Abstract
Background/Objectives: The anterior cerebral artery (ACA), as one of the terminal branches of the internal carotid artery, supplies the medial and superior portions of the frontal lobes as well as the anterior portions of the parietal lobes. The present meta-analysis aims to consolidate current knowledge regarding the anatomy and variations in the ACA, providing a comprehensive resource for physicians. Methods: To conduct this meta-analysis, we systematically searched prominent online medical databases, including PubMed, Scopus, Embase, Web of Science, Cochrane Library, and Google Scholar, to identify all studies that investigated the anatomy of the ACA. Results: The results of the present study were based on a total of 73 articles. In the aforementioned studies, a total of 24,015 patients were evaluated. The pooled mean total length of the A1 segment of the ACA, based on all evaluated cases, was 14.47 mm (SE = 0.28). The pooled mean total diameter of the A1 segment measured 2.00 mm on average (SE = 0.07). The overall pooled prevalence of the median ACA was 2.65% (95% CI: 1.57–3.99%). Conclusions: This systematic review and meta-analysis provide valuable insights into the anatomy and variations in the ACA. The current data may support clinicians and neurosurgeons in the management of cerebrovascular diseases and associated procedures, potentially enhancing procedural safety and therapeutic outcomes.
1. Introduction
The anterior cerebral artery (ACA) originates from the terminal bifurcation of the internal carotid artery and primarily supplies the medial and superior regions of the frontal lobes as well as the anterior part of the parietal lobe. It also provides arterial supply to parts of the corpus callosum and to deep cerebral structures, such as the basal ganglia []. From its origin, the ACA runs rostrally and medially toward the longitudinal cerebral fissure, where it connects with its counterpart through the anterior communicating artery. It continues to follow the path of the longitudinal cerebral fissure, curving around the genu of the corpus callosum, and then extends posteriorly along its body. As the ACA courses anterior to the genu of the corpus callosum, it typically bifurcates into its two terminal branches: the pericallosal and callosomarginal arteries. Near the splenium of the corpus callosum, these branches form anastomoses with the distal branches of the middle and posterior cerebral arteries [,,]. Considering the distinct topography along its trajectory, the ACA is conventionally divided into five segments (A1–A5; see Figure 1). The precommunicating segment (A1) extends from the bifurcation of the internal carotid artery to the origin of the anterior communicating artery. This segment usually courses superior to the optic chiasm and optic nerves and inferior to the anterior perforated substance. The infracallosal segment (A2), also referred to as the vertical or postcommunicating segment, curves around the rostrum of the corpus callosum, running from the anterior communicating artery to the genu of the corpus callosum as far as the origin of the callosomarginal artery. The precallosal segment (A3) originates at the callosomarginal artery, wraps around the genu of the corpus callosum, and then turns posteriorly to ascend over the rostral portion of the corpus callosum body. The supracallosal segment (A4) travels along the dorsal surface of the corpus callosum anterior to the coronal suture, whereas the postcallosal segment (A5) extends posteriorly above the corpus callosum beyond the coronal suture []. Numerous variants of the ACA have been reported, particularly concerning its course and blood supply territory. Among the most frequently described are the median ACA (MedACA), the bihemispheric ACA (BihemACA), and the azygos ACA (AzACA) []. AzACA results from fusion of the right and left A2 segments into a single A2 trunk. Although uncommon, this configuration has been documented in several studies [,]. A BihemACA occurs when one of the A2 segments is hypoplastic or terminates early, causing the contralateral ACA to supply both hemispheres. Additionally, a MedACA refers to a third branch that supplies the medial surface of one or both hemispheres and can originate from the anterior communicating artery or the A1/A2 segments []. Adequate knowledge of the anatomy and variations in the ACA is important across clinical and neurosurgical practice, especially during the diagnosis of strokes, endovascular procedures, and interhemispheric surgeries [,,,]. Therefore, the present meta-analysis aims to consolidate current knowledge regarding the anatomy and variations in the ACA, providing a comprehensive resource for physicians. By synthesizing data from multiple studies, this study offers insights that may enhance surgical planning, improve clinical decision-making, and ultimately contribute to better outcomes in cerebrovascular interventions.
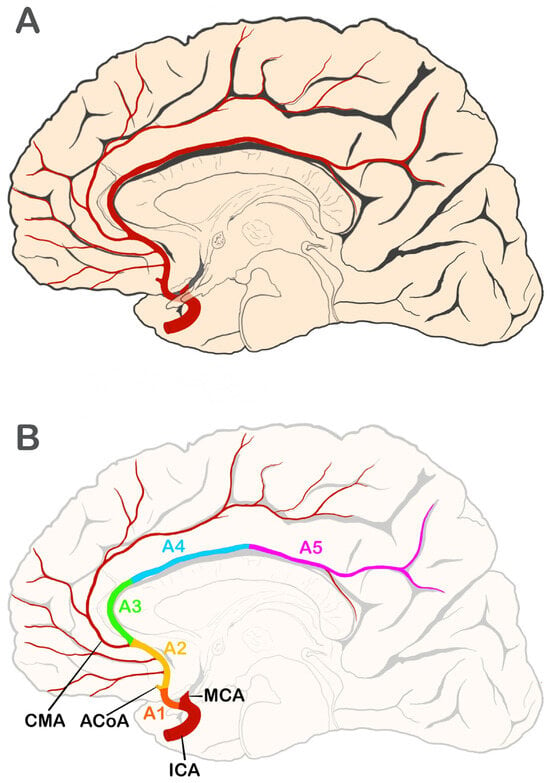
Figure 1.
Anatomy and segments of the anterior cerebral artery (ACA). (A) Illustration showing general topographical relationships—medial view of the right hemisphere. (B) Schematic representation of ACA segments. ACoA—anterior communicating artery; CMA—callosomarginal artery; ICA—internal carotid artery; MCA—middle cerebral artery. ACA segments: A1—horizontal or precommunicating segment; A2—vertical, postcommunicating or infracallosal segment; A3—precallosal segment; A4—supracallosal segment; A5—postcallosal segment. Prepared by G. Wysiadecki.
2. Materials and Methods
2.1. Search Strategy
To conduct this meta-analysis, we systematically searched prominent online medical databases, including PubMed, Scopus, Embase, Web of Science, Cochrane Library, and Google Scholar, to identify all studies that investigated the anatomy of the ACA. The comprehensive search was carried out in three distinct stages. In the first step, the following search terms were used in all databases: (anterior cerebral artery) AND ((anatomy) OR (topography) OR (morphology) OR (variation) OR (variant) OR (pattern) OR (branches) OR (origin) OR (diameter) OR (length)). No restrictions regarding date, language, article type, or text availability were applied. In the second step, the databases were searched again using another set of search phrases: (a) (anterior cerebral artery [Title/Abstract]) AND (anatomy [Title/Abstract]); (b) (anterior cerebral artery [Title/Abstract]) AND (topography [Title/Abstract]); (c) (anterior cerebral artery [Title/Abstract]) AND (morphology [Title/Abstract]); (d) (anterior cerebral artery [Title/Abstract]) AND (variations [Title/Abstract]). Each phrase was evaluated to determine its dependence on grammatical variations, and adjustments were made to tailor it to the specific requirements of each database. In the third stage, a manual search was conducted through the reference lists of the initially identified studies. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed throughout the study. To ensure the highest quality of the findings, the Critical Appraisal Tool for Anatomical Meta-Analyses (CATAM) and the Anatomical Quality Assessment (AQUA) tools were used to evaluate the included studies [,,].
2.2. Eligibility Assessment
A total of 11,282 articles were initially evaluated by two independent researchers. Of these, 8569 records were excluded for being irrelevant to the studied topic. Articles such as case reports, case series, conference reports, reviews, letters to the editor, and studies providing incomplete or irrelevant data were also excluded. The inclusion criteria encompassed original studies containing retrievable numerical data pertaining to the origin, diameter, length, or any other information relevant to the comprehensive anatomy, morphology, topography, or variations in the ACA. Ultimately, 73 studies were included in the present review [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,]. The flow chart presenting the study inclusion process is shown in Figure 2.
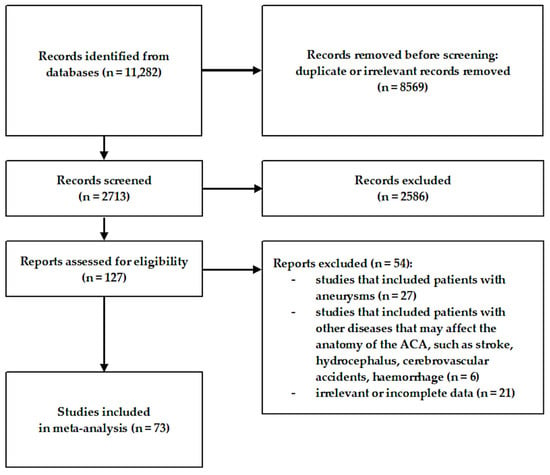
Figure 2.
Flow diagram presenting the process of collecting data included in this meta-analysis.
2.3. Data Extraction
Data from eligible articles were extracted by two independent researchers. Qualitative data, such as methodology, year of publication, and country of origin, were assessed. In addition, quantitative data about the anatomy of the ACA were extracted. Any discrepancies between the reviewers were resolved through contact with the original study authors whenever possible or by consensus with a third reviewer.
2.4. Statistical Analysis
To carry out the meta-analyses, MetaXL (version 5.3; EpiGear International Pty Ltd., Wilston, QLD, Australia), alongside Comprehensive Meta-analysis software (version 4.0; Biostat, Inc., Englewood, NJ, USA), were applied. All statistical analyses were conducted using a random-effects model. Heterogeneity among the included studies was evaluated using the I2 statistic [,]. Statistical significance was assessed based on p-values and confidence intervals, with results considered significant when p < 0.05. When confidence intervals overlapped, the differences were treated as statistically nonsignificant. Interpretation of I2 values followed standard thresholds: 0–40% suggesting low or negligible heterogeneity, 30–60% indicating moderate heterogeneity, 50–90% reflecting substantial heterogeneity, and 75–100% representing considerable heterogeneity [].
3. Results
3.1. General Characteristics
The results of the present study were based on a total of 73 articles. In these studies, a total of 24,015 patients were evaluated. The meta-analysis was performed only on data that met the required statistical criteria and were eligible to be analyzed without potential bias. Data from the remaining articles are described below. Most of the included articles were conducted in Asia (n = 24) and Europe (n = 20). The majority of the studies (n = 48) were based on cadaveric dissections, while the remaining (n = 26) were based on radiological images. Despite methodological differences, no statistically significant differences (p > 0.05) were found between the results of the radiological and cadaveric studies in the categories included in the meta-analysis. The characteristics of the included studies are presented in Table 1.

Table 1.
Characteristics of included studies. CTA—Computed Tomography Angiography. MRI—Magnetic Resonance Imaging. MRA—Magnetic Resonance Angiography.
Table 1.
Characteristics of included studies. CTA—Computed Tomography Angiography. MRI—Magnetic Resonance Imaging. MRA—Magnetic Resonance Angiography.
| First Author | Year | Continent | Country | Method |
|---|---|---|---|---|
| Madkour, N.A.A. [] | 2023 | Africa | Egypt | MRA |
| Luckrajh, J.S. et al. [] | 2022 | Africa | South Africa | CTA |
| Riveros, A. et al. [] | 2022 | South America | Chile | Cadavers |
| Giotta Lucifero, A. et al. [] | 2021 | Europe | Italy | Cadavers |
| Beyhan, M. et al. [] | 2020 | Asia | Turkey | CTA + MRA + MRI + DSA |
| Quijano Blanco, Y. & García Orjuela, D. [] | 2020 | South America | Colombia | Cadavers |
| Sharma, S. et al. [] | 2020 | Asia | India | CTA |
| Zaki, S.M. et al. [] | 2019 | Africa | Egypt | MRA |
| Thenmozhi, A. et al. [] | 2019 | Asia | India | Cadavers |
| Shatri, J. et al. [] | 2019 | Europe | Germany | MRA |
| Canaz, H. et al. [] | 2018 | Europe | Turkey | Cadavers |
| Jiménez-Sosa, M.S. et al. [] | 2017 | South America | Mexico | CT |
| Ozturk, S. et al. [] | 2017 | Europe | Turkey | MRI |
| Yu, L-H. et al. [] | 2017 | Asia | China | Cadavers |
| Shatri, J. et al. [] | 2017 | Europe | Germany | MRA |
| Cilliers, K. & Page, B.J. [] | 2017 | Africa | South Africa | Cadavers |
| Cilliers, K. & Page, B.J. [] | 2016 | Africa | South Africa | Cadavers |
| Karatas, A. et al. [] | 2016 | Europe | Turkey | Cadavers |
| Shinde, S. & Shroff, G. [] | 2016 | Asia | India | Cadavers |
| Aggarwal, N. et al. [] | 2016 | Asia | India | MRA |
| Arat, Y. et al. [] | 2015 | Asia | Turkey | CTA |
| d’Avella, E. et al. [] | 2015 | Europe | Spain | Cadavers + CT + MR |
| Klimek-Piotrowska, W. et al. [] | 2015 | Europe | Poland | Cadavers |
| Karatas, A. et al. [] | 2015 | Europe | Turkey | CTA |
| Gunnal, S.A. et al. [] | 2013 | Asia | India | Cadavers |
| Flores, B.C. et al. [] | 2013 | North America | USA | CTA |
| Hamidi, C. et al. [] | 2013 | Asia | Turkey | CTA |
| Kedia, S. et al. [] | 2013 | Asia | India | Cadavers |
| Stefani, M.A. et al. [] | 2013 | South America | Brasil | MRA |
| Aggarwal, N. et al. [] | 2012 | Asia | India | MRA |
| Swetha, B. [] | 2012 | Asia | India | Cadavers |
| Shi, W.-Y. et al. [] | 2014 | Asia | China | MRI |
| Nordon, D. & Rodrigues Junior, O. [] | 2012 | South America | Brasil | Cadavers |
| Maaly, M.A. & Ismail, A.A. [] | 2011 | Africa | Egypt | MRA |
| Żurada, A. & Gielecki, J. [] | 2010 | Europe | Poland | CT |
| Ozdogmus, O. et al. [] | 2008 | Europe | Turkey | Cadavers |
| Kahilogullari, G. et al. [] | 2008 | Asia | Turkey | Cadavers |
| Kapoor, K. et al. [] | 2008 | Asia | India | Cadavers |
| Lehecka, M. et al. [] | 2008 | Europe | Finland | CTA |
| Saidi, H. et al. [] | 2008 | Africa | Kenya | Cadavers |
| Mandiola, E. et al. [] | 2007 | South America | Chile | Cadavers |
| Tao, X. & Yu, X.J. [] | 2006 | Asia | China | Cadavers |
| Forero, P. [] | 2006 | South America | Colombia | Cadavers |
| Ugur, H.C. et al. [] | 2006 | Asia | Turkey | Cadavers |
| Pai, S.B. et al. [] | 2005 | Asia | India | Cadavers |
| Ugur, H.C. et al. [] | 2005 | Asia | Turkey | Cadavers |
| Paul, S. & Mishra, S. [] | 2004 | Asia | India | Cadavers |
| Kulenović, A. et al. [] | 2003 | Europe | Croatia | Cadavers |
| Avci, E. et al. [] | 2001 | North America | USA | Cadavers |
| Stefani, M.A. et al. [] | 2000 | South America | Brazil | Cadavers |
| Serizawa, T. et al. [] | 1997 | Asia | Japan | Cadavers |
| Macchi, C. et al. [] | 1996 | Europe | Italy | MRA |
| Piepgras, A. et al. [] | 1993 | Europe | Germany | Cadavers |
| Sanders, W.P. et al. [] | 1993 | North America | USA | Agniograms |
| van der Zwan, A. et al. [] | 1992 | North America | USA | Cadavers |
| Krabbe-Hartkamp, M.J. et al. [] | 1988 | Europe | The Netherlands | MRA |
| Gomes, F.B. et al. [] | 1986 | North America | USA | Cadavers |
| Orlandini, G.E. & Ruggiero, C. [] | 1985 | Europe | Italy | Cadavers |
| Kamath, S. [] | 1980 | Asia | India | Cadavers |
| Huber, P. & Braun, J. [] | 1980 | Europe | Switzerland | Angiograms |
| Perlmutter, D. & Rhoton, A.L. [] | 1978 | North America | USA | Cadavers |
| Tulleken, C.A.F. [] | 1978 | Europe | The Netherlands | Cadavers |
| Ozaki, T. et al. [] | 1977 | Asia | Japan | Cadavers |
| Perlmutter, D. & Rhoton, A.L. [] | 1976 | North America | USA | Cadavers |
| Dunker, R.O. & Harris, A.B. [] | 1976 | North America | USA | Cadavers |
| Ring, B.A. & Waddington, M.M. [] | 1968 | North America | USA | Cadavers |
| Wollschlaeger, G. et al. [] | 1967 | South America | Colombia | Angiograms |
| Lemay, M. & Gooding, C.A. [] | 1966 | North America | USA | Arteriograms |
| Fisher, C. [] | 1965 | North America | USA | Cadavers |
| Jain, K.K. [] | 1964 | Asia | India | Cadavers |
| Murray, K.D. [] | 1964 | Australia | South Australia | Cadavers |
| Baptista, A.G. [] | 1963 | South America | Brazil | Cadavers |
| Windle, B.C. [] | 1888 | Europe | England | Cadavers |
3.2. Length of the A1 Segment of the ACA
The pooled mean total length of the A1 segment of the ACA, based on all evaluated cases, was 14.47 mm (SE = 0.28). Based solely on cadaveric studies, the pooled mean length was 14.61 mm (SE = 0.64), while for radiological images, it was 14.11 mm (SE = 0.20). The complete results of this part of the meta-analysis, along with remaining data from the literature not included in the analysis, are presented in Table 2.

Table 2.
Statistical results of this meta-analysis regarding the length of the A1 segment of the Anterior Cerebral Artery (ACA). (*)—The results of this part of the analysis were based on the following studies: Kamath, S. []; Gomes, F.B. et al. []; Tao, X. & Yu, X.J. []; Mandiola, E. et al. []; Aggarwal, N. et al. []; d’Avella, E. et al. []; Karatas, A. et al. []; Karatas, A. [et al. []; Yu, L.-H. et al. []; Canaz, H. et al. []; Shatri, J. et al. []; Sharma, S. et al. []; Luckrajh, J.S. et al. []; Riveros, A. et al. []. (**)—The rest of the results were gathered from the literature, but not included in the analysis due to insufficient data or bias prevention.
Table 2.
Statistical results of this meta-analysis regarding the length of the A1 segment of the Anterior Cerebral Artery (ACA). (*)—The results of this part of the analysis were based on the following studies: Kamath, S. []; Gomes, F.B. et al. []; Tao, X. & Yu, X.J. []; Mandiola, E. et al. []; Aggarwal, N. et al. []; d’Avella, E. et al. []; Karatas, A. et al. []; Karatas, A. [et al. []; Yu, L.-H. et al. []; Canaz, H. et al. []; Shatri, J. et al. []; Sharma, S. et al. []; Luckrajh, J.S. et al. []; Riveros, A. et al. []. (**)—The rest of the results were gathered from the literature, but not included in the analysis due to insufficient data or bias prevention.
| Category | Pooled Mean | Standard Error | Variance | Lower Limit | Upper Limit | Z-Value | p-Value |
|---|---|---|---|---|---|---|---|
| A1 Segment Length [mm] * | |||||||
| Total Length [Overall] | 14.47 | 0.28 | 0.08 | 13.92 | 15.03 | 51.44 | 0.00 |
| Total Length [Cadavers] | 14.61 | 0.64 | 0.41 | 13.36 | 15.87 | 22.84 | 0.00 |
| Total Length [Radiological Studies] | 14.11 | 0.20 | 0.04 | 13.71 | 14.50 | 70.33 | 0.00 |
| Right ACA Length [Overall] | 14.49 | 0.26 | 0.07 | 13.98 | 15.00 | 55.72 | 0.00 |
| Right ACA Length [Cadavers] | 14.46 | 0.40 | 0.16 | 13.68 | 15.25 | 36.04 | 0.00 |
| Right ACA Length [Radiological Studies] | 14.68 | 0.46 | 0.21 | 13.77 | 15.58 | 31.71 | 0.00 |
| Left ACA Length [Overall] | 14.19 | 0.27 | 0.07 | 13.66 | 14.71 | 52.80 | 0.00 |
| Left ACA Length [Cadavers] | 14.08 | 0.34 | 0.11 | 13.42 | 14.74 | 41.92 | 0.00 |
| Left ACA Length [Radiological Studies] | 14.61 | 0.59 | 0.35 | 13.45 | 15.77 | 24.66 | 0.00 |
| Other Results from the Literature ** | |||||||
| Author | Data | ||||||
| Total Length [mm] | |||||||
| Giotta Lucifero, A. et al. [] | Mean = 12.7 | ||||||
| Shatri, J. et al. [] | Mean = 13.96; Minimum = 1.4 | ||||||
| Avci, E. et al. [] | Minimum = 7.07; Maximum = 15.5 | ||||||
| Perlmutter, D. & Rhoton, A.L. [] | Mean = 13; Minimum = 7; Maximum = 18 | ||||||
| Perlmutter, D. & Rhoton, A.L. [] | Mean = 12.7; Minimum = 7.2; Maximum = 18 | ||||||
| Dunker, R.O. & Harris, A.B. [] | Median = 13 | ||||||
| Right ACA Length [mm] | |||||||
| Thenmozhi, A., 2019 [] | Mean = 14.44 | ||||||
| Shinde, S. & Shroff, G. [] | Mean = 12 | ||||||
| Kedia, S. et al. [] | Mean = 12.09 | ||||||
| Pai, S.B. et al. [] | Mean = 14.6 | ||||||
| Orlandini, G.E. & Ruggiero, C. [] | Mean = 14.1 | ||||||
| Murray, K.D. [] | Mean = 13.2 | ||||||
| Left ACA Length [mm] | |||||||
| Thenmozhi, A., 2019 [] | Mean = 13.6 | ||||||
| Shinde, S. & Shroff, G. [] | Mean = 13 | ||||||
| Kedia, S. et al. [] | Mean = 12 | ||||||
| Pai, S.B. et al. [] | Mean = 14.5 | ||||||
| Orlandini, G.E. & Ruggiero, C. [] | Mean = 13.6 | ||||||
| Murray, K.D. [] | Mean = 12.9 | ||||||
3.3. Diameter of the A1 Segment of the ACA
The pooled mean diameter of the A1 segment of the ACA, based on all evaluated cases, was 2.00 mm (SE = 0.07). In cadaveric studies, the pooled mean diameter was 1.86 mm (SE = 0.15), while in radiological studies, it was 2.12 mm (SE = 0.09). The complete results of this part of the meta-analysis, together with additional data from the literature, are presented in Table 3.

Table 3.
Statistical results of this meta-analysis regarding the diameter of the A1 segment of the Anterior Cerebral Artery (ACA). (*)—The results of this part of the analysis were based on the following studies: Kamath, S. []; Gomes, F.B. et al. []; Piepgras, A. et al. []; Stefani, M.A. et al. []; Tao, X. & Yu, X.J. []; Mandiola, E. et al. []; Ozdogmus, O. et al. []; Maaly, M.A. & Ismail, A.A. []; Shi, W.-Y. et al. []; Flores, B.C. et al. []; Stefani, M.A. et al. []; Arat, Y. et al. []; Klimek-Piotrowska, W. et al. []; Karatas, A. et al. []; Karatas, A. et al. []; Aggarwal, N. et al. []; Jiménez-Sosa, M.S. et al. []; Shatri, J. et al. []; Canaz, H. et al. []; Shatri, J. et al. []; Sharma, S. et al. []; Zaki, S.M. et al. []; Riveros, A. et al. []; Luckrajh, J.S. et al. []. (**)—The rest of the results were gathered from the literature, but not included in the analysis due to insufficient data or bias prevention.
Table 3.
Statistical results of this meta-analysis regarding the diameter of the A1 segment of the Anterior Cerebral Artery (ACA). (*)—The results of this part of the analysis were based on the following studies: Kamath, S. []; Gomes, F.B. et al. []; Piepgras, A. et al. []; Stefani, M.A. et al. []; Tao, X. & Yu, X.J. []; Mandiola, E. et al. []; Ozdogmus, O. et al. []; Maaly, M.A. & Ismail, A.A. []; Shi, W.-Y. et al. []; Flores, B.C. et al. []; Stefani, M.A. et al. []; Arat, Y. et al. []; Klimek-Piotrowska, W. et al. []; Karatas, A. et al. []; Karatas, A. et al. []; Aggarwal, N. et al. []; Jiménez-Sosa, M.S. et al. []; Shatri, J. et al. []; Canaz, H. et al. []; Shatri, J. et al. []; Sharma, S. et al. []; Zaki, S.M. et al. []; Riveros, A. et al. []; Luckrajh, J.S. et al. []. (**)—The rest of the results were gathered from the literature, but not included in the analysis due to insufficient data or bias prevention.
| Category | Pooled Mean | Standard Error | Variance | Lower Limit | Upper Limit | Z-Value | p-Value |
|---|---|---|---|---|---|---|---|
| A1 Segment Diameter [mm] * | |||||||
| Total Diameter [Overall] | 2.00 | 0.07 | 0.01 | 1.86 | 2.14 | 27.58 | 0.00 |
| Total Diameter [Cadavers] | 1.86 | 0.15 | 0.02 | 1.57 | 2.15 | 12.55 | 0.00 |
| Total Diameter [Radiological Studies] | 2.12 | 0.09 | 0.01 | 1.95 | 2.29 | 24.28 | 0.00 |
| Right ACA Diameter [Overall] | 2.04 | 0.05 | 0.00 | 1.94 | 2.13 | 44.17 | 0.00 |
| Right ACA Diameter [Cadavers] | 2.00 | 0.10 | 0.01 | 1.80 | 2.21 | 19.43 | 0.00 |
| Right ACA Diameter [Radiological Studies] | 2.09 | 0.05 | 0.00 | 1.99 | 2.19 | 40.30 | 0.00 |
| Left ACA Diameter [Overall] | 2.17 | 0.06 | 0.00 | 2.06 | 2.28 | 38.66 | 0.00 |
| Left ACA Diameter [Cadavers] | 2.11 | 0.11 | 0.01 | 1.88 | 2.33 | 18.36 | 0.00 |
| Left ACA Diameter [Radiological Studies] | 2.25 | 0.07 | 0.01 | 2.11 | 2.39 | 31.61 | 0.00 |
| Other Results from the Literature ** | |||||||
| Author | Data | ||||||
| Total Diameter [mm] | |||||||
| Giotta Lucifero, A. et al. [] | Mean = 2.5 | ||||||
| Krabbe-Hartkamp, M.J. et al. [] | Mean = 2.2 | ||||||
| Perlmutter, D. & Rhoton, A.L. [] | Mean = 2.6 | ||||||
| Right ACA Diameter [mm] | |||||||
| Quijano Blanco, Y. & García Orjuela, D. [] | Mean = 2.29 | ||||||
| Shinde, S. & Shroff, G. [] | Mean = 2.1 | ||||||
| Kedia, S. et al. [] | Mean = 2.32 | ||||||
| Forero, P, 2006 [] | Mean = 2.21 | ||||||
| Pai, S.B. et al. [] | Mean = 2.8 | ||||||
| Avci, E. et al. [] | Mean = 1.9 | ||||||
| Krabbe-Hartkamp, M.J. et al. [] | Mean = 2.3 | ||||||
| Left ACA Diameter [mm] | |||||||
| Quijano Blanco, Y. & García Orjuela, D. [] | Mean = 2.33 | ||||||
| Shinde, S. & Shroff, G. [] | Mean = 2.4 | ||||||
| Kedia, S. et al. [] | Mean = 2.36 | ||||||
| Forero, P, 2006 [] | Mean = 1.16 | ||||||
| Pai, S.B. et al. [] | Mean = 2.9 | ||||||
| Avci, E. et al. [] | Mean = 2.1 | ||||||
| Krabbe-Hartkamp, M.J. et al. [] | Mean = 2.2 | ||||||
3.4. Length of the A2 Segment of the ACA
The pooled mean length of the right A2 segment of the ACA, based solely on radiological studies, was 18.39 mm (SE = 6.31), while the corresponding value for the left ACA was 18.34 mm (SE = 6.72). Reported values in the literature for the total length of the A2 segment range from 4.42 mm to 69.63 mm. Full results of this part of the meta-analysis, along with additional literature data, are presented in Table 4.

Table 4.
Statistical results of this meta-analysis regarding the length of the A2 segment of the Anterior Cerebral Artery (ACA). (*)—The results of this part of the analysis were based on the following studies: Luckrajh, J.S. et al. []; Żurada, A. & Gielecki, J. [] (**)—The rest of the results were gathered from the literature, but not included in the analysis due to insufficient data or bias prevention.
Table 4.
Statistical results of this meta-analysis regarding the length of the A2 segment of the Anterior Cerebral Artery (ACA). (*)—The results of this part of the analysis were based on the following studies: Luckrajh, J.S. et al. []; Żurada, A. & Gielecki, J. [] (**)—The rest of the results were gathered from the literature, but not included in the analysis due to insufficient data or bias prevention.
| Category | Pooled Mean | Standard Error | Variance | Lower Limit | Upper Limit | Z-Value | p-Value |
|---|---|---|---|---|---|---|---|
| A2 Segment Length [mm] * | |||||||
| Right ACA Length [Radiological Studies] | 18.39 | 6.31 | 39.88 | 6.02 | 30.77 | 2.91 | 0.00 |
| Left ACA Length [Radiological Studies] | 18.34 | 6.72 | 45.16 | 5.17 | 31.51 | 2.73 | 0.01 |
| Other Results from the Literature ** | |||||||
| Author | Data | ||||||
| Total Length [mm] | |||||||
| Quijano Blanco, Y. & García Orjuela, D. [] | Mean = 69.63 | ||||||
| Yu, L.-H. et al. [] | Mean = 4.42; Standard Deviation = 1.78 | ||||||
| d’Avella, E. et al. [] | Mean = 7; Standard Deviation = 1 | ||||||
| Żurada, A. & Gielecki, J. [] | Mean = 11.83; Standard Deviation = 4.89 | ||||||
| Perlmutter, D. & Rhoton, A.L. [] | Mean = 28 | ||||||
| Right ACA Length [mm] | |||||||
| Canaz, H. et al. [] | Mean = 18.83; Standard Deviation = 3.18 | ||||||
| Cilliers, K. & Page, B.J. [] | Mean = 19.1 | ||||||
| Swetha, B. [] | Mean = 38.89 | ||||||
| Left ACA Length [mm] | |||||||
| Canaz, H. et al. [] | Mean = 18.73; Standard Deviation = 3.02 | ||||||
| Cilliers, K. & Page, B.J. [] | Mean = 19.5 | ||||||
| Swetha, B. [] | Mean = 41.01 | ||||||
3.5. Diameter of the A2 Segment of the ACA
The pooled mean diameter of the A2 segment of the ACA, based solely on radiological studies, was 1.76 mm (SE = 0.07). The pooled mean diameters of the right and left A2 segments, based on all evaluated cases, were 1.87 mm (SE = 0.08) and 1.87 mm (SE = 0.07), respectively. Based on cadaveric studies alone, the pooled mean diameter was 2.16 mm (SE = 0.32) for the right ACA and 2.11 mm (SE = 0.28) for the left ACA. The full results of this part of the meta-analysis, along with other literature data, are presented in Table 5.

Table 5.
Statistical results of this meta-analysis regarding the diameter of the A2 segment of the Anterior Cerebral Artery (ACA). (*)—The results of this part of the analysis were based on the following studies: Gomes, F.B. et al. []; Żurada, A. & Gielecki, J. []; Flores, B.C. et al. []; Jiménez-Sosa, M.S. et al. []; Canaz, H. et al. []; Luckrajh, J.S. et al. []. (**)—The rest of the results were gathered from the literature, but not included in the analysis due to insufficient data or bias prevention.
Table 5.
Statistical results of this meta-analysis regarding the diameter of the A2 segment of the Anterior Cerebral Artery (ACA). (*)—The results of this part of the analysis were based on the following studies: Gomes, F.B. et al. []; Żurada, A. & Gielecki, J. []; Flores, B.C. et al. []; Jiménez-Sosa, M.S. et al. []; Canaz, H. et al. []; Luckrajh, J.S. et al. []. (**)—The rest of the results were gathered from the literature, but not included in the analysis due to insufficient data or bias prevention.
| Category | Pooled Mean | Standard Error | Variance | Lower Limit | Upper Limit | Z-Value | p-Value |
|---|---|---|---|---|---|---|---|
| A2 Segment Diameter [mm] * | |||||||
| Total Diameter [Radiological Studies] | 1.76 | 0.07 | 0.00 | 1.63 | 1.89 | 26.74 | 0.00 |
| Right ACA Diameter [Overall] | 1.87 | 0.08 | 0.01 | 1.70 | 2.03 | 22.59 | 0.00 |
| Right ACA Diameter [Cadavers] | 2.16 | 0.32 | 0.10 | 1.53 | 2.79 | 6.76 | 0.00 |
| Right ACA Diameter [Radiological Studies] | 1.71 | 0.12 | 0.01 | 1.48 | 1.95 | 14.27 | 0.00 |
| Left ACA Diameter [Overall] | 1.87 | 0.07 | 0.00 | 1.74 | 2.00 | 28.04 | 0.00 |
| Left ACA Diameter [Cadavers] | 2.11 | 0.28 | 0.08 | 1.56 | 2.65 | 7.53 | 0.00 |
| Left ACA Diameter [Radiological Studies] | 1.74 | 0.14 | 0.02 | 1.47 | 2.02 | 12.45 | 0.00 |
| Other Results from the Literature ** | |||||||
| Author | Data | ||||||
| Total Diameter [mm] | |||||||
| Cilliers, K. & Page, B.J. [] | Mean = 2.3 | ||||||
| Ugur, H.C. et al. [] | Mean = 2.75 | ||||||
| Stefani, M.A. et al. [] | Mean = 2.6; Standard Deviation = 0.3 | ||||||
| Right ACA Diameter [mm] | |||||||
| Quijano Blanco, Y. & García Orjuela, D. [] | Mean = 1.98 | ||||||
| Cilliers, K. & Page, B.J. [] | Mean = 2.3 | ||||||
| Swetha, B. [] | Mean = 2 | ||||||
| Forero, P. [] | Mean = 2.54 | ||||||
| Left ACA Diameter [mm] | |||||||
| Quijano Blanco, Y. & García Orjuela, D. [] | Mean = 2.21 | ||||||
| Cilliers, K. & Page, B.J. [] | Mean = 2.4 | ||||||
| Swetha, B. [] | Mean = 2.01 | ||||||
| Forero, P. [] | Mean = 2.43 | ||||||
3.6. Anomalous ACA
The overall pooled prevalence of the azygos ACA was 1.32% (95% CI: 0.84–1.89%). The pooled prevalence of the median ACA was 2.65% (95% CI: 1.57–3.99%), and of the bihemispheric ACA was 1.12% (95% CI: 0.57–1.83%). Interestingly, in all categories, the prevalence rates based on cadaveric studies were higher than those based on radiological studies. Although no statistically significant differences were found (p > 0.05) due to the wide confidence intervals, these results may suggest that certain anatomical variations in the ACA may remain undetected through radiological methods. Full results are shown in Table 6.

Table 6.
Statistical results of this meta-analysis regarding the pooled prevalence of anomalous Anterior Cerebral Artery (ACA). The presented results are based on the following studies: Windle, B.C. []; Baptista, A.G. []; Jain, K.K. []; Fisher, C. []; Lemay, M. & Gooding, C.A. []; Wollschlaeger, G. et al. []; Ring, B.A. & Waddington, M.M. []; Dunker, R.O. & Harris, A.B. []; Ozaki, T. et al. []; Tulleken, C.A.F. []; Huber, P. & Braun, J. []; van der Zwan, A. et al. []; Sanders, W.P. et al. []; Macchi, C. et al. []; Serizawa, T. et al. []; Stefani, M.A. et al. []; Avci, E. et al. []; Kulenović, A. et al. []; Paul, S. & Mishra, S. []; Ugur, H.C. et al. []; Ugur, H.C. et al. []; Kahilogullari, G. 2008; Kapoor, K. et al. []; Saidi, H. et al. []; Lehecka, M. et al. []; Nordon, D. & Rodrigues Junior, O. []; Shi, W.-Y. et al. []; Gunnal, S.A. et al. []; Cilliers, K. & Page, B. []; Kedia, S. et al. []; Hamidi, C. et al. []; Stefani, M.A. et al. []; Cilliers, K. & Page, B.J. []; Jiménez-Sosa, M.S. et al. []; Shatri, J. et al. []; Madkour, N.A.A. []. LCI—lower confidence interval. HCI—higher confidence interval. Q—Cochran’s Q.
Table 6.
Statistical results of this meta-analysis regarding the pooled prevalence of anomalous Anterior Cerebral Artery (ACA). The presented results are based on the following studies: Windle, B.C. []; Baptista, A.G. []; Jain, K.K. []; Fisher, C. []; Lemay, M. & Gooding, C.A. []; Wollschlaeger, G. et al. []; Ring, B.A. & Waddington, M.M. []; Dunker, R.O. & Harris, A.B. []; Ozaki, T. et al. []; Tulleken, C.A.F. []; Huber, P. & Braun, J. []; van der Zwan, A. et al. []; Sanders, W.P. et al. []; Macchi, C. et al. []; Serizawa, T. et al. []; Stefani, M.A. et al. []; Avci, E. et al. []; Kulenović, A. et al. []; Paul, S. & Mishra, S. []; Ugur, H.C. et al. []; Ugur, H.C. et al. []; Kahilogullari, G. 2008; Kapoor, K. et al. []; Saidi, H. et al. []; Lehecka, M. et al. []; Nordon, D. & Rodrigues Junior, O. []; Shi, W.-Y. et al. []; Gunnal, S.A. et al. []; Cilliers, K. & Page, B. []; Kedia, S. et al. []; Hamidi, C. et al. []; Stefani, M.A. et al. []; Cilliers, K. & Page, B.J. []; Jiménez-Sosa, M.S. et al. []; Shatri, J. et al. []; Madkour, N.A.A. []. LCI—lower confidence interval. HCI—higher confidence interval. Q—Cochran’s Q.
| Category | Total n | Pooled Prevalence | LCI | HCI | Q | I2 |
|---|---|---|---|---|---|---|
| Azygos ACA | ||||||
| Overall | 21,795 | 1.32% | 0.84% | 1.89% | 199.52 | 82.46 |
| Cadavers | 2563 | 1.67% | 0.81% | 2.82% | 54.80 | 61.68 |
| Radiological Studies | 19,232 | 0.97% | 0.50% | 1.60% | 111.37 | 88.33 |
| Median ACA | ||||||
| Overall | 21,795 | 2.65% | 1.57% | 3.99% | 694.12 | 94.96 |
| Cadavers | 2563 | 4.56% | 2.35% | 7.41% | 146.14 | 85.63 |
| Radiological Studies | 19,232 | 0.82% | 0.28% | 1.63% | 210.74 | 93.83 |
| Bihemispheric ACA | ||||||
| Overall | 21,795 | 1.12% | 0.57% | 1.83% | 384.19 | 90.89 |
| Cadavers | 2563 | 1.95% | 0.45% | 4.32% | 188.15 | 88.84 |
| Radiological Studies | 19,232 | 0.33% | 0.07% | 0.74% | 114.92 | 88.69 |
3.7. Other Results from the Literature
The total length of the ACA, without segmentation, was measured by Ozturk et al., 2017 [], with values ranging from 32 mm to 42 mm and a mean of 37.5 mm.
The comparison of A1 segment thickness between the right and left sides was studied by Ozaki et al., 1977 []. In 118 cases, the right and left ACAs were equally thick; in 8 cases, the right ACA was thicker, and in another 8, the left ACA was thicker.
The total length of the A3 segment was reported in two articles [,], with mean values ranging from 36.3 mm to 41.0 mm. Differences between the right and left ACA were addressed in two studies [,]; the mean right A3 length ranged from 37.2 mm to 40.39 mm, while the left ranged from 35.7 mm to 39.37 mm.
The diameter of the A3 segment was established in one study [] and reported to be 2.1 mm. However, two articles [,] examined differences between the right and left sides, with reported values ranging from 1.09 mm to 2.00 mm for the right A3 and from 1.07 mm to 2.2 mm for the left A3.
The total length of the A4 segment was measured in two studies [,], with mean values ranging from 25.4 mm to 27.0 mm. A difference between the right and left ACA was reported in one article [], where the mean right A4 length was 26.1 mm and the left 24.5 mm.
The diameter of the A4 segment was studied in only one article [], which found an overall value of 1.6 mm, with right and left sides measured at 1.6 mm and 1.7 mm, respectively.
Azygos ACA is a vascular anomaly characterized by the formation of a single A2 segment in the midline, resulting from the persistence of the embryonic median artery of the corpus callosum []. The occurrence of azygos ACA types was examined in two studies [,], each using different classification methods. According to Beyhan et al., Type A (branching at the root of the A2 segment) occurred in 1.75% of patients, Type B (branching at the genu of the corpus callosum) in 7.02%, Type C (branching between the genu and mid-body) in 84.21%, and Type D (branching after the mid-body) in 7.02%. According to Gunnal et al., Type 1 (classical azygos ACA) occurred in 2.70% of patients, Type 2 (short median stem) in 1.80%, Type 3 (two A2 segments, one of which is short and terminates early) in 3.60%, Type 4 (azygos pericallosal artery) in 2.70%, and Type 5 (third azygos median A2 artery) in 0.90%. The first percentages refer to the number of azygos ACA cases studied, while the second refer to the total number of patients.
The mean diameter of the median and bihemispheric ACA was studied by Cilliers et al., 2016 [], with both variations having a mean diameter of 1.8 mm and standard deviations of 0.3 and 0.4, respectively.
Atypical origins of the ACA were analyzed in one study [], which reported that the ACA originated from the superior internal parietal artery in 7.30% of cases, from the paracentral lobule artery in 3.70%, from the inferior internal parietal artery in 3.30%, from the middle internal frontal artery in 0.70%, and from the posterior internal frontal artery in 0.70%.
4. Discussion
This meta-analysis provides a comprehensive overview of the anatomy and variations in the ACA, consolidating data from 24,015 cases. The findings enhance our understanding of ACA morphology, particularly its critical role in cerebrovascular and neurosurgical procedures.
The pooled mean length of the A1 segment was 14.47 mm across all studies, with slight differences between cadaveric (14.61 mm) and radiological (14.11 mm) data. Although minor, this variation may reflect methodological differences in measurement precision between dissection and imaging studies. These results are relatively consistent with previously published literature, such as the studies by Luckrajh et al. [] and Sharma et al. []. The A1 segment’s diameter also showed variability, with a pooled mean of 2.00 mm overall, slightly smaller in cadaveric studies (1.86 mm) and larger in radiological studies (2.12 mm).
The A2 segment demonstrated more variability, with pooled mean lengths of 18.39 mm (right ACA) and 18.34 mm (left ACA) in radiological studies. The substantial standard errors (6.31 mm for the right and 6.72 mm for the left) indicate high individual variability, as confirmed by studies such as those by Quijano Blanco et al. [] and Yu et al. [], which reported a wide range from 4.42 mm to over 69 mm. Moreover, the pooled mean diameter of the A2 segment was 1.76 mm. This wide range highlights the morphometric variability of the A2 segment. These findings are significant because precise knowledge of ACA measurements is critical when treating aneurysms with either surgical clipping or endovascular techniques, where even slight anatomical differences may affect outcomes [,].
As previously discussed, anomalies of the ACA are classified into three types: AzACA, MedACA, and BihemACA. The present meta-analysis is the first to report pooled prevalence rates of these anomalies, which are essential not only anatomically but also in clinical practice []. The pooled prevalence of the AzACA was 1.32%, with a higher rate in cadaveric studies (1.67%) compared to radiological studies (0.97%). This variation can complicate neurosurgical procedures, as the AzACA often supplies both cerebral hemispheres, meaning damage or occlusion may result in bilateral ischemia []. Identifying this variation preoperatively is therefore essential to prevent potentially catastrophic outcomes.
The pooled prevalence of the MedACA was 2.65%, with a significantly higher prevalence in cadaveric studies (4.56%) than in radiological studies (0.82%). Detection of this anomaly is particularly important in cases involving interhemispheric tumors or vascular malformations approached via the interhemispheric route []. The discrepancy between cadaveric and radiological data suggests that some anomalies may be missed during clinical imaging, highlighting the need for more detailed radiological evaluations.
The BihemACA had the lowest pooled prevalence at 1.12% overall, again higher in cadaveric studies (1.95%) compared to radiological studies (0.33%). Similarly to the AzACA, the BihemACA—where one ACA supplies both hemispheres—poses a significant risk during surgery or endovascular intervention [,]. Inadvertent damage or occlusion may result in bilateral cerebral infarction, making its identification crucial in surgical planning [].
The anatomical variations and morphometric properties of the ACA demonstrated in this study have several clinical implications. The variability in ACA length and diameter necessitates precision in diagnostic imaging and surgical intervention. For instance, aneurysms frequently occur at ACA bifurcation points, and the presence of an AzACA or BihemACA may alter the approach to endovascular coiling or surgical clipping. In the case of an AzACA, the fusion of the two A2 segments into a single vessel means that both hemispheres may rely on one artery. This elevates the risk during aneurysm treatment, as any compromise to the AzACA could lead to bilateral ischemia [,]. The surgeon must consider altered hemodynamics and ensure sufficient collateral circulation during and after the procedure.
Similarly, identifying a MedACA can influence decisions during interhemispheric surgery, as this vessel may supply vital areas of the medial frontal cortex. The MedACA may follow an unusual course, making it important for surgeons to carefully navigate around it to avoid damage. In procedures such as corpus callosotomy or tumor resection, an unrecognized MedACA may lead to ischemic complications if injured [,,]. Detailed preoperative imaging is therefore essential to map its anatomy and ensure safe outcomes.
Understanding ACA variability also has implications for ischemic stroke management. Recognizing ACA anomalies may help predict the extent of cerebral ischemia and guide treatment strategies [].
This study acknowledges certain limitations, including potential biases due to the heterogeneous nature of the source data. The reliability of findings is constrained by differences across studies, and some analyses could not be performed due to insufficient consistent data. Nonetheless, this meta-analysis offers a robust estimation of ACA anatomy based on literature that meets the standards of evidence-based anatomical research.
5. Conclusions
This systematic review and meta-analysis provides valuable insights into the anatomy and variations in the ACA. The findings reveal that the pooled mean length of the A1 segment is 14.47 mm, while the pooled mean diameter is 2.00 mm. For the A2 segment, the pooled mean lengths were 18.39 mm for the right ACA and 18.34 mm for the left ACA, with a pooled mean diameter of 1.76 mm. Notably, the analysis also identified significant anatomical variations, with an overall pooled prevalence of 1.32% for the AzACA, 2.65% for the MedACA, and 1.12% for the BihemACA. It is hoped that the results of the present study will assist clinicians and neurosurgeons in managing various cerebrovascular disorders and procedures, ultimately enhancing the safety and outcomes of these interventions.
Author Contributions
Conceptualization, M.B., K.M., A.M., J.T., P.O., A.E. and A.Y.; methodology, M.B., K.M., A.M., J.T., P.O., A.E. and A.Y.; validation, M.B., K.M., A.M., J.T., P.O., A.E., A.Y., M.K., M.G., S.O., A.Ż., P.W., M.P. and G.W.; formal analysis, M.B., K.M., A.M., J.T., P.O., A.E., A.Y., M.K., M.G., S.O., A.Ż., P.W., M.P. and G.W.; resources, M.K., M.P. and G.W.; data curation, M.B., K.M., A.M., J.T., P.O., A.E. and A.Y.; writing—original draft preparation, M.B., K.M., A.M., J.T., P.O., A.E., A.Y., M.K., M.G., S.O., A.Ż., P.W., M.P. and G.W.; writing—review and editing, M.B., K.M., A.M., J.T., P.O., A.E., A.Y., M.K., M.G., S.O., A.Ż., P.W., M.P. and G.W.; supervision, M.K., M.P., A.Ż. and G.W.; visualization, G.W.; project administration, M.B., K.M., A.M., J.T., P.O., A.E., A.Y., M.K., M.G., S.O., A.Ż., P.W., M.P. and G.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All the data is included in the article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ACA | Anterior cerebral artery |
| AzACA | Azygos ACA |
| BihemACA | Bihemispheric ACA |
| MedACA | Median ACA |
| CTA | Computed Tomography Angiography |
| DSA | Digital Subtraction Angiography |
| MRA | Magnetic Resonance Angiography |
| MRI | Magnetic Resonance Imaging |
References
- Moore, K.L.; Dalley, A.F.; Agur, A. Clinically Oriented Anatomy, 8th ed.; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2017. [Google Scholar]
- Haines, D.E.; Gregory, A.; Mihailoff, G.A. Fundamental Neuroscience for Basic and Clinical Applications; Elsevier: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Żytkowski, A.; Clarke, E.; Olszewska, A.; Mazurek, A.; Dubrowski, A.; Radek, M. Early Bifurcation of the Middle Cerebral Artery—A Case Report with Commentaries on the Clinical Significance. Transl. Res. Anat. 2022, 26, 100161. [Google Scholar] [CrossRef]
- Cilliers, K.; Page, B.J. Detailed Description of the Anterior Cerebral Artery Anomalies Observed in a Cadaver Population. Ann. Anat.—Anat. Anz. 2016, 208, 1–8. [Google Scholar] [CrossRef]
- González Zavala, P.A.; Falcón Molina, J.E.; Lozano Guzmán, I.; Abdo Toro, M.A.; Téllez Medina, I.; García López, R.; Salazar Ramírez, Z.E.; Sandoval Ramírez, C.J. Anterior Interhemispheric Approach for the Surgical Treatment of Azygos Anterior Cerebral Artery Aneurysms: A Case Series. Cureus 2024, 16, e58808. [Google Scholar] [CrossRef]
- Asai, T.; Oyama, T.; Takita, W.; Ohno, M.; Suzaki, N.; Kajita, Y.; Takahashi, T. Mechanical Thrombectomy for Azygos Anterior Cerebral Artery Occlusion: A Case Report and Literature Review. J. Neuroendovascular Ther. 2021, 15, 609–614. [Google Scholar] [CrossRef]
- Anetsberger, S.; Gonzalez-Lopez, P.; Elsawaf, Y.; Giotta Lucifero, A.; Luzzi, S.; Elbabaa, S. Interhemispheric Approach. Acta Biomed. 2022, 92, e2021351. [Google Scholar] [CrossRef]
- Zhai, X.-D.; Yu, J.-X.; Li, C.-J.; Ren, J.; Ji, Z.; He, C.; Ye, M.; Hu, P.; Zhang, H.-Q. Morphological Characteristics of Pericallosal Artery Aneurysms and Their High Propensity for Rupture. World Neurosurg. 2020, 133, e320–e326. [Google Scholar] [CrossRef]
- Żytkowski, A.; Mazurek, A.; Dubrowski, A.; Clarke, E.; Barszcz, K.; Balawender, K.; Szmyd, B.; Radek, M. Atypical Formation of Pericallosal Artery A4 Segment Altering the Corpus Callosum—Anatomical Case Report. Transl. Res. Anat. 2022, 27, 100197. [Google Scholar] [CrossRef]
- D’Antoni, A.V.; Tubbs, R.S.; Patti, A.C.; Higgins, Q.M.; Tiburzi, H.; Battaglia, F. The Critical Appraisal Tool for Anatomical Meta-analysis: A Framework for Critically Appraising Anatomical Meta-analyses. Clin. Anat. 2022, 35, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Henry, B.M.; Tomaszewski, K.A.; Ramakrishnan, P.K.; Roy, J.; Vikse, J.; Loukas, M.; Tubbs, R.S.; Walocha, J.A. Development of the Anatomical Quality Assessment (AQUA) Tool for the Quality Assessment of Anatomical Studies Included in Meta-Analyses and Systematic Reviews. Clin. Anat. 2017, 30, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Henry, B.M.; Vikse, J.; Pekala, P.; Loukas, M.; Tubbs, R.S.; Walocha, J.A.; Jones, D.G.; Tomaszewski, K.A. Consensus Guidelines for the Uniform Reporting of Study Ethics in Anatomical Research within the Framework of the Anatomical Quality Assurance (AQUA) Checklist. Clin. Anat. 2018, 31, 521–524. [Google Scholar] [CrossRef] [PubMed]
- Windle, B.C. The Arteries Forming the Circle of Willis. J. Anat. Physiol. 1888, 22, 289–293. [Google Scholar]
- Baptista, A.G. Studies on the Arteries of the Brain. Neurology 1963, 13, 825. [Google Scholar] [CrossRef]
- Murray, K.D. Dimensions of the Circle of Willis and Dynamic Studies Using Electrical Analogy. J. Neurosurg. 1964, 21, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Jain, K.K. Some Observations On The Anatomy of The Middle Cerebral Artery. Can. J. Surg. 1964, 7, 134–139. [Google Scholar] [PubMed]
- Fisher, C. The Circle of Willis: Anatomical Variations. Vasc. Dis. 1965, 2, 99–105. [Google Scholar]
- Lemay, M.; Gooding, C.A. The Clinical Significance of The Azygos Anterior Cerebral Artery (A.C.A.). Am. J. Roentgenol. 1966, 98, 602–610. [Google Scholar] [CrossRef]
- Wollschlaeger, G.; Wollschlaeger, P.B.; Lucas, F.V.; Lopez, V.F. Experience and Result With Postmortem Cerebral Angiography Performed As Routine Procedure of The Autopsy. Am. J. Roentgenol. 1967, 101, 68–87. [Google Scholar] [CrossRef] [PubMed]
- Ring, B.A.; Waddington, M.M. Roentgenographic Anatomy of The Pericallosal Arteries. Am. J. Roentgenol. 1968, 104, 109–118. [Google Scholar] [CrossRef]
- Dunker, R.O.; Harris, A.B. Surgical Anatomy of the Proximal Anterior Cerebral Artery. J. Neurosurg. 1976, 44, 359–367. [Google Scholar] [CrossRef]
- Perlmutter, D.; Rhoton, A.L. Microsurgical Anatomy of the Anterior Cerebral-Anterior Communicating-Recurrent Artery Complex. J. Neurosurg. 1976, 45, 259–272. [Google Scholar] [CrossRef]
- Ozaki, T.; Handa, H.; Tomimoto, K.; Hazama, F. Anatomical Variations of the Arterial System of the Base of the Brain. Nihon Geka Hokan 1977, 46, 3–17. [Google Scholar]
- Tulleken, C.A.F. A Study of the Anatomy of the Anterior Communicating Artery with the Aid of the Operating Microscope. Clin. Neurol. Neurosurg. 1978, 80, 169–173. [Google Scholar] [CrossRef]
- Perlmutter, D.; Rhoton, A.L. Microsurgical Anatomy of the Distal Anterior Cerebral Artery. J. Neurosurg. 1978, 49, 204–228. [Google Scholar] [CrossRef]
- Huber, P.; Braun, J.; Hirschmann, D.; Agyeman, J.F. Incidence of Berry Aneurysms of the Unpaired Pericallosal Artery: Angiographic Study. Neuroradiology 1980, 19, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Kamath, S. Observations on the Length and Diameter of Vessels Forming the Circle of Willis. J. Anat. 1981, 133, 419–423. [Google Scholar] [PubMed]
- Orlandini, G.E.; Ruggiero, C.; Zecchi Orlandini, S.; Gulisano, M. Blood Vessel Size of Circulus Arteriosus Cerebri (Circle of Willis): A Statistical Research on 100 Human Subjects. Cells Tissues Organs 1985, 123, 72–76. [Google Scholar] [CrossRef]
- Gomes, F.B.; Dujovny, M.; Umansky, F.; Berman, S.K.; Diaz, F.G.; Ausman, J.I.; Mirchandani, H.G.; Ray, W.J. Microanatomy of the Anterior Cerebral Artery. Surg. Neurol. 1986, 26, 129–141. [Google Scholar] [CrossRef]
- Krabbe-Hartkamp, M.J.; van der Grond, J.; de Leeuw, F.E.; de Groot, J.C.; Algra, A.; Hillen, B.; Breteler, M.M.; Mali, W.P. Circle of Willis: Morphologic Variation on Three-Dimensional Time-of-Flight MR Angiograms. Radiology 1998, 207, 103–111. [Google Scholar] [CrossRef]
- van der Zwan, A.; Hillen, B.; Tulleken, C.A.F.; Dujovny, M.; Dragovic, L. Variability of the Territories of the Major Cerebral Arteries. J. Neurosurg. 1992, 77, 927–940. [Google Scholar] [CrossRef] [PubMed]
- Sanders, W.P.; Sorek, P.A.; Mehta, B.A. Fenestration of Intracranial Arteries with Special Attention to Associated Aneurysms and Other Anomalies. AJNR Am. J. Neuroradiol. 1993, 14, 675–680. [Google Scholar]
- Piepgras, A.; Bise, K.; Schmiedek, P. Morphometry of Intraluminal Side-to-Side Differences in Human Basal Cerebral Arteries. Ultrasound Med. Biol. 1993, 19, 193–195. [Google Scholar] [CrossRef]
- Macchi, C.; Catini, C.; Federico, C.; Gulisano, M.; Pacini, P.; Cecchi, F.; Corcos, L.; Brizzi, E. Magnetic Resonance Angiographic Evaluation of Circulus Arteriosus Cerebri (Circle of Willis): A Morphologic Study in 100 Human Healthy Subjects. Ital. J. Anat. Embryol. 1996, 101, 115–123. [Google Scholar] [PubMed]
- Serizawa, T.; Saeki, N.; Yamaura, A. Microsurgical Anatomy and Clinical Significance of the Anterior Communicating Artery and Its Perforating Branches. Neurosurgery 1997, 40, 1211–1218. [Google Scholar] [CrossRef]
- Stefani, M.A.; Schneider, F.L.; Marrone, A.C.H.; Severino, A.G.; Jackowski, A.P.; Wallace, M.C. Anatomic Variations of Anterior Cerebral Artery Cortical Branches. Clin. Anat. 2000, 13, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Avci, E.; Fossett, D.; Erdogan, A.; Egemen, N.; Attar, A.; Aslan, M. Perforating Branches of the Anomalous Anterior Communicating Complex. Clin. Neurol. Neurosurg. 2001, 103, 19–22. [Google Scholar] [CrossRef]
- Kulenović, A.; Dilberović, F.; Ovcina, F. [Variation in the Flow and Branching of the Anterior and Middle Cerebral Arteries]. Med. Arh. 2003, 57, 3–5. [Google Scholar]
- Ugur, H.C.; Kahilogullari, G.; Coscarella, E.; Unlu, A.; Tekdemir, I.; Morcos, J.J.; Elhan, A.; Baskaya, M.K. Arterial Vascularization of Primary Motor Cortex (Precentral Gyrus). Surg. Neurol. 2005, 64, S48–S52. [Google Scholar] [CrossRef]
- Pai, S.B.; Varma, R.; Kulkarni, R. Microsurgical Anatomy of the Middle Cerebral Artery. Neurol. India 2005, 53, 186. [Google Scholar] [CrossRef] [PubMed]
- Ugur, H.C.; Kahilogullari, G.; Esmer, A.F.; Comert, A.; Odabasi, A.B.; Tekdemir, I.; Elhan, A.; Kanpolat, Y. A Neurosurgical View of Anatomical Variations of the Distal Anterior Cerebral Artery: An Anatomical Study. J. Neurosurg. 2006, 104, 278–284. [Google Scholar] [CrossRef]
- Tao, X.; Yu, X.J.; Bhattarai, B.; Li, T.H.; Jin, H.; Wei, G.W.; Ming, J.S.; Ren, W.; Jiong, C. Microsurgical Anatomy of the Anterior Communicating Artery Complex in Adult Chinese Heads. Surg. Neurol. 2006, 65, 155–161. [Google Scholar] [CrossRef]
- Mandiola, E.; Alarcon, E.; Onate, J.C.; Sanhueza, P.; del Sol, M.; Olave, E. Biometrical Aspects of the Anterior Cerebral Artery in Its Proximal Segment (A1) and Internal Carotid Artery. Int. J. Morphol. 2007, 25, 915–919. [Google Scholar] [CrossRef]
- Saidi, H.; Kitunguu, P.; Ogeng’O, J. Variant Anatomy of The Anterior Cerebral Artery In Adult Brains. Afr. J. Neurol. Sci. 2008, 27, 97–105. [Google Scholar]
- Lehecka, M.; Dashti, R.; Hernesniemi, J.; Niemelä, M.; Koivisto, T.; Ronkainen, A.; Rinne, J.; Jääskeläinen, J. Microneurosurgical Management of Aneurysms at the A2 Segment of Anterior Cerebral Artery (Proximal Pericallosal Artery) and Its Frontobasal Branches. Surg. Neurol. 2008, 70, 232–246. [Google Scholar] [CrossRef]
- Kapoor, K.; Singh, B.; Dewan, L.I.J. Variations in the Configuration of the Circle of Willis. Anat. Sci. Int. 2008, 83, 96–106. [Google Scholar] [CrossRef]
- Kahilogullari, G.; Comert, A.; Arslan, M.; Esmer, A.F.; Tuccar, E.; Elhan, A.; Tubbs, R.S.; Ugur, H.C. Callosal Branches of the Anterior Cerebral Artery: An Anatomical Report. Clin. Anat. 2008, 21, 383–388. [Google Scholar] [CrossRef]
- Ozdogmus, O.; Çakmak, Ö.; Yalin, A.; Keklik, D.; Üzün, Ý.; Çavdar, S. Changing Diameters of Cerebral Vessels with Age in Human Autopsy Specimens: Possible Relationships to Atherosclerotic Changes. Zentralblatt Neurochir.—Cent. Eur. Neurosurg. 2008, 69, 139–143. [Google Scholar] [CrossRef]
- Żurada, A.; Gielecki, J.; Tubbs, R.S.; Loukas, M.; Cohen-Gadol, A.A.; Chlebiej, M.; Maksymowicz, W.; Nowak, D.; Zawiliński, J.; Michalak, M. Three-dimensional Morphometry of the A2 Segment of the Anterior Cerebral Artery with Neurosurgical Relevance. Clin. Anat. 2010, 23, 759–769. [Google Scholar] [CrossRef] [PubMed]
- Maaly, M.A.; Ismail, A.A. Three Dimensional Magnetic Resonance Angiography of the Circle of Willis: Anatomical Variations in General Egyptian Population. Egypt. J. Radiol. Nucl. Med. 2011, 42, 405–412. [Google Scholar] [CrossRef]
- Nordon, D.; Rodrigues Junior, O. Variations in the Brain Circulation—The Circle of Willis. J. Morphol. Sci. 2012, 29, 243–247. [Google Scholar]
- Shi, W.-Y.; Li, M.-H.; Gu, B.-X.; Li, Y.-D.; Tan, H.-Q. Azygous Anterior Cerebral Artery and Associated Aneurysms: Detection and Identification Using 3-Dimensional Time-of-Flight Magnetic Resonance Angiography. J. Neuroimaging 2014, 24, 18–22. [Google Scholar] [CrossRef]
- Swetha, B. Anatomic Features of Distal Anterior Cerebral Artery Supply on Corpus Callosum: A Detailed Study on 140 Cerebral Hemispheres. J. Neurol. Sci. Turk. 2012, 29, 046–056. [Google Scholar]
- Aggarwal, N.; Paul, M.; Mukherjee, M.; Toppo, J.; Kaur, M.; Goel, G. Length of the Anterior Cerebral Artery (ACA) on MRI Angiograms. J. Clin. Diagn. Res. 2012, 6, 764–766. [Google Scholar]
- Stefani, M.A.; Schneider, F.L.; Marrone, A.C.H.; Severino, A.G. Influence of the Gender on Cerebral Vascular Diameters Observed during the Magnetic Resonance Angiographic Examination of Willis Circle. Braz. Arch. Biol. Technol. 2013, 56, 45–52. [Google Scholar] [CrossRef]
- Kedia, S.; Daisy, S.; Mukherjee, K.; Salunke, P.; Srinivasa, R.; Narain, M. Microsurgical Anatomy of the Anterior Cerebral Artery in Indian Cadavers. Neurol. India 2013, 61, 117. [Google Scholar] [CrossRef]
- Hamidi, C.; Bükte, Y.; Hattapoğlu, S.; Ekici, F.; Tekbaş, G.; Önder, H.; Gümüş, H.; Bilici, A. Display with 64-Detector MDCT Angiography of Cerebral Vascular Variations. Surg. Radiol. Anat. 2013, 35, 729–736. [Google Scholar] [CrossRef]
- Flores, B.C.; Scott, W.W.; Eddleman, C.S.; Batjer, H.H.; Rickert, K.L. The A1-A2 Diameter Ratio May Influence Formation and Rupture Potential of Anterior Communicating Artery Aneurysms. Neurosurgery 2013, 73, 845–853. [Google Scholar] [CrossRef] [PubMed]
- Gunnal, S.A.; Farooqui, M.S.; Wabale, R.N. Anatomical Variations of the Circulus Arteriosus in Cadaveric Human Brains. Neurol. Res. Int. 2014, 2014, 687281. [Google Scholar] [CrossRef] [PubMed]
- Karatas, A.; Coban, G.; Cinar, C.; Oran, I.; Uz, A. Assessment of the Circle of Willis with Cranial Tomography Angiography. Med. Sci. Monit. 2015, 21, 2647–2652. [Google Scholar] [CrossRef]
- Klimek-Piotrowska, W.; Rybicka, M.; Wojnarska, A.; Wójtowicz, A.; Koziej, M.; Hołda, M.K. A Multitude of Variations in the Configuration of the Circle of Willis: An Autopsy Study. Anat. Sci. Int. 2016, 91, 325–333. [Google Scholar] [CrossRef]
- D’Avella, E.; De Notaris, M.; Enseñat, J.; Berenguer, J.; Gragnaniello, C.; Mavar, M.; Ferrer, E.; Prats-Galino, A. The Extended Endoscopic Endonasal Transplanum Transtuberculum Approach to the Anterior Communicating Artery Complex: Anatomic Study. Acta Neurochir. 2015, 157, 1495–1503. [Google Scholar] [CrossRef]
- Arat, Y.; Arat, A.; Aydin, K. Angiographic Morphometry of Internal Carotid Circulation in Turkish Children. Turk. Neurosurg. 2015, 25, 608–616. [Google Scholar] [CrossRef]
- Aggarwal, N.; Paul, M.M.; Mukherjee, M. Diameter of Anterior Cerebral Artery On Mri Angiograms. Int. J. Anat. Res. 2016, 4, 2245–2250. [Google Scholar] [CrossRef]
- Shinde, S.; Shroff, G. Anatomical Variations In Anterior Cerebral Artery In Human Cadavers. Int. J. Anat. Res. 2016, 4, 2269–2272. [Google Scholar] [CrossRef]
- Karatas, A.; Yilmaz, H.; Coban, G.; Koker, M.; Uz, A. The Anatomy of Circulus Arteriosus Cerebri (Circle of Willis): A Study in Turkish Population. Turk. Neurosurg. 2015, 26, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Cilliers, K.; Page, B.J. Description of the Anterior Cerebral Artery and Its Cortical Branches: Variation in Presence, Origin, and Size. Clin. Neurol. Neurosurg. 2017, 152, 78–83. [Google Scholar] [CrossRef]
- Shatri, J.; Bexheti, D.; Bexheti, S.; Kabashi, S.; Krasniqi, S.; Ahmetgjekaj, I.; Zhjeqi, V. Influence of Gender and Age on Average Dimensions of Arteries Forming the Circle of Willis Study by Magnetic Resonance Angiography on Kosovo’s Population. Open Access Maced. J. Med. Sci. 2017, 5, 714–719. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.-H.; Shang-Guan, H.-C.; Chen, G.-R.; Zheng, S.-F.; Lin, Y.-X.; Lin, Z.-Y.; Yao, P.-S.; Kang, D.-Z. Monolateral Pterional Keyhole Approaches to Bilateral Cerebral Aneurysms: Anatomy and Clinical Application. World Neurosurg. 2017, 108, 572–580. [Google Scholar] [CrossRef]
- Ozturk, S.; Ayan, E.; Kaplan, M. Morphological Changes of Anterior Cerebral Artery (ACA) in Hydrocephalic Pediatric Patients. Iran. J. Child. Neurol. 2017, 11, 37–42. [Google Scholar]
- Jiménez-Sosa, M.S.; Cantu-Gonzalez, J.R.; Morales-Avalos, R.; de la Garza-Castro, O.; Quiroga-Garza, A.; Pinales-Razo, R.; Elizondo-Riojas, G.; Elizondo-Omaña, R.E.; Guzmán- López, S. Anatomical Variants of Anterior Cerebral Arterial Circle: A Study by Multidetector Computerized 3D Tomographic Angiography. Int. J. Morphol. 2017, 35, 1121–1128. [Google Scholar] [CrossRef]
- Canaz, H.; Arslan, M.; Hacıoglu, H.; Tokmak, M.; Canaz, G.; Cavdar, S. Morphometric Analysis of the Arteries of Willis Polygon. Rom. Neurosurg. 2018, 32, 56–64. [Google Scholar] [CrossRef]
- Shatri, J.; Cerkezi, S.; Ademi, V.; Reci, V.; Bexheti, S. Anatomical Variations and Dimensions of Arteries in the Anterior Part of the Circle of Willis. Folia Morphol. 2019, 78, 259–266. [Google Scholar] [CrossRef]
- Thenmozhi, A.; Kalpana, R.; Subadha, C. Anatomic Variants of The Anterior Part of The Cerebral Arterial Circle: A Cadaveric Study. Int. J. Anat. Res. 2019, 7, 6516–6520. [Google Scholar] [CrossRef]
- Zaki, S.M.; Shaaban, M.H.; Abd Al Galeel, W.A.; El Husseiny, A.A.W. Configuration of the Circle of Willis and Its Two Parts among Egyptian: A Magnetic Resonance Angiographic Study. Folia Morphol. 2019, 78, 703–709. [Google Scholar] [CrossRef]
- Sharma, S.; Dixit, S.G.; Khera, P.S.; Nayyar, A.K.; Ghatak, S. Morphometric Evaluation of Anterior Cerebral Artery (on Digital Subtraction Angiography)–Potential Implications. Morphologie 2020, 104, 109–116. [Google Scholar] [CrossRef]
- Blanco, Y.Q.; Orjuela, D.G. Variantes anatómicas del círculo arterial cerebral en un anfiteatro universitario en Bogotá (Colombia). Rev. Cienc. de la Salud 2020, 18, 121–132. [Google Scholar] [CrossRef]
- Beyhan, M.; Gökçe, E.; Karakuş, K. Radiological Classification of Azygos Anterior Cerebral Artery and Evaluation of the Accompanying Vascular Anomalies. Surg. Radiol. Anat. 2020, 42, 1345–1354. [Google Scholar] [CrossRef]
- Giotta Lucifero, A.; Baldoncini, M.; Bruno, N.; Tartaglia, N.; Ambrosi, A.; Marseglia, G.L.; Galzio, R.; Campero, A.; Hernesniemi, J.; Luzzi, S. Microsurgical Neurovascular Anatomy of the Brain: The Anterior Circulation (Part I). Acta Biomed. 2021, 92, e2021412. [Google Scholar] [CrossRef]
- Riveros, A.; Vega, C.; Negroni, M.; Villagrán, F.; Binvignat, O.; Olave, E. Variations of the Cerebral Arterial Circle. Morphological and Clinical Analysis. Int. J. Morphol. 2022, 40, 632–639. [Google Scholar] [CrossRef]
- Luckrajh, J.S.; Harrichandparsad, R.; Satyapal, K.S.; Lazarus, L. A Clinical Investigation of the Anatomy of the Proximal Anterior Cerebral Artery and Its Association with Anterior Communicating Artery Aneurysm. Transl. Res. Anat. 2022, 27, 100200. [Google Scholar] [CrossRef]
- Madkour, N.A.A. Magnetic Resonance Angiography in Assessment of Anomalies of Anterior Cerebral Artery in Adults. Anat. Cell Biol. 2023, 56, 469–473. [Google Scholar] [CrossRef] [PubMed]
- Forero, P. Variaciones Del Círculo Arterial Cerebral (Willis) y de Las Arterias Cere-Brales: Un Estudio Anatómico Directo. Master’s Thesis, Escuela de Medicina, Universidad Industrial de Santander, Santander, Colombia, 2006. [Google Scholar]
- Paul, S.; Mishra, S. Variations of the Anterior Cerebral Artery in Human Cadavers: A Dissection Study. J. Anat. Soc. India 2004, 53, 15–16. [Google Scholar]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Version 6.5 (Updated August 2024); Cochrane: Chichester, UK, 2024; Available online: www.cochrane.org/handbook (accessed on 3 November 2025).
- Henry, B.M.; Tomaszewski, K.A.; Walocha, J.A. Methods of Evidence-Based Anatomy: A Guide to Conducting Systematic Reviews and Meta-Analysis of Anatomical Studies. Ann. Anat.—Anat. Anz. 2016, 205, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Cilliers, K.; Page, B. Review of the Anatomy of the Distal Anterior Cerebral Artery and Its Anomalies. Turk. Neurosurg. 2015, 26, 653–661. [Google Scholar] [CrossRef]
- Liao, L.; Derelle, A.-L.; Merlot, I.; Civit, T.; Audibert, G.; Tonnelet, R.; Gory, B.; Anxionnat, R.; Bracard, S. Endovascular Treatment of Distal Anterior Cerebral Artery Aneurysms: Long-Term Results. J. Neuroradiol. 2020, 47, 33–37. [Google Scholar] [CrossRef]
- Kubota, Y.; Hanaoka, Y.; Aoyama, T.; Fujii, Y.; Ogiwara, T.; Seguchi, T.; Horiuchi, T. Single-Lane Clipping Technique for a Ruptured Aneurysm of A1 Fenestration of the Anterior Cerebral Artery: A Case Report and Literature Review. Nagoya J. Med. Sci. 2023, 85, 157–166. [Google Scholar] [CrossRef]
- Lee, J.W.; Lee, K.C.; Kim, Y.B.; Huh, S.K. Surgery for Distal Anterior Cerebral Artery Aneurysms. Surg. Neurol. 2008, 70, 153–159. [Google Scholar] [CrossRef]
- Uchino, K.; Kondo, K.; Harada, N.; Aoki, Y.; Noguchi, Y.; Oishi, H.; Sugo, N. A Case of a Ruptured Aneurysm at the Supracallosal Portion (A4–A5) of the Bihemispheric Anterior Cerebral Artery Treated with Endovascular Surgery. J. Neuroendovascular Ther. 2022, 16, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Rusu, M.C.; Lazăr, M.; Vrapciu, A.D. Bihemispheric Right Anterior Cerebral Artery, Fenestrated Origin of the Left Pericallosal Artery, Fenestrated Basilar Artery, Double Right Posterior Cerebral Artery. J. Craniofacial Surg. 2023, 34, e521–e523. [Google Scholar] [CrossRef] [PubMed]
- Hori, T.; Kawamata, T.; Amano, K.; Aihara, Y.; Ono, M.; Miki, N. Anterior Interhemispheric Approach for 100 Tumors in and Around the Anterior Third Ventricle. Oper. Neurosurg. 2010, 66, ons65–ons74. [Google Scholar] [CrossRef]
- Ito, H.; Morino, M.; Niimura, M.; Takamizawa, S.; Shimizu, Y. Posterior Callosotomy Using a Parietooccipital Interhemispheric Approach in the Semi-Prone Park-Bench Position. J. Neurosurg. 2015, 123, 1322–1325. [Google Scholar] [CrossRef]
- Thirugnanachandran, T.; Beare, R.; Mitchell, M.; Wong, C.; Vuong, J.; Singhal, S.; Slater, L.-A.; Hilton, J.; Sinnott, M.; Srikanth, V.; et al. Anterior Cerebral Artery Stroke: Role of Collateral Systems on Infarct Topography. Stroke 2021, 52, 2930–2938. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).