Featured Application
Monitoring motion increases exercise performance and lower leg circulation after TKR.
Abstract
(1) Background: deep venous thrombosis (DVT) has long been recognized as the most devastating complication after total knee replacement (TKR). To prevent DVT, intermittent pneumatic compression to improve venous return in the lower leg has been advocated by surgeons. Physical activities such as active ankle pumping and early mobilization have been recommended as auxiliary measures to increase venous return in the lower leg and help in ambulation after TKR. In this study, in order to remind patients to exercise their ankle actively and efficiently after TKR, a foot band with motion sensor and reminder alarm was used. (2) Methods: The patients were randomly allocated into three groups according to the therapeutic protocols. The patients in group 1 conducted active ankle pumping without any reminders, those in group 2 underwent intermittent pneumatic compression, and those in group 3 conducted active ankle pumping with ankle motion sensor/reminder. The parameters of blood flow, namely, peak flow velocity and flow volume, in the bilateral common femoral vein and popliteal vein on the 1st, 3rd, and 14th days after surgery were measured using the echo technique, an index to evaluate the effect on promotion of venous return, among the three groups. (3) Results: The peak flow velocity and flow volume of the operative limb in group 3 (with motion sensor/reminder) were significantly higher than those in other groups. The peak flow velocity and flow volume in the popliteal vein in group 3 increased by 112% and 93.8%, respectively, compared to group 1 on the 14th day. No significant difference in peak flow velocity or flow volume was found in the nonoperative limb between the groups. (4) Conclusions: According to the results, a motion sensor/reminder with vibration alarms can improve the performance of active ankle pumping exercises in improving lower leg circulation, and hence may reduce the risk of DVT.
1. Introduction
It has been estimated that 1 million patients underwent total knee replacement (TKR) surgery in 2020, and this is projected to increase to 1.9 million in 2030 just in the US [1]. In Asia, the reported incidence of DVT after TKR is about 34–48.6% [2,3]. Deep venous thrombosis (DVT) is a serious complication that usually occurs within 2 weeks after TKR [4,5,6,7], although the incidence is rare [5,8,9]. Possible damage to the vessel wall during the surgery, venous stasis caused by bed rest, and hypercoagulability of the blood after surgery are the three main reasons for the formation of DVT. In most cases, the thrombi resolve spontaneously; however, some of them (approximately 1–2.3%) may develop into symptomatic and even fatal DVT [9]. Anticoagulants such as aspirin are traditionally used for patients after TKR to prevent DVT [8,10], but carry a risk of GI bleeding [11,12]. In addition to aspirin, physical therapies, including active ankle pumping exercise and intermittent pneumatic compression, have shown reduction in the risk and incidence of DVT [13,14,15,16,17,18]. The mechanism of active ankle pumping exercise for DVT prevention is the extrusion of the veins in the lower leg with the contraction of the calf muscles [19]. The extrusion force from muscle contraction helps the venous blood to go against gravity and back to the heart. The mechanism of intermittent pneumatic compression for DVT prevention is similar to that of active ankle pumping exercises [20]. Ankle pumping exercises and pneumatic compression differ in the power source. Muscle contraction is the power source of ankle pumping exercises, whereas the external motor power is the power source of pneumatic compression. Both ankle pumping exercise and intermittent pneumatic compression can reduce the risk of DVT [13,14,16,17].
For DVT prevention with ankle pumping exercises after TKR, patients are asked to exercise automatically, particularly after returning home from the hospital. However, exercise execution and effects of active ankle pumping exercises on DVT prevention is uncertain. In addition, since ankle pumping exercises and intermittent pneumatic compression can both prevent DVT, which one is more effective method is still not reported. To remind the patients to exercise, a device with a motion sensor and vibration alarm, manufactured by ZMI Electronics (Kaohsiung, Taiwan), was developed to promote patient compliance with exercise regularly for their ankles after TKR. The alarm turns off if an adequate number of ankle movement with more than 40 degrees has been performed.
This study compared 1. the effect of active ankle pumping exercise performed with and without an alarm reminder, and 2. the effect of intermittent pneumatic compression and active ankle pumping exercise without alarm reminder on the prevention of DVT in the hospital. It is hypothesized that reminders can improve the performance of active ankle pumping exercises to improve lower leg circulation.
2. Materials and Methods
2.1. Ethics Statement
The study protocol was reviewed and approved by the Institutional Review Board of Show Chwan Memorial Hospital (1080704 on 17 October 2019 and 1090604 on 6 August 2020). All subjects provided written informed consent prior to the TKR surgery and therapeutic procedures during hospitalization. All treatment procedures, including surgery and physical therapy, were in accordance with the Declaration of Helsinki.
2.2. Study Subjects
This study was a cluster randomized controlled trial that compared lower leg circulation using different approaches. Ninety patients undergoing traditional TKR surgery between 1 January to 31 December 2020 at Chang Hua Show Chwan Memorial Hospital were enrolled in this study. The eligibility criterion was unilateral primary TKR for knee osteoarthritis. Patients with a history of cardiovascular disease, such as DVT, dyslipidemia, hypertension, myocardial infarction, and hemorrhagic disease, were excluded from this study. Patients were allocated to three groups, namely, groups 1, 2, and 3, in a 1:1:1 ratio, based on the participation date. Patients who participated in the same period were assigned to only one group [21]. However, one patient was moved from group 2 to group 1 because of bleeding with intermittent pneumatic compression at the beginning of postoperative nursing care. Finally, there were 31, 29, and 30 patients in groups 1, 2, and 3, respectively.
2.3. Surgical Technique and Postoperative Nursing Care
Cruciate retaining (CR)-type prostheses (UOC, New Taipei, Taiwan) with extramedullary guide in kinematic alignment were used for the TKR. In all patients, an air tourniquet was applied after elevation of the leg without elastic bandage exsanguination [22]. The patella was replaced with an inset-type component [23]. Periarticular injection of analgesics, including Marcaine 20 mL, morphine 5 mg, ketorolac 30 mg, epinephrine 0.1 mg and transamin 500 mg were given routinely [24]. The tourniquet was released after cementing of all components and bleeders were checked with electrocautery. A 1/8 inch Hemovac drain was then inserted before wound closure.
The routine postoperative nursing for the patients in each group included an X-ray examination of the knee after the surgery [25]. Medications included 100 mg aspirin q.d., 200 mg Celebrex g.d., Ultracet half a tablet q.i.d., and famotidine b.i.d. were given orally from the first postoperative day [10]. The patients were encouraged to get up from bed as soon as possible (mostly within 8 h after surgery) without routine urinary catherization. The Hemovac drain was removed on the third postoperative day or when the daily drainage amount was less than 200 mL.
2.4. Intervention Method
Group 1 patients learned active ankle pumping exercise for the operative limb and practiced regularly under the supervision of the nursing staff in the hospital. They were instructed to do the same at home after being discharged (Figure 1). The ankle pumping exercise consisted of rotating the ankle in a circle for 2 min, 20° dorsiflexion for 3 min, and 40° plantar flexion for 3 min in sequence. The ankle movements were performed at a frequency of once per second and at a cycle of 8 min, 1 cycle every 30 min, and 24 cycles per day [13]. Patients can execute the exercise in the supine, long sitting, sitting, and standing positions. An assistive device, such as a walker or cane, should be used if needed. In group 2, intermittent pneumatic compression was applied to the operative low limb during their stay in the hospital. The intermittent pneumatic compression used was an Active Compression System (Flowtron ACS900, ArjoHuntleigh Polska Sp. z o.o., Komorniki, Poland). The frequency of the intermittent pneumatic compression was set to once/min, and the duration was 16 h per day. The maximum pressure was set to 45 mmHg. They were also taught and instructed to do an active ankle pumping exercise, as those for group 1, after discharge. In group 3, in addition to active ankle pumping exercises for the operative limb, a foot band containing a reminder device and a strap (Figure 2) was used to remind the patients to perform the exercise. The reminder device, which was firmly attached to the strap, was worn around the wrist or midfoot while resting. Using a vibration alarm, the device reminded patients to exercise every 30 min. At the set time points, the vibration alarm started, and the patients had to put the device on their foot with the band. The sensor inside the device autodetected the movement of the ankle joint. The alarm stopped if an adequate number of ankle movements of more than 40 degrees were performed. The alarm started again at the next time point. Patients and their caregivers were taught about its usage during the hospital stay and instructed to continue using it at home after discharge. The band on the midfoot and above the slipper’s upper vamp does not hinder in-door walking. The foot band was used throughout the day except during sleeping hours. The foot band was removed on the follow-up visit of the patient after fourteen days. The only difference between groups 1 and 3 was the use of a reminding vibration alarm for exercise during the hospital stay and after discharge for group 3. The intervention was performed in the operative limb, while the nonoperative limb did not undergo intervention.
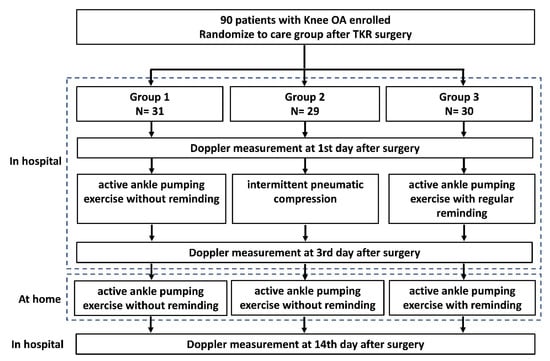
Figure 1.
Flowchart of the present study. OA: osteoarthritis.
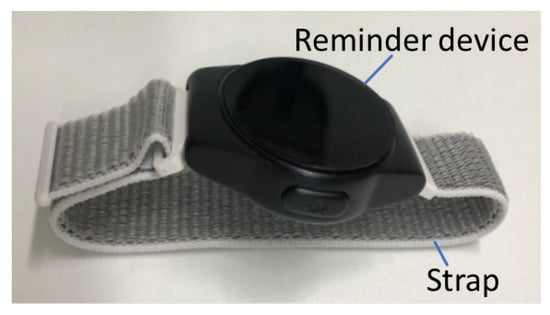
Figure 2.
The foot band used in this study.
2.5. Index for Sonographic Assessment of Lower Limb Veins
Assessment of the effects was done through detection of blood clots in the calf and thigh veins using ultrasonographic imaging, and a Doppler parameter of venous flow speed, volume, and stasis that indicated the tendency toward blood clot formation. The color Doppler ultrasound was done by an experienced technician in musculoskeletal systems and reexamined by a physician well trained in vascular diseases. The assessor was blinded to the grouping of the participants. Four different indices, namely, peak flow velocity, flow volume, stasis, and DVT of the bilateral common femoral vein (CFV) and popliteal vein (PV), were determined on the 1st, 3rd, and 14th days after the TKR surgery to assess the risk of DVT. The initial condition of the veins immediately after surgery was recorded on the first day. The patients were often discharged 3–5 days after surgery; hence, the second examination was completed on the third day after surgery. The third examination was conducted at the first time the patient returned to the hospital again for checkup, which was about the 14th day after the surgery.
The peak flow velocity and flow volume were directly detected using the Doppler images [26]. Venous stasis was defined by a peak flow velocity lower than 10 cm/s and the color of the blood inside the vein represented in the echo image was gray [27]. In addition, the contour of the vein was compressible under a slight compression force with an echo transducer. If the peak blood flow, flow volume, and blood echo image were the same as that of stasis, but the contour of the vein was incompressible under a slight compression, the cases were recorded as DVT [27]. The color of the normal blood flow in the echo image should be black, while the color changed to gray, indicating that blood was pooling in the vein and that further thrombosis was likely to occur. Other clinical signs, including pain and swelling in the foot, ankle, or leg and the skin over the affected area turning pale or a reddish or bluish color in the case of DVT were also recorded.
2.6. Follow-Up
All cases were followed up for 3 months after surgery to detect the incidence of DVT. Contact with the patient was conducted via telephone every 2 weeks. If the patient reported any clinical symptoms of DVT, they were asked to return to the hospital, and a Doppler examination was performed again to confirm the incidence of DVT. Medical interventions were adopted in patients with confirmed DVT.
2.7. Sample Size Calculation
Gpower version 3.197 was used for sample-size estimation. The required sample size was estimated based on median effect size d = 0.3, α = 0.05, and power = 0.8, and three groups were expected using analysis of variance (ANOVA). A total of 84 samples were required, considering a possible loss of 10% of the samples; therefore, the total number of samples was estimated to be 90.
2.8. Data Analysis
The collected data were analyzed using IBM SPSS Statistics for Windows version 24.0. (IBM Corp., Armonk, NY, USA). Frequency, percentage, mean, and standard deviation were used for descriptive statistics. Fisher’s exact test and ANOVA were used to compare the differences between groups, and p < 0.05 was considered significant.
2.9. Limitations
The design of this study has some limitations. The major limitation is the unknown exact number of active ankle pumping exercises performed during this period. Hence, the degree of exercise performance is unknown. Furthermore, the quality of exercises among the three groups was unclear, and the relationship between exercise quality and blood flow could not be determined. A greater degree of ROM achieved during the exercise would involve more muscle and lead to a greater pumping effect on the return of the blood in the vein, which would reduce the risk of DVT after TKR surgery. Finally, age differences were not considered because of the small sample.
3. Results
3.1. Baseline Characteristics
There were no significant differences in sex, age, surgical site, or bleeding among the three groups (Table 1). The volume of Hemovac drainage in group 3 was significantly less (p = 0.013) than that in groups 1 and 2. The drainage volume was 552.7 mL in group 3, whereas it was 753 mL in group 2.

Table 1.
The baseline characteristics of the three groups in this study.
3.2. Peak Flow Velocity and Flow Volume
The results indicated that the peak flow velocities of the CFV and PV in the operative limb in group 3 were significantly higher (p < 0.001) than those of group 1 on the 1st, 3rd, and 14th days after surgery (Table 2). Furthermore, the peak flow velocity of the CFV on the 1st, 3rd, and 14th days and that of the PV on the 14th day in the operative limb in group 3 was significantly higher (p < 0.001) than that in group 2. Compared with group 1, the peak flow velocity of the PV in group 3 increased by 100% (from 13.4 to 26.8 cm/s), 124% (from 13.4 to 30 cm/s), and 112% (from 13.7 to 29 cm/s) on the 1st, 3rd, and 14th days, respectively. Additionally, the peak flow velocity of the PV in group 3 increased by 49.5% (from 19.4 to 29 cm/s) on the 14th day compared to group 2. In the nonoperative limb, there was no significant difference in the peak flow velocity of the CFV and PV between the three groups.

Table 2.
Peak flow velocity in the common femoral vein (CFV) and popliteal vein (PV) after the surgery.
The flow volume of the CFV and PV on the operative limb in group 3 was significantly higher (p ≤ 0.001) than that in group 1 on the 1st, 3rd, and 14th days after surgery (Table 3). Furthermore, on the 14th day, the flow volume of the CFV and PV on the operative limb in group 3 was significantly higher (p ≤ 0.001) than that in group 2. Compared with group 1, the flow volume of the PV in group 3 increased by 69% (from 92.1 to 155.6 mL/min), 91.3% (from 87.6 to 167.6 mL/min), and 93.8% (from 98 to 189.9 mL/min) on the 1st, 3rd, and 14th days, respectively. In the nonoperative limb, there was no significant difference in the flow volume of the CFV or PV between the three groups.

Table 3.
Flow volume in the common femoral vein (CFV) and popliteal vein (PV) after the surgery.
A subgroup analysis was performed to stratify comparisons by sex (Table 4), and the differences between groups remained highly significant (p ≤ 0.001) in women; however, the results in men showed less significant differences, indicating different effectiveness between men and women.

Table 4.
Peak flow velocity and flow volume in the common femoral vein (CFV) and popliteal vein (PV) after the surgery stratified by gender.
3.3. Stasis
Venous stasis was significantly more common (p ≤ 0.009) in group 1 than in groups 2 and 3 in both limbs (Table 5). The number of cases of venous stasis in the operative limb in group 1 was four, two, and five on the 1st, 3rd and 14th day, respectively, after surgery. No venous stasis was found in the operative limb in group 3 after the surgery. Additionally, in the nonoperative limb, the number of cases of venous stasis in group 1 was four, five, and nine on the 1st, 3rd, and 14th, respectively, day after surgery, while only one case was found with stasis in the nonoperative limb in groups 2 and 3.

Table 5.
Case numbers with stasis after the surgery.
3.4. Occurrence of DVT during Follow-Up
None of the patients had any clinical sign of DVT during the hospitalization or follow-up period.
4. Discussion
In the present study, the risk of DVT was assessed for three groups of patients. In one of the groups, a regular reminder to the patient through vibration alarms of a foot band with motion sensor was used to increase the performance of the ankle pumping exercises, and the results confirmed a positive effect on peak venous blood flow and blood flow volume with Doppler after the surgery. Despite the absence of DVT incidence in this study, the Doppler examination provides additional evidence to support the contribution of the proposed approach in reducing the risk for DVT.
Ankle pumping exercise is a proposed strategy to prevent the formation of DVT, but it is challenging to know the performance of the exercise, particularly when the patient is discharged to home. In the present study, the occurrence rate of stasis was 17.2% in the patient without exercise alarm for 11 days at home (group 1), while none of the patients with the same exercise and regular with exercise alarm had signs of stasis. A simple reminder with the alarm could reduce the incidence of stasis after TKR. Furthermore, regular reminders to the patients for exercise also significantly increased the peak blood velocity and flow volume in the vessels. These results demonstrate the effect of regular reminders to increase the effect of active ankle pumping exercises after TRK without supervision at home.
Postoperative swelling and edema are common after TKR. Negative pressure drainage is typically used to remove stagnant tissue fluid. In addition to drainage, exercise has been suggested to reduce postsurgery edema [28]. In the present study, group 3 executed the exercise with reminders; hence, the execution rate of the exercise was certain. Because exercise helps reduce edema, the drainage volume is also reduced. In group 1, the execution of exercise was uncertain, and the drainage volume was greater than that in group 3. Although pneumatic compression has been reported to be beneficial in the acceleration of venous blood reflex, the effect of pneumatic compression on reducing edema remains uncertain. Hence, the drainage volume was more than that in group 3.
Intermittent pneumatic compression, except for active ankle pumping exercises, is also a standard approach to prevent the formation of DVT [16,17]. In the present study, despite the use of intermittent pneumatic compression for the first 3 days in the hospital after the surgery, the occurrence rate of stasis was lower than that of the active ankle pumping exercise without reminders, both in the hospital and at home. The same exercise was suggested for groups 1 and 2 at home after discharge, and the incidence of stasis was found to be 3.2% in group 2 and 17.2% in group 1 after the same exercises for 13 days. The reason for this is unknown, because the difference in exercise performance between the two groups is unknown. This is worth investigating in future studies.
In the ultrasound examination data, the peak flow velocity and flow volume with intermittent pneumatic compression were higher than those with active ankle exercises on the 1st and 3rd days. On the 14th day, just the results in the popliteal vein were higher in group 2 than in group 1. The blood in the popliteal vein is more accurate than that in the common femoral vein for evaluating the formation of DVT. Since the popliteal vein is more distal than the common femoral vein, the popliteal vein can represent the blood-return condition in the distal limb. In contrast, the common femoral vein is more proximal than the popliteal vein and receives backflow blood from the thigh muscles; hence, the differences in peak flow velocity and flow volume were not significant.
The results of stasis were both very good with intermittent pneumatic compression and exercise with reminders. No stasis occurred during hospitalization, and only one patient had signs of stasis on the 14th day in each group. Furthermore, the echo data demonstrated that the peak flow velocity and flow volume with exercise reminders were higher than those with intermittent pneumatic compression on the 14th day after surgery. No significant difference in peak flow velocity or flow volume was observed between the two groups on the 3rd day, while better results were obtained with regular reminders when performing the same exercise. The results confirmed the effect of exercise reminders to increase the performance of exercise.
The proposed approach with a reminder device for TKA patients to exercise is similar to telerehabilitation and virtual rehabilitation. The aim of this approach was to increase exercise execution. Supervised telerehabilitation is an effective approach to enhance functional recovery after TKR [29]. In addition, the effectiveness of virtual rehabilitation is similar to that of traditional home or clinic physical therapy [30]. In the present study, a non-real-time device was found to increase TKR patients’ exercise habits at home. Such platforms encourage clinician–patient interaction even after discharge, and they have many advantages, including low cost, convenience, and lack of traffic movement [31].
Based on the results of this study, TKR surgery not only affects the surgical limb but also the nonoperative limb. Venous stasis was found in the nonoperative limb in the three groups; however, the incidence with active exercise and without reminding was obviously higher than that with intermittent pneumatic compression and active exercise with reminders. Although in the echo examination, there was no significant difference between the three groups, a prevention strategy for DVT should also be considered for the nonoperative limb, particularly in cases with a history of vascular disease.
In this study, Doppler echocardiography was used to detect the flow velocity in the vein, while plethysmography was used in previous studies [13,14]. The advantages of Doppler echocardiography are the direct measurement of the flow velocity inside the vessels, instead of an indirect speculation of the venous status. Furthermore, the level of evidence of the direct measurement is stronger than that of indirect speculation. The patients are more comfortable with Doppler technology because a higher pressure to stop blood flow in plethysmography is not needed during Doppler determination.
No DVT was observed in the present study. This might be due to the use of aspirin; hence, the coagulation mechanism was partially inhibited. Although stasis appeared in some patients, no DVT was found. Another possible reason is race: Asians have been reported to have lower DVT incidence than blacks [32]. Although no real DVT occurred, prophylaxis against DVT is still warranted, particularly in the high-risk group with a history of vascular disease.
5. Conclusions
This study proposed a new approach using regular alarm reminders on the ankle to increase the performance of active ankle pumping exercises and reducing the risk of DVT after TKR. Based on the present results, we recommend regular reminders with voice alarms and vibration from a watch for patients with TKR to increase the performance of active ankle pumping exercises after TKR during hospital stays and at home, particularly for patients who are not suitable for aspirin. Although an intermittent pneumatic compression is also another recommended option for the prevention of DVT, we do not recommend active ankle pumping exercise without any reminders or supervision.
Author Contributions
Conceptualization, M.-C.K.; methodology, Y.-H.T.; software, Y.-T.T.; validation, P.-C.C.; formal analysis, M.-T.L.; investigation, M.-C.K.; resources, T.-I.Y.; data curation, H.-W.H.; writing—original draft preparation, Y.-N.C.; writing—review and editing, Y.-N.C.; visualization, Y.-H.T.; supervision, M.-C.K.; project administration, M.-F.L.; funding acquisition, M.-C.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Ministry of Economic Affairs, Taiwan, grant number E10800026004-004 and Show Chwan Memorial Hospital, grant number RB19013.
Institutional Review Board Statement
The study protocol was reviewed and approved by the committee of the Institutional Review Board of Show Chwan Memory Hospital (080704 on 17 October 2019 and 1090604 on 6 August 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Maradit Kremers, H.; Larson, D.R.; Crowson, C.S.; Kremers, W.K.; Washington, R.E.; Steiner, C.A.; Jiranek, W.A.; Berry, D.J. Prevalence of total hip and knee replacement in the united states. J. Bone Jt. Surg. Am. Vol. 2015, 97, 1386–1397. [Google Scholar] [CrossRef] [PubMed]
- Itou, J.; Kuwashima, U.; Itoh, M.; Okazaki, K. No difference in the incidence or location of deep venous thrombosis according to use of pharmacological prophylaxis following total knee arthroplasty. BMC Musculoskelet. Disord. 2021, 22, 819. [Google Scholar] [CrossRef] [PubMed]
- Fujita, S.; Hirota, S.; Oda, T.; Kato, Y.; Tsukamoto, Y.; Fuji, T. Deep venous thrombosis after total hip or total knee arthroplasty in patients in japan. Clin. Orthop. Relat. Res. 2000, 375, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Warren, J.A.; Sundaram, K.; Kamath, A.F.; Molloy, R.M.; Krebs, V.E.; Mont, M.A.; Piuzzi, N.S. Venous thromboembolism rates did not decrease in lower extremity revision total joint arthroplasty from 2008 to 2016. J. Arthroplast. 2019, 34, 2774–2779. [Google Scholar]
- Boylan, M.R.; Perfetti, D.C.; Kapadia, B.H.; Delanois, R.E.; Paulino, C.B.; Mont, M.A. Venous thromboembolic disease in revision vs primary total knee arthroplasty. J. Arthroplast. 2017, 32, 1996–1999. [Google Scholar] [CrossRef] [PubMed]
- Shahi, A.; Chen, A.F.; Tan, T.L.; Maltenfort, M.G.; Kucukdurmaz, F.; Parvizi, J. The incidence and economic burden of in-hospital venous thromboembolism in the united states. J. Arthroplast. 2017, 32, 1063–1066. [Google Scholar] [CrossRef]
- Shahi, A.; Bradbury, T.L.; Guild, G.N., 3rd; Saleh, U.H.; Ghanem, E.; Oliashirazi, A. What are the incidence and risk factors of in-hospital mortality after venous thromboembolism events in total hip and knee arthroplasty patients? Arthroplast. Today 2018, 4, 343–347. [Google Scholar] [CrossRef]
- Matharu, G.S.; Kunutsor, S.K.; Judge, A.; Blom, A.W.; Whitehouse, M.R. Clinical effectiveness and safety of aspirin for venous thromboembolism prophylaxis after total hip and knee replacement: A systematic review and meta-analysis of randomized clinical trials. JAMA Intern. Med. 2020, 180, 376–384. [Google Scholar] [CrossRef]
- Millar, J.S.; Lawes, C.M.; Farrington, B.; Andrew, P.; Misur, P.; Merriman, E.; Walker, M. Incidence of venous thromboembolism after total hip, total knee and hip fracture surgery at waitemata district health board following a peer-reviewed audit. N. Z. Med. J. 2020, 133, 52–60. [Google Scholar]
- Anderson, D.R.; Dunbar, M.; Murnaghan, J.; Kahn, S.R.; Gross, P.; Forsythe, M.; Pelet, S.; Fisher, W.; Belzile, E.; Dolan, S.; et al. Aspirin or rivaroxaban for vte prophylaxis after hip or knee arthroplasty. N. Engl. J. Med. 2018, 378, 699–707. [Google Scholar] [CrossRef]
- Sung, J.J.; Lau, J.Y.; Ching, J.Y.; Wu, J.C.; Lee, Y.T.; Chiu, P.W.; Leung, V.K.; Wong, V.W.; Chan, F.K. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: A randomized trial. Ann. Intern. Med. 2010, 152, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lanas, A. Gastrointestinal bleeding associated with low-dose aspirin use: Relevance and management in clinical practice. Expert Opin. Drug Saf. 2011, 10, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Guan, X.H.; Wang, R.; Li, B.; Ning, B.; Su, W.; Sun, T.; Li, H.Y. Active ankle movements prevent formation of lower-extremity deep venous thrombosis after orthopedic surgery. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2016, 22, 3169–3176. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Chen, Q.; Ye, M.; Shi, G.H.; Zhang, B. Active ankle movement may prevent deep vein thrombosis in patients undergoing lower limb surgery. Ann. Vasc. Surg. 2016, 32, 65–72. [Google Scholar] [CrossRef]
- Snyder, M.A.; Sympson, A.N.; Scheuerman, C.M.; Gregg, J.L.; Hussain, L.R. Efficacy in deep vein thrombosis prevention with extended mechanical compression device therapy and prophylactic aspirin following total knee arthroplasty: A randomized control trial. J. Arthroplast. 2017, 32, 1478–1482. [Google Scholar] [CrossRef]
- Tyagi, V.; Tomaszewski, P.; Lukasiewicz, A.; Theriault, S.; Pelker, R. The role of intraoperative intermittent pneumatic compression devices in venous thromboembolism prophylaxis in total hip and total knee arthroplasty. Orthopedics 2018, 41, e98–e103. [Google Scholar] [CrossRef]
- Kim, K.I.; Kim, D.K.; Song, S.J.; Hong, S.J.; Bae, D.K. Pneumatic compression device does not show effective thromboprophylaxis following total knee arthroplasty in a low incidence population. Orthop. Traumatol. Surg. Res. OTSR 2019, 105, 71–75. [Google Scholar] [CrossRef]
- Chen, Q.; Huang, S.; Chen, X.; Feng, L.; Zhu, X. Clinical efficacy of multi-pattern detumescence after total knee arthroplasty treated with acupoint massage and mild moxibustion. Zhongguo Zhen Jiu = Chin. Acupunct. Moxibust. 2016, 36, 471–475. [Google Scholar]
- Moloney, M.C.; Lyons, G.M.; Egan, M.; Wallis, F.; Burke, P.E.; Kavanagh, E.; Grace, P.A. Does size matter? The impact of calf muscle volume on venous return in patients with venous leg ulcers. Phlebology 2007, 22, 65–69. [Google Scholar] [CrossRef]
- Zhen, K.Y.; Zhai, Z.G. Progress of intermittent pneumatic compression device application in prevention of venous thromboembolism in inpatients. Zhonghua Jie He He Hu Xi Za Zhi = Zhonghua Jiehe He Huxi Zazhi = Chin. J. Tuberc. Respir. Dis. 2020, 43, 599–603. [Google Scholar]
- Esserman, D.; Allore, H.G.; Travison, T.G. The method of randomization for cluster-randomized trials: Challenges of including patients with multiple chronic conditions. Int. J. Stat. Med. Res. 2016, 5, 2–7. [Google Scholar] [PubMed]
- Arthur, J.R.; Spangehl, M.J. Tourniquet use in total knee arthroplasty. J. Knee Surg. 2019, 32, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Ku, M.C.; Chen, W.J.; Lo, C.S.; Chuang, C.H.; Ho, Z.P.; Kumar, A. Femoral component alignment with a new extramedullary femoral cutting guide technique. Indian J. Orthop. 2019, 53, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Soffin, E.M.; Memtsoudis, S.G. Anesthesia and analgesia for total knee arthroplasty. Minerva Anestesiol. 2018, 84, 1406–1412. [Google Scholar] [CrossRef]
- Lucas, B. Total hip and total knee replacement: Postoperative nursing management. Br. J. Nurs. Mark Allen Publ. 2008, 17, 1410–1414. [Google Scholar] [CrossRef]
- Werkmeister, R.M.; Dragostinoff, N.; Palkovits, S.; Told, R.; Boltz, A.; Leitgeb, R.A.; Gröschl, M.; Garhöfer, G.; Schmetterer, L. Measurement of absolute blood flow velocity and blood flow in the human retina by dual-beam bidirectional doppler fourier-domain optical coherence tomography. Investig. Ophthalmol. Vis. Sci. 2012, 53, 6062–6071. [Google Scholar] [CrossRef]
- Line, B.R. Pathophysiology and diagnosis of deep venous thrombosis. Semin. Nucl. Med. 2001, 31, 90–101. [Google Scholar] [CrossRef]
- O’Brien, J.G.; Chennubhotla, S.A.; Chennubhotla, R.V. Treatment of edema. Am. Fam. Physician 2005, 71, 2111–2117. [Google Scholar]
- Fortier, L.M.; Rockov, Z.A.; Chen, A.F.; Rajaee, S.S. Activity recommendations after total hip and total knee arthroplasty. J. Bone Jt. Surg. Am. Vol. 2021, 103, 446–455. [Google Scholar] [CrossRef]
- Prvu Bettger, J.; Green, C.L.; Holmes, D.N.; Chokshi, A.; Mather, R.C., 3rd; Hoch, B.T.; de Leon, A.J.; Aluisio, F.; Seyler, T.M.; Del Gaizo, D.J.; et al. Effects of virtual exercise rehabilitation in-home therapy compared with traditional care after total knee arthroplasty: Veritas, a randomized controlled trial. J. Bone Jt. Surg. Am. Vol. 2020, 102, 101–109. [Google Scholar] [CrossRef]
- Chughtai, M.; Kelly, J.J.; Newman, J.M.; Sultan, A.A.; Khlopas, A.; Sodhi, N.; Bhave, A.; Kolczun, M.C., 2nd; Mont, M.A. The role of virtual rehabilitation in total and unicompartmental knee arthroplasty. J. Knee Surg. 2019, 32, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Owens, J.M.; Bedard, N.A.; Dowdle, S.B.; Gao, Y.; Callaghan, J.J. Venous thromboembolism following total knee arthroplasty: Does race matter? J. Arthroplast. 2018, 33, S239–S243. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).