Abstract
In recent years, nanomaterials have attracted significant research interest for applications in biomedicine. Many kinds of engineered nanomaterials, such as lipid nanoparticles, polymeric nanoparticles, porous nanomaterials, silica, and clay nanoparticles, have been investigated for use in drug delivery systems, regenerative medicine, and scaffolds for tissue engineering. Some of the most attractive nanoparticles for biomedical applications are nanoclays. According to their mineralogical composition, approximately 30 different nanoclays exist, and the more commonly used clays are bentonite, halloysite, kaolinite, laponite, and montmorillonite. For millennia, clay minerals have been extensively investigated for use in antidiarrhea solutions, anti-inflammatory agents, blood purification, reducing infections, and healing of stomach ulcers. This widespread use is due to their high porosity, surface properties, large surface area, excellent biocompatibility, the potential for sustained drug release, thermal and chemical stability. We begin this review by discussing the major nanoclay types and their application in biomedicine, focusing on current research areas for halloysite in biomedicine. Finally, recent trends and future directions in HNT research for biomedical application are explored.
1. Introduction
Nanoclays are inexpensive materials that constitute sedimentary rocks and derived soils and are classified into natural and synthetic clays [1,2,3]. They have at least one dimension in the order of 1–100 nm [4,5,6], have a high aspect ratio, a thickness of less than one nanometer, and a surface area in the range of 700 m squared per gram [6,7]. Nanoclay nanoparticles are mineral silicates with layered structural units that can form complex clay crystallites by stacking these layers [4]. The principal clay types include kaolinite, laponite, montmorillonite, and halloysite (Figure 1, Table 1) [1]. Nanoclays are abundant, mined at low cost, and do not threaten the environment. Accordingly, nanoclays have been studied and developed for aerospace, biomedical, commercial, and industrial applications [2]. Nanoclays, in general, have no mutagenic effect on the body [4], are cyto- and biocompatible [6], and are environmentally friendly [6,7].
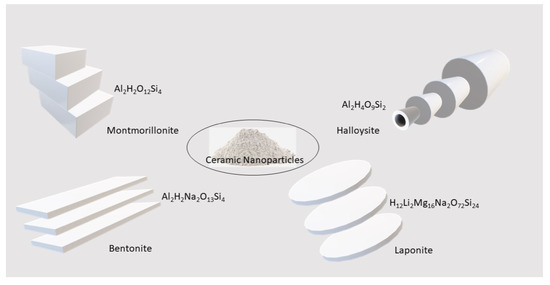
Figure 1.
Ceramic nanoparticle types and their morphologies.

Table 1.
Major types of clay nanoparticles.
Nanoclays are typically used as additives for polymeric materials, and their addition results in significant improvements in mechanical and thermal resistance and overall durability [8,9]. The market for nanoclays is in automotive, biomaterials, biomedicine, cosmetics, flame retardant materials, paints, pigments and dyes, packaging, and textiles [9,10]. For example, bentonite is used for exterior waterproofing treatment, an agent for removing impurities in oil, and as an absorbent and carrier for fertilizers or pesticides. Kaolinite is widely used in producing ceramics and porcelain. As with many nanoclays, it is also used as a bulk filler for paint, rubber, and plastics.
Due to their wide availability, relatively low cost, and relatively low and environmental impact, nanoclays have been widely used in preparing polymer matrix–nanoclay biomedical composites. These include bone repair, cancer therapy, drug delivery, tissue engineering, wound healing, and 3D printing [3,6,8,10]. Laponite, halloysite, and montmorillonite are among the most widely used clays. Halloysite nanotubes (HNTs) and montmorillonite have been used for drug delivery, gene delivery, cancer therapeutics, tissue engineering, and wound healing applications. Halloysite has been intensively studied because of such properties as high mechanical strength, high porosity, thermal resistance, and sustained drug release capability. Because of these properties, increased research is being focused on using HNTs as drug delivery systems and in bioactive bandages, tissue engineering scaffolds, and regenerative medicine. After a brief overview of the major nanoclays, this review will focus on the therapeutic applications of HNTs.
2. Nanoclay Types
2.1. Montmorillonite
Montmorillonite is an abundant phyllosilicate clay material composed of layered silica sheets. Each layer consists of two sheets, octahedral and tetrahedral sheets [11]. The octahedral sheet is aluminum and magnesium bonded with six oxygen and a hydroxyl group. The tetrahedral sheet is composed of linked silicon-oxygen tetrahedral and bonds with octahedra. It can be modified chemically to form nanocomposites. The loosely packed silicates layers can let water infiltrate the sheets, and the clay can swell. It also has excellent cation exchange capacity, producing nanocomposites from the naturally occurring montmorillonite [11,12]. Montmorillonite is the main constituent of bentonite clay.
As a nanoclay, montmorillonite can have particle length and breadth between 1.5 µm to 1/10th of a micron. The pore diameter is small compared to the length of the particle (~1 nm). Refs. [11,12] Because of its property to hold water and hydrophilic molecules, montmorillonite nanocomposites have been used as a filler material to make bioactive scaffolds. As montmorillonite also enhances the mechanical properties of the scaffold materials, it has been used as an additive to hydrogel or polymer scaffolds [11,12,13]. Montmorillonite has been combined with different scaffold materials such as chitosan, methyl methacrylate, gelatin, starch, and polycaprolactone for tissue engineering applications [14,15,16]. Montmorillonite nanoclay composite scaffolds have been studied for their applications in bone tissue engineering [15,16], controlled drug delivery [17], and wound healing [18,19].
2.2. Bentonite
Bentonite is an aluminum and phyllosilicate clay formed by weathering volcanic ash by water. Montmorillonite is a significant component of bentonite in addition to feldspar and quartz [11]. Being hydrophilic makes bentonite a very absorbent clay. Exfoliation of sodium and potassium salts from bentonite might result in plates 1 nm in thickness [11]. Bentonite being absorptive would make a suitable wound dressing additive. As a nanoclay in combination with scaffold materials, Bentonite has been studied for hemostatic effect in wound healing [20,21,22,23]. Bentonite or any other nanoclay material is a cost-efficient alternative to biological hemostatic agents such as fibrin, as biological hemostatic agents cost more in production and purification [24,25]. Since Bentonite has montmorillonite as its primary component, it has also been explored to manufacture scaffold materials used for skeletal tissue engineering applications. It would improve the mechanical properties of the soft scaffolding materials such as hydrogels [25,26,27]. Montmorillonite layers and sheets in bentonite make it a suitable nanoclay for drug delivery [28,29]. Its use in sustained and targeted drug release for targeted chemotherapy has also been investigated [30,31,32].
2.3. Laponite
Laponite®, synthetic clay nanoparticles (25–30 nm diameter, 1 nm thickness), closely resembles the natural clay mineral hectorite in both structure and composition [33,34]. Laponite is a 1:2 layered clay nanoparticle. One central octahedral magnesia sheet is sandwiched between two tetrahedral silica layered sheets. It is widely used in conserving stone, metals, organic materials, ceramics, and paintings. As a bulk filler and reinforcement agent, it is employed in agrochemical, cosmetics, mining, petroleum, and pharmaceutical industries. Laponite possesses an anisotropic nanometric shape and has different charge distribution [33]. Laponite, as a biomedical material, has been applied in drug delivery [34] and tissue engineering [35,36].
3. Halloysite Structure and Applications
3.1. HNT Structure
Halloysite nanotubes (HNTs) are naturally occurring aluminosilicate nanoparticles empirical formula Al2Si2O5(OH)4) with a chemical composition similar to kaolinite, dickite, or nacrite [37,38,39] (Figure 2). However, unlike kaolinite, dickite, and nacrite, the unit layers in halloysite are separated by a monolayer of water molecules [38,39]. As a result, a hydrated halloysite has a basal (d001) spacing of 10 Å, approximately 3 Å larger than kaolinite. Halloysite-(10 Å) can readily and irreversibly dehydrate to give the corresponding halloysite-(7 Å) form when halloysite-(10 Å) is heated to 90–150 °C. HNTs can be found in China, France, Belgium, New Zealand, America, and Brazil [40]. The chemical composition for halloysite-(7 Å) and halloysite-(10 Å) is Al2Si2O5(OH)4٠nH2O where n = 0 and 2, respectively [41,42,43]. If n is 2, the HNTs are hydrated, and if n is 0, the HNTs are dehydrated [10,11]. Therefore, AIPEA Nomenclature Committee recommended terms halloysite-(10 Å) for the hydrated mineral and halloysite-(7 Å) for the dehydrated form.

Figure 2.
The structure of halloysite and its potential for surface modification.
The layers of aluminum and silicate with alternating positive and negatively charged layers in halloysite make them suitable adsorbents for cations and anions [41]. Apart from the conventional use of halloysite to manufacture porcelain and in petrochemical applications, halloysite has been explored as a carrier material for drug delivery [37,38], tissue engineering [41,42], and wound healing applications [43]. HNTs can adopt a variety of morphologies. For example, an elongated tubule short tubular, spheroidal and platy nanoparticle shapes have been reported [44]. Spheroidal halloysite occurs widely, and it is common to find pseudo-spherical or spheroidal particles in weathered volcanic ashes and pumices [38,39,45].
The hollow tubular form in the submicrometer range is most commonly used. These tubules may be extended and thin, short and stubby, or emerging from other tubes [10]. The halloysite tubules’ size varies from 500–1000 nm in length with an outer diameter of 10–50 nm and an inner diameter measuring 5–20 nm depending on the deposit [43,44,45]. The neighboring alumina and silica layers, their hydration layers, create a packing disorder that induces curvature and the layers roll up, forming multilayer tubes. The HNT external surface comprises O-Si-O bonds with terminal hydroxyl groups [37,38]. The inner lumen comprises O-Al-O bonds, terminating in hydroxyl groups [46,47]. At pH 8.5 and below, these inner hydroxyl groups are mostly protonated, resulting in a positively charged inner lumen.
A wide range of active agents, including antibiotics, cancer drugs, marine biocides, and biological molecules, can be entrapped within the inner lumen and void spaces within the aluminosilicate shells [47,48,49,50]. HNTs nanotubes are non-cytotoxic on several cell types (up to concentrations of 0.1 mg/mL), including chondrocytes, dermal fibroblasts, osteoblasts, and stem cells on halloysite nanofilms or within HNT-hydrogel composites [48,49,50,51,52,53,54]. Examination of halloysite with in-vitro assays showed cells proliferated and maintained their cellular phenotype. Recent biocompatibility studies have shown that HNTs do not provoke a cytotoxic or host immune response [51,52]. As halloysite nanotubes have been shown to exhibit high biocompatibility levels and very low cytotoxicity, it represents an ideal candidate for new drug delivery and polymer systems.
3.2. HNTs in Cancer Therapeutics
HNTs have been studied for multiple applications. Currently, modified surface HNTs are being researched as an efficient delivery system for cancer drugs. For example, Chitosan oligosaccharide modified HNTs (HNTs-g-COS) demonstrated the ability to enhance the therapeutic efficacy of the anticancer drug doxorubicin (DOX) [53]. In vitro, DOX loaded HNTs-g-COS released in cell lysate in a controlled manner and increased the apoptosis effects of MCF-7 cells in flow cytometry results [53]. In vivo, the tumor inhibition ratio of DOX loaded HNTs-g-COS was two times higher than free DOX and no apparent systemic toxicity in DOX loaded HNTs-g-COS groups [53].
Synthesized chitosan grafted HNTs (HNTs-g-CS) also showed great potential as nanovehicles for anticancer drug delivery in cancer therapy [54]. The research found that HNTs-g-CS had a significantly enhanced curcumin loading capability and good serum stability. However, the curcumin-loaded HNTs-g-CS show specific toxicity to various cancer cell lines, including HepG2, MCF-7, SV-HUC-1, EJ, Caski, and HeLa demonstrate an inhibition concentration of IC50 at 5.3–192 mM as assessed by cytotoxicity studies [54]. In addition, this nanocomposite has a too high anticancer activity in EJ cells compared to the other cancer cell lines [54].
Folate-conjugated HNTs can be an efficient drug carrier for targeted breast cancer therapy via intravenous injection [55]. HNT conjugated with polyethylene glycol and folate (HNTs-PEG-FA) is designed as a targeted drug delivery system [55]. Doxorubicin (DOX) loaded HNTs-PEG-FA shows significant inhibition of proliferation and induction of death in MCF-7 cells with a positive folate receptor [55]. DOX-loaded HNTs-PEG-FA leads to more mitochondrial damage and apoptosis than the same dose of DOX [55]. In contrast to DOX, DOX-loaded HNTs-PEG-FA effectively reduces heart toxicity and inhibits substantial tumor growth with higher cleaved caspase-3 protein levels in tumor tissue of 4T1-bearing mice [55]. DOX-loaded HNTs-PEG-FA reveals more DOX in tumor tissue than in other normal tissues, including the heart, spleen, lung, and kidney.
3.3. HNTs in Drug Delivery
HNTs have been used as a drug delivery carrier for many clinically meaningful drugs [56,57]. HNT can be loaded with different drugs, including anticancer drugs, antibiotics, analgesics, antihypertension, anti-inflammatory drugs, and therapeutic nucleic acids [57]. HNTs have also been used for the controlled release of antibiotics, including tetracycline, ofloxacin, norfloxacin, amoxicillin, and ciprofloxacin [57]. Amoxicillin (AMX) loaded HNT is incorporated into a polylactic acid-glycolic acid copolymer (PLGA) solution, which is electrospun with water-soluble chitosan nanofibers in two different syringes simultaneously, thereby making a composite material [58]. Compared to loading the drug directly into the polymer matrix, HNT extends the release time of AMX and reduces the initial burst release [58].
Analgesic drugs and anti-inflammatories, such as ibuprofen (IBU), diclofenac sodium, and aspirin, have low water solubility and bioavailability [59]. Therefore, developing an efficient drug delivery system by encapsulating drugs in a nanoparticle system to enhance their bioavailability is urgently needed [59]. 3-aminopropyltriethoxysilane (APTES) functionalized surface HNT as a carrier for IBU could promote IBU loading [60]. By restricting the APTES oligomerization in the lumen, free lumen space was preserved, resulting in a 25.4% greater loading rate than that in unmodified halloysite. In order to sustain a more significant release of IBU, an ideal hydrophobic sustained-release drug delivery system was designed [60]. The HNT lumen (EHNT) was enlarged, and hydrophobic modification of the external surface by organosilane (OS) was done prior to loading IBU [60]. The OS composite of EHNT demonstrated a sustained-release performance for IBU (100 h) [60].
Halloysite has been used in other drug delivery systems such as anti-hypertension and gene therapeutic agent-delivery systems. Polydopamine was used to cap HNT for a controlled drug release [61]. After dispersion in a sodium alginate matrix and crosslinking via Fe3+, HNTs were used to deliver diltiazem hydrochloride, widely used in high blood pressure therapy [61]. In gene therapeutic agent-delivery systems, HNTs were surface-modified with γ-aminopropyltriethoxysilane and assembled with antisense oligodeoxynucleotides (ASODNs) [62]. These functional HNT complexes showed improved intracellular delivery efficiency and inhibited the tumor growth activity of ASODNs [62].
3.4. HNTs in Tissue Engineering
Halloysite has a variety of applications in the field of tissue engineering. They are used in bone implants, dental fillings, and tissue scaffolds [63]. HNTs mixed with bone cement and used as a drug carrier and release system are promising applications. The research found HNTs loaded with the antibiotic gentamicin sulfate with a concentration of 5–8 wt% in the cement (PMMA) provide sustained release up to 300–400 h [40]. This PMMA/halloysite/gentamicin composite tensile strength does not deteriorate compared with pure cement, and its adhesion to bone is significantly increased [53]. HNTs resin-dentin bond is similar to halloysite-PMMA bone cement [64]. HNTs and functionalized HNTs improved mechanical properties significantly [64,65,66]. Silver nanoparticle immobilized HNT (HNT/Ag) fillers significantly improved mechanical properties [67]. This filler also showed a significant antibacterial activity observed on S. mutans [67]. Karnik et al., 2015 were the first to show that a nanoenhanced hydrogel could significantly enhance the biological activity of bone progenitor cells and achieve a sustained release of BMP-2 for over a week [49].
Currently, hydrogel scaffolds are being applied to transplant cells and engineer nearly every tissue in the body, including cartilage, bone, and smooth muscle [68]. Compared to pure alginate scaffolds, alginate/halloysite nanotube (HNTs) composite scaffolds significantly enhance compressive strength and compressive modulus in dry and wet states [69]. Furthermore, HNTs increased the scaffold density, decreased the swelling ratio in water, and improved alginate’s thermal stability [69]. In addition, the alginate/HNT composite scaffolds have better cytocompatibility [69]. Chitosan–halloysite nanotubes (HNTs) nanocomposite (NC) scaffolds have similar results as alginate HNTs composite scaffolds [70]. Compared to the pure chitosan scaffold, the NC scaffolds exhibited significantly improved compressive strength, compressive modulus, and thermal stability [70]. Furthermore, the chitosan–HNTs nanocomposites were cytocompatible even when the HNTs load was 80% [70].
3.5. HNTs in Wound Healing
The absorptive capacity of HNTs has been used in several wound healing applications. An HNT/chitosan oligosaccharide nanocomposite was tested for its healing capacity in a mouse model [71]. The nanocomposite allowed enhanced skin reepithelization and reorganization compared to controls and the. Results suggested it has potential as a medical device for wound healing. Chitosan has been combined with HNTs in many would bandage and healing applications. Li et al. (2014) showed that the HNT/chitosan sponges significantly increased wound closure ratio compared with pure chitosan. HNT addition also aided in re-epithelialization and collagen deposition [72].
HNTs and other nanoclays such as montmorillonite used as scaffolds also possess the capability of improving the wound healing response. For example, Sandri et al. (2020) produced electrospun scaffolds incorporating these nanoclays, and their results showed enhanced fibroblast cell attachment and proliferation with very little to no proinflammatory activity [73]. A final example of potential wound healing applications using HNTs as a key contributor is the study by Wali et al. (2019) [74]. This study loaded electrospun cellulose ether-PVA nanofiber mats with HNTs and gentamicin sulfate. As a result, the mats offered sustained gentamicin release and advanced wound healing in an animal model [74]. The above studies have demonstrated that HNTs, especially chitosan-HNTs nanocomposites, have significant potential for burns, chronic wounds, and diabetic foot ulcers.
4. Recent Trends in HNT Research
4.1. HNTs as a Drug Carrier
As mentioned previously, HNTs have been used for various biomedical areas because of unique properties such as hemostatic properties. However, one of the most critical applications of HNT is drug delivery systems, and it is used as a drug carrier. For instance, in 2020, Cheng et al. [75] used HNTs to fabricate smart hydrogels with H2O2—responsive release properties. The researchers first prepared drug loaded HNTs and then, they characterized the composite hydrogels by FTIR, TGA, XPS, XRD, and TEM. The smart hydrogel was prepared with polyvinyl alcohol and released the drugs under a pathological concentration ([H2O2] = 200 μm) because of degradation of the hydrogel in the presence of H2O2 (Figure 3). Core-shell gel-based chitosan fabricated by a dropping method and HNTs because of hollow cavity used as a carrier [76]. In this study, Lisuzzo et al. [76] utilized alginate as a coating layer (shell). In the hybrid gel beads, HNTs showed proper dispersion within the beads, and because of the core-shell structure of gel, the release of the drug was controllable.
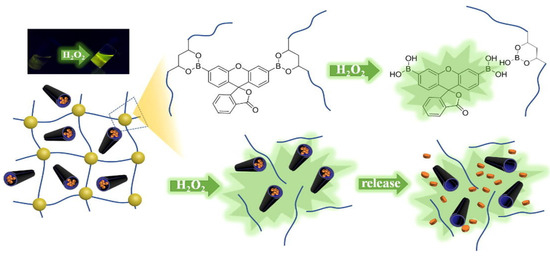
Figure 3.
Schematic of the mechanism of release when hydrogel under pathological concentration. Reprinted by permission of the publisher.
4.2. HNTs in Coatings and Films
Akrami-Hasan-Kohal et al. [77] used the solution casting process to fabricate nanocomposite films with HNTs. In this study, the various concentrations of HNTs were loaded into the nanocomposites films. As expected, mechanical properties and water absorption were improved, and the films were cytocompatible. Xie et al. [78] used HNT for preparing nanocomposite films based on chitosan for biomedical applications. The film exhibited decent mechanical properties, and dosages of HNT had a direct effect on this property because of creating a three-dimensional network.
Additionally, water-resistance and the nanocomposite films’ thermal stability were improved meaningfully. In 2019, Devi et al. [79] ternary nanocomposite films were fabricated using solution casting. This film used chitosan, starch, and HNTs to improve mechanical properties, water absorption capacity, water solubility, and water vapor transmission rate. Furthermore, these hydrophilic films were non-hemolytic and impermeable to bacteria. Mohebali et al. [80] prepared elastomeric nanocomposites based on HNT surface modification using APTES and then a polyvinyl alcohol (PVA) coating applied through the layer-by-layer assembly. As a result, the nanocomposite film exhibited antibacterial properties and had a synergistic anti-infection effect (Figure 4). Furthermore, drug release was sustained and controllable.
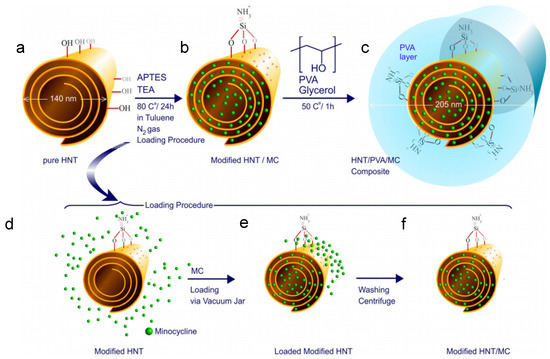
Figure 4.
SEM image of pure HNT (a), surface of HNT/PVA (b), cross section of HNT/PVA (c), surface of HNT/PVA/MC, Schematic of drug loading, surface modification, and synthesis of HNT/PVA nanocomposites (d–f). Reprinted by permission of the publisher.
4.3. HNTs and 3D Printing
HNTs and 3D printing have also supported tissue regeneration of bone defects. For example, Weisman et al. [81] used PLA and gentamicin-doped HNTs to print a range of medical devices. For example, Tappa et al. [82] used doped HNTs and PLA to 3D print customized bioactive and absorbable surgical screws, pins, and bone plates for localized drug delivery.
HNTs and 3D printing have also been used to support tissue regeneration of bone defects. Illustration, Wu et al. [83] in 2019, used HNTs for coating on 3D printed scaffolds to guide human mesenchymal stem cells (hMSCs) orientation. Polylactic acid scaffolds consisting of different patterns were printed and functionalized by a polydopamine. Using field emission scanning electron microscopy (FE-SEM), the researcher found HNTs successfully coated on various patterns. Because of HNT addition, the scaffolds’ surface roughness and hydrophilicity properties improved, and scaffolds could induce cell orientation. Moreover, the adhesion and proliferation of cells increased because of this supportive cell coating (Figure 5).
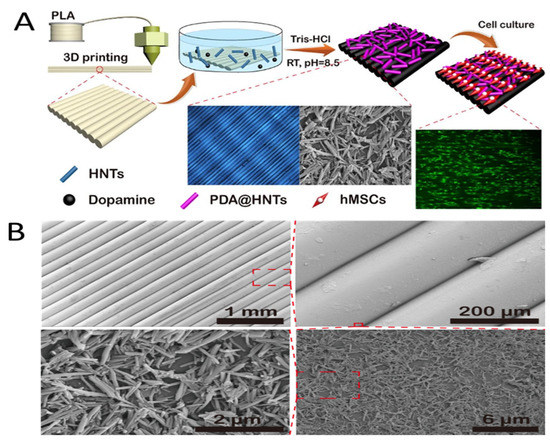
Figure 5.
(A) Graphic abstract of the HNTs coated PLA printed scaffolds with different pattern for HNT patterns guiding cell orientation. (B) FE-SEM images of HNTs coated printed pattern surfaces with various magnification. Reprinted by permission of the publisher.
4.4. Metalized HNT Applications
Early in human history, metal and metal salts were used for various applications. For example, Greek and Roman cultures used silver vessels to preserve liquids [84]. Colloidal silver was used extensively in medical treatment, and copper-based medicines were used in treating eczema, lupus, anemia, chorea, syphilis, and zinc salts were used in wound treatment. Understanding how metallic nanostructures interact with microorganisms is a rapidly growing area of inquiry in the biomedical field will offer significant advantages in diagnostic and therapeutic applications (Table 2). Nanoparticles offer unique physical properties that have associated benefits for drug delivery. For example, some metal nanoparticles have bactericidal effects due to their high surface-to-volume ratio and small size, allowing them to interact with bacterial cell membranes rather than release metal ions into the solution. Copper, silver, and zinc nanoparticles, in particular, are known for their excellent antimicrobial properties and have additional beneficial functionalities [84,85].

Table 2.
Potential applications of metalized HNTs.
Surface functionalization of HNTs with different components, including metals, antibiotics, and bioactive compounds, is of increased importance for their potential use in biomedical devices, antimicrobial surface coatings, drug delivery systems, radiation absorbent composites, elastomer composites, electronic components, and as industrial catalysts (Figure 6) [86]. The outer surface of HNTs can be used for adsorption of metal NPs thus preventing their aggregation, reducing toxicity, and providing more sustained antimicrobial/viral action. Boyer and. Mills (2016) used a simple method (US Patent #9,981,074 B1) for the fabrication of HNT- supported metal nanoparticles [87]. Metals nanoparticles, such as silver, copper, gold, and other metal nanoparticles can be directly deposited onto the surfaces of HNTs. Existing fabrication methods include lengthy multi-step processes that include metal-salts or organic compounds, reducing agents, high temperatures, and expensive equipment to achieve metallization of the halloysite surface [88].

Figure 6.
Biomedical and industrial applications of metallized HNTs.
A strategy for controlled weight deposition of positively charged metal ions on negatively charged HNTs dispersed in an aqueous medium where the extent of metallization can be controlled through changes in voltage, solvent medium, time, and other electrolytic parameters. Additionally, this process does not require the use of any toxic chemicals, expensive reagents, or lengthy pre-processing steps [88].
This rapid and low-cost method was used in various applications, from 3D printing to surface coats. PLA 3D printed scaffolds incorporating metal coated HNTs for bone tissue regeneration have recently been published. Luo et al. [89] used a surface modification method to reduce the hydrophobicity of PLA. This study used fetal bovine serum and NaOH to coat PLA scaffolds containing Zn-coated HNTs (Figure 7). The scaffolds possessed high mechanical strength and showed an osteoinductive potential. A strategy for controlled weight deposition of positively charged metal ions on negatively charged.

Figure 7.
(A) Optical and laser combined image of 3D printed PLA square. (B) EDS elemental analysis for coated PLA square [87].
HNTs dispersed in an aqueous medium where metallization can be controlled using changes in voltage, solvent medium, time, and other electrolytic parameters without using any toxic chemicals, expensive reagents, or lengthy pre-processing steps [88].
This rapid and low-cost method was used in various applications, from 3D printing to surface coats. PLA 3D printed scaffolds incorporating metal coated HNTs for bone tissue regeneration have recently been published. Luo et al. [87] used a surface modification method to reduce the hydrophobicity of PLA. This study used fetal bovine serum and NaOH to coat PLA scaffolds containing Zn-coated HNTs (Figure 6). The scaffolds possessed high mechanical strength and showed an osteoinductive potential.
Furthermore, the external coating of antibiotics preserved the osteogenic properties but also significantly reduced bacterial growth. [87] A similar study used 3D printed PLA scaffolds modified using an alkali treatment to increase hydrophilicity and the surface-functionalized using a suspension of Zinc/HNTs-Ag-Chitosan Oligosaccharide Lactate [88].
5. Future Directions in HNT Research
Nanoclays are promising drug delivery carriers and additive or bioactive agents for tissue regenerative medicine and engineering. The reason is their biocompatibility, low toxicity, ease of surface modification, material enhancement properties, cost, and capability of encapsulating drugs. The application of clay nanomaterials allows the nanoparticle-based on size, solubility, surface charge, cationic exchange capacity, dispersibility, and drug release rate. Bioactive agents or drugs can be incorporated into the layered spaces or nanopores of montmorillonite, kaolinite, halloysite nanotube through various reactions. Current research on nanoclays explores novel drug/clay or drug/clay/polymer composites as sustained drug delivery systems. The objective is to deliver a ‘focal and local’ drug dosage to target sites with low toxicity. Nanoclay modification methods can modify surface properties for added functionalities or targeted drug delivery.
The future of HNTs in biomedicine looks promising. The US FDA regards them as generally regarded as safe (GRAS). HNTs have been used for drug delivery, gene delivery, cancer therapeutics, tissue engineering, and wound healing applications and are one of the most promising nanoclays. HNTs are biocompatible, possess high mechanical strength, high porosity, offer sustained drug release profiles, and their surfaces can be easily modified. As a result, HNTs have been used in numerous novel applications ranging from stem cell encapsulation and tissue engineering to intracellular and extracellular drug systems.
HNTs added to a polymer and fabricated as a scaffold can be fabricated through blow spinning, electrospinning, 3D printing, and bioprinting with appropriate pore size, mechanical strength and loaded with bioinstructive molecules.
During the last decade, increased research has been focused on using HNTs for non-medical applications, including adsorbents, chemical and corrosion resistance, curation of archeological and cultural materials, electromagnetic protection, and water purification. Here, surface modification of the HNT surface enables customized and tailored solutions for numerous biotechnological, aerospace, environmental, and military needs.
While HNTs have demonstrated promising potential in drug delivery, cancer therapy, gene therapy, and tissue engineering applications, many challenges are still ahead before their widespread clinical application. As an anti-cancer nanoparticle, a significant issue is the exact mechanism of cell death necrosis or apoptosis. They are entering inside the cells by this route, though several studies have examined cell uptake. In addition, while many studies suggest that HNTs are cyto- and biocompatible, there is no clear understanding of the mechanism(s) of interaction with living cells, organs, and organisms. Therefore, the biological responses to HNTs must be thoroughly investigated through additional in-vitro and in-vivo research leading to a complete understanding of HNT impact on cellular pathways, further toxicity profiling, and how HNTs are stored within the body or eliminated. Lacking this knowledge limits their usage for advanced drug delivery, bone regeneration, or therapeutic medical applications.
Author Contributions
All authors contributed equally to writing and editing of the manuscript. The conceptual framework for the manuscript was conceived by D.K.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by NASA EPSCoR Rapid Response Research Opportunity. 21-EPSCoR-R3-0009 entitled Nano-based Ceramic-metal Composites to Support Planetary Agrosystems.
Institutional Review Board Statement
No humans or animals were used in this study.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Savic, I.; Stojiljkovic, S.; Savic, I.; Gajic, D. Industrial application of clays and clay minerals. In Clays and Clay Minerals: Geological Origin, Mechanical Properties and Industrial Applications; Wesley, L.R., Ed.; Nova Science Publishers: New York, NY, USA, 2014; pp. 379–402. [Google Scholar]
- Guo, F.; Aryana, S.; Han, Y.; Jiao, Y. A review of the synthesis and applications of polymer–nanoclay composites. Appl. Sci. 2018, 8, 1696. [Google Scholar] [CrossRef]
- Sandri, G.; Bonferoni, M.C.; Rossi, S.; Ferrari, F.; Aguzzi, C.; Viseras, C.; Caramella, C. Clay minerals for tissue regeneration, repair, and engineering. In Wound Healing Biomaterials; Ågren, M.S., Ed.; Elsevier: Amsterdam, The Netherlands, 2016; pp. 385–402. ISBN 9781782424567. [Google Scholar]
- Suresh, R.; Borkar, N.S.; Sawant, V.A.; Shende, V.S.; Dimble, S.K. Nanoclay drug delivery system. Inter. J. Pharma. Sci. Nanotech. 2010, 3, 901–905. [Google Scholar]
- Kotal, M.; Bhowmick, A.K. Polymer nanocomposites from modified clays: Recent advances and challenges. Prog. Polym. Sci. 2015, 51, 127–187. [Google Scholar] [CrossRef]
- Sánchez-Fernández, A.; Peña-Parás, L.; Vidaltamayo, R.; Cué-Sampedro, R.; Mendoza-Martínez, A.; Zomosa-Signoret, V.C.; Rivas-Estilla, A.M.; Riojas, P. Synthesization, characterization, and in vitro evaluation of cytotoxicity of biomaterials based on halloysite nanotubes. Materials 2014, 7, 7770–7780. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Long, M.; Huang, P.; Yang, H.; Chang, S.; Hu, Y.; Tang, A.; Mao, L. Emerging integrated nanoclay-facilitated drug delivery system for papillary thyroid cancer therapy. Sci. Rep. 2016, 6, 33335. [Google Scholar] [CrossRef]
- Jawaid, M.; Qaiss, A.K.; Bouhfid, R. Nanoclay Reinforced Polymer Composites: Nanocomposites and Bionanocomposites; Springer: Singapore, 2016. [Google Scholar]
- Lau, L.; Gu, C.; Hui, D. A critical review on nanotube and nanotube/nanoclay related polymer composite materials. Compos. Part B Eng. 2006, 37, 425–436. [Google Scholar] [CrossRef]
- Uddin, F. Montmorillonite: An Introduction to Properties and Utilization; IntechOpen: London, UK, 2018. [Google Scholar]
- Ali, A. Effect of incorporation of montmorillonite on Xylan/Chitosan conjugate scaffold. Colloids Surf. Part B 2019, 180, 75–82. [Google Scholar] [CrossRef]
- Cui, Z.-K.; Kim, S.; Baljon, J.J.; Wu, B.M.; Aghaloo, T.; Lee, M. Microporous methacrylated glycol chitosan-montmorillonite nanocomposite hydrogel for bone tissue engineering. Nat. Commun. 2019, 10, 3523. [Google Scholar] [CrossRef] [PubMed]
- Haroun, A.A.; Gamal-Eldeen, A.; Harding, D.R.K. Preparation, characterization and in vitro biological study of biomimetic three-dimensional gelatin–montmorillonite/cellulose scaffold for tissue engineering. J. Mater. Sci. Mater. Med. 2009, 20, 2527–2540. [Google Scholar] [CrossRef] [PubMed]
- Mauro, N.; Chiellini, F.; Bartoli, C.; Gazzarri, M.; Laus, M.; Antonioli, D.; Griffiths, P.; Manfredi, A.; Ranucci, E.; Ferruti, P. RGD-mimic polyamidoamine–montmorillonite composites with tunable stiffness as scaffolds for bone tissue-engineering applications. J. Tissue Eng. Regen. Med. 2017, 1, 2164–2175. [Google Scholar] [CrossRef]
- Jamshidi, M. Nanoclay reinforced starch-polycaprolactone scaffolds for bone tissue Engineering. J. Tissues Mater. 2019, 2, 55–63. [Google Scholar]
- Chen, M. Fabrication and characterization of a rapid prototyped tissue engineering scaffold with embedded multicomponent matrix for controlled drug release. Int. J. Nanomed. 2012, 2012, 4285–4297. [Google Scholar] [CrossRef]
- Noori, S. Nanoclay enhanced the mechanical properties of poly(vinylalcohol)/chitosan/montmorillonite nanocomposite hydrogel as wound dressing. Procedia Mater. Sci. 2015, 1, 52–156. [Google Scholar]
- Garcia-Villen, F. Montmorillonite-norfloxacin nanocomposite intended for healing of infected wounds. Int. J. Nanomed. 2019, 14, 5051–5060. [Google Scholar] [CrossRef]
- Emami-Razavi, S.H. Effect of bentonite on skin wound healing: Experimental study in the rat model. Acta Med. Iran. Vol. 2016, 44, 235–240. [Google Scholar]
- Alavi, M.; Totonchi, A.; Okhovat, M.A.; Motazedian, M.; Rezaei, P.; Atefi, M. The effect of a new impregnated gauze containing bentonite and halloysite minerals on blood coagulation and wound healing. Blood Coagul. Fbrinolysis 2014, 25, 856–859. [Google Scholar] [CrossRef]
- Khoshmohabat, H.; Dalfardi, B.; Dehghanian, A.; Rasouli, H.R.; Mortazavi, S.M.J.; Paydar, S. The effect of CoolClot hemostatic agent on skin wound healing in rats. J. Surg. Res. 2015, 200, 732–737. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R. Kaolin and halloysite deposits of China. Clay Miner. 2004, 39, 1–15. [Google Scholar] [CrossRef]
- Liu, M.; Shen, Y.; Daib, L.; Zhou, C. The improvement of hemostatic and wound healing property of chitosan by halloysite nanotubes. RSC Adv. 2014, 4, 23540–23553. [Google Scholar] [CrossRef]
- Fang, F.; Xu, Y.; Wang, Z.; Zhou, W.; Yan, L.; Fan, F.; Liu, H. 3D porous chitin sponge with high absorbency, rapid shape recovery, and excellent antibacterial activities for noncompressible wound. Chem. Eng. J. 2020, 388, 124169. [Google Scholar] [CrossRef]
- Devi, N. Preparation and characterization of chitosan-bentonite nanocomposite films for wound healing application. Int. J. Biol. Macromol. 2017, 104, 1897–1904. [Google Scholar] [CrossRef] [PubMed]
- Adams, L.A. Bentonite clay and waterglass porous monoliths Via the sol-gel process. J. Met. Mat. Min. 2011, 21, 1–6. [Google Scholar]
- Essien, E.R.; Adams, L.A.; Shaibu, R.O.; Oki, A. Sol-gel bioceramic material from bentonite clay. J. Biomed. Sci. Eng. 2013, 6, 258–264. [Google Scholar] [CrossRef][Green Version]
- Shahbuddin, N.S. Alumina Foam (AF) Fabrication optimization and SBF immersion studies for AF, hydroxyapatite (HA) coated AF (HACAF) and HA-bentonite coated AF (HABCAF) Bone Tissue Scaffolds. Procedia Chem. 2016, 19, 884–890. [Google Scholar] [CrossRef]
- Adams, L.A.; Essien, E.R.; Kaufmann, E.E. Mechanical and bioactivity assessment of wollastonite/PVA composite synthesized from bentonite clay. Ceramica 2019, 65, 246–251. [Google Scholar] [CrossRef]
- Bajaj, H.; Kevadiya, B.; Joshi, G.; Patel, H.; Abdi, S. Montmorillonite-alginate composites as a drug delivery system: Intercalation and In vitro release of diclofenac sodium. Indian J. Pharm. Sci. 2010, 72, 732–737. [Google Scholar] [CrossRef]
- Park, J.-H.; Shin, H.-J.; Kim, M.H.; Kim, J.-S.; Kang, N.; Lee, J.-Y.; Kim, K.-T.; Lee, J.I.; Kim, D.-D. Application of montmorillonite in bentonite as a pharmaceutical excipient in drug delivery systems. J. Pharm. Investig. 2016, 46, 363–375. [Google Scholar] [CrossRef]
- Hosseini, F.; Hosseini, F.; Jafari, S.M.; Taheri, A. Bentonite nanoclay-based drug-delivery systems for treating melanoma. Clay Miner. 2018, 53, 53–63. [Google Scholar] [CrossRef]
- Aguzzi, C.; Cerezo, P.; Viseras, C.; Caramella, C. Use of clays as drug delivery systems: Possibilities and limitations. Appl. Clay Sci. 2007, 36, 22–36. [Google Scholar] [CrossRef]
- Thomas, H.; Alves, C.S.; Rodrigues, J. Laponite®: A key nanoplatform for biomedical applications? Nanomed. Nanotechnol. Biol. Med. 2018, 14, 2407–2420. [Google Scholar] [CrossRef]
- Das, S.S.; Neelam; Hussain, K.; Singh, S.; Hussain, A.; Faruk, A.; Tebyetekerwa, M. Laponite-based nanomaterials for biomedical applications: A Review. Curr. Pharm. Des. 2019, 25, 424–443. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Wang, S.; Li, K.; Ju, Y.; Li, J.; Zhang, Y.; Li, J.; Liu, X.; Shi, X.; Zhao, Q. Preparation of laponite bioceramics for potential Bbne tissue engineering applications. PLoS ONE 2014, 9, e99585. [Google Scholar] [CrossRef]
- Levis, S.; Deasy, P. Characterisation of halloysite for use as a microtubular drug delivery system. Int. J. Pharm. 2002, 243, 125–134. [Google Scholar] [CrossRef]
- Jousseni, E.; Petit, S.; Churchman, J.; Theng, B.; Delvaux, D.R.B. Halloysite clay minerals: A review. Clay Min. 2005, 40, 383–426. [Google Scholar] [CrossRef]
- Noro, H. Hexagonal platy halloysite in an altered tuff bed, Komaki City, Aichi Prefecture, Central Japan. Clay Miner. 1986, 21, 401. [Google Scholar] [CrossRef]
- Wei, W.; Abdllayev, E.; Goeders, A.; Hollister, A.; Lvov, L.; Mills, D.K. Clay nanotube/poly(methyl methacrylate) bone cement composite with sustained antibiotic release. Macromol. Mat. Eng. 2012, 297, 645–653. [Google Scholar] [CrossRef]
- De Silva, R.T.; Dissanayake, R.K.; Mantilaka, M.M.M.G.P.G.; Wijesinghe, W.P.S.L.; Kaleel, S.S.; Premachandra, T.N.; Weerasinghe, L.; Amaratunga, G.A.J.; de Silva, K.M.N. Drug-loaded halloysite nanotube-reinforced electrospun alginate-based nanofibrous scaffolds with sustained antimicrobial protection. ACS Appl. Mater. Interfaces 2018, 10, 33913–33922. [Google Scholar] [CrossRef]
- Karnik, S.; Mills, D.K. Clay nanotubes as growth factor delivery vehicle for bone tissue engineering. J. Nanomed. Nanotechnnol. 2013, 4, 102. [Google Scholar]
- Satish, S.; Tharmavaram, M.; Rawtani, D. Halloysite nanotubes as a nature’s boon for biomedical applications. Nanobiomedicine 2019, 6, 1849543519863625. [Google Scholar] [CrossRef]
- Pasbakhsh, P.; De Silva, R.; Vahedi, V.; Churchman, G.J. Halloysite nanotubes: Prospects and challenges of their use as additives and carriers—A focused review. Clay Miner. 2016, 51, 479–487. [Google Scholar] [CrossRef]
- Lvov, Y.; Abdullayev, E. Functional polymer–clay nanotube composites with sustained release of chemical agents. Prog. Polym. Sci. 2013, 38, 1690–1719. [Google Scholar] [CrossRef]
- Mousavi, S.M.; Hashemi, S.A.; Salahi, S.; Hosseini, M.; Ali Mohammad Amani, A.M.; Aziz Babapoor, A. Development of clay nanoparticles toward bio and medical applications. In Chapter 8 in Current Topics in the Utilization of Clay in Industrial and Medical Applications; InTech Open: Zagreb, Croatia, 2018. [Google Scholar]
- Tharmavaram, M.; Gaurav, P.; Deepak, R. Surface modified halloysite nanotubes: A flexible interface for biological, environmental and catalytic applications. Adv. Colloid Interface Sci. 2018, 261, 82–101. [Google Scholar] [CrossRef]
- Patel, S.; Jammalamadaka, U.; Sun, L.; Tappa, K.; Mills, D.K. Sustained release of antibacterial agents from doped halloysite nanotubes. Bioengineering 2015, 3, 1. [Google Scholar] [CrossRef] [PubMed]
- Karnik, S.; Hines, K.; Mills, D.K. Nanoenhanced hydrogel system with sustained release capabilities. J. Biomed. Mater. Res. Part A 2014, 103, 2416–2426. [Google Scholar] [CrossRef]
- Romero-Trigueros, C.; Parra, M.; Bayona, J.M.; Nortes, P.; Alarcón, J.J.; Nicolás, E. Effect of deficit irrigation and reclaimed water on yield and quality of grapefruits at harvest and postharvest. LWT Food Sci. Technol. 2017, 85, 405–411. [Google Scholar] [CrossRef]
- Fakhrullina, G.I.; Akhatova, F.S.; Lvov, Y.M.; Fakhrullin, R.F. Toxicity of halloysite clay nanotubes in vivo: A Caenorhabditis elegans study. Environ. Sci. Nano 2014, 2, 54–59. [Google Scholar] [CrossRef]
- Kryuchkova, M.; Danilushkina, A.; Lvov, Y.; Fakhrullin, R. Evaluation of toxicity of nanoclays and graphene oxide in vivo: A Paramecium caudatum study. Environ. Sci. Nano 2016, 3, 442–452. [Google Scholar] [CrossRef]
- Yang, J.; Wu, Y.; Shen, Y.; Zhou, C.; Li, Y.-F.; He, R.-R.; Liu, M. Enhanced Therapeutic Efficacy of Doxorubicin for Breast Cancer Using Chitosan Oligosaccharide-Modified Halloysite Nanotubes. ACS Appl. Mater. Interfaces 2016, 8, 26578–26590. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Chang, Y.; Yang, J.; You, Y.; He, R.; Chen, T.; Zhou, C. Functionalized halloysite nanotube by chitosan grafting for drug delivery of curcumin to achieve enhanced anticancer efficacy. J. Mater. Chem. B 2016, 4, 2253–2263. [Google Scholar] [CrossRef]
- Wu, Y.-P.; Yang, J.; Gao, H.-Y.; Shen, Y.; Jiang, L.; Zhou, C.; Li, Y.-F.; He, R.-R.; Liu, M. Folate-Conjugated Halloysite Nanotubes, an Efficient Drug Carrier, Deliver Doxorubicin for Targeted Therapy of Breast Cancer. ACS Appl. Nano Mater. 2018, 1, 595–608. [Google Scholar] [CrossRef]
- Lvov, Y.M.; Devilliers, M.M.; Fakhrullin, R.F. The application of halloysite tubule nanoclay in drug delivery. Expert Opin. Drug Deliv. 2016, 13, 977–986. [Google Scholar] [CrossRef] [PubMed]
- Fizir, M.; Dramou, P.; Dahiru, N.S.; Ruya, W.; Huang, T.; He, H. Halloysite nanotubes in analytical sciences and in drug delivery: A review. Microchim. Acta 2018, 185, 389. [Google Scholar] [CrossRef] [PubMed]
- Tohidi, S.; Ghaee, A.; Barzin, J. Preparation and characterization of poly (lactic-co-glycolic acid)/chitosan electrospun membrane containing amoxicillin-loaded halloysite nanoclay. Poly. Adv. Techn. 2016, 27, 1020–1028. [Google Scholar] [CrossRef]
- Li, H.; Zhu, X.; Zhou, H.; Zhong, S. Functionalization of halloysite nanotubes by enlargement and hydrophobicity for sustained release of analgesic. Colloids Surf. Physicochem. Eng. Asp. 2015, 487, 154–161. [Google Scholar] [CrossRef]
- Tan, D.; Yuan, P.; Annabi-Bergaya, F.; Yu, H.; Liu, D.; Liu, H.; He, H. Natural halloysite nanotubes as mesoporous carriers for the loading of ibuprofen. Microporous Mesoporous Mater. 2013, 179, 89–98. [Google Scholar] [CrossRef]
- Ganguly, S.; Das, T.K.; Mondal, S.; Das, N.C. Synthesis of polydopamine-coated halloysite nanotube-based hydrogel for controlled release of a calcium channel blocker. RSC Adv. 2016, 6, 105350–105362. [Google Scholar] [CrossRef]
- Shi, Y.-F.; Tian, Z.; Zhang, Y.; Shen, H.-B.; Jia, N.-Q. Functionalized halloysite nanotube-based carrier for intracellular delivery of antisense oligonucleotides. Nanoscale Res. Lett. 2011, 6, 608. [Google Scholar] [CrossRef]
- Santos, A.C.; Ferreira, C.; Veiga, F.; Ribeiro, A.; Panchal, A.; Lvov, Y.; Agarwal, A. Halloysite clay nanotubes for life sciences applications: From drug encapsulation to bioscaffold. Adv. Colloid Interface Sci. 2018, 257, 58–70. [Google Scholar] [CrossRef]
- Bottino, M.C.; Batarseh, G.; Palasuk, J.; Alkatheeri, M.S.; Windsor, L.J.; Platt, J.A. Nanotube-modified dentin adhesive—Physicochemical and dentin bonding characterizations. Dent. Mater. 2013, 29, 1158–1165. [Google Scholar] [CrossRef]
- Chen, Q.; Zhao, Y.; Wu, W.; Xu, T.; Fong, H. Fabrication and evaluation of Bis-GMA/TEGDMA dental resins/composites containing halloysite nanotubes. Dent. Mater. 2012, 28, 1071–1079. [Google Scholar] [CrossRef]
- Feitosa, S.A.; Münchow, E.A.; Al-Zain, A.O.; Kamocki, K.; Platt, J.A.; Bottino, M.C. Synthesis and characterization of novel halloysite-incorporated adhesive resins. J. Dent. 2015, 43, 1316–1322. [Google Scholar] [CrossRef]
- Barot, T.; Rawtani, D.; Kulkarni, P. Physicochemical and biological assessment of silver nanoparticles immobilized halloysite nanotubes-based resin composite for dental applications. Heliyon 2020, 6, e03601. [Google Scholar] [CrossRef] [PubMed]
- Drury, J.L.; Mooney, D.J. Hydrogels for tissue engineering: Scaffold design variables and applications. Biomaterials 2003, 24, 4337–4351. [Google Scholar] [CrossRef]
- Fakhrullin, R.F.; Lvov, Y.M. Halloysite clay nanotubes for tissue engineering. Nanomedicine 2016, 11, 2243–2246. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Han, S.S. Enhanced mechanical, biomineralization, and cellular response of nanocomposite hydrogels by bioactive glass and halloysite nanotubes for bone tissue regeneration. Mater. Sci. Eng. 2021, 128, 112236. [Google Scholar] [CrossRef]
- Sandri, G.; Aguzzi, C.; Rossi, S.; Bonferoni, M.C.; Bruni, G.; Boselli, C.; Cornaglia, A.I.; Riva, F.; Viseras, C.; Caramella, C.; et al. Halloysite and chitosan oligosaccharide nanocomposite for wound healing. Acta Biomater. 2017, 57, 216–224. [Google Scholar] [CrossRef]
- Wang, L.; You, X.; Dai, C.; Tong, T.; Wu, J. Hemostatic nanotechnologies for external and internal hemorrhage management. Biomater. Sci. 2020, 8, 4396–4412. [Google Scholar] [CrossRef]
- Sandri, G.; Faccendini, A.; Longo, M.; Ruggeri, M.; Rossi, S.; Bonferoni, M.C.; Miele, D.; Prina-Mello, A.; Aguzzi, C.; Viseras, C.; et al. Halloysite- and Montmorillonite-Loaded Scaffolds as Enhancers of Chronic Wound Healing. Pharmaceutics 2020, 12, 179. [Google Scholar] [CrossRef]
- Wali, A.; Gorain, M.; Inamdar, S.; Kundu, G.C.; Badiger, M.V. In vivo wound healing performance of halloysite clay and gentamicin-incorporated cellulose ether-PVA electrospun nanofiber mats. ACS Appl. Bio Mater. 2019, 2, 4324–4334. [Google Scholar] [CrossRef]
- Cheng, C.; Gao, Y.; Song, W.; Zhao, Q.; Zhang, H.; Zhang, H. Halloysite nanotube-based H2O2-responsive drug delivery system with a turn on effect on fluorescence for real-time monitoring. Chem. Eng. J. 2020, 380, 122474. [Google Scholar] [CrossRef]
- Lisuzzo, L.; Cavallaro, G.; Parisi, F.; Milioto, S.; Fakhrullin, R.; Lazzara, G. Core/shell gel beads with embedded halloysite nanotubes for controlled drug release. Coatings 2019, 9, 70. [Google Scholar] [CrossRef]
- Akrami-Hasan-Kohal, M.; Ghorbani, M.; Mahmoodzadeh, F.; Nikzad, B. Development of reinforced aldehyde-modified kappa-carrageenan/gelatin film by incorporation of halloysite nanotubes for biomedical applications. Int. J. Biol. Macromol. 2020, 160, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Xie, M.; Huang, K.; Yang, F.; Wang, R.; Han, L.; Yu, H.; Ye, Z.; Wu, F. Chitosan nanocomposite films based on halloysite nanotubes modification for potential biomedical applications. Int. J. Biol. Macromol. 2019, 151, 1116–1125. [Google Scholar] [CrossRef]
- Devi, N.; Dutta, J. Development and in vitro characterization of chitosan/starch/halloysite nanotubes ternary nanocomposite films. Int. J. Biol. Macromol. 2019, 127, 222–231. [Google Scholar] [CrossRef]
- Mohebalia, A.; Abdoussa, M.; Faramarz, A.; Taromib, A. Fabrication of biocompatible antibacterial nanowafers based on HNT/PVA nanocomposites loaded with minocycline for burn wound dressing. Mater. Sci. Eng. 2020, 110, 110685. [Google Scholar] [CrossRef]
- Weisman, J.A.; Jammalamadaka, U.; Tappa, K.; Mills, D.K. Doped Halloysite Nanotubes for Use in the 3D Printing of Medical Devices. Bioengineering 2017, 4, 96. [Google Scholar] [CrossRef] [PubMed]
- Tappa, K.; Jammalamadaka, U.; Weisman, J.A.; Ballard, D.H.; Wolford, D.D.; Pascual-Garrido, C.; Wolford, L.M.; Woodard, P.K.; Mills, D.K. 3D Printing Custom Bioactive and Absorbable Surgical Screws, Pins, and Bone Plates for Localized Drug Delivery. J. Funct. Biomater. 2019, 10, 17. [Google Scholar] [CrossRef]
- Wu, F.; Zheng, J.; Li, Z.; Liu, M. Halloysite nanotubes coated 3D printed PLA pattern for guiding human mesenchymal stem cells (hMSCs) orientation. Chem. Eng. J. 2018, 359, 672–683. [Google Scholar] [CrossRef]
- Arvizo, R.R.; Bhattacharyya, S.; Kudgus, R.A.; Giri, K.; Bhattacharya, R.; Mukherjee, P. Intrinsic therapeutic applications of noble metal nanoparticles: Past, present and future. Chem. Soc. Rev. 2012, 41, 2943–2970. [Google Scholar] [CrossRef]
- Azharuddin, M.; Zhu, G.H.; Das, D.; Ozgur, E.; Uzun, L.; Turner, A.P.F.; Patra, H.K. A repertoire of biomedical applications of noble metal nanoparticles. Chem. Commun. 2019, 55, 6964–6996. [Google Scholar] [CrossRef]
- Massaro, M.; Cavallaro, G.; Colletti, C.G.; Lazzara, G.; Milioto, S.; Noto, R.; Riela, S. Chemical modification of halloysite nanotubes for controlled loading and release. J. Mater. Chem. B 2018, 6, 3415–3433. [Google Scholar] [CrossRef] [PubMed]
- Boyer, C.; Mills, D.K. Method for Preparing Halloysite Supported Metal Nanoparticles through Electrolysis. U.S. Patent US9981074B1, 25 September 2015. [Google Scholar]
- Luo, Y.; Humayun, A.; Mills, D.K. Surface Modification of 3D Printed PLA/Halloysite Composite Scaffolds with Antibacterial and Osteogenic Capabilities. Appl. Sci. 2020, 10, 3971. [Google Scholar] [CrossRef]
- Humayun, A.; Luo, Y.; Mills, D.K. 3D printed antimicrobial PLA constructs functionalized with zinc-coated halloysite nanotubes-Ag-chitosan oligosaccharide lactate. Mater. Technol. 2020, 8, 1–8. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).