Abstract
Background: Obesity and insomnia are prevalent public health issues with shared behavioral and physiological pathways. However, their interplay remains understudied in occupational cohorts. Obesity and insomnia are prevalent public health issues with shared behavioral and physiological pathways. However, their interplay remains understudied in occupational cohorts. This study aimed to evaluate the associations of sociodemographic factors, lifestyle habits, and insomnia severity with multiple obesity indices in a large population of Spanish workers. Methods: We conducted a cross-sectional analysis of 84,898 workers (2021–2024). Data were obtained from annual occupational health assessments conducted across multiple Spanish regions between 2020 and 2024. Insomnia severity was assessed using the Insomnia Severity Index (ISI), dietary quality using the 14-item Mediterranean Diet Adherence Screener (MEDAS-14), and physical activity using the International Physical Activity Questionnaire—Short Form (IPAQ-SF). Adiposity was measured using Body Mass Index (BMI), waist-to-height ratio (WtHR), the Clínica Universidad de Navarra–Body Adiposity Estimator (CUN-BAE), and the Metabolic Score for Visceral Fat (METS-VF). Multivariable logistic regression models were used to examine associations adjusted for age, sex, education, and occupational social class. Results: Higher ISI scores were significantly and independently associated with elevated adiposity across all indices, with the strongest association observed for METS-VF (odds ratio = 1.19, 95% CI 1.14–1.25, p < 0.001). Women showed higher mean CUN-BAE and METS-VF values than men (CUN-BAE: 37.4 ± 6.2 vs. 25.6 ± 6.4; p < 0.001; METS-VF: 5.7 ± 0.7 vs. 6.4 ± 0.6; p < 0.001), despite lower BMI (25.3 ± 4.8 vs. 26.8 ± 4.3; p < 0.001). Lower physical activity (OR = 5.70; 95% CI 4.91–6.50), poor adherence to the Mediterranean diet (OR = 3.29; 95% CI 2.88–3.70), smoking (OR = 1.29; 95% CI 1.22–1.36), and lower occupational class (Class III: OR = 1.77; 95% CI 1.56–1.97) were also significantly associated with higher obesity markers. Associations were more pronounced among women and participants with severe insomnia symptoms. Conclusions: Insomnia severity, sociodemographic disadvantage, and unhealthy behaviors (low physical activity, poor diet, smoking) were all independent correlates of general and visceral adiposity. The findings underscore the need for comprehensive workplace health programs that integrate sleep quality assessment, dietary improvement, and physical activity promotion to prevent obesity and its metabolic consequences.
1. Introduction
Obesity is a multifactorial and chronic condition characterized by excessive or abnormal accumulation of body fat that impairs health and increases the risk of numerous non-communicable diseases. Over the past decades, the global prevalence of obesity has reached pandemic levels, affecting more than 1 billion individuals worldwide [1,2] and contributing substantially to the burden of cardiovascular disease, type 2 diabetes mellitus (T2DM), certain cancers, musculoskeletal disorders, and premature mortality [3,4,5,6,7,8]. In Spain, recent estimates indicate that over 21% of adults meet the criteria for obesity, with an upward trend particularly evident in working-age populations [9,10].
From a pathophysiological perspective, obesity is associated with complex disturbances in neuroendocrine regulation, adipokine signaling, energy balance, and inflammatory pathways. Visceral adipose tissue, in particular, functions as a metabolically active endocrine organ that secretes cytokines and adipokines such as interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), leptin, and adiponectin, contributing to systemic inflammation, insulin resistance, and endothelial dysfunction [11,12,13,14,15,16]. These mechanisms promote the development of cardiometabolic conditions, including hypertension, dyslipidemia, non-alcoholic fatty liver disease (NAFLD), and atherosclerosis [17,18,19,20].
Traditionally, the body mass index (BMI) has been used as a standard tool to define obesity; however, it presents significant limitations. Despite extensive evidence linking individual behaviors to obesity, few large-scale occupational studies have simultaneously evaluated sociodemographic, behavioral, and sleep-related factors, leaving a gap in understanding how these determinants interact to influence obesity risk. BMI does not account for differences in fat distribution or distinguish between lean and fat mass, leading to diagnostic inaccuracies, especially in individuals with sarcopenic obesity or normal-weight central adiposity [21]. Consequently, alternative anthropometric and metabolic indices have been proposed to more accurately reflect body fat composition and cardiometabolic risk. Among these, the waist-to-height ratio (WtHR) offers a simple yet powerful measure of central obesity, with a cut-off value of 0.5 serving as a reliable predictor of metabolic dysfunction [22].
Given that each anthropometric index has inherent limitations, several complementary measures were included to improve the robustness of the analyses [23,24,25,26,27,28,29,30].
While lifestyle factors such as diet quality, physical activity, and smoking habits are well-established contributors to obesity, emerging evidence also points to the role of sleep health—particularly insomnia—in shaping adiposity patterns and metabolic outcomes. Insomnia is a prevalent sleep disorder characterized by difficulty initiating or maintaining sleep, or experiencing non-restorative sleep, despite adequate opportunity and circumstances for rest [31]. Chronic insomnia is associated with significant impairments in daytime functioning, mood disturbances, and reduced quality of life [32,33,34].
Epidemiological studies report that 10% to 30% of adults experience clinically significant insomnia, with higher prevalence among women, older individuals, and those in high-stress occupations [35]. The pathophysiology of insomnia involves dysregulation of the hypothalamic–pituitary–adrenal (HPA) axis, increased sympathetic activity, and alterations in sleep–wake homeostasis, all of which may affect appetite regulation, glucose metabolism, and fat storage [36,37,38]. Sleep restriction and poor sleep quality have been shown to impair leptin and ghrelin balance, increase cortisol levels, and elevate proinflammatory cytokines, thereby promoting weight gain and central fat accumulation [39,40,41].
Several population-based studies have demonstrated associations between insomnia and increased risk of obesity, metabolic syndrome, hypertension, and T2DM, even after adjusting for traditional risk factors [42,43,44]. However, few large-scale investigations have comprehensively examined how insomnia severity relates to validated adiposity indices, particularly within working populations exposed to high stress, sedentary behavior, and irregular schedules.
Accordingly, the present study aims to assess the associations between sociodemographic factors, lifestyle habits (diet, smoking, physical activity), and insomnia severity with multiple obesity indices in a large population of Spanish workers. By integrating anthropometric, metabolic, behavioral, and sleep-related variables, this study seeks to contribute new insights into the multidimensional determinants of obesity and support the development of more targeted and holistic workplace health interventions.
A secondary objective was to explore sex-specific differences in the associations among sociodemographic, behavioral, and obesity-related factors.
2. Methods
2.1. Study Design and Population
This cross-sectional observational study was carried out as part of a nationwide occupational health surveillance program in Spain. Data were collected between January 2021 and December 2024 during routine medical evaluations conducted at certified occupational health centers (Figure 1). Health surveillance was performed by Quirónprevención, a national occupational health provider in Spain. Participants were recruited from the industrial, commercial, and service sectors through company-based occupational health programs. They were drawn from various occupational health services across several Spanish Autonomous Communities that voluntarily agreed to participate in the study.
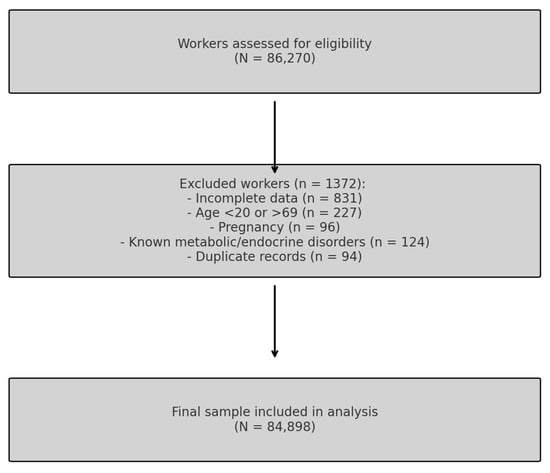
Figure 1.
Participant Flow Diagram.
All data were anonymized before analysis to ensure participant confidentiality. The study was approved by the Institutional Research Ethics Committee and complied with the ethical principles outlined in the Declaration of Helsinki. All participants provided written informed consent prior to their inclusion in the study.
2.2. Eligibility Criteria
To ensure internal validity and generalizability, strict inclusion and exclusion criteria were applied.
Inclusion criteria:
- Age between 18 and 69 years at the time of assessment, to represent the active working population.
- Employment as an active worker in any economic sector with a registered occupational record
- Availability of complete and validated data for all variables of interest, including anthropometric, biochemical, lifestyle, sociodemographic, and sleep-related measures
Exclusion criteria:
- Incomplete or missing data essential for the calculation of obesity indices or insomnia severity
- Age < 18 or >69 years
- Pregnancy at the time of examination
- Diagnosed metabolic or endocrine disorders (e.g., uncontrolled diabetes, thyroid dysfunction, malignancy, advanced chronic kidney disease)
- Duplicate records or inconsistencies in key demographic identifiers
From an initial pool of 86,270 individuals, 1372 workers were excluded based on these criteria, yielding a final sample of 84,898 participants eligible for analysis (Figure 1).
2.3. Data Collection and Variable Definitions
Anthropometric and clinical parameters were measured by trained personnel using standardized techniques and calibrated instruments. Height and weight were measured with participants in light clothing and without shoes. Waist circumference was measured at the midpoint between the lower rib and the iliac crest; hip circumference at the widest part of the buttocks. Systolic and diastolic blood pressure were measured in a seated position after at least five minutes of rest. Blood samples were drawn after a 10–12 h overnight fast to assess fasting plasma glucose, triglycerides, total cholesterol, HDL-c, and LDL-c, which were analyzed in ISO-certified laboratories.
Sociodemographic variables included sex, age, and occupational social class, the latter determined based on the Spanish National Classification of Economic Activities (CNAE-11). Social class was categorized as Class I (managers, professionals), Class II (intermediate occupations), or Class III (manual and routine occupations), following the guidelines of the Spanish Society of Epidemiology [45].
2.3.1. Assessment of Lifestyle Factors
Health-related lifestyle habits were self-reported using validated tools.
- Dietary quality was evaluated through the 14-item Mediterranean Diet Adherence Screener (MEDAS-14) [46]. A score ≥ 9 indicated adequate adherence to the Mediterranean dietary pattern, which emphasizes the consumption of fruits, vegetables, whole grains, legumes, olive oil, and moderate intake of fish and red wine [47].
- Physical activity was assessed using the International Physical Activity Questionnaire—Short Form (IPAQ-SF), a validated instrument used to estimate activity levels in population studies. Participants were classified as physically active or inactive according to standardized scoring protocols [48,49].
- Smoking status was classified as current smoker or non-smoker based on self-report.
2.3.2. Evaluation of Insomnia Severity
Sleep disturbances were assessed using the Insomnia Severity Index (ISI), a 7-item self-administered questionnaire that evaluates difficulties in sleep initiation, sleep maintenance, early morning awakenings, sleep dissatisfaction, interference with daily functioning, noticeability of sleep problems, and distress caused by poor sleep. The Insomnia Severity Index (ISI) is a validated and widely used tool in both clinical and research settings. It evaluates perceived insomnia symptoms over the past two weeks through seven items addressing sleep onset latency, sleep maintenance, satisfaction, interference with daily functioning, and distress [50]. The ISI has demonstrated strong psychometric properties and clinical utility for grading insomnia severity in occupational health studies.
Insomnia severity was analyzed primarily as a categorical variable, classified into four levels according to established cutoffs [51]:
- No insomnia (0–7)
- Subthreshold insomnia (8–14)
- Moderate insomnia (15–21)
- Severe insomnia (22–28)
The ISI is a widely validated instrument in both clinical and occupational populations and has shown high internal consistency and test–retest reliability.
2.3.3. Obesity and Adiposity Indices
A multidimensional approach was used to evaluate adiposity through four validated indices, providing a more comprehensive understanding of body fat distribution and metabolic risk.
While BMI is the most commonly used measure, it does not distinguish between fat and lean mass.
The waist-to-height ratio (WtHR) offers a simple yet effective proxy for central adiposity, while the Clínica Universidad de Navarra–Body Adiposity Estimator (CUN-BAE) estimates total body fat percentage by accounting for age and sex.
The Metabolic Score for Visceral Fat (METS-VF) is a novel index that integrates sex, age, WtHR, fasting glucose, and triglycerides to estimate visceral adiposity and its associated metabolic dysfunction.
The four indices were defined and calculated as follows:
- Body Mass Index (BMI): calculated as weight in kilograms divided by height in meters squared (kg/m2); obesity defined as BMI ≥ 30 kg/m2.
- Waist-to-Height Ratio (WtHR): waist circumference (cm) divided by height (cm); central obesity defined as WtHR ≥ 0.50.
- Clínica Universidad de Navarra–Body Adiposity Estimator (CUN-BAE): a regression-based formula incorporating age, sex, and BMI to estimate body fat percentage; obesity defined as CUN-BAE ≥ 35% [52].
- Metabolic Score for Visceral Fat (METS-VF): a composite index that integrates sex, age, WtHR, fasting glucose, and triglycerides; a score ≥ 6.3 was used to define high visceral adiposity [53].
These indices were selected based on prior validation in Mediterranean and working populations and offer complementary perspectives on adiposity distribution and metabolic risk (Figure 2).
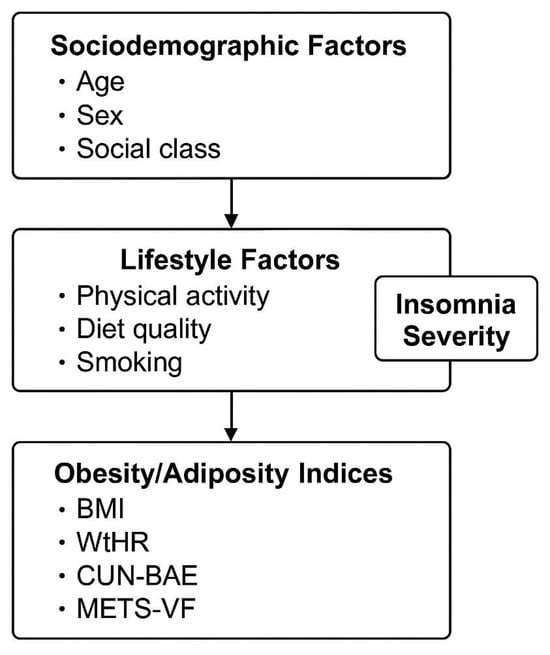
Figure 2.
Conceptual framework illustrating the unidirectional associations between sociodemographic factors, lifestyle factors (physical activity, diet quality, and smoking), and insomnia severity (independent variables) with obesity/adiposity indices (BMI, WtHR, CUN-BAE, and METS-VF). Arrows represent hypothesized directional associations, not causal relationships.
2.4. Statistical Analysis
Descriptive statistics were used to summarize the characteristics of the population. Continuous variables were reported as means and standard deviations (SD), and categorical variables as frequencies and percentages. Comparisons between groups were made using Student’s t-test or ANOVA for continuous variables and the chi-square test for categorical variables.
To examine the independent associations between sociodemographic characteristics, health behaviors, insomnia severity, and the presence of obesity, a series of multivariate logistic regression models were fitted for each adiposity index. Between-group analyses were performed to compare men and women with respect to sociodemographic, lifestyle, and clinical variables using Student’s t-tests for continuous data and chi-square tests for categorical data. Subsequently, multivariable logistic regression models were fitted for each adiposity index as the dependent variable, with sociodemographic characteristics, lifestyle factors, and insomnia severity entered as independent predictors. Sensitivity analyses were performed by sex. Results were reported as odds ratios (ORs) with 95% confidence intervals (CIs). Statistical significance was defined as p < 0.05. All analyses were conducted using IBM SPSS Statistics for Windows, version 29.0 (IBM Corp., Armonk, NY, USA).
3. Results
Table 1 provides a comprehensive overview of the sociodemographic, anthropometric, clinical, and lifestyle characteristics of the study population, stratified by sex. Significant sex-based differences were observed across all variables (p < 0.001). Standard deviations were reported to describe population variability rather than precision of the mean, as recommended for large epidemiological datasets. Men presented higher mean values for weight, waist circumference, blood pressure, triglycerides, LDL-c, and glucose, while women showed higher HDL-c levels and healthier lifestyle behaviors, such as adherence to the Mediterranean diet and physical activity. Notably, insomnia severity differed markedly by sex, with women more frequently reporting no insomnia (64.8%) and men showing a higher prevalence of moderate to severe insomnia. These findings highlight relevant sex-specific differences in cardiometabolic risk profiles and sleep disturbances in occupational cohorts.

Table 1.
Sociodemographic, Clinical, and Lifestyle Characteristics of the Study Population, Stratified by Sex.
Table 2 presents the distribution of BMI, waist-to-height ratio (WtHR), CUN-BAE, and METS-VF across categories of age, social class, smoking status, dietary habits, physical activity, and insomnia severity. A consistent trend of increasing adiposity was observed with age and lower socioeconomic status in both sexes. Physical inactivity and poor adherence to the Mediterranean diet were associated with markedly higher values in all obesity indices. Importantly, there was a stepwise increase in obesity index scores across insomnia severity categories, with the highest values among those with severe insomnia. These findings suggest a cumulative burden of sociodemographic disadvantages, unhealthy behaviors, and sleep disturbances on obesity and visceral fat accumulation.

Table 2.
Mean Values of Four Obesity and Adiposity Indices According to Sociodemographic and Lifestyle Variables, by Sex.
Table 3 reports the prevalence of obesity and high adiposity across four indices (BMI, WtHR, CUN-BAE, METS-VF), stratified by relevant sociodemographic and behavioral factors. The data reveal that the proportion of individuals with elevated adiposity rises with age, lower social class, smoking, poor diet, and physical inactivity. Importantly, a clear dose–response relationship is evident between insomnia severity and all obesity metrics. For example, severe insomnia is associated with markedly higher obesity prevalence (e.g., 39.8% for BMI in men, 37.2% in women). This table underscores the need to integrate sleep health into comprehensive strategies addressing obesity and metabolic risk in the workplace.

Table 3.
Prevalence of Obesity and High Adiposity Based on Four Indices According to Sociodemographic and Lifestyle Variables, by Sex.
Table 4 displays the adjusted odds ratios (ORs) and 95% confidence intervals for having obesity or high visceral adiposity based on four indices, considering sex, age group, social class, smoking status, diet, physical activity, and insomnia severity. Male sex, older age, lower social class, smoking, unhealthy diet, and physical inactivity were significantly associated with increased odds of obesity across all indices. Insomnia severity showed a strong and independent association with obesity risk: compared to those without insomnia, individuals with moderate or severe insomnia had substantially higher ORs for all outcomes, with the strongest associations observed for METS-VF. These results highlight insomnia as a potential modifiable risk factor for visceral obesity and support the inclusion of sleep assessments in occupational health programs.

Table 4.
Adjusted Odds Ratios for Obesity and High Visceral Adiposity According to Sociodemographic, Lifestyle, and Insomnia Variables.
Figure 3 presents a forest plot of the associations between insomnia severity and obesity indices. BMI obesity, WtHR high, CUN-BAE obesity, and METS-VF high. Notably, METS-VF shows markedly higher ORs across all subgroups, particularly in men and older age groups, suggesting a stronger association with visceral adiposity. Lifestyle-related variables, such as physical inactivity and non-adherence to the Mediterranean diet, demonstrate the highest ORs across all indices, highlighting their critical role in metabolic health. One extreme value among male participants was retained after data validation and is presented as an outlier in Figure 3 to reflect the true range of adiposity observed. These findings underscore the importance of comprehensive lifestyle interventions in reducing obesity-related cardiometabolic risk.
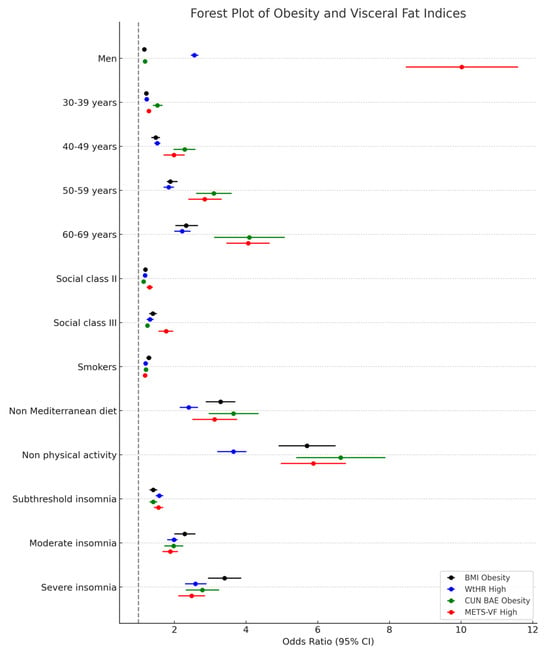
Figure 3.
Forest Plot of Obesity and Visceral Fat Indices.
4. Discussion
This study demonstrates that insomnia severity, unhealthy lifestyle behaviors, and sociodemographic disadvantage are independently associated with higher levels of adiposity in both men and women. These findings highlight the importance of integrating sleep assessment and behavioral health promotion into workplace health strategies.
To our knowledge, this is the first large-scale occupational study in Spain to simultaneously examine insomnia severity, lifestyle habits, and multiple validated adiposity indices within the same analytical framework. By combining both traditional (BMI, WtHR) and emerging indices (CUN-BAE, METS-VF), this work provides a multidimensional view of obesity and its determinants among employed adults.
4.1. Main Findings and Interpretation
In this large cross-sectional sample of Spanish workers, several consistent associations emerged. Female sex, lower physical activity, poorer adherence to the Mediterranean diet, smoking, and higher insomnia severity were all independently linked to increased adiposity. Importantly, higher insomnia scores were strongly associated with greater visceral fat accumulation, as reflected by elevated METS-VF values. These results reinforce the multifactorial nature of obesity and suggest that sleep quality represents a key, yet often overlooked, component of metabolic health in working populations.
4.2. Comparison with Previous Studies
Our results align with previous evidence indicating that short sleep duration and poor sleep quality are significant contributors to obesity and metabolic dysregulation [54]. For instance, meta-analyses have shown that individuals with insomnia symptoms have higher risks of obesity and cardiometabolic disturbances [55]. Similarly, large European cohorts have reported associations between insufficient sleep and increased BMI and waist circumference [56]. The strong link between insomnia and visceral adiposity observed here is consistent with the ELSA-Brasil study, which found that poor sleep quality was correlated with greater visceral fat measured by imaging techniques [57].
Physiological mechanisms may explain these associations. Sleep restriction and insomnia can disrupt leptin and ghrelin balance, elevate cortisol levels, and promote systemic inflammation—all of which contribute to increased appetite, reduced energy expenditure, and visceral fat deposition [58]. Furthermore, chronic sympathetic overactivation and altered hypothalamic–pituitary–adrenal (HPA) axis activity may exacerbate insulin resistance and metabolic imbalance in individuals with poor sleep quality [59].
In terms of lifestyle, our findings corroborate previous research showing that physical inactivity and low adherence to the Mediterranean diet are major risk factors for obesity in Mediterranean populations [60,61]. The additive role of insomnia further supports recent hypotheses suggesting a bidirectional relationship between poor sleep and unhealthy behaviors: individuals who sleep poorly are more likely to make suboptimal dietary choices and engage in sedentary lifestyles, which in turn worsen sleep patterns [62].
We also observed that women exhibited higher mean CUN-BAE and METS-VF values despite lower BMI, underscoring the need for sex-specific approaches when assessing adiposity and metabolic risk. This pattern is consistent with prior studies reporting that women may be more susceptible to sleep-related metabolic alterations, potentially mediated by hormonal and psychosocial factors [63,64].
Regarding tobacco use, our findings add to a complex body of evidence. Previous studies have shown inconsistent relationships between smoking and obesity [65], with some indicating lower body weight among smokers and others linking tobacco use to increased central adiposity [66]. In our study, smoking was independently associated with higher adiposity levels, suggesting that metabolic and behavioral factors—such as altered appetite regulation, reduced physical fitness, or compensatory dietary patterns—may contribute to this relationship among working adults.
4.3. Strengths and Limitations
Key strengths of this study include its large, heterogeneous occupational cohort, the use of multiple validated adiposity indices, and the standardized assessment of sleep, dietary habits, and physical activity. Incorporating both CUN-BAE and METS-VF provided a more comprehensive understanding of total and visceral fat distribution, improving the clinical interpretability of our findings.
However, several limitations must be acknowledged. The cross-sectional design prevents causal inference, and the self-reported nature of some measures (such as ISI, MEDAS-14, and IPAQ-SF) may introduce recall or social desirability bias. Residual confounding due to unmeasured factors—such as sleep apnea, chronic stress, or mental health disorders—cannot be ruled out. Additionally, because the sample consists of employed adults undergoing occupational health evaluations, the generalizability to unemployed or retired populations may be limited.
4.4. Implications and Future Directions
These findings underscore the need for integrated workplace interventions that simultaneously address sleep hygiene, physical activity, and dietary habits. Occupational health programs should routinely include sleep quality assessments—such as the Insomnia Severity Index—alongside metabolic screenings. Tailored interventions may be particularly beneficial for women, given their greater susceptibility to sleep-related metabolic disturbances.
Future research should employ longitudinal designs to establish causality and explore potential mediating mechanisms between sleep and obesity. Objective sleep measures (e.g., actigraphy, polysomnography) and biomarkers of stress and inflammation would further elucidate the biological pathways involved. Moreover, examining psychosocial stress, work schedules, and shift patterns could deepen understanding of how occupational factors influence the sleep–obesity relationship.
5. Conclusions
In summary, this study identifies insomnia severity, poor lifestyle behaviors, and sociodemographic disadvantage as independent correlates of general and visceral adiposity in Spanish workers. Poor sleep quality emerges as a key determinant of metabolic health, highlighting the need to incorporate sleep assessment into comprehensive workplace wellness programs. Interventions that jointly promote adequate sleep, healthy diet, and regular physical activity are likely to be most effective in preventing obesity and its associated comorbidities. Future longitudinal studies should confirm these associations and evaluate the impact of integrated, sex-sensitive health strategies in occupational settings.
Author Contributions
Conceptualization: J.L.R.V., C.B.-C. and Á.A.L.G.; Data collection and analysis: P.J.T.L., I.C.C. and J.L.R.V.; Data curation: J.L.R.V. and P.J.T.L. Methodology: Á.A.L.G. and I.C.C. Validation: J.I.R.-M.; Formal analysis: C.B.-C.; Investigation J.L.R.V.; Draft: J.L.R.V., P.J.T.L., I.C.C., J.I.R.-M. and Revision: Á.A.L.G., C.B.-C. and J.I.R.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This work was undertaken without any financial assistance. No funding was obtained from governmental bodies, academic institutions, or commercial sponsors.
Institutional Review Board Statement
The research was designed and conducted following national and international ethical guidelines for human studies, including the ethical principles outlined in the Declaration of Helsinki. All protocols prioritized participant autonomy, confidentiality, and data protection. Before enrollment, participants received comprehensive written and oral information explaining the purpose, procedures, and scope of the study. Participation was entirely voluntary, and each subject signed an informed consent form prior to any data collection. Ethical approval for this study was issued by the Balearic Islands Research Ethics Committee (Comité de Ética de la Investigación de las Islas Baleares, CEI-IB), under protocol number IB 4383/20, on 26 November 2020. Personal identifiers were encrypted and accessible solely to the principal investigator to ensure strict confidentiality. Under no circumstances will individual-level data be shared or made public. The study was also conducted in full accordance with Spain’s Organic Law 3/2018 concerning the protection of personal data and the European General Data Protection Regulation (EU GDPR 2016/679). Participants were duly informed of their rights to access, correct, restrict, or delete their personal information.
Informed Consent Statement
All participants gave their express written consent after being informed of the study’s objectives, procedures, and potential consequences.
Data Availability Statement
Data derived from this research are securely maintained within the facilities of ADEMA University School. The management and safeguarding of these data comply with relevant data protection laws and are overseen by the institution’s appointed Data Protection Officer, Ángel Arturo López González.
Acknowledgments
The authors would like to sincerely thank all individuals who took part in this research, whose engagement and willingness were essential for its successful completion. Special recognition is given to the occupational health teams and professionals responsible for the collection, anonymization, and organization of both clinical and behavioral data. We are also grateful for the continued support provided by the technical and administrative personnel of ADEMA University School. Their assistance throughout the different stages of the project, as well as that of the partner institutions who offered infrastructure and data access, was invaluable.
Conflicts of Interest
The authors report no conflicts of interest—financial or otherwise—related to the planning, execution, analysis, or dissemination of this research.
References
- World Health Organization. Obesity and Overweight; WHO: Geneva, Switzerland, 2024; Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 12 July 2025).
- Lin, X.; Li, H. Obesity: Epidemiology, Pathophysiology, and Therapeutics. Front. Endocrinol. 2021, 12, 706978. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sastre-Alzamora, T.; Tomás-Gil, P.; Paublini, H.; Pallarés, L.; Ramírez-Manent, J.I.; López-González, A.A. Relationship between different scales of overweight and obesity and heart age values in 139634 spanish workers. Acad. J. Health Sci. 2023, 38, 137–144. [Google Scholar] [CrossRef]
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ruze, R.; Liu, T.; Zou, X.; Song, J.; Chen, Y.; Xu, R.; Yin, X.; Xu, Q. Obesity and type 2 diabetes mellitus: Connections in epidemiology, pathogenesis, and treatments. Front. Endocrinol. 2023, 14, 1161521. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Belladelli, F.; Montorsi, F.; Martini, A. Metabolic syndrome, obesity and cancer risk. Curr. Opin. Urol. 2022, 32, 594–597. [Google Scholar] [CrossRef] [PubMed]
- Holanda, N.; Crispim, N.; Carlos, I.; Moura, T.; Nóbrega, E.; Bandeira, F. Musculoskeletal effects of obesity and bariatric surgery—A narrative review. Arch. Endocrinol. Metab. 2022, 66, 621–632. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, X.; Ma, N.; Lin, Q.; Chen, K.; Zheng, F.; Wu, J.; Dong, X.; Niu, W. Body Roundness Index and All-Cause Mortality Among US Adults. JAMA Netw. Open 2024, 7, e2415051, Erratum in JAMA Netw. Open 2024, 7, e2426540. https://doi.org/10.1001/jamanetworkopen.2024.26540. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aranceta-Bartrina, J.; Pérez-Rodrigo, C.; Alberdi-Aresti, G.; Ramos-Carrera, N.; Lázaro-Masedo, S. Prevalence of General Obesity and Abdominal Obesity in the Spanish Adult Population (Aged 25-64 Years) 2014-2015: The ENPE Study. Rev. Esp. Cardiol. Engl. Ed. 2016, 69, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Marina Arroyo, M.; Ramírez Gallegos, I.; López-González, A.A.; Vicente-Herrero, M.T.; Vallejos, D.; Tárraga López, P.J.; Manent, J.I.R. Equation Córdoba body fat values according to sociodemographic variables and healthy habits in 386924 Spanish workers. Acad. J. Health Sci. 2024, 39, 31–39. [Google Scholar] [CrossRef]
- Koc, G.; Doran, T.; Uygur, M.M.; Kirac, D. Obesity is associated with IL-6 gene polymorphisms rs1800795 and rs1800796 but not SOCS3 rs4969170. Mol. Biol. Rep. 2023, 50, 2041–2048. [Google Scholar] [CrossRef] [PubMed]
- Hasan Azeez, S. Influence of IL-10, IL-6 and TNF-α gene polymorphism on obesity. Cell. Mol. Biol. 2023, 69, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Obradovic, M.; Sudar-Milovanovic, E.; Soskic, S.; Essack, M.; Arya, S.; Stewart, A.J.; Gojobori, T.; Isenovic, E.R. Leptin and Obesity: Role and Clinical Implication. Front. Endocrinol. 2021, 12, 585887. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, J.Y.; Barua, S.; Jeong, Y.J.; Lee, J.E. Adiponectin: The Potential Regulator and Therapeutic Target of Obesity and Alzheimer’s Disease. Int. J. Mol. Sci. 2020, 21, 6419. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yazıcı, D.; Demir, S.Ç.; Sezer, H. Insulin Resistance, Obesity, and Lipotoxicity. Adv. Exp. Med. Biol. 2024, 1460, 391–430. [Google Scholar] [CrossRef] [PubMed]
- Engin, A. Endothelial Dysfunction in Obesity and Therapeutic Targets. Adv. Exp. Med. Biol. 2024, 1460, 489–538. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.E.; Mouton, A.J.; da Silva, A.A.; Omoto, A.C.M.; Wang, Z.; Li, X.; Carmo, J.M.D. Obesity, kidney dysfunction, and inflammation: Interactions in hypertension. Cardiovasc. Res. 2021, 117, 1859–1876. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vekic, J.; Stefanovic, A.; Zeljkovic, A. Obesity and Dyslipidemia: A Review of Current Evidence. Curr. Obes. Rep. 2023, 12, 207–222. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Almoyna Rifá, E.; Tomás-Gil, P.; Coll Villalonga, J.L.; Ramírez-Manent, J.I.; Martí-Lliteras, P.; López-González, A.A. Relationship between nonalcoholic fatty liver disease and liver fibrosis risk scales with overweight and obesity scales in 219,477 spanish workers. Acad. J. Health Sci. 2023, 38, 92–100. [Google Scholar] [CrossRef]
- Delker, E.; AlYami, B.; Gallo, L.C.; Ruiz, J.M.; Szklo, M.; Allison, M.A. Chronic Stress Burden, Visceral Adipose Tissue, and Adiposity-Related Inflammation: The Multi-Ethnic Study of Atherosclerosis. Psychosom. Med. 2021, 83, 834–842. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wu, Y.; Li, D.; Vermund, S.H. Advantages and Limitations of the Body Mass Index (BMI) to Assess Adult Obesity. Int. J. Environ. Res. Public Health 2024, 21, 757. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ashwell, M.; Gibson, S. Waist-to-height ratio as an indicator of ‘early health risk’: Simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open 2016, 6, e010159. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Costa, A.; Konieczna, J.; Reynés, B.; Martín, M.; Fiol, M.; Palou, A.; Romaguera, D.; Oliver, P. CUN-BAE Index as a Screening Tool to Identify Increased Metabolic Risk in Apparently Healthy Normal-Weight Adults and Those with Obesity. J. Nutr. 2021, 151, 2215–2225. [Google Scholar] [CrossRef] [PubMed]
- Torun, C.; Ankaralı, H.; Caştur, L.; Uzunlulu, M.; Erbakan, A.N.; Akbaş, M.M.; Gündüz, N.; Doğan, M.B.; Oğuz, A. Is Metabolic Score for Visceral Fat (METS-VF) a Better Index Than Other Adiposity Indices for the Prediction of Visceral Adiposity. Diabetes Metab. Syndr. Obes. 2023, 16, 2605–2615. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tripathi, H.; Singh, A.; Farheen Prakash, B.; Dubey, D.K.; Sethi, P.; Jadon, R.S.; Ranjan, P.; Vikram, N.K. The Metabolic Score for Visceral Fat (METS-VF) as a predictor of diabetes mellitus: Evidence from the 2011-2018 NHANES study. PLoS ONE 2025, 20, e0317913. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kuang, M.; Qiu, J.; Li, D.; Hu, C.; Zhang, S.; Sheng, G.; Zou, Y. The newly proposed Metabolic Score for Visceral Fat is a reliable tool for identifying non-alcoholic fatty liver disease, requiring attention to age-specific effects in both sexes. Front. Endocrinol. 2023, 14, 1281524. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Feng, L.; Chen, T.; Wang, X.; Xiong, C.; Chen, J.; Wu, S.; Ning, J.; Zou, H. Metabolism Score for Visceral Fat (METS-VF): A New Predictive Surrogate for CKD Risk. Diabetes Metab. Syndr. Obes. 2022, 15, 2249–2258. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tan, A.; Yang, S.; Pan, Y.; Lin, Q. Metabolism score for visceral fat (METS-VF): An innovative and powerful predictor of stroke. Arch. Med. Sci. 2024, 20, 1710–1714. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhou, X.; Xiang, J.; Zhang, S.; Yang, J.; Tang, Y.; Wang, Y. Investigating the role of the metabolic score for visceral Fat in assessing the prevalence of chronic kidney disease from the NHANES 1999-2018. Sci. Rep. 2025, 15, 2397. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jia, S.; Huo, X.; Zuo, X.; Zhao, L.; Liu, L.; Sun, L.; Chen, X. Association of metabolic score for visceral fat with all-cause mortality, cardiovascular mortality, and cancer mortality: A prospective cohort study. Diabetes Obes. Metab. 2024, 26, 5870–5881. [Google Scholar] [CrossRef] [PubMed]
- Kutscher, S.; Juang, C. Insomnia. Continuum 2023, 29, 1167–1187. [Google Scholar] [CrossRef] [PubMed]
- Riemann, D.; Benz, F.; Dressle, R.J.; Espie, C.A.; Johann, A.F.; Blanken, T.F.; Leerssen, J.; Wassing, R.; Henry, A.L.; Kyle, S.D.; et al. Insomnia disorder: State of the science and challenges for the future. J. Sleep Res. 2022, 31, e13604. [Google Scholar] [CrossRef] [PubMed]
- Palagini, L.; Geoffroy, P.A.; Miniati, M.; Perugi, G.; Biggio, G.; Marazziti, D.; Riemann, D. Insomnia, sleep loss, and circadian sleep disturbances in mood disorders: A pathway toward neurodegeneration and neuroprogression? A theoretical review. CNS Spectr. 2022, 27, 298–308. [Google Scholar] [CrossRef] [PubMed]
- Alimoradi, Z.; Jafari, E.; Broström, A.; Ohayon, M.M.; Lin, C.Y.; Griffiths, M.D.; Blom, K.; Jernelöv, S.; Kaldo, V.; Pakpour, A.H. Effects of cognitive behavioral therapy for insomnia (CBT-I) on quality of life: A systematic review and meta-analysis. Sleep Med. Rev. 2022, 64, 101646. [Google Scholar] [CrossRef] [PubMed]
- Morin, C.M.; Jarrin, D.C. Epidemiology of Insomnia: Prevalence, Course, Risk Factors, and Public Health Burden. Sleep Med. Clin. 2022, 17, 173–191. [Google Scholar] [CrossRef] [PubMed]
- Vgontzas, A.N.; Fernandez-Mendoza, J.; Lenker, K.P.; Basta, M.; Bixler, E.O.; Chrousos, G.P. Hypothalamic-pituitary-adrenal (HPA) axis response to exogenous corticotropin-releasing hormone (CRH) is attenuated in men with chronic insomnia. J. Sleep Res. 2022, 31, e13526. [Google Scholar] [CrossRef] [PubMed]
- Greenlund, I.M.; Carter, J.R. Sympathetic neural responses to sleep disorders and insufficiencies. Am. J. Physiol. Heart Circ. Physiol. 2022, 322, H337–H349. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Grimaldi, D.; Reid, K.J.; Papalambros, N.A.; Braun, R.I.; Malkani, R.G.; Abbott, S.M.; Ong, J.C.; Zee, P.C. Autonomic dysregulation and sleep homeostasis in insomnia. Sleep 2021, 44, zsaa274. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Manoharan, N.; Parasuraman, R.; Jayamurali, D.; Muthusamy, P.; Govindarajulu, S. Role of Thymoquinone on sleep restriction and its mitigating effect on leptin-mediated signaling pathway in rat brain. Mol. Biol. Rep. 2024, 51, 769. [Google Scholar] [CrossRef] [PubMed]
- McHill, A.W.; Hull, J.T.; Klerman, E.B. Chronic Circadian Disruption and Sleep Restriction Influence Subjective Hunger, Appetite, and Food Preference. Nutrients 2022, 14, 1800. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vidal, A.S.; de Campos Reis, N.F.; De Lorenzo, B.H.P.; Alvares-Saraiva, A.M.; Xander, P.; Novaes EBrito, R.R. Impact of sleep restriction in B-1 cells activation and differentiation. Immunobiology 2022, 227, 152280. [Google Scholar] [CrossRef] [PubMed]
- Itani, O.; Jike, M.; Watanabe, N.; Kaneita, Y. Short sleep duration and health outcomes: A systematic review, meta-analysis, and meta-regression. Sleep Med. 2017, 32, 246–256. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.S.; Aouad, R. The Effects of Insomnia and Sleep Loss on Cardiovascular Disease. Sleep Med. Clin. 2022, 17, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Duan, D.; Kim, L.J.; Jun, J.C.; Polotsky, V.Y. Connecting insufficient sleep and insomnia with metabolic dysfunction. Ann. N. Y. Acad. Sci. 2023, 1519, 94–117. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ramírez-Manent, J.I.; Tomás-Gil, P.; Coll-Villalonga, J.L.; Marti-Lliteras, P.; López-González, A.A.; Paublini, H. Influence of sociodemographic variables and tobacco consumption on the prevalence of atherogenic dyslipidemia and lipid triad in 418.343 spanish workers. Acad. J. Health Sci. 2023, 38, 84–89. [Google Scholar] [CrossRef]
- Bekar, C.; Goktas, Z. Validation of the 14-item mediterranean diet adherence screener. Clin. Nutr. ESPEN 2023, 53, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Mestre Font, M.; Busquets-Cortés, C.; Ramírez-Manent, J.I.; Vallejos, D.; Sastre Alzamora, T.; López-González, A.A. Influence of sociodemographic variables and healthy habits on the values of cardiometabolic risk scales in 386924 spanish workers. Acad. J. Health Sci. 2024, 39, 112–121. [Google Scholar] [CrossRef]
- Meh, K.; Jurak, G.; Sorić, M.; Rocha, P.; Sember, V. Validity and Reliability of IPAQ-SF and GPAQ for Assessing Sedentary Behaviour in Adults in the European Union: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 4602. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mestre-Font, M.; Busquets-Cortés, C.; Ramírez-Manent, J.I.; Tomás-Gil, P.; Paublini, H.; López-González, A.A. Influence of sociodemographic variables and healthy habits on the values of type 2 diabetes risk scales. Acad. J. Health Sci. 2024, 39, 99–106. [Google Scholar] [CrossRef]
- Manzar, M.D.; Jahrami, H.A.; Bahammam, A.S. Structural validity of the Insomnia Severity Index: A systematic review and meta-analysis. Sleep Med. Rev. 2021, 60, 101531. [Google Scholar] [CrossRef] [PubMed]
- Nagy, S.M.; Emert, S.E.; Leete, J.J.; Taylor, D.J.; Dietch, J.R.; Slavish, D.C.; Ruggero, C.J.; Kelly, K. Psychometric Evaluation of the Insomnia Severity Index in Nurses. Behav. Sleep Med. 2024, 22, 779–789. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gómez-Ambrosi, J.; Silva, C.; Catalán, V.; Rodríguez, A.; Galofré, J.C.; Escalada, J.; Valentí, V.; Rotellar, F.; Romero, S.; Ramírez, B.; et al. Clinical usefulness of a new equation for estimating body fat. Diabetes Care 2012, 35, 383–388. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Huang, J.C.; Huang, Y.C.; Lu, C.H.; Chuang, Y.S.; Chien, H.H.; Lin, C.I.; Chao, M.-F.; Chuang, H.-Y.; Ho, C.-K.; Wang, C.-L.; et al. Exploring the Relationship Between Visceral Fat and Coronary Artery Calcification Risk Using Metabolic Score for Visceral Fat (METS-VF). Life 2024, 14, 1399. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Figorilli, M.; Velluzzi, F.; Redolfi, S. Obesity and sleep disorders: A bidirectional relationship. Nutr. Metab. Cardiovasc. Dis. 2025, 35, 104014. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.L.; Wang, S.B.; Zhong, B.L.; Zhang, L.; Ungvari, G.S.; Ng, C.H.; Li, L.; Chiu, H.F.K.; Lok, G.K.I.; Lu, J.-P.; et al. The prevalence of insomnia in the general population in China: A meta-analysis. PLoS ONE 2017, 12, e0170772. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vgontzas, A.N.; Fernandez-Mendoza, J.; Liao, D.; Bixler, E.O. Insomnia with objective short sleep duration: The most biologically severe phenotype of the disorder. Sleep Med. Rev. 2013, 17, 241–254. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aielo, A.N.; Santos, R.B.; Giatti, S.; Silva, W.A.; Parise, B.K.; Cunha, L.F.; Souza, S.P.; Lotufo, P.A.; Bensenor, I.M.; Drager, L.F. Excessive daytime sleepiness, but not sleep apnea, sleep duration or insomnia, was associated with poor adherence to anti-hypertensive treatment: The ELSA-Brasil study. Sleep Med. 2023, 104, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.P.; McHill, A.W.; Cox, R.C.; Broussard, J.L.; Dutil, C.; da Costa, B.G.G.; Sampasa-Kanyinga, H.; Wright, K.P., Jr. The role of insufficient sleep and circadian misalignment in obesity. Nat. Rev. Endocrinol. 2023, 19, 82–97. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mestre-Font, M.; Busquets-Cortés, C.; Ramírez-Manent, J.I.; Tomás-Gil, P.; Paublini, H.; López-González, A.A. Influence of sociodemographic variables and healthy habits. Acad. J. Health Sci. 2024, 39, 27–35. [Google Scholar] [CrossRef]
- Dominguez, L.J.; Veronese, N.; Di Bella, G.; Cusumano, C.; Parisi, A.; Tagliaferri, F.; Ciriminna, S.; Barbagallo, M. Mediterranean diet in the management and prevention of obesity. Exp. Gerontol. 2023, 174, 112121. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Figares Vicioso, M.P.; del Barrio Fernández, J.L.; López-González, A.A.; Ramírez-Manent, J.I.; Vicente Herrero, M.T. Prevalencia de factores de riesgo cardiometabólico. Comparativa sector Comercio vs. Industria y variables asociadas. Acad. J. Health Sci. 2024, 39, 59–66. [Google Scholar] [CrossRef]
- Crönlein, T. Insomnia and obesity. Curr. Opin. Psychiatry 2016, 29, 409–412. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Wing, Y.K. Sex differences in insomnia: A meta-analysis. Sleep 2006, 29, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.H.; Cho, E.H.; Hur, J.; Shin, D. Association of Sleep Duration and Obesity According to Gender and Age in Korean Adults: Results from the Korea National Health and Nutrition Examination Survey 2007-2015. J. Korean Med. Sci. 2018, 33, e345. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aguiló Juanola, M.C.; López-González, A.A.; Tomás-Gil, P.; Paublini, H.; Tárraga-López, P.J.; Ramírez-Manent, J.I. Influence of tobacco consumption on the values of different overweight and obesity scales in 418,343 spanish people. Acad. J. Health Sci. 2023, 38, 111–117. [Google Scholar] [CrossRef]
- Selvamani, Y.; Pradhan, J.; Fong, J.H. Tobacco Use, Food Insecurity, and Low BMI in India’s Older Population. Nutrients 2024, 16, 3649. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).