Simple Summary
The aim of the study was to evaluate the outcomes of a cervical distraction–stabilization technique using an intervertebral anchored fusion device (C-LOX) combined with a locking compression plate (LCP plate) for the treatment of disc-associated cervical spondylomyelopathy (DA-CSM) in dogs, based on clinical and radiographical follow-up data. Thirteen dogs affected by DA-CSM were included in the study. After the surgical procedure, an improvement in neurological status was documented in 9/13 cases. This cervical distraction–stabilization technique seems to be a valuable surgical alternative to treat this canine pathology.
Abstract
Canine disc-associated cervical spondylomyelopathy (DA-CSM) is a form of caudal CSM, characterized by the compression of the spinal cord and nerve roots due to an intervertebral disc protrusion. It is more frequent in large canine breeds. A variety of surgical techniques has been proposed for DA-CSM. The aim of the study was to evaluate the outcomes of a cervical distraction–stabilization technique using an intervertebral anchored fusion device (C-LOX) combined with a locking compression plate (LCP plate) for the treatment of DA-CSM in dogs, based on clinical and radiographical follow-up data. Thirteen dogs affected by DA-CSM were included in the study. After the surgical procedure, an improvement in neurological status was documented in 9/13 cases. This cervical distraction–stabilization technique seems to be a valuable surgical alternative to treat this canine pathology.
1. Introduction
Caudal cervical spondylomyelopathy (CCSM), also known as wobbler syndrome, is a multifactorial disease affecting large and giant breed dogs that causes compression of the spinal cord and nerve roots [1,2,3,4,5,6,7,8,9].
This compression, caused by a combination of several factors such as degenerative and progressive disorders of the intervertebral disc, ligaments, and articular facet joints, leads to varying degrees of neurological dysfunction, cervical hyperesthesia, and pain [1,2,10,11] There are two recognized forms of CSM, which can occur separately or concurrently: disc-associated cervical spondylomyelopathy (DA-CSM) and osseous-associated cervical spondylomyelopathy (OA-CSM) [1,10,11,12,13,14,15]. Compression of the spinal cord due to DA-CSM typically occurs at the intervertebral disc spaces between the fifth (C5) and seventh cervical (C7) vertebrae in large breeds of dog such as Dobermann Pinschers [16]. Giant breeds of dog such as Great Danes also develop lesions of the more cranial vertebrae, including stenosis of both osseous and soft tissue origin [17]. This has also been observed in chondrodystrophic breeds such as Basset Hounds [18].
Various surgical approaches for the treatment of DA-CSM have been described. The proposed surgical techniques are commonly divided into direct decompressive (by a ventral or dorsal approach), indirect decompressive with motion preservation (total disc replacement by arthroplasty), and indirect decompressive without preservation of motion [19]. The latter involves vertebral distraction and stabilization in order to restore the intervertebral disc and foraminal width, and to stabilize the vertebral segment to prevent ongoing dynamic concussive injury to the spinal cord [10,11,20,21]. The most commonly decompressive procedures include fixation methods with or without the implantation of intervertebral spacers [22,23,24], alone or in combination with other devices, such as screws or ventrally applied locking plates [25,26,27,28,29,30,31,32,33,34]. Among the intervertebral devices described in the literature, C-LOX combines the effect of an intervertebral fusion cage with a ventral locking plate in a single implant. The features of C-LOX allow its easy and safe placement, decreasing the risk of iatrogenic injury by spinal cord penetration thanks to monocortical locking screws [22]. The main advantage of the additional ventral stabilization compared with other intervertebral devices is the reduced risk of ventral displacement with implant failure [22,35]. Despite this, the rate of complications such as loosening or breakage of the screws resulting in ventral displacement of the implant remains high [22,23]. Combining an interbody fusion cage with plate fixation has been found to reduce the displacement and subsidence of the implant, increase the construct’s rigidity [36], and increase the rate of spinal fusion in humans [37].
Considering the variety of treatments proposed for this pathology and the complications associated with implants, the aim of this study was to describe the surgical treatment of canine traction-responsive DA-CSM through a cervical distraction–stabilization technique using a spinal disk replacement implant associated with a ventral fixation plate, and to report the outcomes and complications in 13 dogs.
2. Materials and Methods
2.1. Inclusion Criteria
Between 2014 and 2018, 19 dogs were treated for traction-responsive DA-CSM. The patients included in this study underwent a surgical procedure of cervical distraction–stabilization using an intervertebral cage (C-LOX, Rita Leibinger Medical®, Muehlheim, BW, Germany) combined with a ventral plate (locking compression plate (LCP), De Puy Synthes®, West Chester, PA, USA).
Dogs affected by systemic diseases (n = 6) were excluded from the study, as well as subjects who failed to comply with the follow-ups planned after the surgical procedure (n = 20).
Thirteen client-owned dogs met the inclusion criteria. For each patient, informed consent was obtained.
The definite diagnosis of DA-CSM was confirmed by magnetic resonance imaging (MRI) using a Hitachi Airis Vento 0.3 Tesla machine (Hitachi Medical Corporation, Tokyo, Japan) which also allowed for surgical planning and implant selection. All dogs were sedated and placed in dorsal recumbency. The protocol of the MR examination included T2-weighted series (T2W; TR 4000 ms; TE 120 ms) in the sagittal and transverse planes and T1-weighted (T1W; TR 520 ms; TE 20 ms) pre- and postcontrast series in two transverse planes for intervertebral disc regions. Then T2-weighted images in sagittal and transverse planes were taken under traction of the patient’s neck to evaluate the dynamism of the cervical lesion.
Each dog underwent clinical, neurological, and radiographical examinations before and immediately after the surgical treatment and at 6 weeks after surgery (short-term follow-up). Radiographical examinations were performed under sedation to obtain optimal patient positioning. Clinical and neurological assessments were also performed at 6 months after surgery (medium-term follow-up). Biochemical analysis (complete blood count, azotemia, urea, transaminases, total proteins) was performed preoperatively.
Short-term neurological status was compared pre- and postoperatively, and dogs were rated as normal, improved with residual dysfunction, unchanged, or worsened. Neurological signs were graded according to a modified Frankel scale [38]: Grade 0, normal neurological examination; Grade 1, cervical pain during manipulation; Grade 2, mild pelvic limb ataxia with no proprioceptive deficits; Grade 3, mild ambulatory tetraparesis with proprioceptive deficits; Grade 4, severe ambulatory tetraparesis with proprioceptive deficits; Grade 5, non-ambulatory tetraparesis; Grade 6: tetraplegia.
Postoperative X-rays were performed in both orthogonal standard projections to assess the implant’s placement, stability, and integrity. Ventral vertebral fusion (non-interrupted new bone formation) was assessed at the short-term follow-up by radiographs.
Complications and relapses of the clinical signs were recorded. Complications were classified as major or minor, and whether or not they required additional treatment to resolve, respectively; an unacceptable permanent function or death were considered to be catastrophic complications. Moreover, complications were divided into intraoperative, short-term (6 weeks after surgery), and medium-term (6 months after surgery).
2.2. Surgical Technique
The anesthetic protocol included premedication with acepromazine (Prequillan, Fatro S.p.A., Bologna, Italy; 0.02–0.04 mg/kg) and methadone (Semfortan 10 mg/mL, Eurovet Animal Health B.V., Bladel, The Netherlands; 0.2 mg/kg IM), the induction of anesthesia with propofol (Propovet Multidose 10 mg/mL, Zoetis S.r.l., Rome, Italy; 4 mg/kg EV), and maintenance with sevoflurane (SevoFlo 100% 250 mL, Zoetis Belgium SA, Louvain-la-Neuve, Belgium; 3.5%). Intraoperative pain management with fentanyl (Fentadon, Eurovet Animal Health B.V., Bladel, The Netherlands; 2–4 mg/kg IV) at a constant rate of infusion was performed. During anesthesia, electrocardiography, heart and respiratory rate, end-tidal CO2, saturation of blood O2, and non-invasive blood pressure were recorded.
All dogs received antibiotic treatment with cefazolin (Cefazolina TEVA, Milan, Italy; 20 mg/kg) administered IV at the time of the induction of general anesthesia and then every 90 min until the end of the procedure.
After the induction of general anesthesia, each patient was positioned in dorsal recumbency with the caudal cervical spine raised about 5 cm above the table by a padded support, avoiding excessive extension. The thoracic limbs were caudally distracted and fixed to both sides of the chest. The maxilla was fixed to the operating table to maintain axial alignment and prevent movement during surgery. A standard ventral median approach to the cervical spine was performed [39]. A median longitudinal incision of the skin and subcutis was made, moving the various planes up to the muscular one. The sternohyoid and sternocephalic muscles were longitudinally incised to isolate the trachea and esophagus, which were moved laterally through the use of a retractor (e.g., a Balfour retractor), together with the large vessels and the recurrent nerves.
The intervertebral space involved was first localized through palpation of the ventral processes and subsequently exposed by incision of the longissimus colli muscle with the aid of a bipolar electrosurgical unit for hemostasis and a periosteal elevator. The vertebrae were carefully distracted by a Caspar retractor.
The intervertebral disc was incised and, with the help of a spinal disc broaching curette, all the remains of the nucleus pulposus were carefully removed from the intervertebral space, safeguarding the subchondral bone and the dorsal part of the fibrous ring. After the endplate chondrectomy had been performed, the correct fit was verified by inserting the test spacer, fixed to the special positioning rod. Once the optimal size was determined, the trial spacer was removed and replaced by the corresponding C-LOX device (Rita Leibinger GmbH & Co. KG, Mühlheim/Donau, Germany) (Figure 1 and Figure 2). The distractor was removed, allowing for vertebral repositioning and, if necessary, the “ears” were slightly bent for optimal bone contact. Implants of different sizes, with variations in height (14 mm, 16 mm, 18 mm, 20 mm), thickness (4 mm, 5 mm, 6 mm, 7 mm, 8 mm), and width (8 mm, 10 mm, 12 mm) were used. Two caudal and two cranial 1.8 mm locking screws were incorporated into the plate by the means of slightly flexible “ears” featuring threaded, locking screw holes. The 1.8 mm screws were of several lengths, including 10 mm, 12 mm, 14 mm, 16 mm, 18 mm, 20 mm, 22 mm, and 24 mm.

Figure 1.
Titanium cage (C-LOX, Rita Leibinger®) used in the surgical technique: intraoperative photo.
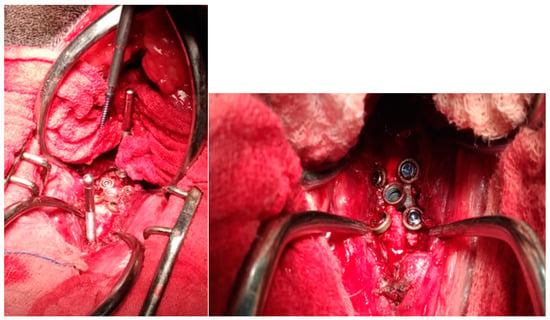
Figure 2.
Application of the titanium cage (C-LOX, Rita Leibinger®): intraoperative photo.
The threaded drill guide was attached to the implant, and a dedicated 1.8 mm drill bit was used to drill holes for the locking, self-drilling cortex screws. This tip forms a unit with the screw’s centering sleeve, limiting the penetration to the ventral cortex and eliminating the risk of iatrogenic medullary damage. The four screws were then inserted into the appropriate holes, concluding the anchoring of the implant to the vertebral bodies. An autologous cancellous bone graft (ACBG) was then removed from the proximal humerus and placed along the ventral surface of the disc space and the adjacent vertebral bodies. Finally, to ensure the greater stability of the implant, the ventral fixation plate (LCP plate, locking compression plate, Synthes®) was applied (Figure 3). Paired 7-hole (2.7 mm, 67 mm in length) LCP plates and monocortical locking screws were utilized for all patients. The plates were aligned on the underlying vertebrae, and three screws on each vertebral body were placed in the respective holes. This left only one open hole above the C-LOX device.
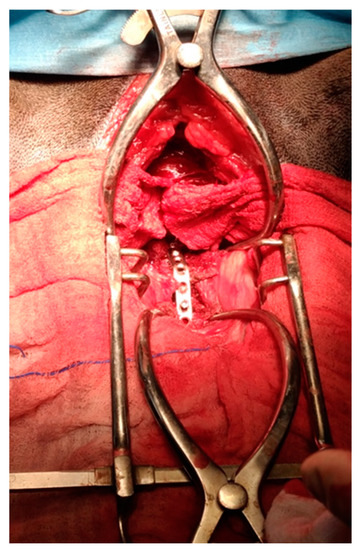
Figure 3.
Application of the locking compression plate (Synthes®).
The procedure was closed routinely. The mean duration of surgery was 1.9 h (range: 1.5–2.6 h).
During the first 36 h postoperatively, each dog received IV cefazolin twice daily. Postoperative care and analgesia were adapted to the neurological status and clinical course of the individual patient. For analgesia, methadone at 0.2 mg/kg intramuscularly was administered as needed, and no later than 5 days.
Anti-inflammatory drugs (prednisolone, Vetsolone, PROVET S.A., Bayer, Milan, Italy; 0.5–1 mg/kg) were orally administered for 10–15 days postoperatively; antibiotic (cefadroxil, Cefa-Cure Tabs cpr, MSD Animal Health S.r.l., Milan, Italy; 20 mg/kg SID os) and gastroprotective treatments (omeprazole, 1 mg/kg and sucralfate (50 mg/kg) were applied for 10 and 20 days, respectively. Finally, oral supplementation with palmitoylethanolamide (PEA) and quercetin (Alevica®, Innovet, Saccolongo—Padua, Italy) SID was prescribed for at least 20 days.
All patients underwent physiotherapy sessions to accelerate motor rehabilitation, as previously reported [34]. The owners were given clear and strict instructions to follow during the postoperative period. These include maintaining strict confinement of the patient in a confined space, avoiding sudden exertion or jumps from any height, and providing as few walks as possible, of short duration and always with a support harness.
At 6 weeks, the brace was removed, and control cervical radiographs were performed. If the radiographic follow-up showed positive results, a gradual increase in walking frequency and length was allowed for another 6 weeks before resuming unrestricted activity.
2.3. Statistical Analysis
The calculation software Prism 9.0 (Graph Pad Software, San Diego, CA, USA) was used to perform the statistical analysis. A 2-tailed, paired Student’s t-test was used to compare the preoperative neurologic scores with postoperative and 6-week and 6-month outcomes. Significance was established for all tests at p < 0.05.
3. Results
3.1. Demographics
The study group included 13 dogs with ages ranging from 6 to 10 years, and nine males (70%) and four females (30%) (Table 1). The weight ranged from 27 kg to 63 kg, with a mean value of 40 ± 11 kg). Dogs were fed with commercial food and led both indoor and outdoor lifestyles.

Table 1.
Signalment and neurological scores in 13 dogs with CCSM.
3.2. Preoperative Assessment
Diagnosis was achieved with radiographs and MRI.
The MRI examination showed that the main lesion was located at C5–C6 in 10 (77%) dogs and at C6–C7 in 3 (33%) dogs (Figure 4).
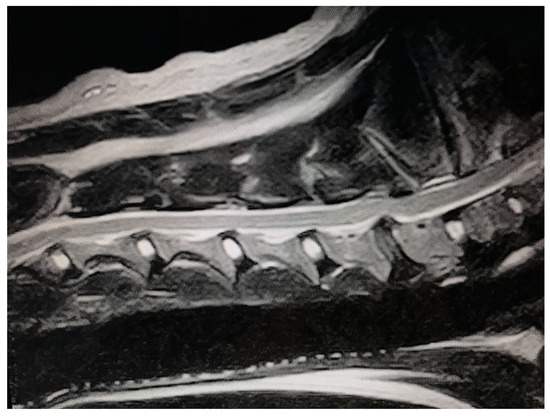
Figure 4.
Sagittal T2-weighted MR image of a Swiss Shepherd (male, 94 months).
At the level of C7, moderate vertebral tipping was observed. At the level of C6–C7, a bulging intervertebral disc was also noted, with a reduction in the diameter of the dorsal–ventral canal at the space affected.
The most frequently observed clinical signs were hindlimb weakness that started months before and gradually worsened, ambulatory tetraparesis with mild neurological deficits, and, in one case, non-ambulatory tetraparesis. Hindlimb manifestations were more severe than forelimb ones in all patients. On clinical examination, all patients showed marked atrophy of the supra- and infraspinatus muscles, which made the spine of the scapula easily palpable.
Due to proprioceptive deficits, the skin on the back of the hind and front legs exhibited abrasions caused by continuous rubbing against the ground. No consistent abnormalities were found in the complete blood counts or the serum’s biochemical profiles.
On neurological examination, 9/13 dogs (70%) showed a posture with a lower neck, 12/13 dogs (93%) showed ambulatory tetraparesis with a short and stiff gait of the forelimbs and an dysmetrical gait of the hindlimbs (two-neuron gait), proprioceptive deficits in all limbs, hyporeflexia of the flexor reflex of the hindlimbs, and normal spinal reflexes (flexor and patellar) in the hindlimbs. One dog (1/13, 7%) showed non-ambulatory tetraparesis (Dog 7). All patients showed normal cranial nerves. Neck pain was often present.
3.3. Postoperative Assessment
Figure 5 shows the radiographic study performed before and after the surgical procedure in a treated dog.
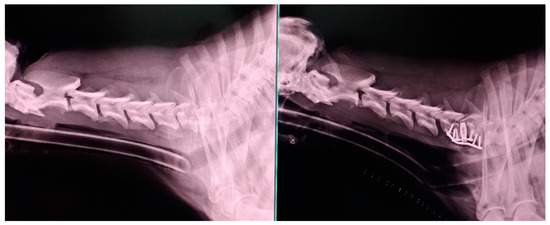
Figure 5.
Radiographic images of a Swiss Shepherd (male, 94 months): lateral view of the cervical spine before and after surgical treatment. The correct application of the titanium cage and plate can be observed.
In one dog (Dog 13), detachment of the fixation plate occurred within some days of surgery. A second surgery was performed to remove the plate and replace it with a new one. No complications occurred during the replacement procedure. The new plate was the same as the others.
The neurologic score of four dogs was unchanged immediately postoperatively, and improved in nine dogs.
The neurologic scores at 6 weeks after surgery were significantly different from the preoperative scores (paired t-test, p = 0.0003; t = 5.017, df = 12). The neurologic score of 9/13 dogs (70%) were improved at 6 weeks postoperatively. Five dogs showed cervical pain with or without mild to moderate pelvic limb ataxia. A neurologic score of 0 was noted in 4/13 dogs at 6 weeks postoperatively. Out of all cases, 3/13 (23%) dogs had no neurological improvement, and 1/13 (7%) had a worsening of the symptoms (Dog 7), deteriorating from severe non-ambulatory tetraparesis preoperatively to tetraplegia immediately postoperatively.
At the medium-term examination, 10 dogs were neurologically normal without signs of pain. One dog had mild hindlimb ataxia without signs of pain. A significant difference between the neurologic scores at 6 months and 6 weeks postoperatively was reported (p = 0.0028; t = 3.742, df = 12).
No vertebral fusion occurred in all dogs at medium-term follow-up. Minor complications were seen in only one dog, showing the loosening of a screw, which was not associated with neurological deterioration (Figure 6).
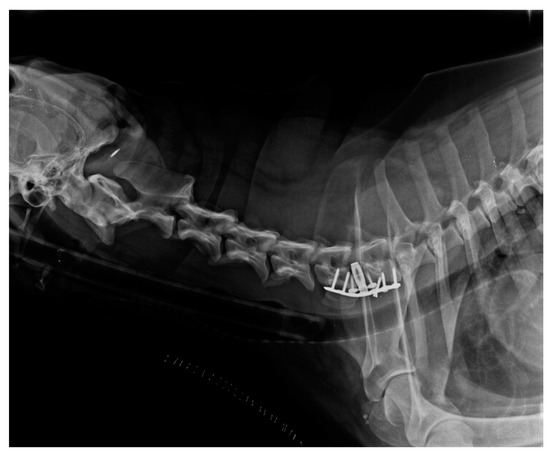
Figure 6.
Short-term radiographic image of a treated dog: the loosening of a screw can be observed.
No complications that caused unsolvable permanent damage or for which euthanasia was required were observed.
4. Discussion
Caudal cervical spondylomyelopathy (CCSM) is a canine progressive disease characterized by degenerative changes that, through direct compression of the spinal cord and the surrounding vascular and nerve structures, can potentially lead to severe neurological damage and permanent disability [40].
Identifying the early signs and providing an early diagnosis and effective treatment before the development of irreversible spinal cord damage are essential to maintaining canine quality of life.
DA-CSM, frequently identified in large-breed dogs [1], can cause non-traction-responsive (static lesions) and traction-responsive (dynamic lesions) cord compressions [41]. The ideal management for traction-responsive DA-CSM is still controversial. Conservative treatment, despite initial improvement, may lead to further progression of the clinical signs [6,14,41].
When a dynamic lesion has to be managed, the surgical procedure should have the purpose of reducing neurological deficits and relieving the compression of the spinal cord, stabilizing the cervical vertebrae [1,41].
The surgical techniques proposed for the treatment of DA-CSM in dogs reported positive results in 70–90% of DA-CSM cases [5,16,22,24,25,27,28,29,30,32,33,34].
Recently, the use of intervertebral body cages with or without adjuvant ventral plates to realize an interbody arthrodesis has become a more popular technique for dogs [24,27,28,29,30,32,33,34,40].
In the choice of a surgical technique for the treatment of DA-CSM, the potential risks of complications such as implant failure and subsidence should be considered [16,22,24,27,28,29,30,31,32,33,41]. Iatrogenic damage is only one of the several potential risks of distraction–fusion surgery, along with postoperative neurological deterioration, penetration of the implants into the neural tissue, subsidence of the implant, and adjacent segment disease (ASD or domino lesions). Early implant failure with loss of distraction before stabilization is another very common complication [25,30,42]. Intervertebral cages also have a high risk of ventral dislocation, and further stabilization may be required, using monocortical screws [27,43] or spinal locking plate systems, which are widely used in human medicine [11].
The C-LOX spacer used in this study combines an intervertebral spacer with a conventional screw fixation mechanism, and it was designed to stabilize and restore the function of the cervical spine. Despite fixation of the implant with monocortical screws, a recent study evaluating its efficacy in 37 dogs reported screws loosening as the most common complication, making revision surgeries with a ventral plate necessary. The screws alone may not have been able to withstand the high torsional forces occurring in this region of the cervical spine, mostly concentrated at the junction between the head and the shaft, resulting in loosening or breakage of the screws and ventral dislocation of the implant [22].
In our study, to minimize the rate of complications of the C-LOX device used alone, such as screw loosening, breakage, and ventral cage dislocation, and to ensure the increased rigidity and stability of the implant, we combined this intervertebral device with a ventral fixation plate system.
Combining a fixation plate with a distraction device as a cage has been found to improve the rate of intervertebral fusion in humans [37], with the rate of the non-union of bone grafts being up to 26% without the use of a cervical plate [44]; moreover, locking plate fixation has become a widely accepted method in the treatment of DA-CSM [22].
In our study, vertebral body fusion was not evident in any dog at medium-term follow-up, in accordance with previous studies reporting that serial radiographs over a longer period may be required to accurately assess bone bridging [23,32].
The effects of this combination of an intervertebral spacer and a fixation system with ventral plates have already been documented in two previous studies, showing both short- and long-term positive clinical and radiographical outcomes [24,34]. Despite some complications, such as loosening of the implant, plate fixation promotes better stability, ensuring good construct rigidity [34].
Based on our findings, the use of C-LOX device in combination with a ventral locking compression plate may be a viable surgical treatment for DA-CSM. The surgical procedure was relatively simple, the duration was considered to be reasonable, and the duration of hospitalization was comparable with other techniques. No substantial intraoperative complications were detected, and only one case had a displacement of the angular stability plate. Nine dogs (70%) had neurological improvements 6 months after surgery.
Our study presents some limitations, such as the lack of a control group and the small number of dogs enrolled. Further studies are needed to confirm the efficacy of this methodology in a larger sample, although the enrollment of treated dogs could be made difficult by the high costs of the procedures.
Moreover, a radiological assessment at medium-term follow-up in order to evaluate the status of the implant and fusion was not performed due to a lack of permission from the owners to sedate their dogs again. This condition may have underestimated both the degree of improvement and the incidence of implant complications, although clinical and neurological evaluations of the treated dogs showed significant neurological improvements and the absence of clinical signs.
5. Conclusions
The clinical outcomes of the 13 dogs reported here were good. The application of the C-LOX device in association with fixation plates and ACBG led to satisfactory results for the treatment of DA-CCSM, as demonstrated by the clinical and radiographic findings. Our results provide useful information to help surgeons broaden their choices of surgical techniques for the treatment of DA-CCSM.
Author Contributions
Conceptualization, F.M. and G.B.; methodology, M.T. and D.F.; validation, D.M., V.F. and N.M.I.; formal analysis, G.L.C.; investigation, D.F.; data curation, S.D.P.; writing—original draft preparation, M.T. and D.F.; writing—review and editing, M.T., C.D.I. and S.D.P.; supervision, F.M. and C.D.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
All treatments, housing, and animal care were carried out in accordance with the standards recommended by European Directive 2010/63/EU for animal experiments. The work described in this manuscript involved the use of non-experimental (owned or unowned) animals. Established and internationally recognized high standards (“best practice”) of veterinary clinical care for the individual patients were always followed. Ethical approval from a committee was therefore not specifically required.
Informed Consent Statement
Written informed consent was obtained from the owner or legal custodian of all animals described in this work for all procedures undertaken. No animals or people are identifiable within this publication; therefore, additional informed consent for publication was not required. Written informed consent was obtained from the patients’ owners to publish this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- da Costa, R.C. Cervical spondylomyelopathy (wobbler syndrome) in dogs. Vet. Clin. N. Am. Small Anim. Pract. 2010, 40, 881–913. [Google Scholar] [CrossRef] [PubMed]
- De Decker, S.; da Costa, R.C.; Volk, H.A.; Van Ham, L.M. Current insights and controversies in the pathogenesis and diagnosis of disc-associated cervical spondylomyelopathy in dogs. Vet. Rec. 2012, 171, 531–537. [Google Scholar] [CrossRef]
- Breit, S.; Künzel, W. Osteological features in pure-bred dogs predisposing to cervical spinal cord compression. J. Anat. 2001, 199 Pt 5, 527–537. [Google Scholar] [CrossRef] [PubMed]
- De Decker, S.; Gielen, I.M.; Duchateau, L.; Van Soens, I.; Bavegems, V.; Bosmans, T.; van Bree, H.J.; Van Ham, L.M. Low-field magnetic resonance imaging findings of the caudal portion of the cervical region in clinically normal Doberman Pinschers and foxhounds. Am. J. Vet. Res. 2010, 71, 428–434. [Google Scholar] [CrossRef] [PubMed]
- De Risio, L.; Muñana, K.; Murray, M.; Olby, N.; Sharp, N.J.; Cuddon, P. Dorsal laminectomy for caudal cervical spondylomyelopathy: Postoperative recovery and long-term follow-up in 20 dogs. Vet. Surg. 2002, 31, 418–427. [Google Scholar] [CrossRef]
- da Costa, R.C.; Parent, J.M.; Holmberg, D.L.; Sinclair, D.; Monteith, G. Outcome of medical and surgical treatment in dogs with cervical spondylomyelopathy: 104 cases (1988–2004). J. Am. Vet. Med. Assoc. 2008, 233, 1284–1290. [Google Scholar] [CrossRef]
- da Costa, R.C.; Echandi, R.L.; Beauchamp, D. Computed tomography myelographic findings in dogs with cervical spondylomyelopathy. Vet. Radiol. Ultrasound. 2012, 53, 64–70. [Google Scholar] [CrossRef]
- Murthy, V.D.; Gaitero, L.; Monteith, G. Clinical and magnetic resonance imaging (MRI) findings in 26 dogs with canine osseous-associated cervical spondylomyelopathy. Can. Vet. J. 2014, 55, 169–174. [Google Scholar]
- Gasper, J.A.; Rylander, H.; Stenglein, J.L.; Waller, K.R., 3rd. Osseous-associated cervical spondylomyelopathy in dogs: 27 cases (2000–2012). J. Am. Vet. Med. Assoc. 2014, 244, 1309–1318. [Google Scholar] [CrossRef]
- Lewis, M.; Olby, N.J.; Sharp, N.J.; Early, P. Long-term effect of cervical distraction and stabilization on neurological status and imaging findings in giant breed dogs with cervical stenotic myelopathy. Vet. Surg. 2013, 42, 701–709. [Google Scholar] [CrossRef]
- McKee, W.M.; Pink, J.J.; Gemmill, T.J. Cement plug technique for the management of disc-associated cervical spondylopathy in 52 Dobermann Pinscher dogs. Vet. Comp. Orthop. Traumatol. 2016, 29, 195–201. [Google Scholar] [PubMed]
- Lewis, D. Cervical spondylomyelopathy (“wobbler” syndrome) in the dog: A study based on 224 cases. J. Small Anim. Pract. 1989, 30, 657–665. [Google Scholar] [CrossRef]
- da Costa, R.C.; Parent, J.M.; Partlow, G.; Dobson, H.; Holmberg, D.L.; Lamarre, J. Morphologic and morphometric magnetic resonance imaging features of Doberman Pinschers with and without clinical signs of cervical spondylomyelopathy. Am. J. Vet. Res. 2006, 67, 1601–1612. [Google Scholar] [CrossRef] [PubMed]
- De Decker, S.; Bhatti, S.F.; Duchateau, L.; Martlé, V.A.; Van Soens, V.; Van Meervenne, S.A.E.; Saunders, J.H.; Van Hamet, L.M. Clinical evaluation of 51 dogs treated conservatively for disc-associated wobbler syndrome. J. Small Anim. Pract. 2009, 50, 136–142. [Google Scholar] [CrossRef]
- De Decker, S.; Gielen, I.M.; Duchateau, L.; Saunders, J.H.H.; van Bree, H.J.J.; Polis, I.; Van Ham, L.M.L. Magnetic resonance imaging vertebral canal and body ratios in Doberman Pinschers with and without diskassociated cervical spondylomyelopathy and clinically normal English foxhounds. Am. J. Vet. Res. 2011, 2, 1496–1504. [Google Scholar] [CrossRef]
- Rusbridge, C.; Wheeler, S.; Torrington, A.; Pead, M.J.; Carmichael, S. Comparison of two surgical techniques for the management of cervical spondylomyelopathy in dobermanns. J. Small Anim. Pract. 1998, 39, 425–431. [Google Scholar] [CrossRef]
- Lipsitz, D.; Levitski, R.; Chauvet, A.E.; Berry, W.L. Magnetic resonance imaging features of cervical stenotic myelopathy in 21 dogs. Vet. Radiol. Ultrasound. 2001, 42, 20–27. [Google Scholar] [CrossRef]
- Palmer, A.; Wallace, C.; Margaret, E. Deformation of cervical vertebrae in Basset hounds. Vet. Rec. 1967, 80, 430–433. [Google Scholar] [CrossRef]
- Driver, C.J.; Lopez, V.; Walton, B.; Jones, D.; Fentem, R.; Tomlinson, A.; Rose, J. Instrumented cervical fusion using patient specific end-plate conforming interbody devices with a micro-porous structure in nine dogs with disk-associated cervical spondylomyelopathy. Front. Vet. Sci. 2023, 10, 1208593. [Google Scholar] [CrossRef]
- Jeffery, N.D.; McKee, W.M. Surgery for disc-associated wobbler syndrome in the dog—An examination of the controversy. J. Small Anim. Pract. 2001, 42, 574–581. [Google Scholar] [CrossRef]
- Ramos, R.M.; da Costa, R.C.; Oliveira, A.L.; Kodigudla, M.K.; Goel, V.K. Effects of flexion and extension on the diameter of the caudal cervical vertebral canal in dogs. Vet. Surg. 2015, 44, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Rohner, D.; Kowaleski, M.P.; Schwarz, G.; Forterre, F. Short-term clinical and radiographical outcome after application of anchored intervertebral spacers in dogs with disc-associated cervical spondylomyelopathy. Vet. Comp. Orthop. Traumatol. 2019, 2, 158–164. [Google Scholar] [CrossRef] [PubMed]
- King, J.C.; Corfield, G.S.; Mouatt, J.G.; Kan, C.Y.; Moses, P.A. Surgical management and long-term outcome of dogs with cervical spondylomyelopathy with an anchored intervertebral titanium device. Aust. Vet. J. 2020, 98, 156–163. [Google Scholar] [CrossRef]
- De Decker, S.; Caemaert, J.; Tshamala, M.C.; Gielen, I.M.V.L.; Van Bree, H.J.J.; Bosmans, T.; Wegge, B.; Van Ham, L.M.L. Surgical treatment of disk-associated wobbler syndrome by a distractable vertebral titanium cage in seven dogs. Vet. Surg. 2011, 40, 544–554. [Google Scholar] [CrossRef]
- McKee, W.M.; Sharp, N.J. Cervical spondylopathy. In Textbook of Small Animal Surgery, 3rd ed.; Slatter, D.H., Ed.; Saunders: Philadelphia, PA, USA, 2003; pp. 1180–1193. [Google Scholar]
- Sharp, N.J.; Wheeler, S.J. Cervical spondylomyelopathy. In Small Animal Spinal Disorders Diagnosis and Surgery, 2nd ed.; Sharp, N.J.H., Wheeler, S.J., Eds.; Elsevier Mosby: Philadelphia, PA, USA, 2005; pp. 211–246. [Google Scholar]
- Voss, K.; Steffen, F.; Montavon, P.M. Use of the ComPact UniLock System for ventral stabilization procedures of the cervical spine: A retrospective study. Vet. Comp. Orthop. Traumatol. 2006, 19, 21–28. [Google Scholar]
- Hettlich, B.F.; Allen, M.J.; Glucksman, G.S.; Fosgate, G.T.; Litsky, A.S. Effect of an intervertebral disk spacer on stiffness after monocortical screw/polymethylmethacrylate fixation in simulated and cadaveric canine cervical vertebral columns. Vet. Surg. 2014, 43, 988–994. [Google Scholar] [CrossRef]
- Shamir, M.H.; Chai, O.; Loeb, E. A method for intervertebral space distraction before stabilization combined with complete ventral slot for treatment of disc-associated wobbler syndrome in dogs. Vet. Surg. 2008, 37, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Trotter, E.J. Cervical spine locking plate fixation for treatment of cervical spondylotic myelopathy in large breed dogs. Vet. Surg. 2009, 38, 705–718. [Google Scholar] [CrossRef]
- Adrega Da Silva, C.; Bernard, F.; Bardet, J.F. Caudal cervical arthrodesis using a distractable fusion cage in a dog. Vet. Comp. Orthop. Traumatol. 2010, 23, 209–213. [Google Scholar]
- Solano, M.A.; Fitzpatrick, N.; Bertran, J. Cervical distraction-stabilization using an intervertebral spacer screw and string-of pearl (SOPTM) plates in 16 dogs with disc-associated Wobbler Syndrome. Vet. Surg. 2015, 44, 627–641. [Google Scholar] [CrossRef]
- Steffen, F.; Voss, K.; Morgan, J.P. Distraction-fusion for caudal cervical spondylomyelopathy using an intervertebral cage and locking plates in 14 dogs. Vet. Surg. 2011, 40, 743–752. [Google Scholar] [CrossRef]
- Reints Bok, T.E.; Willemsen, K.; van Rijen, M.H.; Grinwis, G.C.; Tryfonidou, M.A.; Meij, B.P. Instrumented cervical fusion in nine dogs with caudal cervical spondylomyelopathy. Vet. Surg. 2019, 48, 1287–1298. [Google Scholar] [CrossRef]
- Schöllhorn, B.; Bürki, A.; Stahl, C.; Howard, J.; Forterre, F. Comparison of the biomechanical properties of a ventral cervical intervertebral anchored fusion device with locking plate fixation applied to cadaveric canine cervical spines. Vet. Surg. 2013, 42, 825–831. [Google Scholar] [CrossRef] [PubMed]
- Bergman, R.L.; Levine, J.M.; Coates, J.R.; Bahr, A.; Hettlich, B.F.; Kerwin, S.C. Cervical spinal locking plate in combination with cortical ring allograft for a one level fusion in dogs with cervical spondylotic myelopathy. Vet. Surg. 2008, 37, 530–536. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, M.G.; Haid, R.W., Jr.; Subach, B.R.; Barnes, B.; Rodts, G.E., Jr. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 2002, 50, 229–238. [Google Scholar] [PubMed]
- Olby, N.; Griffith, E.; Levine, J.; CANSORT SCI Investigators. Comparison of Gait Assessment Scales in Dogs with Spinal Cord Injury from Intervertebral Disc Herniation. J. Neurotrauma 2020, 37, 1991–1998. [Google Scholar] [CrossRef] [PubMed]
- Platt, S.R.; da Costa, R.C. Cervical vertebral column and spinal cord. In Veterinary Surgery, 2nd ed.; Johnston, S.A., Tobias, K.M., Eds.; Elsevier Health Sciences: St Louis, MO, USA, 2017; pp. 465–467. [Google Scholar]
- Bonelli, M.d.; da Costa, L.B.d.S.B.C.; da Costa, R.C. Magnetic resonance imaging and neurological findings in dogs with disc-associated cervical spondylomyelopathy: A case series. BMC Vet. Res. 2021, 17, 145. [Google Scholar] [CrossRef]
- Falzone, C.; Tranquillo, V.; Gasparinetti, N. Comparison of Two Surgical Techniques for the Treatment of Canine Disc Associated-Cervical Spondylomyelopathy. Front. Vet. Sci. 2022, 9, 880018. [Google Scholar] [CrossRef]
- Bruecker, K.A.; Seim, H.B., 3rd; Withrow, S.J. Clinical evaluation of three surgical methods for treatment of caudal cervical spondylomyelopathy of dogs. Vet. Surg. 1989, 18, 197–203. [Google Scholar] [CrossRef]
- Pitzen, T.; Barbier, D.; Tintinger, F.; Steudel, W.I.; Strowitzki, M. Screw fixation to the posterior cortical shell does not influence peak torque and pullout in anterior cervical plating. Eur. Spine J. 2002, 11, 494–499. [Google Scholar]
- Alvarez, J.A.; Hardy, R.W. Anterior cervical discectomy for one-and two-level cervical disc disease: The controversy surrounding the question of whether to fuse, plate, or both. Crit. Rev. Neurosurg. 1999, 9, 234–251. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).