Abstract
The aim of this clinical study was to evaluate the impact of an additional use of a flowable composite on the clinical success of Class I and II composite restorations. Furthermore, different clinical criteria were recorded to determine if the combination with a flowable material shows significant advantages compared to the composite material alone. In 50 patients, one cavity was solely filled with a nano-hybrid composite (control group) and the second cavity in combination with an additional layer of flowable composite (test group) using a universal adhesive system in the self-etch modus. Clinical assessments were performed according to the modified criteria proposed by USPHS/Ryge. After 24 months, 47 patients were examined resulting in a recall rate of 94%. The cumulative survival rate for all restorations after 24 months was 96.8%. Three restorations (3.2%) failed due to the loss of vitality. All failed restorations were located in the test group (6.4%), and none in the control group (0%). This resulted in a cumulative success rate in the control group of 100% and 93.6% in the test group, showing a significantly different annual failure rate (AFR) of 0% and 3.2%, respectively (p < 0.05; Mann–Whitney U-test). Beside the differences regarding the tooth vitality, success rate, and AFR, no significant influence of the flowable composite on the different evaluated clinical parameters could be detected. Therefore, the application of an additional layer of the flowable composite might have neither a positive nor a negative effect on composite restorations in clinical practice.
1. Introduction
Today, resin-based direct composite restorations in the posterior teeth have become a well-established and common procedure in dental practice [1,2,3]. These restorations meet the demands of the patient and the practitioner for an aesthetic and minimally invasive therapeutic concept. Marginal adaptation followed by secondary caries is still a well-known problem with composite restorations, in particular on the approximal wall of Class II restorations [4]. Insufficient marginal sealing has been correlated with postoperative sensitivity, restoration failure, and secondary caries [5]. Furthermore, the main intention of using flowable composites as cavity liners is to avoid occlusal and particularly approximal leakage.
However, the effect of flowable composites applied as cavity liners on the long-term success of composite restorations remain inconclusive and no common consensus exists [4,6,7,8,9,10]. Despite the limited scientific evaluation, there is an increased use in the general practice of a flowable resin composite as a cavity lining and stress-relieving gingival increment in Class I and II restorations [11,12,13]. The flowable composite (Grandio®SO Heavy Flow) used in the present study is a flowable nano-hybrid composite with a higher viscosity (Table 1). Due to these properties, it could be used as a flowable composite lining in the posterior teeth instead of a conventional flowable composite when increased strength is required [14]. While some flowable composites in combination with conventional composite materials have already produced promising in vitro results and good clinical experience [1,15,16], clinical data for a flowable composite exhibiting a higher viscosity are scarce. Considering the positive in vitro studies of a high-viscosity composite [17,18], it was the aim of the present study to test the clinical performance of such a material as a cavity liner.

Table 1.
Material properties of the composites used in this study.
Therefore, the objective of the study was to determine whether the additional use of a flowable composite in combination with a nano-hybrid composite is suitable for the restoration of Class I and II occlusion-bearing cavities and that the combination of both increased the performance of the restorations.
The following main hypothesis was stated:
- The main objective of this study was to investigate the impact of an additional use of a flowable composite layer (Grandio®SO Heavy Flow) in combination with a nano-hybrid composite (Grandio®SO) on the clinical success of Class I and II restorations.
The objectives of the study were as follows:
- The differences in different criteria (secondary caries, tooth vitality, postoperative sensitivity, filling integrity/fracture, proximal contact, surface roughness, marginal adaption, marginal discoloration, and color match) should be identified.
- Is the dentin-bonding system Futurabond® DC (VOCO GmbH, Cuxhaven, Germany) used in the self-etch modus capable of ensuring a long-lasting seal of the fillings in the enamel and dentin over time? Can Futurabond® DC effectively prevent postoperative pain?
- How does the nano-hybrid composite Grandio®SO, which has been on the market since 2010, perform in terms of abrasion, shade stability, and surface roughness in occlusal-loaded Class I and II cavities?
2. Materials and Methods
2.1. Study Design
Fifty patients who had at least two premolars or molars requiring Class I or II restorations were included in the present study. The study design was approved by the Ethic Committee of the Martin Luther University Halle-Wittenberg, Germany (protocol number: 225/17.11.10/8). All patients received verbal and written information on the study and signed consent forms to participate. The inclusion criteria for this study were as follows: Patients had to be at least 18 years old, with a restorative need of at least two Class I or II restorations in molars or premolars and also have a positive vitality. Furthermore, these included teeth should be in antagonistic contact and, for Class II restorations, in contact with adjacent teeth. The bucco-oral extent of the cavities should be at least 1/3 of the cusp distance. Teeth with deep carious lesions receiving indirect pulp capping were, following the study protocol, also included. Indirect pulp capping was performed using a calcium hydroxide preparation (Calcicur®, VOCO GmbH, Cuxhaven, Germany). The subjects agreed to receive restorations as part of the study and signed the informed consent form. The following criteria led to the exclusion of participation: severe systemic diseases, proven allergies to the ingredients, bruxism, pregnancy or lactation period, and poor oral hygiene (e.g., plaque index > 1 and gingival index > 0), or not completed hygiene phase. Included teeth must demonstrate sound pulpal conditions; this means teeth with signs of pulpal inflammation, endodontic treatment, or direct pulp capping are excluded. Patients who were not expected to be able to attend the recall appointments were also excluded.
2.2. Clinical Procedure
Treatment planning included a medical history, dental examination, and initial radiographic diagnosis to evaluate restorative needs, caries lesions, and apical pathologies. As the clinical investigation was planned in a split-mouth design, two almost comparably sized defects were selected per patient, which were randomly assigned to the respective treatment group (control and test group). Photographs of the teeth before and after restoration were taken. The fillings of the control group were placed with the nano-hybrid composite. In the test group, an additional dentin-covering layer of Grandio®SO Heavy Flow was applied. Isolation of the tooth to be restored was ensured by the use of rubber dam. Cavity preparations were performed using 80 μm diamonds and the cavity margins were finished using 25 μm diamonds. If necessary, after removal of the insufficient filling or caries, a punctual indirect capping of the areas close to the pulp was performed using Ca(OH)2 preparation. After cavity preparations, Futurabond® DC, used in self-etch modus, was scrubbed into the tooth with a microbrush for at least 20 s, starting on enamel. The applied material was blown by a stream of air removing excess and forming a thin, homogeneous, and glossy film on the surface, which was polymerized for 10 s with a high-power LED light unit (Celalux® 2, VOCO GmbH, Cuxhaven, Germany). The fillings of the control group were layered in single increments of maximum 2 mm thickness of the nano-hybrid composite. In the test group, a thin dentin-covering layer of maximum 0.5 mm flowable composite was applied to all cavity walls and polymerized beforehand. Each increment was polymerized for 30 s using the above-mentioned polymerization device. The fillings were then finished with fine-grained diamonds (Komet, Brasseler, Lemgo, Germany) and polished to a high gloss with polishers (Diamanto®, VOCO GmbH, Cuxhaven, Germany) under maximum water cooling. Finally, fluoridation with Bifluorid 12® (VOCO GmbH, Cuxhaven, Germany) was applied on the restored teeth. All restorations were placed by one experienced dentist.
2.3. Report (Baseline, 6 Months, 12 Months, 24 Months)
All follow-up examinations were performed by one blinded experienced and instructed examiner. The baseline examination was performed approx. 2 weeks after the filling was placed, the first follow-up examination was repeated after 6 months, and the second follow-up examination after 12 months. If necessary, professional tooth cleaning or filling polishing was done. Photo documentation was performed using a digital reflex camera (Canon EOS 60D, EF-S 60 mm f/2.8 Macro USM, Canon, Tokyo, Japan) at baseline and all phases of follow-up. The clinical evaluation was based on the modified USPHS/Ryge criteria (Table 2) [19,20,21]. The lateral view of the test teeth in occlusion as well as the single occlusal view were documented photographically. In addition, the following findings were recorded: pulp status per cold vitality test (Endo-Frost®, Roeko, Langenau, Germany), postoperative sensitivity, marginal discoloration, marginal adaptation, secondary caries, contact situation, surface texture, shade adaptation, proximal contacts, fracture of the restoration, loss of filling as well as gingival index (GI), and proximal plaque index (PI) proposed by Silness and Löe, 1964 (Table 3) [22,23].

Table 2.
Summary of the modified USPHS/Ryge criteria used for the clinical evaluation.

Table 3.
Plaque index and gingival index (Silness and Löe).
2.4. Statistical Analysis
The sample size was calculated upon the assumption that the primary endpoint (annual failure rate) will be 1.5 in the test group and 2.1 in the control group with a standard deviation of 1 in both groups. This clinically relevant difference can be detected with 80% power by a t-test to the 5%-level if 44 patients (44 restorations per arm using split-mouth design) will be included. To allow some moderate dropout, 50 patients (50 restorations per arm) were included.
Statistical analysis was performed by SPSS® 25.0 (IBM®, Ehningen, Germany). To determine statistically significant differences between investigated groups, the Mann–Whitney U-test was used at a 5% level of significance.
3. Results
3.1. Study Population
In the study, 29 female and 21 male patients (Figure 1) were initially included and restored with 100 Class I and II restorations (Figure 1).
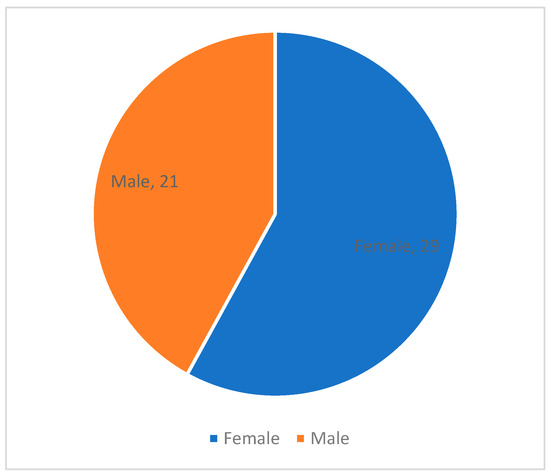
Figure 1.
Gender distribution of the included patients.
In total, 32 Class I and 68 Class II fillings were placed at baseline, with a ratio of 20:30 in the control group and 12:38 in the test group (Figure 2).
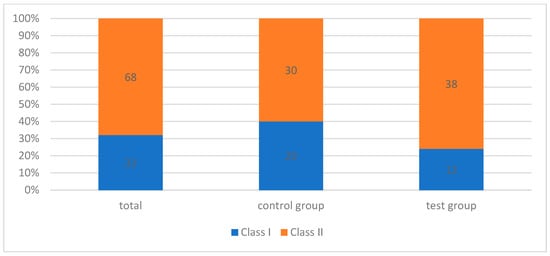
Figure 2.
Black’s classification of dental lesions included in the study.
Of the total 42 premolars, 22 teeth and, of the total 58 molars, 28 cavities were assigned to the control group (Figure 3).
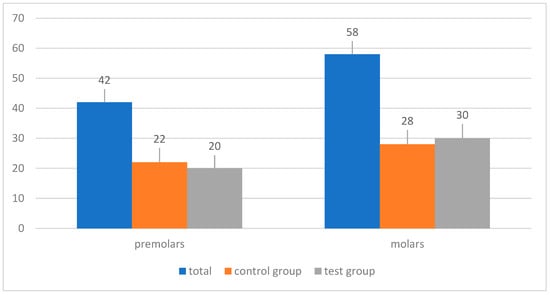
Figure 3.
Distribution of the study teeth at baseline.
3.2. Success after 24 Months
After 24 months, 47 patients out of 50 could be followed up. This is equivalent to a recall rate of 94%. At this point, 28 female and 19 male patients with 94 Class I and Class II restorations could be re-examined. Altogether, 30 Class I and 64 Class II fillings with a contribution of 19:28 in the control group and 11:36 in the test group were evaluated. The cumulative survival rate for all restorations after 24 months was 96.8%. Three restorations (3.2%) failed. Three of the failed restorations were located in the test group (6.4%), and none in the control group (0%), resulting in a cumulative success rate in the control group of 100% and 93.6% in the test group. Finally, these findings resulted in significantly different annual failure rates (AFR) of 0% and 3.2%, respectively (p < 0.05; Mann–Whitney U-test).
3.3. Secondary Caries
After 24 months, none of the 94 restorations in both groups (the control and test group) exhibited any signs of secondary caries (Table 4).

Table 4.
Summary of evaluated parameters (A = Alpha, B = Bravo, C = Charlie, and D = Delta).
3.4. Tooth Vitality
Following the initial restoration, three out of 94 teeth required endodontic treatment (Code Delta). Therefore, they were recorded as failures. The suffering teeth were located in the test group. The other 91 included teeth showing a positive vitality of the pulp (Table 4).
3.5. Postoperative Sensitivity
With the exception of the three endodontically treated teeth, all the teeth examined showed regular sensitivity after two years. Immediately after filling therapy, nine patients reported increased sensitivity to temperature and biting (Code Bravo). However, the complaints were of short duration, so no additional treatment was indicated. At the time of the baseline examination, the patients reported a clear improvement. Six months after the filling therapy, no increased sensitivity of the restored study teeth was detectable (Code Alpha). The clinical re-examination after 24 months showed no signs of increased sensitivity. Therefore, it was rated as Code Alpha in all cases (Table 4).
3.6. Filling Integrity/Fracture
Two fillings of the test group showed a discreet chipping of the superficial composite material of the distal margin at the first re-examination after 12 months (Code Bravo). After the smoothing and polishing of the defect, the fillings could remain in situ without the loss of proximal contact or other functions. This situation showed satisfactory stability after 24 months and was scored again as Code Bravo (Table 4).
3.7. Marginal Discoloration
Regarding marginal discoloration, after 6 months, the included restorations showed three discolored filling margins in two patients (Code Bravo). One restoration was found in the control and two in the test group. Between 12 and 24 months, this number increased to four patients and finally five restorations revealed the marginal discoloration of the filling margins (Code Bravo). The ratio, based on the distribution of the investigated groups, is now 2:3 (Figure 4). The difference was not statistically different (p > 0.05, Mann–Whitney U-test, Table 4).
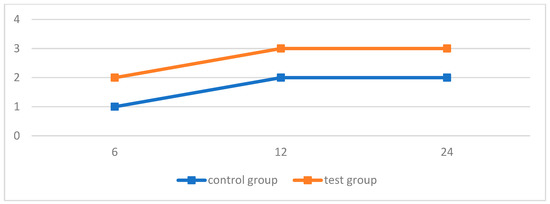
Figure 4.
Marginal discoloration within both groups.
3.8. Other Parameters
The examinations of proximal contact, surface roughness, marginal adaption, and color match showed no abnormalities in the control group after 24 months. Regarding the parameter marginal adaption, one restoration was rated as Code Bravo in the test group. (Table 4). The statistical comparison of both groups regarding these parameters showed no significant differences (p > 0.05, Mann–Whitney U-test) (Figure 5, Figure 6 and Figure 7).
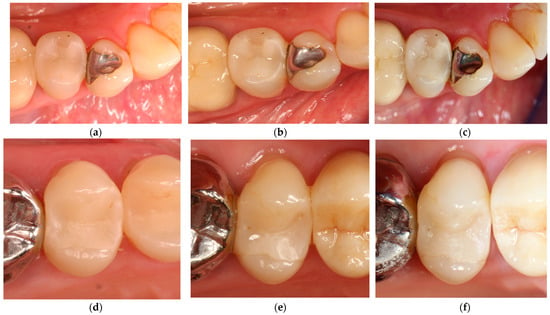
Figure 5.
Clinical situation of Pat. No. 16: filling 45 mod without flowable composite: control group, all criteria were rated Code Alpha: (a) baseline; (b) after 12 months; and (c) after 24 months. Clinical situation of filling 15 mod with flowable composite as intermediate liner: test group, all criteria Code Alpha except margin discoloration was evaluated as Code Beta: (d) baseline; (e) after 12 months; and (f) after 24 months.
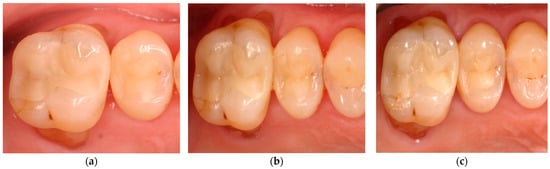
Figure 6.
Clinical situation of Pat. No. 18: filling 15 od without flowable composite: control group, all criteria Code Alpha; filling 16 mod with flowable composite as intermediate liner: test group: margin adaption was evaluated as Code Beta all other criteria were rated Code Alpha: (a) baseline; (b) after 12 months; and (c) after 24 months.
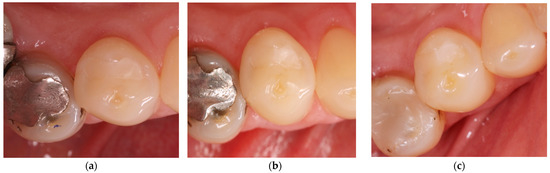
Figure 7.
Clinical situation of Pat. No. 6: filling 44 od with flowable composite: test group, all criteria Code Alpha. (a) baseline; (b) after 12 months; and (c) after 24 months.
3.9. Plaque and Ginigval Index
Regarding the plaque index at baseline, six subjects and, after 6 months, seven patients had an index of 1; i.e., a thin plaque film was visible when scraped with a dental probe. This trend of seven study participants continues after 12 months. After 24 months, there is a reduction to five patients showing a plaque index of 1 (Figure 8). In contrast to the plaque index, only two patients showed a gingival index of 1, i.e., low inflammation with slight discoloration of the gingiva without bleeding (Figure 9). After 24 months, no significant difference with regard to PI and GI could be detected between the control and test group (p > 0.05, Mann–Whitney U-test, Table 3).
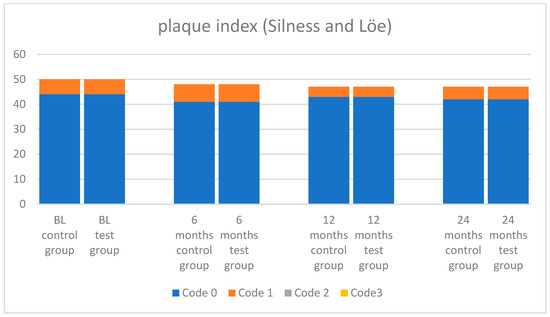
Figure 8.
Plaque index (Silness and Löe) [22,23].
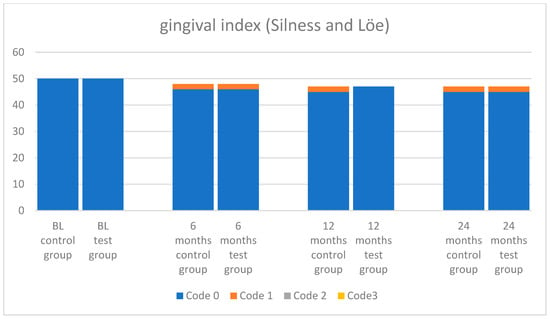
Figure 9.
Gingival index (Silness and Löe) [22,23].
4. Discussion
This clinical study evaluated the clinical performance and effectiveness of a flowable composite as an intermediate stress-breaking cavity liner in posterior cavities combined with a conventional nano-hybrid composite material. This study was conducted in vivo and in a split-mouth design; consequently, the individual differences with regard to risk factors such as oral hygiene, saliva composition, and dietary habits can be almost eliminated [24,25,26,27,28]. Furthermore, the study was performed in a randomized-controlled, single-blinded manner, thus increasing internal validity [29,30].
This study showed a recall rate of 94% after 24 months. In comparison with other studies evaluating the 24-month results, this is an acceptable recall rate as demonstrated in similar clinical trials (recall rate: 89.9% [18], recall rate: 95% [31]). The overall cumulative survival rate after 2 years, combining all Alpha and Bravo codes, was 96.8% according to the modified USPHS/Ryge criteria, considering both groups with and without the additional use of a flowable composite together. Significant differences in the cumulative success rate between the control group (100%) and the test group (93.6%) could be detected within the observation period. After 24 months, three restorations out of the test group showed Code Delta because of negative tooth vitality and root canal treatment. One of these teeth received an initial Class I restoration and developed an approximal lesion on the mesial aspect of the tooth within the following 24 months leading to irreversible pulpitis with endodontic treatment needs. The second endodontic-treated tooth of another patient underwent endodontic therapy abroad. The third endodontically treated tooth was diagnosed with irreversible pulpitis within the first 24 months. In this case, the possible impact of temperature changes during polymerization might be an explanation for the loss of vitality. It is known that these temperature changes can cause pulpitis [32]. However, in all three cases, endodontic therapy was necessary due to pulpal inflammation after deep caries excavation prior to restoration. In all three cases, indirect pulp capping using a calcium hydroxide liner (Calcicur®, VOCO GmbH, Cuxhaven, Germany) was performed. The applied restorations showed no secondary caries or marginal failures. Based on these facts, it can be assumed that these three teeth were correctly restored using both of the composite materials. The fact that all teeth were assigned to the test group must be rated as a random incident. Unfortunately, according to our study protocol and the used USPHS/Ryge criteria, the three teeth had to be rated as failures. Comparing the success rates with another randomized clinical trial of the same conventional and heavy flowable composites Grandio®SO, no Code Charlie or Delta was detected as well after 24 months (survival rate 100%) [18]. Another clinical trial on composite filling by Ernst et al. [31] showed that 92.8% of composite restorations placed with the additional use of a flowable composite as a liner survived compared to a 94.6% survival rate without the flowable composite. These results are in accordance with our findings. Other authors described further clinical layering approaches, which might help to perform quick, predictable, and natural-looking restorations, reducing the need for occlusal adjustments [33]. This is different from our dentin lining using a flowable composite to increase adaption to the dentin and avoid polymerization stress. Among the 94 teeth, 12 indirect capping procedures with a calcium hydroxide preparation were performed [34,35]. Seven teeth from the control group and five teeth from the test group were indirectly capped. It is remarkable that nine of twelve teeth showed a positive and regular sensitivity after 24 months of observation. Three teeth of the test group had to receive endodontic treatment (see above). Only one tooth in the test group showed an increased sensitivity to temperature and occlusion immediately after capping. However, the complaints were of short duration, so no therapeutic intervention was indicated. At the time of the baseline examination (2 weeks after restoration), the patient reported an improvement and, at the first follow-up examinations, that tooth showed regular sensitivity without complaints.
Postoperative sensitivity is, in principle, a possible complication after composite restorations and therefore often a secondary outcome measure in clinical trials while examining composite materials [16,36]. Many authors focused on the impact of the used dentin adhesive system regarding the presence or absence of postoperative sensitivity [37,38,39,40,41].
Nevertheless, despite the significant improvements of adhesive systems, the bonded interface remains the weakest area of the composite restorations. The failure or degradation of this interface can result in poor marginal adaption, marginal discoloration, and the subsequent loss of retention or secondary caries of the restoration, as typical clinical findings. The interface between the tooth and restorative material is subjected to varying stresses during its lifetime. The volumetric shrinkage of the resin material during polymerization is dependent on the properties of the material used, the volume of resin material cured, filler type and amount, degree of polymerization, C-factor, monomer content, and application technique [42]. Laboratory and clinical studies have demonstrated excellent success rates for total-etch adhesives over the years [43,44,45,46,47]. Unfortunately, many clinical investigations have shown that postoperative hypersensitivity after a complete cavity etching is still a problem. To reduce technique sensitivity and the risk of postoperative sensitivity by dentin etching, self-etch adhesives that operate by acid etching with simultaneous monomer infiltration were developed. It is expected that self-etch adhesives prevent or reduce postoperative sensitivity due to their less aggressive and more superficial interaction with dentin [48,49]. In the present investigation after 24 months, no postoperative hypersensitivity was detected (0%). Comparable results are difficult to evaluate in other studies, because the number of trials directly comparing the self-etch and etch and rinse system is small [36]. All fillings in this study were placed under absolute dryness using a rubber dam; the adhesive system was applied according to the manufacturer’s instructions as a self-etch system. The recommended layer thickness and light-curing time of the placed composite materials was obeyed. The fact that one experienced dentist placed all the restorations might provide a further explanation. In addition, all the fillings were prepared under water cooling with the same grain size of the diamond burs. The present undesirable reactions of the pulp–dentin unit are therefore not due to gross processing errors of the materials investigated.
Secondary caries was not detected after 24 months in any case. This is a comparable result to the research of Torres et al. [18]. Trials exist that showed secondary caries after two years with the additional use of a flowable composite as a liner [31,50]. However, the number of secondary caries is very low [31]. Furthermore, two fillings of the test group showed a discreet chipping of the superficial composite material of the distal margin after 12 months (Code Bravo). These fillings could remain in situ without the loss of proximal contact or other functions and showed satisfactory stability after 24 months. These findings are in accordance with the results of other studies [1,18]. Regarding marginal discoloration, higher abnormalities were detected in comparable studies after 24 months [18,31]. Recently published studies showed that polymerization time improved the mechanical properties of composite materials [51]. In the present study, each increment was light-cured for 30 s. This might explain the favorable outcome regarding the quality of the placed restorations (surface roughness, marginal adaption, marginal discoloration, and color match) in the present investigation. While the study of Torres et al. with the same composite material Grandio®SO evaluated Code Bravo at 39.5% in the test group and 32.5% in the control group, Ernst et al. detected Code Bravo at 23.6% in the test and 32.1% in the control group. For the use of flowable composites as an intermediate stress-breaking layer, a number of in vitro studies [7,12,13,52] describe a reduction in marginal microleakage and internal cavities as well as an improved adaptation of the composite to the tooth structure, while other studies did not find any positive effects on marginal adaptation [7,53,54]. The effect of flowable composite materials as an intermediate stress-absorbing layer in Class I and II cavities compared to the use without using this layer has been investigated in few clinical studies so far [55,56]. Furthermore, the present study supports the findings that there is no significant influence of the flowable composite on the clinical quality of the fillings. Since, in our study, the adhesive system Futurabond® DC was used as a self-etch system on dentin as well as on enamel, this must be taken into account when evaluating the marginal seal. Some studies show the advantages of selective enamel etching for the bond between the tooth structure and the composite [57,58]. Regarding the used adhesive system in the self-etch modus, the authors have shown that the bond strength values are comparable between the etch and rinse and self-etch modus when testing Futurabond® DC in both application modes [59]. Furthermore, this system is known to be effective in establishing a sufficient bond to tooth structures [60]. This might be an explanation for the present finding, that restorations in both groups showed no abnormalities after 24 months in the deterioration of the marginal adaptation. On average, the formation of a marginal leakage and subsequently secondary caries is more than 2 years [1,61,62,63,64], so longer assessment periods are required.
Considering that biofilm is an important parameter in the etiology of caries formation around composite restorations [24], patients with an initial plaque accumulation were encouraged to improve their oral hygiene, and a thorough professional dental cleaning including oral hygiene instructions was performed. As a result, after a follow-up at 2 years, plaque accumulation was reduced from seven to five patients. In the case of study results obtained by in vivo examinations, individual differences must be taken into account. In the present study, a split-mouth design was used to avoid the impact of individual concerns. However, the different oral hygiene of the individual subjects is a parameter that can be influenced but not directly controlled. Finally, this depends on the compliance of the patient. To minimize this complication, good oral hygiene was taken into account when selecting the study participants. These findings are in accordance with the absence of secondary caries in all re-examined teeth. The improvement of oral hygiene might be the relevant factor. Unfortunately, one tooth developed an approximal lesion followed by endodontic treatment in the test group.
In summary, in vitro and clinical data do not significantly support any particular method or material type in achieving an optimal performance in restoring Class I and II restorations with current composites [65,66,67,68].
5. Conclusions
Apart from the three endodontic treatments, the materials for direct adhesive restorations in this study provided an acceptable clinical performance in the posterior teeth of Class I or II over a period of 24 months in both groups. After 2 years, the results of the additional use of a flowable composite ultimately led to significantly different annual failure rates (AFR) of 0% and 3.2%, respectively (p < 0.05; Mann–Whitney U test). Beside the differences regarding the tooth vitality, success rate, and AFR, no significant influence of the flowable composite on the different evaluated clinical parameters could be observed at this time. Therefore, the application of an additional layer of the flowable composite might have neither a positive nor a negative effect on composite restorations in clinical practice. However, further long-term studies are required for a final evaluation of pluggable composites and the advantage of an additional use of flowable composites as a liner.
Author Contributions
Conceptualization, C.R.G.; methodology, C.R.G.; validation, C.R.G. and M.M.; formal analysis, C.R.G., A.D.N., M.M. and N.P.; investigation, C.R.G. and M.M.; resources, C.R.G.; data curation, A.D.N., M.M., N.P. and C.R.G.; writing—original draft preparation, C.R.G., A.D.N. and N.P.; writing—review and editing, C.R.G., A.D.N. and N.P.; visualization, A.D.N., M.M. and N.P.; supervision, C.R.G.; project administration, C.R.G.; funding acquisition, C.R.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by VOCO GmbH, Cuxhaven, Germany. No. 31308004KZEP.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the Medical Faculty of the Martin Luther University Halle-Wittenberg, protocol number: 225/17.11.10/8.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data are available upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Boeckler, A.; Schaller, H.G.; Gernhardt, C.R. A prospective, double-blind, randomized clinical trial of a one-step, self-etch adhesive with and without an intermediary layer of a flowable composite: A 2-year evaluation. Quintessence Int. 2012, 43, 279–286. [Google Scholar] [PubMed]
- Dietschi, D.; Olsburgh, S.; Krejci, I.; Davidson, C. In vitro evaluation of marginal and internal adaptation after occlusal stressing of indirect class II composite restorations with different resinous bases. Eur. J. Oral Sci. 2003, 111, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Veloso, S.R.M.; Lemos, C.A.A.; de Moraes, S.L.D.; do Egito Vasconcelos, B.C.; Pellizzer, E.P.; de Melo Monteiro, G.Q. Clinical performance of bulk-fill and conventional resin composite restorations in posterior teeth: A systematic review and meta-analysis. Clin. Oral Investig. 2019, 23, 221–233. [Google Scholar] [CrossRef]
- Aggarwal, V.; Singla, M.; Yadav, S.; Yadav, H. Effect of flowable composite liner and glass ionomer liner on class II gingival marginal adaptation of direct composite restorations with different bonding strategies. J. Dent. 2014, 42, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Sarrett, D.C. Clinical challenges and the relevance of materials testing for posterior composite restorations. Dent. Mater. 2005, 21, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Boruziniat, A.; Gharaee, S.; Sarraf Shirazi, A.; Majidinia, S.; Vatanpour, M. Evaluation of the efficacy of flowable composite as lining material on microleakage of composite resin restorations: A systematic review and meta-analysis. Quintessence Int. 2016, 47, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Chuang, S.F.; Liu, J.K.; Chao, C.C.; Liao, F.P.; Chen, Y.H. Effects of flowable composite lining and operator experience on microleakage and internal voids in class II composite restorations. J. Prosthet. Dent. 2001, 85, 177–183. [Google Scholar] [CrossRef]
- Leevailoj, C.; Cochran, M.A.; Matis, B.A.; Moore, B.K.; Platt, J.A. Microleakage of posterior packable resin composites with and without flowable liners. Oper. Dent. 2001, 26, 302–307. [Google Scholar]
- Szesz, A.; Parreiras, S.; Martini, E.; Reis, A.; Loguercio, A. Effect of flowable composites on the clinical performance of non-carious cervical lesions: A systematic review and meta-analysis. J. Dent. 2017, 65, 11–21. [Google Scholar] [CrossRef]
- Sadeghi, M.; Lynch, C.D. The effect of flowable materials on the microleakage of Class II composite restorations that extend apical to the cemento-enamel junction. Oper. Dent. 2009, 34, 306–311. [Google Scholar] [CrossRef]
- Labella, R.; Lambrechts, P.; Van Meerbeek, B.; Vanherle, G. Polymerization shrinkage and elasticity of flowable composites and filled adhesives. Dent. Mater. 1999, 15, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Al Sunbul, H.; Silikas, N.; Watts, D.C. Polymerization shrinkage kinetics and shrinkage-stress in dental resin-composites. Dent. Mater. 2016, 32, 998–1006. [Google Scholar] [CrossRef]
- Korkmaz, Y.; Ozel, E.; Attar, N. Effect of flowable composite lining on microleakage and internal voids in Class II composite restorations. J. Adhes. Dent. 2007, 9, 189–194. [Google Scholar] [PubMed]
- Jager, S.; Balthazard, R.; Dahoun, A.; Mortier, E. Filler Content, Surface Microhardness, and Rheological Properties of Various Flowable Resin Composites. Oper. Dent. 2016, 41, 655–665. [Google Scholar] [CrossRef]
- Geurtsen, W.; Schoeler, U. A 4-year retrospective clinical study of Class I and Class II composite restorations. J. Dent. 1997, 25, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Swift, E.J., Jr.; Ritter, A.V.; Heymann, H.O.; Sturdevant, J.R.; Wilder, A.D., Jr. 36-month clinical evaluation of two adhesives and microhybrid resin composites in Class I restorations. Am. J. Dent. 2008, 21, 148–152. [Google Scholar] [PubMed]
- Sagsoz, O.; Ilday, N.O.; Karatas, O.; Cayabatmaz, M.; Parlak, H.; Olmez, M.H.; Demirbuga, S. The bond strength of highly filled flowable composites placed in two different configuration factors. J. Conserv. Dent. 2016, 19, 21. [Google Scholar] [CrossRef]
- Torres, C.R.G.; Rêgo, H.M.C.; Perote, L.C.C.C.; Santos, L.F.T.F.; Kamozaki, M.B.B.; Gutierrez, N.C.; Di Nicoló, R.; Borges, A.B. A split-mouth randomized clinical trial of conventional and heavy flowable composites in class II restorations. J. Dent. 2014, 42, 793–799. [Google Scholar] [CrossRef]
- Ryge, G. Clinical criteria. Int. Dent. J. 1980, 30, 347–358. [Google Scholar]
- Ryge, G.; Snyder, M. Evaluating the clinical quality of restorations. J. Am. Dent. Assoc. 1973, 87, 369–377. [Google Scholar] [CrossRef]
- Estay, J.; Martín, J.; Vildosola, P.; Mjor, I.A.; Oliveira, O.B., Jr.; Andrade, M.F.; Moncada, G.; Gordan, V.V.; Fernández, E. Effect of Refurbishing Amalgam and Resin Composite Restorations After 12 Years: Controlled Clinical Trial. Oper. Dent. 2017, 42, 587–595. [Google Scholar] [CrossRef]
- Loe, H.; Silness, J. Periodontal Disease in Pregnancy I. Prevalence and Severity. Acta Odontol. Scand. 1963, 21, 533–551. [Google Scholar] [CrossRef]
- Silness, J.; Loe, H. Periodontal Disease in Pregnancy II. Correlation Between Oral Hygiene and Periodontal Condition. Acta Odontol. Scand. 1964, 22, 121–135. [Google Scholar] [CrossRef] [PubMed]
- Lima, F.G.; Romano, A.R.; Correa, M.B.; Demarco, F.F. Influence of microleakage, surface roughness and biofilm control on secondary caries formation around composite resin restorations: An in situ evaluation. J. Appl. Oral Sci. 2009, 17, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Lesaffre, E.; Philstrom, B.; Needleman, I.; Worthington, H. The design and analysis of split-mouth studies: What statisticians and clinicians should know. Stat. Med. 2009, 28, 3470–3482. [Google Scholar] [CrossRef]
- Hatirli, H.; Yasa, B.; Çelik, E.U. Clinical performance of high-viscosity glass ionomer and resin composite on minimally invasive occlusal restorations performed without rubber-dam isolation: A two-year randomised split-mouth study. Clin. Oral Investig. 2021, 25, 5493–5503. [Google Scholar] [CrossRef] [PubMed]
- Pandis, N.; Walsh, T.; Polychronopoulou, A.; Katsaros, C.; Eliades, T. Split-mouth designs in orthodontics: An overview with applications to orthodontic clinical trials. Eur. J. Orthod. 2013, 35, 783–789. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, C.M. Randomized controlled trials. Plast. Reconstr. Surg. 2011, 127, 1707–1712. [Google Scholar] [CrossRef]
- Bhide, A.; Shah, P.S.; Acharya, G. A simplified guide to randomized controlled trials. Acta Obstet. Gynecol. Scand. 2018, 97, 380–387. [Google Scholar] [CrossRef]
- Pihlstrom, B.L.; Curran, A.E.; Voelker, H.T.; Kingman, A. Randomized controlled trials: What are they and who needs them? Periodontol 2000. 2012, 59, 14–31. [Google Scholar] [CrossRef]
- Ernst, C.-P.; Canbek, K.; Aksogan, K.; Willershausen, B. Two-year clinical performance of a packable posterior composite with and without a flowable composite liner. Clin. Oral Investig. 2003, 7, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Szalewski, L.; Szalewska, M.; Jarosz, P.; Woś, M.; Szymańska, J. Temperature Changes in Composite Materials during Photopolymerization. Appl. Sci. 2021, 11, 474. [Google Scholar] [CrossRef]
- Scolavino, S.; Paolone, G.; Orsini, G.; Devoto, W.; Putignano, A. The Simultaneous Modeling Technique: Closing gaps in posteriors. Int. J. Esthet. Dent. 2016, 11, 58–81. [Google Scholar] [PubMed]
- Nair, M.; Gurunathan, D. Clinical and Radiographic Outcomes of Calcium Hydroxide vs Other Agents in Indirect Pulp Capping of Primary Teeth: A Systematic Review. Int. J. Clin. Pediatr. Dent. 2019, 12, 437–444. [Google Scholar] [CrossRef]
- Gyanendra, K.; Dhillon, J.K. Comparative evaluation of clinical outcome of indirect pulp treatment with calcium hydroxide, calcium silicate and Er, Cr: YSGG laser in permanent molars. Laser Ther. 2019, 28, 123–130. [Google Scholar] [CrossRef]
- Berkowitz, G.; Spielman, H.; Matthews, A.; Vena, D.; Craig, R.; Curro, F.; Thompson, V. Postoperative hypersensitivity and its relationship to preparation variables in Class I resin-based composite restorations: Findings from the practitioners engaged in applied research and learning (PEARL) Network. Part 1. Compend. Contin. Educ. Dent. 2013, 34, e44–e52. [Google Scholar] [CrossRef]
- Sancakli, H.S.; Yildiz, E.; Bayrak, I.; Ozel, S. Effect of different adhesive strategies on the post-operative sensitivity of class I composite restorations. Eur. J. Dent. 2014, 8, 15–22. [Google Scholar] [CrossRef]
- Scotti, N.; Bergantin, E.; Giovannini, R.; Delbosco, L.; Breschi, L.; Migliaretti, G.; Pasqualini, D.; Berutti, E. Influence of multi-step etch-and-rinse versus self-etch adhesive systems on the post-operative sensitivity in medium-depth carious lesions: An in vivo study. Am. J. Dent. 2015, 28, 214–218. [Google Scholar]
- Reis, A.; Dourado Loguercio, A.; Schroeder, M.; Luque-Martinez, I.; Masterson, D.; Cople Maia, L. Does the adhesive strategy influence the post-operative sensitivity in adult patients with posterior resin composite restorations?: A systematic review and meta-analysis. Dent. Mater. 2015, 31, 1052–1067. [Google Scholar] [CrossRef]
- Bekes, K.; Boeckler, L.; Gernhardt, C.R.; Schaller, H.G. Clinical performance of a self-etching and a total-etch adhesive system - 2-year results. J. Oral Rehabil. 2007, 34, 855–861. [Google Scholar] [CrossRef]
- Boeckler, A.; Boeckler, L.; Eppendorf, K.; Schaller, H.G.; Gernhardt, C.R. A prospective, randomized clinical trial of a two-step self-etching vs two-step etch-and-rinse adhesive and SEM margin analysis: Four-year results. J. Adhes. Dent. 2012, 14, 585–592. [Google Scholar] [CrossRef] [PubMed]
- Kahler, B.; Kotousov, A.; Borkowski, K. Effect of material properties on stresses at the restoration-dentin interface of composite restorations during polymerization. Dent. Mater. 2006, 22, 942–947. [Google Scholar] [CrossRef] [PubMed]
- Bottenberg, P.; Jacquet, W.; Alaerts, M.; Keulemans, F. A prospective randomized clinical trial of one bis-GMA-based and two ormocer-based composite restorative systems in class II cavities: Five-year results. J. Dent. 2009, 37, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Manhart, J.; Chen, H.Y.; Hickel, R. Clinical evaluation of the posterior composite Quixfil in class I and II cavities: 4-year follow-up of a randomized controlled trial. J. Adhes. Dent. 2010, 12, 237–243. [Google Scholar] [CrossRef]
- Armstrong, S.R.; Vargas, M.A.; Chung, I.; Pashley, D.H.; Campbell, J.A.; Laffoon, J.E.; Qian, F. Resin-dentin interfacial ultrastructure and microtensile dentin bond strength after five-year water storage. Oper. Dent. 2004, 29, 705–712. [Google Scholar]
- Efes, B.G.; Dorter, C.; Gomec, Y. Clinical evaluation of an ormocer, a nanofill composite and a hybrid composite at 2 years. Am. J. Dent. 2006, 19, 236–240. [Google Scholar]
- Frankenberger, R.; Tay, F.R. Self-etch vs etch-and-rinse adhesives: Effect of thermo-mechanical fatigue loading on marginal quality of bonded resin composite restorations. Dent. Mater. 2005, 21, 397–412. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; Yoshihara, K.; Yoshida, Y.; Mine, A.; De Munck, J.; Van Landuyt, K.L. State of the art of self-etch adhesives. Dent. Mater. 2011, 27, 17–28. [Google Scholar] [CrossRef]
- Giannini, M.; Makishi, P.; Ayres, A.P.; Vermelho, P.M.; Fronza, B.M.; Nikaido, T.; Tagami, J. Self-etch adhesive systems: A literature review. Braz. Dent. J. 2015, 26, 3–10. [Google Scholar] [CrossRef]
- Worthington, H.V.; Khangura, S.; Seal, K.; Mierzwinski-Urban, M.; Veitz-Keenan, A.; Sahrmann, P.; Schmidlin, P.R.; Davis, D.; Iheozor-Ejiofor, Z.; Rasines Alcaraz, M.G. Direct composite resin fillings versus amalgam fillings for permanent posterior teeth. Cochrane Database Syst. Rev. 2021, 8, CD005620. [Google Scholar] [CrossRef]
- Szalewski, L.; Wójcik, D.; Sofińska-Chmiel, W.; Kuśmierz, M.; Różyło-Kalinowska, I. How the Duration and Mode of Photopolymerization Affect the Mechanical Properties of a Dental Composite Resin. Materials. 2023, 16, 113. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Jepsen, S.; Albers, H.K.; Eberhard, J. Flowable materials as an intermediate layer could improve the marginal and internal adaptation of composite restorations in Class-V-cavities. Dent. Mater. 2006, 22, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Neme, A.M.; Maxson, B.B.; Pink, F.E.; Aksu, M.N. Microleakage of Class II packable resin composites lined with flowables: An in vitro study. Oper. Dent. 2002, 27, 600–605. [Google Scholar]
- Tredwin, C.J.; Stokes, A.; Moles, D.R. Influence of flowable liner and margin location on microleakage of conventional and packable class II resin composites. Oper. Dent. 2005, 30, 32–38. [Google Scholar]
- Shaalan, O.O.; Abou-Auf, E.; El Zoghby, A.F. Clinical evaluation of flowable resin composite versus conventional resin composite in carious and noncarious lesions: Systematic review and meta-analysis. J. Conserv. Dent. 2017, 20, 380–385. [Google Scholar] [CrossRef]
- Badr, C.; Spagnuolo, G.; Amenta, F.; Khairallah, C.; Mahdi, S.S.; Daher, E.; Battineni, G.; Baba, N.Z.; Zogheib, T.; Qasim, S.S.B.; et al. A Two-Year Comparative Evaluation of Clinical Performance of a Nanohybrid Composite Resin to a Flowable Composite Resin. J. Funct. Biomater. 2021, 12, 51. [Google Scholar] [CrossRef] [PubMed]
- Diniz, A.C.; Bandeca, M.C.; Pinheiro, L.M.; Dos Santosh Almeida, L.J., Jr.; Torres, C.R.; Borges, A.H.; Pinto, S.C.; Tonetto, M.R.; De Jesus Tavarez, R.R.; Firoozmand, L.M. Influence of Different Etching Modes on Bond Strength to Enamel using Universal Adhesive Systems. J. Contemp. Dent. Pract. 2016, 17, 820–825. [Google Scholar] [CrossRef]
- Rosa, W.L.; Piva, E.; Silva, A.F. Bond strength of universal adhesives: A systematic review and meta-analysis. J. Dent. 2015, 43, 765–776. [Google Scholar] [CrossRef]
- Abdalla, A.I.; El Zohairy, A.A.; Abdel Mohsen, M.M.; Feilzer, A.J. Bond efficacy and interface morphology of self-etching adhesives to ground enamel. J. Adhes. Dent. 2010, 12, 19–25. [Google Scholar] [CrossRef]
- Taneja, S.; Kumari, M.; Bansal, S. Effect of saliva and blood contamination on the shear bond strength of fifth-, seventh-, and eighth-generation bonding agents: An in vitro study. J. Conserv. Dent. 2017, 20, 157–160. [Google Scholar] [CrossRef]
- Ástvaldsdóttir, Á.; Dagerhamn, J.; van Dijken, J.W.V.; Naimi-Akbar, A.; Sandborgh-Englund, G.; Tranæus, S.; Nilsson, M. Longevity of posterior resin composite restorations in adults – A systematic review. J. Dent. 2015, 43, 934–954. [Google Scholar] [CrossRef] [PubMed]
- Ersin, N.K.; Candan, U.; Aykut, A.; önçag, ö.; Eronat, C.; Kose, T. A clinical evaluation of resin-based composite and glass ionomer cement restorations placed in primary teeth using the ART approach: Results at 24 months. J. Am. Dent. Assoc. 2006, 137, 1529–1536. [Google Scholar] [CrossRef] [PubMed]
- Moorthy, A.; Hogg, C.H.; Dowling, A.H.; Grufferty, B.F.; Benetti, A.R.; Fleming, G.J.P. Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. J. Dent. 2012, 40, 500–505. [Google Scholar] [CrossRef] [PubMed]
- van Dijken, J.W.; Pallesen, U. Clinical performance of a hybrid resin composite with and without an intermediate layer of flowable resin composite: A 7-year evaluation. Dent. Mater. 2011, 27, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Gerula-Szymańska, A.; Kaczor, K.; Lewusz-Butkiewicz, K.; Nowicka, A. Marginal integrity of flowable and packable bulk fill materials used for class II restorations -A systematic review and meta-analysis of in vitro studies. Dent. Mater. J. 2020, 39, 335–344. [Google Scholar] [CrossRef]
- Cavalheiro, C.P.; Scherer, H.; Imparato, J.C.P.; Collares, F.M.; Lenzi, T.L. Use of flowable resin composite as an intermediate layer in class II restorations: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 5629–5639. [Google Scholar] [CrossRef]
- Ferracane, J.L.; Lawson, N.C. Probing the hierarchy of evidence to identify the best strategy for placing class II dental composite restorations using current materials. J. Esthet. Restor. Dent. 2021, 33, 39–50. [Google Scholar] [CrossRef]
- Leyton, B.S.; Rached, R.N.; Ignácio, S.A.; Souza, E.M. Fracture strength of extended class I composite restorations with different restorative techniques. Odontology. 2022, 110, 269–277. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).