Abstract
The integration of artificial intelligence (AI) in healthcare management marks a significant advance in technological innovation, promising transformative effects on healthcare processes, patient care, and the efficacy of emergency responses. The scientific novelty of the study lies in its integrated approach, combining systematic review and predictive algorithms to provide a comprehensive understanding of AI’s role in improving healthcare management across different contexts. Covering the period between 2019 and 2023, which includes the global challenges posed by the COVID-19 pandemic, this research investigates the operational, strategic, and emergency response implications of AI adoption in the healthcare sector. It further examines how the impact of AI varies across temporal and geographical contexts. The study addresses two main research objectives: to explore how AI influences healthcare management in operational, strategic, and emergency response domains, and to identify variations in the impact of AI on healthcare management based on temporal and geographical contexts. Utilizing an integrated approach, we compared various prediction algorithms, including logistic regression, and interpreted the results through SHAP (SHapley Additive exPlanations) analysis. The findings reveal five key thematic areas: AI’s role in enhancing quality assurance, resource management, technological innovation, security, and the healthcare response to the COVID-19 pandemic. The study highlights AI’s positive influence on operational efficiency and strategic decision making, while also identifying challenges related to data privacy, ethical considerations, and the need for ongoing technological integration. These insights provide opportunities for targeted interventions to optimize AI’s impact in current and future healthcare landscapes. In conclusion, this work contributes to a deeper understanding of the role of AI in healthcare management and provides insights for policymakers, healthcare professionals, and researchers, offering a roadmap for addressing both the opportunities and challenges posed by AI integration in the healthcare sector.
1. Introduction
The technological advancements of the past decade have positioned artificial intelligence (AI) as a transformative force across various sectors, with particularly significant impacts in the realm of healthcare management. The integration of AI promises to revolutionize healthcare processes, improve patient care, and optimize emergency responses by leveraging complex data to inform rapid, evidence-based decisions. However, despite growing enthusiasm, the adoption of AI in healthcare also presents unique challenges, necessitating a careful examination of its operational, strategic, and emergency implications. In addition to AI, other emerging technologies, such as augmented reality (AR), have shown potential in optimizing processes and improving outcomes in various sectors, including healthcare and training. For instance, recent studies on AR for corporate training demonstrate its ability to enhance learning outcomes and reduce errors through real-time, immersive experiences [1]. (Marengo et al., 2018).
In the face of widespread health challenges that have put global healthcare systems under intense pressure, AI has offered innovative solutions for managing unprecedented health crises, highlighting the urgency of scientifically assessing its impact. Thus, this study contributes by providing a comprehensive evaluation of AI’s impact on healthcare management, focusing on its potential to enhance operational efficiency, strategic decision making, and emergency preparedness. Additionally, this work explores variations in AI’s impact based on temporal and geographical contexts, offering valuable insights into how AI can be optimally integrated into diverse healthcare systems. The integration of artificial intelligence (AI) in the healthcare sector represents one of the most significant technological advancements in recent years, promising to transform healthcare management through process optimization, improvement in patient care, and effectiveness in emergency responses.
The integration of AI in healthcare improves the quality of medical education and scientific publications, while also enhancing the resilience of healthcare facilities during emergencies [2]. The implementation of AI technologies has been shown to support the reproducibility of scientific findings, a cornerstone for advancing medical knowledge and practices [3]. Furthermore, the development and testing of tools to assess the flexibility and resilience of healthcare infrastructure highlight AI’s potential to prepare and adapt healthcare systems for emergency situations [4].
It is crucial to emphasize the importance of ethical and regulatory oversight in the use of artificial intelligence in the healthcare sector, to ensure that AI applications are safe and that the privacy of patient data is respected [5]. Additionally, the need to develop specific guidelines for reporting and evaluating AI in healthcare has been identified, to support systematic reviews and meta-analyses that ensure transparency and reproducibility of results [6]. In the United States and Europe, regulatory frameworks are evolving to keep pace with advancements in artificial intelligence in healthcare. Regulators, such as the FDA in the United States, are working to balance technological innovation with patient safety and privacy [7]. In Europe, the 2021 European Union Health Technology Assessment (HTA) regulation represents a significant step towards harmonizing evaluation procedures for technologies, including AI-based tools, across member states. This regulation aims to ensure that AI adoption in healthcare meets standards of safety, efficacy, and transparency, contributing to the overall improvement of healthcare quality [8]. Similarly, in Asia, countries like China and Japan are heavily investing in AI integration within their healthcare systems. In China, privacy protection is a central concern in AI regulation in healthcare, with specific regulations and accountability mechanisms needed to safeguard personal data. This aligns with regulatory efforts in the United States and European Union [9]. However, challenges remain in harmonizing regulations across diverse healthcare systems and policies throughout Asia. Further research has highlighted the fragmentation of the regulatory landscape of AI in Africa, indicating an urgent need for regulatory development to facilitate future adoption of AI in healthcare on the continent [10].
These insights underline the complexity of integrating AI into healthcare management, highlighting both the revolutionary potential and the regulatory, ethical, and operational challenges that accompany the adoption of this technology.
While the potential of AI is vast and diverse, it is essential to systematically understand how this technology is influencing the sector in terms of operational, strategic, and emergency response aspects, as well as its variations based on temporal and geographical contexts. Through the analysis of peer-reviewed articles published between 2019 and 2023, this work intends to outline how AI is shaping the future of healthcare management, highlighting both the opportunities and challenges posed by its integration. This leads to formulating the following research questions:
Q1:
How does artificial intelligence affect healthcare management, considering various operational, strategic, and emergency response aspects?
Q2:
What are the variations in the impact of artificial intelligence on healthcare management depending on temporal and geographical contexts?
These questions will guide the analysis towards a deeper understanding of the impact of AI, allowing for the identification of opportunities, challenges, and areas of priority intervention in the current and future healthcare context.
The remainder of this document is organized as follows: Section 2 presents the methodological approach used for the systematic review. In Section 3, the results are provided, detailing the analyses by year, country, focus, methodology, results, and challenges for each of the five identified topic areas. Section 4 discusses these five areas in depth, integrating an experimental phase with the application of predictive algorithms. Finally, Section 5 concludes the study by highlighting its limitations and offering suggestions for future research directions.
2. Materials and Methods
To address the questions raised by the research inquiries, this study implemented a systematic literature review, focusing on exploring the impact of artificial intelligence on healthcare management, and its variations based on temporal and geographical contexts. The methodological approach adopted follows the guidelines proposed by Marengo and Pagano (2023), which provide a detailed framework for conducting systematic research in this field. The methodological process is structured in sequential phases: defining the research strategy, applying inclusion and exclusion criteria, selecting and screening studies, and finally, extracting and analyzing data. This document thoroughly describes each step, ensuring that the methodology is clear, transparent, and reproducible [11].
2.1. Search Strategy
A comprehensive search was conducted in electronic databases for peer-reviewed articles published between 2019 and 2023, a period marked by significant global health challenges. The databases selected for this search include Google Scholar, ScienceDirect, Scopus, PubMed, IEEE Xplore, and Springer. This choice aims to optimize data collection and ensure comprehensive coverage of relevant literature. The search terms used were “artificial intelligence”, “healthcare”, “hospital management”, employing Boolean operators such as AND and OR. The search focused on article titles, abstracts, and keywords. This multi-database approach was adopted to minimize the risk of omitting relevant studies, following best practices in systematic research in the field of healthcare information systems.
2.2. Inclusion and Exclusion Criteria
To ensure that the selected articles met criteria of high quality and relevance, precise selection and exclusion parameters were defined. The review included articles that:
- Were written in English, as it is the predominant means of communication in the scientific field, selecting works for a detailed analysis that could adequately cover the themes of AI adoption. Both open-access publications and those accessible through subscription or academic libraries were considered, with an emphasis on open-access sources to facilitate broader accessibility.
- Presented empirical studies on factors driving AI adoption in the healthcare sector, with the aim of focusing on research offering significant contributions and insights. This criterion was aimed at identifying studies that provide a deep understanding of the drivers behind AI integration in healthcare contexts.
- Were published in scientific journals or recognized conference proceedings, to encompass a broad spectrum of research contributions. This inclusion was further refined to articles published between 2019 and 2023, and limited to works available in scientific journals or conference proceedings, ensuring the inclusion of the most current and high-quality information.
- Fell within the subject areas of computer sciences, social sciences, business management and accounting, and economics, econometrics, and finance, reflecting a multidisciplinary approach to understanding the multifaceted impact of AI on healthcare management.
Articles that did not conform to these standards were excluded, particularly those not in English due to language limitations, or those that, while addressing related topics, did not specifically focus on factors of AI adoption in hospital management, in order to maintain focus on the central themes of the review. This methodology aimed to ensure the inclusion of significant and relevant contributions, limiting the scope to high-quality and accessible sources, to provide a comprehensive and in-depth overview of AI’s impact on healthcare management.
2.3. Screening and Selection
A systematic approach was employed for the identification and elimination of duplicates. Initially, the Orange software version 3.36.2. was utilized to remove exact duplicates, focusing on title and author information. This was followed by a manual inspection of the remaining articles to ensure no duplicates were missed. The articles that passed this scrutiny were then reviewed in full text, adhering to predefined inclusion and exclusion criteria.
After applying the inclusion criteria and removing duplicates, the full texts of the selected articles were independently read by all five authors. The evaluations were discussed in subsequent group meetings, and any discrepancies were resolved through a consensus process. This approach ensured that the interpretations and conclusions reflected the collective judgment of the entire team, thereby enhancing the consistency and transparency of the article evaluation process.
2.4. Data Extraction and Analysis
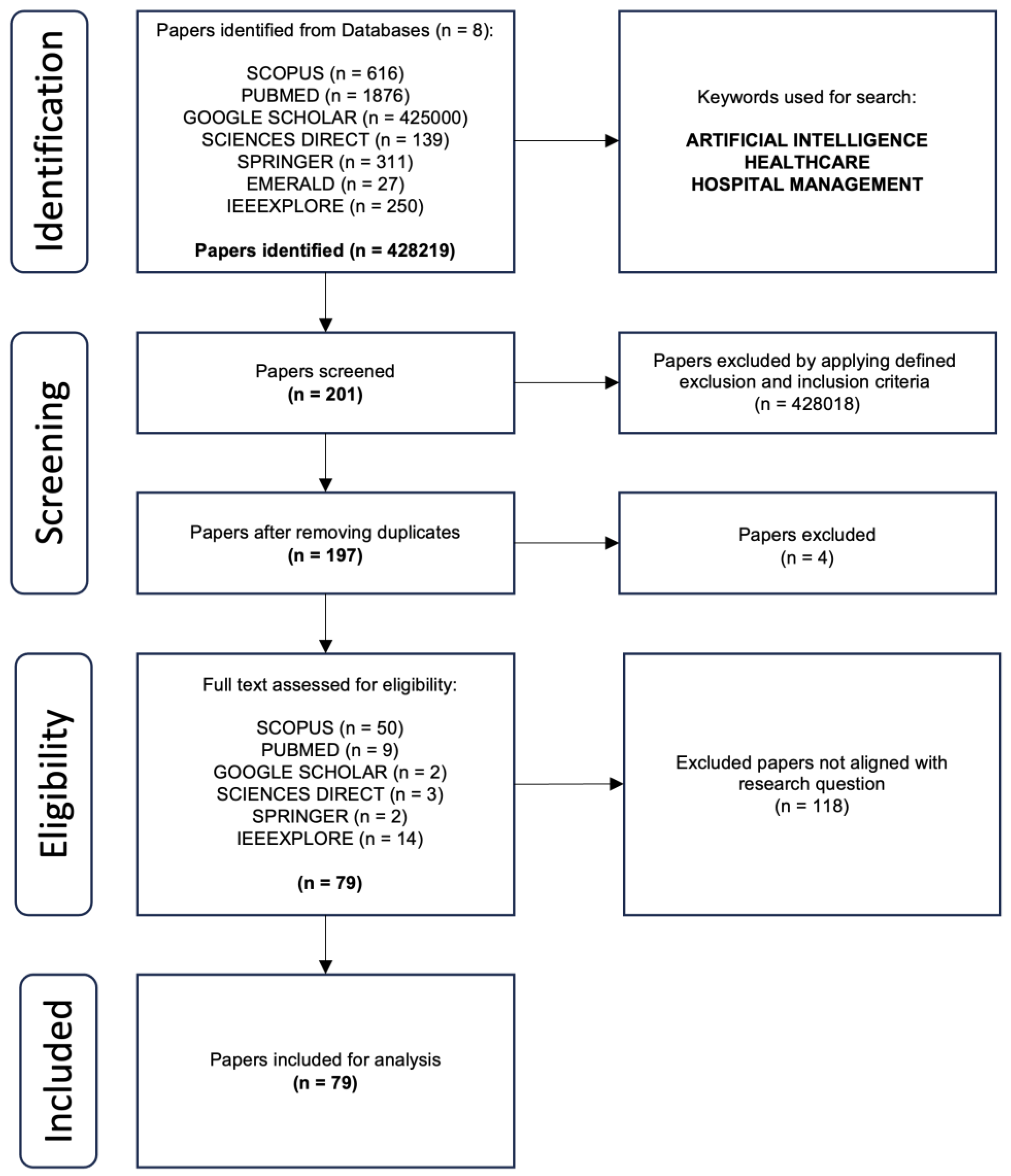
The data extraction process was conducted to capture key information such as the context of AI use in healthcare management, factors influencing adoption and effectiveness, and the main outcomes of the studies. These factors were identified and categorized into main groups based on recurring themes and patterns. The 5 topics identified after a rigorous analysis are illustrated in Section 3 and discussed in Section 4. To ensure the rigor of the review, PRISMA guidelines were followed, enhancing the reliability and validity of the results. Figure 1 will demonstrate the number of articles included in this study and the selection process.
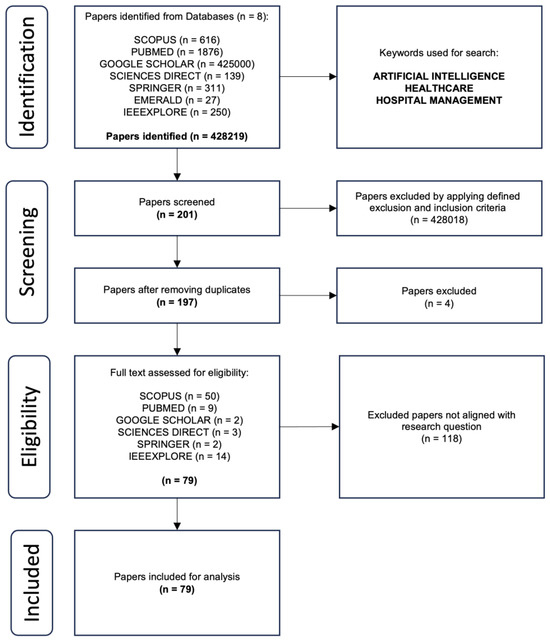
Figure 1.
PRISMA flow chart for this study.
As shown in Figure 1, 79 articles out of 428,219 were included in this study. The reduction was achieved through a rigorous screening and selection process based on specific inclusion and exclusion criteria. Initially, 428,018 articles were removed by applying the established inclusion and exclusion criteria, resulting in 201 articles. Next, 4 duplicates were identified and excluded, resulting in 197 unique articles. These articles were then subjected to a thorough review, excluding 118 articles deemed not aligned with the research question. The remaining 79 articles were further screened by subjecting them to a comprehensive review and deemed suitable to provide substantive insights into the influence and role of AI for healthcare management. These methodological steps made it possible to conduct a focused and thorough systematic review on the influence of AI on healthcare management, providing a solid basis for understanding the current state of research and prospects in this dynamic and rapidly evolving field.
3. Results
After carefully selecting and analyzing 79 studies in the period 2019–2023, our systematic review, responding to research question Q1, has revealed five main thematic areas, reflecting the impact and role of artificial intelligence in the management of the healthcare sector. These areas have been identified as follows in Table 1:

Table 1.
Topic areas identified.
These five thematic areas, each offering a unique perspective on AI in the context of healthcare management, will be the focal point of our investigation. We will delve into how AI contributes to healthcare quality, resource management, security, technological innovation, and the response to healthcare emergencies, with a particular emphasis on AI’s pivotal role during the COVID-19 pandemic. We have assigned a representative keyword to each of these thematic areas, which will assist us in the subsequent stages of analysis. These keywords succinctly capture the focus of each thematic area and will enable us to explore them in detail throughout our research.
These dimensions will provide us with a comprehensive and in-depth view of the intersection between AI and the healthcare sector, unveiling new insights and extraordinary opportunities.
3.1. Artificial Intelligence for Quality Assurance and Stakeholders Engagement
The adoption of artificial intelligence (AI) in the healthcare sector represents a pivotal shift in the management of care quality and stakeholder engagement, as evidenced by the detailed analysis in Table 2. This table provides a global and temporal view, through a series of studies conducted in various countries over the past few years, offering a unique perspective on the dynamics and challenges associated with the integration of AI in the medical field.

Table 2.
International research on AI for quality assurance and stakeholder engagement.
The adoption of artificial intelligence (AI) in healthcare represents a crucial turning point in the management of care quality and stakeholder engagement, as detailed in the analysis of Table 2. This table provides a global and temporal perspective through a series of studies conducted in various countries over recent years, offering a unique insight into the dynamics and challenges associated with integrating AI in the medical field.
The emergence of AI in healthcare signifies a shift in innovation and quality management. The use of AI in hospital settings has highlighted the need for robust quality control measures, essential to ensure effective and reliable clinical decisions [13]. At the same time, the criticality of addressing issues of diversity and inclusion within AI is recognized, a vital aspect to ensure that AI-based solutions are equitably distributed and bias-free [14].
AI also plays a fundamental role in improving patient engagement and communication with healthcare providers. Through telemedicine and advanced communication tools, AI allows patients to access more accurate and personalized information about their health, fostering a better understanding of their conditions and promoting active participation in the treatment process [22]. AI-based systems, such as virtual assistants and chatbots, streamline communication, reduce wait times, and enhance understanding of therapeutic interventions. These technologies support shared decision making by giving patients immediate access to their health data and treatment options, fostering a more collaborative relationship with their healthcare providers [23]. In addition, AI can remind patients of medication schedules or appointments, improving adherence to therapies and enhancing patient autonomy.
AI applications in medical diagnostics open new horizons for early disease detection and treatment personalization, promising significant improvements in recovery probabilities and care customization [12,15]. Particular attention has been focused on the importance of integrating AI competencies into medical curricula, recognizing the need to prepare future healthcare professionals for an increasingly technological clinical environment. The continuous evolution of AI/ML algorithms requires constant monitoring and updating, underscoring the importance of maintaining high standards of quality and reliability in AI clinical applications [16]. This dynamic further emphasizes the need for constructive and multidisciplinary dialogue among technologists, clinicians, and patients, to ensure AI use that is not only technically advanced but also pragmatic and ethically responsible in clinical practice [18]. AI can be employed to enhance quality assurance and stakeholder engagement in the healthcare sector, underscoring the importance of addressing ethical and governance challenges, such as data privacy and algorithmic bias, for a responsible adoption of AI in healthcare [17]. Addressing ethical and governance challenges, such as data privacy and algorithmic bias, is crucial for a responsible adoption of AI in healthcare. This implies the importance of robust governance and strict ethics, guiding AI implementation in a balanced and fair manner [19,20]. Commitment to research, innovation, and collaboration is essential to overcome current challenges and harness AI’s transformative potential in medicine. As recent studies have shown, AI can play a critical role in managing complex conditions like irritable bowel syndrome, offering new pathways for more effective and accurate diagnoses and treatments [21].
3.2. AI in the Healthcare Response to the COVID-19 Pandemic
The introduction to the role of artificial intelligence in the management of the COVID-19 pandemic focuses on the importance of AI in healthcare responses. Through Table 3, we outline innovative approaches and applications of AI that supported diagnostics, monitoring, and resource management during the crisis, highlighting significant advances and challenges that emerged in this critical context.

Table 3.
International research for AI in the healthcare response to the COVID-19 pandemic.
The COVID-19 pandemic has spurred an unprecedented acceleration in the field of artificial intelligence (AI), marking an era where technology has become inextricably intertwined with global healthcare strategy [24]. AI has emerged not just as a tool, but as a key protagonist in managing one of the most severe health crises of the century [25]. Amidst the tumultuous heart of the pandemic, AI took on a visionary role, leveraging advanced data mart architectures to make sense of previously unfathomable data flows [26]. It transformed raw information into lifesaving insights, improving real-time management and predicting critical conditions [27]. Early diagnosis emerged as a field where AI revolutionized response capabilities, turning radiological images and biological data into rapid and accurate diagnoses, thereby refining our lens through which we view and understand the virus [29], and accelerating the identification process for timely interventions [30]. In this context, the importance of AI in enhancing diagnostic accuracy through medical image analysis was further highlighted, providing healthcare professionals with advanced tools for rapid and precise diagnosis, crucial for timely and effective treatment of COVID-19 patients [28]. Beyond diagnosis, AI served as an architect of the future, modeling the virus’s spread with sophisticated predictive models [31], not just as a technical demonstration but as a beacon of hope, providing tools to anticipate and mitigate the virus’s impact [32]. With each prediction and simulation, AI has contributed to building a future where humanity is one step ahead of the virus, not a step behind [33]. However, the adoption of AI has not been without obstacles. It has raised complex and pressing issues regarding privacy, ethics, and governance [34]. These challenges were not mere hurdles but pivotal moments of reflection, pushing the global community to consider not just the power of AI but also the wisdom with which it is utilized [35]. In these debates, AI has been at the center of a broader conversation about how technology should be governed in an increasingly digital and interconnected world [36]. Therefore, this collection of studies is not just a set of research; it narrates a collective struggle and renewed hope. It illustrates a journey where AI has evolved from a futuristic concept to a daily ally, showing that even in the darkest times, innovation can light the path to a safer and more resilient future. This narrative underscores the crucial role of AI in pandemic management and the boundless potential awaiting when humanity and technology collaborate for the common good [37].
3.3. Technological Innovation and AI in Enhancing Healthcare
At the heart of the healthcare sector’s evolution stands AI and its revolutionary potential. This transformation is driven by technological advancements that promise to significantly enhance the efficiency and sustainability of healthcare. In this context, several pioneering studies outline a more efficient and promising future. Table 4 summarizes the key studies analyzed in the context of the impact of artificial intelligence (AI) in the healthcare sector.

Table 4.
International research for technological innovations and AI in enhancing healthcare.
The explosive growth in adopting innovative healthcare technologies is evident in research exploring various aspects of the sector. Virtual reality, for instance, is being used innovatively to enhance doctors’ skills in critical situations, showing how technology can transform the medical field [38]. The revolution in the sector is further fueled by the integration of AI, machine learning, and the Internet of Things, leading to epochal transformations [40]. A study in 2020 developed a model that improved clinical decision-making efficiency and computational costs [51], highlighting AI’s potential. However, significant challenges remain in integrating these methodologies in clinical contexts and balancing accuracy, interpretability, and computational costs. Efficient health data management, aimed at maximizing efficiency and privacy, is a key element in this evolving landscape [41]. The adoption of innovative healthcare technologies utilizes AI to improve disease diagnosis and management, increasing efficiency and reducing costs. A 2019 study in Canada developed a framework to evaluate doctors’ skills through simulations, offering a robust approach to assessing medical competencies [39]. Yet, integrating this framework into medical institutions and its validation remain open issues. Simultaneously, AI-based decision support systems are becoming crucial in the clinical environment, integrating into workflows and enhancing treatment efficacy and care quality [42,43]. AI can be leveraged to efficiently utilize untapped clinical information from electronic health records (EHRs), improving the diagnosis and management of diseases such as chronic kidney disease (CKD), thereby increasing efficiency and reducing costs [52]. The importance of standardization and safety in managing health data is emphasized, reflecting the need to adapt to modern challenges [44,45]. The interoperability and integration of health systems mark another frontier of innovation, merging technology with healthcare in revolutionary ways [46]. Further studies show how a comprehensive approach to health data management can transform care, positively affecting both patients and healthcare professionals [47].
In this evolving context, the influence of AI on clinical pathways has become particularly evident in several therapeutic areas. In the field of prevention, AI is being used to identify high-risk patients and tailor preventive interventions, utilizing data from wearable devices, electronic health records, and genomic information [65,66]. This approach not only optimizes resource allocation but also enhances the effectiveness of preventive care, reducing the overall burden on healthcare systems [67,68]. The adoption of AI and telemedicine is transforming clinical pathways by allowing patient–physician contact to be based on clinical need rather than set schedules. This shift significantly reduces unnecessary visits and hospitalizations, optimizing healthcare resources and improving the efficiency of care delivery [69,70]. Studies show that AI facilitates continuous health monitoring, enabling the prediction of acute conditions and the timely initiation of preventive measures. Specifically, integrating machine-learning models into telemedicine has demonstrated high predictive accuracy, contributing to more effective prevention and enhancing both healthcare quality and system efficiency [71]. In managing acute conditions, AI-driven triage systems are facilitating faster and more accurate diagnoses in emergency situations by processing real-time data on symptoms and vital signs [72,73]. This enables healthcare providers to respond more efficiently, improving patient outcomes. AI is also transforming the management of chronic diseases, enabling continuous patient monitoring and personalized adjustments to therapy. For example, wearable devices equipped with AI can track vital signs in real time, allowing for individualized treatment plans for conditions like Parkinson’s disease [74,75]. This reduces the strain on healthcare professionals while ensuring better adherence to treatment by patients [76]. Rehabilitation, though not as widely discussed, is another area where AI is making significant strides. Personalized rehabilitation programs that adapt to the patient’s progress are now possible through AI, and remote monitoring via telemedicine ensures that patients can continue their rehabilitation at home, maintaining continuity in their care while reducing the need for hospital visits [77,78,79].
In the evolving healthcare sector, AI and emerging technologies play a critical role in providing personalized, high-quality care. These tools address current challenges and pave the way for a future where healthcare is enhanced by AI integration, underscoring the importance of innovation, collaboration, and adaptation. Studies have highlighted AI’s use in customizing care, enabling targeted treatments [48], and its application in early disease diagnosis, opening new avenues for preventive health [49]. The synergy between healthcare professionals and AI systems has been explored to optimize care [50]. Research has also delved into specific areas like AI in diagnosing and treating mental illnesses, presenting innovative solutions to improve patient life quality [53], chronic disease management using AI, Big Data, IoT, and knowledge graphs [54], and the centralized, secure management of health data leveraging cloud and AI capabilities [55]. Analyses of deep-learning methods in various medical conditions provides an innovative perspective on these technologies’ potential to enhance diagnosis and treatment [56]. Further research explores chronic disease management using AI, Big Data, IoT, and knowledge graphs for optimized long-term care [57]. The maturity of hospital management models, particularly in light of lessons learned from COVID-19, indicates improvement areas for future models [58,59,60,61,62,63,64]. Advanced data analysis and sophisticated methods like feature engineering in EEG are opening new frontiers in diagnosing and treating mental disorders, demonstrating how technology–medical integration can significantly improve patient life quality [53]. Developments in telemedicine technologies, ranging from handwriting analysis to neonatal sound analysis, are revolutionizing remote care access and quality [54]. The centralized and secure management of health data, utilizing the cloud and AI power, offers new possibilities for clinical management, albeit with challenges in stakeholder collaboration and data integration [55].
3.4. Security and Intelligent Platfroms: AI as a Driver or Change in Healthcare
In the era of healthcare digitalization, big data and artificial intelligence (AI) are emerging as powerful catalysts for innovation and transformation in the sector. These technologies not only improve security, efficiency, and quality of care, but are also redefining healthcare management. A detailed overview of these innovations and their impacts can be found in Table 5, which summarizes key international research in the field.

Table 5.
International Research for Security and Intelligent Platforms.
The convergence of big data and AI is opening new frontiers in innovation and predictive analysis in healthcare, introducing intelligent platforms that improve population health management and value-based care. For instance, the integration of a big data and ML platform in Colombia has led to significant improvements in healthcare outcomes and decision making [80]. A notable example is the design of a healthcare knowledge management system in Vietnam [81], which demonstrated how the integration of big data and AI can facilitate the effective management of large volumes of healthcare data. This study highlights the importance of well-designed knowledge management systems for processing and analyzing complex data in healthcare.
The use of AI and big data is revolutionizing decision making in healthcare. For example, in China, a big data-based decision-making model for prostate cancer has shown improvement in diagnostic efficiency, offering a concrete example of how these technologies can be applied in real clinical contexts [82]. However, challenges such as the need to ensure data privacy and the integration of these technologies into existing systems also emerge. Additionally, the use of big data and AI in rheumatic and musculoskeletal diseases (RMDs) in the European Union [84] has highlighted the ability to identify relevant data sources and analysis methods, essential for improving diagnosis and treatment of these conditions.
In the field of disease diagnosis, a joint study between Saudi Arabia and South Korea [87] proposed a deep-learning model for the Internet of Medical Things (IoMT), enhancing privacy and efficacy in disease diagnosis. This approach represents a significant step forward in ensuring the security of sensitive data in connected environments. In Indonesia, the development of a smart healthcare system based on a cyber-physical system and deep federated learning architectures [85] has demonstrated how the integration of advanced technologies can improve the efficiency and security of healthcare systems, addressing challenges of both a technical and data privacy nature.
In terms of data security, the implementation of blockchain technology, as illustrated in a global study [83], has significantly improved the security and interoperability of healthcare data. This emphasizes the need for specific technological innovations to address security challenges in an increasingly digitalized environment.
These innovations also require updates in healthcare policies and medical training, to adapt to technological changes and ensure effective use of these technologies. For example, the federated learning model in Italy for brain tumor segmentation [86] has not only improved effectiveness but also laid the foundation for new skills needed by healthcare professionals. The “DeepBlockShield” [88] represents a qualitative leap in healthcare data security, employing blockchain to effectively protect clinical data, especially those from the deep web. Developed in South Korea, this model establishes new standards in data protection in the healthcare sector, underscoring the growing importance of data security in the digital era. Looking to the future, the expected evolution of intelligent platforms and AI in healthcare includes the development of advanced AI systems and the integration of these technologies into new clinical areas. These studies represent a body of work that not only documents the innovative use of AI and intelligent platforms but also lays the groundwork for their future use in more complex care scenarios, enhancing the resilience and effectiveness of healthcare systems [89,90,91].
The increasing use of AI and big data in the healthcare sector not only testifies to their crucial role in healthcare management but also highlights the limitless potential that awaits when technology and human ingenuity work together for the common good.
3.5. Artificial Intelligence and Resource Management in Healthcare: Towards a Smart and Sustainable Future
Artificial intelligence (AI) emerges as a true force of change, shaping the future of healthcare systems by endowing them not only with greater intelligence but also with remarkable sensitivity to individual needs. The innovations within these systems, guided by a data-driven multimodal approach, have been meticulously documented in Table 6.

Table 6.
International Research for AI and resource management in healthcare.
These solutions, ranging from disease analysis to diagnosis and treatment, underscore the crucial importance of effective data management and improved decision-making processes [92]. This evolution has been inspired by the rapid development of AI-based medical services, which are radically transforming healthcare delivery. In this rapidly evolving context, the study by Almalawi et al. (2022) represents a further advancement, exploring the use of artificial intelligence to optimize resource management in the healthcare sector [93].
The management of healthcare information is currently at a critical juncture, with the need to integrate numerous independent applications into more cohesive and reliable systems [94]. This demand for coherence and quality in healthcare information systems is driving innovative solutions that can significantly enhance the efficiency and dependability of intelligent healthcare systems. Simultaneously, the study by Wu (2023) makes a significant contribution by investigating the impact of AI on treatment personalization and patient management, highlighting how AI can facilitate more accurate diagnoses and tailored treatments [95].
However, a critical element for the success of efficient and intelligent healthcare systems is trust in AI. Despite the sometimes-human-like performance of AI models, their perception as “black boxes” limits practical application, especially in the healthcare field. This is where explainable artificial intelligence (XAI) comes into play [96]. XAI provides transparency in model predictions and encourages the use of AI systems in the healthcare sector, paving the way for the development of holistic systems for smart cities. Furthermore, the study by Yang et al. (2022) offers an innovative perspective on the use of AI to enhance patient safety and risk management, demonstrating how AI-based decision support systems can identify potential risks in real time [97].
Each research endeavor in this field contributes to a broader narrative, showcasing not only the evolution of healthcare in the digital age but also anticipating the future of the sector. This future envisions AI and emerging technologies as essential partners in delivering enhanced and personalized healthcare [98,99,100], integrating resource management into an increasingly intelligent and efficient context.
Similarly, these studies do not confine themselves to immediate challenges but also address the specific implications of AI in key sectors. For example, some studies explore the innovation of federated learning in the healthcare sector [101], while others focus on security in the context of Healthcare 5.0 [102]. Still, others analyze the positive impact of AI and human resources analytics in the healthcare sector [103] or tackle resource management in healthcare economics through data-driven methods [104]. Meanwhile, some studies examine patient and public perceptions of AI in healthcare [105] or advocate for the use of semantic ontologies for more effective integration [106]. Finally, others offer innovative approaches to optimize inventory management in the healthcare sector [107], thereby contributing to more intelligent resource management in an increasingly advanced healthcare environment.
4. Discussion
Our systematic review, which scrutinized 79 studies from 2019 to 2023, has illuminated how artificial intelligence (AI) is significantly shaping the healthcare sector, outlining five main thematic areas that reflect the broad spectrum of applications and challenges associated with AI in healthcare management. These areas include: 1. AI for quality assurance and stakeholder engagement, 2. AI in the healthcare response to the COVID-19 pandemic, 3. Technological innovations to enhance healthcare, 4. Security and smart platforms as drivers of change, and 5. Resource management towards a sustainable future. These themes underscore the versatility and transformative potential of AI.
AI for quality assurance and stakeholder engagement (QUALITY) emphasizes the importance of maintaining high standards of care and actively involving all healthcare sector stakeholders in the digitalization process. This aspect is crucial to ensure that technological innovations genuinely enhance patient care and are embraced by doctors, patients, and other healthcare professionals. AI in the healthcare response to the COVID-19 pandemic (COVID-19) has shown how advanced technologies can be swiftly employed to address global health emergencies, offering tools for diagnosis, contact tracing, and hospital resource management. This has highlighted AI as an essential tool in combating pandemics and other health crises. Technological innovations and AI in enhancing healthcare (TECHINNOVATION) reflect the sector’s ongoing evolution, where AI contributes to pushing the boundaries of medicine, from discovering new treatments to personalizing care. This thematic area highlights AI’s role in accelerating innovation and improving operational efficiency. Security and smart platforms (SECURITY) focus on the need to protect sensitive patient data and ensure the safety of implemented AI systems. The increasing integration of AI raises privacy and security issues that must be addressed to maintain user trust and comply with regulations. Lastly, AI and resource management in healthcare (RESOURCE) shed light on how AI can contribute to more efficient resource use, both in terms of costs and environmental sustainability. Optimizing resource management is vital to address the sector’s future challenges, including the growing demand for services.
In conclusion, our analysis reveals that, despite the considerable opportunities offered by AI in healthcare, significant challenges persist, particularly regarding data privacy, ethics, and technological integration. It is evident that a holistic and collaborative approach, involving all stakeholders and guided by robust governance and clear ethical principles, will be crucial to fully leverage AI’s potential in improving healthcare. Our research underscores the importance of continuing to explore these thematic areas to maximize AI’s benefits, overcoming current obstacles and unlocking its full transformative potential in the healthcare sector.
4.1. Experiments
In this section, we will apply predictive machine-learning algorithms to explore the impact of artificial intelligence (AI) on healthcare management from 2019 to 2023, with a particular focus on different global geographical areas. Using the analysis tables from the review, we have categorized the columns after careful analysis, distinguishing the target variable “Topic” (Table 1) and the model features (Discipline, Methodologies, Challenges, Results). This methodology will allow us to evaluate in detail the influence of AI in various national contexts, providing an overview of trends, challenges, and future opportunities in the healthcare sector. The selected variables have been categorized as described in Table 7.

Table 7.
Variable classification for the predictive model.
The dataset consists of 79 instances, each representing a unique study identified in the systematic review. The studies are categorized according to the target variable “Topic” and features, which include discipline, methodologies, challenges, and results. This classification provides a structured approach to understanding AI’s impact across different regions and healthcare contexts.
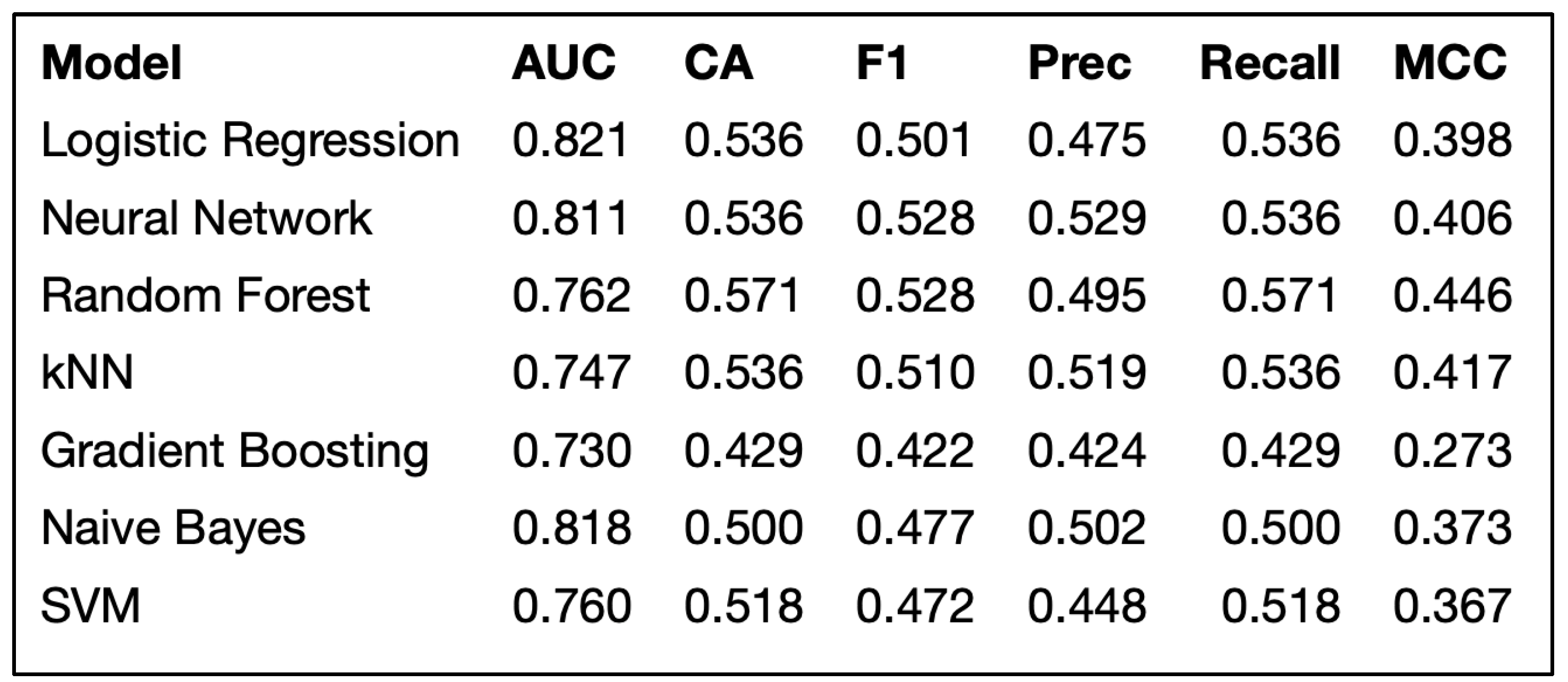
4.2. Application of the Predictive Model
By employing a dual-validation approach, combining data sampling with 70% for training and 30% for testing, alongside a 10-fold cross-validation, we rigorously assessed machine-learning predictive models including logistic regression, Neural Networks, Naive Bayes, Random Forest, SVM, Gradient Boosting, and kNN. This method provided a reliable estimate of model performance, identifying logistic regression as the most effective based on key metrics [108]. The relevance of such machine-learning techniques in deriving relevant insights and predictive frameworks from complex data sets has been previously highlighted and confirmed in analogous research within the realm of hospital facility efficiency analysis, public health efficacy, and the resulting patient health mobility [109,110,111]. logistic regression demonstrated an AUC of 0.821, showcasing its effectiveness in healthcare management analysis. These findings, depicted in Figure 2, offer a solid foundation for the informed selection of the most suitable predictive model for analyzing AI’s impact on healthcare management. The AUC was chosen as the primary metric due to its ability to provide a comprehensive measure of model performance across all classification thresholds, offering a balanced evaluation of both sensitivity and specificity.
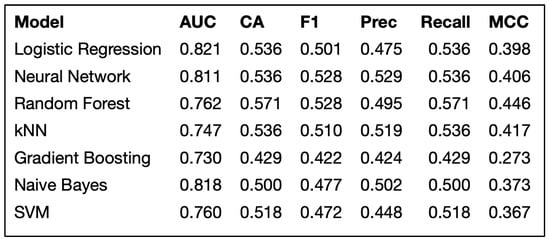
Figure 2.
Predictive models performances.
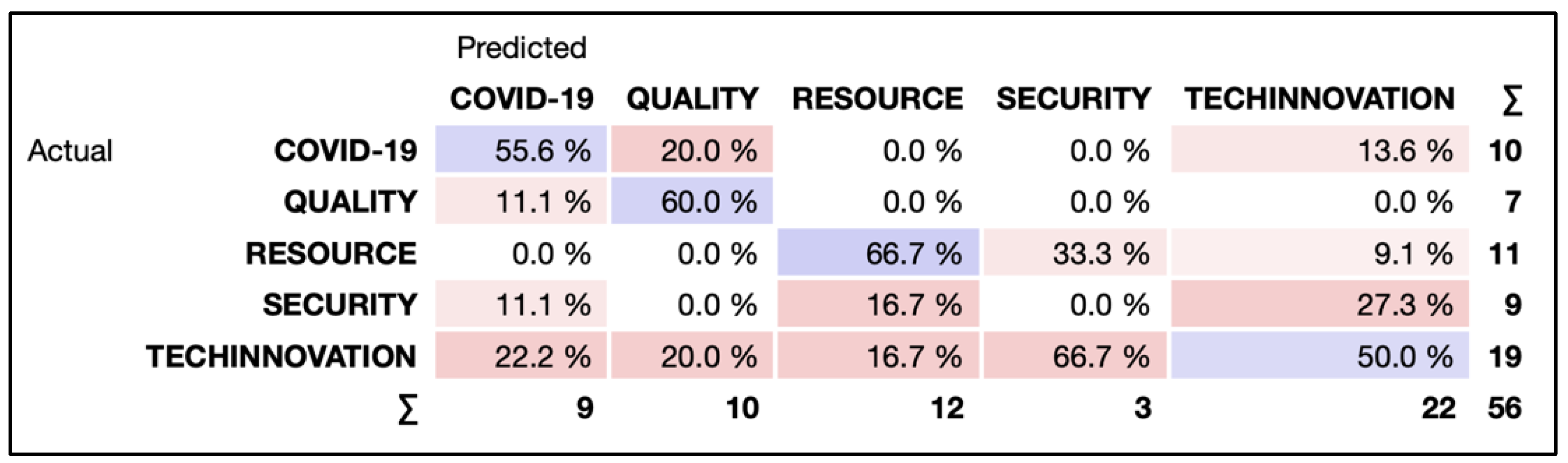
The analysis provided by the confusion matrix, shown in Figure 3, offers an optimistic view on the predictive model’s effectiveness in classifying studies and research within AI in healthcare management. Its notable percentage of 55.6% in correctly recognizing COVID-19 related research highlights the model’s strength in identifying specific themes, despite challenges from overlapping areas like service quality and technological innovation. The colors in Figure 3 aid visual interpretation, with purple tones representing correct classifications and red indicating misclassifications; darker shades correspond to higher percentages. This outcome underscores the importance of continually refining classification strategies to address such challenges.
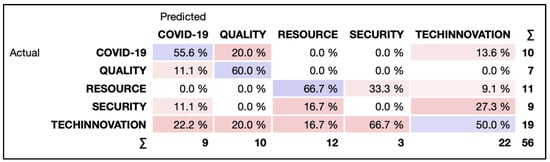
Figure 3.
Confusion matrix for logistic regression.
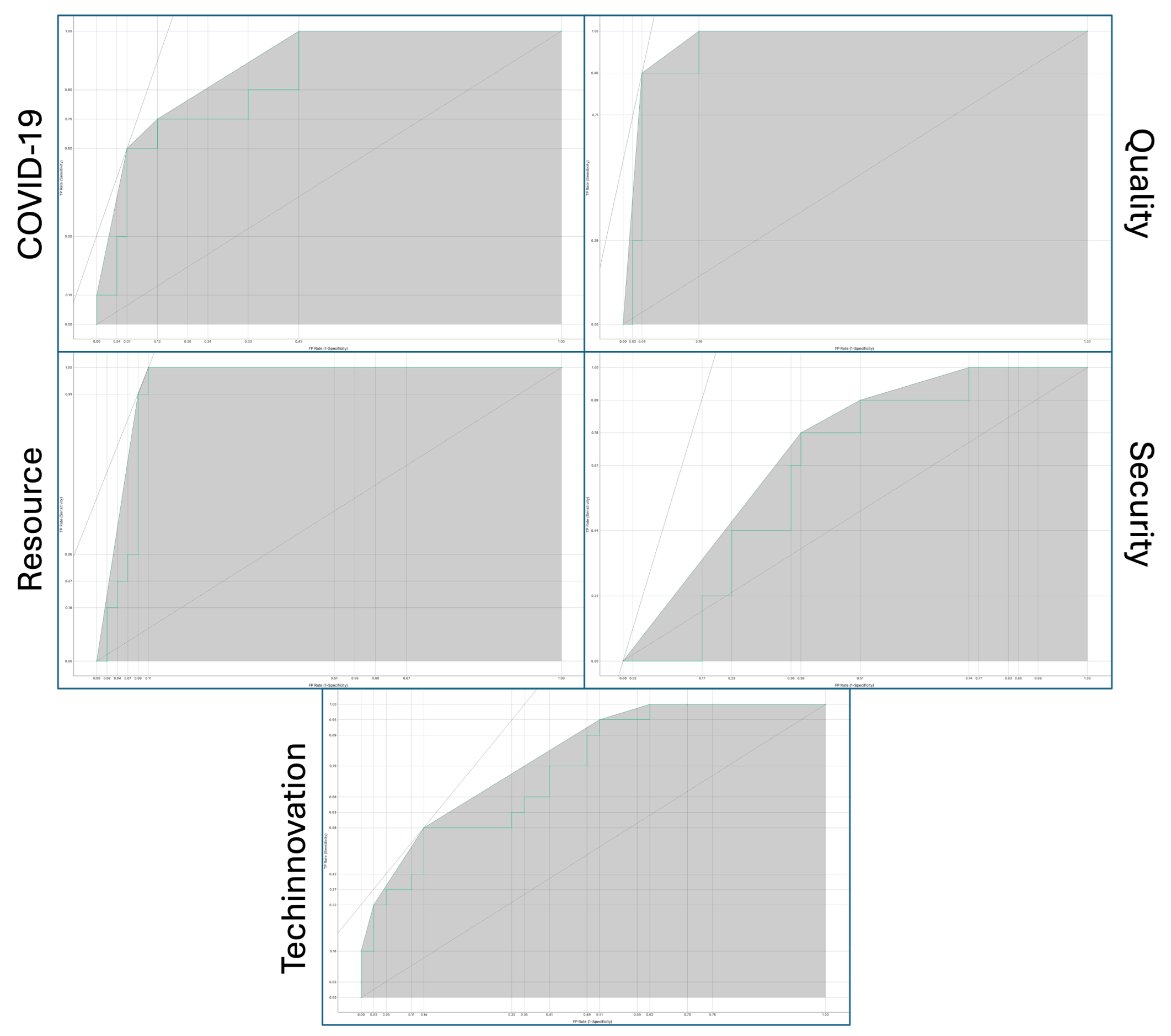
Simultaneously, the model demonstrated good performance in correctly identifying studies on resource management, with a percentage of 66.7%, and on quality, with a percentage of 60.0%. These results highlight the model’s value in enhancing operational efficiency and sustainability in healthcare. However, the precision in the security category was low, with a percentage of 0.0%, while for technological innovation, the model achieved a percentage of 50.0%. This suggests that despite difficulties in precisely attributing some research to a specific category, technological innovation remains a powerful and pervasive driver of progress in healthcare. Figure 4, a key graphical element in the study, displays the logistic regression ROC curves for each of the five target variable classes, providing a visual assessment of the model’s ability to correctly classify observations within each specific category by showing the trade-off between true positive rates and false positive rates at various decision thresholds. The area under the ROC curve (AUC) value for each category further evaluates and compares model performance in terms of sensitivity and specificity.
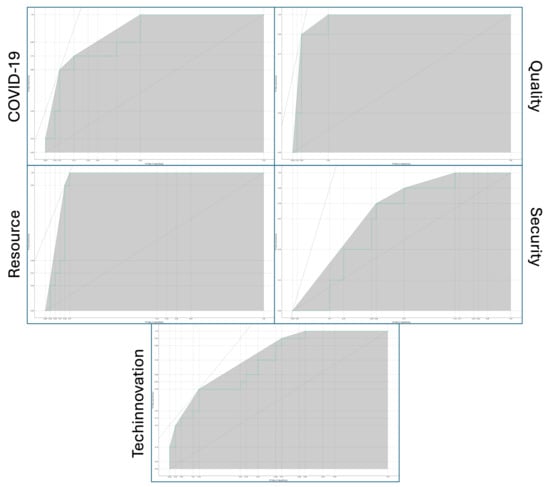
Figure 4.
Receiver Operating Characteristic (ROC) Curves for logistic regression across five target classes.
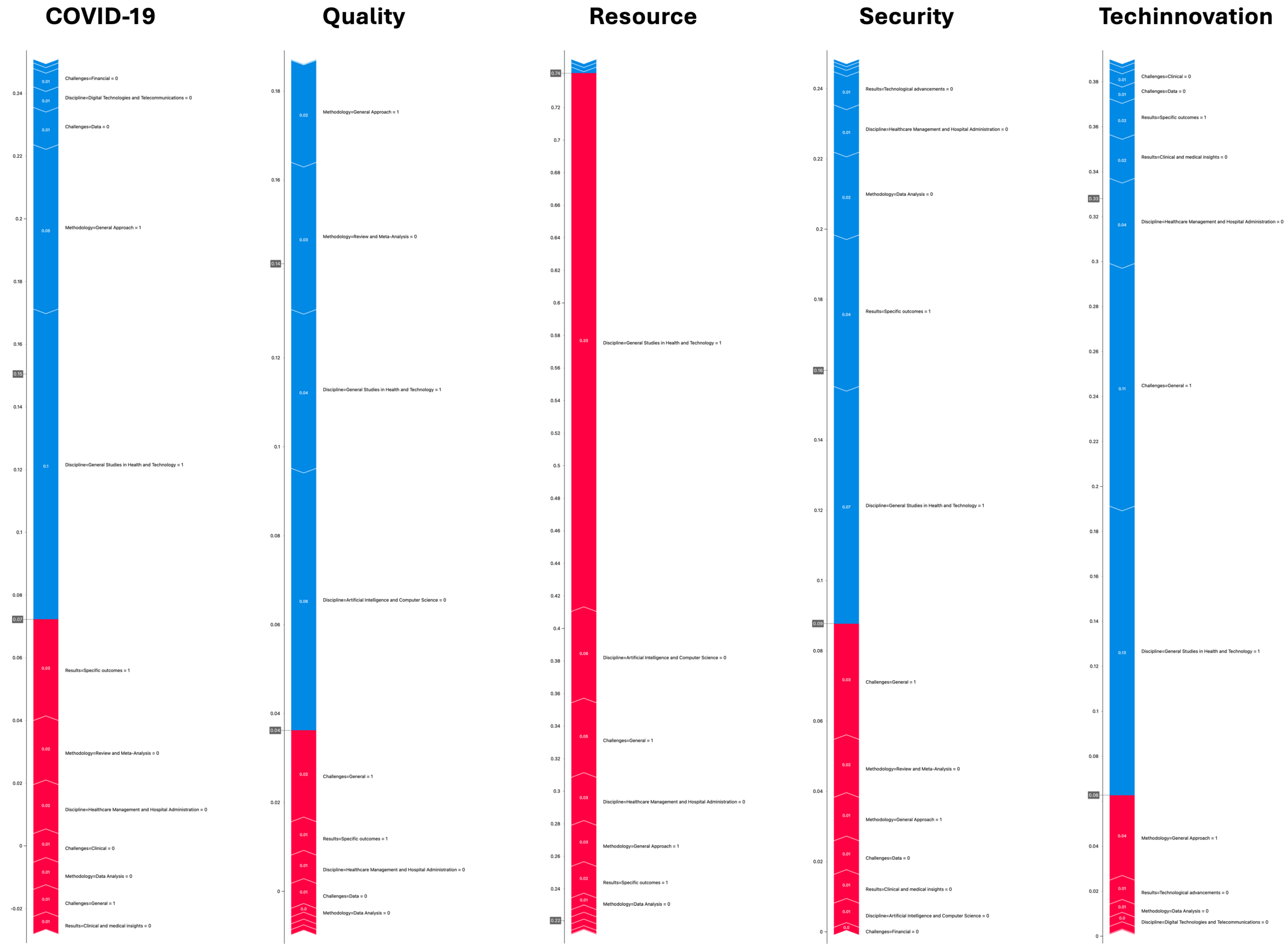
To delve deeper into our predictive model’s predictions, we utilized the SHAP (SHapley Additive exPlanations) algorithm, an advanced tool for interpreting machine-learning model decisions. This algorithm’s application has enabled us to understand the impact of each feature on the model’s decisions, providing a transparent and easily interpretable view of the dynamics underlying the predictions. The results of this analysis for the five target variable classes are shown in Figure 5, highlighting the contribution of each independent variable to the model’s predicted outcome. The SHAP numerical values are represented in Table 8.
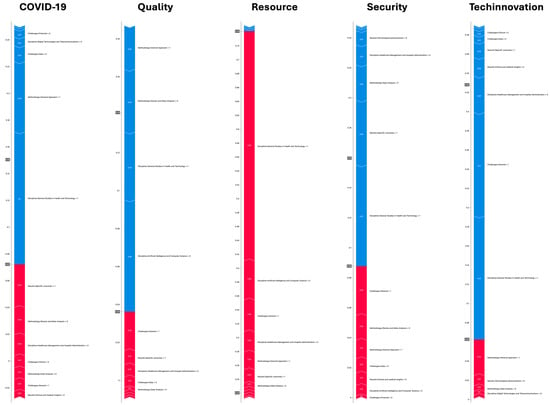
Figure 5.
SHAP value analysis for predictive model targets.

Table 8.
SHAP numeric value for predictive model targets.
Based on the updated SHAP values provided for each instance and for each column, related to the five topics of our systematic review on the impact of artificial intelligence on healthcare management, we can interpret the results as follows:
- Clinical and Medical Insights: These have a moderate positive impact on COVID-19, Quality, and Resource, with SHAP values of 0.00558636, 0.00117473, and 0.00446783, respectively. This suggests that clinical insights are slightly more influential in research related to COVID-19 and resource management. However, they have a significant negative impact on Techinnovation (−0.0194271), indicating that for technological innovations, other factors may be more relevant.
- Specific Outcomes: They show a significant positive impact on COVID-19 (0.0322289) and on Quality and Resource with smaller values, but a very negative impact on Security (−0.0431382). This could reflect the importance of specific outcomes in COVID-19 research and their lesser relevance for security studies.
- Clinical Challenges: Clinical challenges have a small positive impact on COVID-19 (0.00912065) and Quality (0.00155511), suggesting that clinical issues are relevant but not dominant in these fields. It is interesting to note the slight negative impact on Resources (−0.00374929), perhaps indicating that clinical challenges are less central in resource management.
- Data Challenges: These challenges show a negative impact on COVID-19 (−0.0119134) but a positive, albeit smaller, impact on Quality (0.00559921). This may indicate that while data-related challenges are perceived as problematic in COVID-19 research, they may provide opportunities for improvement in quality.
- General: A significant variation in the impact of general challenges, with a strong positive impact on Resource (0.0458024) and a very negative impact on Techinnovation (−0.107902), highlights how general challenges are seen as crucial in resource management but hinder technological innovation.
- Methodology—General Approach: This has a strong negative impact on COVID-19 (−0.0524088) and Quality (−0.0229678) but a positive impact on Techinnovation (0.0377616), suggesting that a nonspecific methodological approach is less useful for direct studies but advantageous for technological innovation.
- Discipline—General Studies in Health and Technology: These studies have an extremely positive impact on Resources (0.330612) but a negative impact on Techinnovation (−0.128479), highlighting the importance of general research in resource management and its limiting impact on technological innovation.
- Model Predictions: The model predictions show the highest confidence in the Resource category (0.74) compared to others, suggesting that the analyzed features are particularly indicative of studies focused on resource management.
The analysis of SHAP values thus provides valuable insights into how different features influence the classification of studies in the target categories, highlighting the intersection of methodology, discipline, challenges, and outcomes in AI research in healthcare management. This detailed understanding helps delineate specific areas of strength and potential improvements in the predictive model.
4.3. Analysis of Topics by Years and Geographical Area
In response to research question Q2, which aims to analyze the evolution of artificial intelligence (AI) in healthcare between 2019 and 2023, we refer to a contingency table that correlates the assignment of topics we identified to the 79 articles emerging from our systematic review (Table 9). These themes, defined as “COVID-19, Quality, Resource, Security, and Techinnovation”, are arranged in columns and represent the areas of greatest investigative interest. The rows of the table are allocated to both the years from 2019 to 2023 and various geographical areas, allowing us to outline not only the temporal evolution of research themes but also to assess how these trends are distributed globally. The studies analyzed have been grouped into broad geographical areas such as Africa, Asia Pacific, Europe, International, Latin America, the Middle East, and North America, providing a comprehensive overview of regional dynamics. This approach highlights how various factors, including technological innovations, health emergencies, and health policy priorities, have influenced the adoption and development of AI solutions in healthcare across different geographical contexts. This multidimensional analysis enables a deep understanding of the global impact of AI on research and healthcare practices over the considered period.

Table 9.
Contingency table.
The updated contingency table, alongside the χ2 test results, provides a detailed analysis of the research distribution across the 79 initially selected articles, focusing on the impact of artificial intelligence (AI) on healthcare management across different geographical areas and time periods, within the five thematic scopes of our systematic review. Each geographical area exhibits a distinct profile of interest and focus that evolves over time, as evidenced by the thematic distribution percentages.
In 2022, Africa stands out for its exclusive focus on COVID-19 research, accounting for 3% of the total publications, suggesting a peak of interest or a response to specific needs imposed by the pandemic in that year, with no research recorded in other periods.
The Asia Pacific region demonstrates an evolution of interests, moving from RESOURCE and SECURITY themes, which constituted 22.2% of the research in 2019, to an increased focus on TECHINNOVATION, representing 13.6% of the research by 2023. This trend reflects a growing propensity towards the adoption of innovative technological solutions, with a significant rise in interest towards TECHINNOVATION reaching 40.9% of the total in 2023.
Europe displays a diversified interest across the years, with a peak for QUALITY themes, representing 12.1% in 2022, and an even distribution between QUALITY and TECHINNOVATION in 2023, indicating a shift towards research on technological and quality innovation. This is highlighted by TECHINNOVATION constituting 18.2% of the total research in 2023.
International collaborations show a pronounced inclination towards RESOURCE and TECHINNOVATION themes, emphasizing the significance of these areas in broad studies and cross-national cooperation, with TECHINNOVATION accounting for 33.3% of the research in 2019 and 30.0% in 2021.
Latin America reveals an exclusive interest in TECHINNOVATION in 2020, potentially reflecting a pivotal moment or event that focused attention on this area, though no research is recorded in other years.
The Middle East presents a variety of interests in 2022, with an equal distribution among QUALITY, RESOURCE, and TECHINNOVATION, indicating a holistic approach to healthcare research that considers various aspects of AI use. This is represented by a distribution of 12.1% across different themes in 2022.
North America, in 2022 and 2023, heavily focuses on TECHINNOVATION, highlighting how technological innovation has become a central pillar of research in the region, with interest remaining steady at 3.0% in 2022 and increasing to 9.1% in 2023.
The aggregated χ2 test analysis reveals a significant variation in AI research themes within healthcare management, with a χ2 value of 44.9 and a p-value of 0.006, suggesting that changes over the years, such as the emergence of COVID-19 or technological advancements, have influenced research priorities. This statistical significance underscores the impact of global events and technological evolution on healthcare research interests, emphasizing the importance of temporal analysis to understand the dynamics driving focus towards specific research themes.
5. Conclusions
In addressing the research question of “The role of artificial intelligence (AI) in healthcare management”, a complex picture emerges where AI is positioned as a transformative force with significant impacts, inherent limitations, and promising prospects. AI is revolutionizing healthcare by offering innovative tools for diagnostics, personalized treatment, crisis management, and resource optimization. Through analyzing large data volumes and learning from complex patterns, AI enhances care quality, diagnostic accuracy, and operational efficiency, contributing to more informed and outcome-based healthcare management.
The impacts of AI are tangible and multifaceted. In health crises, like the COVID-19 pandemic, AI has proven to be a vital tool for rapid data analysis, virus spread forecasting, and early diagnosis assistance. Moreover, AI-based intelligent systems are enhancing healthcare resource management, optimizing hospital bed allocation, staff distribution, and medication stock management. These systems not only make healthcare more responsive but also contribute to more strategic and forward-thinking planning.
The widespread acceptance of internet-connected mobile devices, like smartphones and wearables, has positioned AI and telemedicine as ideal solutions for enhancing healthcare in a practical and cost-effective way. This shift aligns perfectly with the growing demand for faster, more accessible, and personalized care, while also optimizing the effectiveness and efficiency of healthcare services.
AI has proven effective in identifying high-risk patients, managing acute conditions through advanced triage systems, and enabling personalized monitoring of chronic diseases via wearable devices. Additionally, AI-based telemedicine supports home rehabilitation by ensuring continuity of care and reducing the need for hospital visits. These advancements reinforce AI’s role as a crucial tool for real-time healthcare management, fostering a more personalized and responsive approach to patient care.
AI and telemedicine are reshaping clinical pathways by replacing scheduled appointments with interactions based on real clinical needs. This flexible model, aligned with the growing use of digital health devices, reduces unnecessary interventions and optimizes resources and time. Additionally, AI’s predictive capacity provides a preventive edge, allowing timely interventions that ensure more targeted and effective care.
However, integrating AI into healthcare is not without limits and challenges. Issues related to privacy, data security, and the risk of algorithmic bias require constant attention. The “black box” nature of many AI systems raises concerns about transparency and explainability in AI-based medical decisions. Additionally, resistance to change within healthcare institutions and the need for proper medical staff training represent further obstacles to widespread AI adoption.
Our study has both theoretical and practical objectives, supported by concrete recommendations. Theoretically, it clarifies AI’s role in healthcare management through a combined approach of systematic review and predictive algorithms, providing an overview of its impact on processes, patient care, and emergency response. Practically, it examines how AI enhances efficiency, reduces costs, and optimizes resources at operational, strategic, and emergency response levels, with specific focus on the period 2019–2023 and the challenges posed by the pandemic.
We provide recommendations to support responsible AI adoption in healthcare, emphasizing a collaborative approach that includes all stakeholders, robust data privacy and security, and continuous training for healthcare professionals. Finally, we highlight the importance of ongoing research to improve AI capabilities and address emerging ethical challenges.
The study presents some limitations related to the use of traditional machine-learning methods, such as logistic regression, which, while offering interpretability, do not fully capture the complexity of nonlinear relationships in the data. Additionally, the SHAP (SHapley Additive exPlanations) algorithm has not been fully explored in interpreting models on large datasets or complex nonlinear relationships, limiting transparency in decision making in these scenarios.
In the future, adopting more advanced techniques, such as deep learning or ensemble methods, could improve performance, especially for larger or more complex datasets. These approaches, although more computationally intensive, can reveal deeper patterns and correlations in healthcare data. Integrating the SHAP algorithm into these advanced models could enhance the interpretability of AI-driven decisions, helping to overcome the “black box” problem and fostering greater trust and acceptance among clinicians and patients.
Despite these limitations, the prospects of AI in healthcare management are broad and promising. Ongoing research and the development of more transparent and interpretable AI models can improve trust and adoption of these technologies. Increasing focus on explainable artificial intelligence (XAI) aims to make AI systems more understandable and reliable for clinicians and patients. Simultaneously, the evolution of privacy and data security regulations can provide a more solid framework for sensitive information protection.
In conclusion, AI represents a powerful catalyst for change in the healthcare sector, with the potential to significantly improve healthcare management. Its impacts are vast, the limitations non-negligible, and the prospects full of opportunities to overcome current challenges. As AI continues to evolve, a deep understanding and a balanced approach will be essential to fully leverage its potential for the benefit of global health.
Author Contributions
Conceptualization, V.S., C.T., N.F., M.I. and A.M.; Methodology, V.S., C.T., N.F., M.I. and A.M.; Software, V.S. and A.M.; Validation, V.S., C.T., N.F. and M.I.; Formal analysis, V.S., C.T., N.F., M.I. and A.M.; Data curation, A.M.; Writing – original draft, V.S., C.T., N.F., M.I. and A.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable
Informed Consent Statement
Not applicable
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Marengo, A.; Pagano, A.; Ladisa, L. Towards a mobile augmented reality prototype for corporate training. In Proceedings of the 16th European Conference on e-Learning (ECEL), Porto, Portugal, 26–27 October 2017; pp. 362–366. [Google Scholar]
- Johnson, J.; Simms-Ellis, R.; Janes, G.; Mills, T.; Budworth, L.; Atkinson, L.; Harrison, R. Can we prepare healthcare professionals and students for involvement in stressful healthcare events? A mixed-methods evaluation of a resilience training intervention. BMC Health Serv. Res. 2020, 20, 1094. [Google Scholar] [CrossRef] [PubMed]
- Dave, M.; Patel, N. Artificial intelligence in healthcare and education. Br. Dent. J. 2023, 234, 761–764. [Google Scholar] [CrossRef] [PubMed]
- Brambilla, A.; Sun, T.-Z.; Elshazly, W.; Ghazy, A.; Barach, P.; Lindahl, G.; Capolongo, S. Flexibility during the COVID-19 Pandemic Response: Healthcare Facility Assessment Tools for Resilient Evaluation. Int. J. Environ. Res. Public Health 2021, 18, 11478. [Google Scholar] [CrossRef]
- Prakash, S.; Balaji, J.N.; Joshi, A.; Surapaneni, K.M. Ethical Conundrums in the Application of Artificial Intelligence (AI) in Healthcare-A Scoping Review of Reviews. J. Pers. Med. 2022, 12, 1914. [Google Scholar] [CrossRef] [PubMed]
- Cacciamani, G.E.; Chu, T.N.; Sanford, D.I.; Abreu, A.; Duddalwar, V.; Oberai, A.; Kuo, C.-C.J.; Liu, X.; Denniston, A.K.; Vasey, B.; et al. PRISMA AI reporting guidelines for systematic reviews and meta-analyses on AI in healthcare. Nat. Med. 2023, 29, 14–15. [Google Scholar] [CrossRef]
- Joshi, G.; Jain, A.; Araveeti, S.R.; Adhikari, S.; Garg, H.; Bhandari, M. FDA-Approved Artificial Intelligence and Machine Learning (AI/ML)-Enabled Medical Devices: An Updated Landscape. Electronics 2024, 13, 498. [Google Scholar] [CrossRef]
- Pisapia, A.; Banfi, G.; Tomaiuolo, R. The novelties of the regulation on health technology assessment, a key achievement for the European union health policies. Clin. Chem. Lab. Med. CCLM 2022, 60, 1160–1163. [Google Scholar] [CrossRef]
- Wang, C.; Zhang, J.; Lassi, N.; Zhang, X. Privacy Protection in Using Artificial Intelligence for Healthcare: Chinese Regulation in Comparative Perspective. Healthcare 2022, 10, 1878. [Google Scholar] [CrossRef] [PubMed]
- Townsend, B.A.; Sihlahla, I.; Naidoo, M.; Naidoo, S.; Donnelly, D.-L.; Thaldar, D.W. Mapping the regulatory landscape of AI in healthcare in Africa. Front. Pharmacol. 2023, 14, 1214422. [Google Scholar] [CrossRef]
- Marengo, A.; Pagano, A. Investigating the Factors Influencing the Adoption of Blockchain Technology across Different Countries and Industries: A Systematic Literature Review. Electronics 2023, 12, 3006. [Google Scholar] [CrossRef]
- Moldt, J.-A.; Festl-Wietek, T.; Madany Mamlouk, A.; Nieselt, K.; Fuhl, W.; Herrmann-Werner, A. Chatbots for future docs: Exploring medical students’ attitudes and knowledge towards artificial intelligence and medical chatbots. Med. Educ. Online 2023, 28, 2182659. [Google Scholar] [CrossRef] [PubMed]
- Bartels, R.; Dudink, J.; Haitjema, S.; Oberski, D.; van ‘t Veen, A. A Perspective on a Quality Management System for AI/ML-Based Clinical Decision Support in Hospital Care. Front. Digit. Health 2022, 4, 942588. [Google Scholar] [CrossRef] [PubMed]
- Shams, R.A.; Zowghi, D.; Bano, M. AI and the quest for diversity and inclusion: A systematic literature review. AI Ethics 2023. [Google Scholar] [CrossRef]
- Thomassin-Naggara, I.; Balleyguier, C.; Ceugnart, L.; Heid, P.; Lenczner, G.; Maire, A.; Séradour, B.; Verzaux, L.; Taourel, P.; Conseil, national professionnel de la radiologie et imagerie medicale (G4). Artificial intelligence and breast screening: French Radiology Community position paper. Diagn. Interv. Imaging 2019, 100, 553–566. [Google Scholar] [CrossRef]
- Feng, J.; Phillips, R.V.; Malenica, I.; Bishara, A.; Hubbard, A.E.; Celi, L.A.; Pirracchio, R. Clinical artificial intelligence quality improvement: Towards continual monitoring and updating of AI algorithms in healthcare. npj Digit. Med. 2022, 5, 66. [Google Scholar] [CrossRef]
- Boonstra, A.; Laven, M. Influence of artificial intelligence on the work design of emergency department clinicians a systematic literature review. BMC Health Serv. Res. 2022, 22, 669. [Google Scholar] [CrossRef] [PubMed]
- Lorenzon, M.; Spina, E.; Franco, F.T.D.; Giovannini, I.; Vita, S.D.; Zabotti, A. Salivary Gland Ultrasound in Primary Sjögren’s Syndrome: Current and Future Perspectives. Open Access Rheumatol. Res. Rev. 2022, 14, 147–160. [Google Scholar] [CrossRef]
- Hogg, H.D.J.; Al-Zubaidy, M.; Talks, J.; Denniston, A.K.; Kelly, C.J.; Malawana, J.; Papoutsi, C.; Teare, M.D.; Keane, P.A.; Beyer, F.R.; et al. Stakeholder Perspectives of Clinical Artificial Intelligence Implementation: Systematic Review of Qualitative Evidence. J. Med. Internet Res. 2023, 25, 39742. [Google Scholar] [CrossRef]
- Miller, G.J. Stakeholder roles in artificial intelligence projects. Proj. Leadersh. Soc. 2022, 3, 100068. [Google Scholar] [CrossRef]
- Kordi, M.; Dehghan, M.J.; Shayesteh, A.A.; Azizi, A. The impact of artificial intelligence algorithms on management of patients with irritable bowel syndrome: A systematic review. Inform. Med. Unlocked 2022, 29, 100891. [Google Scholar] [CrossRef]
- Alcocer Alkureishi, M.; Lenti, G.; Choo, Z.-Y.; Castaneda, J.; Weyer, G.; Oyler, J.; Lee, W.W. Teaching Telemedicine: The Next Frontier for Medical Educators. JMIR Med. Educ. 2021, 7, e29099. [Google Scholar] [CrossRef] [PubMed]
- Ponce, B.A.; Brabston, E.W.; Zu, S.; Watson, S.L.; Baker, D.; Winn, D.; Guthrie, B.L.; Shenai, M.B. Telemedicine with mobile devices and augmented reality for early postoperative care. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 4411–4414. [Google Scholar] [CrossRef]
- Murri, R.; Masciocchi, C.; Lenkowicz, J.; Fantoni, M.; Damiani, A.; Marchetti, A.; Sergi, P.D.A.; Arcuri, G.; Cesario, A.; Patarnello, S.; et al. A real-time integrated framework to support clinical decision making for COVID-19 patients. Comput. Methods Programs Biomed. 2022, 217, 106655. [Google Scholar] [CrossRef] [PubMed]
- Enughwure, A.A.; Febaide, I.C. Applications of Artificial Intelligence in Combating COVID-19: A Systematic Review. Open Access Libr. J. 2020, 7, 8. [Google Scholar] [CrossRef]
- Ortiz-Barrios, M.; Arias-Fonseca, S.; Ishizaka, A.; Barbati, M.; Avendaño-Collante, B.; Navarro-Jiménez, E. Artificial intelligence and discrete-event simulation for capacity management of intensive care units during the COVID-19 pandemic: A case study. J. Bus. Res. 2023, 160, 113806. [Google Scholar] [CrossRef]
- Chee, M.L.; Ong, M.E.H.; Siddiqui, F.J.; Zhang, Z.; Lim, S.L.; Ho, A.F.W.; Liu, N. Artificial intelligence applications for COVID-19 in intensive care and emergency settings: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 4749. [Google Scholar] [CrossRef]
- Xu, Z.; Su, C.; Xiao, Y.; Wang, F. Artificial intelligence for COVID-19: Battling the pandemic with computational intelligence. Intell. Med. 2022, 2, 13–29. [Google Scholar] [CrossRef] [PubMed]
- Zaman, T.U.; Alharbi, E.K.; Bawazeer, A.S.; Algethami, G.A.; Almehmadi, L.A.; Alshareef, T.M.; Alotaibi, Y.A.; Karar, H.M.O. Artificial intelligence: The major role it played in the management of healthcare during COVID-19 pandemic. IAES Int. J. Artif. Intell. 2023, 12, 505–513. [Google Scholar] [CrossRef]
- Ismail, L.; Materwala, H. Blockchain paradigm for healthcare: Performance evaluation. Symmetry 2020, 12, 1200. [Google Scholar] [CrossRef]
- Aravazhi, A.; Helgheim, B.I.; Aadahl, P. Decision-Making Based on Predictive Process Monitoring of Patient Treatment Processes: A Case Study of Emergency Patients. Adv. Oper. Res. 2023, 2023, 8867057. [Google Scholar] [CrossRef]
- Văduva, L.L.; Nedelcu, A.-M.; Stancu, D.; Bălan, C.; Purcărea, I.-M.; Gurău, M.; Cristian, D.A. Digital Technologies for Public Health Services after the COVID-19 Pandemic: A Risk Management Analysis. Sustainability 2023, 15, 3146. [Google Scholar] [CrossRef]
- Ho, C.W.-L.; Caals, K.; Zhang, H. Heralding the Digitalization of Life in Post-Pandemic East Asian Societies. J. Bioethical Inq. 2020, 17, 657–661. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.J.; Lin, L.-C.; Yang, S.-T.; Hwang, K.-S.; Liao, C.-T.; Ho, W.-H. High-Reliability Non-Contact Photoplethysmography Imaging for Newborn Care by a Generative Artificial Intelligence. IEEE Access 2023, 11, 90801–90810. [Google Scholar] [CrossRef]
- Suhaimy, A.M.B.; Anwar, T. Intelligent healthcare on hydrocephalus management using artificial neural network algorithm. Int. J. Eng. Adv. Technol. 2019, 9, 6108–6115. [Google Scholar] [CrossRef]
- Ortíz-Barrios, M.A.; Coba-Blanco, D.M.; Alfaro-Saíz, J.-J.; Stand-González, D. Process improvement approaches for increasing the response of emergency departments against the COVID-19 pandemic: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 8814. [Google Scholar] [CrossRef]
- Zemmar, A.; Lozano, A.M.; Nelson, B.J. The rise of robots in surgical environments during COVID-19. Nat. Mach. Intell. 2020, 2, 566–572. [Google Scholar] [CrossRef]
- Nti, I.K.; Adekoya, A.F.; Weyori, B.A.; Keyeremeh, F. A bibliometric analysis of technology in sustainable healthcare: Emerging trends and future directions. Decis. Anal. J. 2023, 8, 100292. [Google Scholar] [CrossRef]
- Free, R.C.; Lozano Rojas, D.; Richardson, M.; Skeemer, J.; Small, L.; Haldar, P.; Woltmann, G. A data-driven framework for clinical decision support applied to pneumonia management. Front. Digit. Health 2023, 5, 1237146. [Google Scholar] [CrossRef] [PubMed]
- Khalique, F.; Khan, S.A.; Nosheen, I. A Framework for Public Health Monitoring, Analytics and Research. IEEE Access 2019, 7, 101309–101326. [Google Scholar] [CrossRef]
- Atek, S.; Bianchini, F.; De Vito, C.; Cardinale, V.; Novelli, S.; Pesaresi, C.; Eugeni, M.; Mecella, M.; Rescio, A.; Petronzio, L.; et al. A predictive decision support system for coronavirus disease 2019 response management and medical logistic planning. Digital Health 2023, 9, 20552076231185475. [Google Scholar] [CrossRef]
- Sulis, E.; Terna, P.; Di Leva, A.; Boella, G.; Boccuzzi, A. Agent-oriented Decision Support System for Business Processes Management with Genetic Algorithm Optimization: An Application in Healthcare. J. Med. Syst. 2020, 44, 157. [Google Scholar] [CrossRef]
- Cho, M.; Song, M.; Yoo, S.; Reijers, H.A. An Evidence-Based Decision Support Framework for Clinician Medical Scheduling. IEEE Access 2019, 7, 15239–15249. [Google Scholar] [CrossRef]
- Tam, W.; Alajlani, M.; Abd-Alrazaq, A. An Exploration of Wearable Device Features Used in UK Hospital Parkinson Disease Care: Scoping Review. J. Med. Internet Res. 2023, 25, 42950. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Shih, P.-C.; Zhu, Y.; Gao, W. An integrated model for medical expense system optimization during diagnosis process based on artificial intelligence algorithm. J. Comb. Optim. 2022, 44, 2515–2532. [Google Scholar] [CrossRef] [PubMed]
- Alruwaili, F.F. Artificial intelligence and multi agent based distributed ledger system for better privacy and security of electronic healthcare records. PeerJ Comput. Sci. 2020, 6, e323. [Google Scholar] [CrossRef]
- Iadanza, E.; Benincasa, G.; Ventisette, I.; Gherardelli, M. Automatic Classification of Hospital Settings through Artificial Intelligence. Electronics 2022, 11, 1697. [Google Scholar] [CrossRef]
- Fatoum, H.; Hanna, S.; Halamka, J.D.; Sicker, D.C.; Spangenberg, P.; Hashmi, S.K. Blockchain integration with digital technology and the future of health care ecosystems: Systematic review. J. Med. Internet Res. 2021, 23, 19846. [Google Scholar] [CrossRef]
- Chen, I.Y.; Szolovits, P.; Ghassemi, M. Can AI help reduce disparities in general medical and mental health care? AMA J. Ethics 2019, 21, 167–179. [Google Scholar] [CrossRef]
- Anudjo, M.N.K.; Vitale, C.; Elshami, W.; Hancock, A.; Adeleke, S.; Franklin, J.M.; Akudjedu, T.N. Considerations for environmental sustainability in clinical radiology and radiotherapy practice: A systematic literature review and recommendations for a greener practice. Radiography 2023, 29, 1077–1092. [Google Scholar] [CrossRef]
- Raja, B.S.; Asghar, S. Disease classification in health care systems with game theory approach. IEEE Access 2020, 8, 83298–83311. [Google Scholar] [CrossRef]
- Shang, Y.; Tian, Y.; Zhou, M.; Zhou, T.; Lyu, K.; Wang, Z.; Xin, R.; Liang, T.; Zhu, S.; Li, J. EHR-Oriented Knowledge Graph System: Toward Efficient Utilization of Non-Used Information Buried in Routine Clinical Practice. IEEE J. Biomed. Health Inform. 2021, 25, 2463–2475. [Google Scholar] [CrossRef]
- García-Ponsoda, S.; García-Carrasco, J.; Teruel, M.A.; Maté, A.; Trujillo, J. Feature engineering of EEG applied to mental disorders: A systematic mapping study. Appl. Intell. 2023, 53, 23203–23243. [Google Scholar] [CrossRef]
- Celesti, A.; De Falco, I.; Pecchia, L.; Sannino, G. Guest Editorial Enabling Technologies for Next Generation Telehealthcare. IEEE J. Biomed. Health Inform. 2021, 25, 4240–4242. [Google Scholar] [CrossRef]
- Zhai, K.; Masoodi, N.A.; Zhang, L.; Yousef, M.S.; Qoronfleh, M.W. Healthcare Fusion: An Innovative Framework for Health Information Management. Electron. J. Knowl. Manag. 2022, 20, 179–192. [Google Scholar] [CrossRef]
- Nisar, D.-E.-M.; Amin, R.; Shah, N.-U.-H.; Ghamdi, M.A.A.; Almotiri, S.H.; Alruily, M. Healthcare Techniques through Deep Learning: Issues, Challenges and Opportunities. IEEE Access 2021, 9, 98523–98541. [Google Scholar] [CrossRef]
- Yu, G.; Tabatabaei, M.; Mezei, J.; Zhong, Q.; Chen, S.; Li, Z.; Li, J.; Shu, L.; Shu, Q. Improving chronic disease management for children with knowledge graphs and artificial intelligence. Expert Syst. Appl. 2022, 201, 117026. [Google Scholar] [CrossRef]
- Vargas, V.B.; De Oliveira Gomes, J.; Fernandes, P.C.; Vallejos, R.V.; De Carvalho, J.V. Influential Factors for Hospital Management Maturity Models in a post-COVID-19 scenario—Systematic Literature Review. J. Inf. Syst. Eng. Manag. 2023, 8, 12868. [Google Scholar] [CrossRef]
- Murala, D.K.; Panda, S.K.; Dash, S.P. MedMetaverse: Medical Care of Chronic Disease Patients and Managing Data Using Artificial Intelligence, Blockchain, and Wearable Devices State-of-the-Art Methodology. IEEE Access 2023, 11, 138954–138985. [Google Scholar] [CrossRef]
- Soellner, M.; Koenigstorfer, J. Motive perception pathways to the release of personal information to healthcare organizations. BMC Med. Inform. Decis. Mak. 2022, 22, 240. [Google Scholar] [CrossRef]
- Alanazi, F.; Gay, V.; Alturki, R. Poor Compliance of Diabetic,Pa.tients with AI-Enabled E-Health Self-Care Management in Saudi Arabia. Information 2022, 13, 509. [Google Scholar] [CrossRef]
- Ramchand, S.; Tsang, G.; Cole, D.; Xie, X. RetainEXT: Enhancing Rare Event Detection and Improving Interpretability of Health Records using Temporal Neural Networks. In Proceedings of the 2022 IEEE-EMBS International Conference on Biomedical and Health Informatics (BHI), Ioannina, Greece, 27–30 September 2022. [Google Scholar] [CrossRef]
- Yang, N. Financial Big Data Management and Control and Artificial Intelligence Analysis Method Based on Data Mining Technology. Wirel. Commun. Mob. Comput. 2022, 2022, 7596094. [Google Scholar] [CrossRef]
- Chen, Y.; Huang, W.; Jiang, X.; Zhang, T.; Wang, Y.; Yan, B.; Wang, Z.; Chen, Q.; Xing, Y.; Li, D.; et al. UbiMeta: A Ubiquitous Operating System Model for Metaverse. Int. J. Crowd Sci. 2023, 7, 180–189. [Google Scholar] [CrossRef]
- Huang, J.-D.; Wang, J.; Ramsey, E.; Leavey, G.; Chico, T.J.A.; Condell, J. Applying Artificial Intelligence to Wearable Sensor Data to Diagnose and Predict Cardiovascular Disease: A Review. Sensors 2022, 22, 8002. [Google Scholar] [CrossRef] [PubMed]
- Shumba, A.-T.; Montanaro, T.; Sergi, I.; Bramanti, A.; Ciccarelli, M.; Rispoli, A.; Carrizzo, A.; De Vittorio, M.; Patrono, L. Wearable Technologies and AI at the Far Edge for Chronic Heart Failure Prevention and Management: A Systematic Review and Prospects. Sensors 2023, 23, 6896. [Google Scholar] [CrossRef]
- Hughes, A.; Shandhi, M.M.H.; Master, H.; Dunn, J.; Brittain, E. Wearable Devices in Cardiovascular Medicine. Circ. Res. 2023, 132, 652–670. [Google Scholar] [CrossRef]
- Yu, S.; Chen, Z.; Wu, X. The Impact of Wearable Devices on Physical Activity for Chronic Disease Patients: Findings from the 2019 Health Information National Trends Survey. Int. J. Environ. Res. Public Health 2023, 20, 887. [Google Scholar] [CrossRef]
- Bhaskar, S.; Bradley, S.; Sakhamuri, S.; Moguilner, S.; Chattu, V.K.; Pandya, S.; Schroeder, S.; Ray, D.; Banach, M. Designing Futuristic Telemedicine Using Artificial Intelligence and Robotics in the COVID-19 Era. Front. Public Health 2020, 8, 556789. [Google Scholar] [CrossRef]
- Burrell, D.N. Dynamic Evaluation Approaches to Telehealth Technologies and Artificial Intelligence (AI) Telemedicine Applications in Healthcare and Biotechnology Organizations. Merits 2023, 3, 700–721. [Google Scholar] [CrossRef]
- Christopoulou, S.C. Machine Learning Models and Technologies for Evidence-Based Telehealth and Smart Care: A Review. BioMedInformatics 2024, 4, 754–779. [Google Scholar] [CrossRef]
- Senthilkumaran, R.K.; Prashanth, M.; Viswanath, H.; Kotha, S.; Tiwari, K.; Bera, A. ARTEMIS: AI-driven robotic triage labeling and emergency medical information system. arXiv 2023, arXiv:2309.08865. [Google Scholar]
- Tyler, S.; Olis, M.; Aust, N.; Patel, L.; Simon, L.; Triantafyllidis, C.; Patel, V.; Lee, D.W.; Ginsberg, B.; Ahmad, H. Use of Artificial Intelligence in Triage in Hospital Emergency Departments: A Scoping Recview. Cureus 2024, 16, e59906. [Google Scholar] [CrossRef]
- Antonini, A.; Reichmann, H.; Gentile, G.; Garon, M.; Tedesco, C.; Frank, A.; Falkenburger, B.; Konitsiotis, S.; Tsamis, K.; Rigas, G.; et al. Toward objective monitoring of Parkinson’s disease motor symptoms using a wearable device: Wearability and performance evaluation of PDMonitor®. Front. Neurol. 2023, 14, 1080752. [Google Scholar] [CrossRef] [PubMed]
- Badidi, E. Edge AI for Early Detection of Chronic Diseases and the Spread of Infectious Diseases: Opportunities, Challenges, and Future Directions. Future Internet 2023, 15, 370. [Google Scholar] [CrossRef]
- Lu, L.; Zhang, J.; Xie, Y.; Gao, F.; Xu, S.; Wu, X.; Ye, Z. Wearable Health Devices in Health Care: Narrative Systematic Review. JMIR Mhealth Uhealth 2020, 8, e18907. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Yang, B.; Wong, T.W.-L.; Ng, S.S.M.; Hu, X. Personalized robots for long-term telerehabilitation after stroke: A perspective on technological readiness and clinical translation. Front. Rehabil. Sci. 2024, 4, 1329927. [Google Scholar] [CrossRef]
- Monge, J.; Ribeiro, G.; Raimundo, A.; Postolache, O.; Santos, J. AI-Based Smart Sensing and AR for Gait Rehabilitation Assessment. Information 2023, 14, 355. [Google Scholar] [CrossRef]
- Neo, J.R.E.; Ser, J.S.; Tay, S.S. Use of large language model-based chatbots in managing the rehabilitation concerns and education needs of outpatient stroke survivors and caregivers. Front. Digit. Health 2024, 6, 1395501. [Google Scholar] [CrossRef]
- López-Martínez, F.; Núñez-Valdez, E.R.; García-Díaz, V.; Bursac, Z. A case study for a big data and machine learning platform to improve medical decision support in population health management. Algorithms 2020, 13, 102. [Google Scholar] [CrossRef]
- Phan, A.-C.; Phan, T.-C.; Trieu, T.-N. A Systematic Approach to Healthcare Knowledge Management Systems in the Era of Big Data and Artificial Intelligence. Appl. Sci. 2022, 12, 4455. [Google Scholar] [CrossRef]
- Liu, K.; Chen, Z.; Wu, J.; Tan, Y.; Wang, L.; Yan, Y.; Zhang, H.; Long, J. Big Medical Data Decision-Making Intelligent System Exploiting Fuzzy Inference Logic for Prostate Cancer in Developing Countries. IEEE Access 2019, 7, 2348–2363. [Google Scholar] [CrossRef]
- Rana, S.K.; Rana, S.K.; Nisar, K.; Ag Ibrahim, A.A.; Rana, A.K.; Goyal, N.; Chawla, P. Blockchain Technology and Artificial Intelligence Based Decentralized Access Control Model to Enable Secure Interoperability for Healthcare. Sustainability 2022, 14, 9471. [Google Scholar] [CrossRef]
- Kedra, J.; Radstake, T.; Pandit, A.; Baraliakos, X.; Berenbaum, F.; Finckh, A.; Fautrel, B.; Stamm, T.A.; Gomez-Cabrero, D.; Pristipino, C.; et al. Current status of use of big data and artificial intelligence in RMDs: A systematic literature review informing EULAR recommendations. RMD Open 2019, 5, e001004. [Google Scholar] [CrossRef] [PubMed]
- Hermawan, D.; Kansa Putri, N.M.D.; Kartanto, L. Cyber Physical System Based Smart Healthcare System with Federated Deep Learning Architectures with Data Analytics. Int. J. Commun. Netw. Inf. Secur. 2022, 14, 222–233. [Google Scholar] [CrossRef]
- Camajori Tedeschini, B.; Savazzi, S.; Stoklasa, R.; Barbieri, L.; Stathopoulos, I.; Nicoli, M.; Serio, L. Decentralized Federated Learning for Healthcare Networks: A Case Study on Tumor Segmentation. IEEE Access 2022, 10, 8693–8708. [Google Scholar] [CrossRef]
- Ahmad, S.; Khan, S.; AlAjmi, M.F.; Dutta, A.K.; Dang, L.M.; Joshi, G.P.; Moon, H. Deep Learning Enabled Disease Diagnosis for Secure Internet of Medical Things. Comput. Mater. Contin. 2022, 73, 965–979. [Google Scholar] [CrossRef]
- Kim, J.; Kim, M. Deepblockshield: Blockchain agent-based secured clinical data management model from the deep web environment. Mathematics 2021, 9, 1069. [Google Scholar] [CrossRef]
- Almalawi, A.; Khan, A.I.; Alsolami, F.; Abushark, Y.B.; Alfakeeh, A.S. Managing Security of Healthcare Data for a Modern Healthcare System. Sensors 2023, 23, 3612. [Google Scholar] [CrossRef]
- Zhai, Y.; Li, R.; Yan, Z. Research on Application of Meticulous Nursing Scheduling Management Based on Data-Driven Intelligent Optimization Technology. Comput. Intell. Neurosci. 2022, 2022, 3293806. [Google Scholar] [CrossRef]
- Mehta, N.; Pandit, A.; Shukla, S. Transforming healthcare with big data analytics and artificial intelligence: A systematic mapping study. J. Biomed. Inform. 2019, 100, 103311. [Google Scholar] [CrossRef]
- Cai, Q.; Wang, H.; Li, Z.; Liu, X. A Survey on Multimodal Data-Driven Smart Healthcare Systems: Approaches and Applications. IEEE Access 2019, 7, 133583–133599. [Google Scholar] [CrossRef]
- Almalawi, A.; Khan, A.I.; Alsolami, F.; Abushark, Y.B.; Alfakeeh, A.S.; Mekuriyaw, W.D. Analysis of the Exploration of Security and Privacy for Healthcare Management Using Artificial Intelligence: Saudi Hospitals. Comput. Intell. Neurosci. 2022, 2022, 4048197. [Google Scholar] [CrossRef]
- Loh, H.W.; Ooi, C.P.; Seoni, S.; Barua, P.D.; Molinari, F.; Acharya, U.R. Application of explainable artificial intelligence for healthcare: A systematic review of the last decade (2011–2022). Comput. Methods Programs Biomed. 2022, 226, 107161. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.-S. Applying frontier approach to measure the financial efficiency of hospitals. Digit. Health 2023, 9, 20552076231162987. [Google Scholar] [CrossRef]
- Nazir, T.; Mushhood Ur Rehman, M.; Asghar, M.R.; Kalia, J.S. Artificial intelligence assisted acute patient journey. Front. Artif. Intell. 2022, 5, 962165. [Google Scholar] [CrossRef]
- Yang, J.; Luo, B.; Zhao, C.; Zhang, H. Artificial intelligence healthcare service resources adoption by medical institutions based on TOE framework. Digit. Health 2022, 8, 20552076221126034. [Google Scholar] [CrossRef] [PubMed]
- Mengash, H.A.; Alharbi, L.A.; Alotaibi, S.S.; AlMuhaideb, S.; Nemri, N.; Alnfiai, M.M.; Marzouk, R.; Salama, A.S.; Duhayyim, M.A. Deep Learning Enabled Intelligent Healthcare Management System in Smart Cities Environment. Comput. Mater. Contin. 2023, 74, 4483–4500. [Google Scholar] [CrossRef]
- Maki, O.; Alshaikhli, M.; Gunduz, M.; Naji, K.K.; Abdulwahed, M. Development of Digitalization Road Map for Healthcare Facility Management. IEEE Access 2022, 10, 14450–14462. [Google Scholar] [CrossRef]
- Wan, H.C.; Chin, K.S. Exploring internet of healthcare things for establishing an integrated care link system in the healthcare industry. Int. J. Eng. Bus. Manag. 2021, 13, 18479790211019526. [Google Scholar] [CrossRef]
- Nguyen, D.C.; Pham, Q.-V.; Pathirana, P.N.; Ding, M.; Seneviratne, A.; Lin, Z.; Dobre, O.; Hwang, W.-J. Federated learning for smart healthcare: A survey. ACM Comput. Surv. (Csur) 2022, 55, 1–37. [Google Scholar] [CrossRef]
- Wazid, M.; Das, A.K.; Mohd, N.; Park, Y. Healthcare 5.0 Security Framework: Applications, Issues and Future Research Directions. IEEE Access 2022, 10, 129429–129442. [Google Scholar] [CrossRef]
- Cavanagh, J.; Pariona-Cabrera, P.; Halvorsen, B. In what ways are HR analytics and artificial intelligence transforming the healthcare sector? Asia Pac. J. Hum. Resour. 2023, 61, 785–793. [Google Scholar] [CrossRef]
- Huang, C.-H.; Batarseh, F.A. Measuring Outcomes in Healthcare Economics using Artificial Intelligence: With Application to Resource Allocation. In Proceedings of the International Florida Artificial Intelligence Research Society Conference (FLAIRS), Miami, FL, USA, 16–19 May 2021; Volume 34. [Google Scholar] [CrossRef]
- Katirai, A.; Yamamoto, B.A.; Kogetsu, A.; Kato, K. Perspectives on artificial intelligence in healthcare from a Patient and Public Involvement Panel in Japan: An exploratory study. Front. Digit. Health 2023, 5, 1229308. [Google Scholar] [CrossRef] [PubMed]
- Luschi, A.; Petraccone, C.; Fico, G.; Pecchia, L.; Iadanza, E. Semantic Ontologies for Complex Healthcare Structures: A Scoping Review. IEEE Access 2023, 11, 19228–19246. [Google Scholar] [CrossRef]
- Jordon, K.; Dossou, P.-E.; Junior, J.C. Using lean manufacturing and machine learning for improving medicines procurement and dispatching in a hospital. Procedia Manuf. 2019, 38, 1034–1041. [Google Scholar] [CrossRef]
- Toki, E.I.; Tsoulos, I.G.; Santamato, V.; Pange, J. Machine Learning for Predicting Neurodevelopmental Disorders in Children. Appl. Sci. 2024, 14, 837. [Google Scholar] [CrossRef]
- Santamato, V.; Esposito, D.; Tricase, C.; Faccilongo, N.; Marengo, A.; Pange, J. Assessment of Public Health Performance in Relation to Hospital Energy Demand, Socio-Economic Efficiency and Quality of Services: An Italian Case Study. In Computational Science and Its Applications—ICCSA 2023 Workshops; Gervasi, O., Murgante, B., Rocha, A.M.A.C., Garau, C., Scorza, F., Karaca, Y., Torre, C.M., Eds.; Springer Nature: Cham, Switzerland, 2023; pp. 505–522. [Google Scholar] [CrossRef]
- Santamato, V.; Tricase, C.; Faccilongo, N.; Iacoviello, M.; Pange, J.; Marengo, A. Machine Learning for Evaluating Hospital Mobility: An Italian Case Study. Appl. Sci. 2024, 14, 6016. [Google Scholar] [CrossRef]
- Santamato, V.; Tricase, C.; Faccilongo, N.; Marengo, A.; Pange, J. Healthcare performance analytics based on the novel PDA methodology for assessment of efficiency and perceived quality outcomes: A machine learning approach. Expert Syst. Appl. 2024, 252, 124020. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).