Abstract
Southern Thailand suffers from floods due to heavy rainfalls every year. Post-flood increases in indoor fungi are a public health concern. Here, we investigated fungal assemblages on indoor surfaces with visible mold growth in homes after the 2016 flood disaster in Trang Province in Southern Thailand, using swab sampling followed by high-throughput DNA sequencing of the fungal internal transcribed spacer 1 region. The most abundant phyla detected were Ascomycota and Basidiomycota, with respective mean relative abundances of 87% and 13%. The dominant genera and their mean relative abundances were Leptospora (12.0%), Cystobasidium (7.7%), and Pyrenochaetopsis (6.5%). P-tests showed that indoor visible fungal assemblages in flooded homes in Thailand were significantly different from those in the non-flooded mold-laden homes observed in our previous study in South Korea. We detected 20 genera that contain species that can induce type I allergies, including Alternaria (3.8%) and Trichoderma (4.0%). Genera related to infectious, melanized, and toxigenic fungi were also detected. Indoor fungal measurements gathered using a DNA-based approach revealed fungal communities in homes in Thailand and provide important information about the potential health risks. Future research should examine the fungal infections and allergies that might be caused by flood disasters in less well studied tropical countries.
1. Introduction
Thailand is a Southeast Asian country connected to its neighboring countries, namely Myanmar to the west and north, Laos People’s Democratic Republic and Cambodia in the east, and Malaysia to the south. In general, there are four regions classified by topography: the north, central, northeastern, and southern regions. Southern Thailand is quite unique compared to other regions, since the region is a peninsula surrounded by the Andaman Sea on the western side and the South China Sea on the eastern side. This region in located in a tropical zone with heavy rainfall throughout the year. The rainy season in the southern region is different from that in other parts of Thailand; abundant rain occurs during both the northeast and southwest monsoons. The number of rainy days and rainfall (mm) in the southern region are higher than in the upper parts of Thailand. The numbers of rainy days in the south during the 1981–2010 period were 145 and 178 days for the east and west coasts, respectively, whereas the numbers of rainy days in other regions were in the range of 110 to 130 days []. During the monsoon season, this region suffers from floods that detrimentally affect residences and human health due to the increase in pathogenic microbes after the disasters. Indoor biological agents such as bacteria, fungi, viruses, mites, and their toxic substances and metabolites can have adverse human health effects []. Increased concentrations of airborne fungi have been reported in flood-damaged homes [,]. Under flood conditions, the water content in the air becomes high, promoting fungal growth in indoor environments [].
Increased indoor fungal levels in water-damaged homes create risks for human diseases such as respiratory illnesses and allergies [,]. Exposure to indoor fungi can occur via inhalation of airborne fungal spores and/or allergenic substances that can induce immunoglobulin E (IgE)-mediated hypersensitive reactions []. Indoor fungal exposure can impact human health and lead to respiratory infection, irritation, allergy, and asthma [,]. Indoor humidity is another factor that can increase levels of abiotic pollutants such as formaldehyde [,]. Such abiotic pollutants may exacerbate human health issues synergistically with biotic substances, including fungal allergens.
Previous studies have reported indoor airborne fungi in water-damaged homes [,,,,]. For instance, one study reported that levels of fungal spores in flooded homes in New Orleans, USA were significantly higher indoors than outdoors and in non-flooded homes []. A study conducted in Taiwan reported increased concentrations of airborne fungi and altered fungal assemblages after flooding []. In Thailand, post-flood measurements were recorded for indoor concentrations of airborne fungi in a hospital after the 2011 flood disaster [,].
Previous studies have reported indoor airborne fungal concentrations in Thailand [,,]. However, little is known about fungal assemblages on surfaces in homes in Thailand. It is important to characterize the compositions and diversities of indoor visible molds, since they are known to be associated with allergies and respiratory illnesses []. In this study, we report our post-flood measurements of fungal assemblages on indoor surfaces with visible mold growths in homes in Thailand. The results offer benefits for human health in terms of warning systems, intervention, and mitigation measures in post-flood implementation plans.
2. Materials and Methods
2.1. Sample Collection
Indoor surface samples were collected from visible moldy spots in 13 homes in an area of Trang Province in Thailand from 25–27 December 2016 (Figure 1). The sampling was conducted about one month after the flood disaster that began on 2 December 2016. The selected homes had been partially recovered at the time of sampling, for example by cleaning the dirty walls by water washing, eliminating the accumulated mud from the ground floor, and/or installing new furniture. In each home, three to five moldy spots on the walls of rooms on the ground floor in which residents spent most of their time were sampled using sterile cotton swabs wetted with sterile saline. Molds on the sampled surfaces were likely flood-derived since they were not present before the flood event, based on the information provided by the residents. The sampled swabs were temporarily stored at 4 °C for 1 day in Trang Province, and transported at room temperature for 1 h on an airplane and another 2 h on local transportation (from home to the airport and the airport to laboratory) to the laboratory in Bangkok at Mahidol University in Thailand, where they were maintained at −20 °C.
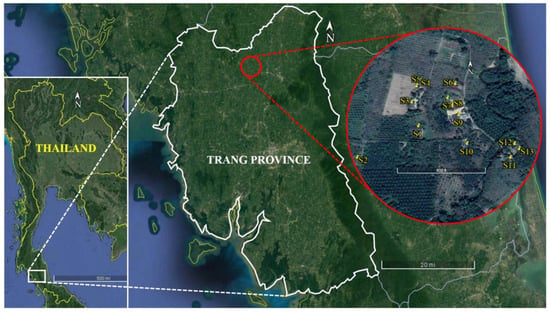
Figure 1.
Locations of the homes sampled in an area of Trang Province in Thailand.
2.2. DNA Extraction
The samples were analyzed at Seoul National University in South Korea. The DNA extraction method used was described previously []. Briefly, each swab sample was cut using sterilized scissors, enclosed in a 2 mL tube provided with the PowerMax® Soil DNA Isolation kit (Mobio Laboratory, Carlsbad, CA, USA), and homogenized with supplemental 0.1 mm diameter glass beads (300 mg) and 0.5 mm diameter glass bead, (100 mg) [] for 3 min using a bead beater (BioSpec Products, Bartlesville, OK, USA). DNA was purified according to the manufacturer’s protocol and eluted in 50 μL TE (10 mM Tris-HCl, 1 mM EDTA, pH = 8.0). The eluted DNA was stored at −80 °C.
2.3. DNA Sequencing
The internal transcribed spacer 1 (ITS1) region [] was amplified using universal fungal primers ITS1F and ITS2 [,] attached with the adapter sequences for Illumina MiSeq (Illumina, Inc., San Diego, CA, USA). Each polymerase chain reaction (PCR) mixture (30 μL) contained 1 µL DNA template, 0.33 µM of each primer, 2× PCR Solution Premix TaqTM DNA polymerase (Takara Bio Inc., Otsu, Shiga, Japan), and ultrapure water. The thermal conditions were: 5 min at 95 °C for initial denaturation, followed by 35 cycles of 30 s at 95 °C for denaturation, 30 s at 55 °C for annealing, and 30 s at 72 °C for extension. The final elongation was conducted for 10 min at 72 °C. AMPure XP beads (Beckman Coulter, Inc., Brea, CA, USA) were used to remove remaining primers and primer dimers. Index PCR was performed with the purified PCR products and a Nextera XT Index kit (Illumina). Each reaction mixture contained 5 µL of the purified PCR amplicons, 5 µL of the index primer pair, 25 µL of 2× PCR Solution Premix TaqTM DNA polymerase (Takara), and 15 µL of ultrapure water. The thermal conditions were: 3 min at 95 °C for initial denaturation, followed by 10 cycles of 30 s at 95 °C for denaturation, 30 s at 55 °C for annealing, and 30 s at 72 °C for extension. The final elongation was conducted for 5 min at 72 °C. The indexed PCR products were purified using the AMPure XP beads (Beckman, Pasadena, CA, USA), normalized to 4 nM with 10 mM Tris-HCL (pH = 8.5) and pooled with an internal control PhiX (30%). The pooled, heat-denatured amplicons were loaded onto the v3 600 cycle kit reagent cartridge (Illumina, San Diego, CA, USA). Illumina MiSeq was used for 2 × 300 bp paired-end sequencing. The raw sequencing data were uploaded to the Sequence Read Archive of the NCBI under the accession number PRJNA513204.
2.4. Sequence Procsesing and Analyses
An Illumina MiSeq Reporter v2.5 was used to remove the sequence reads with quality scores below 20. Trimmomatic-0.36 [] was used to trim poly(N) tails. Each of the resultant paired-end reads was concatenated by QIIME 1.8.0 [], from which the chimeric sequence was excluded using the “chimera.vsearch” command [] in mothur v.1.39.5 [] against the database “uchime_reference_dataset_ITS1_28.06.2017.fasta” []. Reads shorter than 100 bp were removed on the Galaxy web platform []. From a total of 13 libraries, 436,925 sequences were obtained, with the number of the reads ranging from 1342 to 51,987 per library. The mean read length of each library ranged from 259 to 309 bp. The sequences were taxonomically assigned by BLASTN2.2.28+ [] against the UNITE database “UNITEdatabaseinFHiTINGSformat20-11-2016release.fasta” with FHiTHINGS version 1.4 []. To check for potential database biases, the sequences were also searched against the fungal ITS RefSeq database (PRJNA177353) [], downloaded on 13 March 2019.
For the diversity analyses, 1000 sequences were sampled from each library using mothur v.1.39.5 []. The sampled sequences were assembled into operational taxonomic units (OTUs) at a 97% sequence similarity. For the β-diversity analysis, we compared the fungal assemblages with those obtained during our previous study in South Korea []. The results were comparable since the methods used were identical, i.e., the same sampling, analytical, and sequence-processing methods with the same primers, ITS1F and ITS2, were used across these two studies. From each of the Thai and Korean libraries, 1000 sequences were sampled, assembled into 97% OTUs, and mapped onto the same OTU table. The Jaccard indices and Yue and Clayton theta similarity coefficients were calculated to compare fungal assemblage memberships and structures, respectively. P-tests were performed to analyze statistical differences in fungal assemblages between Thailand and South Korea. For the α-diversity analysis, singleton OTUs were removed by the “remove.rare” command, and the observed richness, Chao1 estimators, Shannon indices, and Simpson indices were calculated using mothur v.1.39.5 [].
3. Results
3.1. Fungal Diversity
Table 1 shows the α-diversity measures of fungal assemblages in indoor visible molds in homes in southern Thailand, with the observed richness ranging from 3 to 20, Chao1 estimators ranging from 3 to 20, Shannon indices ranging from 0.02 to 1.67, and Simpson indices ranging from 0.25 to 0.99. Figure 2 shows the principal coordinate analysis plots used to compare the fungal assemblages sampled in this study with those obtained by our previous study in South Korea []. P-tests showed significant differences in the fungal assemblage memberships (p < 0.001) and structures (p = 0.0005) between the two countries.

Table 1.
α-Diversity measures of fungal assemblages sampled from indoor surfaces with visible mold growths in homes in southern Thailand 1.
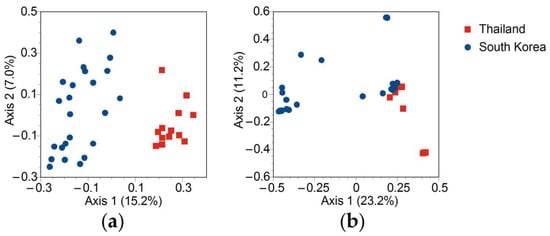
Figure 2.
Principal coordinate analysis plots based on the fungal internal transcribed spacer 1 (ITS1) operational taxonomic units (OTUs) at a 97% sequence similarity. The results of this study (Thailand) were compared with the results of An and Yamamoto’s South Korean study []. (a) Fungal assemblage memberships in terms of Jaccard similarity coefficients and (b) fungal assemblage structures in terms of Yue and Clayton theta (θ) similarity coefficients.
3.2. Fungal Assemblages
Ascomycota and Basidiomycota were the predominant phyla detected from the studied homes, with respective mean relative abundances of 87% and 13% (Figure 3). Ascomycota were detected in all 13 sampled homes, whereas Basidiomycota were detected in 11 homes. The relative abundance of Basidiomycota in Sample 8 was high because a distinctively high relative abundance of Cystobasidium, a basidiomycete yeast closely related to Rhodotorula, was observed in Sample 8. Zygomycota and Glomeromycota were detected with low abundances, i.e., less than 0.01% of all sequences. At the class level, Dothideomycetes was the most abundant (47.5%), followed by Sordariomycetes (32.5%), Cystobasidiomycetes (7.7%), and Saccharomycetes (4.5%) (Figure 4).
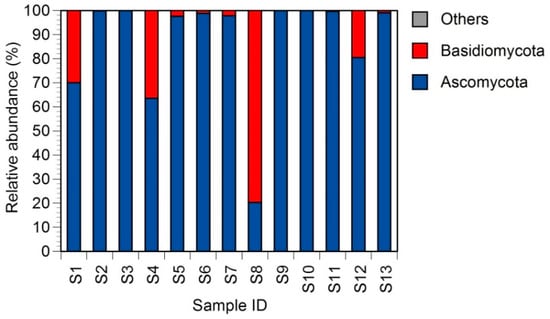
Figure 3.
Fungal compositions at the phylum level. The “others” category includes ambiguous sequences.
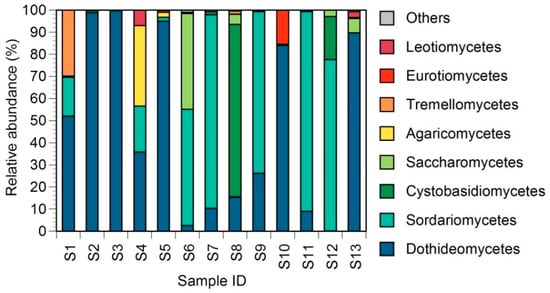
Figure 4.
Fungal compositions at the class level. The “others” category includes ambiguous sequences.
3.3. Predominant Fungal Genera
At the genus level, a total of 75 genera were detected with more than 10 sequences from all samples combined. The proportions of the 50 most abundant fungal genera are shown in Figure 5. The predominant genera detected against both the UNITE and RefSeq databases were Leptospora (12.0%), Cystobasidium (7.7%), Pyrenochaetopsis (6.5%), Trichoderma (4.0%), Alternaria (3.8%), and Neodevriesia (2.9%). Except for Wickerhamomyces (2.5%), these results were reproducible regardless of the selection of the reference databases (Figure 6). Lower relative abundances were observed for fungal genera commonly found in homes in temperate countries, e.g., Aspergillus (0.053%), Candida (0.53%), Cladosporium (0.055%), Epicoccum (0.020%), Fusarium (0.13%), Penicillium (0.77%), Rhodotorula (0.14%), and Stachybotrys (0.74%).
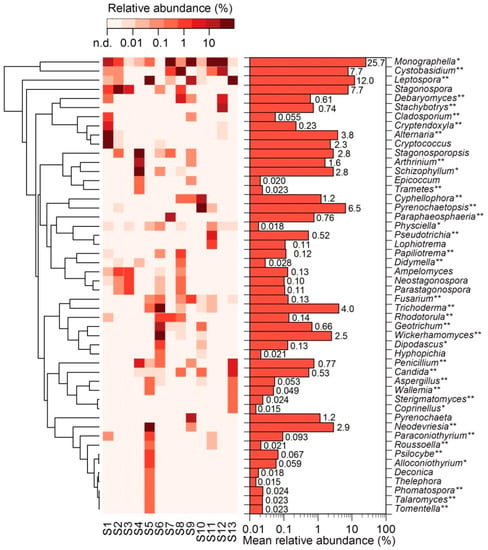
Figure 5.
Relative abundances at the genus level. The 50 most abundant genera are shown. The tree represents between-genus similarity of log-transformed relative abundances based on Euclidean distance. Double asterisks (**) indicate genera detected against both the UNITE and RefSeq databases. Single asterisks (*) indicate genera detected only against the UNITE database that were absent in the RefSeq database. The genera without asterisks are those detected only against the UNITE database, even though they were present in the RefSeq database. n.d.: not detected.
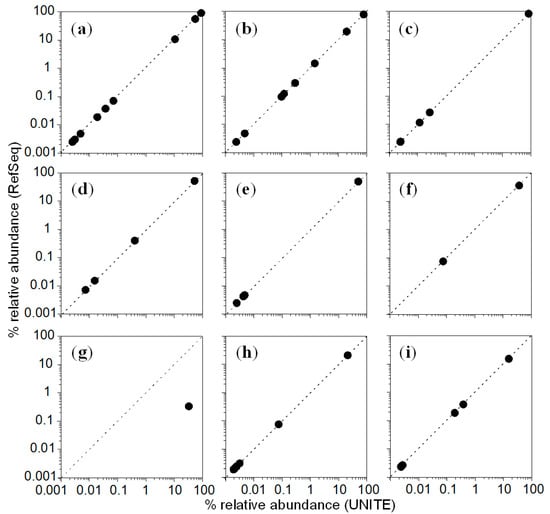
Figure 6.
Relative abundances of the nine most abundant genera detected against both the UNITE and RefSeq databases. (a) Leptospora, (b) Cystobasidium, (c) Pyrenochaetopsis, (d) Trichoderma, (e) Alternaria, (f) Neodevriesia, (g) Wickerhamomyces, (h) Arthrinium, and (i) Cyphellophora. Dashed lines indicate 1:1 ratios.
4. Discussion
Indoor dampness and visible mold growth are known to be linked to allergies and respiratory illnesses []. However, knowledge is limited regarding these molds’ compositions and diversities, especially in tropical countries such as Thailand. In this study, we aimed to characterize fungal assemblages on indoor surfaces with visible mold growths in homes in Thailand. We compared the results of this Thai study with those of our previous study in South Korea []. It is important to understand the possible geographical differences, since dampness problems differ between countries with different climate characteristics and building structures []. There are four categories of sources of dampness in buildings: outdoor, indoor, building sources, and accidents []. The sources might be different in each country. For instance, indoor dew condensation due to cold outdoor temperatures might be a major source of dampness in winter heating seasons in South Korea (indoor source) [], whereas floods might be an important source of dampness in monsoon seasons in southern Thailand (outdoor source).
To date, several studies have reported airborne fungi in flood-damaged homes [,,,]. In Thailand, previous studies reported post-flood measurements of concentrations of airborne fungi in a hospital after the 2011 flood disaster [,]. It is similarly important to conduct post-flood measurements of fungal communities on surfaces, since airborne fungi originate from indoor surfaces laden with mold growths []. In this study, we analyzed fungal assemblages on indoor surfaces laden with visible mold growths in homes after the 2016 flood disaster in the historically neglected southern part of Thailand. The sampling site is situated in a tropical zone that experiences heavy rainfalls every year. Flood disasters are known to be followed by human health problems []. In this study, we analyzed fungal communities, including the genera related to human allergens and infectious pathogens, using high-throughput DNA sequencing. The Institute of Medicine indicated the association of indoor dampness and molds with upper respiratory tract symptoms such as coughing, wheezing, asthma, and hypersensitivity pneumonitis in susceptible individuals []. Thus, the indoor molds observed in this study might present a risk for such symptoms in residents in flood-damaged homes in the southern rural parts of Thailand.
Our previous study conducted in South Korea showed that Cladosporium was the most abundant genus, with a mean relative abundance of 41%, on indoor surfaces with visible molds []. Our present study in Thailand showed that Cladosporium was not abundant, with a mean relative abundance of 0.055%, on surfaces with visible molds in flood-damaged homes (Figure 5). P-tests showed significant differences in the fungal assemblage memberships (p < 0.001) and structures (p = 0.0005) between the two countries (Figure 2). These results suggest that indoor visible fungal communities are different between the two countries. Various factors can affect indoor visible fungal communities, which might include building structure as well as regional climate and mycofloral characteristics. Additionally, the communities might be affected by the different sources of dampness (i.e., flood vs. dew condensation). We do not know the causes of the difference in fungal assemblages on indoor visible molds observed between our two different studies. Nonetheless, our observations indicate possible geographical differences in the taxonomic structures of indoor visible molds. We also observed commonalities between the two countries. For instance, we found that the Shannon indices observed in this study, ranging from 0.02 to 1.67, were similarly low to those observed in South Korea, ranging from 0.14 to 2.29 []. This suggests that each moldy spot includes a small number of fungal species, regardless of geographical differences.
In addition to our previous study conducted in South Korea [], several similar high-throughput DNA-sequencing-based studies have analyzed fungal communities on indoor surfaces using swab sampling followed by high-throughput sequencing [,,]. Fouquier et al. [] analyzed fungal communities on public restroom floors in California in the U.S. and reported that Cladosporium, Saccharomyces, and Alternaria were the three most abundant genera. Hegarty et al. [] analyzed fungal communities in visible molds in a damp building in Connecticut in the U.S. and found Sterigmatomyces, Stachybotrys, and Aspergillus to be the dominant genera. Fu et al. [] analyzed fungal communities on doorframes in rooms of hotels in 19 countries in Europe and Asia, and reported that the abundances of Aspergillus were higher in the countries with low altitudes, including Thailand. The tendency was opposite to the findings of our studies, but the difference was small, i.e., 0.053% in Thailand vs. 0.094% in South Korea.
Exposure to indoor fungi can cause respiratory illnesses such as infection and allergies [,,,]. For instance, indoor mold exposure and dampness are known to reduce lung function among nonasthmatic adults and are related to asthma development and aggravation in children, whereas asthma in adults can be aggravated by indoor dampness and mold exposure [,]. Toxigenic fungi, such as Stachybotrys chartarum, in water-damaged buildings are associated with respiratory illnesses [,]. Thus, one of the aims of this study was to investigate potential fungal pathogens and allergens that might cause such respiratory illnesses in residents of flood-damaged homes. To date, about 80 fungal genera have been identified to cause type I allergies [], and we found several genera that contain such allergenic species, e.g., Trichoderma (4.0%) and Alternaria (3.8%) (Figure 5). Tricoderma also contains human pathogens such as Tricoderma harzianum, Tricoderma lixii, and Tricoderma longibrachiatum [,]. We identified several genera that contain opportunistic infectious pathogens, e.g., Aspergillus (0.053%), Candida (0.53%), Fusarium (0.13%), and Penicillium (0.77%). Melanized fungi, which are thought to cause infection in humans [,], were also detected, with examples including Cladosporium (0.055%), and Cyphellophora (1.2%). Genera associated with toxigenic species [,] were also detected. These genera included Stachybotrys (0.74%), Fusarium (0.13%), and Trichoderma (4.0%).
Yeasts and yeast-like fungi were also detected in the flood-damaged homes in Thailand. Examples include Rhodotorula, which is a saprophytic yeast that can be isolated from both environment and clinical specimens. Rhodotorula contains opportunistic human pathogenic species such as Rhodotorula mucilaginosa [,]. Another yeast genus detected was Candida, which includes pathogenic species that can cause candidiasis and candidemia [,]. Cyphellophora, which is a black yeast-like fungal genus, was detected with a mean relative abundance of 1.2% (Figure 5). This melanized genus includes human pathogenic species such as Cyphellophora europaea, and is isolated from black biofilms in wet indoor environments such as kitchens and bathrooms [,,].
5. Conclusions
To date, several studies have reported airborne fungi in indoor environments in Thailand [,,]. However, few have evaluated the diversity of these fungi. Most of these studies were based on growth-dependent techniques that are unable to detect nonculturable species that are potentially clinically important. To the best of our best knowledge, this was the first study to use a growth-independent high-throughput DNA-sequencing technique to analyze fungal communities in indoor visible molds in Thailand. Indoor fungal manifestations after flood disasters are a critical public health concern in tropical countries. This study demonstrated the geographical differences in fungal communities in indoor visible mold growths between temperate and tropical countries. This might result in potential geographical differences in the types of illnesses in residents. We also detected genera related to human allergens and pathogens in the flood-damaged homes in Thailand. The findings of this study are important since they provide insights into how flood-induced fungal communities affect the health of residents. Future research should further scrutinize disease-causing fungal species and strains, for example, by combining sequencing with growth-dependent methods to elucidate the relationships between indoor fungi and health in residents in homes damaged by flood disasters.
Author Contributions
Conceptualization, N.Y. and K.T.; methodology, K.T. and C.W.; formal analysis, N.P. and C.W.; investigation, W.K.; resources, N.Y. and K.T.; writing—original draft preparation, N.P. and C.W.; writing—review and editing, N.Y. and K.T.; visualization, N.P. and N.Y.; supervision, N.Y. and K.T.; project administration, N.Y. and K.T.; funding acquisition, N.Y. and K.T. All authors have read and agreed to the published version of the manuscript.
Funding
This work was partially supported by the Aspiring Researcher Program through Seoul National University (SNU) in 2014.
Acknowledgments
The authors would like to thank the house owners to their kindness for supporting our samplings, the Center for Health Impact Assessment Study (CHIAS), the Department of Social and Environmental Medicine, Faculty of Tropical Medicine, Mahidol University for providing our materials and sampling equipment.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Meteorological Department. The Climate of Thailand. Available online: https://www.tmd.go.th/en/archive/thailand_climate.pdf (accessed on 20 July 2020).
- Becher, R.; Hongslo, J.K. Biological pollution of indoor air. Tidsskr Nor Laegeforen 1994, 114, 2722–2724. [Google Scholar] [PubMed]
- Rao, C.Y.; Riggs, M.A.; Chew, G.L.; Muilenberg, M.L.; Thorne, P.S.; Van Sickle, D.; Dunn, K.H.; Brown, C. Characterization of airborne molds, endotoxins, and glucans in homes in New Orleans after Hurricanes Katrina and Rita. Appl. Environ. Microbiol. 2007, 73, 1630–1634. [Google Scholar] [CrossRef] [PubMed]
- Hsu, N.Y.; Chen, P.Y.; Chang, H.W.; Su, H.J. Changes in profiles of airborne fungi in flooded homes in southern Taiwan after Typhoon Morakot. Sci. Total Environ. 2011, 409, 1677–1682. [Google Scholar] [CrossRef]
- Azuma, K.; Ikeda, K.; Kagi, N.; Yanagi, U.; Hasegawa, K.; Osawa, H. Effects of water-damaged homes after flooding: Health status of the residents and the environmental risk factors. Int. J. Environ. Health Res. 2014, 24, 158–175. [Google Scholar] [CrossRef] [PubMed]
- Emerson, J.B.; Keady, P.B.; Brewer, T.E.; Clements, N.; Morgan, E.E.; Awerbuch, J.; Miller, S.L.; Fierer, N. Impacts of flood damage on airborne bacteria and fungi in homes after the 2013 Colorado Front Range flood. Environ. Sci. Technol. 2015, 49, 2675–2684. [Google Scholar] [CrossRef] [PubMed]
- Beezhold, D.H.; Green, B.J.; Blachere, F.M.; Schmechel, D.; Weissman, D.N.; Velickoff, D.; Hogan, M.B.; Wilson, N.W. Prevalence of allergic sensitization to indoor fungi in West Virginia. Allergy Asthma Proc. 2008, 29, 29–34. [Google Scholar] [CrossRef]
- Rogers, C.A. Indoor fungal exposure. Immunol. Allergy Clin. N. Am. 2003, 23, 501–518. [Google Scholar] [CrossRef]
- Mi, Y.H.; Norback, D.; Tao, J.; Mi, Y.L.; Ferm, M. Current asthma and respiratory symptoms among pupils in Shanghai, China: Influence of building ventilation, nitrogen dioxide, ozone, and formaldehyde in classrooms. Indoor Air 2006, 16, 454–464. [Google Scholar] [CrossRef]
- Arundel, A.V.; Sterling, E.M.; Biggin, J.H.; Sterling, T.D. Indirect health effects of relative humidity in indoor environments. Environ. Health Perspect. 1986, 65, 351–361. [Google Scholar] [CrossRef]
- Baughman, A.V.; Arens, E.A. Indoor humidity and human health-Part I: Literature review of health effects of humidity-influenced indoor pollutants. ASHRAE Trans. 1996, 102, 193–211. [Google Scholar]
- Solomon, G.M.; Hjelmroos-Koski, M.; Rotkin-Ellman, M.; Hammond, S.K. Airborne mold and endotoxin concentrations in New Orleans, Louisiana, after flooding, October through November 2005. Environ. Health Perspect. 2006, 114, 1381–1386. [Google Scholar] [CrossRef] [PubMed]
- Apisarnthanarak, A.; Khawcharoenporn, T.; Mundy, L.M. Black-water floods and hospital-based postflood mold investigations. Infect. Control Hosp. Epidemiol. 2012, 33, 1266–1268. [Google Scholar] [CrossRef] [PubMed]
- Khawcharoenporn, T.; Apisarnthanarak, A.; Thongphubeth, K.; Yuekyen, C.; Damnin, S.; Hayden, M.K.; Weinstein, R.A. Post-flood measurement of fungal bio-aerosol in a resource-limited hospital: Can the settle plate method be used? J. Hosp. Infect. 2013, 83, 150–152. [Google Scholar] [CrossRef] [PubMed]
- Luksamijarulkul, P.; Ratthanakhot, Y.; Vatanasomboon, P. Microbial counts and particulate matter levels in indoor air samples collected from a child home-care center in Bangkok, Thailand. J. Med. Assoc. Thai. 2012, 95 (Suppl. 6), S161-8. [Google Scholar]
- Siwarom, S.; Puranitee, P.; Plitponkarnpim, A.; Manuyakorn, W.; Sinitkul, R.; Arj-Ong Vallipakorn, S. Association of indoor air quality and preschool children’s respiratory symptoms. Asian Pac. J. Allergy Immunol. 2017, 35, 119–126. [Google Scholar] [CrossRef]
- Mendell, M.J.; Mirer, A.G.; Cheung, K.; Tong, M.; Douwes, J. Respiratory and allergic health effects of dampness, mold, and dampness-related agents: A review of the epidemiologic evidence. Environ. Health Perspect. 2011, 119, 748–756. [Google Scholar] [CrossRef]
- An, C.; Yamamoto, N. Fungal compositions and diversities on indoor surfaces with visible mold growths in residential buildings in the Seoul Capital Area of South Korea. Indoor Air 2016, 26, 714–723. [Google Scholar] [CrossRef]
- Hospodsky, D.; Yamamoto, N.; Peccia, J. Accuracy, precision, and method detection limits of quantitative PCR for airborne bacteria and fungi. Appl. Environ. Microbiol. 2010, 76, 7004–7012. [Google Scholar] [CrossRef]
- Schoch, C.L.; Seifert, K.A.; Huhndorf, S.; Robert, V.; Spouge, J.L.; Levesque, C.A.; Chen, W. Nuclear ribosomal internal transcribed spacer (ITS) region as a universal DNA barcode marker for Fungi. Proc. Natl. Acad. Sci. USA 2012, 109, 6241–6246. [Google Scholar] [CrossRef]
- White, T.J.; Bruns, T.; Lee, S.; Taylor, J.W. Amplification and direct sequencing of fungal ribosomal RNA genes for phylogenetics. In PCR Protocols: A Guide to Methods and Applications; Innis, M.A., Gelfand, D.H., Sninsky, J.J., White, T.J., Eds.; Academic Press: New York, NY, USA, 1990; pp. 315–322. [Google Scholar]
- Gardes, M.; Bruns, T.D. ITS primers with enhanced specificity for Basidiomycetes: Application to the identification of mycorrhizae and rusts. Mol. Ecol. Notes 1993, 2, 113–118. [Google Scholar] [CrossRef]
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef] [PubMed]
- Caporaso, J.G.; Kuczynski, J.; Stombaugh, J.; Bittinger, K.; Bushman, F.D.; Costello, E.K.; Fierer, N.; Pena, A.G.; Goodrich, J.K.; Gordon, J.I.; et al. QIIME allows analysis of high-throughput community sequencing data. Nat. Methods 2010, 7, 335–336. [Google Scholar] [CrossRef] [PubMed]
- Rognes, T.; Flouri, T.; Nichols, B.; Quince, C.; Mahé, F. VSEARCH: A versatile open source tool for metagenomics. PeerJ 2016, 4, e2584. [Google Scholar] [CrossRef] [PubMed]
- Schloss, P.D.; Westcott, S.L.; Ryabin, T.; Hall, J.R.; Hartmann, M.; Hollister, E.B.; Lesniewski, R.A.; Oakley, B.B.; Parks, D.H.; Robinson, C.J.; et al. Introducing mothur: Open-source, platform-independent, community-supported software for describing and comparing microbial communities. Appl. Environ. Microbiol. 2009, 75, 7537–7541. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, R.H.; Tedersoo, L.; Ryberg, M.; Kristiansson, E.; Hartmann, M.; Unterseher, M.; Porter, T.M.; Bengtsson-Palme, J.; Walker, D.M.; de Sousa, F.; et al. A comprehensive, automatically updated fungal ITS sequence dataset for reference-based chimera control in environmental sequencing efforts. Microbes Environ. 2015, 30, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Afgan, E.; Baker, D.; van den Beek, M.; Blankenberg, D.; Bouvier, D.; Čech, M.; Chilton, J.; Clements, D.; Coraor, N.; Eberhard, C.; et al. The Galaxy platform for accessible, reproducible and collaborative biomedical analyses: 2016 update. Nucleic Acids Res. 2016, 44, W3–W10. [Google Scholar] [CrossRef] [PubMed]
- Altschul, S.F.; Gish, W.; Miller, W.; Myers, E.W.; Lipman, D.J. Basic local alignment search tool. J. Mol. Biol. 1990, 215, 403–410. [Google Scholar] [CrossRef]
- Dannemiller, K.; Reeves, D.; Bibby, K.; Yamamoto, N.; Peccia, J. Fungal high-throughput taxonomic identification tool for use with next-generation sequencing (FHiTINGS). J. Basic Microbiol. 2014, 54, 315–321. [Google Scholar] [CrossRef]
- Schoch, C.; Robbertse, B.; Robert, V.; Vu, T.; Cardinali, G.; Irinyi, L.; Meyer, W.; Nilsson, R.H.; Hughes, K.; Miller, A.N.; et al. Finding needles in haystacks: Linking scientific names, reference specimens and molecular data for Fungi. Database 2014, 1–21. [Google Scholar] [CrossRef]
- Bornehag, C.G.; Blomquist, G.; Gyntelberg, F.; Järvholm, B.; Malmberg, P.; Nordvall, L.; Nielsen, A.; Pershagen, G.; Sundell, J. Dampness in buildings and health. Nordic interdisciplinary review of the scientific evidence on associations between exposure to “dampness” in buildings and health effects (NORDDAMP). Indoor Air 2001, 11, 72–86. [Google Scholar] [CrossRef]
- DeLeon-Rodriguez, N.; Lathem, T.L.; Rodriguez, R.L.; Barazesh, J.M.; Anderson, B.E.; Beyersdorf, A.J.; Ziemba, L.D.; Bergin, M.; Nenes, A.; Konstantinidis, K.T. Microbiome of the upper troposphere: Species composition and prevalence, effects of tropical storms, and atmospheric implications. Proc. Natl. Acad. Sci. USA 2013, 110, 2575–2580. [Google Scholar] [CrossRef] [PubMed]
- Du, W.; FitzGerald, G.J.; Clark, M.; Hou, X.Y. Health impacts of floods. Prehosp. Disaster Med. 2010, 25, 265–272. [Google Scholar] [CrossRef]
- IOM. Damp Indoor Spaces and Health; National Academy Press: Washington, DC, USA, 2005. [Google Scholar]
- Fouquier, J.; Schwartz, T.; Kelley, S.T. Rapid assemblage of diverse environmental fungal communities on public restroom floors. Indoor Air 2016, 26, 869–879. [Google Scholar] [CrossRef]
- Hegarty, B.; Haverinen-Shaughnessy, U.; Shaughnessy, R.J.; Peccia, J. Spatial gradients of fungal abundance and ecology throughout a damp building. Environ. Sci. Technol. Lett. 2019, 6, 329–333. [Google Scholar] [CrossRef]
- Fu, X.; Li, Y.; Yuan, Q.; Cai, G.-h.; Deng, Y.; Zhang, X.; Norbäck, D.; Sun, Y. Continental-scale microbiome study reveals different environmental characteristics determining microbial richness, composition, and quantity in hotel rooms. mSystems 2020, 5, e00119-20. [Google Scholar] [CrossRef]
- Hamilos, D.L. Allergic fungal rhinitis and rhinosinusitis. Proc. Am. Thorac. Soc. 2010, 7, 245–252. [Google Scholar] [CrossRef]
- Portnoy, J.M.; Kwak, K.; Dowling, P.; VanOsdol, T.; Barnes, C. Health effects of indoor fungi. Ann. Allergy Asthma Immunol. 2005, 94, 313–319. [Google Scholar] [CrossRef]
- Brown, G.D.; Denning, D.W.; Levitz, S.M. Tackling human fungal infections. Science 2012, 336, 647. [Google Scholar] [CrossRef]
- Badiee, P.; Hashemizadeh, Z. Opportunistic invasive fungal infections: Diagnosis & clinical management. Indian J. Med. Res. 2014, 139, 195–204. [Google Scholar]
- Caillaud, D.; Leynaert, B.; Keirsbulck, M.; Nadif, R.; mould_ANSES_working_group. Indoor mould exposure, asthma and rhinitis: Findings from systematic reviews and recent longitudinal studies. Eur. Respir. Rev. 2018, 27, 170137. [Google Scholar] [CrossRef]
- Hernberg, S.; Sripaiboonkij, P.; Quansah, R.; Jaakkola, J.J.; Jaakkola, M.S. Indoor molds and lung function in healthy adults. Respir. Med. 2014, 108, 677–684. [Google Scholar] [CrossRef]
- Hodgson, M.J.; Morey, P.; Leung, W.Y.; Morrow, L.; Miller, D.; Jarvis, B.B.; Robbins, H.; Halsey, J.F.; Storey, E. Building-associated pulmonary disease from exposure to Stachybotrys chartarum and Aspergillus versicolor. J. Occup. Environ. Med. 1998, 40, 241–249. [Google Scholar] [CrossRef]
- Johanning, E.; Biagini, R.; Hull, D.; Morey, P.; Jarvis, B.; Landsbergis, P. Health and immunology study following exposure to toxigenic fungi (Stachybotrys chartarum) in a water-damaged office environment. Int. Arch. Occup. Environ. Health 1996, 68, 207–218. [Google Scholar] [CrossRef]
- Simon-Nobbe, B.; Denk, U.; Poll, V.; Rid, R.; Breitenbach, M. The spectrum of fungal allergy. Int. Arch. Allergy Immunol. 2008, 145, 58–86. [Google Scholar] [CrossRef]
- Molnár-Gábor, E.; Dóczi, I.; Hatvani, L.; Vágvölgyi, C.; Kredics, L. Isolated sinusitis sphenoidalis caused by Trichoderma longibrachiatum in an immunocompetent patient with headache. J. Med. Microbiol. 2013, 62, 1249–1252. [Google Scholar] [CrossRef]
- Sandoval-Denis, M.; Sutton, D.A.; Cano-Lira, J.F.; Gene, J.; Fothergill, A.W.; Wiederhold, N.P.; Guarro, J. Phylogeny of the clinically relevant species of the emerging fungus Trichoderma and their antifungal susceptibilities. J. Clin. Microbiol. 2014, 52, 2112–2125. [Google Scholar] [CrossRef]
- Chowdhary, A.; Perfect, J.; de Hoog, G.S. Black molds and melanized yeasts pathogenic to humans. Cold Spring Harb. Perspect. Med. 2015, 5, a019570. [Google Scholar] [CrossRef]
- Revankar, S.G.; Sutton, D.A. Melanized fungi in human disease. Clin. Microbiol. Rev. 2010, 23, 884–928. [Google Scholar] [CrossRef]
- Edite Bezerra da Rocha, M.; Freire, F.d.C.O.; Erlan Feitosa Maia, F.; Izabel Florindo Guedes, M.; Rondina, D. Mycotoxins and their effects on human and animal health. Food Control 2014, 36, 159–165. [Google Scholar] [CrossRef]
- Hossain, M.A.; Ahmed, M.S.; Ghannoum, M.A. Attributes of Stachybotrys chartarum and its association with human disease. J. Allergy Clin. Immunol. 2004, 113, 200–208. [Google Scholar] [CrossRef]
- De Almeida, G.M.; Costa, S.F.; Melhem, M.; Motta, A.L.; Szeszs, M.W.; Miyashita, F.; Pierrotti, L.C.; Rossi, F.; Burattini, M.N. Rhodotorula spp. isolated from blood cultures: Clinical and microbiological aspects. Med. Mycol. 2008, 46, 547–556. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wirth, F.; Goldani, L.Z. Epidemiology of Rhodotorula: An emerging pathogen. Interdiscip. Perspect. Infect. Dis. 2012, 2012, 465717. [Google Scholar] [CrossRef] [PubMed]
- Pfaller, M.A.; Diekema, D.J.; Gibbs, D.L.; Newell, V.A.; Ellis, D.; Tullio, V.; Rodloff, A.; Fu, W.; Ling, T.A.; Global Antifungal Surveillance, G. Results from the ARTEMIS DISK Global Antifungal Surveillance Study, 1997 to 2007: A 10.5-year analysis of susceptibilities of Candida species to fluconazole and voriconazole as determined by CLSI standardized disk diffusion. J. Clin. Microbiol. 2010, 48, 1366–1377. [Google Scholar] [CrossRef] [PubMed]
- Canton, E.; Peman, J.; Quindos, G.; Eraso, E.; Miranda-Zapico, I.; Alvarez, M.; Merino, P.; Campos-Herrero, I.; Marco, F.; de la Pedrosa, E.G.; et al. Prospective multicenter study of the epidemiology, molecular identification, and antifungal susceptibility of Candida parapsilosis, Candida orthopsilosis, and Candida metapsilosis isolated from patients with candidemia. Antimicrob. Agents Chemother. 2011, 55, 5590–5596. [Google Scholar] [CrossRef][Green Version]
- De Hoog, S.; Mayser, P.; Haase, G.; Horré, R.; Horrevorts, A. A new species, Phialophora europaea, causing superficial infections in humans. Mycoses 2000, 43, 409–416. [Google Scholar] [CrossRef]
- Saunte, D.M.; Tarazooie, B.; Arendrup, M.C.; de Hoog, G.S. Black yeast-like fungi in skin and nail: It probably matters. Mycoses 2012, 55, 161–167. [Google Scholar] [CrossRef]
- Wang, X.; Cai, W.; Gerrits van den Ende, B.; Zhang, J.; Xie, T.; Xi, L.; Li, X.; Sun, J.; de Hoog, S. Indoor wet cells as a habitat for melanized fungi, opportunistic pathogens on humans and other vertebrates. Sci. Rep. 2018, 8, 7685. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).