Featured Application
The goal of leukocyte and platelet-rich plasma (L-PRP) research is to apply it in clinical practice to treat traumatic dental events, such as tooth avulsions. Topical treatment with L-PRP before tooth replantation may provide a better environment for pulpal healing for severely injured teeth.
Abstract
This study aimed to evaluate the effect of leukocyte and platelet-rich plasma (L-PRP) on the pulpal healing process following immediate and intentionally delayed tooth replantation in mice. After the maxillary first molars of 3-week-old mice were extracted, the teeth were immersed for 1 min [immediate reimplantation (IR)] or 30 min [intentionally delayed reimplantation (IDR)] in phosphate-buffered saline (PBS) solution. The alveolar socket was filled with or without 1.5 μL of L-PRP [experimental or control groups (EG or CG)] followed by tooth replantation. Samples were collected from day 1 to week 4 after the operation, processed for histology, and evaluated by immunohistochemistry for Nestin and Ki-67 expression. Quantitative analysis revealed positive Nestin staining during pulpal healing in the EG at week 1 following IR and week 2 following IDR. Hard tissue deposition was significantly increased in the EG after IR at week 2. Cell proliferation was higher in the EG compared with that in the CG at week 1 and significantly decreased in the coronal pulp of the EG after the IDR at week 2. Our data suggest that treatment with L-PRP may have a positive effect on pulpal healing, even in teeth replanted after an extended extra-oral period.
1. Introduction
Platelet concentrates (PCs) are primarily characterized by platelet-rich plasma (PRP) and platelet-rich fibrin (PRF). They are biological autologous products derived from blood samples that combine plasma/platelet-derived bioactive components with fibrin-forming proteins to structure a natural three-dimensional scaffold [1,2]. Among the diverse types of PCs, PRP is defined as an autologous blood clot containing a high concentration of platelets. Its therapeutic potential is based on the synergistic action of its content in plasma and platelets. Although it contains anabolic growth factors, it also contains many biomolecules that may affect the regenerative effects of tissue metabolism [3,4]. Clinically, PRP is widely used in orthopedic diseases involving various tissues, such as bones, cartilage, ligaments, tendons, and muscles, because of its superior regenerative and restorative properties and high platelet concentration above physiological levels [5,6]. In addition, PRP has been used in dentistry to promote bone augmentation following third molar surgeries, the management of endo-perio lesions, placement of dental implants, treatment of temporomandibular joint lesions, and as a scaffold for regenerative endodontic treatments (RETs) [7,8,9,10,11]. PRP may be divided into leukocyte-PRP (L-PRP) and pure-PRP (P-PRP) depending on the number of leukocytes relative to autologous blood [12]. Recently, the concentration and composition of leukocytes have been analyzed because they influence the biological properties of PRP through their immunological and antibacterial properties. They are also required to promote wound healing and regulate local factors [13]. Furthermore, the antibacterial properties of L-PRP induced by the presence of leukocytes are important for its application in tissue healing in areas of high bacterial concentrations, such as the oral cavity. Although there is compelling evidence for the use of L-PRP for bone and periodontal tissue regeneration, there are no reports on the effect of leukocytes on PRP under pulpal pathological conditions [14,15]. Thus, the effect of L-PRP after application to the injured pulpal tissue must be carefully evaluated.
Oral trauma encompasses a series of injuries, including crown and/or root fractures, luxation, subluxation, concussion, and avulsion of either primary or permanent dentition. In the case of tooth avulsions, the nerve and vascular supply are completely disrupted, leading to ischemia in the pulpal tissue. The outcome of such an injury is either total pulp revascularization or the development of partial or total pulpal necrosis, depending on the presence or absence of microorganisms at the injury site [16,17]. Several factors may inhibit pulpal healing in avulsed permanent teeth after replantation, such as bacterial invasion of ischemic pulp segments. Previous studies have shown that the size of the apical foramen should be considered in the outcome of replantation, transplantation, or RETs [18,19,20]. Similarly, the effect of occlusal forces following the replantation of avulsed teeth and the extra-oral time before replantation in the alveolar socket can significantly affect pulpal prognosis [21,22,23]. The latter is particularly important because a longer extra-oral period worsens the prognosis of the pulpal tissue and periodontal ligament. To date, clinical interventions for avulsed teeth have primarily focused on the viability of the periodontal ligament, with the dental pulp being removed by endodontic treatments to limit bacterial contamination [24]. Although conventional guidelines for the management of avulsed teeth are available, new approaches aimed at healing the dental pulp after avulsions should be examined in vitro and in vivo. In recent years, biologically based treatments using autologous sources, such as dentin or bone grafts and PCs, have attracted attention because of their feasibility, low cost, and higher success rates after treatment [25]. Therefore, this study aimed to evaluate the effects of L-PRP on the pulpal healing process following severe tooth injuries, using a model for immediate and intentionally delayed tooth replantation in mice.
2. Materials and Methods
2.1. In Vivo Experimental Procedures
2.1.1. Animals
Animal experiments were conducted following the Animal Research: Reporting of In Vivo Experiments (ARRIVE) guidelines [26] and the protocol established for this project was examined by the Institutional Animal Care and Use Committee and authorized by the President of Niigata University (approval number: SA01338). Crlj: CD1 Institute of Cancer Research (ICR) male mice (n = 63, 3–8 weeks old) were purchased from Charles River Laboratories Japan (Yokohama, Japan). Older mice (4–8 weeks old) were used for blood collection (n = 23), whereas the younger ones (three weeks old) were used as the unit of analysis (n = 40) for the tooth replantation injury model.
2.1.2. L-PRP Preparation
Blood was collected several times from 4–8-week-old ICR mice (Table 1) and we used the same L-PRP that was described in our recent study [27]. Briefly, blood was collected from the tail vein and subjected to double-spin cycle centrifugation (Kubota 3500, Tokyo, Japan). Next, we removed the supernatant and added 1 µL of prostaglandin E1 (Sigma-Aldrich, Saint Louis, MO, USA; product number: P5515) to reduce platelet activation. The final blood cell concentration was determined after a second centrifugation, by measuring 0.1 mL of L-PRP in a Blood Cell Counting Device (pocH iV-diff, Sysmex Corporation, Kobe, Japan). Although there is no specific baseline for in vivo experiments, the extracted L-PRP was available for use in replantation experiments after the leukocyte and platelet concentrations in the PRP were confirmed to be consistent with previous results (i.e., platelet concentrations at least 2- to 3-fold higher than whole blood).

Table 1.
Quality of L-PRP, including platelet and white blood cell concentrations, and the type of replantation (modified from [27]). The number of experimental animals used per operation is shown in the “Target subjects (n)” column and the observation time point is indicated in parentheses.
2.1.3. Tooth Replantation Injury Model
We previously reported the usefulness of a tooth replantation injury model to simulate severe trauma for the assessment of the pulpal response, including longer extra-oral times (e.g., 30 min) to exacerbate hypoxia [28,29,30]. Animals were deeply anesthetized according to our previous paper [27]. The upper left and right molars of each experimental animal (two teeth per mouse) were extracted using a modified pair of dental forceps, and the extracted teeth were immersed for 1 min (immediate reimplantation, IR) or 30 min (intentionally delayed reimplantation, IDR) in phosphate-buffered saline (PBS). The extracted teeth were then reimplanted into their original sockets, after the application of 1.5 µL of freshly prepared L-PRP into each socket (experimental group) or without L-PRP (control group). Our previous trials showed that the alveolar socket of mice can be filled with 1.5 mL of L-PRP without overflow. No further treatment (e.g., fixation of teeth or relief of occlusion) was performed on the replanted teeth. Details on the animal number and the distribution of groups are provided in Supplementary Table S1.
2.2. Tissue Preparation
The experimental animals in the L-PRP group (EG) and control group (CG) were sacrificed from groups of 4–5 mice on day 1 through week 4 following the operation. At each observation point, the experimental animals were transcardially perfused under deep anesthesia according to our previous study [27]. The maxillae were treated according to our previous study [28]. The paraffin sections were stained with hematoxylin–eosin (H&E) to evaluate morphological variations, AZAN staining to evaluate collagen-related structures in the healing pulp, and subjected to immunohistochemistry.
2.3. Immunohistochemistry
Sections were processed for Nestin and Ki67 according to our previous studies [28,30]. For the visualization of the immunoperoxidase reaction, 0.05 M of Tris-HCl buffer (pH 7.6) containing 0.04% 3-3′-diaminobenzidine tetrahydrochloride and 30% H2O2 was used. Counterstaining was performed with hematoxylin.
2.4. Statistical Analysis
Data from H&E staining and Nestin and Ki-67 immunohistochemistry from day 1 to week 4 were analyzed according to our previous studies [27,28,29,30]. The normality of the data was analyzed using the Shapiro–Wilk test.
For comparisons between groups, the Bonferroni multiple comparison test was used after assessing the normality and homogeneity of variance in the data. Samples without a normal distribution were compared using the Kruskal–Wallis test for three or more groups or the Mann–Whitney U-test for two groups.
3. Results
3.1. Histological and Immunohistochemical Evaluation of the Dental Pulp in the Control and L-PRP Groups Following Tooth Replantation
3.1.1. Immediate Replantation (1 min)
One day after replantation, expanded inflammatory reactions were evident in the dental pulp of the samples from the EG and CG, including the presence of numerous inflammatory cells and hemorrhagic areas. Blood vessel lumens disappeared from the odontoblast layer, which showed disruptive features along the pulp-dentin border of the replanted teeth (Supplementary Figure S1A,G). Nestin expression was completely absent in the odontoblast layer in the samples from the CG and EG during this observation period (Supplementary Figure S1D,J). On day 3, the inflammatory cells appeared to decrease in number in the pulpal tissue, whereas the odontoblast layer continued to show degenerative features in both groups (Supplementary Figure S1B,H). Nestin expression remained absent in the odontoblast layer; however, some Nestin-positive filamentous structures were observed in the pulpal floor, particularly in the L-PRP-treated teeth (Supplementary Figure S1E,K). On day 5, the dental pulp began to recover its characteristic features, including the presence of blood vessels, although these were primarily located in the central pulp or near the subodontoblastic layer (Supplementary Figure S1C,I). Eosinophilic amorphous matrices, particularly under the coronal cusps, were observed in the pulpal tissue of the EG (Supplementary Figure S1I). Nestin-positive cells and filamentous structures were observed in the central pulp of the CG, but not under the predentin, as the odontoblast layer was not yet re-organized (Supplementary Figure S1F). In contrast, in the EG, Nestin-positive newly differentiated odontoblast-like cells were detected in the root and pulpal floor (Supplementary Figure S1L). Quantitative analysis of Nestin immunostaining revealed a positive trend in the replanted teeth treated with L-PRP at days 3 and 5, although no significant differences were observed between the groups or time points (Supplementary Figure S2). Similarly, one week after replantation, the dental pulp of the CG showed the presence of eosinophilic amorphous matrices beneath the odontoblast layer (Figure 1A), which corresponded to areas of AZAN-positive staining (Figure 1B) and Nestin-positive filamentous structures in the central pulp. In addition, newly differentiated odontoblast-like cells beneath the predentin exhibited a positive reaction to Nestin (Figure 1C). The healing process was improved in the dental pulp in most samples of the EG, which showed more blood vessels compared with that in the CG and partial re-organization of its normal morphology, particularly in the root pulp, central coronal pulp, and pulpal floor (Figure 1D). Collagen deposition, as revealed by AZAN blue staining, was located in the subodontoblastic layer (Figure 1E), whereas intense Nestin immunoreactivity was detected in odontoblast-like cells along the dentin-pulp border as well as in cells and filamentous structures in the subodontoblast layer and pulpal floor (Figure 1F). Two weeks after replantation, a higher percentage of newly formed hard tissues was observed in the pulp of replanted teeth in the EG compared with that in the CG (Figure 2A,D). Collagen-related blue areas were identified in the newly formed hard tissue by AZAN blue staining, which was consistently observed in the EG. Nestin immunohistochemistry enabled the identification of the healing patterns, such as tertiary dentin and/or bone-like tissue in the dental pulp (Figure 2C,F). Analysis of the Nestin-positive perimeter, which provides insight into the progression of the pulpal healing process, showed significant differences between the first and second weeks in the CG and EG (p < 0.002, p < 0.012) (Figure 3A). Moreover, a significant difference was observed between the CG and EG at week 2 in terms of newly formed hard tissue deposition (p < 0.002) (Figure 3C). The established healing patterns did not change over time in the samples from the CG and EG, even at week 4 following the operation, although the pulpal space was reduced because of the continued deposition of hard tissue by newly differentiated hard tissue-forming cells (Supplementary Figure S4A–D).
3.1.2. Intentionally Delayed Replantation (30 min)
The efficacy of L-PRP in the pulpal healing process was tested under more demanding conditions, such a 30 min immersion in PBS before treatment and replantation. At week 1 after the operation, inflammatory reactions were observed in the dental pulp. Eosinophilic matrices were seen on the pulpal horns and central pulp in the CG, with small hemorrhagic areas (arrowheads) in the odontoblast layer (Figure 1G). The dental pulp of the replanted teeth in the EG appeared to recover its characteristic features, with some samples showing early deposition of newly formed hard tissue (arrows) in certain areas of the pulpal floor (Figure 1J). Collagen-related traces were recognized by AZAN staining in the central pulp of samples undergoing healing in the CG (Figure 1H), whereas the positive blue staining was only observed in samples having areas where hard tissue deposition began to occur (Figure 1K). At this stage, Nestin immunostaining was more intense in the whole dental pulp of the CG compared with that in the EG (Figure 1I,L). Consequently, at week 2 after replantation, thick areas of newly formed hard tissue were observed in the dental pulp of the CG and EG. The deposition of hard tissue appeared to follow an irregular pattern within the coronal pulp of some samples in the EG (Figure 2J) compared with that in the CG (Figure 2G). Numerous collagen-related blue areas detected by AZAN staining were less evident in the CG (Figure 2H) compared with that in the EG (Figure 2K). In the CG, Nestin expression was clearly localized in the odontoblast-like cells aligned beneath the areas where tertiary dentin formation occurred. Negative Nestin immunostaining enabled the identification of bone-like tissue formation in the dental pulp (Figure 2I). Furthermore, Nestin-positive filaments and cells were observed within the dental pulp of EG along with newly differentiated odontoblast-like cells around the areas where tertiary dentin was secreted (Figure 2L). Quantitative analysis of the pulpal healing process by Nestin immunohistochemistry showed a positive trend in the CG at week 1, but this was reversed at week 2, with a positive trend in the EG (Figure 3B). Similarly, a positive trend was observed at week 2 on the rate of hard tissue deposition (Figure 3D).
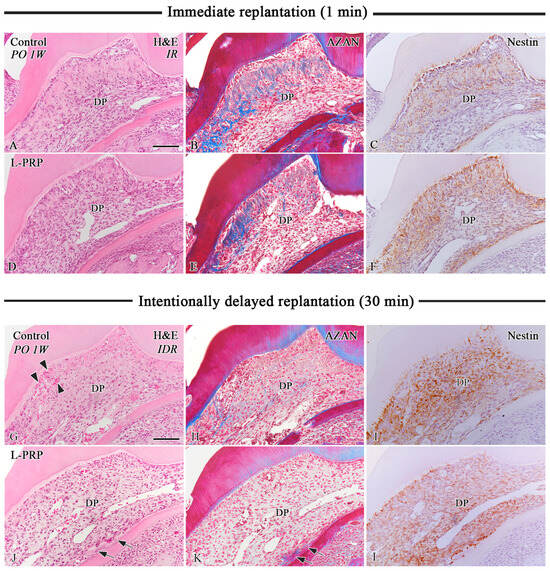
Figure 1.
Hematoxylin–eosin (H&E) (A,D,G,J) and AZAN (B,E,H,K) staining, and immunohistochemistry for Nestin (C,F,I,L) in samples from the CG (A–C,G–I) and EG (D–F,J–L) one week after IR (A–F) and IDR (G–L). (A,G) The dental pulp of the CG after IR and IDR shows eosinophilic amorphous matrices and small hemorrhagic areas in the odontoblast layer (arrowheads in G). (D,J) Fewer inflammatory lesions and more blood vessels are observed in the dental pulp of samples from the EG after IR and IDR. (J,K) Some samples show early deposition of newly formed hard tissue (arrows) in certain areas of the pulpal floor after IDR. (B,E) Collagen-related blue areas are consistently detected by AZAN staining in the CG and EG after IR. (H,K) Weak AZAN staining is observed in the dental pulp of samples from the CG and EG after IDR. (C,F) Samples from the CG and EG show a positive reaction for Nestin in odontoblast-like cells, pulpal cells, and filamentous structures after IR. (I,L) Nestin immunoreaction is more intensely detected in the whole dental pulp in samples from the CG and EG after IDR. DP: Dental pulp. Scale bars: 100 µm (A–L).
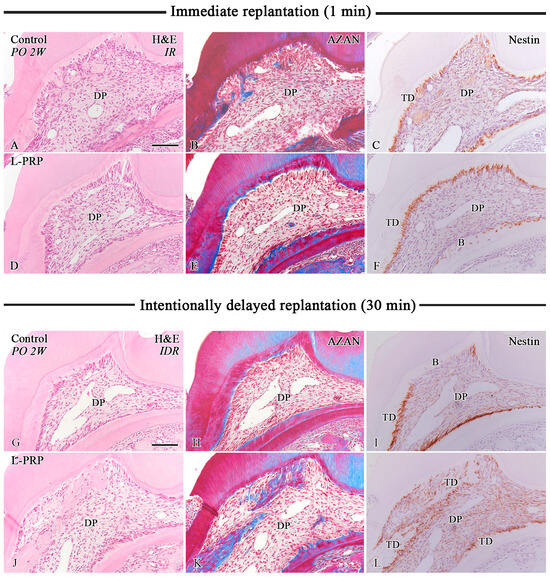
Figure 2.
H&E (A,D,G,J) and AZAN staining (B,E,H,K), and immunohistochemistry for Nestin (C,F,I,L) in samples from the CG (A–C,G–I) and EG (D–F,J–L) at week 2 after IR (A–F) and IDR (G–L). (A,D,G,J) Newly formed hard tissue is observed in the dental pulp of the CG and EG after IR and IDR. (B,H) Collagen-related blue areas in the hard tissue areas are evident following AZAN staining in samples from the CG. (E,K) AZAN-positive areas are more abundant in the pulpal tissue of the EG following IR and IDR. (C,F,I,L) Nestin expression is localized in the odontoblast-like cells aligned beneath the newly formed tertiary dentin in samples from the CG and EG after IR and IDR. (F,I) Bone-like tissue formation in some samples of the CG and EG lacks Nestin immunoreactivity following either IR or IDR. B: Bone-like tissue, DP: Dental pulp, TD: Tertiary dentin. Scale bars: 100 µm (A–L).
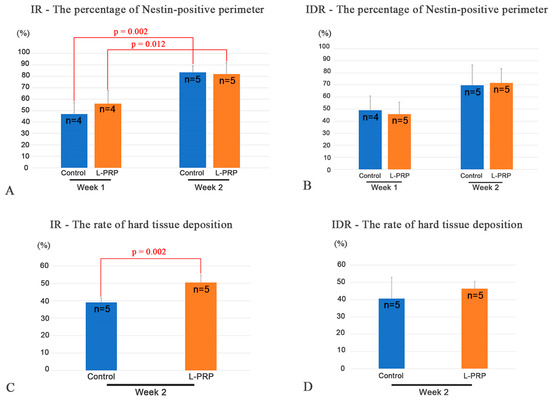
Figure 3.
Quantitative analysis of H&E staining and immunohistochemistry for Nestin in the control and L-PRP teeth after IR and IDR. (A) Significant differences (p < 0.002, p < 0.012) in the percentage of Nestin-positive perimeter are evident between observation points in the CG and EG after IR. (B) No significant differences are noted between groups or observation periods at week 2 after IDR. (C) The occurrence rate of hard tissue deposition in the dental pulp differed significantly between the CG and EG after IR (p < 0.002). (D) A slight positive trend in the EG was noted at this stage following IDR.
3.2. Assessment of Cell Proliferation in the Dental Pulp of Replanted Teeth by Ki-67 Immunostaining
The proliferative activity of pulpal cells after application or absence of L-PRP before replantation was evaluated using Ki-67 immunohistochemistry from day 1 to week 2 after IR and at weeks 1 and 2 after IDR. Following immediate replantation, the number of proliferative cells seemed to be slightly lower in the EG group, particularly in the root pulp, at day 1 (Supplementary Figure S3A,D). At day 3, the positive cells were slightly higher in the crown and root pulp of the EG (Supplementary Figure S3B,E), and in the root pulp at day 5 (Supplementary Figure S3C,F). No significant differences were found at week 1 (Figure 4A,B) or 2 (Figure 4C,D) after replantation. In contrast, quantitative analysis of Ki-67 in the samples from the IDR injury model indicated that the L-PRP treatment did not improve the pulpal cell proliferation activity in the coronal or root pulp one week after replantation (Figure 4E,F); however, cell proliferation was decreased in the EG at week 2, particularly in the coronal pulp (p < 0.047) (Figure 4G,H).
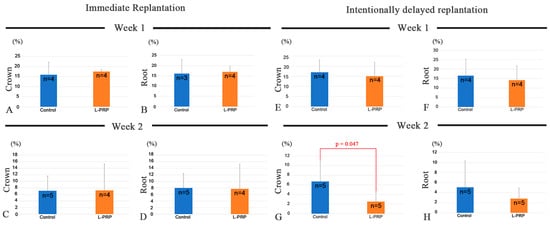
Figure 4.
The percentage of Ki-67-positive cells in the crown (A,C,E,G) and root pulp (B,D,F,H) at weeks 1 (A,B,E,F) and 2 (C,D,G,H) after IR (A–D) and IDR (E–H). (A,B) There are no significant differences in the number of proliferating cells at week 1 in the crown and root pulp between CG and EG after IR. (C,D) Similarly, no significant differences are noted between groups at week 2 after IR. (E,F) Cell proliferation appears slightly higher in the CG in the coronal and root pulp at week 1 after IDR. (G,H) The proliferative cells further decrease at week 2, whereas a significant difference between the CG and EG is observed in the coronal pulp at this stage (p < 0.047).
4. Discussion
This study for the first time evaluated the effectiveness of a topical treatment of L-PRP on the pulpal healing process using a mouse model for tooth replantation. The treatment with L-PRP induced a better healing of the pulpal tissue, showing a significantly positive effect in the IR model and a positive trend in the IDR model regarding the rate of newly formed hard tissue. Considering the lack of studies addressing the effects of L-PRP in the pulpal healing following exogenous tooth injuries, the results become important for understanding the implications of PCs as adjuvants in endodontic therapies, particularly in RETs. For example, the use of PRP as a scaffold in RET has been previously evaluated using a dog model, in which the teeth sustained apical periodontitis. PRP was placed at the enamel–cementum junction after filling the canal space with blood induced from the periapical tissues. The histological evaluation showed no statistical differences between the PRP group and the conventional blood clot in terms of apical closure and newly formed tissues, including pulp-like tissue [31]. In this present study, the direct exposure of the still immature apical papilla to L-PRP did not significantly accelerate odontoblast-like cell differentiation between the groups at weeks 1 or 2 following IR or IDR. However, L-PRP induced a faster deposition of tertiary dentin, bone-like tissue, or a combination of both in the repaired pulp compared with the untreated replanted teeth at week 2 after the operation. This observation is supported by our findings regarding the proliferative activity in the dental pulp during the same observation period, when the number of proliferative cells decreased in the L-PRP group, particularly after IDR. We also found a positive trend in the number of proliferating cells in the L-PRP group at the early phases of the pulpal healing process after IDR. Because cell proliferation precedes cell differentiation, the presence of endogenous collagen and thrombin in the apical pulp tissue may facilitate the sustained release of growth factors available in L-PRP, thereby promoting an ideal environment for cell proliferation and differentiation [32]. To date, few studies have examined the mechanisms underlying the beneficial effects of PRP; however, an in vitro study demonstrated that treatment of human dental pulp cells (hDPCs) with PRP at various concentrations (5–20%) promoted cell migration, proliferation, and differentiation. Furthermore, PRP induced autophagic activity, thus promoting tissue regeneration [33]; however, further in vitro mechanistic studies are needed to understand the effects of PRP on tissue repair and regeneration.
The presence of leukocytes remains controversial in PRP-related therapies. Although leukocytosis may improve antibacterial properties to create a favorable environment for faster tissue repair/regeneration, a systematic review found insufficient evidence for this favorable effect. PRP preparations with or without leukocytes showed bacteriostatic effects, suggesting that L-PRP preparations may be useful as a prophylactic measure to reduce bacterial load and promote healing, rather than solely as a treatment [13]. Similarly, the concentration of leukocytes is another factor to consider for understanding the effects of L-PRP for clinical applications [12]. In this present study, white blood cell concentrations in the L-PRP preparations ranged from 52 × 102/µL to 138 × 102/µL. The variations in the concentration of these cells did not appear to be significantly related to the improvement of the pulpal healing process. In this context, a recent study from our group showed that L-PRP containing white blood cell concentrations ranging from 21 × 102/µL to 172 × 102/µL positively enhanced osseointegration after implant placement in mice [27]. Although these values were obtained from animal models and are not directly applicable to humans, they demonstrate the importance of the quantitative assessment of leukocyte counts prior to the application of L-PRP in a clinical setting. Nevertheless, this question requires further studies in vitro and in vivo.
Extra-oral time is an important factor for the healing of the afflicted dental pulp following tooth injuries. A previous study showed the influence of the extra-oral time on the prognosis of replanted teeth. Thirty or more minutes of extra-oral time resulted in the deposition of bone-like tissue in the pulp chamber of replanted teeth in mice as well as root ankylosis [21]. In this present study, the 30 min immersion in PBS followed by topical treatment with L-PRP improved the healing process of the pulpal tissue in a similar fashion to that after IR. Thus, the impact of extra-oral time on the pulpal and supporting tissues of the extracted teeth appears to be attenuated by the type of biomaterial used before replantation in the original socket, as demonstrated in previous studies using anti-microbial solutions or immunomodulators prior to tooth replantation [28,30]. In this context, the use of L-PRP in combination with antibacterial solutions such as the triple antibiotic mixture (3Mix) may be advantageous in the treatment of avulsed teeth with exposed immature apices. First, the avulsed tooth can be immersed in the 3Mix solution to disinfect the apical papilla and damaged periodontal tissue [28]. Then, L-PRP can be topically administered into the alveolar socket before replantation, thus creating an optimal situation to accelerate the healing of the dental pulp, and possibly the periodontal ligament to avoid root ankylosis. Similarly, L-PRP can be used with the technique of intentional pulpal floor perforation to improve revascularization after tooth replantation [29]. After perforation, application of L-PRP into the alveolar socket may improve pulpal wound healing because the growth factors available in the platelet concentrate can help in the acceleration of the pulpal healing. The effectiveness of these alternatives needs to be evaluated using animal models in future work. The limitations of this study include the difficulty in obtaining tail vein blood samples in mice, the variability in platelet and leukocyte concentrations in L-PRP between blood samples, and the variability of tissue healing depending on the animal. In addition, the differences between human and mouse models should be considered when considering the clinical application of L-PRP.
5. Conclusions
Future clinical applications of L-PRP in human patients should be conducted following a validated protocol for its extraction using consistent volumes of blood. For example, we propose that the platelet concentrate should be in the 2–3-fold range versus whole blood, based on previous clinical reports and our in vivo observations. Regardless of this preliminary approach, the data suggest that L-PRP may have a positive effect on pulpal healing by promoting hard tissue deposition in the dental pulp, even in teeth replanted after a long period of time.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app142311358/s1, Table S1: The distribution of experimental animals; Figure S1: Chronological changes in the dental pulp during the early stages after IR; Figure S2: The percentage of Nestin-positive perimeter during the early stages after IR; Figure S3: The proliferative activity in the coronal and root pulp during the early stages after IR; Figure S4: H&E and Nestin immunohistochemistry of replanted teeth after IR at week 4.
Author Contributions
Conceptualization, H.O.; methodology, H.O., K.S.-B. and A.Q.-S.; validation, A.Q.-S., K.S.-B., M.Z.-S., T.W., T.K. and H.O.; formal analysis, A.Q.-S., M.Z.-S. and H.O.; investigation, A.Q.-S., K.S.-B. and H.O.; data curation, A.Q.-S. and H.O.; writing—original draft preparation, A.Q.-S., K.S.-B. and H.O.; writing—review and editing, A.Q.-S., K.S.-B., M.Z.-S., T.W., T.K. and H.O.; visualization, A.Q.-S. and H.O.; supervision, H.O.; funding acquisition, H.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Japan Society for the Promotion of Science (JSPS) KAKENHI (Grant Numbers 22K21011 and 23H03078).
Institutional Review Board Statement
The animal study protocol was approved by the Institutional Animal Care and Use Committee and approved by the President of Niigata University (approval number SA01338, approved date 24 April 2023).
Informed Consent Statement
Not applicable.
Data Availability Statement
The original data presented are included in the article/Supplementary Materials. Further inquiries can be directed to the corresponding author.
Acknowledgments
The authors cordially thank H. Ida-Yonemochi, S. Kenmotsu (†), Y. Abe, and M. Kawachi for their technical assistance and animal care.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Mariani, E.; Pulsatelli, L. Platelet Concentrates in Musculoskeletal Medicine. Int. J. Mol. Sci. 2020, 21, 1328. [Google Scholar] [CrossRef] [PubMed]
- Ding, Z.Y.; Tan, Y.; Peng, Q.; Zuo, J.; Li, N. Novel applications of platelet concentrates in tissue regeneration (Review). Exp. Ther. Med. 2021, 21, 226. [Google Scholar] [CrossRef] [PubMed]
- Marx, R.E.; Carlson, E.R.; Eichstaedt, R.M.; Schimmele, S.R.; Strauss, J.E.; Georgeff, K.R. Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 1998, 85, 638–646. [Google Scholar] [CrossRef] [PubMed]
- Mercader-Ruiz, J.; Beitia, M.; Delgado, D.; Sánchez, P.; Porras, B.; Gimeno, I.; González, S.; Benito-Lopez, F.; Basabe-Desmonts, L.; Sánchez, M. Current Challenges in the Development of Platelet-Rich Plasma-Based Therapies. Biomed. Res. Int. 2024, 2024, 6444120. [Google Scholar] [CrossRef]
- Huang, J.; Lian, S.L.; Han, J.H.; Lu, Z.C.; Ding, Y. Pure platelet-rich plasma promotes semaphorin-3A expression: A novel insight to ameliorate intervertebral disk degeneration in vitro. J. Orthop. Surg. Res. 2023, 18, 789. [Google Scholar] [CrossRef]
- Liu, X.; Li, Y.; Shen, L.; Yan, M. Leukocyte and Platelet-Rich Plasma (L-PRP) in Tendon Models: A Systematic Review and Meta-Analysis of in vivo/in vitro Studies. Evid. Based Complement. Altern. Med. 2022, 2022, 5289145. [Google Scholar] [CrossRef]
- Costa, M.D.M.A.; Paranhos, L.R.; de Almeida, V.L.; Oliveira, L.M.; Vieira, W.A.; Dechichi, P. Do blood concentrates influence inflammatory signs and symptoms after mandibular third molar surgery? A systematic review and network meta-analysis of randomized clinical trials. Clin. Oral Investig. 2023, 27, 7045–7078. [Google Scholar] [CrossRef]
- BKolcu, M.I.; Yurdakul, H.; Belli, S. Regenerative endodontic treatment of an immature incisor tooth with a novel platelet-rich product: A five-year follow-up case report. Niger. J. Clin. Pract. 2023, 26, 1388–1392. [Google Scholar] [CrossRef]
- Mehta, V.; Fiorillo, L.; Langaliya, A.; Obulareddy, V.T.; Cicciu, M. The Effect of Xenograft and Platelet-Rich Plasma in the Surgical Management of Intrabony Defects in Periodontitis Patients: A Systematic Review. J. Craniofacial Surg. 2023, 34, 2222–2227. [Google Scholar] [CrossRef]
- Prakash, J.; Talukder, D.; Desai, K.; Singh, T.K.; Bagde, R.; Randhawa, G.S.; Jha, S.; Paiwal, K. Intra-articular platelet-rich plasma injection versus hydrocortisone with local anesthetic injections for temporo mandibular disorders. Bioinformation 2022, 18, 991–997. [Google Scholar] [CrossRef]
- Tomar, N.; Dahiya, S.; Sharma, P.K.; Sabu, K.I.; Singh Parihar, A.; Mandal, A.; Sahoo, A.R. A Comparative Clinical Evaluation of Effectiveness of Platelet-Rich Plasma, Synthetic Allograft, and Bioresorbable Xenograft During Immediate Implant Placement. Cureus 2022, 14, e32121. [Google Scholar] [CrossRef] [PubMed]
- Bielecki, T.; Dohan Ehrenfest, D.M.; Everts, P.A.; Wiczkowski, A. The role of leukocytes from L-PRP/L-PRF in wound healing and immune defense: New perspectives. Curr. Pharm. Biotechnol. 2012, 13, 1153–1162. [Google Scholar] [CrossRef] [PubMed]
- D’asta, F.; Halstead, F.; Harrison, P.; Zecchi Orlandini, S.; Moiemen, N.; Lord, J. The contribution of leucocytes to the antimicrobial activity of platelet-rich plasma preparations: A systematic review. Platelets 2018, 29, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Allende, M.; Alkhraisat, M.H. Unravelling Alveolar Bone Regeneration Ability of Platelet-Rich Plasma: A Systematic Review with Meta-Analysis. Bioengineering 2022, 9, 506. [Google Scholar] [CrossRef]
- Chou, T.M.; Chang, H.P.; Wang, J.C. Autologous platelet concentrates in maxillofacial regenerative therapy. Kaohsiung J. Med. Sci. 2020, 36, 305–310. [Google Scholar] [CrossRef]
- Andreasen, F.M.; Kahler, B. Pulpal response after acute dental injury in the permanent dentition: Clinical implications—A review. J. Endod. 2015, 41, 299–308. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Andreasen, F.M.; Andersson, L. Textbook and Color Atlas of Traumatic Injuries to the Teeth, 5th ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2019. [Google Scholar]
- Nakakura-Ohshima, K.; Quispe-Salcedo, A.; Sano, H.; Hayasaki, H.; Ohshima, H. The effects of reducing the root length by apicoectomy on dental pulp revascularization following tooth replantation in mice. Dent. Traumatol. 2021, 37, 677–690. [Google Scholar] [CrossRef]
- Fang, Y.; Wang, X.; Zhu, J.; Su, C.; Yang, Y.; Meng, L. Influence of Apical Diameter on the Outcome of Regenerative Endodontic Treatment in Teeth with Pulp Necrosis: A Review. J. Endod. 2018, 44, 414–431. [Google Scholar] [CrossRef]
- Laureys, W.G.; Cuvelier, C.A.; Dermaut, L.R.; De Pauw, G.A. The critical apical diameter to obtain regeneration of the pulp tissue after tooth transplantation, replantation, or regenerative endodontic treatment. J. Endod. 2013, 39, 759–763. [Google Scholar] [CrossRef]
- Hasegawa, T.; Suzuki, H.; Yoshie, H.; Ohshima, H. Influence of extended operation time and of occlusal force on determination of pulpal healing pattern in replanted mouse molars. Cell Tissue Res. 2007, 329, 259–272. [Google Scholar] [CrossRef]
- Qian, H.; Ding, Y.; Wu, Y.; Li, S. The effects of three modified Hank’s balanced salt solutions on root resorption of late replanted teeth: A pilot study. J. Craniomaxillofac. Surg. 2018, 46, 808–814. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Teixeira, F.B.; Ritter, A.L.; Levin, L.; Trope, M. The effect of intracanal anti-inflammatory medicaments on external root resorption of replanted dog teeth after extended extra-oral dry time. Dent. Traumatol. 2008, 24, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Fouad, A.F.; Abbott, P.V.; Tsilingaridis, G.; Cohenca, N.; Lauridsen, E.; Bourguignon, C.; O’Connell, A.; Flores, M.T.; Day, P.F.; Hicks, L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent. Traumatol. 2020, 36, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhang, L.; Wang, K. Bioactive ceramic-based materials: Beneficial properties and potential applications in dental repair and regeneration. Regen. Med. 2024, 19, 257–278. [Google Scholar] [CrossRef] [PubMed]
- Kilkenny, C.; Browne, W.J.; Cuthi, I.; Emerson, M.; Altman, D.G. Improving Bioscience Research Reporting: The ARRIVE Guidelines for Reporting Animal Research. Vet. Clin. Pathol. 2012, 41, 27–31. [Google Scholar] [CrossRef]
- Zapata-Sifuentes, M.; Quispe-Salcedo, A.; Watanabe, T.; Kawase, T.; Ohshima, H. Effect of leukocyte and platelet-rich plasma on osseointegration after implant placement in mouse maxilla. Regen. Ther. 2024, 26, 741–748. [Google Scholar] [CrossRef]
- Quispe-Salcedo, A.; Ida-Yonemochi, H.; Ohshima, H. Effects of a triple antibiotic solution on pulpal dynamics after intentionally delayed tooth replantation in mice. J. Endod. 2014, 40, 1566–1572. [Google Scholar] [CrossRef]
- Sano, H.; Nakakura-Ohshima, K.; Okada, Y.; Sato, T.; Ohshima, H. The effect of intentionally perforating the floor of the pulp chamber on pulpal healing after tooth replantation in mice. J. Oral Biosci. 2023, 65, 31–39. [Google Scholar] [CrossRef]
- Quispe-Salcedo, A.; Yamazaki, T.; Ohshima, H. Effects of Synthetic Toll-Like Receptor 9 Ligand Molecules on Pulpal Immunomodulatory Response and Repair after Injuries. Biomolecules 2024, 14, 931. [Google Scholar] [CrossRef]
- Zhang, D.D.; Chen, X.; Bao, Z.F.; Chen, M.; Ding, Z.J.; Zhong, M. Histologic comparison between platelet-rich plasma and blood clot in regenerative endodontic treatment: An animal study. J. Endod. 2014, 40, 1388–1393. [Google Scholar] [CrossRef]
- Harrison, S.; Vavken, P.; Kevy, S.; Jacobson, M.; Zurakowski, D.; Murray, M.M. Platelet activation by collagen provides sustained release of anabolic cytokines. Am. J. Sports Med. 2011, 39, 729–734. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Xu, F.; Zhao, J.; Zhou, C.; Liu, J. Platelet-Rich Plasma Induces Autophagy and Promotes Regeneration in Human Dental Pulp Cells. Front. Bioeng. Biotechnol. 2021, 9, 659742. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).