CrossRef]
- Arbyn, M.; Smith, S.B.; Temin, S.; Sultana, F.; Castle, P.; Collaboration, S.-S.; Testing, H.P.V. Detecting cervical precancer and reaching underscreened women by using HPV testing on self samples: Updated meta-analyses. BMJ 2018, 363, k4823. [Google Scholar] [CrossRef]
- Lin, C.; Franceschi, S.; Clifford, G.M. Human papillomavirus types from infection to cancer in the anus, according to sex and HIV status: A systematic review and meta-analysis. Lancet Infect. Dis. 2018, 18, 198–206. [Google Scholar] [CrossRef]
- Cuzick, J.; Cadman, L.; Mesher, D.; Austin, J.; Ashdown-Barr, L.; Ho, L.; Terry, G.; Liddle, S.; Wright, C.; Lyons, D.; et al. Comparing the performance of six human papillomavirus tests in a screening population. Br. J. Cancer 2013, 108, 908–913. [Google Scholar] [CrossRef]
- Hybribio. Human Papilloma Virus Typing Test Kit (37 types). Available online: http://www.hybribio.cn/product-view.aspx?id=20 (accessed on 25 March 2020).
 represents the AOR value and its 95% CI, the dot represents the AOR value, and the length of the line represents the 95% CI range.
represents the AOR value and its 95% CI, the dot represents the AOR value, and the length of the line represents the 95% CI range.
 represents the AOR value and its 95% CI, the dot represents the AOR value, and the length of the line represents the 95% CI range.
represents the AOR value and its 95% CI, the dot represents the AOR value, and the length of the line represents the 95% CI range.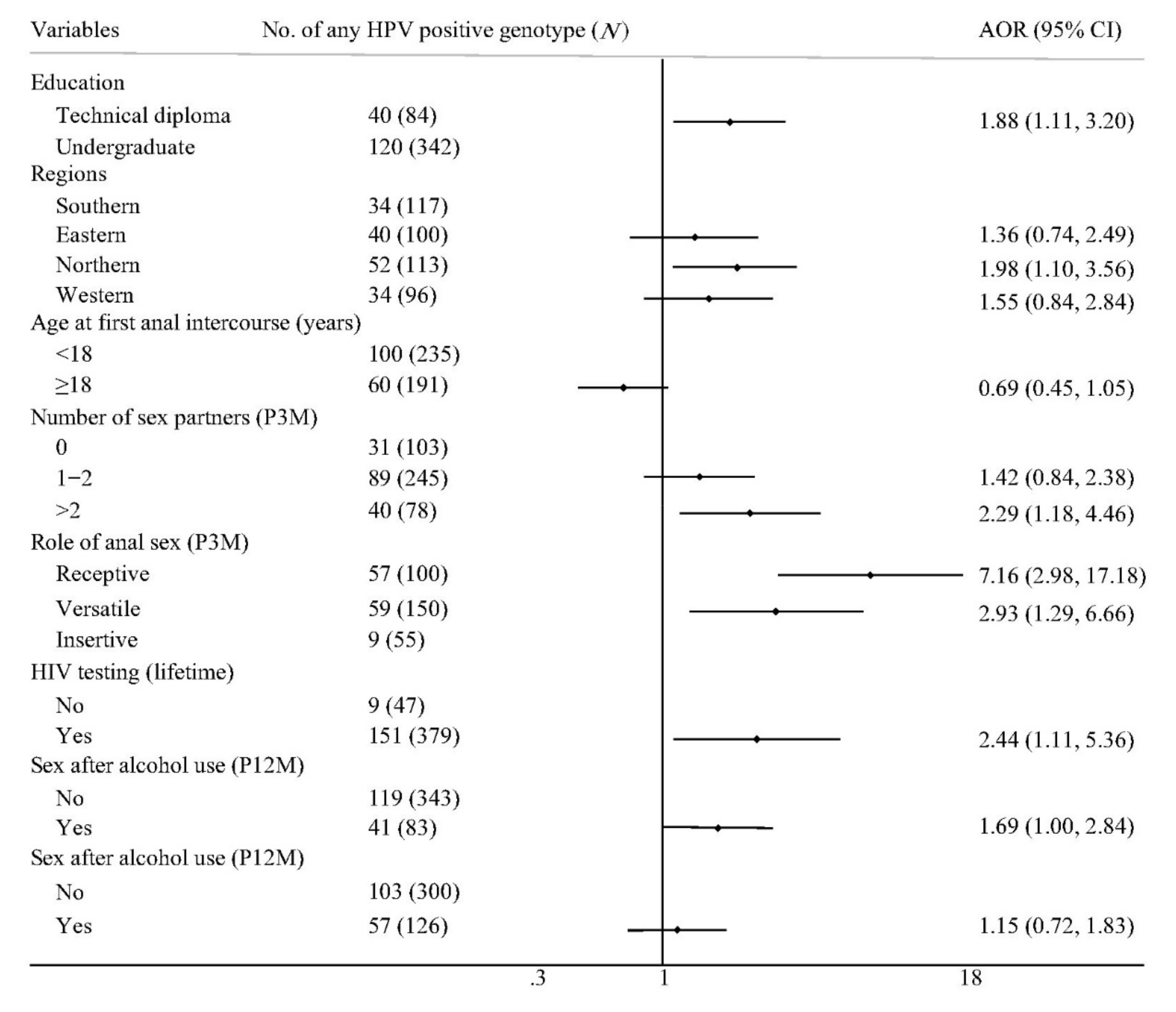
| Variables | n | Any HPV-Positive (n = 160) | Any HPV-Negative (n = 266) | p | ||
|---|---|---|---|---|---|---|
| No. | % | No. | % | |||
| Age (years) | ||||||
| ≤20 | 225 | 78 | 48.8 | 147 | 55.3 | 0.192 |
| >20 | 201 | 82 | 51.3 | 119 | 44.7 | |
| Education | ||||||
| Technical diploma | 84 | 40 | 25.0 | 44 | 16.5 | 0.034 |
| Undergraduate | 342 | 120 | 75.0 | 222 | 83.5 | |
| Academic performance | ||||||
| Average and below | 88 | 33 | 20.6 | 55 | 20.7 | 0.990 |
| Above average | 338 | 127 | 79.4 | 211 | 79.3 | |
| Regions | ||||||
| Southern | 117 | 34 | 21.3 | 83 | 31.2 | 0.058 |
| Eastern | 100 | 40 | 25.0 | 60 | 22.6 | |
| Northern | 113 | 52 | 32.5 | 61 | 22.9 | |
| Western | 96 | 34 | 21.3 | 62 | 23.3 | |
| Sexual orientation | ||||||
| Other | 20 | 6 | 3.8 | 14 | 5.3 | 0.106 |
| Bisexual | 42 | 10 | 6.3 | 32 | 12.0 | |
| Homosexual | 364 | 144 | 90.0 | 220 | 82.7 | |
| Gender of sex partners (n = 414) | ||||||
| Only male | 401 | 155 | 98.1 | 246 | 96.1 | 0.261 |
| Male and female | 13 | 3 | 1.9 | 10 | 3.9 | |
| Age at first anal intercourse (years) | ||||||
| <18 | 235 | 100 | 62.5 | 135 | 50.8 | 0.018 |
| ≥18 | 191 | 60 | 37.5 | 131 | 49.2 | |
| Number of sex partners (P3M) | ||||||
| 0 | 103 | 31 | 19.4 | 72 | 27.1 | 0.012 |
| 1–2 | 245 | 89 | 55.6 | 156 | 58.6 | |
| >2 | 78 | 40 | 25.0 | 38 | 14.3 | |
| Group sex (P3M) | ||||||
| No | 349 | 129 | 80.6 | 220 | 82.7 | 0.589 |
| Yes | 77 | 31 | 19.4 | 46 | 17.3 | |
| Role in anal sex (P3M) (n = 305) | ||||||
| Receptive | 100 | 57 | 45.6 | 43 | 23.9 | <0.001 |
| Versatile | 150 | 59 | 47.2 | 91 | 50.6 | |
| Insertive | 55 | 9 | 7.2 | 46 | 25.6 | |
| Unprotected anal intercourse (P3M) | ||||||
| No | 291 | 103 | 64.4 | 188 | 70.7 | 0.176 |
| Yes | 135 | 57 | 35.6 | 78 | 29.3 | |
| HIV testing (lifetime) | ||||||
| No | 47 | 9 | 5.6 | 38 | 14.3 | 0.006 |
| Yes | 379 | 151 | 94.4 | 228 | 85.7 | |
| HIV status of sex partners (P3M) (n = 196) | ||||||
| Negative | 144 | 51 | 64.6 | 93 | 79.5 | 0.065 |
| Positive | 5 | 3 | 3.8 | 2 | 1.7 | |
| Unknown | 47 | 25 | 31.6 | 22 | 18.8 | |
| Sex after alcohol use (P12M) | ||||||
| No | 343 | 119 | 74.4 | 224 | 84.2 | 0.013 |
| Yes | 83 | 41 | 25.6 | 42 | 15.8 | |
| Recreational drug used in sex (lifetime) | ||||||
| No | 300 | 103 | 64.4 | 197 | 74.1 | 0.034 |
| Yes | 126 | 57 | 35.6 | 69 | 25.9 | |
| HIV status | ||||||
| Negative | 414 | 151 | 94.4 | 263 | 98.9 | 0.012 |
| Positive | 12 | 9 | 5.6 | 3 | 1.1 | |
| Type of Infection | Positive Cases | Prevalence (95% CI) (%) |
|---|---|---|
| Any HPV type | 160 | 37.5 (32.9, 42.2) |
| Any high-risk type | 107 | 25.1 (21.0, 29.3) |
| Any low-risk type | 112 | 26.3 (22.1, 30.5) |
| No. of HPV genotype detections | ||
| Median and range | Median: 2 | Min: 1, Max: 9 |
| 1 type | 79 | 18.5 (14.8, 22.3) |
| 2 types | 44 | 10.3 (7.4, 13.2) |
| 3 types | 18 | 4.2 (2.3, 6.1) |
| 4+ types | 19 | 4.5 (2.5, 6.4) |
| Single infection | ||
| Single high-risk types | 35 | 8.2 (5.6, 10.8) |
| Single low-risk types | 44 | 10.3 (7.4, 13.2) |
| Mixed infection | ||
| Multiple high-risk types | 13 | 3.1 (1.4, 4.7) |
| Multiple low-risk types | 9 | 2.1 (0.7, 3.5) |
| Both high-risk and low-risk types | 59 | 13.8 (10.6, 17.1) |
| High-risk type | ||
| HPV 16 | 37 | 8.7 (6.0, 11.4) |
| HPV 18 | 17 | 4.0 (2.1, 5.9) |
| HPV 31 | 5 | 1.2 (0.1, 2.2) |
| HPV 33 | 7 | 1.6 (0.4, 2.9) |
| HPV 35 | 2 | 0.5 (−0.2, 1.1) |
| HPV 39 | 11 | 2.6 (1.1, 4.1) |
| HPV 45 | 9 | 2.1 (0.7, 3.5) |
| HPV 51 | 16 | 3.8 (1.9, 5.6) |
| HPV 52 | 16 | 3.8 (1.9, 5.6) |
| HPV 56 | 8 | 1.9 (0.6, 3.2) |
| HPV 58 | 9 | 2.1 (0.7, 3.5) |
| HPV 59 | 1 | 0.2 (−0.2, 0.7) |
| HPV 68 | 17 | 4.0 (2.1, 5.9) |
| Low-risk type | ||
| HPV 6 | 38 | 8.9 (6.2, 11.6) |
| HPV 11 | 32 | 7.5 (5.0, 10.0) |
| HPV 40 | 14 | 3.3 (1.6, 5.0) |
| HPV 42 | 8 | 1.9 (0.6, 3.2) |
| HPV 43 | 5 | 1.2 (0.1, 2.2) |
| HPV 44 | 3 | 0.7 (−0.1, 1.5) |
| HPV 53 | 7 | 1.6 (0.4, 2.9) |
| HPV 54 | 6 | 1.4 (0.3, 2.5) |
| HPV 55 | 3 | 0.7 (−0.1, 1.5) |
| HPV 61 | 10 | 2.3 (0.9, 3.8) |
| HPV 66 | 3 | 0.7 (−0.1, 1.5) |
| HPV 67 | 10 | 2.3 (0.9, 3.8) |
| HPV 69 | 1 | 0.2 (−0.2, 0.7) |
| HPV 70 | 1 | 0.2 (−0.2, 0.7) |
| HPV 71 | 1 | 0.2 (−0.2, 0.7) |
| HPV 72 | 2 | 0.5 (−0.2, 1.1) |
| HPV 73 | 5 | 1.2 (0.1, 2.2) |
| HPV 81 | 8 | 1.9 (0.6, 3.2) |
| HPV 82 | 5 | 1.2 (0.1, 2.2) |
| HPV 84 | 6 | 1.4 (0.3, 2.5) |
| Vaccine-preventable types | ||
| 9vHPV | 127 | 29.8 (25.5, 34.2) |
| 4vHPV | 105 | 24.6 (20.5, 28.8) |
| HPV 6/11 | 67 | 15.7 (12.3, 19.2) |
| HPV 16/18 | 49 | 11.5 (8.5, 14.5) |
| No. of vaccine-preventable type detections | ||
| Median and range | Median: 1 | Min: 1, Max: 5 |
| 1 type | 95 | 22.3 (18.3, 26.3) |
| 2 types | 25 | 5.9 (3.6, 8.1) |
| 3 types | 4 | 0.9 (0, 1.9) |
| 4+ types | 3 | 0.7 (−0.1, 1.5) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, S.; Li, P.; Ouyang, L.; Yuan, T.; Gong, H.; Ding, Y.; Luo, Z.; Wu, G.; Yu, M.; Zou, H. Anal Human Papillomavirus Infection among MSM Attending University in China: Implications for Vaccination. Vaccines 2020, 8, 175. https://doi.org/10.3390/vaccines8020175
Fan S, Li P, Ouyang L, Yuan T, Gong H, Ding Y, Luo Z, Wu G, Yu M, Zou H. Anal Human Papillomavirus Infection among MSM Attending University in China: Implications for Vaccination. Vaccines. 2020; 8(2):175. https://doi.org/10.3390/vaccines8020175
Chicago/Turabian StyleFan, Song, Peiyang Li, Lin Ouyang, Tanwei Yuan, Hui Gong, Yi Ding, Zhenzhou Luo, Guohui Wu, Maohe Yu, and Huachun Zou. 2020. "Anal Human Papillomavirus Infection among MSM Attending University in China: Implications for Vaccination" Vaccines 8, no. 2: 175. https://doi.org/10.3390/vaccines8020175
APA StyleFan, S., Li, P., Ouyang, L., Yuan, T., Gong, H., Ding, Y., Luo, Z., Wu, G., Yu, M., & Zou, H. (2020). Anal Human Papillomavirus Infection among MSM Attending University in China: Implications for Vaccination. Vaccines, 8(2), 175. https://doi.org/10.3390/vaccines8020175





