Caregiver Burden in Partners of Parkinsonian Patients with Deep Brain Stimulation
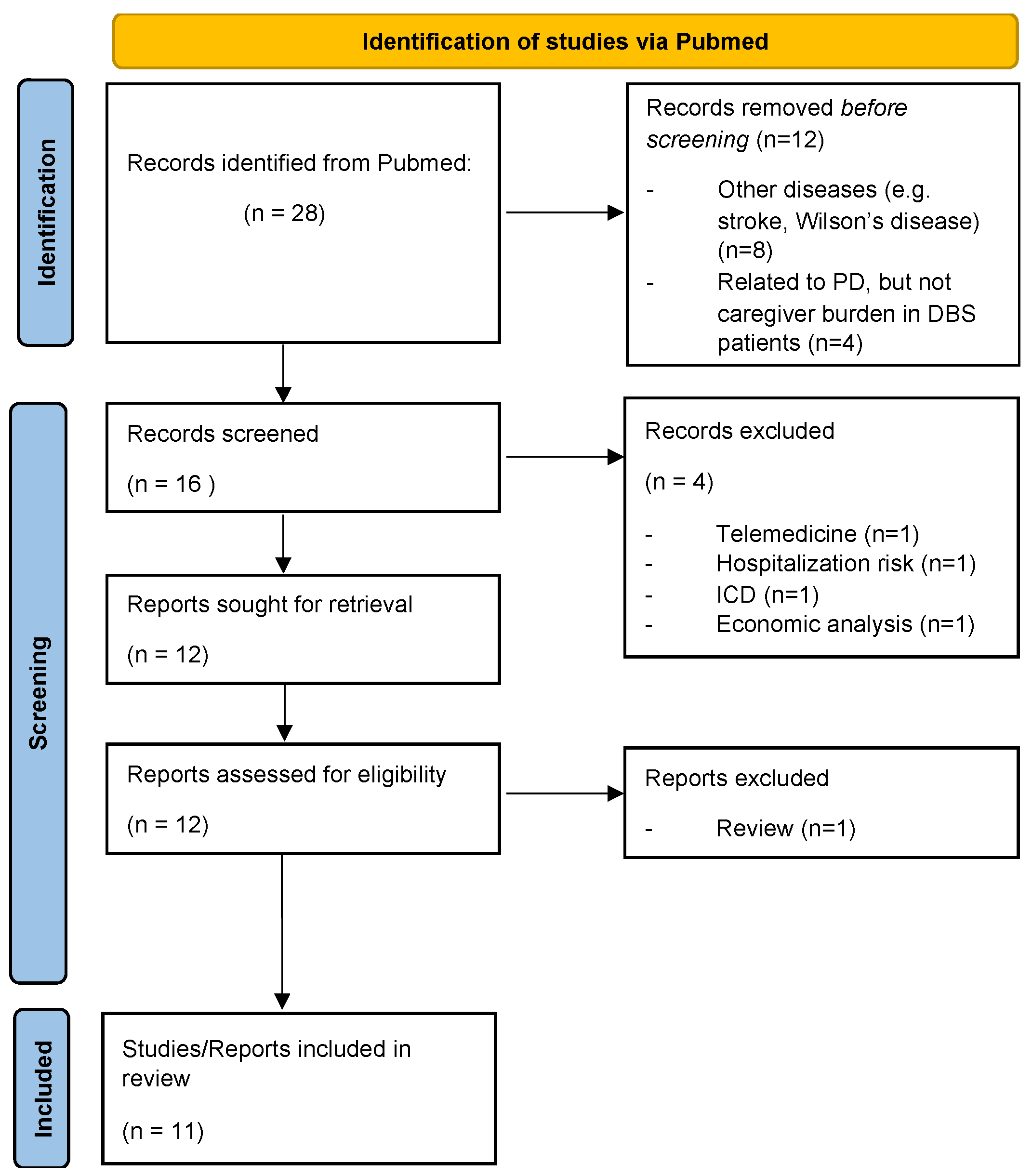
Abstract
1. Introduction
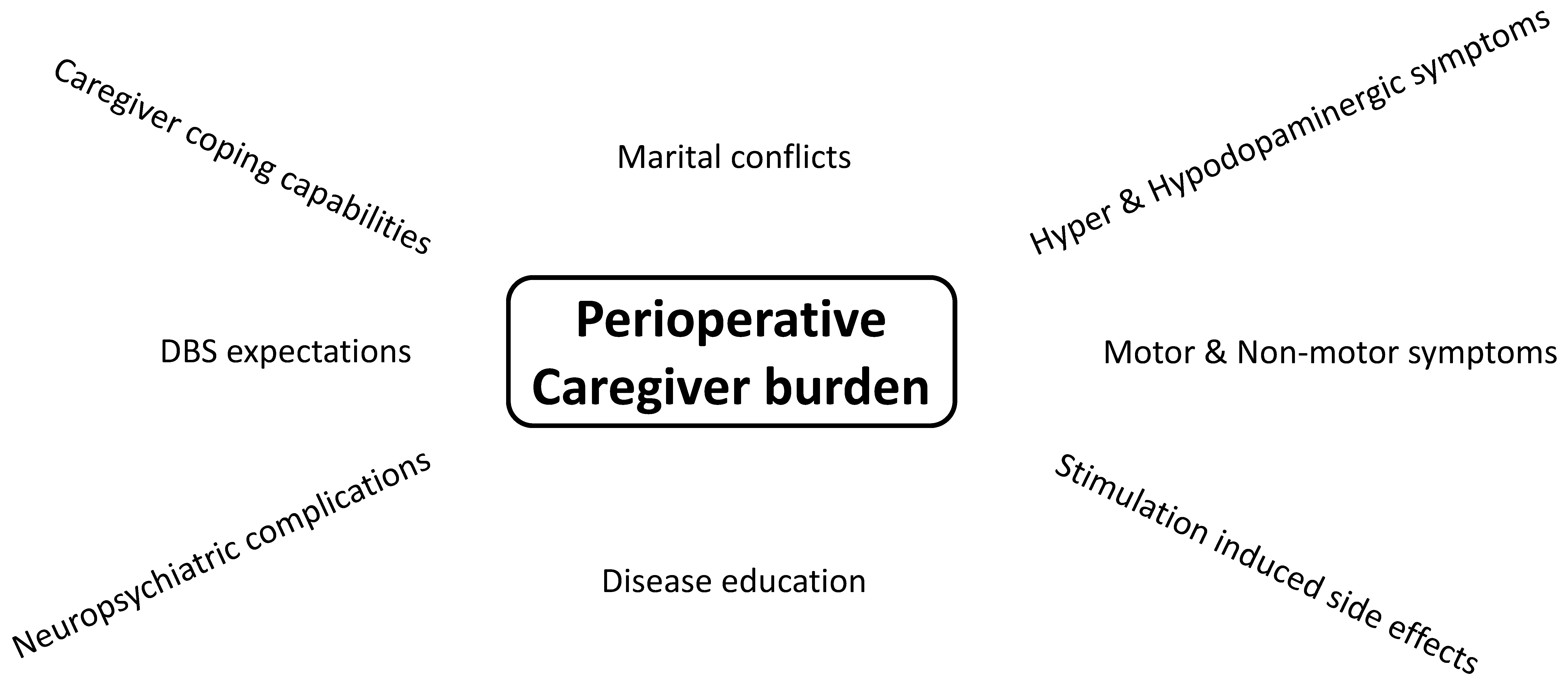
2. Preoperative Caregiver Burden—DBS Yes or No?
2.1. Caregiver Burden Due to Insufficient PD Symptom Control in Advanced Stages
2.2. Caregiver Expectations of DBS
3. Postoperative Aspects of Caregiver Burden
3.1. Caregiver Burden Due to PD Neuropsychiatric Symptoms after STN-DBS
3.2. Caregiver Burden Outcome after STN-DBS Implantation of PD Dependants
- The preexisting neuropsychiatric and medical condition of the caregivers themselves might play a role in the development of postoperative CB. In a prospective, longitudinal study of 25 patients and caregivers with follow-ups at 3 and 12 months, predictive factors for postoperative CB in a logistic regression model were assessed for both caregivers and PD patients [50]. Interestingly, at the 3-month follow-up, the caregivers were more indecisive about their own well-being but at the 1-year follow-up determined. There were caregivers with improved postoperative CB, often reporting “more freedom and better QOL” and that “PD patients showed less unpleasant side effects of medication”. Caregivers with worsening of postoperative CB reported “more conflicts between patients and caregivers”, “more anxiety concerning welfare of the patient” and “more sadness, stress and less freedom”. There were predicting risk factors of caregivers’ characteristics at baseline for increased postoperative CB, such as older age, greater depression, enhanced anxiety and lower quality of life of the caregivers [50]. This finding was interpreted as decreased ability of coping strategies or capabilities in those caregivers to adapt to the new postoperative situation [50]. Higher age of the caregiver is one important mediator of postoperative CB and caregivers’ satisfaction with the DBS operation. [46]. One has to remember that the caregiver grows older along with the PD patient and might also suffer from illnesses. The older the caregiver, the more exhausting the caregiving. Importantly, the preoperative BDI score is the predictor of postoperative caregiver depression one year after DBS surgery [46]. Thus is why the well-being of the caregiver should also be regularly addressed both pre- and postoperatively.
- The postoperative extent of neuropsychiatric symptoms within PD patients significantly influences the CB of their relatives, as described above. Interestingly, CB was not associated with the extent of motor symptom improvement [44] but the patient’s degree of apathy and depression [2,50]. In 64 PD patients and caregivers, postoperative caregiver burden, as measured by the Zarit Burden Interview (ZBI), was significantly related to PD patients’ Beck Depression Inventory (BDI) score, caregiver-rated attentional impulsiveness of PD patients, impaired PD set-shifting, prepotent PD inhibition, patients’ hypersexuality and dopaminergic medication dose [2]. Higher postoperative CB, indexed by ZBI, was correlated with lower relationship quality [2]. In a second step, it was then assessed whether the new onset of stimulation-induced neuropsychiatric side effects in the early perioperative period of 6 weeks was a predictive factor for increased postoperative CB. There was a significant difference between caregivers of PD patients with and without DBS-induced neuropsychiatric side effects. CB decreased after 6 weeks compared to baseline in caregivers of PD patients without DBS-induced neuropsychiatric side effects but increased in a considerable portion of caregivers of PD patients with DBS side effects [2].
- Postoperative marital conflicts due to changes in the relationship affect CB. DBS surgery profoundly changes caregiver responsibilities and disease-related symptoms due to the sudden relief of disability. Following STN-DBS, social maladjustment as a result of a dramatic improvement in clinical status and identity challenges can occur as part of the “burden of normality” syndrome [35]. Interestingly, partners of patients with device-aided therapies report more often changes in relationship satisfaction than patients and show more attachment-related avoidance [51]. Surprisingly, 65% of PD patients experience a conjugal crisis within 2 years of undergoing DBS [26]. Marital conflicts occurred in 17/24 couples, with three couples being divorced postoperatively and 33% of spouses becoming depressed within the 2-year follow-up [49]. Caregivers rate the change in their partnership 1 year post-DBS surgery as negative, with three main sources for marital disturbances: (1) neuropsychiatric changes, as described above with the new onset or ongoing neuropsychiatric symptoms in PD patients; (2) communication problems, e.g., caregivers feel uncertain of how to speak of residual PD symptomatology while the spouse feels healthy postoperatively; (3) caregivers’ overload of responsibilities for the partner and uncertainty about how the load of caregiving develops in the future [52]. About 54.5% of caregivers of PD patients with and without DBS suffer from caregiver overload [42]. During the time that partners spend together because of caring responsibilities, they feel emotionally more distanced [53]. These factors might contribute to an increase in marital conflicts [46]. Marital conflicts are further due to additional changes of social roles within the partnership postoperatively. On the one hand, there is a loss of the caregivers’ attention to the disease condition and the re-emerged responsibility in everyday duties for the PD patients, that PD patients might complain about [48]. Additionally, it was hypothesized that marital conflicts are due to role conflicts according to adaption to the new situation. On the other hand, PD patients rejected their spouse because they regained autonomy by DBS-induced motor improvement, but the spouse could not give up the caregiver role, overprotecting the patient and trying to maintain the patients’ dependency. Besides, patients were also rejected by their spouses, who expected them to resume a normal life with all their duties and social matters after the operation, whereas the patients still felt not able to do this [49]. However, some PD patients with good clinical outcomes also experience a restoration of the “old premorbid self” confirmed by their caregivers. Consequently, in those specific couples with satisfying DBS outcome, CB is lowered, and the relationship flourishes with greater socialization [26]
- DBS is a symptomatic, but not disease-modifying therapy; thus, in the long-term, disease progression with re-emergence of motor symptoms, onset of cognitive impairment and loss of autonomy of PD patients might result in the reoccurrence of increased CB [54]. This might contribute to the observation that CB increases in caregivers of some PD patients within the first 2 years after STN-DBS [55]. However, in another 2-year follow-up of younger (<65 years) and elderly (>65 years) STN-DBS patients, CB decreased in relatives of both patient groups, even in caregivers of elderly PD patients [56]. Observations of long-term results of chronically stimulated patients are of particular interest in the growing numbers of operated and aging PD patients. In terms of PD symptomatology, there is increasing knowledge of long-term effects [57]. There is evidence that subthalamic nucleus DBS improves motor function for up to 10 years, although the magnitude of improvement, particularly of levodopa-resistant symptoms, tends to decline over time. Dyskinesia, motor fluctuations and activities of daily living in off-periods remain improved at 5 years, but quality-of-life scores usually decrease [57]. Nonetheless, in an observational period of about 14 years after STN-DBS surgery, the risk for recurrent falls and psychotic symptoms is lower in PD patients with STN-DBS compared to patients without DBS surgery [58]. Overall, patients’ satisfaction with DBS remains high at long-term follow-up of more than 6 years [7,59]. In a small cohort of late-stage PD patients (Hoehn and Yahr stage ≥4) with marked motor and cognitive impairment treated with STN-DBS for >14 years, patients still benefit partly from stimulation [60]. Interestingly, in this specific patient cohort, caregivers had mild to moderate stable caregiver burden. When the medical decision was made to discontinue DBS stimulation due to the clinical impression of poor stimulation response in this advanced disease stage, PD patients’ global motor state and dysphagia declined with delayed onset, while caregivers’ QOL and CB worsened after DBS discontinuation slightly, but without statistical significance [60]. The observation of mild-moderate CB in this small cohort of very advanced PD patients with a long disease duration of up to 43 years is astonishing and could be due to acceptance of the CB and habituation to the caregiving situation. Still, long-term observations of CB are scarce and need to be obtained in larger cohorts of long-term caregivers (Figure 3).
4. Caregiver Burden in PD Patients with Globus Pallidus Internus Stimulation
5. What Is Next? Future Caregiving Challenges
6. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Zarit, S.H.; Todd, P.A.; Zarit, J.M. Subjective burden of husbands and wives as caregivers: A longitudinal study. Gerontologist 1986, 26, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Mosley, P.E.; Moodie, R.; Dissanayaka, N. Caregiver Burden in Parkinson Disease: A Critical Review of Recent Literature. J. Geriatr. Psychiatry Neurol. 2017, 30, 235–252. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.B.; Woo, H.; Lee, S.Y.; Cheon, S.M.; Kim, J.W. The burden of care and the understanding of disease in Parkinson’s disease. PLoS ONE 2019, 14, e0217581. [Google Scholar] [CrossRef]
- Adelman., R.D.; Tmanova, L.L.; Delgado, D.; Dion, S.; Lachs, M.S. Caregiver burden: A clinical review. JAMA 2014, 311, 1052–1060. [Google Scholar] [CrossRef] [PubMed]
- Henry, R.S.; Lageman, S.K.; Perrin, P.B. The relationship between Parkinson’s disease symptoms and caregiver quality of life. Rehabil. Psychol. 2020, 65, 137–144. [Google Scholar] [CrossRef]
- Thieken, F.; van Munster, M. Deriving Implications for Care Delivery in Parkinson’s Disease by Co-Diagnosing Caregivers as Invisible Patients. Brain Sci. 2021, 11, 1629. [Google Scholar] [CrossRef]
- Hitti, F.L.; Ramayya, A.G.; McShane, B.J.; Yang, A.I.; Vaughan, K.A.; Baltuch, G.H. Long-term outcomes following deep brain stimulation for Parkinson’s disease. J. Neurosurg. 2019, 132, 1–6. [Google Scholar] [CrossRef]
- Lau, B.; Meier, N.; Serra, G.; Czernecki, V.; Schuepbach, M.; Navarro, S.; Cornu, P.; Grabli, D.; Agid, Y.; Vidailhet, M.; et al. Axial symptoms predict mortality in patients with Parkinson disease and subthalamic stimulation. Neurology 2019, 92, e2559–e2570. [Google Scholar] [CrossRef]
- Giannini, G.; Francois, M.; Lhommée, E.; Polosan, M.; Schmitt, E.; Fraix, V.; Castrioto, A.; Ardouin, C.; Bichon, A.; Pollak, P.; et al. Suicide and suicide attempts after subthalamic nucleus stimulation in Parkinson disease. Neurology 2019, 93, e97–e105. [Google Scholar] [CrossRef]
- Lo Monaco, M.R.; Di Stasio, E.; Ricciardi, D.; Solito, M.; Petracca, M.; Fusco, D.; Onder, G.; Landi, G.; Zuccalà, G.; Liperoti, R.; et al. What about the caregiver? A journey into Parkinson’s disease following the burden tracks. Aging Clin. Exp. Res. 2021, 33, 991–996. [Google Scholar] [CrossRef]
- Klietz, M.; Schnur, T.; Drexel, S.; Lange, F.; Tulke, A.; Rippena, L.; Paracka, L.; Dressler, D.; Höglinger, G.U.; Wegner, F. Association of Motor and Cognitive Symptoms with Health-Related Quality of Life and Caregiver Burden in a German Cohort of Advanced Parkinson’s Disease Patients. Parkinsons Dis. 2020, 2020, 5184084. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Martin, P.; Rodriguez-Blazquez, C.; Forjaz, M.J.; Frades-Payo, B.; Agüera-Ortiz, L.; Weintraub, D.; Riesco, A.; Kurtis, M.M.; Chaudhuri, K.R. Neuropsychiatric symptoms and caregiver’s burden in Parkinson’s disease. Parkinsonism Relat. Disord. 2015, 21, 629–634. [Google Scholar] [CrossRef]
- Dlay, J.K.; Duncan, G.W.; Khoo, T.K.; Williams-Gray, C.H.; Breen, D.P.; Barker, R.A.; Burn, D.J.; Lawson, R.A.; Yarnall, A.J. Progression of Neuropsychiatric Symptoms over Time in an Incident Parkinson’s Disease Cohort (ICICLE-PD). Brain Sci. 2020, 10, 78. [Google Scholar] [CrossRef]
- Eichel, H.V.; Heine, J.; Wegner, F.; Rogozinski, S.; Stiel, S.; Groh, A.; Krey, L.; Höglinger, G.U.; Klietz, M. Neuropsychiatric Symptoms in Parkinson’s Disease Patients Are Associated with Reduced Health-Related Quality of Life and Increased Caregiver Burden. Brain Sci. 2022, 12, 89. [Google Scholar] [CrossRef] [PubMed]
- Macchi, Z.A.; Miyasaki, J.; Katz, M.; Galifianakis, N.; Sillau, S.; Kluger, B.M. Prevalence and Cumulative Incidence of Caregiver-Reported Aggression in Advanced Parkinson Disease and Related Disorders. Neurol. Clin. Pract. 2021, 11, e826–e833. [Google Scholar] [CrossRef]
- Rosqvist, K.; Schrag, A.; Odin, P.; CLaSP Consortium. Caregiver Burden and Quality of Life in Late Stage Parkinson’s Disease. Brain Sci. 2022, 12, 111. [Google Scholar] [CrossRef] [PubMed]
- Weiss, D.; Volkmann, J.; Fasano, A.; Kühn, A.; Krack, P.; Deuschl, G. Changing Gears–DBS For Dopaminergic Desensitization in Parkinson’s Disease? Ann. Neurol. 2021, 90, 699–710. [Google Scholar] [CrossRef]
- Schuepbach, W.M.; Rau, J.; Knudsen, K.; Volkmann, J.; Krack, P.; Timmermann, L.; Halbig, T.D.; Hesekamp, H.; Navarro, S.M.; Meier, N.; et al. Neurostimulation for Parkinson’s disease with early motor complications. N. Engl. J. Med. 2013, 368, 610–622. [Google Scholar] [CrossRef]
- Deuschl, G.; Schüpbach, M.; Knudsen, K.; Pinsker, M.O.; Cornu, P.; Rau, J.; Agid, Y.; Schade-Brittinger, C. Stimulation of the subthalamic nucleus at an earlier disease stage of Parkinson’s disease: Concept and standards of the EARLYSTIM-study. Parkinsonism Relat. Disord. 2013, 19, 56–61. [Google Scholar] [CrossRef]
- Schuepbach, W.M.M.; Tonder, L.; Schnitzler, A.; Krack, P.; Rau, J.; Hartmann, A.; Hälbig, T.D.; Pineau, F.; Falk, A.; Paschen, L.; et al. Quality of life predicts outcome of deep brain stimulation in early Parkinson disease. Neurology 2019, 92, e1109–e1120. [Google Scholar] [CrossRef]
- Vizcarra, J.A.; Situ-Kcomt, M.; Artusi, C.A.; Duker, A.P.; Lopiano, L.; Okun, M.S.; Espay, A.J.; Merola, A. Subthalamic deep brain stimulation and levodopa in Parkinson’s disease: A meta-analysis of combined effects. J. Neurol. 2019, 266, 289–297. [Google Scholar] [CrossRef]
- Kleiner-Fisman, G.; Herzog, J.; Fisman, D.N.; Tamma, F.; Lyons, K.E.; Pahwa, R.; Lang, A.E.; Deuschl, G. Subthalamic nucleus deep brain stimulation: Summary and meta-analysis of outcomes. Mov. Disord. 2006, 21, S290–S304. [Google Scholar] [CrossRef] [PubMed]
- Dafsari, H.S.; Silverdale, M.; Strack, M.; Rizos, A.; Ashkan, K.; Mahlstedt, P.; Sachse, L.; Steffen, J.; Dembek, T.A.; Visser-Vandewalle, V.; et al. Nonmotor symptoms evolution during 24 months of bilateral subthalamic stimulation in Parkinson’s disease. Mov. Disord. 2018, 33, 421–430. [Google Scholar] [CrossRef] [PubMed]
- Hiseman, J.P.; Fackrell, R. Caregiver Burden and the Nonmotor Symptoms of Parkinson’s Disease. Int. Rev. Neurobiol. 2017, 133, 479–497. [Google Scholar] [CrossRef] [PubMed]
- Engel, K.; Huckhagel, T.; Gulberti, A.; Pötter-Nerger, M.; Vettorazzi, E.; Hidding, U.; Choe, C.U.; Zittel, S.; Braaß, H.; Ludewig, P.; et al. Towards unambiguous reporting of complications related to deep brain stimulation surgery: A retrospective single-center analysis and systematic review of the literature. PLoS ONE 2018, 13, e0198529. [Google Scholar] [CrossRef]
- Thomson, C.J.; Segrave, R.A.; Racine, E.; Warren, N.; Thyagarajan, D.; Carter, A. “He’s Back so I’m Not Alone”: The Impact of Deep Brain Stimulation on Personality, Self, and Relationships in Parkinson’s Disease. Qual. Health Res. 2020, 30, 2217–2233. [Google Scholar] [CrossRef] [PubMed]
- Heine, J.; von Eichel, H.; Staege, S.; Höglinger, G.U.; Wegner, F.; Klietz, M. Relationship Satisfaction in People with Parkinson’s Disease and Their Caregivers: A Cross-Sectional Observational Study. Brain Sci. 2021, 11, 822. [Google Scholar] [CrossRef]
- Tröster, A.I. Some Clinically Useful Information that Neuropsychology Provides Patients, Carepartners, Neurologists, and Neurosurgeons About Deep Brain Stimulation for Parkinson’s Disease. Arch. Clin. Neuropsychol. 2017, 32, 810–828. [Google Scholar] [CrossRef]
- Prasad, S.; Bhattacharya, A.; Sahoo, L.K.; Batra, D.; Kamble, N.; Yadav, R.; Srinivas, D.; Pal, P.K. Knowledge, Attitude, and Perceptions about Deep Brain Stimulation for Parkinson’s Disease: Observations from a Single Indian Center. J. Mov. Disord. 2021, 14, 60–64. [Google Scholar] [CrossRef]
- Yen, K.; Miyasaki, J.M.; Waldron, M.; Yu, L.; Sankar, T.; Ba, F. DBS-Edmonton App, a Tool to Manage Patient Expectations of DBS in Parkinson Disease. Neurol. Clin. Pract. 2021, 11, e308–e316. [Google Scholar] [CrossRef]
- Oyama, G.; Okun, M.S.; Schmidt, P.; Tröster, A.I.; Nutt, J.; Go, C.L.; Foote, K.D.; Malaty, I.A. Deep brain stimulation may improve quality of life in people with Parkinson’s disease without affecting caregiver burden. Neuromodulation 2014, 17, 126–132. [Google Scholar] [CrossRef]
- Jakobs, M.; Helmers, A.K.; Synowitz, M.; Slotty, P.J.; Anthofer, J.M.; Schlaier, J.R.; Kloss, M.; Unterberg, A.W.; Kiening, K.L. A multicenter, open-label, controlled trial on acceptance, convenience, and complications of rechargeable internal pulse generators for deep brain stimulation: The Multi Recharge Trial. J. Neurosurg. 2019, 11, 822. [Google Scholar] [CrossRef] [PubMed]
- Witt, K.; Kuhn, J.; Timmermann, L.; Zurowski, M.; Woopen, C. Deep Brain Stimulation and the Search for Identity. Neuroethics 2013, 6, 499–511. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lanier-Bohan, E.M.; Heath, S.L. Patient and Caregiver Perspectives of Preoperative Teaching for Deep Brain Stimulation Surgery. J. Neurosci. Nurs. 2016, 48, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Flores Alves Dos Santos, J.; Tezenas du Montcel, S.; Gargiulo, M.; Behar, C.; Montel, S.; Hergueta, T.; Navarro, S.; Belaid, H.; Cloitre, P.; Karachi, C.; et al. Tackling psychosocial maladjustment in Parkinson’s disease patients following subthalamic deep-brain stimulation: A randomised clinical trial. PLoS ONE 2017, 12, e0174512. [Google Scholar] [CrossRef]
- Volkmann, J.; Daniels, C.; Witt, K. Neuropsychiatric effects of subthalamic neurostimulation in Parkinson disease. Nat. Rev. Neurol. 2010, 6, 487–498. [Google Scholar] [CrossRef]
- Castrioto, A.; Thobois, S.; Carnicella, S.; Maillet, A.; Krack, P. Emotional manifestations of PD: Neurobiological basis. Mov. Disord. 2016, 31, 1103–1113. [Google Scholar] [CrossRef]
- Mosley, P.E.; Breakspear, M.; Coyne, T.; Silburn, P.; Smith, D. Caregiver burden and caregiver appraisal of psychiatric symptoms are not modulated by subthalamic deep brain stimulation for Parkinson’s disease. NPJ Parkinsons Dis. 2018, 4, 12. [Google Scholar] [CrossRef]
- Abbes, M.; Lhommée, E.; Thobois, S.; Klinger, H.; Schmitt, E.; Bichon, A.; Castrioto, A.; Xie, J.; Fraix, V.; Kistner, A.; et al. Subthalamic stimulation and neuropsychiatric symptoms in Parkinson’s disease: Results from a long-term follow-up cohort study. J. Neurol. Neurosurg. Psychiatry 2018, 89, 836–843. [Google Scholar] [CrossRef]
- Karl, J.A.; Ouyang, B.; Colletta, K.; Verhagen Metman, L. Long-Term Satisfaction and Patient-Centered Outcomes of Deep Brain Stimulation in Parkinson’s Disease. Brain Sci. 2018, 8, 60. [Google Scholar] [CrossRef]
- Jackowiak, E.M.; Chou, K.L.; Patil, P.G.; Levin, E.; Leventhal, D. Delayed Dopamine Agonist Withdrawal Syndrome After Deep Brain Stimulation for Parkinson Disease. Neurol. Clin. Pract. 2021, 11, e35–e36. [Google Scholar] [CrossRef]
- Crespo-Burillo, J.A.; Rivero-Celada, D.; Saenz-de Cabezón, A.; Casado-Pellejero, J.; Alberdi-Viñas, J.; Alarcia-Alejos, R. Deep brain stimulation for patients with Parkinson’s disease: Effect on caregiver burden. Neurologia 2018, 33, 154–159. [Google Scholar] [CrossRef]
- Okunoye, O.; Kojima, G.; Marston, L.; Walters, K.; Schrag, A. Factors associated with hospitalisation among people with Parkinson’s disease—A systematic review and meta-analysis. Parkinsonism Relat. Disord. 2020, 71, 66–72. [Google Scholar] [CrossRef]
- Soileau, M.J.; Persad, C.; Taylor, J.; Patil, P.G.; Chou, K.L. Caregiver burden in patients with Parkinson disease undergoing deep brain stimulation: An exploratory analysis. J. Parkinsons Dis. 2014, 4, 517–521. [Google Scholar] [CrossRef] [PubMed]
- Lewis, C.J.; Maier, F.; Eggers, C.; Pelzer, E.A.; Maarouf, M.; Moro, E.; Zurowski, M.; Kuhn, J.; Woopen, C.; Timmermann, L. Parkinson’s disease patients with subthalamic stimulation and carers judge quality of life differently. Parkinsonism Relat. Disord. 2014, 20, 514–519. [Google Scholar] [CrossRef] [PubMed]
- van Hienen, M.M.; Contarino, M.F.; Middelkoop, H.A.M.; van Hilten, J.J.; Geraedts, V.J. Effect of deep brain stimulation on caregivers of patients with Parkinson’s disease: A systematic review. Parkinsonism Relat. Disord. 2020, 81, 20–27. [Google Scholar] [CrossRef]
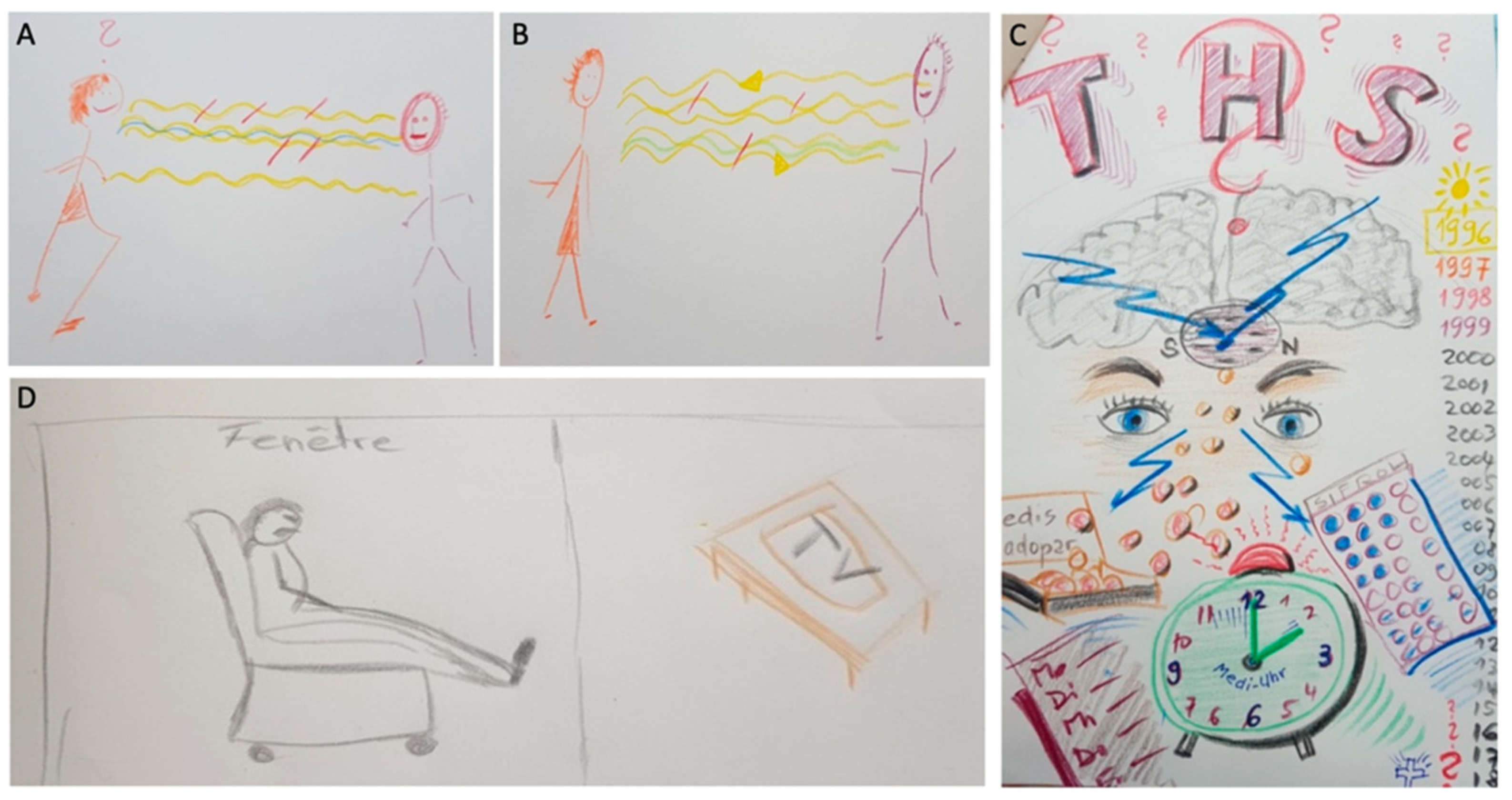
- Chacón Gámez, Y.M.; Brugger, F.; Biller-Andorno, N. Parkinson’s Disease and Deep Brain Stimulation Have an Impact on My Life: A Multimodal Study on the Experiences of Patients and Family Caregivers. Int. J. Environ. Res. Public Health 2021, 18, 9516. [Google Scholar] [CrossRef]
- Perozzo, P.; Rizzone, M.; Bergamasco, B.; Castelli, L.; Lanotte, M.; Tavella, A.; Torre, E.; Lopiano, L. Deep brain stimulation of subthalamic nucleus: Behavioural modifications and familiar relations. Neurol. Sci. 2001, 22, 81–82. [Google Scholar] [CrossRef]
- Schüpbach, M.; Gargiulo, M.; Welter, M.L.; Mallet, L.; Béhar, C.; Houeto, J.L.; Maltête, D.; Mesnage, V.; Agid, Y. Neurosurgery in Parkinson disease: A distressed mind in a repaired body? Neurology 2006, 66, 1811–1816. [Google Scholar] [CrossRef] [PubMed]
- Lewis, C.J.; Maier, F.; Horstkötter, N.; Eggers, C.; Visser-Vandewalle, V.; Moro, E.; Zurowski, M.; Kuhn, J.; Woopen, C.; Timmermann, L. The impact of subthalamic deep brain stimulation on caregivers of Parkinson’s disease patients: An exploratory study. J. Neurol. 2015, 262, 337–345. [Google Scholar] [CrossRef]
- Scharfenort, M.; Timpka, J.; Sahlström, T.; Henriksen, T.; Nyholm, D.; Odin, P. Close relationships in Parkinson´s disease patients with device-aided therapy. Brain Behav. 2021, 11, e02102. [Google Scholar] [CrossRef] [PubMed]
- Witt, K.; Stümpel, J.; Woopen, C. Caregiver burden and the medical ethos. Med. Health Care Philos. 2017, 20, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Vatter, S.; McDonald, K.R.; Stanmore, E.; Clare, L.; McCormick, S.A.; Leroi, I. A qualitative study of female caregiving spouses’ experiences of intimate relationships as cognition declines in Parkinson’s disease. Age Ageing 2018, 47, 604–610. [Google Scholar] [CrossRef] [PubMed]
- Constantinescu, R.; Eriksson, B.; Jansson, Y.; Johnels, B.; Holmberg, B.; Gudmundsdottir, T.; Renck, A.; Berglund, P.; Bergquist, F. Key clinical milestones 15 years and onwards after DBS-STN surgery-A retrospective analysis of patients that underwent surgery between 1993 and 2001. Clin. Neurol. Neurosurg. 2017, 154, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Jackowiak, E.; Maher, A.C.; Persad, C.; Kotagal, V.; Wyant, K.; Heston, A.; Patil, P.G.; Chou, K.L. Caregiver burden worsens in the second year after subthalamic nucleus deep brain stimulation for Parkinson’s disease. Parkinsonism Relat. Disord. 2020, 78, 4–8. [Google Scholar] [CrossRef]
- Vats, A.; Amit, A.; Doshi, P. A comparative study of bilateral subthalamic nucleus DBS in Parkinson’s disease in young versus old: A single institutional study. J. Clin. Neurosci. 2019, 70, 85–91. [Google Scholar] [CrossRef]
- Limousin, P.; Foltynie, T. Long-term outcomes of deep brain stimulation in Parkinson disease. Nat. Rev. Neurol. 2019, 15, 234–242. [Google Scholar] [CrossRef]
- Mahlknecht, P.; Peball, M.; Mair, K.; Werkmann, M.; Nocker, M.; Wolf, E.; Eisner, W.; Bajaj, S.; Quirbach, S.; Peralta, C.; et al. Has Deep Brain Stimulation Changed the Very Long-Term Outcome of Parkinson’s Disease? A Controlled Longitudinal Study. Mov. Disord. Clin. Pract. 2020, 7, 782–787. [Google Scholar] [CrossRef]
- Lin, H.Y.; Hasegawa, H.; Mundil, N.; Samuel, M.; Ashkan, K. Patients’ Expectations and Satisfaction in Subthalamic Nucleus Deep Brain Stimulation for Parkinson Disease: 6-Year Follow-up. World Neurosurg. 2019, 121, e654–e660. [Google Scholar] [CrossRef]
- Fabbri, M.; Zibetti, M.; Rizzone, M.G.; Giannini, G.; Borellini, L.; Stefani, A.; Bove, F.; Bruno, A.; Calandra-Buonaura, G.; Modugno, N.; et al. Should We Consider Deep Brain Stimulation Discontinuation in Late-Stage Parkinson’s Disease? Mov. Disord. 2020, 35, 1379–1387. [Google Scholar] [CrossRef]
- Lachenmayer, M.L.; Mürset, M.; Antih, N.; Debove, I.; Muellner, J.; Bompart, M.; Schlaeppi, J.A.; Nowacki, A.; You, H.; Michelis, J.P.; et al. Subthalamic and pallidal deep brain stimulation for Parkinson’s disease-meta-analysis of outcomes. NPJ Parkinsons Dis. 2021, 7, 77. [Google Scholar] [CrossRef] [PubMed]
- Duffley, G.; Lutz, B.J.; Szabo, A.; Wright, A.; Hess, C.W.; Ramirez-Zamora, A.; Zeilman, P.; Chiu, S.; Foote, K.D.; Okun, M.S.; et al. Home Health Management of Parkinson Disease Deep Brain Stimulation: A Randomized Clinical Trial. JAMA Neurol. 2021, 78, 972–981. [Google Scholar] [CrossRef] [PubMed]
- Hassan, A.; Wu, S.S.; Schmidt, P.; Malaty, I.A.; Dai, Y.F.; Miyasaki, J.M.; Okun, M.S. What are the issues facing Parkinson’s disease patients at ten years of disease and beyond? Data from the NPF-QII study. Parkinsonism Relat. Disord. 2012, 18, S10–S14. [Google Scholar] [CrossRef] [PubMed]
- Bouthour, W.; Mégevand, P.; Donoghue, J.; Lüscher, C.; Birbaumer, N.; Krack, P. Biomarkers for closed-loop deep brain stimulation in Parkinson disease and beyond. Nat. Rev. Neurol. 2019, 15, 343–352. [Google Scholar] [CrossRef]
- Bronte-Stewart, H.M.; Petrucci, M.N.; O’Day, J.J.; Afzal, M.F.; Parker, J.E.; Kehnemouyi, Y.M.; Wilkins, K.B.; Orthlieb, G.C.; Hoffman, S.L. Perspective: Evolution of Control Variables and Policies for Closed-Loop Deep Brain Stimulation for Parkinson’s Disease Using Bidirectional Deep-Brain-Computer Interfaces. Front. Hum. Neurosci. 2020, 14, 353. [Google Scholar] [CrossRef]
- van Halteren, A.D.; Munneke, M.; Smit, E.; Thomas, S.; Bloem, B.R.; Darweesh, S.K.L. Personalized Care Management for Persons with Parkinson’s Disease. J. Parkinsons Dis. 2020, 10, S11–s20. [Google Scholar] [CrossRef]
- Sharma, V.D.; Safarpour, D.; Mehta, S.H.; Vanegas-Arroyave, N.; Weiss, D.; Cooney, J.W.; Mari, Z.; Fasano, A. Telemedicine and Deep brain stimulation–Current practices and recommendations. Parkinsonism Relat. Disord. 2021, 89, 199–205. [Google Scholar] [CrossRef]
- van den Bergh, R.; Bloem, B.R.; Meinders, M.J.; Evers, L.J.W. The state of telemedicine for persons with Parkinson’s disease. Curr. Opin. Neurol. 2021, 34, 589–597. [Google Scholar] [CrossRef]
- Zhang, C.; Zhu, K.; Lin, Z.; Huang, P.; Pan, Y.; Sun, B.; Li, D. Utility of Deep Brain Stimulation Telemedicine for Patients With Movement Disorders During the COVID-19 Outbreak in China. Neuromodulation 2021, 24, 337–342. [Google Scholar] [CrossRef]
- Xu, J.; Wang, J.; Keith, S.; Zhang, M.; Yang, C.; Yuan, Q.; Qiu, Y.; Hu, X.; Wu, X. Management of Parkinson’s disease patients after DBS by remote programming: Preliminary application of single center during quarantine of 2019-nCoV. J. Neurol. 2021, 268, 1295–1303. [Google Scholar] [CrossRef]
- Marceglia., S.; Rossi, E.; Rosa, M.; Cogiamanian, F.; Rossi, L.; Bertolasi, L.; Vogrig, A.; Pinciroli, F.; Barbieri, S.; Priori, A. Web-based telemonitoring and delivery of caregiver support for patients with Parkinson disease after deep brain stimulation: Protocol. JMIR Res. Protoc. 2015, 4, e30. [Google Scholar] [CrossRef][Green Version]
- Hulshoff, M.J.; Book, E.; Dahodwala, N.; Tanner, C.M.; Robertson, C.; Marras, C. Current Knowledge on the Evolution of Care Partner Burden, Needs, and Coping in Parkinson’s Disease. Mov. Disord. Clin. Pract. 2021, 8, 510–520. [Google Scholar] [CrossRef] [PubMed]
- van Munster, M.; Stümpel, J.; Thieken, F.; Pedrosa, D.J.; Antonini, A.; Côté, D.; Fabbri, M.; Ferreira, J.J.; Růžička, E.; Grimes, D.; et al. Moving towards Integrated and Personalized Care in Parkinson’s Disease: A Framework Proposal for Training Parkinson Nurses. J. Pers. Med. 2021, 11, 623. [Google Scholar] [CrossRef] [PubMed]
- Tenison, E.; Smink, A.; Redwood, S.; Darweesh, S.; Cottle, H.; van Halteren, A.; van den Haak, P.; Hamlin, R.; Ypinga, J.; Bloem, B.R.; et al. Proactive and Integrated Management and Empowerment in Parkinson’s Disease: Designing a New Model of Care. Parkinsons Dis. 2020, 2020, 8673087. [Google Scholar] [CrossRef] [PubMed]
- Shahgholi, L.; De Jesus, S.; Wu, S.S.; Pei, Q.; Hassan, A.; Armstrong, M.J.; Martinez-Ramirez, D.; Schmidt, P.; Okun, M.S. Hospitalization and rehospitalization in Parkinson disease patients: Data from the National Parkinson Foundation Centers of Excellence. PLoS ONE 2017, 12, e0180425. [Google Scholar] [CrossRef]
- Archbold, P.G.; Stewart, B.J.; Greenlick, M.R.; Harvath, T. Mutuality and preparedness as predictors of caregiver role strain. Res. Nurs. Health 1990, 13, 375–384. [Google Scholar] [CrossRef]
- Mosley, P.E.; Robinson, K.; Dissanayaka, N.N.; Coyne, T.; Silburn, P.; Marsh, R.; Pye, D. A Pilot Trial of Cognitive Behavioral Therapy for Caregivers After Deep Brain Stimulation for Parkinson’s Disease. J. Geriatr. Psychiatry Neurol. 2021, 34, 454–465. [Google Scholar] [CrossRef]
- Berger, S.; Chen, T.; Eldridge, J.; Thomas, C.A.; Habermann, B.; Tickle-Degnen, L. The self-management balancing act of spousal care partners in the case of Parkinson’s disease. Disabil. Rehabil. 2019, 41, 887–895. [Google Scholar] [CrossRef]
- Hellqvist, C.; Dizdar, N.; Hagell, P.; Berterö, C.; Sund-Levander, M. Improving self-management for persons with Parkinson’s disease through education focusing on management of daily life: Patients’ and relatives’ experience of the Swedish National Parkinson School. J. Clin. Nurs. 2018, 27, 3719–3728. [Google Scholar] [CrossRef]
| Study | Design | PD Age, y ± SD | PD Sample Size | PD Duration, y ± SD | PD Sex (M/F) | Numbers of Caregivers Enrolled | Domain of Interest/Outcome Parameters |
|---|---|---|---|---|---|---|---|
| Duffley et al., 2021 | Parallel, randomized controlled trial | E: 65.0 ± 10.9 SOC: 64.1 ± 10.0 | E: 23 SOC: 19 | E: 12.0 ± 5.9 SOC: 11.5 ± 7.2 | E: 13/10 SOC: 11/8 | E: 22 SOC: 14 | Home health management of PD DBS, MSCI |
| Jackowiak et al., 2020 | Retrospective | 63.3 ± 8.1 | 35 | 10.6 ± 5.2 | 28/7 | 35 | 2-year follow-up after STN-DBS surgery, Caregiver Burden Inventory |
| Mosley et al., 2021 | Prospective clinical trial | - | - | - | - | 10 | Cognitive behavioral therapy for caregivers of PD patients with STN-DBS, ZBI, Parkinson’s Disease Questionnaire-Carer |
| Macchi et al., 2019 | Secondary analysis of randomized controlled trial | 70.6 ± 8.1 | 170 (20 with DBS) | 9.5 ± 6.5 | 70/119 | 170 (20 with PD Patients with DBS) | Physical/sexual aggression, ZBI Caregiver burden, Caregiver-perceived QOL, caregiver anxiety |
| Vats et al., 2019 | Retrospective | <65 y: 51.92 ± 8.2 >65>: 68.75 ± 3.05 | <65 y: 20 >65>: 20 | - - | <65 y: 13/7 >65 y: 7/5 | <65 y: 20 >65>: 20 | 2-year follow-up after STN-DBS surgery, ZBI |
| Mosley et al., 2018 | Prospective clinical trial | 62.2 ± 9.5 | 64 | 9.0 ± 5.2 | 48/16 | 64 | 26-week follow-up after STN-DBS surgery, ZBI, Relationship Quality Inventory, Barratt Impulsiveness Scale, Caregiver-rated Empathy Quotient |
| Witt et al., 2017 | Scientific contribution | - | 21 | - | 14/7 | 21 | Case study with semi-structured qualitative interviews, 1-year follow-up after DBS surgery, changes in partnership (psychological changes, communication problems, overload) |
| Crespo-Burillo et al., 2018 | Cross-sectional observational study | 66.2 ± 7.1 | 11 | 21.5 ± 17 | 7/4 | 11 | Zarit Caregiver Burden Interview, Hospital Anxiety and Depression Scale |
| Soileau et al., 2014 | Retrospective | 66.5 ± 7.2 | 12 | 10.6 ± 4.7 | 9/3 | 12 | 6-month follow-up after STN-DBS surgery, Caregiver Burden Inventory |
| Oyama et al., 2014 | Cross-sectional retrospective study | 62.6 ± 8.8 | 275 | 15.0 ± 6.3 | -/- | 275 | MSCI |
| Hassan et al., 2012 | Multicenter study | 67.8 ± 9.5 | 1835 (411 with DBS) | 15.1 ± 5.3 | 1141/693 | 1617 (88.1% of PD patients with regular caregiver) | PD patients with disease duration ≥ 10 years, MSCI |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gülke, E.; Pötter-Nerger, M. Caregiver Burden in Partners of Parkinsonian Patients with Deep Brain Stimulation. Brain Sci. 2022, 12, 238. https://doi.org/10.3390/brainsci12020238
Gülke E, Pötter-Nerger M. Caregiver Burden in Partners of Parkinsonian Patients with Deep Brain Stimulation. Brain Sciences. 2022; 12(2):238. https://doi.org/10.3390/brainsci12020238
Chicago/Turabian StyleGülke, Eileen, and Monika Pötter-Nerger. 2022. "Caregiver Burden in Partners of Parkinsonian Patients with Deep Brain Stimulation" Brain Sciences 12, no. 2: 238. https://doi.org/10.3390/brainsci12020238
APA StyleGülke, E., & Pötter-Nerger, M. (2022). Caregiver Burden in Partners of Parkinsonian Patients with Deep Brain Stimulation. Brain Sciences, 12(2), 238. https://doi.org/10.3390/brainsci12020238






