Abstract
The prevalence of temporomandibular disorders during childhood and adolescence reported until 2019 was between 7 and 68%. The aim of the present study is to determine the prevalence of temporomandibular disorders in children. This study, registered in The International Prospective Register of Systematic Reviews (CRD42022378908), assessed the prevalence of temporomandibular disorders in children and adolescents through the Research Diagnostic Criteria for Temporomandibular Disorders. Information was restricted based on the age and language of publication. In total, 985 records were identified through databases (EBSCO, PubMed, Web of Science, Scopus, and Cochrane Library) and 45 through grey literature sources (SciELO, Google Scholar, and Latindex). After removing duplicates and irrelevant records, 285 studies were screened, of which 32 had their full text assessed. Eight were included for qualitative and quantitative synthesis. The prevalence of muscle pain ranged from 0% to 31%; arthralgia ranged from 0.8% to 3.5%; disc displacement with reduction ranged from 0.4% to 14.4%; disc displacement without reduction ranged from 0% to 0.3%; osteoarthritis ranged from 0% to 0.6%; and osteoarthritis (in another context) ranged from 0% to 2.2%. This review highlights the varying prevalence of temporomandibular disorders (TMDs) in children and adolescents, with muscle pain as the most common symptom. Despite advancements in diagnostic criteria, gaps in imaging and psychological evaluation persist.
1. Introduction
Temporomandibular disorders have had a significant percentage increase in the population; however, in the last 4 years post-pandemic, the increase has included children and adolescents [1], having clinical manifestations in masticatory muscles, the condyle disc complex itself, and associated structures, in addition to psychological alterations such as stress and depression, with consequences such as joint noises, alteration of movement in the jaw, limitation of mouth opening, preauricular pain, facial pain, and headaches and jaw pain with movement, with progressive evolution [2]. The prevalence of TMD during childhood and adolescence reported until 2019 indicated a 7 to 68% occurrence of sleep bruxism in children, with clinical findings of temporomandibular and parafunctional disorders in primary or mixed dentition [3].
Manfredini et al. indicate that bruxism is considered physiologically normal in children up to 6 years of age. However, if it persists beyond this age, it may develop into a parafunctional behaviour known as awake bruxism, which requires parental observation and confirmation for diagnosis. Pain is one of the most frequent TMD symptoms observed during clinical examination in children, with a prevalence of 34% [1]. Overall, 12% of patients have an alteration in the maximum mouth opening. This condition is generated by ligamentous hypo-laxity, which produces a mandibular deflection that can be uni or bilateral, depending on where the over force in the ligaments is generated. Intracapsular disorders due to malocclusion should also not go unnoticed in the diagnosis [4]. The limitations of mouth opening can be caused by a muscular disorder or intercapsular disorder (8 to 10%) in children and adolescents. Joint sounds (25%) suggest the existence of disc displacement, demonstrated as crepitus or clicking (noise) [5]. The use of RDC/TMD (Research Diagnostic Criteria for Temporomandibular Disorders) enables the evaluation of clinical aspects of the temporomandibular joint, such as muscular pathologies, the disc condyle complex itself, and inflammatory processes in Axis I. Psychological alterations are effectively addressed by the RDC/TMD Axis II, which has been specifically refined by a Delphi group of global experts. This emphasizes the importance of employing appropriate and standardized methods to identify the presence of TMD. Such methods are crucial for improving the understanding of pathological aspects and enabling timely and preventive interventions. In particular, the evidence-based RDC/TMD is recommended for clinical and research applications in children and adolescents. It facilitates the identification of patients presenting with a spectrum of simple to complex TMD cases, thereby enhancing diagnostic precision and treatment strategies.
The American Society of Temporomandibular Joint (ASTMJS) proposes a classification of TMD in children that suggests dividing it into four categories: temporomandibular joint disorders, masticatory muscle disorders, headache disorders and associated structural disorders [6].
The evaluation process for children presenting with chronic craniofacial pain can be demanding and lengthy, and it is necessary to rule out serious diseases and help track the child’s physical, emotional and psychological responses to pain [7]. The most common clinical signs of TMD (on palpation) include muscle and joint tenderness, as well as limitations in jaw movements [8]. Additionally, patients often report associated symptoms such as bruxism and difficulty opening the mouth. Even though the signs and symptoms of TMD can lead to inflammatory (painful) disorders, joint disorders, such as disc displacements (nonpainful) [9], and muscle disorders, there is a small and clinically challenging population of children and adolescents who eventually become chronic pain patients with emotional distress [10]. The aim of the present study is to determine the prevalence of temporomandibular disorders in children and adolescents.
2. Materials and Methods
This systematic review respected the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) protocol and the International Prospective Register of Systematic Reviews (PROSPERO), number CRD42022378908.
2.1. PECO Question
The PECO question was as follows: In children and adolescents aged 7 to 17 years with temporomandibular disorders (P), how does the presence of at least one sign or symptom of TMD (E) compared with differences by age in those presenting TMJ symptoms (C) affect the determination of the prevalence of TMD (O)?
2.2. Search Strategy and Database Screening
The Rayyan QCRI program (Qatar Computing Research Institute, Doha, Qatar) was employed to identify eligible articles due to its efficiency in managing systematic reviews. This tool enhances the identification and screening of articles through features such as blind screening and intuitive tagging, which improve collaboration among researchers. Its compatibility with multiple databases ensures a comprehensive and systematic approach to data selection, crucial for high-quality reviews. The search strategy included screening various databases, including MEDLINE via PubMed, EMBASE via OVID, Web of Science, Scopus, Cochrane Library, and Clinical Trials, and five WHO regional bibliographic databases (AIM, LILACS, IMEMR, IMSEAR, WPRIM), as well as the Conference Proceedings Citation Index. A combination of keywords and terms was tailored for each database. The core keywords used were [“Temporomandibular disorders in children”] OR [“Prevalence of temporomandibular disorders”] OR [“TMD in childhood and adolescence”] AND [“Pediatric bruxism”] OR [“TMD diagnosis”] OR [“Temporomandibular joint disorders”]. To ensure a thorough review, the search also extended to grey literature sources such as OpenGrey, Google Scholar, and ProQuest Dissertations and Theses. This process was supplemented by a manual search of peer-reviewed journals containing relevant content.
2.3. Eligibility Criteria
Cross-sectional studies that evaluated the prevalence of TMD in children and adolescents through RDC/TMD were respected, with a restriction in the language of publication, accepting only English studies due to the relevance and number of articles available in this language. Very old studies were also excluded due to the possible use of outdated diagnostic methods.
Reports of painful and nonpainful TMD were accepted. The types of TMD considered were muscle pain, arthralgia, disc displacement (DD) and degenerative joint disease (DJD). We searched for primary studies with patients who had no signs or symptoms of orofacial pain or with a diagnosis of TMD.
The exclusion criteria were as follows: (1) studies that did not use RDC/TMD (studies published before 2018); (2) patients with orthopedic treatment or orthodontics; (3) immunosuppressed patients (diabetes, renal failure, syndromes associated with TMD; (4) annual monitoring data for TMD; (5) studies that did not provide separate data from pooled diagnoses; (6) studies that evaluated TMD in children and adolescents who were younger than 6 years or older than 18 years; and (7, 8) studies that could not be accessed fully (abstract only).
2.4. Quality Assessment
Blinded reviewers (AA, MC, YS, RP, ST) independently evaluated adherence to the Consolidated Standards of Reporting Trials (CONSORT). Consensus was achieved through discussions within the research team. For cases where agreement could not be reached, a third author (SL) acted as a mediator to resolve disagreements.
The answers were categorized as “yes”, “unclear” and “no”. The selection of articles was categorized as follows: studies that scored 45% on the questions rated “yes” were classified as “high RoB”; 49 to 65% as “moderate RoB”; and more than 66% as “low RoB”.
2.5. Inclusion Criteria
We included studies that evaluated the prevalence of TMD in children, including muscle pathologies and temporo mandibular joint pathologies. We evaluated muscle pain, disc displacement with reduction (DDwR), disc displacement without reduction (DDwoR), arthralgia, and osteoarthritis.
2.6. Statistical Analysis
Meta-Analysis
A meta-analysis of proportions was conducted using R Statistics software version 4.0.2 (The R Foundation, Vienna, Austria). The metaphor package was utilized for estimating the overall proportions. The confidence interval for individual studies was calculated using the Clopper–Pearson interval. To analyze statistical heterogeneity, the following parameters were calculated: Cochran’s Q (χ2), I-squared (I2), Tau-squared (τ2), and the prediction interval. Additionally, τ2 was calculated using the restricted maximum likelihood method. Given the anticipated distribution of true effect sizes among the included studies, a random effects model was applied.
3. Results
3.1. Selection of Studies
We found a total of n = 985 articles in the main electronic databases and n = 90 studies in the grey literature and reference lists. After removing duplicates, n = 450 records remained for the selection of titles and abstracts (phase 1), where n = 50 studies were eligible for full evaluation and full-text reading (phase 2), 188 studies were excluded (online resource 2), and 8 were included for qualitative and quantitative synthesis. In cases where the full text could not be accessed, two processes were used to confirm its exclusion: a search for articles in the library service (Universidad de Las Americas UDLA Biblioteca Carlos Larreategui) in collaboration with a specialist librarian and three attempts to contact the corresponding author or some other author of the article by email or through the website “research gate” for two consecutive weeks. In the absence of a response, the study was excluded as “full text not available” (Figure 1).
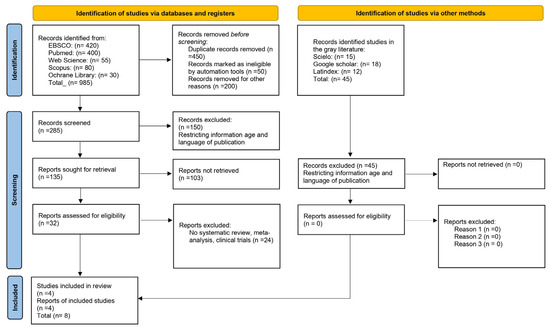
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines.
3.2. Study Characteristics
The 8 studies in children and adolescents included 11,134 females and 27,483 males aged 7 years/17 years [11,12,13]. We selected studies conducted in 16 different countries with sample sizes ranging from 400 to 11,500 participants. [14,15,16] (Table 1).

Table 1.
Summary of the Robins-E according to Consolidated Standards.
The studies met the methodological quality criteria: four studies were at low risk of bias, two were at moderate risk and two were at high risk. Adequate determination of size and subgroups was made, and it was determined that some of the studies did not separate multiple joint and muscle diagnoses of TMD, limiting some analyses (Table 2). The use of CD/DTM provided the following prevalence outcomes for children/adolescents: muscle pain (chewing muscles), 15%, arthralgia, 0.8 to 3.5%; DDwR, 0.4 to 14.4% [20,21,22]; DDwoR without limited aperture, 0 up to 0.3%; osteoarthritis, 0 to 0.6%; and osteoarthrosis, 0 up to 2.2% [23,24,25,26]. The prevalence of groups determined the following values in children/adolescents: arthralgia, 1.2%; DDwR, 5.4%; and DDwR with intermittent blocking, 0.6%. The diagnoses of DDwoR without limited aperture, DDwoR with limited aperture, DJD, and subluxation were included in this study; however, their prevalence was limited and reported only in studies with available data. These conditions were analyzed but were not the primary focus due to the low number of cases and high variability in reporting across studies. The high heterogeneity in the meta-analysis was due to the characteristics of the sample, methodological heterogeneity and risk of bias. With random selection, the overall prevalence of TMD in children and adolescents meeting the CD/DTM was 11%, 8.3% for the DD group, and 0.4% for the DJD group (Table 3).

Table 2.
Summary of the risk of bias.

Table 3.
Systematic review.
In the meta-analysis results, muscle pain was identified as the most prevalent disorder, with a prevalence of 15% (95% CI: 9.6–19.4), followed by general joint diagnoses at 11.3% (95% CI: 7.6–16.4). Disc displacements showed an overall prevalence of 8.3% (95% CI: 5.2–13.0), with those involving reduction being more common (7.4%, 95% CI: 2.3–21.2). In contrast, disc displacements without reduction and degenerative disorders such as osteoarthritis (0.3%, 95% CI: 0.1–1.0) and osteoarthrosis (0.2%, 95% CI: 0.0–1.0) were rare. The estimates showed high heterogeneity across most categories, except for low-prevalence diagnoses, where heterogeneity was minimal, Table 4.

Table 4.
Summary of prevalence of temporomandibular joint disorders from meta-analysis.
4. Discussion
The systematic review and meta-analysis provided an assessment of the prevalence of temporomandibular disorders in children and adolescents, revealing that muscle pain was the most frequently observed TMD condition [17,18,27]. The most used tool to determine the diagnosis was DC/TMD Axis II [19,28,29]; its design facilitated the selection of studies providing adequate visualization [30,31] and correct identification of symptoms, including myalgias in masticator muscles and masseters, temporal, external and internal pterygoids, trapezius [32,33] and scalene evaluated with the VAS pain scale and Rocabado’s pain map, which helped with the clarity of the clinical diagnoses. The alterations in the condyle–disc complex were minimal, with inflammatory processes in the temporomandibular joint showing low and clinically insignificant prevalence. However, psychological factors were identified as relevant and warrant further investigation [34]. These factors, which are often overlooked in the early stages of the condition, must be considered, as they may contribute to the persistence and exacerbation of symptoms. [35] The RDC/TMD criteria were created in 1992 for research purposes, while the DC/TMD (2014) broadens the spectrum by including clinical observations; they are reliable and establish a valuable clinical standardization for the diagnosis of TMD [36] such as arthralgia, DDwR and DJD (osteoarthritis, osteoarthritis) [37].
The age of children and adolescents was variable in the results; however, 11.3% presented some symptom of TMD. When radiographic magnets were included to diagnose DD and DJD, the prevalence percentages of these pathologies were irrelevant [38,39].
To determine and confirm diagnoses, the use of DC/TMD is recommended, as it considers joint sounds within short time frames (30 days) [40] and reports of crepitus as clinical signs that can better guide their differential diagnosis. It should be clarified that parafunctions in children between 3 and 8 years old are considered physiological, and they are even factors that stimulate facial growth. Outside this range, they become parafunctions, triggering joint pathologies if they are not diagnosed and treated. It should be noted that clinical examination protocols have little validity for diagnosing DDwoR compared to magnetic resonance imaging (MRI) [41] and the drawback found is that MRI is only used for cases with diagnostic difficulties. This leads to the idea that imaging may increase the prevalence rate in these cases by providing a more accurate form of verification. Unfortunately, there were few articles that used this diagnostic method [42]. The criteria for CD/TMD for children/adolescents found osteoarthritis and osteoarthritis in the categories of low prevalence, indicating that they are less frequent disorders. It is reiterated that DD can be considered a false negative diagnosis, and the clinical signs must be confirmed with imaging tests [43]. The condylar position is difficult to determine through clinical history alone; the only reliable method to assess it is through complementary radiographic examinations, such as computed tomography (CT) and MRI [44]. Patients with hypermobility and/or subluxation should confirm their diagnosis by avoiding pathologies such as alterations in the opening and closing of the mouth that, in the long term, can generate problems of joint adhesions or ankylosis [45]. According to preliminary studies, the prevalence of DDwR increases with age: the prevalence of symptomatic DD is approximately 6%, increasing in the population between 16 and 19 years of age [46].
Prevalence estimates in most of the included studies were obtained from children and adolescents registered with the Ministry of Education and the national health system, ensuring a diverse sample from public and private schools, as well as multicenter, randomly selected populations. It should be noted that the sample did not originate from orofacial pain treatment clinics to avoid potential data bias [47].
Marpaung’s study included only children and adolescents and raised awareness of high rates of some specific types of TMD [18,48]. Appropriate strategies for early and correct diagnosis are crucial for effective treatment management. Most cases are asymptomatic, with patients often reporting only mild discomfort due to joint noise. According to the literature, only a small proportion of affected adolescents seek treatment for the condition. When pain is present, it is typically exacerbated by activities such as chewing or other jaw movements [49]. Some dentists and specialists advise their patients that the symptoms generally resolve over time due to the natural and harmless progression of disc disorders, but cases of persistent symptomatology are a concern, where conservative non-surgical treatment is the main option [50]. In this review, the limitations identified include the scarcity of studies that report the psychological aspects of temporomandibular disorders. Although it has been established that errors in the diagnosis and progression of the disorder can be influenced by conditions such as headaches and depression, it is recommended that more studies be conducted that consider these factors.
This systematic review examined the prevalence of temporomandibular disorders (TMDs) in children and adolescents aged 7 to 17. It focused on the presence of at least one sign or symptom, such as muscle pain, arthralgia or disc displacement, while comparing differences in symptom presentation across age groups. The findings showed a wide range of symptom prevalences, with muscle pain being the most common symptom (up to 31%) and disc displacement with reduction frequently observed in older adolescents (up to 14.4%) [51]. These results highlight the need to standardize diagnostic methods and consider factors like age in clinical assessments.
Strengths and Limitations
Among the main strengths of this study is the use of a well-structured protocol based on PRISMA guidelines, along with registration in PROSPERO, which ensures a robust and transparent methodology. Additionally, the literature search covered multiple recognized databases and grey literature sources, increasing the comprehensiveness of the data collected. Advanced tools such as the Rayyan QCRI program were also used for article selection and evaluation, improving the efficiency of the review process and minimizing biases in study selection.
However, an important limitation was the exclusion of articles published in languages other than English, which may have restricted the generalization of findings and increased the risk of systematic bias. Additionally, the limited use of advanced imaging techniques, such as magnetic resonance imaging, and the lack of integration of more detailed psychological assessments represent significant methodological gaps. Additional limitations of the manuscript include the absence of forest plots, attributed to the inconsistency and lack of comparable data across studies, which made it unfeasible to generate meaningful results without risking misinterpretation. Finally, the high heterogeneity in the reported data and selection bias in some included studies underscore the need for more standardized and consistent approaches in future research.
5. Conclusions
This systematic review highlights the varying prevalence of temporomandibular disorders (TMDs) in children and adolescents, emphasizing muscle pain as the most common symptom. Despite advancements in diagnostic criteria, gaps in imaging utilization and psychological assessment remain. Future studies should focus on standardized methodologies and longitudinal data to better understand TMD etiology and progression. These findings underscore the importance of early diagnosis and tailored interventions to mitigate the impact of TMD in younger populations.
Author Contributions
Conceptualization, B.V.R. and A.P.-J.; methodology, A.A.M., A.P.-J., J.S.-P., M.C.T., S.L.L. and J.S.-P.; software, B.V.R. and L.C.-B.; validation, A.A.M., M.C.T., S.L.L., A.P.-J., J.S.-P. and B.V.R.; formal analysis, R.V.T. and B.V.R.; investigation, R.V.T., A.A.M., M.C.T. and S.L.L.; resources, A.A.M.; data curation, B.V.R., A.P.-J., L.C.-B., A.P.-J. and J.S.-P.; writing—original draft preparation, A.A.M., M.C.T. and S.L.L.; writing—review and editing, B.V.R., L.C.-B., A.P.-J. and J.S.-P.; visualization, A.A.M., M.C.T. and S.L.L.; supervision, B.V.R. and A.P.-J.; project administration, A.A.M.; funding acquisition, A.A.M. and B.V.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Acknowledgments
The authors would like to express their special thanks to Universidad de Las Américas.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| TMDs | Temporo Mandibular Disorders |
| TMJ | Temporo Mandibular Joint |
| CD/DTM | Diagnostic Criteria for Temporomandibular Disorders |
| RDC/TMD | Research Diagnostic Criteria for Temporo Mandibular Disorders |
| ADDR | Anterior Disc Displacement with Reduction |
| DDwR | Disc Displacement with Reduction |
| DdwoR | Disc Displacement Without Reduction |
| DJD | Degenerative Diseases Temporomandibular Joint |
| DD | Disc Displacement |
| VAS | Visual Analogue Scale |
| MRI | Magnetic Resonance Imaging |
| CD | Computed Tomography |
References
- Mélou, C.; Sixou, J.L.; Sinquin, C.; Chauvel-Lebret, D. Temporomandibular disorders in children and adolescents: A review. Arch. Pediatr. 2023, 30, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Al-Khatieeb, M.M.; Nissan, L.M.; Al-Labban, Y.R.; Abid, M. Occlusal Features and Temporomandibular Joint Disorder: A Cross-Sectional Study. Int. J. Dent. 2024, 8715166. [Google Scholar] [CrossRef] [PubMed]
- Almasan, O.; Corneliu, D.; Buduru, S. Disc Displacement of the Temporomandibular Joint and Facial Asymmetry in Children and Adolescents: A Systematic Review and Meta-Analysis. Children 2022, 9, 1297. [Google Scholar] [CrossRef] [PubMed]
- Al-Khotani, A.; Naimi-Akbar, A.; Albadawi, E.; Ernberg, M.; Hedenberg, B.; Christidis, N. Prevalence of diagnosed temporomandibular disorders among Saudi Arabian children and adolescents. J. Headache Pain 2016, 17, 41. [Google Scholar] [CrossRef]
- Bender, S.D. Temporomandibular disorders, facial pain, and headaches. Headache 2012, 52 (Suppl. 1), 22–25. [Google Scholar] [CrossRef]
- Bertoli, F.M.P.; Bruzamolin, C.D.; Pizzatto, E.; Losso, E.M.; Brancher, J.A.; de Souza, J.F. Prevalence of diagnosed temporomandibular disorders: A cross-sectional study in Brazilian adolescents. PLoS ONE 2018, 13, e0192254. [Google Scholar] [CrossRef]
- Bulanda, S.; Ilczuk-Rypuła, D.; Nitecka-Buchta, A.; Nowak, Z.; Baron, S.; Postek-Stefańska, L. Sleep Bruxism in Children: Etiology, Diagnosis, and Treatment—A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 9544. [Google Scholar] [CrossRef]
- Christidis, N.; Ndanshau, E.; Sandberg, A.; Tsilingaridis, G. Prevalence and treatment strategies regarding temporomandibular disorders in children and adolescents—A systematic review. J. Oral Rehabil. 2019, 46, 291–301. [Google Scholar] [CrossRef]
- De Baat, C.; Verhoeff, M.; Ahlberg, J.; Manfredini, D.; Winocur, E.; Zweers, P.; Rozema, F.; Vissink, A.; Lobbezoo, F. Medications and addictive substances potentially inducing or attenuating sleep bruxism and/or awake bruxism. J. Oral Rehabil. 2021, 48, 343–354. [Google Scholar] [CrossRef]
- De Oliveira Reis, L.; Ribeiro, R.A.; Martins, C.C.; Devito, K.L. Association between bruxism and temporomandibular disorders in children: A systematic review and meta-analysis. Int. J. Paediatr. Dent. 2019, 29, 585–595. [Google Scholar] [CrossRef]
- De Melo Júnior, P.C.; Aroucha, J.; Arnaud, M.; Lima, M.; Gomes, S.; Ximenes, R.; Rosenblatt, A.; Caldas, A.d.F. Prevalence of TMD and level of chronic pain in a group of Brazilian adolescents. PLoS ONE 2019, 14, e0205874. [Google Scholar] [CrossRef] [PubMed]
- Valesan, L.F.; Da-Cas, C.D.; Réus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; de Souza, B.D.M. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 441–453. [Google Scholar] [CrossRef] [PubMed]
- Storari, M.; Aprile, M.; Denotti, G.; Viscuso, D. Long-term efficacy of onabotulinum toxin in treating persistent myofascial pain and masticatory muscles hypertone in an adolescent with bruxism. A 7-year follow-up case report. Eur. J. Pediatr. Dent. 2022, 23, 291–294. [Google Scholar]
- Checinska, K.; Turosz, N.; Brozowska, A.; Chlubek, D.; Sikora, M. Current Clinical Research Directions on Temporomandibular Joint Intra-Articular Injections: A Mapping Review. J. Clin. Med. 2023, 12, 4655. [Google Scholar] [CrossRef] [PubMed]
- Hee Lee, Y. Relationship Analogy Between Sleep Bruxism and Temporomandibular Disorders in Children: A Narrative Review. Children 2022, 9, 1466. [Google Scholar] [CrossRef]
- Khayat, N.; Winocur, E.; Emodi, A.; Friedman, P.; Gafni, Y.; Shpack, N. The prevalence of posterior crossbite, deep bite, and sleep or awake bruxism in temporomandibular disorder (TMD) patients compared to a non-TMD population: A retrospective study. Cranio 2021, 39, 398–404. [Google Scholar] [CrossRef]
- Macri, M.; Murmura, G.; Scarano, A.; Festa, F. Prevalence of temporomandibular disorders and its association with malocclusion in children: A transversal study. Front. Public Health 2022, 10, 860833. [Google Scholar] [CrossRef]
- Marpaung, C.; van Selms, M.K.A.; Lobbezoo, F. Temporomandibular joint anterior disc displacement with reduction in a young population: Prevalence and risk indicators. Int. J. Pediatr. Dent. 2018, 29, 66–73. [Google Scholar] [CrossRef]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Fiorillo, L.; Cervino, G.; Cicciù, M. Prevalence of temporomandibular disorders in children and adolescents evaluated with Diagnostic Criteria for Temporomandibular Disorders: A systematic review with meta-analysis. J. Oral Rehabil. 2023, 50, 522–530. [Google Scholar] [CrossRef]
- Khojastepour, L.; Omidi, M.; Vojdani, M.; Bagheri, K. Investigating Possible Correlation between Condylar Asymmetry and Clinical Dysfunction Indices in Patients with Temporomandibular Dysfunction Using Cone-Beam Computed Tomographic. J. Cranio-Maxillofac. Surg. 2019, 47, 438–442. [Google Scholar] [CrossRef]
- Lobbezoo, F.; Ahlberg, J.; Raphael, K.; Wetselaar, P.; Glaros, A.; Kato, T.; Santiago, V.; Winocur, E.; De Laat, A.; De Leeuw, R.; et al. International consensus on the assessment of bruxism: Report of a work in progress. J. Oral Rehabil. 2018, 45, 837–844. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Liu, M.; Zhang, Q.; Tian, Y.; Wang, L.; Yan, X.; Ren, D.; Yuan, X. Wnt/β-catenin signaling pathway is activated in the progress of mandibular condylar cartilage degeneration and subchondral bone loss induced by overloaded functional orthopedic force (OFOF). Heliyon 2022, 8, e10847. [Google Scholar] [CrossRef] [PubMed]
- Dinsdale, A.; Thomas, L.; Forbes, R.; Treleaven, J. Is proprioception affected in those with persistent intra-articular temporomandibular disorders? A cross-sectional study exploring joint position sense and force sense of the jaw. Musculoskelet. Sci. Pract. 2023, 69, 102904. [Google Scholar] [CrossRef] [PubMed]
- List, T.; Jensen, R.H. Temporomandibular disorders: Old ideas and new concepts. Cephalalgia 2017, 37, 692–704. [Google Scholar] [CrossRef]
- Lövgren, A.; Österlund, C.; Ilgunas, A.; Lampa, E.; Hellström, F. A high prevalence of TMD is related to somatic awareness and pain intensity among healthy dental students. Acta Odontol. Scand. 2018, 76, 387–393. [Google Scholar] [CrossRef]
- Loster, J.; Osiewicz, M.; Groch, M.; Ryniewicz, W.; Wieczorek, A. The prevalence of TMD in polish young adults. J. Prosthodont. 2015, 26, 284–288. [Google Scholar] [CrossRef]
- Manfredini, D.; Lobbezoo, F. Sleep bruxism and temporomandibular disorders: A scoping review of the literature. J. Dent. 2021, 111, 103711. [Google Scholar] [CrossRef]
- Michalek-Zrabkowska, M.; Wieckiewicz, M.; Smardz, J.; Gac, P.; Poreba, R.; Wojakowska, A.; Mazur, G.; Martynowicz, H. Determination of Inflammatory Markers, Hormonal Disturbances, and Sleepiness Associated with Sleep Bruxism Among Adults. Nat. Sci. Sleep 2020, 12, 969–979. [Google Scholar] [CrossRef]
- Miettinen, T.; Myllymaa, K.; Muraja-Murro, A.; Westeren-Punnonen, S.; Hukkanen, T.; Töyräs, J.; Lappalainen, R.; Mervaala, E.; Sipilä, K.; Myllymaa, S. Polysomnographic scoring of sleep bruxism events is accurate even in the absence of video recording but unreliable with EMG-only setups. Sleep Breath. 2020, 24, 893–904. [Google Scholar] [CrossRef]
- Nicot, R.; Chung, K.; Vieira, A.R.; Raoul, G.; Ferri, J.; Sciote, J. Condyle Modeling Stability, Craniofacial Asymmetry and ACTN3 Genotypes: Contribution to TMD Prevalence in a Cohort of Dentofacial Deformities. PLoS ONE 2020, 15, e0236425. [Google Scholar] [CrossRef]
- Lin, L.H.; Lin, T.Y.; Chang, K.V.; Wu, W.T.; Özçakar, L. Muscle energy technique to reduce pain and disability in cases of non-specific neck pain: A systematic review and meta-analysis of randomized controlled trials. Heliyon 2023, 9, e22469. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.S.; Zaghi, S.; Ghodousi, N.; Peterson, C.; Silva, D.; Lavigne, G.J.; Yoon, A.J. Determinants of probable sleep bruxism in a pediatric mixed dentition population: A multivariate analysis of mouth vs. nasal breathing, tongue mobility, and tonsil size. Sleep Med. 2021, 77, 7–13. [Google Scholar] [CrossRef]
- Ooi, K.; Inoue, N.; Matsushita, K.; Mikoya, T.; Minowa, K.; Kawashiri, S.; Tei, K. Relations between Anterior Disc Displacement and Maxillomandibular Morphology in Skeletal Anterior Open Bite with Changes to the Mandibular Condyle. Br. J. Oral Maxillofac. Surg. 2020, 58, 1084–1090. [Google Scholar] [CrossRef]
- Paduano, S.; Bucci, R.; Rongo, R.; Silva, R.; Michelotti, A. Prevalence of temporomandibular disorders and oral parafunctions in adolescents from public schools in Southern Italy. Cranio 2018, 38, 370–375. [Google Scholar] [CrossRef]
- Quirino, L.; de Toledo, I.P.; Pupo, Y.; Porporatti, A.; De Luca, C.G.; Zwir, L.; Guerra, E. Prevalence of degenerative joint disease of the temporomandibular joint: A systematic review. Clin. Oral Investig. 2019, 23, 2475–2488. [Google Scholar]
- Polmann, H.; Domingos, F.L.; Melo, G.; Stuginski-Barbosa, J.; Guerra, E.; Porporatti, A.; Dick, B.D.; Flores-Mir, C.; Canto, G.D.L. Association between sleep bruxism and anxiety symptoms in adults: A systematic review. J. Oral Rehabil. 2019, 46, 482–491. [Google Scholar] [CrossRef]
- Zheng, H.; Shi, L.; Lu, H.; Liu, Z.; Yu, M.; Wang, Y.; Wang, H. Influence of edentulism on the structure and function of temporomandibular joint. Heliyon 2023, 9, e20307. [Google Scholar] [CrossRef]
- Pupo, Y.; Pantoja, L.; Veiga, F.; Stechman-Neto, J.; Zwir, L.; Farago, P.; De Luca, C.; Porporatti, A. Diagnostic validity of clinical protocols to assess temporomandibular disk displacement disorders: A meta-analysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 122, 572–586. [Google Scholar] [CrossRef]
- Reis, P.; Laxe, L.; Lacerda-Santos, R.; Münchow, E.A. Distribution of anxiety and depression among different subtypes of temporomandibular disorder: A systematic review and meta-analysis. J. Oral Rehabil. 2022, 49, 754–767. [Google Scholar] [CrossRef]
- Rongo, R.; Ekberg, E.; Nilsson, I.M.; Al-Khotani, A.; Alstergren, P.; Conti, P.; Durham, J.; Goulet, J.P.; Hirsch, C.; Kalaykova, S.; et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for children and adolescents: An international Delphi study—Part 1-Development of Axis I. J. Oral Rehabil. 2021, 48, 836–845. [Google Scholar] [CrossRef] [PubMed]
- Nassar, H.; Al-Dabbagh, N.; Aldabbagh, R.; Albahiti, M.; Jadu, F.M.; Qutob, A.; Mawardi, H. Dental follow-up and maintenance index: The development of a novel multidisciplinary protocol. Heliyon 2020, 6, e03954. [Google Scholar] [CrossRef] [PubMed]
- Santana-Mora, U.; López-Cedrún, J.; Suárez-Quintanilla, J.; Varela-Centelles, P.; Mora, M.J.; Da Silva, J.L.; Figueiredo-Costa, F.; Santana-Penín, U. Asymmetry of Dental or Joint Anatomy or Impaired Chewing Function Contribute to Chronic Temporomandibular Joint Disorders. Ann. Anat. Anat. Anz. 2021, 238, 151793. [Google Scholar] [CrossRef]
- Walker, B.M.; Donnell, C.C. Does dental rehabilitation under general anaesthetic contribute to the development of temporomandibular disorders in children and adolescents? A scoping review. J. Oral Rehabil. 2023, 50, 902–913. [Google Scholar] [CrossRef] [PubMed]
- Schmitter, M.; Essig, M.; Seneadza, V.; Balke, Z.; Schroder, J.; Rammelsberg, P. Prevalence of clinical and radiographic signs of osteoarthrosis of the temporomandibular joint in an older person community. Dentomaxillofacial Radiol. 2010, 39, 231–234. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Groupdagger. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Toh, A.; Chan, J.; Leung, Y. Mandibular Asymmetry as a Possible Etiopathology Factor in Temporomandibular Disorder: A Prospective Cohort of 134 Patients. Clin. Oral Investig. 2021, 25, 4445–4450. [Google Scholar] [CrossRef]
- Chen, K.; Zhang, Z.; Jiang, J.; Wang, J.; Wang, J.; Sun, Y.; Xu, X.; Guo, C. Prediction of condylar movement envelope surface based on facial morphology. Heliyon 2023, 9, e17769. [Google Scholar] [CrossRef]
- Asquini, G.; Devecchi, V.; Borromeo, G.; Viscuso, D.; Morato, F.; Locatelli, M.; Falla, D. Predictors of pain reduction following a program of manual therapies for patients with temporomandibular disorders: A prospective observational study. Musculoskelet. Sci. Pract. 2022, 62, 102634. [Google Scholar] [CrossRef]
- Vlăduțu, D.; Popescu, S.; Mercuț, R.; Ionescu, M.; Scrieciu, M.; Glodeanu, A.; Stănuși, A.; Rîcă, A.; Mercuț, V. Associations between Bruxism, Stress, and Manifestations of Temporomandibular Disorder in Young Students. Int. J. Environ. Res. Public Health 2022, 29, 5415. [Google Scholar] [CrossRef]
- Xie, Q.; Yang, C.; He, D.; Cai, X.; Ma, Z.; Shen, Y.; Abdelrehem, A. Will Unilateral Temporomandibular Joint Anterior Disc Displacement in Teenagers Lead to Asymmetry of Condyle and Mandible? A Longitudinal Study. J. Cranio-Maxillofac. Surg. 2016, 44, 590–596. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).