Caring for Dementia Caregivers: Psychosocial Factors Related to Engagement in Self-Care Activities
Abstract
:1. Introduction
1.1. Dementia Caregivers and Health
1.2. Self-Care
1.3. Caregiving Involvement and Self-Care
1.4. Social Support, Self-Care, and Caregiving Outcome
1.5. The Current Study
1.6. Hypotheses
2. Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.3.1. Background Characteristics
2.3.2. Self-Care Activity
Physical Health Check-Up
Restorative Activity
Sleep
2.3.3. Caregiver Involvement
ADL/IADL Support
Use of Formal Care and Services
Preparedness
Care Recipient’s Physical Symptoms
Care Recipient’s Psychological Symptoms
2.3.4. Social Support
Received Support
Social Interaction
Satisfaction with Support
2.3.5. Caregiver Outcomes
Caregiver Burden
Positive Aspects of Caregiving
Depression
2.4. Analyses
3. Results
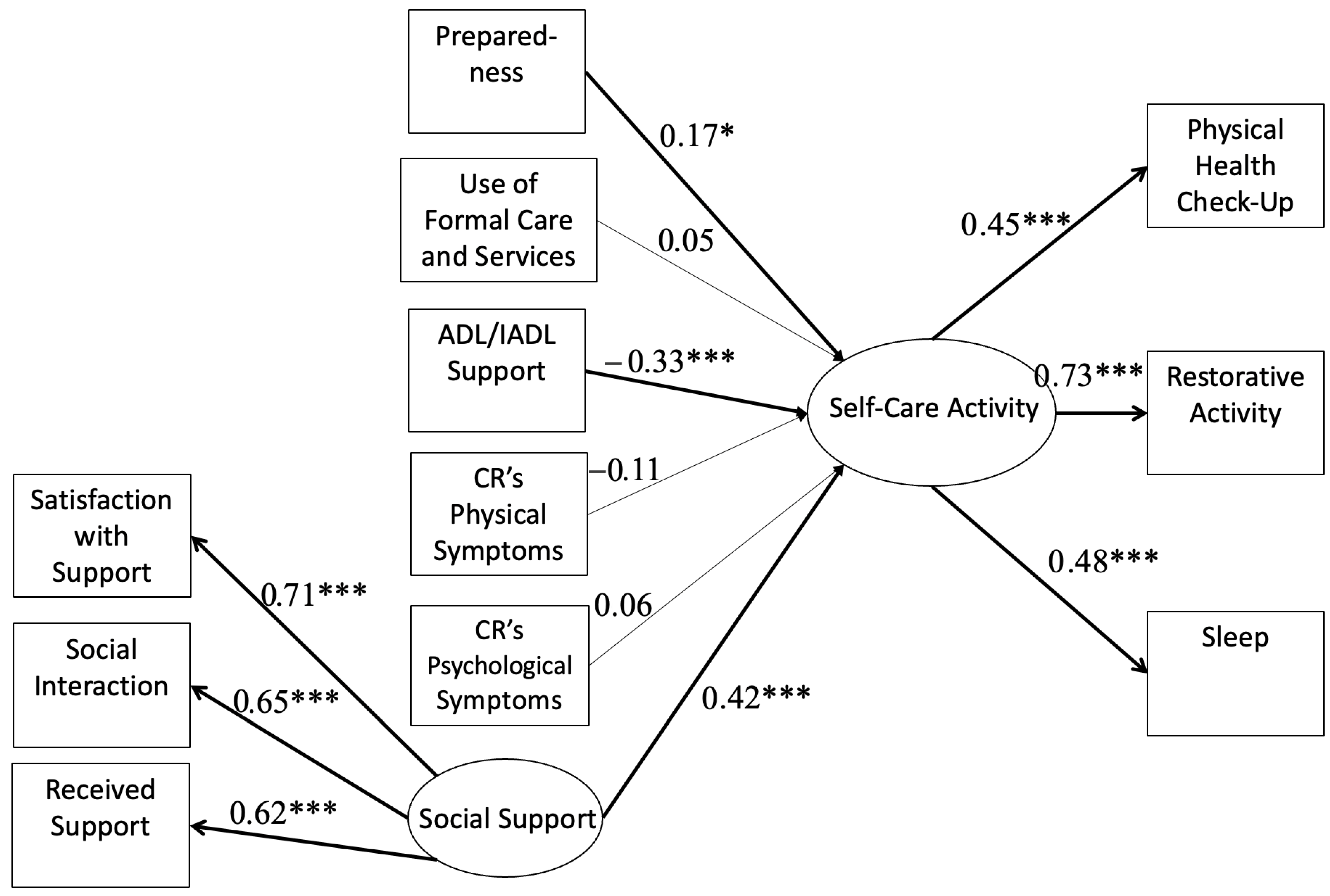
3.1. Caregiver Involvement and Social Support Predicting Engagement in Self-Care Activities
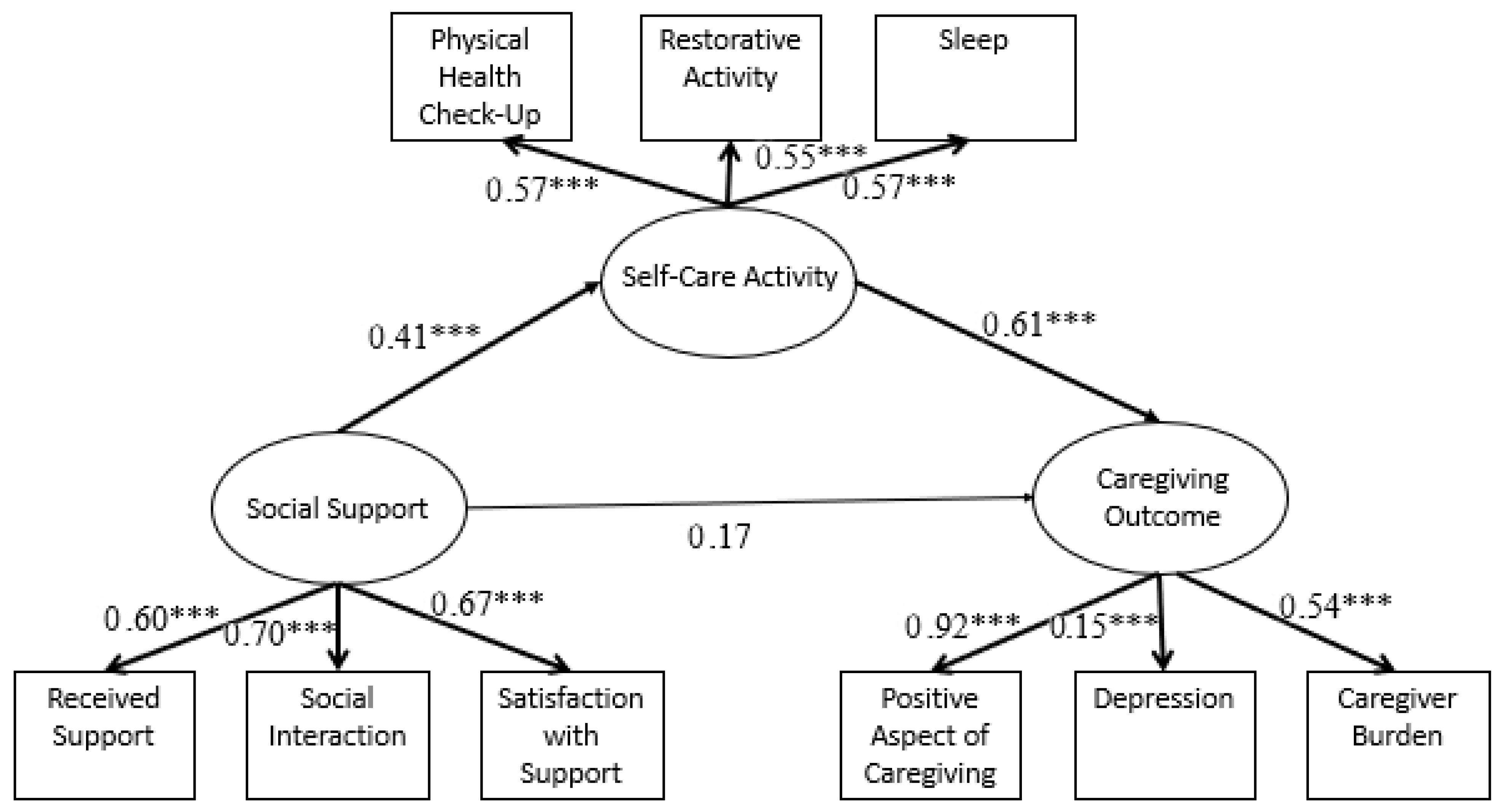
3.2. Self-Care Activity as A Mediator in the Relationship between Social Support and Caregiving Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alhasan, D.M.; Hirsch, J.A.; Jackson, C.L.; Miller, M.C.; Cai, B.; Lohman, M.C. Neighborhood Characteristics and the Mental Health of Caregivers Cohabiting with Care Recipients Diagnosed with Alzheimer’s Disease. Int. J. Environ. Res. Public Health 2021, 18, 913. [Google Scholar] [CrossRef] [PubMed]
- Alzheimer’s Association. 2023 Alzheimer’s Disease Facts and Figures. Alzheimer’s & Dementia. 2023. Available online: https://alz-journals.onlinelibrary.wiley.com/doi/10.1002/alz.13016 (accessed on 25 April 2023).
- Anderson, J.G.; Hundt, E.; Dean, M.; Rose, K.M. “A Fine Line That We Walk Every Day”: Self-Care Approaches Used by Family Caregivers of Persons with Dementia. Issues Ment. Health Nurs. 2019, 40, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Andresen, E.M.; Malmgren, J.A.; Carter, W.B.; Patrick, D.L. Screening for Depression in Well Older Adults: Evaluation of a Short Form of the CES-D. Am. J. Prev. Med. 1994, 10, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Archbold, P.G.; Stewart, B.J.; Greenlick, M.R.; Harvath, T. Mutuality and preparedness as predictors of caregiver role strain. Res. Nurs. Health 1990, 13, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Barrera, M.; Sandler, I.N.; Ramsay, T.B. Preliminary development of a scale of social support: Studies on college students. Am. J. Community Psychol. 1981, 9, 435–447. [Google Scholar] [CrossRef]
- Bédard, M.; Molloy, D.W.; Squire, L.; Dubois, S.; Lever, J.A.; O’Donnell, M. The Zarit Burden Interview: A new short version and screening version. Gerontologist 2001, 41, 652–657. [Google Scholar] [CrossRef]
- Belle, S.H.; Burgio, L.; Burns, R.; Coon, D.; Czaja, S.J.; Gallagher-Thompson, D.; Gitlin, L.N.; Klinger, J.; Koepke, K.M.; Lee, C.C.; et al. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: A randomized, controlled trial. Ann. Intern. Med. 2006, 145, 727–738. [Google Scholar] [CrossRef]
- Blok, A.C. A Middle-Range Explanatory Theory of Self-Management Behavior for Collaborative Research and Practice. Nurs. Forum 2017, 52, 138–146. [Google Scholar] [CrossRef]
- Brandt, J.; Spencer, M.; Folstein, M. The Telephone Interview for Cognitive Status. Neuropsychiatry Neuropsychol. Behav. Neurol. 1988, 1, 111–117. [Google Scholar] [CrossRef]
- Chan, C.Y.; Cheung, G.; Martinez-Ruiz, A.; Chau, P.Y.K.; Wang, K.; Yeoh, E.K.; Wong, E.L.Y. Caregiving burnout of community-dwelling people with dementia in Hong Kong and New Zealand: A cross-sectional study. BMC Geriatr. 2021, 21, 261. [Google Scholar] [CrossRef]
- Cohen, S.A.; Cook, S.; Kelley, L.; Sando, T.; Bell, A.E. Psychosocial factors of caregiver burden in child caregivers: Results from the new national study of caregiving. Health Qual. Life Outcomes 2015, 13, 120. [Google Scholar] [CrossRef]
- Feldman, S.J.; Solway, E.; Kirch, M.; Malani, P.; Singer, D.; Roberts, J.S. Correlates of Formal Support Service Use among Dementia Caregivers. J. Gerontol. Soc. Work. 2021, 64, 135–150. [Google Scholar] [CrossRef] [PubMed]
- Greenwood, N.; Smith, R. Motivations for being informal carers of people living with dementia: A systematic review of qualitative literature. BMC Geriatr. 2019, 19, 169. [Google Scholar] [CrossRef] [PubMed]
- Hartweg, D. Dorothea Orem: Self-Care Deficit Theory; SAGE Publications: Thousand Oaks, CA, USA, 1991. [Google Scholar]
- Jutkowitz, E.; Gaugler, J.E.; Trivedi, A.N.; Mitchell, L.L.; Gozalo, P. Family caregiving in the community up to 8-years after onset of dementia. BMC Geriatr. 2020, 20, 216. [Google Scholar] [CrossRef] [PubMed]
- Katz, S.; Ford, A.B.; Moskowitz, R.W.; Jackson, B.A.; Jaffe, M.W. Studies of Illness in the Aged. The Index of ADL: A Standardized Measure of Biological and Phychological Funcation. JAMA 1963, 185, 914–919. [Google Scholar] [CrossRef]
- Krause, N. Negative interaction and satisfaction with social support among older adults. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 1995, 50B, P59–P73. [Google Scholar] [CrossRef]
- Lee, J.; Baik, S.; Becker, T.D.; Cheon, J.H. Themes describing social isolation in family caregivers of people living with dementia: A scoping review. Dementia 2022, 21, 701–721. [Google Scholar] [CrossRef]
- Liang, J.; Aranda, M.P.; Lloyd, D.A. Association between Role Overload and Sleep Disturbance among Dementia Caregivers: The Impact of Social Support and Social Engagement. J. Aging Health 2020, 32, 1345–1354. [Google Scholar] [CrossRef]
- Lin, X.Y.; Zhang, L.; Yoon, S.; Zhang, R.; Lachman, M.E. A Social Exergame Intervention to Promote Physical Activity, Social Support, and Well-Being in Family Caregivers. Gerontologist 2023. online ahead of print. [Google Scholar] [CrossRef]
- Lubben, J.E. Assessing social networks among elderly populations. Fam. Community Health J. Health Promot. Maint. 1988, 11, 42–52. [Google Scholar] [CrossRef]
- Muthen, L.K.; Muthen, B. Mplus Version 8 User’s Guide; Muthen & Muthen: Los Angeles, CA, USA, 2017. [Google Scholar]
- Oliveira, D.; Sousa, L.; Orrell, M. Improving health-promoting self-care in family carers of people with dementia: A review of interventions. Clin. Interv. Aging 2019, 2019, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Pearlin, L.I.; Mullan, J.T.; Semple, S.J.; Skaff, M.M. Caregiving and the Stress Process: An Overview of Concepts and Their Measures. Gerontologist 1990, 30, 583–594. [Google Scholar] [CrossRef] [PubMed]
- Pressman, S.D.; Matthews, K.A.; Cohen, S.; Martire, L.M.; Scheier, M.; Baum, A.; Schulz, R. Association of Enjoyable Leisure Activities with Psychological and Physical Well-Being. Psychosom. Med. 2009, 71, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Qiu, D.; Hu, M.; Yu, Y.; Tang, B.; Xiao, S. Acceptability of psychosocial interventions for dementia caregivers: A systematic review. BMC Psychiatry 2019, 19, 23. [Google Scholar] [CrossRef] [PubMed]
- Sabo, K.; Chin, E. Self-care needs and practices for the older adult caregiver: An integrative review. Geriatr. Nurs. 2020, 42, 570–581. [Google Scholar] [CrossRef]
- Sheehan, O.C.; Haley, W.E.; Howard, V.J.; Huang, J.; Rhodes, J.D.; Roth, D.L. Stress, Burden, and Well-Being in Dementia and Nondementia Caregivers: Insights From the Caregiving Transitions Study. Gerontologist 2021, 61, 670–679. [Google Scholar] [CrossRef]
- Shyu, Y.-I.L.; Yang, C.-T.; Huang, C.-C.; Kuo, H.-C.; Chen, S.-T.; Hsu, W.-C. Influences of Mutuality, Preparedness, and Balance on Caregivers of Patients with Dementia. J. Nurs. Res. 2010, 18, 155–163. [Google Scholar] [CrossRef]
- Tarlow, B.J.; Wisniewski, S.R.; Belle, S.H.; Rubert, M.; Ory, M.G.; Gallagher-Thompson, D. Positive Aspects of Caregiving: Contributions of the REACH Project to the Development of New Measures for Alzheimer’s Caregiving. Res. Aging 2004, 26, 429–453. [Google Scholar] [CrossRef]
- von Känel, R.; Mausbach, B.T.; Patterson, T.L.; Dimsdale, J.E.; Aschbacher, K.; Mills, P.J.; Ziegler, M.G.; Ancoli-Israel, S.; Grant, I. Increased Framingham Coronary Heart Disease Risk Score in Dementia Caregivers Relative to Non-Caregiving Controls. Gerontology 2008, 54, 131–137. [Google Scholar] [CrossRef]
- Waligora, K.J.; Bahouth, M.N.; Han, H.-R. The Self-Care Needs and Behaviors of Dementia Informal Caregivers: A Systematic Review. Gerontologist 2019, 59, e565–e583. [Google Scholar] [CrossRef]
- Wang, X.R.; Robinson, K.M.; Carter-Harris, L. Prevalence of chronic illnesses and characteristics of chronically ill informal caregivers of persons with dementia. Age Ageing 2014, 43, 137–141. [Google Scholar] [CrossRef]
- Wang, X.; Liu, S.; Robinson, K.M.; Shawler, C.; Zhou, L. The impact of dementia caregiving on self-care management of caregivers and facilitators: A qualitative study. Psychogeriatrics 2019, 19, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E.; Sherbourne, C.D. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual Framework and Item Selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Weierbach, F.M.; Cao, Y. A Model of Health for Family Caregivers of Elders. Healthcare 2016, 5, 1. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.Y.; Saksono, H.; Stowell, E.; Lachman, M.E.; Castaneda-Sceppa, C.; Parker, A.G. Go&Grow: An Eval-uation of a Pervasive Social Exergame for Caregivers of Loved Ones with Dementia. Proc. ACM Hum.-Comput. Interact. 2020, 4, 151. [Google Scholar] [CrossRef]
- Win, K.K.; Chong, M.S.; Ali, N.; Chan, M.; Lim, W.S. Burden among Family Caregivers of Dementia in the Oldest-Old: An Exploratory Study. Front. Med. 2017, 4, 205. [Google Scholar] [CrossRef]
- Xian, M.; Xu, L. Social support and self-rated health among caregivers of people with dementia: The mediating role of caregiving burden. Dementia 2020, 19, 2621–2636. [Google Scholar] [CrossRef]
- Yáñez, J.J. Resilience among Latinx Caregivers of Older Adults with a Major Neurocognitive Disorder: Caregiving Effects on Mood, Stress, and Cognition [Ph.D., Alliant International University]. 2021. Available online: https://www.proquest.com/docview/2419100711/abstract/5EDBB4366B6246E2PQ/1 (accessed on 25 April 2023).
| Variables | Mean or % | Standard Deviation | |
|---|---|---|---|
| Background Characteristics | Age | 61.27 | 12.94 |
| Gender (% of Female) | 83.60% | ||
| Race/Ethnicity | |||
| White | 32.40% | ||
| African American | 22.50% | ||
| Hispanic | 45.10% | ||
| Relationship to the Care Recipient | |||
| Spouse | 40.60% | ||
| Other Relationships | 59.40% | ||
| Employment Status | |||
| Full-Time | 27% | ||
| Part-Time | 11.50% | ||
| Homemaker | 7% | ||
| Retired | 37.70% | ||
| Unemployed | 16.80% | ||
| Self-Care Activity | Physical Health Check-Up | 6.09 | 2.24 |
| Restorative Activity | 17.74 | 8.26 | |
| Sleep | 2.51 | 0.86 | |
| Caregiver Involvement | ADL/IADL Support | 9.04 | 0.86 |
| Formal Use of Care and Services | 1.43 | 1.18 | |
| Preparedness | 2.27 | 0.76 | |
| Care Recipient’s Physical Symptoms | 2.58 | 1.63 | |
| Care Recipient’s Psychological Symptoms | 14.78 | 8.60 | |
| Social Support | Received Support | 6.25 | 2.74 |
| Satisfaction with Support | 7.77 | 3.49 | |
| Social Interaction | 8.38 | 3.25 | |
| Caregiving Outcome | Caregiver Burden | 19.09 | 8.29 |
| Positive Aspect of Caregiving | 23.86 | 8.66 | |
| Depression | |||
| Physical Health Check-Up | Restorative Activity | Sleep | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | t or F | p | M | SD | t or F | p | M | SD | t or F | p | |
| Age | ||||||||||||
| Under 65 | 5.39 | 2.19 | −6.7 | <0.001 | 16.69 | 8.23 | −2.54 | 0.01 | 2.41 | 0.90 | −2.24 | 0.03 |
| Over 65 | 7.21 | 1.83 | 19.43 | 8.08 | 2.67 | 0.78 | ||||||
| Gender | ||||||||||||
| Female | 5.95 | 2.16 | −2.3 | 0.02 | 17.67 | 8.36 | −0.30 | 0.77 | 2.51 | 0.87 | −0.12 | 0.91 |
| Male | 6.83 | 2.50 | 18.09 | 7.83 | 2.53 | 0.85 | ||||||
| Race/Ethnicity | ||||||||||||
| White | 6.47 | 2.15 | 1.83 | 0.16 | 19.64 | 8.29 | 4.19 | 0.02 | 2.62 | 0.81 | 1.04 | 0.36 |
| African American | 5.80 | 2.06 | 18.26 | 7.85 | 2.53 | 0.86 | ||||||
| Hispanic | 5.96 | 2.37 | 16.13 | 8.20 | 2.43 | 0.90 | ||||||
| Relationship to the Care Recipient | ||||||||||||
| Spouse | 6.78 | 2.11 | −4.30 | <0.001 | 17.83 | 7.71 | −0.25 | 0.80 | 2.63 | 0.79 | −1.93 | 0.06 |
| Other | 5.56 | 2.19 | 17.56 | 8.66 | 2.42 | 0.90 | ||||||
| Employment Status | ||||||||||||
| Full-Time | 5.83 | 1.92 | 7.32 | <0.001 | 16.73 | 7.78 | 1.11 | 0.35 | 2.56 | 0.96 | 2.87 | 0.02 |
| Part-Time | 5.25 | 2.50 | 16.83 | 8.00 | 2.32 | 0.86 | ||||||
| Homemaker | 5.29 | 2.17 | 18.74 | 8.29 | 2.59 | 0.71 | ||||||
| Retired | 7.00 | 1.91 | 19.03 | 8.14 | 2.67 | 0.79 | ||||||
| Unemployed | 5.37 | 2.59 | 16.70 | 9.36 | 2.17 | 0.83 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, X.; Moxley, J.H.; Czaja, S.J. Caring for Dementia Caregivers: Psychosocial Factors Related to Engagement in Self-Care Activities. Behav. Sci. 2023, 13, 851. https://doi.org/10.3390/bs13100851
Lin X, Moxley JH, Czaja SJ. Caring for Dementia Caregivers: Psychosocial Factors Related to Engagement in Self-Care Activities. Behavioral Sciences. 2023; 13(10):851. https://doi.org/10.3390/bs13100851
Chicago/Turabian StyleLin, Xinyao, Jerad H. Moxley, and Sara J. Czaja. 2023. "Caring for Dementia Caregivers: Psychosocial Factors Related to Engagement in Self-Care Activities" Behavioral Sciences 13, no. 10: 851. https://doi.org/10.3390/bs13100851
APA StyleLin, X., Moxley, J. H., & Czaja, S. J. (2023). Caring for Dementia Caregivers: Psychosocial Factors Related to Engagement in Self-Care Activities. Behavioral Sciences, 13(10), 851. https://doi.org/10.3390/bs13100851






